Abstract
Human Gnathostoma hispidum infection is extremely rare in the world literature and has never been reported in the Republic of Korea. A 74-year-old Korean man who returned from China complained of an erythematous papule on his back and admitted to our hospital. Surgical extraction of the lesion and histopathological examination revealed sections of a nematode larva in the deep dermis. The sectioned larva had 1 nucleus in each intestinal cell and was identified as G. hispidum. The patient recalled having eaten freshwater fish when he lived in China. We designated our patient as an imported G. hispidum case from China.
Keywords: Gnathostoma hispidum, gnathostome, case report, deep dermis
INTRODUCTION
Gnathostomiasis is a rare, infectious disease caused by migration of nematode larvae of the genus Gnathostoma in the human skin, subcutaneous tissues, or internal organs [1]. Most human cases were reported from Thailand and Japan until the 1980s [2]. Since then, its geographical distribution has extended to East Asia and America [2]. This disease is now highlighted because it is not only an emerging disease [1,3] but also an imported disease which affects overseas travelers [4,5]. Human infections can occur by consuming undercooked freshwater fish or other animals, including reptiles and birds, containing infective third-stage larvae, or by drinking water containing copepods infected with second-stage larvae [6]. The larvae never develop into adults in humans, and humans are regarded as a paratenic host [6]. Various domestic and wild animals, including dogs, cats, pigs, leopards, and tigers serve, as the definitive hosts [6].
A total of 13 species of Gnathostoma have been reported worldwide, and 5 of them are known to infect humans; G. spinigerum, G. hispidum, G. doloresi, G. nipponicum, and G. binucleatum [7,8]. Among them, G. spinigerum is the species that most frequently infects humans, and G. hispidum, G. doloresi, G. nipponicum, or G. binucleatum infections are rare [7,8]. G. hispidum, one of the rare Gnathostoma species infecting humans, was first found in wild pigs and swine in Hungary in 1872, and then in swine in Austria, Germany, and Rumania [6]. Later, G. hispidum was discovered in Asian countries, including China, Taiwan, Thailand, the Philippines, Malaysia, and Vietnam [6]. In Japan, G. hispidum was not reported until the 1980s, when a sporadic outbreak of presumed G. hispidum infection, due to ingestion of raw loaches, Misgurnus anguillicaudatus, imported from China, occurred [9]. Six parasitologically-proven cases of G. hispidum infection have since been reported in Japan [10-13] and 1 case was diagnosed in a French who traveled to Southeast Asia [4].
In the Republic of Korea, G. hispidum larvae were reported in a snake of unknown geographical origin purchased in Pusan [14]. However, it is uncertain whether the life cycle of G. hispidum is indigenously maintained in Korea [14]; the snake might have been the one which was imported from China [14]. Regarding human G. hispidum infection, neither indigenous nor imported cases were reported in the Republic of Korea. Here we report for the first time an imported G. hispidum case in a Korean man returning from China.
CASE RECORD
The patient, a 74-year-old man, was born in Cheongdo, Gyeonsangbuk-do (province), Republic of Korea, and lived there until 10 years of age when his family moved to Jilin, China. He lived in Jilin, China for almost 60 years, when he returned permanently to Korea in December 2003. He noted an erythematous skin lesion on his back skin 1-2 years before he moved to Korea. The lesion moved within limited regions during this time and persisted. He was seen at the Department of Plastic and Reconstructive Surgery, Inje University Ilsan Paik Hospital in December, 2007. He had no history of hypertension or diabetes mellitus. On physical examination, an erythematous plaque, about 1 cm in diameter, was observed on the left side of his back (Fig. 1). He complained of little symptoms due to the lesion except for mild itching but he was nervous about that. He recalled having eaten freshwater fish when he lived in China. Serological tests to check antibodies were not performed. Informed consent was obtained, and a needle biopsy was performed on the skin lesion.
Fig. 1.
The patient with an erythematous plaque (arrow) on his back due to infection with a Gnathostoma hispidum larva.
The skin tissue was fixed immediately in 10% neutral buffered formalin and was processed for routine histopathological examinations. Briefly, the tissue sample was dehydrated in a graded series of ethanol, embedded in paraffin, and sectioned longitudinally at a thickness of approximately 5 µm, stained with hematoxylin and eosin, and observed by light microscopy.
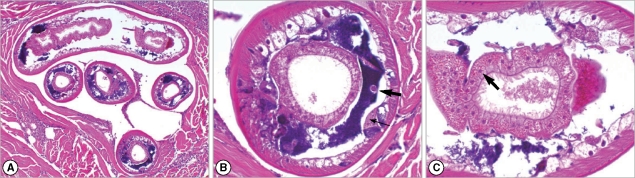
In the deep dermis layer, 5 sections of a nematode larva, 200-220 µm in diameter, were found surrounded by the collagen tissue (Fig. 2). Four were in cross-section, and 1 was in nearly longitudinal section. The larva had tegumental structures, including the cuticle, minute cuticular spines, and hypodermis. It also had polymyarian-coelomyarian somatic muscles and lateral and ventral cords. Its internal organs and structures included the intestine, genital primordia, and body cavity (Fig. 2). The intestinal canal consisted of 27-31 lining cells and each cell had 1 large nucleus in the center (Fig. 2). Based on these findings, the larva was identified as an advanced third-stage larva of G. hispidum. In the dermis around the larva, there were severe inflammatory reactions with cell infiltrations, and tunnel-like tracts formed presumably by the migration of the larva.
Fig. 2.
Sections of a Gnathostoma hispidum larva in the skin biopsy. (A) Sections showing the anterior (lower 4 sections) and posterior (upper 1 section) parts of the larva. × 40. (B) A cross section showing the internal structures, including the cuticle, hypodermis, muscles, lateral cord (thin arrow), genital primordium (thick arrow), and intestine of the larva. × 200. (C) Another cross section showing the morphology of the intestine and intestinal cells. Note that the number of intestinal cells is about 30, and that each cell has a single nucleus (arrow). × 200.
After the skin biopsy, the patient was comfortable and was discharged. No evidence of recurrence was noticed at a follow-up examination.
DISCUSSION
With regard to gnathostomiasis in the Republic of Korea, an imported case of G. spinigerum infection in the brain was reported from a Thai woman suffering from meningoencephalitis [15]. On the other hand, there was an outbreak of gnathostomiasis, presumably due to G. spinigerum, among 60 Korean emigrants who consumed raw fish dish in Yangon, Myanmar [7]. Some patients returned to Korea after this outbreak. Our patient recalled that his cutaneous symptoms developed in China 1-2 years before his return to Korea. Therefore, we designated our patient as an imported case of G. hispidum infection.
The diagnosis of our patient was based on histopathological findings of the biopsy specimen where sections of a gnathostome larva were found. When a Gnathostoma larva is observed in tissue sections, the shape of head-bulb hooks (if sectioned), and more importantly, the morphology of intestinal epithelium (the number and morphology of intestinal cells and the number of nuclei in each intestinal cell) are useful for differentiation of species [6]. Larvae of G. hispidum can be differentiated from those of G. spinigerum in that the former has 19-35 spherical intestinal cells and usually 1 large nucleus in the center of each cell, whereas the latter has 21-29 columnar or cylindrical intestinal cells and 3-7 small scattered nuclei in each cell [6,11,12]. In our specimens, about 30 (27-31) intestinal cells, each with a large nucleus in the center, were recognized and was compatible to the descriptions of G. hispidum. Because some Asian people, including Koreans and Japanese, like to eat raw fish, human G. hispidum infection should be regarded as an emerging disease.
ACKNOWLEDGEMENTS
We thank Prof. Katsuhiko Ando, Department of Medical Zoology, Mie University School of Medicine, Japan, for his kindness in identifying the sectioned histopathological specimens of our patient.
References
- 1.Herman JS, Chiodini PL. Gnathostomiasis, another emerging imported disease. Clin Microbiol Rev. 2009;22:484–492. doi: 10.1128/CMR.00003-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McCarthy J, Moore TA. Emerging helminth zoonoses. Int J Parasitol. 2000;30:1351–1360. doi: 10.1016/s0020-7519(00)00122-3. [DOI] [PubMed] [Google Scholar]
- 3.Moore DAJ, McCroddan J, Dekumyoy P, Chiodini PL. Gnathostomiasis: an emerging imported disease. Emerg Infect Dis. 2003;9:647–650. doi: 10.3201/eid0906.020625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ménard A, Dos Santos G, Dekumyoy P, Ranque S, Delmont J, Danis M, Bricaire F, Caumes E. Imported cutaneous gnathostomiasis: report of five cases. Trans R Soc Trop Med Hyg. 2003;97:200–202. doi: 10.1016/s0035-9203(03)90119-2. [DOI] [PubMed] [Google Scholar]
- 5.Ferman JS, Wall EC, van Tulleken C, Godfrey-Faussett P, Bailey RL, Chiodini PL. Gnathostomiasis acquired by British trourists in Botswana. Emerg Infect Dis. 2009;15:594–597. doi: 10.3201/1504.081646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miyazaki I. An Illustrated Book of Helminthic Zoonoses. Tokyo, Japan: International Medical Foundation of Japan; 1991. Section III. Nematode Zoonoses. 33. Gnathostomiasis; pp. 368–409. [Google Scholar]
- 7.Chai JY, Han ET, Shin EH, Park JH, Chu JP, Hirota M, Nakamura-Uchiyama F, Nawa Y. An outbreak of gnathostomiasis among Korean emigrants in Myanmar. Am J Trop Med Hyg. 2003;69:67–73. [PubMed] [Google Scholar]
- 8.Ando K, Tsunemori M, Akahane H, Tesana S, Hasegawa H, Chinzei Y. Comparative study on DNA sequences of ribosomal DNA and cytochrome c oxidase subunit 1 of mitochondrial DNA among five species of gnathostomes. J Helminthol. 2006;80:7–13. doi: 10.1079/joh2005315. [DOI] [PubMed] [Google Scholar]
- 9.Akahane H, Iwata K, Miyazaki I. Studies on Gnathostoma hispidum Fedchenko, 1872 parasitic in loaches imported from China. Jpn J Parasitol. 1982;35:465–467. (in Japanese) [Google Scholar]
- 10.Kagei N. Morphological identification of parasites in biopsied specimens from creeping disease lesions. Jpn J Parasitol. 1991;40:437–445. [Google Scholar]
- 11.Taniguchi Y, Ando K, Isoda KI, Shimizu M, Sonobe K. Human gnathostomiasis: successful removal of Gnathostoma hispidum. Int J Dermatol. 1992;31:175–177. doi: 10.1111/j.1365-4362.1992.tb03927.x. [DOI] [PubMed] [Google Scholar]
- 12.Akahane H, Sano M, Kobayashi M. Three cases of human gnathostomiasis caused by Gnathostoma hispidum, with particular reference to the identification of parasitic larvae. Southeast Asian J Trop Med Public Health. 1998;29:611–614. [PubMed] [Google Scholar]
- 13.Taniguchi Y, Ando K, Sugimoto K, Yamanaka KI. Creeping eruption due to Gnathostoma hispidum-one way to find the causative parasite with artificial digestion method. Int J Dermatol. 1999;38:873–880. doi: 10.1046/j.1365-4362.1999.00762.x. [DOI] [PubMed] [Google Scholar]
- 14.Sohn WM, Lee SH. The first discovery of larval Gnathostoma hispidum (Nematoda: Gnathostomidae) from a snake host, Agkistrodon brevicaudus. Korean J Parasitol. 1998;36:81–89. doi: 10.3347/kjp.1998.36.2.81. [DOI] [PubMed] [Google Scholar]
- 15.Lee SH, Hong ST, Chai JY. Description of a male Gnathostoma spinigerum recovered from a Thai Woman with meningoencephalitis. Korean J Parasitol. 1988;26:33–38. [Google Scholar]