Abstract
Despite an accumulating body of literature addressing racial/ethnic disparities in children’s health and health care, there have been few published studies of interventions that have been successful in eliminating these disparities. The objectives of this article, therefore, are to (1) describe 3 interventions that have been successful in eliminating racial/ethnic disparities in children’s health and health care, (2) high-light tips and pitfalls regarding devising, implementing, and evaluating pediatric disparities interventions, and (3) propose a research agenda for pediatric disparities interventions. Key characteristics of the 3 successful interventions include rigorous study designs; large sample sizes; appropriate comparison groups; community-based interventions that are culturally and linguistically sensitive and involve collaboration with participants; research staff from the same community as the participants; appropriate blinding of outcomes assessors; and statistical adjustment of outcomes for relevant covariates. On the basis of these characteristics, I propose tips, pitfalls, an approach, and a research agenda for devising, implementing, and evaluating successful pediatric disparities interventions. Examination of 3 successful interventions indicates that pediatric health care disparities can be eliminated. Achievement of this goal requires an intervention that is rigorous, evidence-based, and culturally and linguistically appropriate. The intervention must also include community collaboration, minimize attrition, adjust for potential confounders, and incorporate mechanisms for sustainability.
Keywords: disparities, minority groups, children, intervention studies, African Americans, Hispanic Americans, Native Americans
Published studies are accumulating on racial/ethnic disparities in children’s health and health care. Recent national data, for example, reveal that racial/ethnic minority children in the United States experience multiple disparities in medical and oral health, access to care, and use of services.1 Indeed, these data reveal that minority children in America often face a “triple threat” of greater risks of suboptimal medical and oral health status, impaired access to medical and dental care, and lower receipt of prescription medications and essential medical and dental services. The authors of this nationwide analysis1 also documented that certain pediatric disparities are particularly marked for specific racial/ethnic groups and that multiracial children experience many disparities.
Despite the accumulating body of literature addressing racial/ethnic disparities in children’s health and health care, there have been few published studies of rigorous interventions that specifically have targeted and successfully eliminated these disparities. In addition, previous work has neither examined the key elements of the few such successful interventions nor provided practical guidance on how to devise, implement, and evaluate pediatric disparities interventions. The objectives of this article, therefore, are to (1) describe several interventions that have been successful in eliminating racial/ethnic disparities in children’s health and health care, (2) highlight tips and pitfalls regarding devising, implementing, and evaluating pediatric disparities interventions, and (3) propose a research agenda for pediatric disparities interventions.
EXAMPLES OF SUCCESSFUL PEDIATRIC DISPARITIES INTERVENTIONS
In the following sections, 3 examples of published randomized, controlled trials (RCTs) of interventions that have been successful in reducing or eliminating racial/ethnic disparities in children’s health and health care are examined. These studies were identified via a PubMed search of interventions that targeted racial/ethnic disparities in children; they were selected because they (1) are particularly cogent cases of the reduction or elimination of pediatric disparities, (2) targeted 3 major US racial/ethnic minority groups (Native Americans, African Americans, and Latinos) that are considered to experience some of the most stark pediatric disparities and represent some of the most underserved populations of children, and (3) were methodologically rigorous.
Increasing Breastfeeding Rates in Native American Infants
Native American infants have some of the lowest rates of breastfeeding among US racial/ethnic groups, with only 61% ever initiating breastfeeding, compared with 75% in non-Latino white infants.2 In a population-based observational study of a Navajo community, Wright et al3 examined the impact of a breastfeeding-promotion program on breastfeeding rates. Before intervention implementation, the researchers used qualitative approaches, including ethnographic interviews and participant observation, along with a survey, to identify factors associated with infant feeding practices in the Navajo community.4–6 The qualitative research findings were then used to develop a culturally sensitive breastfeeding-promotion intervention specifically intended to overcome breastfeeding obstacles. This 1-year intervention had 3 components: (1) a community intervention that consisted of radio public-service announcements, a video, a billboard message, and t-shirts for infants supplied through the Supplemental Nutrition Program for Women, Infants, and Children (WIC); (2) a health care system intervention composed of a 3-day health care provider conference on lactation management, formation of a task force, and videotaped instruction for WIC caseworkers; and (3) breastfeeding education for families, including use of a video, several brochures, and a tribal foster-grandparent program.7
To assess the impact of the breastfeeding intervention, medical records were reviewed for all infants born in 1 Navajo community during the year before implementation (n = 977) and the year after intervention implementation (n = 858).3 The main study outcome was postintervention changes in the proportions that were exclusively breastfeeding; other outcomes included incidence of common infant illnesses in the first year and feeding-group illness incidence.
The proportion of infants exclusively breastfed for any period of time significantly increased after the intervention from 16% to 55%. After the intervention, the proportion of infants fed formula from birth decreased from 84% to 45% (P < .0004), the proportion of infants ever breastfed increased from 71% to 81% (P < .001), the mean age of formula introduction increased from 12 to 49 days (P < .001), and the mean breastfeeding duration increased from 101 to 132 days (P < .001) among infants ever breastfeeding. The proportion of infants diagnosed with pneumonia and gastroenteritis also declined significantly after the intervention. Feeding-group–specific rates of illnesses were unchanged, however, indicating that the observed reductions were attributable to increases in breastfeeding.
Enhancing HIV-Preventive Behaviors in African-American Adolescent Girls
African-American adolescent girls have the highest risk of contracting HIV/AIDS of any racial/ethnic group of female adolescents in the United States, accounting for more than two thirds of new HIV/AIDS cases among adolescent girls. This population has more than quadruple the number of cases than white female adolescents, although their total population is far smaller.8 In an RCT, DiClemente et al9 evaluated the efficacy of an HIV-prevention intervention for African-American adolescent girls. Researchers collaborated with African-American girls in the community to devise the study protocol. The theoretical framework for the intervention was derived from social cognitive theory10 and the theory of gender and power.11 The intervention consisted of interactive group sessions that focused on racial/ethnic and gender pride, HIV knowledge, communication, condom-use skills, and healthy relationships. Sessions were led by a trained health educator and 2 peer educators who were all African-American females. The comparison group attended sessions that addressed exercise and nutrition. All intervention- and comparison-group participants attended four 4-hour sessions on consecutive Saturdays at a family medicine clinic; sessions were attended by an average of 10 to 12 participants.
The study objective was to evaluate the efficacy of the intervention in reducing sexual risk behaviors, sexually transmitted diseases, and pregnancy and in enhancing mediators of HIV-preventive behaviors.9 Subjects consisted of 522 sexually experienced African-American girls 14 to 18 years old enrolled at 4 community health agencies. Outcome measures included consistent condom use (during every episode of vaginal intercourse), sexual behaviors, observed condom-application skills, sexually transmitted infections, self-reported pregnancy, and mediators of HIV-preventive behaviors. Outcomes were assessed 6 and 12 months after enrollment.
Compared with the control group, girls in the intervention group had significantly higher adjusted odds over the entire 12-month period of reported condom use in the previous 30 days (adjusted odds ratio [aOR]: 2.0 [95% confidence interval (CI): 1.28 –3.17]) and previous 6months (aOR: 2.30 [95% CI: 1.51–3.50]) and condom use at last intercourse (aOR: 3.94 [95% CI: 2.58–6.03]) and were significantly less likely to have had a new vaginal sex partner in the past 30 days (aOR: 0.40 [95% CI: 0.19–0.82]).9 Girls in the intervention group were also significantly more likely than controls at the 12-month assessment to apply condoms to sex partners (adjusted relative change: 38%; P < .001), have better condom-application skills (adjusted relative change: 32%; P < .001), a higher percentage of condom-protected sex acts, fewer unprotected vaginal sex acts in the past 6 months (adjusted relative change: −45%; P = .001), and higher adjusted scores on measures of mediators including HIV knowledge, condom attitudes, condom barriers, condom-use self-efficacy, and frequency with which HIV-preventive practices were discussed with partners. Compared with controls, girls in the intervention group also had a lower adjusted risk of chlamydia infections (aOR: 0.17 [95% CI: 0.03– 0.92]) and a statistically nonsignificant trend toward reduced risk of self-reported pregnancy (aOR: 0.53 [95% CI: 0.27–1.03]; P = .06).
The authors concluded that a culturally congruent, gender-tailored intervention for African-American adolescent girls can enhance HIV-preventive behaviors, skills, and mediators, and might have the potential to reduce pregnancy and chlamydia infection.9
Insuring Uninsured Latino Children
Latinos continue to be the most uninsured racial/ethnic group of US children. In 2007, 20% of Latino children had no health insurance, compared with 7% of white, 12% of African- American, and 12% of Asian/Pacific Islander children.12 In an RCT, Flores et al13 evaluated the effectiveness of a community-based case manager intervention in insuring uninsured Latino children. Before intervention implementation, the investigators conducted qualitative research by using 6 focus groups of parents of uninsured Latino children. The groups identified reasons why parents were unable to insure uninsured Latino children in a state in which all low-income children were eligible for insurance.14 The qualitative research findings were then used to develop a culturally sensitive, linguistically appropriate intervention that was aimed at eliminating barriers to insuring uninsured children.
The intervention consisted of assignment of the uninsured child and his or her family to a community-based case manager, who was a bilingual Latina caseworker who had attended a 1-day intensive training session and was from the same communities as the participants.13 Case managers performed the following functions for intervention children and their families: (1) provided information on types of insurance programs available and the application process; (2) provided information and assistance on program eligibility requirements; (3) completed the child’s insurance application with the parent and submitted the application for the family; (4) expedited final coverage decisions by early and frequent contact with the Division of Medical Assistance (DMA) (the state agency that administers Medicaid in Massachusetts) or the Department of Public Health (DPH) (the state agency that is responsible for the Children’s Medical Security Plan, which insures non–Medicaid-eligible children in Massachusetts, including noncitizens); (5) served as a family advocate by being the liaison between the family and the DMA or DPH; and (6) rectified with the DMA and DPH situations in which a child was inappropriately deemed ineligible for insurance or had coverage inappropriately discontinued.13 The control group received only traditional Medicaid and State Children’s Health Insurance Program (SCHIP) outreach and enrollment.
The study outcomes were receipt of health insurance, coverage continuity, time interval to obtain coverage, and parental satisfaction with the process of obtaining insurance for their children. All participants were contacted monthly for 1 year to monitor outcomes by a researcher who was blinded to group assignment.
A total of 139 subjects were randomly assigned to the intervention and 136 to the control group. Children in the intervention group were more likely than control children to obtain health insurance (96% vs 57%; P <.0001) and had more than double the adjusted likelihood (adjusted relative risk: 2.30 [95% CI: 1.87–2.81]) and 8 times the adjusted odds (a OR: 7.78 [95% CI: 5.20–11.64]) of obtaining insurance. Seventy-eight percent of the children in the intervention group were continuously insured versus 30% of the controls (P < .0001). In addition, children in the intervention group obtained insurance more quickly (mean: 87.5 vs 134.8 days; P < .009), and their parents were more satisfied with the process of obtaining insurance (P < .0001).
The authors concluded that community-based case managers are more effective than traditional Medicaid/State Children’s Health Insurance Program outreach and enrollment in insuring uninsured Latino children. They also stated that case management may be a useful mechanism for further reducing the number of uninsured children, especially among high-risk populations. 13 This intervention also was found to have successfully eliminated a racial/ethnic disparity, given that the uninsurance rate among Latino children receiving the intervention was 4%, compared with national uninsurance rates of 21% for Latino children and 7% of non-Latino white children at the time when the study was conducted.
Comparison of Selected Features of Successful Disparities Interventions
It is useful to compare and contrast selected characteristics of the 3 featured successful interventions (Table 1). Two of the 3 studies were RCTs. The RCT is generally considered to be the gold standard in medical research because of its rigor, objectivity, and power to minimize bias.15,16 When RCTs are not feasible or ethical or when they are too expensive, however, observational studies are a suitable alternative research design.17 This was the case with the Navajo breastfeeding intervention, 3 because it would not have been ethical or feasible to randomly assign infants to breast or formula feeding.
TABLE 1.
Comparison of Selected Features of 3 Interventions That Were Successful in Eliminating Racial/Ethnic Disparities in Children’s Health and Health Care
| Intervention Characteristic | Native American Breastfeeding Intervention |
African-American HIV- Prevention Intervention |
Latino Health Insurance Intervention |
|---|---|---|---|
| Study design | Observational pre/post (retrospective) | RCT | RCT |
| Total sample size, N | 1835 | 522 | 275 |
| Comparison/control group | + | + | + |
| Community based | + | + | + |
| Culturally and linguistically sensitive | + | + | + |
| Intervention included collaboration with study participants and families | + | + | + |
| Preliminary qualitative work performed in community | + | − | + |
| Intervention components | Community social marketing; health care system intervention; family education | Interactive educational group sessions at family medicine clinic | Community-based case managers |
| Intervention included bilingual (when relevant) personnel or peers from same community and racial/ethnic group | + | + | + |
| Blinding of researchers (assessors) to group allocation | Partial | − | + |
| Blinding of participants to group allocation | Not applicable | − | − |
| Duration of monitoring outcomes, y | 1 | 1 | 1 |
| Statistical analysis included multivariable adjustment of outcomes | − | + | + |
All 3 studies had large sample sizes of hundreds or thousands of participants, which are crucial for achieving sufficient statistical power to detect important clinical differences in outcomes. The 3 studies also included relevant comparison groups within the racial/ethnic population being studied; these comparison groups are critical for demonstrating comparative improvement in outcomes. Some might argue that a suitable comparison group in a disparities intervention study should consist of white subjects, to demonstrate reduction or elimination of the disparity in comparison to outcome rates in whites. This approach, however, may not only be unfeasible or unethical but, more importantly, it goes beyond the scientific and conceptual frameworks of disparity reduction/elimination, which focus on significantly reducing an adverse health care outcome within a high-risk population.
All 3 interventions were community based and culturally and linguistically sensitive. In addition, the interventions included collaboration with study participants and families, and 2 studies devised the intervention on the basis of preliminary qualitative work performed in the community (Table 1). All 4 of these components are critical for ensuring that the intervention is tailored to the target population and has a high probability of effectiveness.
The 3 studies had diverse components in the individual interventions, but all 3 interventions included bilingual (when relevant) personnel or peers from the same community and racial/ethnic group as the participants (Table 1).
Blinding of research team members who were assessing outcomes is critical for preventing ascertainment bias, 18 especially for more subjective outcomes. Two of the studies included at least partial blinding of the assessors. Blinding of participants to group allocation is challenging in community-based disparities research, because the participants and families often realize immediately whether the intervention was received, and none of the 3 studies blinded its participants. All 3 studies monitored outcomes for 1 year, and 2 performed multivariable adjustment of outcomes to control for relevant potential confounders.
TIPS FOR AND PITFALLS IN CONDUCTING DISPARITIES-ELIMINATION INTERVENTIONS
In this section, we examine tips for and pitfalls in successfully conducting disparities-elimination interventions on the basis of the 3 interventions reviewed above and personal perspectives and experiences from my 8 years as a principal investigator on 3 RCTs of disparities interventions.
Tips
Incorporate Community Collaboration in All Study Phases
Collaboration with the community throughout all study phases can be an important determinant of whether a disparities intervention study will succeed or fail. Community engagement and cooperation are usually essential when initiating a study and obtaining institutional review board (IRB) approval, particularly when the study is community based. Lack of community collaboration may seriously hinder or prevent participant recruitment and follow-up. Failure to sustain community collaboration and involvement at the study’s conclusion and during the dissemination phase may foster resentment and the perception that residents were used as “guinea pigs,” preclude future studies, and hinder applying study findings to improving the health and health care of children.
Community collaboration can be achieved through partnerships with community leaders and community-based organizations, having community members serve on the study advisory committee and IRB, and partnering with community-based organizations and small businesses to recruit participants and disseminate study findings.
Consider Qualitative Approaches in the Initial Study Phase
Focus groups, ethnographic interviews, and other qualitative approaches can be powerful tools to use when devising and implementing successful disparities interventions. Properly executed qualitative approaches can result in instant community engagement and collaboration; permit an evidence-based framework for intervention development and tailoring; and ensure that the intervention is relevant, feasible, and culturally appropriate. For example, in developing and implementing an intervention to insure uninsured Latino children,13 focus groups of parents of uninsured Latino children14 allowed our research team to engage and collaborate with the local Latino community, confirm several hypotheses about key barriers to insuring children (such as lack of knowledge about programs and eligibility), reject certain hypotheses in the literature (such as that families did not want to insure their uninsured children), obtain new relevant information (such as system problems and misinformation from insurance representatives), tailor the intervention to families’ needs and priorities, and obtain pilot data regarding the acceptability and potential feasibility of the intervention.
Carefully Calculate Power and Sample Size
Considerable investments of time, money, and effort often are required to successfully execute and complete a disparities intervention. One of the most tragic, disastrous, and preventable outcomes occurs when an investigator realizes at the conclusion of a study that it is underpowered to detect a statistically significant difference between study groups. This adverse outcome can be avoided by carefully calculating power and sample size well ahead of the initiation of the intervention, and confirming feasibility by collecting pilot data on realistic participant recruitment target numbers.
Anticipate Substantial Attrition
Even with careful power and sample-size calculations and extensive pilot work, a disparities intervention can be doomed to failure if substantial participant attrition occurs. In my experience, attrition is particularly salient and challenging when one is working with disadvantaged populations, the members of which often have limited financial resources, are frequently highly mobile and transient, are challenged by chaotic lives, and not infrequently confront multiple competing demands. In 2 RCTs of disparities interventions, 13,19 we experienced attrition rates of 28% to 40%. We therefore always build an attrition rate of 40% into power and sample-size calculations for community-based RCTs.
Employ Study Personnel From the Community
Our research teams have found that employing personnel from the study community is invaluable because it (1) establishes immediate community collaboration, (2) frequently results in greater engagement from study staff, who are highly invested in their community of residence, (3) creates strong bonds between participants and research staff because of the shared community, (4) enhances empathy for fellow community residents, (5) raises awareness of current and potential barriers to intervention success and practical mechanisms for overcoming barriers, and (6) provides employment in communities that frequently have high levels of unemployment. Of course, proper training on confidentiality should be a priority for personnel hired from the community, given that they may handle the protected health information of study participants who live in their community.
Provide Participation Incentives
Our research teams have found that study participants view participation incentives as appropriate rewards and important gestures of respect for the often considerable investments of time and effort required for participants and their families to participate in an intervention study. In addition to an enrollment incentive, smaller incentives for each follow-up assessment completed and a larger incentive at study completion can minimize attrition and ensure that each participant completes the study.
Use Multiple Approaches to Ensure Optimal Participant Follow-up
Because our intervention studies frequently have enrolled participants in communities with limited resources, high mobility, and occasional lack of access to a consistent telephone number, our research teams routinely collect multiple telephone numbers (home, cell, work, pager, and those of relatives and friends) and addresses (home, work, and those of relatives and friends) for each participant in an effort to minimize attrition. In addition, when multiple means of communication fail, research staff make repeated home visits to avoid dropping participants from the study.
Adjust for Key Covariates in Analyzing Outcomes
The main study outcomes may be subject to substantial confounding by relevant covariates such as family income, parental education, language barriers, and severity of the child’s illness. Although randomization is a powerful mechanism for eliminating many baseline intergroup differences, such differences may still occur or even arise during the course of a study. Failure to adjust for such covariates through block randomization, multivariable analyses, stratification, or other relevant statistical procedures may lead to confounding and false-positive or false-negative conclusions regarding the efficacy of an intervention.
Pitfalls
IRB Approval
Disparities intervention studies and community-based research are still relatively new entrants to the medical research field, so it has been our experience that IRB members may have variable familiarity with and expertise in these types of research (particularly in institutions with a heavy focus on basic science). The result can be delayed IRB approval, unnecessary protocol changes, or even outright protocol rejection. In addition, members of IRBs may have limited experience with commonly faced obstacles in disparities intervention research, such as recruitment challenges and difficulties in working with poor, inner-city, immigrant, uninsured, or limited English-proficient populations. Our research teams have overcome these pitfalls by establishing early relationships with IRBs, preparing protocols with extra attention to rigor and additional explanations of health services research concepts, and encouraging disparities researchers and community members to apply for open IRB positions.
Attrition
Although attrition was addressed in the tips section, it should be noted that substantial attrition may still occur even when such tips (such as careful power and sample-size calculations and pilot work) are implemented. Delays in IRB approval, worse-than-expected subject recruitment, seasonal variation in medical visits and hospitalizations, unanticipated expenses, unforeseen departures of research staff, and unexpected reductions in (or complete loss of) grant funding can conspire to jeopardize sufficient participant accrual and study completion. The only safeguards against such pitfalls are building into the study protocol such “safety nets” as added time in the recruitment phase in case of setbacks, diligent efforts to minimize study dropouts and withdrawals, and amending the study protocol to broaden the potential recruitment pool.
Sustaining Successful Interventions
Even highly successful disparities interventions are likely to be discontinued if no mechanism exists for sustainability. Lack of success in procuring renewal of research grants; institutional or philanthropic commitments; or local, state, or federal programmatic funding can spell the end of effective interventions. Sustaining successful disparities interventions, therefore, requires substantial planning, extensive dissemination of study findings, collaborations with policy makers, and innovative approaches to ensure long-term continuation of effective interventions.
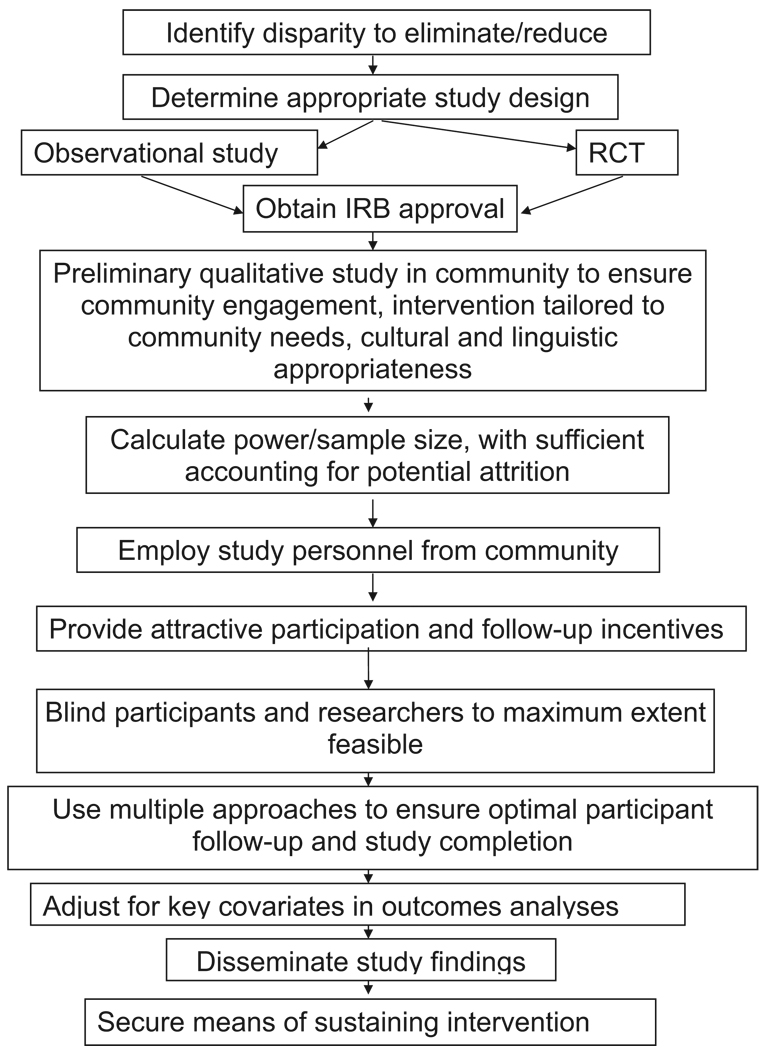
An Approach: Devising, Implementing, and Evaluating Successful Disparities Interventions
Figure 1 summarizes an approach to devising, implementing, and evaluating an intervention to eliminate or reduce racial/ethnic disparities in children’s health and health care. This diagram is an attempt to incorporate the principles described above from comparisons of the 3 successful disparities intervention, as well as the tips and pitfalls.
FIGURE 1.
An approach to devising, implementing, and evaluating an intervention to eliminate or reduce racial/ethnic disparities in children’s health and health care.
RESEARCH AGENDA
It is beyond the scope of this article to provide a comprehensive review of racial/ethnic disparities in children’s health and health care along with a systematic examination of disparities in need of interventions. A suggested research agenda, however, is proposed, comprising one perspective on selected urgent priorities and unanswered questions that need to be addressed through clinical and community-based pediatric disparities interventions (Table 2).
TABLE 2.
A Proposed Research Agenda for Clinical and Community-Based Interventions for Selected Racial/Ethnic Disparities in Children’s Health and Health Care
| Condition-specific disparity targets |
| Health and dental insurance |
| Nonfinancial access barriers to health and dental care |
| Infant mortality |
| Childhood and adolescent mortality |
| Mental health care |
| Organ transplantation |
| Survival rates for Down syndrome and congenital heart defects |
| Pediatric disparity domains with major knowledge gaps in need of intervention studies |
| Does culturally competent and linguistically appropriate care improve minority outcomes and reduce/eliminate disparities? |
| Can quality-improvement approaches reduce/eliminate disparities? |
| Multicenter disparities interventions |
Condition-Specific Disparity Targets
Most racial/ethnic minority groups of children have higher adjusted odds than white children of having no health insurance or being sporadically insured, and Native American children have higher adjusted odds than white children of having no dental insurance.1 Greater adjusted odds of no health or dental insurance and sporadic insurance also occur for children in households in which a language other than English is spoken, compared with those in households with English as the primary language.20 To date, only 1 RCT (in Latinos) has evaluated an intervention to eliminate racial/ethnic disparities in children’s health or dental insurance coverage,13 so more such studies are needed among diverse groups of minority children, including multicenter studies. Multiple racial/ethnic and linguistic disparities among US children also exist in nonfinancial barriers to health and dental care,1,20 but essentially nothing is known about interventions that might be effective in eliminating these disparities.
The infant mortality rate among African Americans and Native Americans is substantially higher than that of whites and has changed little over the most recent 7-year period for which data are available.21 There have been no published studies (to my knowledge), however, on interventions that are effective in reducing or eliminating infant mortality disparities. Substantial racial/ethnic disparities in childhood mortality also exist for all 4major racial/ethnic groups of US children (compared with whites), including significantly higher risks of all-cause mortality,22 drowning deaths,23 injury fatalities,24 and mortality from congenital heart defects.25 Again, there have been no published studies (to my knowledge) on interventions that are effective in reducing or eliminating racial/ethnic disparities in all-cause or condition-specific mortality.
There are several other condition-specific pediatric disparities in urgent need of efficacious interventions. Compared with white children, racial/ethnic minority children experience multiple disparities in mental health care, including significantly higher unmet need for mental health services and significantly lower access to mental health care specialists and antidepressant medications.26–29 Compared with their white peers, African-American children have a significantly lower adjusted likelihood of being activated on the kidney transplant waiting list, and a significantly higher median age at heart transplant (8 vs 5 years old in whites) and likelihood of heart transplant graft failure.30,31 Stark disparities also exist in survival for African-Americans for 2 conditions that first present in childhood: the median age at death for Down syndrome (25 vs 50 years old among whites)32 and the average age at death from congenital heart defects (3 to 6 times lower age than in whites).25
Disparity Domains With Major Knowledge Gaps in Need of Intervention Studies
There is an urgent need for intervention studies in several pediatric racial/ethnic disparity domains with major knowledge gaps. Rigorous intervention studies are still needed to evaluate the impact of culturally competent and linguistically appropriate care on outcomes among racial/ethnic minority children, including whether such interventions can reduce or eliminate disparities.33 It has been cogently argued that several racial/ethnic disparities in children’s health and health care can be framed as quality-of-care issues,34 and several studies have documented such gaps in quality of care for minority children.35 Research is still lacking, however, on interventions that are efficacious in reducing or eliminating such quality disparities. Multicenter intervention studies have the potential to address critical pediatric disparities issues by providing large sample sizes and the statistical power needed to examine clinically significant subgroups, but there have been no published multicenter evaluations (to my knowledge) of interventions aimed at reducing or eliminating pediatric racial/ethnic disparities.
SUMMARY AND CONCLUSIONS
Despite an accumulating body of literature addressing racial/ethnic disparities in children’s health and health care, there have been few published studies of interventions that have been successful in eliminating these disparities. Key characteristics of 3 successful interventions include rigorous study designs, large sample sizes, appropriate comparison groups, community-based interventions that are culturally and linguistically sensitive and involve collaboration with participants, research staff that include personnel from the same community as participants, appropriate blinding of outcomes assessors, and statistical adjustment of outcomes for relevant covariates.
Tips for successfully conducting pediatric disparities elimination interventions include community collaboration in all study phases, preintervention qualitative research, careful sample-size and power calculations that account for attrition, and using multiple approaches to ensure optimal participant follow-up. Pitfalls in conducting pediatric disparities-elimination interventions include IRB approval, attrition, and barriers to sustainability.
A research agenda is proposed for clinical and community-based interventions that address pediatric disparities in health and dental insurance, nonfinancial access barriers to care, infant and childhood mortality, mental health care, organ transplantation, and survival rates for children with Down syndrome and congenital heart defects. Interventions also are needed to address major disparities knowledge gaps regarding the impact of culturally and linguistically appropriate care and quality-improvement approaches on pediatric disparities, and multicenter disparities interventions are still lacking.
Examination of 3 successful interventions indicates that pediatric health care disparities can be eliminated. Achievement of this goal requires an intervention that is rigorous, evidence based, and culturally and linguistically appropriate. The intervention must also include community collaboration, minimize attrition, adjust for potential confounders, and incorporate mechanisms for sustainability.
ACKNOWLEDGMENTS
This work was funded in part by grants to Dr Flores from the Commonwealth Fund and the Improving Chronic Illness Care program of the Robert Wood Johnson Foundation.
ABBREVIATIONS
- RCT
randomized, controlled trial
- aOR
adjusted odds ratio
- CI
confidence interval
- DMA
Division of Medical Assistance
- DPH
Department of Public Health
- IRB
institutional review board
Footnotes
The views presented in this article are those of the author, not the organizations with which he is affiliated.
This work was presented in part at the Starting Early: A Life-Course Perspective on Child Health Disparities—Developing a Research Action Agenda conference; November 7, 2008; Washington, DC.
FINANCIAL DISCLOSURE: The author has indicated he has no financial relationships relevant to this article to disclose.
Reprints Information about ordering reprints can be found online: http://www.pediatrics.org/misc/reprints.shtml
REFERENCES
- 1.Flores G, Tomany-Korman SC. Racial and ethnic disparities in medical and dental health, access to care, and use of services in US children. Pediatrics. 2008;121(2) doi: 10.1542/peds.2007-1243. Available at: www.pediatrics.org/cgi/content/full/121/2/e286. [DOI] [PubMed] [Google Scholar]
- 2.Singh GK, Kogan MD, Dee DL. Nativity/immigrant status, race/ethnicity, and socioeconomic determinants of breastfeeding initiation and duration in the United States, 2003. Pediatrics. 2007;119 suppl 1:S38–S46. doi: 10.1542/peds.2006-2089G. [DOI] [PubMed] [Google Scholar]
- 3.Wright AL, Bauer M, Naylor A, Sutcliffe E, Clark L. Increasing breastfeeding rates to reduce infant illness at the community level. Pediatrics. 1998;101(5):837–844. doi: 10.1542/peds.101.5.837. [DOI] [PubMed] [Google Scholar]
- 4.Wright AL, Clark C, Bauer M. Maternal employment and infant feeding practices among the Navajo. Med Anthropol Q. 1993;7(2):260–281. [Google Scholar]
- 5.Wright AL, Bauer M, Clark C, Morgan F, Begishe K. Cultural interpretations and individual beliefs about breastfeeding among the Navajo. Am Ethnol. 1993;20(4):781–796. [Google Scholar]
- 6.Bauer M, Wright AL. Integrating qualitative and quantitative methods to model infant feeding behavior among Navajo mothers. Hum Organ. 1996;55(2):183–192. [Google Scholar]
- 7.Wright AL, Naylor A, Wester R, Bauer M, Sutcliffe E. Using cultural knowledge in health promotion: breastfeeding among the Navajo. Health Educ Behav. 1997;24(5):625–639. doi: 10.1177/109019819702400509. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Racial/ethnic disparities in diagnoses of HIV/AIDS: 33 states, 2001–2004. MMWR Morb Mortal Wkly Rep. 2006;55(5):121–125. [PubMed] [Google Scholar]
- 9.DiClemente RJ, Wingood GM, Harrington KF, et al. Efficacy of an HIV prevention intervention for African American adolescent girls: a randomized controlled trial. JAMA. 2004;292(2):171–179. doi: 10.1001/jama.292.2.171. [DOI] [PubMed] [Google Scholar]
- 10.Bandura A. Social cognitive theory and exercise of control over HIV infection. In: Di-Clemente RJ, Peterson J, editors. Preventing AIDS: Theories and Methods of Behavioral Interventions. New York, NY: Plenum Publishing Corp; 1994. pp. 25–59. [Google Scholar]
- 11.Wingood GM, DiClemente RJ. The theory of gender and power: a social structural theory for guiding the design and implementation of public health interventions to reduce women’s risk of HIV. In: DiClemente RJ, Crosby RA, Kegler M, editors. Emerging Theories in Health Promotion Practice and Research: Strategies for Enhancing Public Health. San Francisco, CA: Jossey-Bass; 2002. pp. 313–347. [Google Scholar]
- 12.DeNavas-Walt C, Proctor BD, Smith JC. Income, Poverty, and Health Insurance Coverage in the United States: 2007. Washington, DC: US Government Printing Office; 2008. US Census Bureau. Current Population Reports publication P60-235. [Google Scholar]
- 13.Flores G, Abreu M, Chaisson CE, et al. A randomized trial of the effectiveness of community-based case management in insuring uninsured Latino children. Pediatrics. 2005;116(6):1433–1441. doi: 10.1542/peds.2005-0786. [DOI] [PubMed] [Google Scholar]
- 14.Flores G, Abreu M, Brown V, Tomany-Korman SC. How Medicaid and the State Children’s Health Insurance Program can do a better job of insuring uninsured children: the perspectives of parents of uninsured Latino children. Ambul Pediatr. 2005;5(6):332–340. doi: 10.1367/A04-067R2.1. [DOI] [PubMed] [Google Scholar]
- 15.Feinstein AR. Clinical Epidemiology: The Architecture of Clinical Research. Philadelphia, PA: WB Saunders; 1985. [Google Scholar]
- 16.Feinstein AR. Problems of randomized trials. In: Abel U, Koch A, editors. Nonrandomized Comparative Clinical Studies: Proceedings of the International Conference on Nonrandomized Comparative Clinical Studies in Heidelberg; April 10–11, 1997; Düsseldorf, Germany: Symposion Publishing; 1997. [Accessed September 25, 2008]. Available at: www.symposion.com/nrccs/feinstein.htm. [Google Scholar]
- 17.Lawlor DA, Davey Smith G, Kundu D, Bruckdorfer KR, Ebrahim S. Those confounded vitamins: what can we learn from the differences between observational versus randomised trial evidence? Lancet. 2004;363(9422):1724–1727. doi: 10.1016/S0140-6736(04)16260-0. [DOI] [PubMed] [Google Scholar]
- 18.Schulz KF, Grimes DA. Blinding in randomised trials: hiding who got what. Lancet. 2002;359(9307):696–700. doi: 10.1016/S0140-6736(02)07816-9. [DOI] [PubMed] [Google Scholar]
- 19.Flores G, Snowden-Bridon C, Torres S, et al. Improving asthma outcomes in minority children: A randomized, controlled trial of parent mentors. Pediatrics. 2009;124:1522–1532. doi: 10.1542/peds.2009-0230. [DOI] [PubMed] [Google Scholar]
- 20.Flores G, Tomany-Korman S. The language spoken at home and disparities in medical and dental health, access to care, and use of services in US children. Pediatrics. 2008;121(6) doi: 10.1542/peds.2007-2906. Available at: www.pediatrics.org/cgi/content/full/121/6/e1703. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Racial/ethnic disparities in infant mortality: United States, 1995–2002. MMWR Morb Mortal Wkly Rep. 2005;54(22):553–556. [PubMed] [Google Scholar]
- 22.Singh GK, Yu SM. US childhood mortality, 1950 through 1993: trends and socioeconomic differentials. Am J Public Health. 1996;86(4):505–512. doi: 10.2105/ajph.86.4.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saluja G, Brenner RA, Trumble AC, Smith GS, Schroeder T, Cox C. Swimming pool drownings among US residents aged 5–24 years: understanding racial/ethnic disparities. Am J Public Health. 2006;96(4):728–733. doi: 10.2105/AJPH.2004.057067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bernard SJ, Paulozzi LJ, Wallace DL. Centers for Disease Control and Prevention. Fatal injuries among children by race and ethnicity: United States, 1999 –2002. MMWR Surveill Summ. 2007;56(5):1–16. [PubMed] [Google Scholar]
- 25.Boneva RS, Botto LD, Moore CA, Yang Q, Correa A, Erickson JD. Mortality associated with congenital heart defects in the United States: trends and racial disparities, 1979 –1997. Circulation. 2001;103(19):2376–2381. doi: 10.1161/01.cir.103.19.2376. [DOI] [PubMed] [Google Scholar]
- 26.Zimmerman FJ. Social and economic determinants of disparities in professional help-seeking for child mental health problems: evidence from a national sample. Health Serv Res. 2005;40(5 pt 1):1514–1533. doi: 10.1111/j.1475-6773.2005.00411.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kataoka SH, Zhang L, Wells KB. Unmet need for mental health care among U.S. children: variation by ethnicity and insurance status. Am J Psychiatry. 2002;159(9):1548–1555. doi: 10.1176/appi.ajp.159.9.1548. [DOI] [PubMed] [Google Scholar]
- 28.Richardson LP, DiGiuseppe D, Garrison M, Christakis DA. Depression in Medicaid-covered youth: differences by race and ethnicity. Arch Pediatr Adolesc Med. 2003;157(10):984–989. doi: 10.1001/archpedi.157.10.984. [DOI] [PubMed] [Google Scholar]
- 29.Sturm R, Ringel JS, Andreyeva T. Geographic disparities in children’s mental health care. Pediatrics. 2003;112(4) doi: 10.1542/peds.112.4.e308. Available at: www.pediatrics.org/cgi/content/full/112/4/e308. [DOI] [PubMed] [Google Scholar]
- 30.Furth SL, Garg PP, Neu AM, Hwang W, Fivush BA, Powe NR. Racial differences in access to the kidney transplant waiting list for children and adolescents with end-stage renal disease. Pediatrics. 2000;106(4):756–761. doi: 10.1542/peds.106.4.756. [DOI] [PubMed] [Google Scholar]
- 31.Mahle WT, Kanter KR, Vincent RN. Disparities in outcome for black patients after pediatric heart transplantation. J Pediatr. 2005;147(6):739–743. doi: 10.1016/j.jpeds.2005.07.018. [DOI] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention. Racial disparities in median age at death of persons with Down syndrome: United States, 1968 –1997. MMWR Morb Mortal Wkly Rep. 2001;50(22):463–465. [PubMed] [Google Scholar]
- 33.Flores G. Culture, ethnicity and linguistic issues in pediatric care: Urgent priorities, unanswered questions, and a research agenda. Ambul Pediatr. 2004;4(4):276–282. doi: 10.1367/1539-4409(2004)4<276:CEALII>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 34.Beal AC. Policies to reduce racial and ethnic disparities in child health and health care. Health Aff (Milwood) 2004;23(5):171–179. doi: 10.1377/hlthaff.23.5.171. [DOI] [PubMed] [Google Scholar]
- 35.Flores G. Culture and the patient-physician relationship: achieving cultural competency in health care. J Pediatr. 2000;136(1):14–23. doi: 10.1016/s0022-3476(00)90043-x. [DOI] [PubMed] [Google Scholar]