Abstract
Objectives
This analysis compared 3 continuous variables as summary support loss scores with POPQ ordinal stages.
Study Design
We used pooled baseline data from 1141 subjects in 3 randomized trials (CARE, n=322; OPUS, n = 380; ATLAS, n =439) to test 3 support loss measures. The relative responsiveness was assessed using the standardized response mean of 2-year outcome data from the CARE trial.
Results
Each support loss measure was strongly correlated with POPQ ordinal staging; the single most distal POPQ point had the strongest correlation. Improvements in anatomic support were weakly correlated with improvements in POPDI (r = .17-.24, p <.01 for each) but not with changes in POPIQ for all measures of support loss or POPQ stage.
Conclusions
While continuous, single number summary measures compared favorably to ordinal POPQ staging system, the single most distal POPQ point may be preferable to POPQ ordinal stages to summarize or compare group data.
Keywords: Pelvic organ prolapse, prolapse, pelvic surgery, outcome measures, quantification of prolapse
Introduction
A recent U.S. national population-based survey reported that approximately 3% of adult women have symptomatic pelvic organ prolapse (POP) 1. As the population of the United States ages, the number of women with POP will increase with projections from 3.3 million in 2010 to 4.9 million in 2050 2. In 1995, the International Continence Society developed the Pelvic Organ Prolapse Quantification (POPQ) system in order to standardize the anatomic assessment of POP 3. This system, which has been shown to be consistent across examiners, has been adopted worldwide and allowed a common language for clinicians and investigators.
The POPQ, ordinal staging system in which POP is categorized as Stage 0, 1, 2, 3 or 4, quantifies the anatomic descent of the vaginal wall relative to the hymenal ring. The staging system was arbitrarily derived and there is growing sentiment that the POPQ staging system may not optimally differentiate clinically important subgroups. For example, stage 2 prolapse (leading edge within 1 cm proximal or distal to the hymen) is known to include patients who range from asymptomatic to symptomatic, yet the POPQ system does not allow for any differentiation between these groups within stage. Stage 3 is even less anatomically specific as it spans numerous centimeters beyond the points designated as Stage 2. In addition, a patient may change POPQ stage with less than one centimeter of change in vaginal topography. A system which uses a continuous variable to stage prolapse might allow clinicians and investigators to more effectively correlate anatomy with symptoms and to more easily compare results of one type of surgical treatment to another.
The objective of this analysis was to compare several single numerical summary scores that are continuous variables with the established ordinal staging system. Pertinent POPQ points were used to develop equations which give numerical values to specific degrees of prolapse, thereby creating a continuum of degrees of prolapse. Using available prospectively collected data, we assessed the utility of these single continuous measures to describe pelvic organ support loss. Finally, we correlated these support loss measures with symptoms and condition specific quality of life scores, and assessed the utility of these measures in evaluating anatomical outcomes after surgery.
Materials and Methods
We analyzed pooled baseline data from 1141 subjects in 3 randomized trials, CARE, OPUS, and ATLAS, conducted by the Pelvic Floor Disorders Network, (PFDN), an NIH sponsored multi-center network. These clinical trials used standardized tools including the POPQ, the Pelvic Floor Distress Inventory (PFDI) and the Pelvic Floor Impact Questionnaire (PFIQ) 4. The CARE study enrolled women planning sacrocolpopexy for stage 2-4 prolapse without symptoms of stress incontinence and completed follow-up in 2005 5, 6; the OPUS study enrolled stress continent women with anterior vaginal prolapse undergoing vaginal surgery and is ongoing 7; and the ATLAS study enrolled women with stress incontinence and stage 0-2 vaginal support and completed follow-up in 2008 8. Each clinical site and the data coordinating center received institutional review board approval for these studies, and all subjects provided written informed consent.
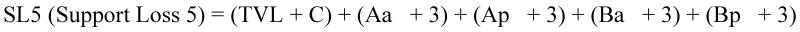
The POPQ measurements Aa, Ba, Ap, Bp and C have positive values when the prolapse extends beyond the hymen and negative when the particular points remain proximal to the hymen. We created three composite measures of support loss (SL) as summary measures, SL3 (includes TVL, C, Ba and Bp), SL5 (includes TVL, C, Aa, Ba, Ap and Bp), and SLmax (includes location of single most distal point) (Figure 1).
Figure One. Equations for Three Summary Scores for Support Loss.
SL3 = (TVL + C) + (Ba + 3) + (Bp + 3); and SLmax = location of single most distal point.
Zero is the theoretical lower limit of SL5 and SL3 and -3 is the limit for SLmax, and represent perfect support. Higher values of SL measures represent greater support loss.
When there is perfect support, POPQ points Aa, Ba, Ap and Bp equal minus 3; thus, the support loss formulas add 3 to each of these values so that, in a situation of perfect support, the resulting measurement of support loss would equal zero. In regard to C (cervix or vaginal cuff), we added this value to total vaginal length (TVL); in a situation of perfect support, the negative C would be similar to TVL and result in a value near zero. We note that in women with a cervix in situ, perfect support may mean that negative C is not the same as TVL since the cervix is anterior and distal to the TVL measurement in the cul-de-sac. Figure 1 contains the equations for the three definitions tested in this analysis.
Each support loss measure was correlated with several measures of pelvic symptoms and severity, as well as condition-specific life impact: the Pelvic Organ Prolapse Quantification (POPQ) system stage 3, 9, total scores for responses to the Pelvic Organ Prolapse Distress Inventory (POPDI) and the Pelvic Organ Prolapse Impact Questionnaire (POPIQ), and responses to questions 4 (“usually have a sensation of bulging or protrusion”) and 5 (“usually have a bulge or something falling out seen/felt”) of the Pelvic Floor Distress Inventory (PFDI) 4. Pearson correlation coefficients and associated p-values are reported. The relationships between POPQ stage with the support loss measures, POPIQ and POPDI were assessed using one-way ANOVA.
In order to assess the utility of these support loss measures to describe long-term anatomical outcomes, only two-year CARE data 10 were used (as the ATLAS and OPUS studies only assessed one year outcomes). The change in each support loss measure, as well as POPQ stage from baseline to 24 months, was calculated. The relative responsiveness of each measure was evaluated using the standardized response mean (SRM). SRM, a commonly used statistic of responsiveness, is defined as the mean change in score over a time period divided by the standard deviation of individuals' changes in scores11. A higher SRM (in absolute value) is indicates better responsiveness. A value of 0.5 is a cutoff for moderate responsiveness, 0.8 good responsiveness, and 1.0 excellent responsiveness 11. Pearson correlation coefficients were calculated for the change from baseline to 24 months in support measures and POPQ stage with corresponding changes in POPDI and POPIQ.
All reported p-values were based on the two-sided statistical tests and intended to be interpreted from a hypothesis-generating framework. The analyses were performed in SAS 9.1.3 for Windows (SAS Inc., Cary, NC).
Results
One thousand one hundred and forty-one subjects who enrolled in one of the three trials considered in this analysis and completed at least baseline POPQ data collection are the subject of this report (CARE trial, n=322; OPUS trial, n = 380; ATLAS trial, n =439). Subject characteristics for this pooled group, as well as for each individual study, are shown in Table 1. Consistent with the inclusion criteria for the studies evaluated, those enrolled in the CARE and OPUS trials had stage 2-4 prolapse while those enrolled in the ATLAS trial had stage 0 - 2 vaginal support. Overall, the distribution of POPQ stage for the pooled group was 4.3% stage 0, 17.9% stage 1, 29.4% stage 2, 40.5% stage 3 and 7.9% stage 4. 66% of subjects complained of vaginal bulging as indicated by an affirmative response to PFDI question number 4 or 5 and 48% of subjects indicated that they were bothered by these symptoms moderately or quite a bit.
Table 1. Baseline Patient Characteristics by Study and for Combined Population.
| CARE Trial | OPUS Trial | ATLAS Trial | Total | ||
|---|---|---|---|---|---|
| N | 322 | 380 | 439 | 1141 | |
| Age, Years | Mean (SD) | 60.9 (10.2) | 63.7 (10.0) | 49.8 (11.9) | 57.6 (12.5) |
| BMI, kg/m2 | Mean (SD) | 27.1 (4.5) | 28.1 (5.5) | 29.5 (6.8) | 28.4 (5.9) |
| Cesarean Deliveries | Median | 0 | 0 | 0 | 0 |
| Min - Max | 0 - 5 | 0 - 4 | 0 - 4 | 0 – 5 | |
| Vaginal Deliveries | Median | 3 | 3 | 2 | 2 |
| Min - Max | 0 - 11 | 0 - 12 | 0 - 11 | 0 – 12 | |
| Race | |||||
| White | 299/322 (92.9) | 331/380 (87.1) | 374/339 (85.2) | 1004/1141 (88.0) | |
| Black | 17/322 (5.3) | 24/380 (6.3) | 44/439 (10.0) | 85/1141 (7.4) | |
| Other | 6/322 (1.8) | 25/380 (6.6) | 21/439 (4.8) | 52/1141 (4.6) | |
| Ethnicity | |||||
| Hispanic | 9/322 (2.8) | 52/380 (13.7) | 32/439 (7.3) | 93/1048 (8.2) | |
| Prior Hysterectomy | 228/271 (84.1) | 143/378 (37.8) | 108/437 (24.7) | 479/1086 (44.1) | |
| Prior UI Surgery | 22/322 (6.8) | 12/379 (3.2) | 27/438 (6.2) | 61/1139 (5.4) | |
| Prior POP Surgery | 126/322 (39.1) | 53/379 (14.0) | 15/439 (3.4) | 194/1140 (17.0) | |
| Prolapse Stage | |||||
| 0 | 0 (0) | 0 (0) | 49/439 (11.2) | 49/1141 (4.3) | |
| 1 | 0 (0) | 0 (0) | 204/439 (46.5) | 204/1141 (17.9) | |
| 2 | 44/322 (13.7) | 106/380 (27.9) | 186/439 (42.4) | 336/1141 (29.4) | |
| 3 | 218/322 (67.7) | 244/380 (64.2) | 0 (0) | 462/1141 (40.5) | |
| 4 | 60/322 (18.6) | 30/380 (7.9) | 0 (0) | 90/1141 (7.9) | |
| PFDI question 4 – “Do you usually have a sensation of bulging or protrusion from the vaginal area?” | |||||
| No | 28/315 (8.9) | 43/346 (12.4) | 346/424 (81.6) | 417/1085 (38.4) | |
| Yes, how much does it bother you? Not at all |
10/315 (3.2) | 11/364 (3.2) | 6/424 (1.4) | 27/1085 (2.5) | |
| Somewhat | 56/315 (17.8) | 67/346 (19.4) | 51/424 (12.0) | 174/1085 (16.0) | |
| Moderate | 45/315 (14.3) | 66/346 (19.1) | 12/424 (2.8) | 123/1085 (11.3) | |
| Quite a bit | 176/315 (55.9) | 159/346 (46.0) | 9/424 (2.1) | 344/1085 (31.7) | |
| PFDI question 5 – “Do you usually have a bulge that can bee seen or felt in the vaginal area?” | |||||
| No | 23/315 (7.3) | 36/346 (10.4) | 388/428 (90.6) | 447/1089 (41.0) | |
| Yes, how much does it bother you? Not at all |
8/315 (2.5) | 13/346 (3.8) | 7/428 (1.6) | 28/1089 (2.6) | |
| Somewhat | 48/315 (15.2) | 63/346 (18.2) | 19/428 (4.4) | 130/1089 (11.9) | |
| Moderate | 53/315 (16.8) | 58/346 (16.8) | 7/428 (1.6) | 118/1089 (10.8) | |
| Quite a bit | 183/315 (58.1) | 176/346 (50.9) | 7/428 (1.6) | 366/1089 (33.6) | |
| POPDI* | Mean (SD) | 107.4 (67.3) | 59.8 (62.6) | 49.9 (48.2) | 69.8 (63.8) |
| Min - Max | 0 - 283.3 | 0 - 300 | 0 - 214.3 | 0 – 300 | |
| POPIQ* | Mean (SD) | 60.5 (77.3) | 50.9 (61.6) | 17.5 (42.7) | 40.5 (63.3) |
| Min - Max | 0 - 371.5 | 0 - 277.6 | 0 - 278.8 | 0 – 371.5 | |
| SL5# | Mean (SD) | 27.36 (11.28) | 23.4 (10.0) | 6.71 (4.00) | 18.10 (12.60) |
| Min - Max | 7 – 60 | 7 -- 58 | 0 – 21.5 | 0 – 60 | |
| SL3# | Mean (SD) | 20.56 (9.69) | 17.09 (8.30) | 4.54 (2.61) | 13.24 (10.06) |
| Min - Max | 4 – 48 | 4 to 46 | 0 – 14 | 0, 48 | |
| SLMAX # | Mean (SD) | 3.92 (2.45) | 2.88 (2.17) | -1.46 (1.00) | 1.50 (3.05) |
| Min - Max | -1 to 12 | -1 to 10 | -3 to 1 | -3 to 12 | |
Data Presented as n/N (%) unless otherwise noted.
BMI, body mass index
POPDI, Pelvic Organ Prolapse Distress Inventory (range 0-300); POPIQ, Pelvic Organ Prolapse Impact Questionnaire (range 0-400); higher scores indicate greater symptoms distress/life impact.
SL5 (Support Loss5) = (TVL + C) + (Aa + 3) + (Ap + 3) + (Ba + 3) + (Bp + 3); SL3 = (TVL + C) + (Ba + 3) + (Bp + 3); SLmax = location of single most distal point. Zero is the theoretical lower limit of SL5 and SL3 and -3 is the limit for SLmax, and represent perfect support. Higher values of SL measures represent greater support loss.
For the pooled group, the mean±SD Support Loss 5 (SL5) was 18.1±12.6 (range 0 to 60), the SL3 was 13.2±10.1 (range: 0 to 48), and the SLmax was 1.5± 3.0 (range: -3 to 12) at their baseline evaluation. The relationship between each support loss measure and POPQ stage is shown in Table 2. Each support loss measure demonstrated a strong correlation with the POPQ ordinal staging with the strongest correlation seen with SLmax (SLmax, r=.93, SL5, r = .87; SL3, r=0.85, p<.001 for each). Each support loss measure demonstrated statistically significant but weak correlations with POPDI and POPIQ scores similar to that of POPQ stage (Table 3). Moderate correlations were noted between each support loss measure and the presence and degree of bother caused by vaginal bulging symptoms (PFDI questions 4 and 5) (r = 0.51-0.69, p <.01 for each) which was also similar to that of POPQ stage (r = .62 and .69, p<.001).
Table 2. Support Loss Outcomes by POPQ Stage.
| POPQ Stage | N | SL5 | SL3 | SLMAX |
|---|---|---|---|---|
| 0 | 49 | 1.47 ±0.97 (0 to 4) |
1.47±0.97 (0 to 4) |
-3.00±** (-3 to -3) |
| 1 | 204 | 4.78 ±1.88 (1 to 12.5) |
3.40±1.52 (1 to 9.5) |
-1.99 ± 0.25 (-3 to -1.5) |
| 2 | 336 | 12.27 ± 4.15 (4 to 24) |
8.21±3.20 (2 to 19) |
-0.05 ± 0.78 (-1 to 1) |
| 3 | 462 | 25.24 ± 7.75 (10.5 to 50.5) |
18.62±6.79 (5.5 to 41.5) |
3.52 ± 1.43 (1.5 to 8) |
| 4 | 90 | 42.52 ±9.68 (16 to 60) |
33.13±8.35 (9 to 48) |
7.31 ±1.68 (3 to 12) |
| P value R2 |
<.001 0.73 |
<.001 0.87 |
||
| R | 0.85 | 0.93 | ||
SL5, SL3, SLMax data presented as mean ± standard deviation (range)
standard deviation undefined
Table 3. Correlation between Baseline Support Loss Outcomes and Pelvic Organ Prolapse Distress Inventory and Impact Questionnaire.
| N=1,141 | POPDI | POPIQ | PFDI Question 4 |
PFDI Question 5 |
|---|---|---|---|---|
| SL5 | 0.25* | 0.24* | 0.57* | 0.64* |
| SL3 | 0.24* | 0.24* | 0.55* | 0.62* |
| SLmax | 0.26* | 0.25* | 0.62* | 0.69* |
| POPQ Stage | 0.24* | 0.24* | 0.62* | 0.69* |
p<0.01
The change in anatomic support in the CARE population two years after abdominal sacrocolpopexy is displayed in Table 4 using the three continuous support loss measures and POPQ stage. Each measure demonstrated excellent responsiveness with SRMs ranging from 1.89 to 2.25 with SLmax demonstrating the greatest responsiveness. However, improvements in anatomic support correlated only weakly with improvements in POPDI (r = 0.17-0.24, p <.01 for each) and did not correlate with changes in POPIQ for all measures of support loss or with POPQ stage (Table 4).
Table 4. Change in Support Loss Measures 2 years after surgery in the CARE Trial.
| Baseline N=322 | 24 Month N=250 | Change from Baseline N=250 | SRM | Correlation of change from baseline and change in POPDI (r) | Correlation with change from baseline and change in POPIQ (r) | |
|---|---|---|---|---|---|---|
| SL5 | ||||||
| Mean (SD) | 27.4 (11.3) | 4.4 (3.3) | -22.7 (10.8)* | 2.10 | 0.24* | 0.10 |
| Range | 7 to 60 | 0 to 15 | -53 to 0 | |||
| SL3 | ||||||
| Mean (SD) | 20.6 (9.7) | 2.6 (2.0) | -17.6 (9.3) | 1.89 | 0.20* | 0.09 |
| Range | 4 to 48 | 0 to 11 | -42 to 0 | |||
| SLmax | ||||||
| Mean (SD) | 3.9 (2.4) | -1.5 (1.2) | -5.4 (2.4)* | 2.25 | 0.22* | 0.08 |
| Range | -1 to 12 | -3 to 3 | -13 to 0 | |||
| POPQ Stage | ||||||
| Mean (SD) | 3.0 (0.6) | 1.3 (0.8) | -1.8 (0.9)* | 2.00 | 0.17* | 0.01 |
| Range | 2 to 4 | 0 to 3 | -4 to 0 | |||
p<0.01
POPDI, Pelvic Organ Prolapse Distress Inventory; POPIQ, Pelvic Organ Prolapse Impact Questionnaire
SRM, standardized response mean; values greater than 1 indicate excellent responsiveness.
Discussion
In this study, we explored other ways, besides POPQ stage, of describing the POPQ examination results with a single summary score. When it was introduced in 1996, the POPQ system represented a significant advance for pelvic floor disorders research by providing clinicians and investigators with a quantitative and reliable tool to measure outcomes 3. Each point in the POPQ system describes a specific part of vaginal support and at this time we recommend no changes in how these data are collected. However, in clinical research a summary score is helpful to compare treatments or groups of patients. Currently, POPQ stage is most frequently used to summarize the six POPQ points. This ordinal 0 through 4 staging system included in the original POPQ report was arbitrarily derived and the numerical measure intervals between the stages are ordinal. Since 1996, evidence has accumulated that Stage 2 prolapse (+/- 1 cm from the hymen) includes both symptomatic and asymptomatic women and normal and abnormal women12-16. In addition, Stage 3 prolapse encompasses a wide range, from prolapse >1 cm below the hymen to nearly complete vaginal prolapse. Finally, the arbitrary and non-linear nature of the ordinal staging system does not allow easy statistical comparisons between groups.
We found that a single numerical variable that is continuously expressed compares similarly to the ordinal POPQ staging system in measuring prolapse symptoms and bother, and prolapse related quality of life. The three different summary scores correlated well with prolapse symptoms, bother, and prolapse quality of life, and all were responsive to change. The SLmax score (also known as maximum vaginal descent) is the easiest to understand and does not require any calculations, and we therefore recommend it for most prolapse outcome studies in which characterization with a continuous score is desired. In our sample of over 1,000 women, the distribution of this measure was slightly right skewed. A desirable feature of a single summary measure would be the ability to be able to report with means and standard deviations with parametric statistical analysis so that results are easily imaged by the reader, improving transparency of surgical outcome reporting. Unlike the relative POP-Q-Index proposed by Lemos et al, in which a POP-Q index (the actual position score of one POP-Q point minus its anatomic (optimal) position score) is divided by the maximum possible POP-Q-Index for that point to create a continuous value expressed as a proportion, the SLmax score provides a summary of the entire vaginal support system, but requires no math or conversion factors17.
Our data and other studies indicate the SLmax score is clinically relevant, as it correlates well with a woman's perception of seeing or feeling a bulge (questions 4 and 5 on the PFDI) 12-16. The weak correlation between the POPIQ and POPDI (∼0.25) and the various summary scores reflects the fact that degree of prolapse correlates poorly with quality of life, which is more likely to be impaired due to pelvic floor symptoms that may or may not be related to the prolapse itself.
Given its ability to provide an easily understood measure of maximum vaginal descent and its high responsiveness, SLmax may serve as a good primary outcome in studies evaluating prolapse treatment. We do not, however, recommend that SLmax be the sole anatomic descriptor of prolapse. If the aim of a surgical procedure is to restore support to a specific compartment, it is logical to provide descriptive statistics for the pre- and post-operative status of that compartment. We recommend including SLmax, rather than or in addition to POPQ stage, and also providing results for all anatomic outcomes relevant to the procedure or treatment performed (generally measures of anterior, posterior and apical support).
Our study is strengthened by including a diverse group of 1141 women with a full range of prolapse stages. However, our data on responsiveness of the summary scores is limited to the CARE data, because the OPUS anatomic outcomes after surgery have not been completed and the ATLAS patients were not treated for prolapse.
In conclusion, we report some new continuous measures that closely correlate with POPQ stage and symptoms, and have statistical advantages and improved transparency. Our data suggest that reporting SLmax, the single most distal point in the ordinal POPQ system, may be preferable to reporting the POPQ ordinal stages when a single summary statistic is desired.
Acknowledgments
Grant Support: Supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institute of Diabetes, Digestive and Kidney Diseases and the NIH Office of Research on Women's Health (U01 HD41249, U10 HD41250, U10 HD41261, U10 HD41267, U10 HD54136, U10 HD54214, U10 HD54215, and U10 HD54241).
Footnotes
Accepted for presentation at the Society of Gynecologic Surgeons, April 12-14, 2010, Tuscon, Arizona, USA
Reprints will not be available.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008 Sep 17;300(11):1311–6. doi: 10.1001/jama.300.11.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu JM, Hundley AF, Fulton RG, Myers ER. Forecasting the prevalence of pelvic floor disorders in U.S. women: 2010 to 2050. Obstetrics & Gynecology. 2009 Dec;114(6):1278–83. doi: 10.1097/AOG.0b013e3181c2ce96. [DOI] [PubMed] [Google Scholar]
- 3.Bump R, Mattiasson A, Bo K, Klarskov P, Smith ARB, Brubaker L, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obest & Gynec. 1996;175:10–7. doi: 10.1016/s0002-9378(96)70243-0. [DOI] [PubMed] [Google Scholar]
- 4.Barber MD, Kuchibhatla MN, Pieper CF, Bump RC. Psychometric evaluation of 2 comprehensive condition-specific quality of life instruments for women with pelvic floor disorders. Am J Obest & Gynec. 2001;185:1388–95. doi: 10.1067/mob.2001.118659. [DOI] [PubMed] [Google Scholar]
- 5.Brubaker L, Cundiff GW, Fine P, Nygaard I, Richter HE, Visco AG, et al. Abdominal sacrocolpopexy with burch colposuspension to reduce urinary stress incontinence. N Engl J Med. 2006 Apr 13;354(15):1557–66. doi: 10.1056/NEJMoa054208. see comment. [DOI] [PubMed] [Google Scholar]
- 6.Brubaker L, Pelvic Floor Disorders Network . Anonymous Colpopexy and urinary reduction efforts (CARE), a randomized trial of abdominal sacrocolpopexy with/without burch colposuspension. International urogynecological association, prague august, and society of gynecologic surgeons; anaheim, CA: march, 2003. [Google Scholar]
- 7.Wei J, Nygaard I, Richter H, Brown M, Barber M, Xiao X, et al. Outcomes following vaginal prolapse repair and mid urethral sling (OPUS) trial--design and methods. Clinical Trials. 2009 Apr;6(2):162–71. doi: 10.1177/1740774509102605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Richter HE, Burgio KL, Goode PS, Borello-France D, Bradley CS, Brubaker L, et al. Non-surgical management of stress urinary incontinence: Ambulatory treatments for leakage associated with stress incontinence (ATLAS) trial. Clinical Trials. 2007;4:92–101. doi: 10.1177/1740774506075237. [DOI] [PubMed] [Google Scholar]
- 9.Weber AM, Abrams P, Brubaker L, Cundiff G, Davis G, Dmochowski RR, et al. The standardization of terminology for researchers in female pelvic floor disorders. International Urogynecology Journal. 2001;12(3):178–86. doi: 10.1007/PL00004033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brubaker L, Nygaard I, Richter HE, Visco A, Weber AM, Cundiff GW, et al. Two-year outcomes after sacrocolpopexy with and without burch to prevent stress urinary incontinence. Obstet Gynecol. 2008 Jul;112(1):49–55. doi: 10.1097/AOG.0b013e3181778d2a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Crosby RD, Kolotkin RL, Williams GR. Defining clinically meaningful change in health-related quality of life. J Clin Epidemiol. 2003 May;56(5):395–407. doi: 10.1016/s0895-4356(03)00044-1. [DOI] [PubMed] [Google Scholar]
- 12.Swift SE, Tate SB, Nicholas J. Correlation of symptoms with degree of pelvic organ support in a general population of women: What is pelvic organ prolapse? American Journal of Obstetrics & Gynecology. 2003 Aug;189(2):372–7. doi: 10.1067/s0002-9378(03)00698-7. discussion 377-9. [DOI] [PubMed] [Google Scholar]
- 13.Bradley CS, Nygaard IE. Vaginal wall descensus and pelvic floor symptoms in older women. Obstetrics & Gynecology. 2005 Oct;106(4):759–66. doi: 10.1097/01.AOG.0000180183.03897.72. [DOI] [PubMed] [Google Scholar]
- 14.Ellerkmann RM, Cundiff GW, Melick CF, Nihira MA, Leffler K, Bent AE. Correlation of symptoms with location and severity of pelvic organ prolapse. Am J Obest & Gynec. 2001;185:1332–8. doi: 10.1067/mob.2001.119078. [DOI] [PubMed] [Google Scholar]
- 15.Tan JS, Lukacz ES, Menefee SA, Powell CR, Nager CW, San Diego Pelvic Floor C Predictive value of prolapse symptoms: A large database study. International Urogynecology Journal. 2005 May-Jun;16(3):203–9. doi: 10.1007/s00192-004-1243-8. discussion 209. [DOI] [PubMed] [Google Scholar]
- 16.Barber MD. Symptoms and outcome measures of pelvic organ prolapse. Clinical Obstetrics & Gynecology. 2005 Sep;48(3):648–61. doi: 10.1097/01.grf.0000170424.11993.73. [DOI] [PubMed] [Google Scholar]
- 17.de Barros Moreira Lemos NL, Flores Auge AP, Lunardelli JL, Brites Frade A, Frade CL, de Oliveira AL, et al. Optimizing pelvic organ prolapse research. International Urogynecology Journal. 2007 Jun;18(6):609–11. doi: 10.1007/s00192-006-0204-9. [DOI] [PubMed] [Google Scholar]