Abstract
Adoptive T cell therapies can produce objective clinical responses in patients with hematologic and solid malignancies. Genetic manipulation of T lymphocytes has been proposed as a means of increasing the potency and range of this anti-tumor activity. We now review how coupling expression of transgenic receptors with countermeasures against potent tumor immune evasion strategies is proving highly effective in pre-clinical models and describe how these approaches are being evaluated in human subjects.
INTRODUCTION
Infusion of antigen-specific cytotoxic T lymphocytes (CTLs) has proven safe and apparently effective for the prophylaxis and treatment of viral infections such as cytomegalovirus (CMV) [1–3], adenovirus (Adv) [3], and Epstein-Barr virus (EBV) [4, 5] that arise in immunocompromised patients. This therapeutic approach has also been extended to the treatment of cancer and has shown some success in patients with melanoma [6] and EBV-associated malignancies such as Hodgkin’s lymphoma [7, 8] and nasopharyngeal carcinoma [9, 10]. This form of “personalized medicine” is now being explored in both early- and late-stage clinical trials. Recent improvements in molecular biology have increased the potential applications and effectiveness of this therapeutic approach by allowing the genetic modification of T cells using genes which confer properties such as new antigen specificity (αβT cell receptors – αβTCRs [11] or chimeric antigen receptors – CARs [12]), improved homing to tumor sites [13], increased resistance to tumor immune evasion strategies [14, 15], and the ability to up- or down- regulate proliferation of the infused cells [16, 17]. This review evaluates recent improvements in T cell engineering and describes their current clinical impact and their future potential as cancer therapeutics.
T CELL IMMUNITY AGAINST TUMOR CELLS
The development of an anti-tumor T cell mediated immune response is a multi step process in which tumor-associated antigens (TAAs) expressed by the tumor cells are processed and presented by professional antigen presenting cells (APCs) to circulating T cells, which become activated. The quality and potency of this T cell response will depend on the nature of the antigen presented, the functionality of the APC itself and the cytokines and co-stimulatory interactions that occur in the T cell/APC microenvironment [18]. Once activated, TAA-specific effector T cells can migrate to the tumor site and target malignant cells expressing the cognate antigen epitope displayed in the context of a major histocompatibility complex (MHC) molecule [18].
The potency and protective abilities of endogenous tumor-specific T cells are evident from studies of immunosuppressed individuals with dysfunctional or absent T cells (such as HIV-infected patients or transplant recipients), who are at increased risk of developing a range of malignances such as non-Hodgkin’s lymphoma (NHL) [19], Kaposi’s sarcoma, and invasive cervical cancer [20]. The importance of the immune system for prevention and control of tumors in immunocompetent individuals, however, is much more controversial [20]. When tumors arise in otherwise normal subjects, the conclusion is that specific T cells were either not induced in vivo, or were unable to destroy the malignant cells. Many of the antigens expressed by tumor cells are not unique to cancer cells and are instead expressed in normal tissues [21]. Consequently, the immune system may have antigen specific T cells that recognize the tumors, but that are rendered unresponsive or tolerant [22]. Efforts to break this unresponsiveness by aggressive vaccination have often failed [23]. An alternative approach is to adoptively transfer non-tolerant T cells that have been expanded in vitro in an environment that is capable of breaking their tolerant state and inducing potent effector cells. For example, EBV-specific CTLs can be generated ex vivo from EBV-specific T cell precursors circulating in the peripheral blood of individuals with EBV+ malignancies [7, 8]. Once returned to the patients, these effector T cells can effectively eradicate tumors that had been resistant to their endogenous precursors, even though both share the same antigenic specificity [7, 8]. Similarly, autologous tumor-infiltrating T lymphocytes (TIL) obtained from melanoma patients, expanded ex vivo and infused, have produced clinical response in about 50% of treated individuals [6, 24].
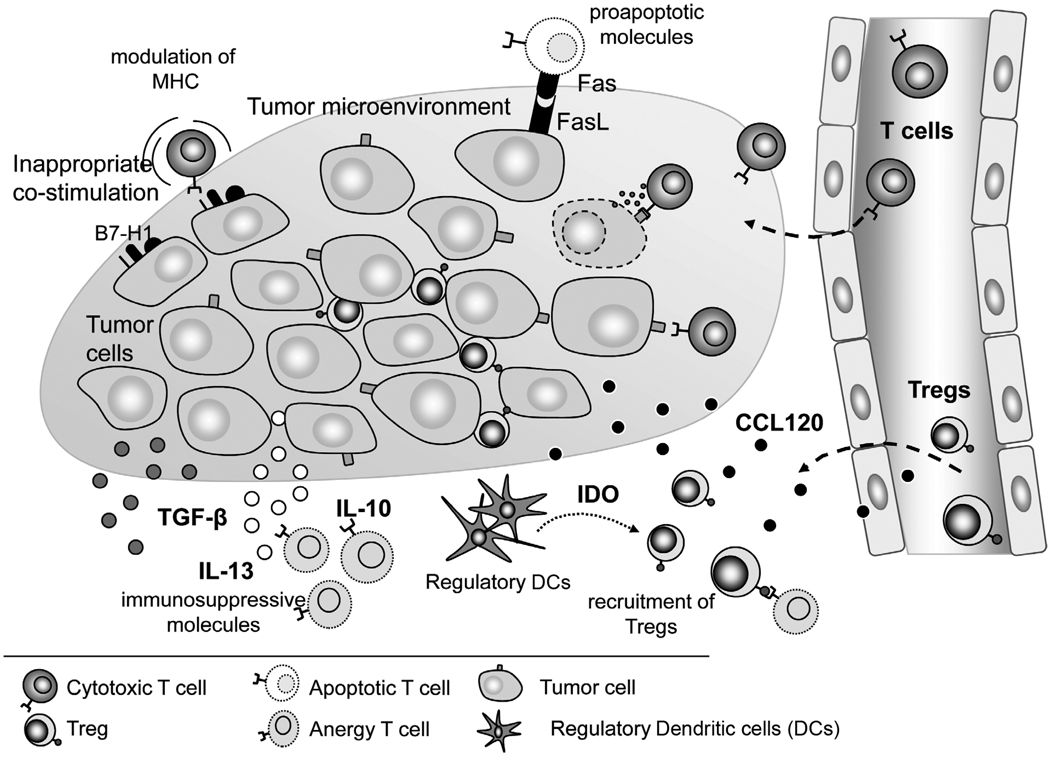
Breaking tolerance alone, however, is often insufficient for CTLs to be able to exert potent in vivo anti-tumor effector function. As illustrated in Fig. (1), malignancies have evolved a number of evasion strategies to mitigate tumor-directed T cell reactivity. These include (i) the secretion of immunosuppressive molecules like TGF-β, interleukin (IL)-10, and IL-13, which inhibit effector T cells [25], (ii) modulation of MHC and costimulatory molecules to prevent antigen-specific T cell recognition [25], (iii) recruitment of regulatory T cells (Tregs) which inhibit effector T cells by direct cell-to-cell contact or by the production of soluble factors [26–29], (iv) constitutive expression of the tryptophan-depleting enzyme, indoleamine 2,3-dioxygenase (IDO) that prevents lymphocyte proliferation [30], (v) expression of Fas ligand which can induce premature apoptosis of activated T cells through Fas-Fas ligand interaction [31] and, (vi) expression of inhibitory cell surface molecules such as PD-L1 (program death ligand), which interacts with PD-1 expressed on activated T cells, and induces T cell exhaustion [32, 33].
Fig. 1. Tumor immune evasion strategies.
Tumors have evolved complex mechanisms to subvert the cellular immune response, including expression of FasL or PD-L1 which induce apoptosis or anergy in effector T cells, recruitment of Tregs, secretion of TGF-β and other immunosuppressive cytokines which inhibit T cell proliferation, constitutive expression of IDO by tumors and regulatory DCs, which depletes tryptophan resulting in T cell anergy and downregulation or modulation of MHC and co-stimulatory molecules.
Genetic modifications have been devised to act as countermeasures to these immune evasion mechanisms, thereby improving the effectiveness of tumor-specific T cells in vivo.
METHODS OF GENE MODIFICATION (VIRAL AND NON VIRAL)
Effective genetic modification of T cells requires systems that produce adequate gene delivery and adequate expression of functional transgenes. While the level and duration of expression required for a given transgene depends on the specific function required, in general, the sustained modification of highly proliferative cells such as the T lymphocytes calls for an efficient integrating vector system that produces at least moderately high expression. The great majority of studies to date have therefore used retroviral vectors (Moloney or Lentivirus based) [5, 34–38] but the more recent development of integrating plasmids has renewed interest in the use of non viral approaches.
Though widely used in clinical studies, viral vectors are expensive to produce and test, and there is often a requirement for onerous and prolonged follow up of treated patients that further adds costs and complexity. Non viral vectors (eg. DNA plasmids) though cheaper to produce and test, require physical (e.g. electroporation) or chemical (e.g. liposomes) approaches to mediate gene transfer [39–41]. Until recently, DNA plasmids also integrated with extremely low efficiency, and so were associated with rapid disappearance in highly proliferating T cells. The discovery of transposon-based gene delivery systems overcomes this limitation by combining transposons and transposases in a plasmid with the gene of interest. Systems such as Sleeping Beauty [42, 43] and Piggybac [44] are currently used to gene modify T lymphocytes.
GENETIC ENGINEERING OF T CELLS
Gene transfer can be used to (i) improve the intrinsic biological activity of T cells (e.g. confer tumor specificity, enhance cytokine production or improve T cell migration), (ii) provide resistance to the immunosuppressive tumor microenvironment, (iii) enhance the safety of adoptively transferred T cells (e.g. addition of suicide genes), or (iv) enable T cell marking or imaging studies.
TRANSFER OF ANTIGEN SPECIFICITY TO THE T CELLS
Because most TAA are either “self” antigens or “naïve” targets for the immune system, the generation of tumor-reactive T cells from cancer patients is often difficult or impossible, even under optimal conditions of ex vivo culture [45, 46]. To overcome this problem, investigators have genetically modified T cells to allow them to recognize antigens expressed by tumor cells. The two most common approaches are (a) expression of CARs that recognize tumors through single-chain variable fragments (scFv) isolated from specific antibodies [47] and (b) gene modification with α and β TCR chains cloned from TAA-specific T cell clones with high antigen avidity [48].
Chimeric Antigen Receptors (CARs)
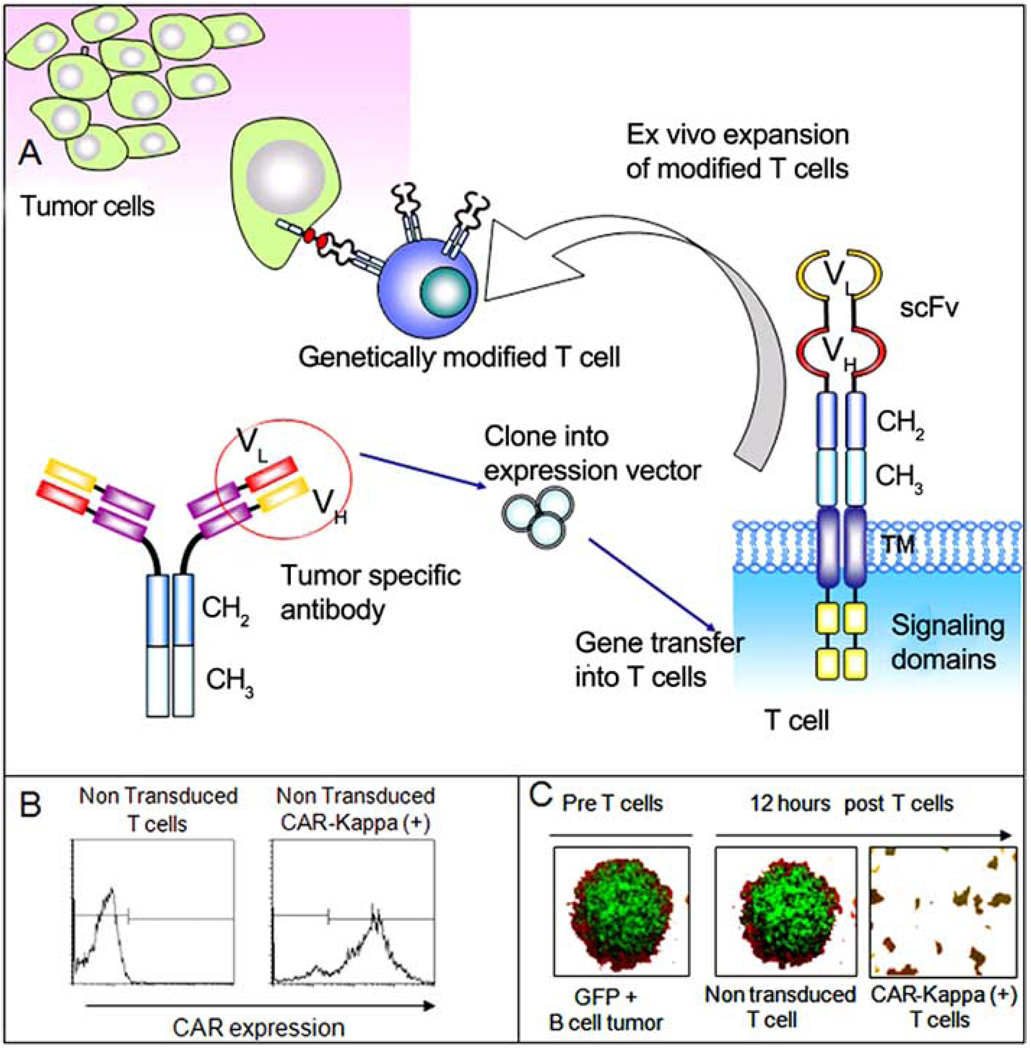
CARs are artificial receptors directed against antigens expressed on the cell surface of tumor cells, but with reduced or absent expression on normal tissues, thereby minimizing “off target” effects. First generation CARs are composed of the single-chain variable fragment (scFv) obtained from a specific antibody linked, via an extracellular spacer, with a transmembrane region and the intracytoplasmatic domain of the CD3ζ [47] (Fig. 2). The endodomain is responsible for transmitting the signal from the chimeric receptor and triggering phosphorylation of ITAM motifs, and the subsequent induction of T cell cytotoxic activity. CARs can combine the antigen specificity of an antibody with the lytic capacity of T cells and mediate antigen recognition in an MHC-unrestricted fashion. They also extend the range of antigens that can be recognized by T cells to include carbohydrates and glycolipids [49–51]. The overall efficacy of CAR-modified T cells against tumor target cells is the result of a complex interaction that includes the avidity of the scFv, the level of expression of CAR molecules on T cells, the density of antigen expressed on the target cells, and the position of the epitope on the target molecule in respect to the length and flexibility of the extracellular spacer sequence incorporated in the CAR.
Fig. 2. Generation and function of CARs.
Panel A) illustrates the structure of a chimeric antigen receptor, and expression by T cells after gene transfer. After modification T cells can be redirected against tumor antigens and elicit a cytotoxic effect. Panel B) shows the expression of a CAR on T cells after retroviral transduction, by using a monoclonal antibody that recognizes the CH2CH3 extracellular component of the protein. Panel C) Cytolysis by gene modified T cells: a B cell tumor (Daudi) expressing green fluorescent protein (GFP) was cultured with non-modified T cells or T cells transduced with a CAR targeting the κ-light chain of human immunoglobulins at a of ratio 5:1 (tumor cells to T cells). After 12 hours in culture, T cells modified with the CAR-κ have destroyed the tumor.
Clinical Studies with CARs
CAR-expressing T cells can specifically recognize and respond to soluble, immobilized and/or tumor antigens expressed on target cells, and to date a range of CARs targeting a variety of surface molecules expressed by many solid tumors and hematological malignancies have been developed [52–61] (Table 1). While preclinical studies demonstrate that T cells expressing CARs can eliminate tumors in murine models [56, 61, 62], clinical trials with “first generation” CARs, containing only the CD3ζ signaling domain, were disappointing [39, 63, 64]. Following engagement with tumor antigens, the CD3ζ endodomain provides insufficient co-stimulatory signaling to the T cells to produce activation, proliferation and cytokine release, while the tumor cells themselves lack sufficient costimulatory signals to accomplish this through the endogenous counter-receptors on CAR-modified T cells [65]. This led to the development of “second generation” CARs, in which additional intracellular co-stimulatory endodomains are added to enhance their function. These endodomains are derived from costimulatory molecules such as CD28, ICOS, CD134 and CD137 [56, 66–70], and T cells expressing these endodomains produce a broad array of cytokines such as IL-2 and TNF-α upon chimeric receptor engagement. These cytokines enhance the proliferation and persistence of genetically modified T cells after recognition of their CAR specific target. More recently “third generation” CARs, characterized by the presence of two costimulatory molecules in addition to the CD3ζ, have been developed [70, 71]. Carpenito and colleagues formally compared the potency of a CAR linked to a range of different endodomains and found that the simultaneous expression of CD137 (41BB) and CD28 endomains was more potent than either endodomain alone [72]. It remains to be demonstrated whether the “superphysiological” activation of T cells also increases the toxicity of CAR-modified T cells.
Table 1.
Chimeric Antigen Receptors
| Specificity | Tumor Target | Reference |
|---|---|---|
| CEA | Colorectal cancer | [59] |
| EGP40 | Colorectal cancer | [128] |
| CD44v 7/8 | Cervical carcinoma | [129] |
| FBP | Ovarian | [130] |
| Le(Y) | Ovarian epithelial | [131] |
| MUC1 | Breast, Ovary | [132] |
| ERB-B2 | Breast and others | [133] |
| PSCA | Prostate | [134] |
| PSMA | Prostate | [135] |
| TAG-72 | Adenocarcinoma | [136] |
| MAGE-A1 | Melanoma | [137] |
| GD3 | Melanoma | [138] |
| GD2 | Neuroblastoma, Melanoma | [12,60,139] |
| KDR | Neo vasculature | [140] |
| VEGF-R2 | Neo vasculature | [141] |
| CD30 | Lymphoma | [13,54,55] |
| CD33 | Myeloid leukemia | [68] |
| CD19 | B cell malignancies | [52,62,69] |
| CD20 | B cell malignancies | [142] |
| Kappa light chain | B cell malignancies | [56] |
| CD22 | B cell malignancies | [143] |
| Her-2 | Medulloblastoma | [61] |
| CAIX | Renal cell carcinoma | [58] |
| α-Folate receptor | Ovarian cancer | [57] |
Factors other than inadequate expression of costimulatory endodomains can result in poor in vivo persistence of CAR-modified T cells. Since most CARs are derived from murine antibodies, the chimera itself can induce an immune response in vivo following adoptive transfer. Lamers and colleagues reported the development of anti-scFv antibodies in three patients treated with T cells expressing a CAIX-specific CAR [58]. Similarly, Kershaw and colleagues observed a CAR-specific antibody response in a patient treated with T cells modified with a CAR directed against the ovarian-associated α-folate receptor (α-FR) [57]. Although this phenomenon has not been observed for all patients treated with CARs, the future use of humanized single chains may reduce the risk of premature deletion of T cells due to immune responses.
CAR-modified T cells may cause significant in vivo toxicities, such as the “on target antigen but off target tissue” toxicity. Lamers et al. reported the development of cholestasis following the infusion of T cells modified with a CAR targeting the carbonic anhydrase as treatment for renal cell carcinoma as biliary epithelial cells also express carbonic anhydrase [58]. Brentjens et al. recently reported renal and respiratory failure in a patient with B-cell chronic lymphocytic leukemia treated with a single dose of 3×107/kg of T cells modified with a second generation CAR targeting the CD19 molecule. This serious adverse event occurred when T cells were infused after high doses of cyclophosphamide to induce host lympohodepletion and may have been due to a cytokine storm or to rapid tumor lysis [73].
T Cell Receptor α/βTCRs
T cells can be genetically modified to express transgenic α and β TCR chains, which have been isolated from T cell clones specific for tumor-associated antigens including MART-1, MAGE-3, MDM2, and WT-1 [11, 74, 75]. Both chains can be accommodated in a single retroviral or lentiviral vector, and transfer of the tumor-specific αβTCR to autologous mitogen-activated T cells allows rapid production of large numbers of tumor peptide-specific T cells. These gene modified T cells acquire MHC-restricted cytotoxic activity against tumor cells expressing the specific epitope. In most examples to date, polyclonal T cells are manipulated to express a second, transgenic, αβTCR in addition to their native αβTCR [11, 74]. The presence of two pairs of receptors in a single cell leads to unwanted cross pairing between endogenous α and transgenic β chains (and vice versa), reducing the affinity of the transgenic receptor for the desired target antigen and potentially creating new and unwanted reactivities [48]. Investigators have manipulated the sequences of the transgenic chains to favor their linkage, and have also tried introducing the receptors into TCR negative effector lymphocytes [76, 77]. At present it is unclear how valuable these approaches will be.
T cells expressing a transgenic αβTCR have been studied in clinical trials of patients with melanoma. Investigators at the National Cancer Institute demonstrated that adoptive transfer of polyclonal T cells transduced with a retroviral vector encoding the αβTCR chains specific for an HLA-A2 restricted MART-1 peptide induced objective clinical response in 13% of the patients [11]. In an effort to increase the frequency of significant tumor responses, the same investigators infused T cells that expressed higher affinity transgenic αβTCRs specific for MART-1 or gp100 peptides [78]. Disappointingly, this strategy only modestly increased the tumor response rate but significantly exacerbated toxicity. The majority of patients developed skin rush, uveitis and hearing loss, attributed to an immune attack on normal melanocytes present in the skin, eye and inner ear [78]. Hence potent T lymphocytes can be generated by appropriate genetic modification, but toxicity may become increasingly evident as potency increases, particularly if the targeted antigen is not unique to the malignant cells.
GENETIC MODIFICATION OF T CELLS TO ENHANCE PERSISTENCE
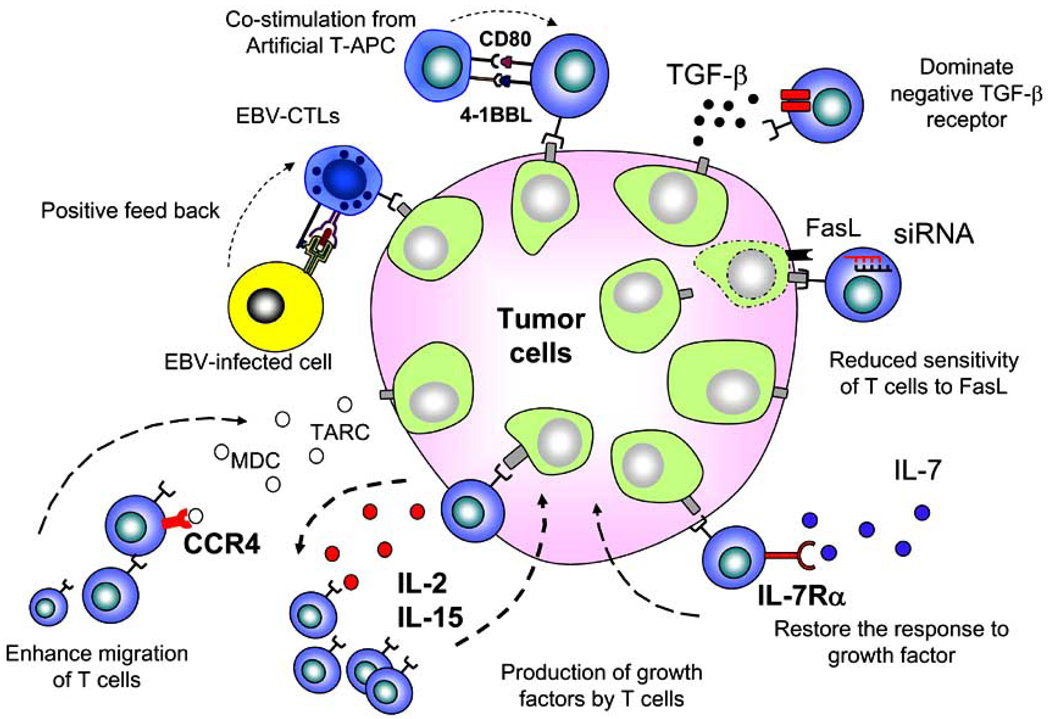
Though antigen specificity can be readily conferred using genetic modification, once infused, the tumor-specific T cells must expand in vivo and/or persist until all malignant cells have been eliminated. T cell proliferation requires continued antigenic stimulation, either via direct interaction with tumor cells or through professional APCs that cross-present tumor antigens, and the presence of appropriate cytokines. Moreover, following in vivo expansion, a proportion of the tumor-specific T cells should ideally enter the memory T cell compartment to provide long-term protection. To prevent these events, tumors have developed potent strategies to avoid effective antigen presentation, inhibit T cell proliferation, and prevent T cell entry into the memory compartment [25]. As a consequence, both preclinical and clinical studies have shown that transferred cells have limited capacity to expand and persist in vivo. Several countermeasures have been developed against these unwanted tumor effects on immune persistence. These include: i) genetic modification of T cells to improve proliferation and survival, ii) the infusion of T cells with memory-type characteristics [79], and iii) genetic modification of infused cells to withstand the tumor microenvironment (Fig. 3).
Fig. 3. Enhancing the anti-tumor effect of gene modified T cells.
Several genetic modifications have been used to improve the antitumor efficacy and longevity of T cells in vivo. These include transgenic expression of IL-2, IL-15, or IL-7Rα to improve proliferation, over-expression of hTERT, Bcl-2, Bcl-XL to increase survival, expression of CD80, 41BBL or modification of antigen-specific T cells to enhance co-stimulation, overexpression of CCR4 to improve migration to tumor sites, expression of a dominant-negative TGF-β receptor as well as downregulation of GCN2 or Fas on T cells to neutralize the inhibitory tumor microenvironment.
IMPROVING PROLIFERATION AND SURVIVAL OF EFFECTOR T CELLS
Cytokines
Cytokines such as IL-2 promote T effector cell expansion and survival, and systemic administration can support adoptive T cell therapies [6, 24]. However, prolonged administration of recombinant IL-2 can also cause significant toxicity [6, 24] and expand Tregs which antagonize the beneficial effects of the cytokine on T effector cells [80]. We and others have explored alternative methods to expand T cells in vivo, by genetically modifying T cells with retroviral vectors encoding the cytokines IL-2 or IL-15 to produce cells which are cytokine self-sufficient and self-sustaining [16, 81, 82]. Extensive characterization demonstrated that these cytokine-transgenic cells conserved their antigen specificity, phenotype and function and also retained their dependence on antigenic stimulation for continued expansion. Importantly, genetically modified T cells had enhanced persistence and superior anti-tumor activity in vivo compared to unmodified cells [16].
T cell growth and survival can also be increased by engineering cells to respond to cytokines in the tumor environment, or which can be safely administered as a recombinant protein, but which do not normally induce T cell growth [83]. We investigated this option by genetically restoring the ability of activated antigen-specific CTLs to respond to IL-7, a cytokine that has been safely administered to human subjects without apparent enhancement of Treg cell number and function [83–85]. Unfortunately, IL-7 has only limited activity on antigen-specific T cells, since IL-7Rα expression is rapidly downregulated by naïve T cells once they have received antigenic stimulation [17]. By forcing the expression of IL-7Rα in antigen-specific T cells, we selectively expanded them in vitro and in vivo in response to IL-7, without inducing unwanted proliferation of other T cell subsets [17]. Clinically, the IL-7 required to support expansion of the transgenic receptor-expressing CTLs may derive either from the physiological release of the cytokine in a lymphodepleted host or from the administration of the recombinant protein.
Pro-survival genes
T cell survival can also be increased by overexpressing the human telomerase reverse transcriptase (hTERT) gene [86]. Although this approach greatly increases the number of population doublings of transduced T cells by preventing telomere erosion, it may also favor genomic instability and limit its safety and hence clinical application. An alternative means of increasing the persistence of infused T cells is to modify them with anti-apoptotic genes, such as Bcl-2 and Bcl-xL, which increase T cell resistance to death and IL-2 cytokine withdrawal [87].
Co-stimulation
T cell proliferation and survival require antigenic stimulation by APCs expressing co-stimulatory molecules. Many tumor cells lack expression of co-stimulatory molecules, such as CD80 and CD86, and substantially reduce the opportunity of T cells to successfully encounter the antigen in a suitably co-stimulatory environment [25, 88]. One way to circumvent this problem is to use CARs or transgenic αβTCRs to retarget virus-specific CTLs, rather than “random” T cells. Such virus-specific CTLs should receive optimal activation and co-stimulation following engagement of their native (virus specific) αβTCRs with viral latent antigens expressed by professional APCs, thus enabling superior anti-tumor activity mediated by their tumor reactive transgenic receptor. This hypothesis has been tested in a clinical trial performed at our institution, in which we compared the longevity of polyclonal activated T cells and polyclonal EBV-specific CTLs each expressing a CAR targeting the GD2 antigen, which is expressed on neuroblastoma [12, 60]. The EBV-specific CTLs remained detectable substantially longer (>18months) than their activated T cell counterparts (<1 month), suggesting the beneficial effects of co-stimulation of EBV-specific CTLs provided by APCs expressing EBV-latent antigens [12].
An alternative means for providing T cell co-stimulation is to force the expression of co-stimulatory ligands, such as CD80 and 4-1BBL, for the co-stimulatory receptors they already possess [89]. Post-infusion, these molecules will insure there is “autocostimulation” and a bystander “transcostimulation”, which substitutes for the lack of appropriate co-stimulation from the tumor cells. Preclinical studies have shown that incorporation of these molecules in CAR-modified T cells enhances their ability to produce effector cytokines (IFNγ, IL-2, TNFα) and, in an in vivo mouse model, promotes tumor rejection in mice with large tumor burden [89].
Resistance to immunosuppressive drugs
In many of the settings in which adoptively transferred T cells will be used, patients are also receiving immunosuppressive and/or T cell inhibitory agents, which can adversely affect the persistence, functional capabilities and survival of adoptively-transferred T cells. For example, solid organ transplant recipients require continued administration of immunosuppressive drugs such as tacrolimus to prevent graft rejection. However, since these agents also impair endogenous T cell function, these patients are at high risk of developing virus-associated complications including EBV-post-transplant lymphomas [90]. Although adoptive transfer of EBV-specific CTLs can still be effective in these patients, the cells do not persist long-term [91–93]. Strategies to make antigen-specific CTLs resistant to the effects of immunosuppressive drugs have been recently developed and include stable siRNA-mediated knock-down of the FK506-binding protein 12 (FKBP12) [94], the key protein that binds FK506, and overexpression of calcineurin mutants [95]. Both strategies protect virus-specific CTLs from inhibitory effects whilst preserving their anti-viral activity.
NEUTRALIZING THE HOSTILE TUMOR MICRO-ENVIRONMENT
Genetic modification of T cells can also be used to counteract the immune-inhibitory tumor microenvironment that can neutralize adoptively transferred antigen-specific CTLs. One of the most widely used tumor evasion strategies is local secretion of TGF-β by the tumor or its stromal elements [25]. TGF-β is a multifunctional cytokine that, among other activities, limits T cell proliferation and effector function and induces tolerance [96]. Antigen-specific CTLs modified to express a dominant-negative TGF-β receptor type II (dnTGF-β-RII) are resistant to the antiproliferative effects of TGF-β in vitro and in vivo [14], and expression prolongs their persistence and enhances tumor elimination in mice bearing TGF-β-expressing tumors [14, 97]. However, the gene modified T cells persisted only as long as the mice were restimulated with antigen, offering reassurance that the cells safely maintained their antigen dependence. A clinical trial to assess the safety and efficacy of dnTGF-β-RII-modified tumor-specific CTLs for the treatment of patients with relapsed/refractory Hodgkin’s lymphoma has recently opened at our institution.
Indoleamine 2,3-dioxygenase (IDO), is an enzyme catalyzing the initial step in the catabolism of tryptophan along the kynurenine pathway [30]. T cells are particularly sensitive to tryptophan shortage, a property exploited by a number of tumors that secrete this enzyme either constitutively or in the presence of proinflammatory cytokines [30, 98, 99]. The inhibitory effects of IDO in T cells may be overcome by gene modification aimed to downregulate GCN2, a major component of IDO-mediated suppression. Munn and colleagues showed in pre-clinical studies that GCN2-knockout cells were refractory to IDO-induced anergy [100].
Fas ligand (FasL/CD95L) is a member of the tumor necrosis factor (TNF) superfamily and can trigger apoptosis through cross-linking of its receptor Fas (CD95). Many tumors express Fas ligand (FasL) as part of their tumor evasion arsenal, and researchers have suggested that this allows “immune privilege” because activated effector T cells express Fas on their cell surfaces and so are sensitive to Fas-mediated apoptosis, impairing T cell-mediated tumor rejection [101–103]. To overcome this, stable gene transfer of small interfering RNA (siRNA) designed to down regulate Fas can render T cells resistant to the apoptotic effects of FasL-expressing tumor cells [15].
At present, we do not know the best means of neutralizing the hostile tumor environment, and it is likely that a combination of the above countermeasures will need to be employed. Nonetheless, as we progressively accrue clinical data to add to the information provided by preclinical models, it should become possible to discern the optimal approach.
REDIRECTING T CELL MIGRATION
The interaction of secreted chemokines and chemokine receptors on the cell surface of the T cells plays a significant role in modulating the in vivo migration of T cells [104, 105]. Tumors can generate a chemokine milieu that significantly modifies the trafficking of Th1, Th2 cells and Tregs [27]. Malignant Hodgkin’s lymphoma cells, for example, produce TARC and MDC which strongly attract Th2 and Tregs since these T cell subsets constitutively express CCR4, the receptor for both chemokines [106, 107]. By contrast, Th1 cells lack CCR4 and hence migrate poorly to HL tumor cells. Gene transfer offers the opportunity to re-shape the migration profile of Th1 cells so that they can exploit the tumor’s own escape mechanisms. We recently produced effector CD8+ CTL migration to TARC+ tumors by transgenic expression of the CCR4 receptor [13]. This genetic modification enhances the anti-tumor effects of Th1 cells without apparent modification to their effector function [13]. Similar approaches could be extended to other human malignancies in which a signature chemokine pattern can be identified [108].
GENETIC MODIFICATION OF T CELLS TO IMPROVE SAFETY
Suicide genes
The genetic approaches described above can enhance the expansion and persistence of T cells, change their homeostatic properties, alter their trafficking pattern and re-direct their antigen specificity to recognize specific antigens. Inevitably, these changes will be associated with an increased risk of direct toxicity and of unwanted proliferation, and even cell transformation due to insertional mutagenesis [109]. To allow the rapid and complete elimination of infused cells, several groups have evaluated safety switches or suicide genes, which can be triggered should toxicity occur.
The best validated of the suicide genes is thymidine kinase from herpes simplex virus I (HSV-tk) [35, 110]. This enzyme phosphorylates the nontoxic prodrug ganciclovir, which then becomes phosphorylated by endogenous kinases to GCV-triphosphate, causing chain termination and single-strand breaks upon incorporation into DNA, thereby killing dividing cells. Several phase I-II studies have shown that Ganciclovir administration can safely eliminate transferred HSV-tk-modified cells in vivo [110, 111]. Unfortunately, the HSV-tk gene product is itself immunogenic and can induce reactive T cells which may prematurely eliminate the infused cells [112], compromising the persistence and hence efficacy of the transferred T cells.
More recently, inducible Fas [113], Fas-associated death domain–containing protein (FADD), and Caspase9 [114, 115] molecules have been considered as alternative non-immunogenic suicide genes. Each of these molecules can act as a suicide switch when fused with a FK-binding protein (FKBP) variant that binds a chemical inducer of dimerization (CID), AP1903, a synthetic drug that has proven safe in healthy volunteers [116]. Administration of this small molecule results in cross-linking and activation of the proapoptotic target molecules. Up to 90% of T cells transduced with inducible Fas or FADD undergo apoptosis after exposure to CID [113]. While promising, elimination of 90% of transduced cells may be insufficient to ensure safety of genetically modified cells in vivo. Moreover, death molecules that act upstream of most apoptosis inhibitors may be ineffective when tried in other cell types. Modification of the late-stage apoptosis pathway molecules such as caspase9 may be preferable [114]. This suicide gene can be stably expressed in human T cells without compromising their functional and phenotypic characteristics [16, 114]. The cells are highly sensitive to the CID, which can induce apoptosis in up to 95% of transduced cells [16, 115]. This suicide gene strategy is currently being tested clinically at our institution as a means of eliminating adoptively-transferred polyclonal T cells after haploidentical transplantation.
Transgenic expression of the CD20 moleucle, which is normally expressed on B cells, has also been postulated as suicide gene for T cell therapies [117]. This strategy relies on the clinical availability of a humanized anti-CD20 antibody (Rituximab) which is widely used to eliminate both normal and neoplastic B cells expressing the CD20 antigen. Thus, infusion of T cells expressing human CD20 and subsequent in vivo administration of Rituximab should efficiently eliminate the infused T cell population, although it will also eliminate normal B cells.
Targeted integration
Reports of leukemia development caused by insertional mutagenesis using retroviral vectors for stem cell modification [109, 118], have spurred development of safer techniques for modifying cell DNA sequences, either by pre-determining the integration site of the transgene or by using modified vectors with a safer profile.
Zinc finger nucleases (ZFN) are artificial restriction enzymes generated by fusing a zinc finger DNA-binding domain to a DNA-cleavage domain. The underlying technology is known as gene targeting and is based on the cellular homologous recombination (HR) pathway, which has evolved to promote genetic recombination during meiosis and the repair of DNA double strand breaks. These ZFN can be customized to generate a DNA double stand break at a preselected site in the human genome and their development has paved the way for both knock-out and knock-in strategies in gene therapy. The therapeutic efficacy of this strategy is currently being evaluated in CD4+ T cells, in which disruption of the chemokine receptor 5 is expected to protect the T cells from infection with the HIV virus. Infected mice engrafted with ZFN-modified human CD4+ T cells had a lower load of HIV1 and higher CD4+ T cell counts than controls [119]. Validation studies using this approach for therapeutic transgenes are in the planning stages. Researchers are also moving away from Moloney based retroviral vectors to lentivectors, which appear less prone to integrate near transcription start sites and may thereby reduce the risk of oncogenesis [120].
T CELL MARKING AND IMAGING
Gene marking was first used clinically as a means of determining the persistence of infused T cells in vivo, and to allow investigators to track their migration and association with adverse effect such as GvHD, rather than as a tool to confer additional biological characteristics to cells [5, 34, 37]. Initial trials included inclusion of integrants such as the neomycin resistance gene [5, 34] and non-functional proteins like the truncated nerve growth factor receptor [36]. Expression of genes that extend this conceptual approach and enable direct T cell imaging in vivo are currently in development. For example, repetitive positron emission tomography and computed tomography (PET-CT) imaging of T cells genetically labeled to express the HSV1-tk reporter gene is possible in small and large animals using 2'-fluoro-2'-deoxy-1-β-D-arabinofuranosyl-5-iodouracil (FIAU), 9-(4-[18F]fluoro-3-(hydroxymethyl)butyl)guanine (18F-FHBG) or 2'-[18F]fluoro-5-ethyl-1-beta-D-arabinofuranosyluracil (18F-FEAU) radiotracer [121–123]. Recently, Yaghoubi et al. [124] reported that 18F-FHBG PET can detect HSV1-tk+ T lymphocytes infused loco-regionally into the site of tumor resection in a patient with grade IV glioblastoma multiforme indicating that these methodologies may be extensively clinically applicable in the future.
T CELL MANUFACTURE (GMP CONSIDERATIONS)
Although the administration of ex vivo activated and expanded primary and antigen-specific CTLs is associated with promising clinical results, there are several limitations to broader implementation. A major practical constraint is the current complexity of production. T cell proliferation in traditional cell cultureware is limited by requirements for nutrients and oxygen (O2), and by accumulation of waste products such as carbon dioxide (CO2) and lactic acid so that cultures must be fed and split regularly [125].
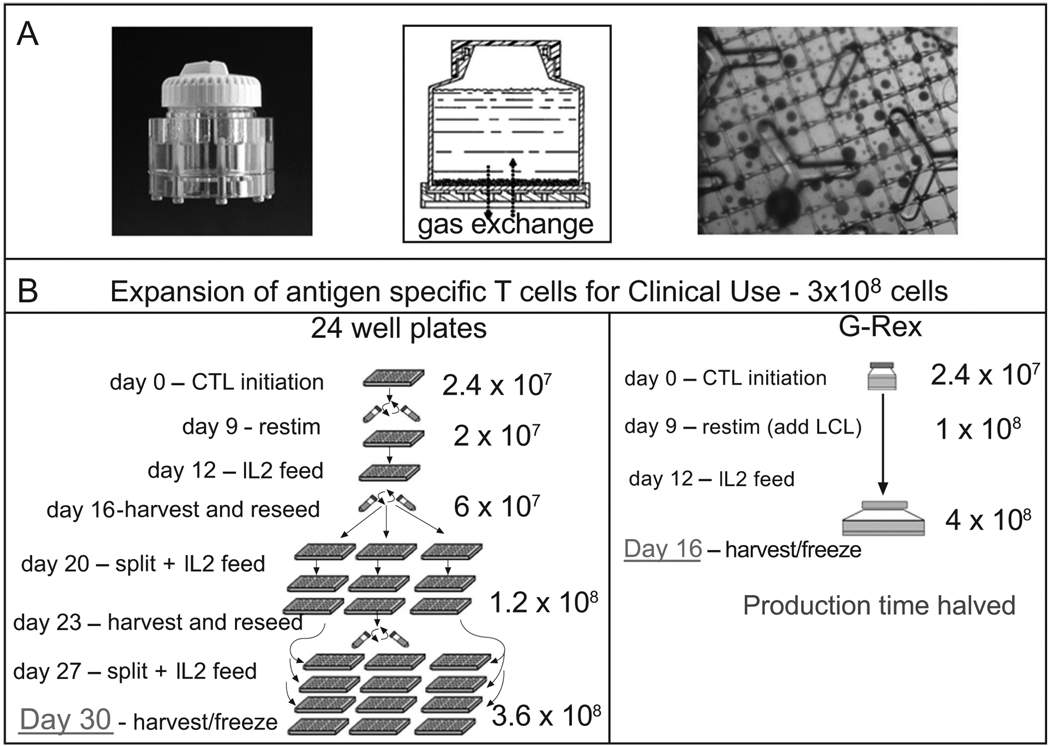
To improve cell output with minimal cell handling, a number of closed-system bioreactors have been explored. Mechanical rocking or stirring increases the availability of O2 in the culture, while media and nutrients can be exchanged by perfusion [126]. We have evaluated a novel gaspermeable rapid expansion cultureware (G-Rex) developed by Wilson Wolf Manufacturing, in which O2 and CO2 are exchanged across a silicone membrane at the base of the flask [127]. Gas exchange from below allows an increased depth of medium above, providing more nutrients and diluting waste. This system supports the expansion of antigen-specific CTLs, as well as genetically modified T cells, is scalable, GMP-compliant, and reduces the number of technician interventions approximately 4-fold while increasing the cell output by 3–20-fold compared with conventional methods (Fig. 4).
Fig. 4. Improving T cell manufacture.
The figure shows the manipulations required for the expansion of antigen-specific CTLs using conventional 24 well plates versus the G-Rex bioreactor. The G-Rex manufacturing increases cell output with minimal manipulation and shortens the required CTL production time.
CONCLUSIONS
To tip the balance of power away from the tumor and in favor of adoptively-transferred T cells many groups have used genetic modification to improve target recognition, enhance T cell persistence and migration, and to increase T cell resistance to the inhibitory tumor microenvironment. Promising pre-clinical data are now being validated in current and future human clinical trials. Even if successful, these therapies will ultimately be limited by the cost and complexity of the cell manufacturing process and simplified and accelerated cell culture systems are now in development and should help to make T cell therapy more accessible.
ACKNOWLEDGEMENTS
This work was supported in part from Leukemia and Lymphoma Society Specialized Center of Research (SCOR; grant no. 7018) (M.K.B.), NIH PO1CA94237, NIH P50CA126752, Leukemia and Lymphoma Society Translational Research grants (G.D.) Doris Duke Charitable Foundation/Clinical Scientist development award (G.D.), the ASBMT New Investigator Award (J.F.V.) and the When Everyone Survives (J.F.V.).
Footnotes
DISCLOSURE
All authors contributed in writing the manuscript. The authors declare no competing financial interests.
REFERENCES
- 1.Cobbold M, Khan N, Pourgheysari B, et al. Adoptive transfer of cytomegalovirus-specific CTL to stem cell transplant patients after selection by HLA-peptide tetramers. J Exp Med. 2005;202:379–386. doi: 10.1084/jem.20040613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Einsele H, Roosnek E, Rufer N, et al. Infusion of cytomegalovirus (CMV)-specific T cells for the treatment of CMV infection not responding to antiviral chemotherapy. Blood. 2002;99:3916–3922. doi: 10.1182/blood.v99.11.3916. [DOI] [PubMed] [Google Scholar]
- 3.Leen AM, Myers GD, Sili U, et al. Monoculture-derived T lymphocytes specific for multiple viruses expand and produce clinically relevant effects in immunocompromised individuals. Nat Med. 2006;12:1160–1166. doi: 10.1038/nm1475. [DOI] [PubMed] [Google Scholar]
- 4.Rooney CM, Smith CA, Ng CY, et al. Infusion of cytotoxic T cells for the prevention and treatment of Epstein-Barr virus-induced lymphoma in allogeneic transplant recipients. Blood. 1998;92:1549–1555. [PubMed] [Google Scholar]
- 5.Heslop HE, Ng CY, Li C, et al. Long-term restoration of immunity against Epstein-Barr virus infection by adoptive transfer of gene-modified virus-specific T lymphocytes. Nat Med. 1996;2:551–555. doi: 10.1038/nm0596-551. [DOI] [PubMed] [Google Scholar]
- 6.Rosenberg SA, Restifo NP, Yang JC, Morgan RA, Dudley ME. Adoptive cell transfer: a clinical path to effective cancer immunotherapy. Nat Rev Cancer. 2008;8:299–308. doi: 10.1038/nrc2355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roskrow MA, Suzuki N, Gan Y, et al. Epstein-Barr virus (EBV)-specific cytotoxic T lymphocytes for the treatment of patients with EBV-positive relapsed Hodgkin's disease. Blood. 1998;91:2925–2934. [PubMed] [Google Scholar]
- 8.Bollard CM, Gottschalk S, Leen AM, et al. Complete responses of relapsed lymphoma following genetic modification of tumor-antigen presenting cells and T-lymphocyte transfer. Blood. 2007;110:2838–2845. doi: 10.1182/blood-2007-05-091280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Straathof KC, Bollard CM, Popat U, et al. Treatment of nasopharyngeal carcinoma with Epstein-Barr virus--specific T lymphocytes. Blood. 2005;105:1898–1904. doi: 10.1182/blood-2004-07-2975. [DOI] [PubMed] [Google Scholar]
- 10.Comoli P, Pedrazzoli P, Maccario R, et al. Cell therapy of stage IV nasopharyngeal carcinoma with autologous Epstein-Barr virus-targeted cytotoxic T lymphocytes. J Clin Oncol. 2005;23:8942–8949. doi: 10.1200/JCO.2005.02.6195. [DOI] [PubMed] [Google Scholar]
- 11.Morgan RA, Dudley ME, Wunderlich JR, et al. Cancer regression in patients after transfer of genetically engineered lymphocytes. Science. 2006;314:126–129. doi: 10.1126/science.1129003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pule MA, Savoldo B, Myers GD, et al. Virus-specific T cells engineered to coexpress tumor-specific receptors: persistence and antitumor activity in individuals with neuroblastoma. Nat Med. 2008;14:1264–1270. doi: 10.1038/nm.1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Di Stasi A, De Angelis B, Rooney CM, et al. T lymphocytes coexpressing CCR4 and a chimeric antigen receptor targeting CD30 have improved homing and antitumor activity in a Hodgkin tumor model. Blood. 2009;113:6392–6402. doi: 10.1182/blood-2009-03-209650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bollard CM, Rossig C, Calonge MJ, et al. Adapting a transforming growth factor beta-related tumor protection strategy to enhance antitumor immunity. Blood. 2002;99:3179–3187. doi: 10.1182/blood.v99.9.3179. [DOI] [PubMed] [Google Scholar]
- 15.Dotti G, Savoldo B, Pule M, et al. Human cytotoxic T lymphocytes with reduced sensitivity to Fas-induced apoptosis. Blood. 2005;105:4677–4684. doi: 10.1182/blood-2004-08-3337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Quintarelli C, Vera JF, Savoldo B, et al. Co-expression of cytokine and suicide genes to enhance the activity and safety of tumor-specific cytotoxic T lymphocytes. Blood. 2007;110:2793–2802. doi: 10.1182/blood-2007-02-072843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vera JF, Hoyos V, Savoldo B, et al. Genetic manipulation of tumor-specific cytotoxic T lymphocytes to restore responsiveness to IL-7. Mol Ther. 2009;17:880–888. doi: 10.1038/mt.2009.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stagg J, Johnstone RW, Smyth MJ. From cancer immunosurveillance to cancer immunotherapy. Immunol Rev. 2007;220:82–101. doi: 10.1111/j.1600-065X.2007.00566.x. [DOI] [PubMed] [Google Scholar]
- 19.Dotti G, Heslop H, Rooney C. Epstein barr virus cell based immunotherapy. In: Robertson ES, editor. Epstein-Barr Virus. Norfolk, England: Caister Academic Press; 2005. pp. 669–690. [Google Scholar]
- 20.Serraino D, Piselli P, Busnach G, et al. Risk of cancer following immunosuppression in organ transplant recipients and in HIV-positive individuals in southern Europe. Eur J Cancer. 2007;43:2117–2123. doi: 10.1016/j.ejca.2007.07.015. [DOI] [PubMed] [Google Scholar]
- 21.Mandelcorn-Monson RL, Shear NH, Yau E, et al. Cytotoxic T lymphocyte reactivity to gp100, MelanA/MART-1, and tyrosinase, in HLA-A2-positive vitiligo patients. J Invest Dermatol. 2003;121:550–556. doi: 10.1046/j.1523-1747.2003.12413.x. [DOI] [PubMed] [Google Scholar]
- 22.Janicki CN, Jenkinson SR, Williams NA, Morgan DJ. Loss of CTL function among high-avidity tumor-specific CD8+ T cells following tumor infiltration. Cancer Res. 2008;68:2993–3000. doi: 10.1158/0008-5472.CAN-07-5008. [DOI] [PubMed] [Google Scholar]
- 23.Kouiavskaia DV, Berard CA, Datena E, et al. Vaccination with agonist peptide PSA: 154–163 (155L) derived from prostate specific antigen induced CD8 T-cell response to the native peptide PSA: 154–163 but failed to induce the reactivity against tumor targets expressing PSA: a phase 2 study in patients with recurrent prostate cancer. J Immunother. 2009;32:655–666. doi: 10.1097/CJI.0b013e3181a80e0d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rosenberg SA, Yannelli JR, Yang JC, et al. Treatment of patients with metastatic melanoma with autologous tumor-infiltrating lymphocytes and interleukin 2. J Natl Cancer Inst. 1994;86:1159–1166. doi: 10.1093/jnci/86.15.1159. [DOI] [PubMed] [Google Scholar]
- 25.Zou W. Immunosuppressive networks in the tumour environment and their therapeutic relevance. Nat Rev Cancer. 2005;5:263–274. doi: 10.1038/nrc1586. [DOI] [PubMed] [Google Scholar]
- 26.Woo EY, Chu CS, Goletz TJ, et al. Regulatory CD4(+)CD25(+) T cells in tumors from patients with early-stage non-small cell lung cancer and late-stage ovarian cancer. Cancer Res. 2001;61:4766–4772. [PubMed] [Google Scholar]
- 27.Curiel TJ, Coukos G, Zou L, et al. Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat Med. 2004;10:942–949. doi: 10.1038/nm1093. [DOI] [PubMed] [Google Scholar]
- 28.Marshall NA, Christie LE, Munro LR, et al. Immunosuppressive regulatory T cells are abundant in the reactive lymphocytes of Hodgkin lymphoma. Blood. 2004;103:1755–1762. doi: 10.1182/blood-2003-07-2594. [DOI] [PubMed] [Google Scholar]
- 29.Terabe M, Berzofsky JA. Immunoregulatory T cells in tumor immunity. Curr Opin Immunol. 2004;16:157–162. doi: 10.1016/j.coi.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 30.Zamanakou M, Germenis AE, Karanikas V. Tumor immune escape mediated by indoleamine 2,3-dioxygenase. Immunol Lett. 2007;111:69–75. doi: 10.1016/j.imlet.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 31.Igney FH, Krammer PH. Immune escape of tumors: apoptosis resistance and tumor counterattack. J Leukoc Biol. 2002;71:907–920. [PubMed] [Google Scholar]
- 32.Keir ME, Butte MJ, Freeman GJ, Sharpe AH. PD-1 and Its Ligands in Tolerance and Immunity. Annu Rev Immunol. 2008;26:677–704. doi: 10.1146/annurev.immunol.26.021607.090331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dotti G. Blocking PD-1 in cancer immunotherapy. Blood. 2009;114:1457–1458. doi: 10.1182/blood-2009-05-223412. [DOI] [PubMed] [Google Scholar]
- 34.Rosenberg SA, Aebersold P, Cornetta K, et al. Gene transfer into humans--immunotherapy of patients with advanced melanoma, using tumor-infiltrating lymphocytes modified by retroviral gene transduction. N Engl J Med. 1990;323:570–578. doi: 10.1056/NEJM199008303230904. [DOI] [PubMed] [Google Scholar]
- 35.Bonini C, Ferrari G, Verzeletti S, et al. HSV-TK gene transfer into donor lymphocytes for control of allogeneic graft-versus-leukemia. Science. 1997;276:1719–1724. doi: 10.1126/science.276.5319.1719. [DOI] [PubMed] [Google Scholar]
- 36.Bonini C, Grez M, Traversari C, et al. Safety of retroviral gene marking with a truncated NGF receptor. Nat Med. 2003;9:367–369. doi: 10.1038/nm0403-367. [DOI] [PubMed] [Google Scholar]
- 37.Brenner MK, Heslop HE. Is retroviral gene marking too dangerous to use? Cytotherapy. 2003;5:190–193. doi: 10.1080/14653240310001307. [DOI] [PubMed] [Google Scholar]
- 38.Humeau LM, Binder GK, Lu X, et al. Efficient lentiviral vector-mediated control of HIV-1 replication in CD4 lymphocytes from diverse HIV+ infected patients grouped according to CD4 count and viral load. Mol Ther. 2004;9:902–913. doi: 10.1016/j.ymthe.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 39.Till BG, Jensen MC, Wang J, et al. Adoptive immunotherapy for indolent non-Hodgkin lymphoma and mantle cell lymphoma using genetically modified autologous CD20-specific T cells. Blood. 2008;112:2261–2271. doi: 10.1182/blood-2007-12-128843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Templeton NS, Lasic DD, Frederik PM, Strey HH, Roberts DD, Pavlakis GN. Improved DNA: liposome complexes for increased systemic delivery and gene expression. Nat Biotechnol. 1997;15:647–652. doi: 10.1038/nbt0797-647. [DOI] [PubMed] [Google Scholar]
- 41.Wells DJ. Gene therapy progress and prospects: electroporation and other physical methods. Gene Ther. 2004;11:1363–1369. doi: 10.1038/sj.gt.3302337. [DOI] [PubMed] [Google Scholar]
- 42.Singh H, Manuri PR, Olivares S, et al. Redirecting specificity of T-cell populations for CD19 using the Sleeping Beauty system. Cancer Res. 2008;68:2961–2971. doi: 10.1158/0008-5472.CAN-07-5600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Huang X, Guo H, Kang J, et al. Sleeping Beauty transposon-mediated engineering of human primary T cells for therapy of CD19+ lymphoid malignancies. Mol Ther. 2008;16:580–589. doi: 10.1038/sj.mt.6300404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wilson MH, Coates CJ, George AL., Jr PiggyBac transposon-mediated gene transfer in human cells. Mol Ther. 2007;15:139–145. doi: 10.1038/sj.mt.6300028. [DOI] [PubMed] [Google Scholar]
- 45.Quintarelli C, Dotti G, De Angelis B, et al. Cytotoxic T lymphocytes directed to the Preferentially Expressed Antigen of Melanoma (PRAME) target chronic myeloid leukemia. Blood. 2008;112:1876–1885. doi: 10.1182/blood-2008-04-150045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Montagna D, Maccario R, Locatelli F. Expansion of antileukaemia CTL lines and clones for adoptive cell therapy in paediatric patients given allogeneic haematopoietic stem cell transplantation. Int J Immunogenet. 2008;35:389–393. doi: 10.1111/j.1744-313X.2008.00797.x. [DOI] [PubMed] [Google Scholar]
- 47.Eshhar Z, Waks T, Gross G, Schindler DG. Specific activation and targeting of cytotoxic lymphocytes through chimeric single chains consisting of antibody-binding domains and the gamma or zeta subunits of the immunoglobulin and T-cell receptors. Proc Natl Acad Sci USA. 1993;90:720–724. doi: 10.1073/pnas.90.2.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schumacher TN. T-cell-receptor gene therapy. Nat Rev Immunol. 2002;2:512–519. doi: 10.1038/nri841. [DOI] [PubMed] [Google Scholar]
- 49.Pule M, Finney H, Lawson A. Artificial T-cell receptors. Cytotherapy. 2003;5:211–226. doi: 10.1080/14653240310001488. [DOI] [PubMed] [Google Scholar]
- 50.Dotti G, Heslop HE. Current status of genetic modification of T cells for cancer treatment. Cytotherapy. 2005;7:262–272. doi: 10.1080/14653240510027217. [DOI] [PubMed] [Google Scholar]
- 51.Sadelain M, Brentjens R, Riviere I. The promise and potential pitfalls of chimeric antigen receptors. Curr Opin Immunol. 2009;21:215–223. doi: 10.1016/j.coi.2009.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cooper LJ, Topp MS, Serrano LM, et al. T-cell clones can be rendered specific for CD19: toward the selective augmentation of the graft-versus-B-lineage leukemia effect. Blood. 2003;101:1637–1644. doi: 10.1182/blood-2002-07-1989. [DOI] [PubMed] [Google Scholar]
- 53.Jensen MC, Cooper LJ, Wu AM, Forman SJ, Raubitschek A. Engineered CD20-specific primary human cytotoxic T lymphocytes for targeting B-cell malignancy. Cytotherapy. 2003;5:131–138. doi: 10.1080/14653240310001028. [DOI] [PubMed] [Google Scholar]
- 54.Hombach A, Heuser C, Sircar R, et al. Characterization of a chimeric T-cell receptor with specificity for the Hodgkin's lymphoma-associated CD30 antigen. J Immunother. 1999;22:473–480. doi: 10.1097/00002371-199911000-00001. [DOI] [PubMed] [Google Scholar]
- 55.Savoldo B, Rooney CM, Di Stasi A, et al. Epstein Barr virus specific cytotoxic T lymphocytes expressing the anti-CD30{zeta} artificial chimeric T-cell receptor for immunotherapy of Hodgkin disease. Blood. 2007;110:2620–2630. doi: 10.1182/blood-2006-11-059139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Vera J, Savoldo B, Vigouroux S, et al. T lymphocytes redirected against the kappa light chain of human immunoglobulin efficiently kill mature B lymphocyte-derived malignant cells. Blood. 2006;108:3890–3897. doi: 10.1182/blood-2006-04-017061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kershaw MH, Westwood JA, Parker LL, et al. A phase I study on adoptive immunotherapy using gene-modified T cells for ovarian cancer. Clin Cancer Res. 2006;12:6106–6115. doi: 10.1158/1078-0432.CCR-06-1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lamers CH, Sleijfer S, Vulto AG, et al. Treatment of metastatic renal cell carcinoma with autologous T-lymphocytes genetically retargeted against carbonic anhydrase IX: first clinical experience. J Clin Oncol. 2006;24:e20–e22. doi: 10.1200/JCO.2006.05.9964. [DOI] [PubMed] [Google Scholar]
- 59.Beecham EJ, Ortiz-Pujols S, Junghans RP. Dynamics of tumor cell killing by human T lymphocytes armed with an anti-carcinoembryonic antigen chimeric immunoglobulin T-cell receptor. J Immunother. 2000;23:332–343. doi: 10.1097/00002371-200005000-00006. [DOI] [PubMed] [Google Scholar]
- 60.Rossig C, Bollard CM, Nuchtern JG, Merchant DA, Brenner MK. Targeting of G(D2)-positive tumor cells by human T lymphocytes engineered to express chimeric T-cell receptor genes. Int J Cancer. 2001;94:228–236. doi: 10.1002/ijc.1457. [DOI] [PubMed] [Google Scholar]
- 61.Ahmed N, Ratnayake M, Savoldo B, et al. Regression of experimental medulloblastoma following transfer of HER2-specific T cells. Cancer Res. 2007;67(12):5957–5964. doi: 10.1158/0008-5472.CAN-06-4309. [DOI] [PubMed] [Google Scholar]
- 62.Brentjens RJ, Latouche JB, Santos E, et al. Eradication of systemic B-cell tumors by genetically targeted human T lymphocytes co-stimulated by CD80 and interleukin-15. Nat Med. 2003;9:279–286. doi: 10.1038/nm827. [DOI] [PubMed] [Google Scholar]
- 63.Park JR, Digiusto DL, Slovak M, et al. Adoptive transfer of chimeric antigen receptor re-directed cytolytic T lymphocyte clones in patients with neuroblastoma. Mol Ther. 2007;15:825–833. doi: 10.1038/sj.mt.6300104. [DOI] [PubMed] [Google Scholar]
- 64.Walker RE, Bechtel CM, Natarajan V, et al. Long-term in vivo survival of receptor-modified syngeneic T cells in patients with human immunodeficiency virus infection. Blood. 2000;96:467–474. [PubMed] [Google Scholar]
- 65.Biagi E, Yvon E, Dotti G, et al. Bystander transfer of functional human CD40 ligand from gene-modified fibroblasts to B-chronic lymphocytic leukemia cells. Hum Gene Ther. 2003;14:545–559. doi: 10.1089/104303403764539332. [DOI] [PubMed] [Google Scholar]
- 66.Maher J, Brentjens RJ, Gunset G, Riviere I, Sadelain M. Human T-lymphocyte cytotoxicity and proliferation directed by a single chimeric TCRzeta /CD28 receptor. Nat Biotechnol. 2002;20:70–75. doi: 10.1038/nbt0102-70. [DOI] [PubMed] [Google Scholar]
- 67.Kowolik CM, Topp MS, Gonzalez S, et al. CD28 costimulation provided through a CD19-specific chimeric antigen receptor enhances in vivo persistence and antitumor efficacy of adoptively transferred T cells. Cancer Res. 2006;66:10995–11004. doi: 10.1158/0008-5472.CAN-06-0160. [DOI] [PubMed] [Google Scholar]
- 68.Finney HM, Lawson AD, Bebbington CR, Weir AN. Chimeric receptors providing both primary and costimulatory signaling in T cells from a single gene product. J Immunol. 1998;161:2791–2797. [PubMed] [Google Scholar]
- 69.Imai C, Mihara K, Andreansky M, et al. Chimeric receptors with 4-1BB signaling capacity provoke potent cytotoxicity against acute lymphoblastic leukemia. Leukemia. 2004;18:676–684. doi: 10.1038/sj.leu.2403302. [DOI] [PubMed] [Google Scholar]
- 70.Pule MA, Straathof KC, Dotti G, Heslop HE, Rooney CM, Brenner MK. A chimeric T cell antigen receptor that augments cytokine release and supports clonal expansion of primary human T cells. Mol Ther. 2005;12:933–941. doi: 10.1016/j.ymthe.2005.04.016. [DOI] [PubMed] [Google Scholar]
- 71.Milone MC, Fish JD, Carpenito C, et al. Chimeric Receptors Containing CD137 Signal transduction domains mediate enhanced survival of t cells and increased antileukemic efficacy in vivo. Mol Ther. 2009;17:1453–1464. doi: 10.1038/mt.2009.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Carpenito C, Milone MC, Hassan R, et al. Control of large, established tumor xenografts with genetically retargeted human T cells containing CD28 and CD137 domains. Proc Natl Acad Sci USA. 2009;106:3360–3365. doi: 10.1073/pnas.0813101106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Brentjens R, Riviere I, Hollyman D, et al. Unexpected toxicity of cyclophosphamide folowed by adoptively transferred CD19-targeted T cells in a patient with bulky CLL. Mol Ther. 2009;17 suppl 1 [Abstract] [Google Scholar]
- 74.Xue SA, Gao L, Hart D, et al. Elimination of human leukemia cells in NOD/SCID mice by WT1-TCR gene-transduced human T cells. Blood. 2005;106:3062–3067. doi: 10.1182/blood-2005-01-0146. [DOI] [PubMed] [Google Scholar]
- 75.Stanislawski T, Voss RH, Lotz C, et al. Circumventing tolerance to a human MDM2-derived tumor antigen by TCR gene transfer. Nat Immunol. 2001;2:962–970. doi: 10.1038/ni1001-962. [DOI] [PubMed] [Google Scholar]
- 76.Robbins PF, Li YF, El-Gamil M, et al. Single and dual amino acid substitutions in TCR CDRs can enhance antigen-specific T cell functions. J Immunol. 2008;180:6116–6131. doi: 10.4049/jimmunol.180.9.6116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kuball J, Dossett ML, Wolfl M, et al. Facilitating matched pairing and expression of TCR chains introduced into human T cells. Blood. 2007;109:2331–2338. doi: 10.1182/blood-2006-05-023069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Johnson LA, Morgan RA, Dudley ME, et al. Gene therapy with human and mouse T-cell receptors mediates cancer regression and targets normal tissues expressing cognate antigen. Blood. 2009;114:535–546. doi: 10.1182/blood-2009-03-211714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Berger C, Jensen MC, Lansdorp PM, Gough M, Elliott C, Riddell SR. Adoptive transfer of effector CD8+ T cells derived from central memory cells establishes persistent T cell memory in primates. J Clin Invest. 2008;118:294–305. doi: 10.1172/JCI32103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ahmadzadeh M, Rosenberg SA. IL-2 administration increases CD4+ CD25(hi) Foxp3+ regulatory T cells in cancer patients. Blood. 2006;107:2409–2414. doi: 10.1182/blood-2005-06-2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Liu K, Rosenberg SA. Transduction of an IL-2 gene into human melanoma-reactive lymphocytes results in their continued growth in the absence of exogenous IL-2 and maintenance of specific antitumor activity. J Immunol. 2001;167:6356–6365. doi: 10.4049/jimmunol.167.11.6356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hsu C, Hughes MS, Zheng Z, Bray RB, Rosenberg SA, Morgan RA. Primary human T lymphocytes engineered with a codon-optimized IL-15 gene resist cytokine withdrawal-induced apoptosis and persist long-term in the absence of exogenous cytokine. J Immunol. 2005;175:7226–7234. doi: 10.4049/jimmunol.175.11.7226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ma A, Koka R, Burkett P. Diverse functions of IL-2, IL-15, and IL-7 in lymphoid homeostasis. Annu Rev Immunol. 2006;24:657–679. doi: 10.1146/annurev.immunol.24.021605.090727. [DOI] [PubMed] [Google Scholar]
- 84.Rosenberg SA, Sportes C, Ahmadzadeh M, et al. IL-7 administration to humans leads to expansion of CD8+ and CD4+ cells but a relative decrease of CD4+ T-regulatory cells. J Immunother. 2006;29:313–319. doi: 10.1097/01.cji.0000210386.55951.c2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sportes C, Hakim FT, Memon SA, et al. Administration of rhIL-7 in humans increases in vivo TCR repertoire diversity by preferential expansion of naive T cell subsets. J Exp Med. 2008;205:1701–1714. doi: 10.1084/jem.20071681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Migliaccio M, Amacker M, Just T, et al. Ectopic human telomerase catalytic subunit expression maintains telomere length but is not sufficient for CD8+ T lymphocyte immortalization. J Immunol. 2000;165:4978–4984. doi: 10.4049/jimmunol.165.9.4978. [DOI] [PubMed] [Google Scholar]
- 87.Charo J, Finkelstein SE, Grewal N, Restifo NP, Robbins PF, Rosenberg SA. Bcl-2 overexpression enhances tumor-specific T-cell survival. Cancer Res. 2005;65:2001–2008. doi: 10.1158/0008-5472.CAN-04-2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gimmi CD, Freeman GJ, Gribben JG, Gray G, Nadler LM. Human T-cell clonal anergy is induced by antigen presentation in the absence of B7 costimulation. Proc Natl Acad Sci USA. 1993;90:6586–6590. doi: 10.1073/pnas.90.14.6586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Stephan MT, Ponomarev V, Brentjens RJ, et al. T cell-encoded CD80 and 4-1BBL induce auto- and transcostimulation, resulting in potent tumor rejection. Nat Med. 2007;13:1440–1449. doi: 10.1038/nm1676. [DOI] [PubMed] [Google Scholar]
- 90.Paya CV, Fung JJ, Nalesnik MA, et al. Epstein-Barr virus-induced posttransplant lymphoproliferative disorders. ASTS/ASTP EBV-PTLD Task Force and The Mayo Clinic Organized International Consensus Development Meeting. Transplantation. 1999;68:1517–1525. doi: 10.1097/00007890-199911270-00015. [DOI] [PubMed] [Google Scholar]
- 91.Straathof KC, Savoldo B, Heslop HE, Rooney CM. Immunotherapy for post-transplant lymphoproliferative disease. Br J Haematol. 2002;118:728–740. doi: 10.1046/j.1365-2141.2002.03594.x. [DOI] [PubMed] [Google Scholar]
- 92.Savoldo B, Heslop HE, Rooney CM. The use of cytotoxic t cells for the prevention and treatment of epstein-barr virus induced lymphoma in transplant recipients. Leuk Lymphoma. 2000;39:455–464. doi: 10.3109/10428190009113376. [DOI] [PubMed] [Google Scholar]
- 93.Comoli P, Labirio M, Basso S, et al. Infusion of autologous Epstein-Barr virus (EBV)-specific cytotoxic T cells for prevention of EBV-related lymphoproliferative disorder in solid organ transplant recipients with evidence of active virus replication. Blood. 2002;99:2592–2598. doi: 10.1182/blood.v99.7.2592. [DOI] [PubMed] [Google Scholar]
- 94.De Angelis B, Dotti G, Quintarelli C, et al. Generation of Epstein-Barr-Virus-specific cytotoxic T lymphocytes resistant to the immunosuppressive drug tacrolimus (FK506) Blood. 2009 doi: 10.1182/blood-2009-07-230482. [In Press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Brein J, Mancao C, Straathof K, et al. Generation of EBV-specific cytotxic T-cells thta are resistant to calcineurin inhibitors for the treatment of post-transplant lymphoproliferative disease. Blood. 2009 doi: 10.1182/blood-2009-07-228387. [In Press] [DOI] [PubMed] [Google Scholar]
- 96.Moutsopoulos NM, Wen J, Wahl SM. TGF-beta and tumors--an illfated alliance. Curr Opin Immunol. 2008;20:234–240. doi: 10.1016/j.coi.2008.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Foster AE, Dotti G, Lu A, et al. Antitumor activity of EBV-specific T lymphocytes transduced with a dominant negative TGF-beta receptor. J Immunother. 2008;31:500–505. doi: 10.1097/CJI.0b013e318177092b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mellor AL, Munn DH. IDO expression by dendritic cells: tolerance and tryptophan catabolism. Nat Rev Immunol. 2004;4:762–774. doi: 10.1038/nri1457. [DOI] [PubMed] [Google Scholar]
- 99.Curti A, Trabanelli S, Salvestrini V, Baccarani M, Lemoli RM. The role of indoleamine 2,3-dioxygenase in the induction of immune tolerance: focus on hematology. Blood. 2009;113:2394–2401. doi: 10.1182/blood-2008-07-144485. [DOI] [PubMed] [Google Scholar]
- 100.Munn DH, Sharma MD, Baban B, et al. GCN2 kinase in T cells mediates proliferative arrest and anergy induction in response to indoleamine 2,3-dioxygenase. Immunity. 2005;22:633–642. doi: 10.1016/j.immuni.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 101.Nagata S, Golstein P. The Fas death factor. Science. 1995;267:1449–1456. doi: 10.1126/science.7533326. [DOI] [PubMed] [Google Scholar]
- 102.O'Connell J, O'Sullivan GC, Collins JK, Shanahan F. The Fas counterattack: Fas-mediated T cell killing by colon cancer cells expressing Fas ligand. J Exp Med. 1996;184:1075–1082. doi: 10.1084/jem.184.3.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hohlbaum AM, Moe S, Marshak-Rothstein A. Opposing effects of transmembrane and soluble Fas ligand expression on inflammation and tumor cell survival. J Exp Med. 2000;191:1209–1220. doi: 10.1084/jem.191.7.1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Dilloo D, Bacon K, Holden W, et al. Combined chemokine and cytokine gene transfer enhances antitumor immunity. Nat Med. 1996;2:1090–1095. doi: 10.1038/nm1096-1090. [DOI] [PubMed] [Google Scholar]
- 105.Gao JQ, Okada N, Mayumi T, Nakagawa S. Immune cell recruitment and cell-based system for cancer therapy. Pharm Res. 2008;25:752–768. doi: 10.1007/s11095-007-9443-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Poppema S, Potters M, Visser L, van den Berg AM. Immune escape mechanisms in Hodgkin's disease. Ann Oncol. 1998;9 Suppl 5:S21–S24. doi: 10.1093/annonc/9.suppl_5.s21. [DOI] [PubMed] [Google Scholar]
- 107.van den BA, Visser L, Poppema S. High expression of the CC chemokine TARC in Reed-Sternberg cells. A possible explanation for the characteristic T-cell infiltratein Hodgkin's lymphoma. Am J Pathol. 1999;154:1685–1691. doi: 10.1016/S0002-9440(10)65424-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kershaw MH, Wang G, Westwood JA, et al. Redirecting migration of T cells to chemokine secreted from tumors by genetic modification with CXCR2. Hum Gene Ther. 2002;13:1971–1980. doi: 10.1089/10430340260355374. [DOI] [PubMed] [Google Scholar]
- 109.Hacein-Bey-Abina S, Garrigue A, Wang GP, et al. Insertional oncogenesis in 4 patients after retrovirus-mediated gene therapy of SCID-X1. J Clin Invest. 2008;118:3132–3142. doi: 10.1172/JCI35700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ciceri F, Bonini C, Marktel S, et al. Antitumor effects of HSV-TK-engineered donor lymphocytes after allogeneic stem-cell transplantation. Blood. 2007;109:4698–4707. doi: 10.1182/blood-2006-05-023416. [DOI] [PubMed] [Google Scholar]
- 111.Ciceri F, Bonini C, Stanghellini MT, et al. Infusion of suicide-gene-engineered donor lymphocytes after family haploidentical haemopoietic stem-cell transplantation for leukaemia (the TK007 trial): a non-randomised phase I-II study. Lancet Oncol. 2009;10:489–500. doi: 10.1016/S1470-2045(09)70074-9. [DOI] [PubMed] [Google Scholar]
- 112.Traversari C, Marktel S, Magnani Z, et al. The potential immunogenicity of the TK suicide gene does not prevent full clinical benefit associated with the use of TK-transduced donor lymphocytes in HSCT for hematologic malignancies. Blood. 2007;109:4708–4715. doi: 10.1182/blood-2006-04-015230. [DOI] [PubMed] [Google Scholar]
- 113.Thomis DC, Marktel S, Bonini C, et al. A Fas-based suicide switch in human T cells for the treatment of graft-versus-host disease. Blood. 2001;97:1249–1257. doi: 10.1182/blood.v97.5.1249. [DOI] [PubMed] [Google Scholar]
- 114.Straathof KC, Pule MA, Yotnda P, et al. An inducible caspase 9 safety switch for T-cell therapy. Blood. 2005;105:4247–4254. doi: 10.1182/blood-2004-11-4564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Tey SK, Dotti G, Rooney CM, Heslop HE, Brenner MK. Inducible caspase 9 suicide gene to improve the safety of allodepleted T cells after haploidentical stem cell transplantation. Biol Blood Marrow Transplant. 2007;13:913–924. doi: 10.1016/j.bbmt.2007.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Iuliucci JD, Oliver SD, Morley S, et al. Intravenous safety and pharmacokinetics of a novel dimerizer drug, AP1903, in healthy volunteers. J Clin Pharmacol. 2001;41:870–879. doi: 10.1177/00912700122010771. [DOI] [PubMed] [Google Scholar]
- 117.Introna M, Barbui AM, Bambacioni F, et al. Genetic modification of human T cells with CD20: a strategy to purify and lyse transduced cells with anti-CD20 antibodies. Hum Gene Ther. 2000;11:611–620. doi: 10.1089/10430340050015798. [DOI] [PubMed] [Google Scholar]
- 118.Hacein-Bey-Abina S, Von Kalle C, Schmidt M, et al. A serious adverse event after successful gene therapy for X-linked severe combined immunodeficiency. N Engl J Med. 2003;348:255–256. doi: 10.1056/NEJM200301163480314. [DOI] [PubMed] [Google Scholar]
- 119.Perez EE, Wang J, Miller JC, et al. Establishment of HIV-1 resistance in CD4+ T cells by genome editing using zinc-finger nucleases. Nat Biotechnol. 2008;26:808–816. doi: 10.1038/nbt1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Montini E, Cesana D, Schmidt M, et al. Hematopoietic stem cell gene transfer in a tumor-prone mouse model uncovers low genotoxicity of lentiviral vector integration. Nat Biotechnol. 2006;24:687–696. doi: 10.1038/nbt1216. [DOI] [PubMed] [Google Scholar]
- 121.Koehne G, Doubrovin M, Doubrovina E, et al. Serial in vivo imaging of the targeted migration of human HSV-TK-transduced antigen-specific lymphocytes. Nat Biotechnol. 2003;21:405–413. doi: 10.1038/nbt805. [DOI] [PubMed] [Google Scholar]
- 122.Soghomonyan S, Hajitou A, Rangel R, et al. Molecular PET imaging of HSV1-tk reporter gene expression using [18F]FEAU. Nat Protoc. 2007;2:416–423. doi: 10.1038/nprot.2007.49. [DOI] [PubMed] [Google Scholar]
- 123.Dotti G, Tian M, Savoldo B, et al. Repetitive noninvasive monitoring of HSV1-tk expressing T-cells intravenously infused into nonhuman primates using PET-CT with 18F-FEAU. Mol Imaging. 2009;8(4):230–237. [PMC free article] [PubMed] [Google Scholar]
- 124.Yaghoubi SS, Jensen MC, Satyamurthy N, et al. Noninvasive detection of therapeutic cytolytic T cells with 18F–FHBG PET in a patient with glioma. Nat Clin Pract Oncol. 2009;6:53–58. doi: 10.1038/ncponc1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Kirouac DC, Zandstra PW. The systematic production of cells for cell therapies. Cell Stem Cell. 2008;3:369–381. doi: 10.1016/j.stem.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 126.Carswell KS, Papoutsakis ET. Culture of human T cells in stirred bioreactors for cellular immunotherapy applications: shear, proliferation, and the IL-2 receptor. Biotechnol Bioeng. 2000;68:328–338. doi: 10.1002/(sici)1097-0290(20000505)68:3<328::aid-bit11>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 127.Avgoustiniatos ES, Hering BJ, Rozak PR, et al. Commercially available gas-permeable cell culture bags may not prevent anoxia in cultured or shipped islets. Transplant Proc. 2008;40:395–400. doi: 10.1016/j.transproceed.2008.01.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Daly T, Royal RE, Kershaw MH, et al. Recognition of human colon cancer by T cells transduced with a chimeric receptor gene. Cancer Gene Ther. 2000;7:284–291. doi: 10.1038/sj.cgt.7700121. [DOI] [PubMed] [Google Scholar]
- 129.Dall P, Herrmann I, Durst B, et al. In vivo cervical cancer growth inhibition by genetically engineered cytotoxic T cells. Cancer Immunol Immunother. 2005;54:51–60. doi: 10.1007/s00262-004-0569-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Wang G, Chopra RK, Royal RE, Yang JC, Rosenberg SA, Hwu P. A T cell-independent antitumor response in mice with bone marrow cells retrovirally transduced with an antibody/Fc-gamma chain chimeric receptor gene recognizing a human ovarian cancer antigen. Nat Med. 1998;4:168–172. doi: 10.1038/nm0298-168. [DOI] [PubMed] [Google Scholar]
- 131.Mezzanzanica D, Canevari S, Mazzoni A, et al. Transfer of chimeric receptor gene made of variable regions of tumor-specific antibody confers anticarbohydrate specificity on T cells. Cancer Gene Ther. 1998;5:401–407. [PubMed] [Google Scholar]
- 132.Wilkie S, Picco G, Foster J, et al. Retargeting of human T cells to tumor-associated MUC1: the evolution of a chimeric antigen receptor. J Immunol. 2008;180:4901–4909. doi: 10.4049/jimmunol.180.7.4901. [DOI] [PubMed] [Google Scholar]
- 133.Haynes NM, Trapani JA, Teng MW, et al. Single-chain antigen recognition receptors that costimulate potent rejection of established experimental tumors. Blood. 2002;100:3155–3163. doi: 10.1182/blood-2002-04-1041. [DOI] [PubMed] [Google Scholar]
- 134.Morgenroth A, Cartellieri M, Schmitz M, et al. Targeting of tumor cells expressing the prostate stem cell antigen (PSCA) using genetically engineered T-cells. Prostate. 2007;67:1121–1131. doi: 10.1002/pros.20608. [DOI] [PubMed] [Google Scholar]
- 135.Gong MC, Chang SS, Sadelain M, Bander NH, Heston WD. Prostate-specific membrane antigen (PSMA)-specific monoclonal antibodies in the treatment of prostate and other cancers. Cancer Metastasis Rev. 1999;18:483–490. doi: 10.1023/a:1006308826967. [DOI] [PubMed] [Google Scholar]
- 136.McGuinness RP, Ge Y, Patel SD, et al. Anti-tumor activity of human T cells expressing the CC49-zeta chimeric immune receptor. Hum Gene Ther. 1999;10:165–173. doi: 10.1089/10430349950018968. [DOI] [PubMed] [Google Scholar]
- 137.Willemsen RA, Ronteltap C, Chames P, Debets R, Bolhuis RL. T cell retargeting with MHC class I-restricted antibodies: the CD28 costimulatory domain enhances antigen-specific cytotoxicity and cytokine production. J Immunol. 2005;174:7853–7858. doi: 10.4049/jimmunol.174.12.7853. [DOI] [PubMed] [Google Scholar]
- 138.Yun CO, Nolan KF, Beecham EJ, Reisfeld RA, Junghans RP. Targeting of T lymphocytes to melanoma cells through chimeric anti-GD3 immunoglobulin T-cell receptors. Neoplasia. 2000;2:449–459. doi: 10.1038/sj.neo.7900108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Yvon E, Del Vecchio M, Savoldo B, et al. Immunotherapy of metastatic melanoma using genetically engineered GD2-specific T cells. Clin Cancer Res. 2009 doi: 10.1158/1078-0432.CCR-08-3163. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Kershaw MH, Westwood JA, Zhu Z, Witte L, Libutti SK, Hwu P. Generation of gene-modified T cells reactive against the angiogenic kinase insert domain-containing receptor (KDR) found on tumor vasculature. Hum Gene Ther. 2000;11:2445–2452. doi: 10.1089/10430340050207939. [DOI] [PubMed] [Google Scholar]
- 141.Niederman TM, Ghogawala Z, Carter BS, Tompkins HS, Russell MM, Mulligan RC. Antitumor activity of cytotoxic T lymphocytes engineered to target vascular endothelial growth factor receptors. Proc Natl Acad Sci USA. 2002;99:7009–7014. doi: 10.1073/pnas.092562399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Jensen M, Tan G, Forman S, Wu AM, Raubitschek A. CD20 is a molecular target for scFvFc:zeta receptor redirected T cells: implications for cellular immunotherapy of CD20+ malignancy. Biol Blood Marrow Transplant. 1998;4:75–83. doi: 10.1053/bbmt.1998.v4.pm9763110. [DOI] [PubMed] [Google Scholar]
- 143.James SE, Greenberg PD, Jensen MC, et al. Antigen sensitivity of CD22-specific chimeric TCR is modulated by target epitope distance from the cell membrane. J Immunol. 2008;180:7028–7038. doi: 10.4049/jimmunol.180.10.7028. [DOI] [PMC free article] [PubMed] [Google Scholar]