Abstract
Ebolavirus is a hemorrhagic fever virus associated with high mortality. Although much has been learned about the viral lifecycle and pathogenesis, many questions remain about virus entry. We recently showed that binding of the receptor binding region (RBR) of the ebolavirus glycoprotein (GP) and infection by GP pseudovirions increase on cell adhesion independently of mRNA or protein synthesis. One model to explain these observations is that, on cell adhesion, an RBR binding partner translocates from an intracellular vesicle to the cell surface. Here, we provide evidence for this model by showing that suspension 293F cells contain an RBR binding site within a membrane-bound compartment associated with the trans-Golgi network and microtubule-organizing center. Consistently, trafficking of the RBR binding partner to the cell surface depends on microtubules, and the RBR binding partner is internalized when adherent cells are placed in suspension. Based on these observations, we reexamined the claim that lymphocytes, which are critical for ebolavirus pathogenesis, are refractory to infection because they lack an RBR binding partner. We found that both cultured and primary human lymphocytes (in suspension) contain an intracellular pool of an RBR binding partner. Moreover, we identified two adherent primate lymphocytic cell lines that bind RBR at their surface and strikingly, support GP-mediated entry and infection. In summary, our results reveal a mode of determining viral entry by a membrane-trafficking event that translocates an RBR binding partner to the cell surface, and they suggest that this process may be operative in cells important for ebolavirus pathogenesis (e.g., lymphocytes and macrophages).
Keywords: filovirus, negative strand RNA virus, virus receptor, lymphocytes, macrophages
Ebolavirus (EBOV), a class A priority pathogen that causes hemorrhagic fever with extremely high mortality rates, is a negative-strand RNA virus of the family Filoviridae. Its genome encodes eight proteins, including one glycoprotein (GP) that is both necessary and sufficient for host-cell binding and entry (1–3). GP is a heavily glycosylated protein consisting of a receptor binding subunit (GP1) and a class I fusion subunit (GP2). GP1 contains a mucin-like domain that is dispensable for in vitro infection and a receptor binding region (RBR; residues 57–149) (3–6). Four lysine residues within the RBR (K95, K114, K115, and K140) are important for receptor binding and infection (3, 6). RBR binding to the surface of permissive cells is saturable and protease-sensitive, and it correlates with the ability to be infected (6), supporting the notion that permissive cells express a proteinaceous RBR receptor (2). Although several cell-surface proteins enhance infection, a definitive RBR receptor has not yet been identified.
EBOV infects a wide array of cell types, with the notable exceptions of B and T lymphocytes, natural killer cells, and neutrophils (1, 2, 7). This tropism has been hypothesized to be caused by expression of a receptor(s) in permissive, but not in nonpermissive, cells (1, 4, 6). In support of this proposal, none of the cultured lymphocytes that have been analyzed bind RBR at their surface (4, 6), and they are not infected by particles bearing EBOV GP (1, 2, 4, 6). However, all of the cultured lymphocytes that have been analyzed grow in suspension, and we recently presented evidence that suspension cells in general bind only low levels of RBR at the cell surface and are poorly infected by EBOV pseudovirions. Both 293F (epithelial-derived) and THP1 (monocyte/macrophage-like) cells grown in suspension bind less RBR at the cell surface and are less efficiently infected than when they are grown as adherent cells. The acquisition of RBR binding to the cell surface occurs in parallel with cell adhesion and spreading (within hours of plating), and it does not require mRNA or protein synthesis (8). Hence, there is a strong relationship between binding of the RBR of EBOV GP to the cell surface and susceptibility to infection.
There are at least two hypotheses to explain the adhesion-dependent increase in RBR binding to the cell surface. One is that suspension cells contain an internal store of an RBR binding partner (hereafter referred to as RBR receptor) that is translocated to the cell surface on adhesion. A second is that adhesion induces a posttranslational modification of an RBR receptor already at the cell surface to a form that is competent to bind RBR. In this study, we provide evidence for the translocation model for the cell adhesion-dependent increase in ebolavirus GP binding and entry in epithelial and monocyte/macrophage cells. We then provide evidence that, contrary to current thinking, lymphocytes contain an RBR receptor and moreover, that adherent lymphocytes (i.e., as they would be in tissues) display the RBR receptor at the cell surface and can be infected by particles bearing ebolavirus GP.
Results
There Is an Intracellular Pool of RBR Receptor in 293F Cells Grown in Suspension.
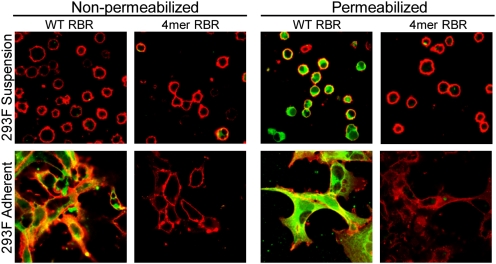
If 293F cells cultured in suspension are allowed to adhere to tissue-culture dishes, they acquire the ability to bind 3- to 5-fold more RBR at their surface without the need for new mRNA or protein synthesis (8). As described above, one of two major hypotheses to explain these observations is that a pool of RBR receptor is held internally when the cells are in suspension but traffics to the cell surface on adhesion. To begin to test this hypothesis, we asked whether 293F cells in suspension contain an intracellular pool of RBR receptor. Cells were either left intact or treated with saponin (to permeabilize all cellular membranes) and then monitored by immunofluorescence for binding of a wild-type (WT) RBR-Fc construct (6). A binding-deficient mutant RBR-Fc construct (4mer RBR; mutated at the four critical lysine residues described above and in ref. 6) was used as a negative control. Consistent with our flow-cytometry analysis (8), adherent, but not suspension, 293F cells bound WT RBR at the cell surface (Fig. 1). However, permeabilization of the cells revealed the presence of an intracellular RBR binding site in the suspension 293F cells. No significant binding was detected in any of the samples with the binding-defective 4mer RBR mutant.
Fig. 1.
There is a pool of an RBR receptor inside suspension 293F cells. Adherent and suspension 293F cells were fixed, and their plasma membranes were labeled with DiD (red); they were either left intact (nonpermeabilized) or permeabilized with saponin and then incubated with Fc-conjugated WT or binding-deficient (4mer mutant) RBR (500 nM) followed by protein A, Alexa Fluor 488 (green). Fluorescent images were captured on a Nikon Eclipse TE2000 confocal microscope using a 100× objective, and the figure was produced as described in Materials and Methods.
Given the importance of macrophages to EBOV pathogenesis, we extended our analysis to monocytes (macrophage progenitors) and macrophages. Consistent with our flow-cytometry analysis (8), THP1 cells grown in suspension (monocyte-like) did not bind RBR at the cell surface when analyzed by immunofluorescence (Fig. S1). However, as seen for suspension 293F cells, intracellular RBR binding was observed when the suspension (monocyte-like) THP1 cells were permeabilized. In contrast, phorbol-12-myristate 13-acetate-(PMA-)-treated THP1 cells (adherent and macrophage-like) bound WT RBR at the cell surface as well as intracellularly (Fig. S1). In complete concordance, primary human monocytes (which are suspension cells) only displayed intracellular RBR binding, whereas primary human macrophages (which are adherent) bound RBR at the cell surface as well as intracellularly (Fig. S1).
Intracellular RBR Binding Site Faces the Lumen of a Membrane-Bound Compartment Associated with the Trans-Golgi Network.
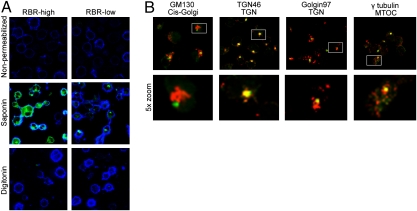
The most likely route for an internal pool of RBR receptor to traffic to the cell surface on adhesion would be through exocytic fusion of a membrane-bound vesicle with the plasma membrane. In this manner, the interior of the vesicle would be exposed at the cell surface, and if, as we hypothesize, the receptor is membrane-associated with a lumenally disposed binding site, the RBR binding site would then be exposed at the cell surface. To test this hypothesis, we used differential membrane permeabilization. Although saponin permeabilizes all cellular membranes, digitonin, when used at a proper concentration, only permeabilizes the plasma membrane (9, 10). If the RBR binding site was lumenally disposed, it would be rendered accessible by saponin but not by digitonin. Consistent with our hypothesis, RBR binding was only seen in saponin-permeabilized samples of suspension 293F cells (Fig. 2A). The selectivity of differential permeabilization was confirmed using antibodies against specific cellular markers (Fig. S2A). Examination of the samples at lower laser intensity revealed a distinct punctum of RBR binding in each saponin-permeabilized cell (Fig. 2A, RBR-low).
Fig. 2.
The RBR binding site in suspension 293F cells faces the lumen of a membrane-bound compartment. (A) Suspension 293F cells were fixed, and their plasma membranes were labeled with DiD (pseudocolored blue). Cells were examined for RBR binding under three conditions: intact (nonpermeabilized), permeabilized with saponin (permeabilizes all membranes), or permeabilized with 1 μM digitonin (permeabilizes only the plasma membrane; intracellular membranes remain intact). RBR binding (green) was examined at both high (RBR-high) and low (RBR-low) laser intensity, the latter to focus on the brightest staining. Controls for selective permeabilization from the same experiment are shown in Fig. S2A. (B) Suspension 293F cells were fixed, permeabilized with saponin, and incubated with Fc-conjugated RBR (500 nM) and anti-rabbit Fab 488 (green) and the indicated marker antibody (red). RBR binding was analyzed at low laser intensity to focus on the area of brightest staining. Lower shows a 5× enlarged view of a single (boxed) cell from the panel directly above. Fluorescent images were captured and processed as in Fig. 1. Images represent findings from multiple experiments in which at least five fields were examined per sample.
To localize the compartment that contains the bulk of the RBR receptor in suspension 293F cells, we assessed colocalization of the RBR binding site with markers for specific intracellular organelles. There was no significant colocalization with early endosomes, late endosomes, lysosomes, or recycling endosomes (Fig. S2B). In contrast, the RBR binding site was found near the cis-Golgi and closely associated with the microtubule-organizing center (MTOC) and two trans-Golgi network (TGN) markers, TGN46 and Golgin97 (Fig. 2B). Collectively, these results indicate that suspension 293F cells contain an intracellular pool of an RBR receptor whose binding site faces the interior of membrane-bound vesicles associated with the TGN.
Translocation of RBR Receptor to the Cell Surface on Adhesion Depends on Microtubules and Internalization of RBR Receptor on Detachment Depends on Actin Filaments.
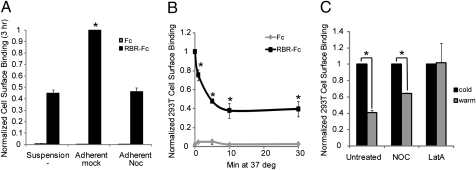
Several proteins traffic from the TGN to the cell surface in a regulated manner (11–13), and most do so along microtubules (14, 15). Because the intracellular pool of RBR receptor was found near the MTOC (Fig. 2B), we asked if the increase in RBR binding to the cell surface seen when 293F cells transition from suspension to adherent growth depends on microtubules. To assess this, suspension 293F cells were treated with nocodazole (Noc), which depolymerizes microtubules, and were then allowed to adhere to fibronectin-coated tissue-culture plates for 1 h (Fig. S3A) or 3 h (Fig. 3A) in the continued presence of Noc. As seen in Fig. 3A and Fig. S3A, Noc prevented the adhesion-dependent increase in RBR binding to the cell surface. These results strongly suggest that, on cell adhesion, vesicles carrying RBR receptor move along microtubules and then fuse with the plasma membrane, thereby delivering more RBR receptor to the cell surface. We next asked if the RBR receptor is internalized from the cell surface on cellular detachment. To examine this possibility, 293F cells which were taken from suspension culture and allowed to adhere for 18 h (Fig. S3B) or 293T cells, which are adherent (Fig. 3B), were analyzed for RBR binding to the cell surface after the cells were detached and held for various times in suspension at 37 °C. For both cell lines, we observed a time-dependent decrease in RBR binding to the cell surface, resulting in ∼60% less surface binding after 30 min in suspension. Internalization of RBR receptor from the cell surface on cellular detachment was prevented by treatment with latrunculin A (Fig. 3C), and thus it seems to be more dependent on the actin cytoskeleton than on the integrity of microtubules. Together, the results in Figs. 1–3 strongly support a model in which binding of RBR to the cell surface (and susceptibility to infection) is modulated by adhesion-dependent membrane trafficking of an RBR receptor.
Fig. 3.
The cell adhesion-dependent differential of RBR binding to the cell surface depends on microtubules and actin filaments. (A) Suspension 293F cells were mock treated or treated with nocodazole (Noc; 10 μM) for 1 h and then examined under three conditions: continued growth in suspension or plated for 3 h on fibronectin-coated dishes in the presence or absence of 10 μM nocodazole. Cells were then chilled, lifted by pipetting with cold PBS++, and assessed for RBR binding as described previously (assay done at 4 °C) (6, 8). Data bars represent the average of triplicate samples from one experiment. Statistical significance compared with the suspension mock-treated sample was determined by Student t test (*P < 0.004). (B) Adherent 293T cells were lifted as in A at 4 °C and then incubated at 37 °C (to allow membrane trafficking). At the indicated times, cells were chilled and then examined for RBR binding as described in A. (C) Adherent 293T cells were left untreated or treated with 10 μM Noc or 1 μM latrunculin A (LatA) for 1 h. All samples were then lifted at 4 °C and either kept at 4 °C (cold) or incubated at 37 °C for 30 min (warm) in the presence or absence of inhibitor. Cells were then examined for RBR binding as above. In B and C, data points represent the averages of at least three experiments (performed in duplicate) normalized to the level of RBR binding to the surface of cells kept on ice for the duration of the experiment (labeled 0 min in B and cold in C). Error bars represent SD of the normalized data. Statistical significance compared with the 0 min/cold sample was determined by Student t test (*P < 0.05).
Suspension Lymphocytes Contain a Similar Intracellular Pool of RBR Receptor.
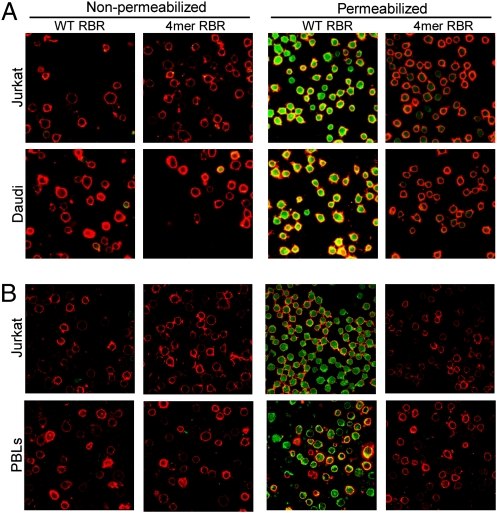
Given that suspension 293F cells (Fig. 1) and (suspension) monocytes (Fig. S1) contain an intracellular pool of RBR receptor, we next asked if suspension lymphocytes do as well. As seen in Fig. 4A, there is an intracellular pool of RBR receptor in suspension T (Jurkat) and B (Daudi) lymphocytes, cultured cells that are resistant to EBOV GP-mediated infection (1, 4, 8) and unable to bind RBR at the cell surface (4, 6, 8). As seen in suspension 293F cells, the RBR binding site within suspension Jurkat T lymphocytes is associated with the TGN and MTOC (Fig. S4). In a separate experiment, we identified an internal pool of RBR receptor in human primary blood lymphocytes (PBLs) (Fig. 4B). These results suggest that the block to EBOV binding in suspension lymphocytes is not because of the lack of an RBR receptor but rather to its sequestration inside the cells.
Fig. 4.
There is an internal pool of RBR receptor in suspension lymphocytes. (A) Jurkat T and Daudi B lymphocytes, which grow in suspension, were fixed, their plasma membranes were labeled with DiD (red) and either left intact (nonpermeabilized) or permeabilized with saponin, and then were incubated with Fc-conjugated RBR (500 nM) and anti-rabbit Fab 488 (green). Images were captured and processed as in Fig.1. (B) Human primary blood lymphocytes (PBLs) and Jurkat cells were processed as in A except that the γ level of the green channel was increased to 1.3 (for all images in B) to compensate for lower laser intensity settings on the microscope (percent laser power and gain). Findings represent results from two or more experiments examining at least five fields per sample.
Adherent B Lymphocytes Bind RBR at the Cell Surface and Are Susceptible to EBOV GP-Mediated Entry and Infection.
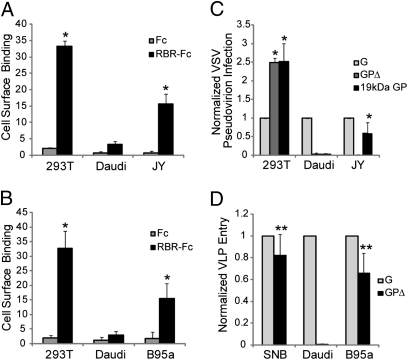
We next tested the ability of two lines of adherent B lymphocytes, a marmoset B lymphoblastoid line (B95a cells) and a human B lymphoblastoid line (JY cells), to bind RBR at the cell surface. As shown in Fig. 5 A and B, both adherent B lymphocytic cell lines bound significantly more RBR at the cell surface than suspension Daudi B lymphocytes. Fig. S5A shows RBR binding to the surface of JY cells using immunofluorescence. We, therefore, asked if JY or B95a (adherent) B lymphocytes are susceptible to EBOV GP-mediated entry and infection. In a first experiment, 293T, Daudi, and JY cells were incubated with vesicular stomatitis virus (VSV) pseudovirions bearing either VSV G, a mucin domain-deleted version of EBOV GP (GPΔ), or a proteolytically primed version of EBOV GP (19 kDa GP) (6, 16, 17); particles with 19 kDa GP are less dependent on endosomal cathepsins for entry than particles bearing GP or GPΔ (5, 16, 17). As seen in Fig. 5C, although all of the cells analyzed were infected by pseudovirions bearing VSV G (albeit to varying levels), only 293T cells were infected by pseudovirions bearing GPΔ. Interestingly, JY cells were infected by pseudovirions bearing the primed 19-kDa form of GP (∼59% of the level seen with pseudovirions bearing VSV G), whereas Daudi cells were resistant (<0.3% of that seen with pseudovirions bearing VSV G).
Fig. 5.
Adherent B lymphocytes bind RBR at the cell surface and are susceptible to EBOV-GP mediated entry and infection. (A) Adherent 293T and JY cells were lifted by pipetting with cold PBS++, whereas suspension Daudi cells were collected and chilled to 4 °C. Cells were then incubated with Fc-conjugated RBR (200 nM) followed by anti-rabbit Fab 488. Rabbit Fc was used as a negative control. Cell-surface binding was analyzed by flow cytometry. (B) 293T, Daudi, and B95a cells were examined for RBR cell-surface binding as in A. Data bars in A and B represent the average percent of cells showing RBR binding at their surface from three independent experiments (each with duplicate samples). Error bars represent SD. Statistical significance compared with RBR binding to the surface of Daudi cells was determined by Student t test (*P < 0.015). (C) 293T, Daudi, and JY cells were infected with VSV pseudovirions bearing either VSV G, EBOV GPΔ, or EBOV 19-kDa GP (6, 16). The average percent of cells infected with pseudovirions bearing VSV G, EBOV GPΔ, and EBOV 19-kDa GP were, respectively: 293T: 21%, 51%, and 53%; Daudi: 12%, 0%, and 0%; JY: 19%, 0%, and 10%. B95a cells are resistant to WT VSV infection (Fig. S5C) and thus, could not be examined in this experiment. (D) SNB19 (SNB), Daudi, and B95a cells were spinoculated with VLPs bearing VSV G or EBOV GPΔ as described in Materials and Methods. The average percent of cells showing entry with VLPs bearing VSV G and EBOV GPΔ were, respectively: SNB19: 91% and 75%; Daudi: 33% and 0%; B95a: 24% and 15%. JY cells could not be examined in this experiment because of high levels of background signal (Fig. S5D). In C and D, bars represent the average percent of cells infected (C) or showing entry (D) normalized to infection or entry by particles bearing VSV G in the same cell type from at least three experiments each with duplicate samples. Error bars represent SD of the normalized data. Statistical significance compared with infection or entry in Daudi cells was determined by Student t test (*P < 0.03; **P < 0.0002).
The observation that JY cells were infected by pseudovirions bearing the primed 19-kDa form of GP but not with pseudovirions bearing GPΔ suggested that the JY cells can bind and internalize GP-bearing particles but have insufficient cathepsins to prime GP (18). Because (adherent) B95a B lymphocytes contain a higher level of cathepsins B+L activity than JY cells (Fig. S5B), we asked if B95a cells are susceptible to entry mediated by GPΔ. To do this, we used EBOV viral-like particles (VLPs) bearing GPΔ and containing VP40 tagged with β-lactamase (19). The VLPs are more analogous, morphologically, to bona fide EBOV than the smaller VSV pseudovirions (20, 21). As seen in Fig. 5D, VLPs bearing VSV G entered all of the cell types examined. Consistent with the VSV pseudovirion experiments (Fig. 5C), VLPs bearing EBOV GPΔ did not enter the nonpermissive (suspension) Daudi B lymphocytes (<1% of cells). Interestingly, however, VLPs bearing GPΔ entered the adherent B95a B lymphocytes (∼65% of the level seen with VLPs bearing VSV G). A similar ratio of infectivity between VLPs bearing GPΔ and those bearing VSV G was seen for (permissive and adherent) SNB19 cells. The results in Fig. 5 indicate that, contrary to current notions, particles bearing EBOV GP can bind to, enter, and infect lymphocytes, as long as the lymphocytes are adherent and contain the requisite fusion-activation machinery.
Discussion
It was previously thought that lymphocytes lack a receptor for ebolavirus (1, 2, 4, 6). Based on our studies showing enhanced binding of the RBR of EBOV GP to the cell surface and enhanced infection of adherent compared with suspension 293F (epithelial derived) and THP1 (monocyte/macrophage-like) cells (8), we hypothesized that suspension cells, including lymphocytes and monocytes, contain an intracellular pool of RBR receptor that translocates to the cell surface on cell adhesion. Indeed, in this study, we identified an internal pool of RBR receptor in all suspension cells analyzed, including cultured and primary monocytes and lymphocytes. Using 293F cells, we showed that, on adhesion, the internal pool of RBR receptor translocates to the cell surface, and that, reciprocally, when adherent cells are detached and held in suspension, surface RBR receptor is internalized. Finally, we documented, contrary to expectations, that adherent lymphocytes are susceptible to EBOV GP-mediated entry. Our findings introduce a means of determining viral entry by cell adhesion-dependent membrane-trafficking, and indicate that EBOV can bind to and enter adherent lymphocytes, a finding that may bear on the pathogenesis of this deadly virus.
Control of EBOV Entry by RBR Receptor Translocation.
Our results reveal a means of controlling viral entry wherein a cell can express an entry receptor but be refractory to infection if the receptor is sequestered intracellularly. We found that all suspension cells analyzed contain a pool of RBR receptor (associated with the TGN and MTOC) and that this pool can translocate to the cell surface on cell adhesion. Our findings with 293F cells are most consistent with a model in which cell adhesion-dependent translocation of an RBR receptor occurs through microtubule-dependent movement of vesicles containing a lumenally oriented RBR binding site from the TGN region to the plasma membrane. On exocytic fusion, RBR binding sites are exposed at the cell surface. Conversely, when adherent cells are detached and held in suspension, the pool of RBR receptor is rapidly internalized from the surface through an actin-dependent process. Lipid rafts (plasma-membrane microdomains marked by cholera toxin B and aerolysin) undergo similar adhesion- and microtubule-dependent cell surface exposure and reciprocally, detachment- and actin-dependent internalization from the cell surface (22). One difference is that lipid rafts are associated with Rab11-positive recycling endosomes in cells in suspension (22), whereas we did not see colocalization of RBR binding sites with Rab11. Like several other proteins (11–13), the RBR receptor may, instead, traffic directly from the TGN to the cell surface.
The process that we have uncovered of adhesion-/deadhesion-dependent RBR receptor trafficking to and from the cell surface likely plays a role in EBOV pathogenesis. During live EBOV infections, macrophages are one of the first cell types infected. Although there have been reports that monocytes (macrophage progenitors) can be infected by ebolavirus (23, 24), neither the precise differentiation status of the infected cells nor the extent of their infection compared with tissue macrophages was directly ascertained. Moreover, one study found that the levels of ebolavirus entry were markedly higher in primary macrophages compared with primary monocytes derived from the same donors (25). We observed that primary (adherent) human macrophages bind more RBR at their surface than freshly isolated primary human monocytes and that PMA-treated (adherent) THP1 macrophage-like cells bind more RBR and are more robustly infected than untreated (monocyte-like) THP1 cells. These findings suggest that monocyte differentiation and the accompanying acquisition of adhesive characteristics result in increased levels of RBR receptor at the cell surface and that this process contributes to the high susceptibility of macrophages to EBOV infection.
Adherent B Lymphocytes Are Susceptible to GP-Mediated Entry and Infection.
To date, there is no convincing evidence for replication of EBOV in lymphocytes. Correspondingly, we (and others) have reported that suspension lymphocytes do not bind EBOV RBR at the cell surface efficiently and are refractory to EBOV GP-mediated entry and infection (1, 2, 4, 6, 8). In contrast, we report in this study that adherent lymphocytes bind significant levels of RBR at the cell surface and importantly, are susceptible to EBOV GP-mediated entry. A trademark of lymphocytes is their high degree of flexibility in terms of cell adhesion. In vivo unstimulated lymphocytes are nonadherent. However, in response to specific cytokines and chemokines, lymphocytes increase the cell-surface expression and activation status of adhesion molecules (e.g., integrins), leading to adhesion with neighboring cells and extracellular matrix components (26). Interestingly, EBOV-infected macrophages, primary targets of EBOV infection, produce many of the cytokines and chemokines that promote the adhesiveness of lymphocytes (23, 27). Lymphocytes also become adhesive when they form immunological synapses with antigen-presenting cells such as macrophages and dendritic cells (28). Our findings suggest that adherent lymphocytes may present a receptor for the RBR of EBOV GP at the cell surface, which would provide a means for EBOV to interact with lymphocytes in tissues.
During early stages of primate infections by EBOV, large numbers of lymphocytes undergo apoptosis (7, 24, 29). The mechanism for this massive bystander apoptosis is not well-understood. Several studies have implicated factors secreted by EBOV-infected dendritic cells and macrophages (7, 23, 24, 27, 29), suggesting an indirect effect of the virus. Alternatively, it has been suggested that there is a more direct role for EBOV in the induction of lymphocyte apoptosis (7, 30). We recognize three ways in which our observations may contribute to lymphocyte apoptosis. In one scenario, binding of EBOV GP (or shed GP) to a receptor on the surface of adherent lymphocytes may trigger apoptosis. Consistent with this, a 17-residue synthetic peptide from the immunosuppressive region in GP2 has been shown to trigger apoptosis of primary lymphocytes in culture (30). In a second scenario, EBOV may not only bind to adherent lymphocytes, but it may also enter them, consistent with our observation that EBOV VLPs can enter an adherent lymphocytic line. In this case, delivery of the EBOV core to the cytoplasm might ignite a signaling cascade that promotes apoptosis. In a third scenario, it is possible that EBOV particles not only enter but also initiate a low level of replication in certain adherent lymphocytes. These cells may then undergo apoptosis before replication can be detected, perhaps because of impaired antiapoptotic mechanisms.
In summary, this study introduces a mode of determining viral entry: by a cell adhesion-dependent membrane-trafficking event that increases the level of a viral receptor at the cell surface. Moreover, our studies suggest that this mechanism may be in play in cell types such as macrophages and lymphocytes, which are critical to the pathogenesis and fatal-disease progression of ebolavirus infections.
Materials and Methods
SI Materials and Methods describes sources of reagents and details. RBR-Fc binding to (intact) cells was measured by flow cytometry essentially as described previously (4, 6, 8). RBR-Fc binding was monitored by immunofluorescence (to intact cells or cells permeabilized with either saponin or digitonin) as described in SI Materials and Methods. Production of VSV pseudovirions (bearing VSV G or EBOV GP, GPΔ, or 19-kDa GP) and their use to infect cells was as described previously (2, 6, 16). EBOV viral-like particles containing VP40-β-lactamase were produced as described in refs. 19 and 31 and were used to infect cells as described in SI Materials and Methods.
Supplementary Material
Acknowledgments
We thank colleagues for reagents (SI Materials and Methods) and Edward Park for excellent technical assistance. D.D., K.L.S., and C.J.S. were supported in part by Training Grants 5T32 AI07046 and 5T32 AI055432 to the University of Virginia. The work was supported by Research Grants from the National Institutes of Health: U54 AI057168 (to C.C.B.) and A122470 and U54 AI057168 (to J.M.W.).
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1008509107/-/DCSupplemental.
References
- 1.Wool-Lewis RJ, Bates P. Characterization of Ebola virus entry by using pseudotyped viruses: Identification of receptor-deficient cell lines. J Virol. 1998;72:3155–3160. doi: 10.1128/jvi.72.4.3155-3160.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Takada A, et al. A system for functional analysis of Ebola virus glycoprotein. Proc Natl Acad Sci USA. 1997;94:14764–14769. doi: 10.1073/pnas.94.26.14764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee JE, Saphire EO. Ebolavirus glycoprotein structure and mechanism of entry. Future Virol. 2009;4:621–635. doi: 10.2217/fvl.09.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuhn JH, et al. Conserved receptor-binding domains of Lake Victoria marburgvirus and Zaire ebolavirus bind a common receptor. J Biol Chem. 2006;281:15951–15958. doi: 10.1074/jbc.M601796200. [DOI] [PubMed] [Google Scholar]
- 5.Kaletsky RL, Simmons G, Bates P. Proteolysis of the Ebola virus glycoproteins enhances virus binding and infectivity. J Virol. 2007;81:13378–13384. doi: 10.1128/JVI.01170-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dube D, et al. The primed ebolavirus glycoprotein (19-kilodalton GP1,2): Sequence and residues critical for host cell binding. J Virol. 2009;83:2883–2891. doi: 10.1128/JVI.01956-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Geisbert TW, et al. Apoptosis induced in vitro and in vivo during infection by Ebola and Marburg viruses. Lab Invest. 2000;80:171–186. doi: 10.1038/labinvest.3780021. [DOI] [PubMed] [Google Scholar]
- 8.Dube D, et al. Cell adhesion promotes Ebola virus envelope glycoprotein-mediated binding and infection. J Virol. 2008;82:7238–7242. doi: 10.1128/JVI.00425-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Diaz R, Stahl PD. Digitonin permeabilization procedures for the study of endosome acidification and function. Methods Cell Biol. 1989;31:25–43. doi: 10.1016/s0091-679x(08)61600-3. [DOI] [PubMed] [Google Scholar]
- 10.Eckhardt M, Gotza B, Gerardy-Schahn R. Membrane topology of the mammalian CMP-sialic acid transporter. J Biol Chem. 1999;274:8779–8787. doi: 10.1074/jbc.274.13.8779. [DOI] [PubMed] [Google Scholar]
- 11.Martin S, Reaves B, Banting G, Gould GW. Analysis of the co-localization of the insulin-responsive glucose transporter (GLUT4) and the trans Golgi network marker TGN38 within 3T3-L1 adipocytes. Biochem J. 1994;300:743–749. doi: 10.1042/bj3000743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chklovskaia E, et al. Cell-surface trafficking and release of flt3 ligand from T lymphocytes is induced by common cytokine receptor gamma-chain signaling and inhibited by cyclosporin A. Blood. 2001;97:1027–1034. doi: 10.1182/blood.v97.4.1027. [DOI] [PubMed] [Google Scholar]
- 13.Gustafson CE, et al. Recycling of AQP2 occurs through a temperature- and bafilomycin-sensitive trans-Golgi-associated compartment. Am J Physiol Renal Physiol. 2000;278:F317–F326. doi: 10.1152/ajprenal.2000.278.2.F317. [DOI] [PubMed] [Google Scholar]
- 14.Hirschberg K, et al. Kinetic analysis of secretory protein traffic and characterization of golgi to plasma membrane transport intermediates in living cells. J Cell Biol. 1998;143:1485–1503. doi: 10.1083/jcb.143.6.1485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Toomre D, Keller P, White J, Olivo JC, Simons K. Dual-color visualization of trans-Golgi network to plasma membrane traffic along microtubules in living cells. J Cell Sci. 1999;112:21–33. doi: 10.1242/jcs.112.1.21. [DOI] [PubMed] [Google Scholar]
- 16.Schornberg K, et al. Role of endosomal cathepsins in entry mediated by the Ebola virus glycoprotein. J Virol. 2006;80:4174–4178. doi: 10.1128/JVI.80.8.4174-4178.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chandran K, Sullivan NJ, Felbor U, Whelan SP, Cunningham JM. Endosomal proteolysis of the Ebola virus glycoprotein is necessary for infection. Science. 2005;308:1643–1645. doi: 10.1126/science.1110656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schornberg KL, et al. Alpha5beta1-integrin controls ebolavirus entry by regulating endosomal cathepsins. Proc Natl Acad Sci USA. 2009;106:8003–8008. doi: 10.1073/pnas.0807578106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tscherne DM, Manicassamy B, García-Sastre A. An enzymatic virus-like particle assay for sensitive detection of virus entry. J Virol Methods. 2010;163:336–343. doi: 10.1016/j.jviromet.2009.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jasenosky LD, Neumann G, Lukashevich I, Kawaoka Y. Ebola virus VP40-induced particle formation and association with the lipid bilayer. J Virol. 2001;75:5205–5214. doi: 10.1128/JVI.75.11.5205-5214.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Licata JM, Johnson RF, Han Z, Harty RN. Contribution of ebola virus glycoprotein, nucleoprotein, and VP24 to budding of VP40 virus-like particles. J Virol. 2004;78:7344–7351. doi: 10.1128/JVI.78.14.7344-7351.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Balasubramanian N, Scott DW, Castle JD, Casanova JE, Schwartz MA. Arf6 and microtubules in adhesion-dependent trafficking of lipid rafts. Nat Cell Biol. 2007;9:1381–1391. doi: 10.1038/ncb1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ströher U, et al. Infection and activation of monocytes by Marburg and Ebola viruses. J Virol. 2001;75:11025–11033. doi: 10.1128/JVI.75.22.11025-11033.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Geisbert TW, et al. Pathogenesis of Ebola hemorrhagic fever in primate models: Evidence that hemorrhage is not a direct effect of virus-induced cytolysis of endothelial cells. Am J Pathol. 2003;163:2371–2382. doi: 10.1016/S0002-9440(10)63592-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yonezawa A, Cavrois M, Greene WC. Studies of ebola virus glycoprotein-mediated entry and fusion by using pseudotyped human immunodeficiency virus type 1 virions: Involvement of cytoskeletal proteins and enhancement by tumor necrosis factor alpha. J Virol. 2005;79:918–926. doi: 10.1128/JVI.79.2.918-926.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kinashi T. Intracellular signalling controlling integrin activation in lymphocytes. Nat Rev Immunol. 2005;5:546–559. doi: 10.1038/nri1646. [DOI] [PubMed] [Google Scholar]
- 27.Hensley LE, Young HA, Jahrling PB, Geisbert TW. Proinflammatory response during Ebola virus infection of primate models: possible involvement of the tumor necrosis factor receptor superfamily. Immunol Lett. 2002;80:169–179. doi: 10.1016/s0165-2478(01)00327-3. [DOI] [PubMed] [Google Scholar]
- 28.Dustin ML. Cell adhesion molecules and actin cytoskeleton at immune synapses and kinapses. Curr Opin Cell Biol. 2007;19:529–533. doi: 10.1016/j.ceb.2007.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reed DS, Hensley LE, Geisbert JB, Jahrling PB, Geisbert TW. Depletion of peripheral blood T lymphocytes and NK cells during the course of ebola hemorrhagic Fever in cynomolgus macaques. Viral Immunol. 2004;17:390–400. doi: 10.1089/vim.2004.17.390. [DOI] [PubMed] [Google Scholar]
- 30.Yaddanapudi K, et al. Implication of a retrovirus-like glycoprotein peptide in the immunopathogenesis of Ebola and Marburg viruses. FASEB J. 2006;20:2519–2530. doi: 10.1096/fj.06-6151com. [DOI] [PubMed] [Google Scholar]
- 31.Manicassamy B, Rong L. Expression of Ebolavirus glycoprotein on the target cells enhances viral entry. Virol J. 2009;6:75–89. doi: 10.1186/1743-422X-6-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.