Abstract
Almost half a century after the first reports describing the limited replicative potential of primary cells in culture, there is now overwhelming evidence for the existence of “cellular senescence” in vivo. It is being recognized as a critical feature of mammalian cells to suppress tumorigenesis, acting alongside cell death programs. Here, we review the various features of cellular senescence and discuss their contribution to tumor suppression. Additionally, we highlight the power and limitations of the biomarkers currently used to identify senescent cells in vitro and in vivo.
Keywords: Telomeres, oncogenes, tumor suppressor genes, senescence, in vivo, biomarkers
Replicative cellular senescence
One of the first observations made for primary cells explanted from human tissue was that such cells do not proliferate indefinitely but instead are “mortal.” In fact, their proliferative capacity upon explantation consistently displays three phases: phase I, corresponding to a period of little proliferation before the first passage, during which the culture establishes; phase II, characterized by rapid cell proliferation; and phase III, during which proliferation gradually grinds to a complete halt (Hayflick and Moorhead 1961). Commenting on the possible causes of the transition to phase III, Hayflick (1965) hypothesized that “The finite lifetime of diploid cell strains in vitro may be an expression of aging or senescence at the cellular level.” The term cellular senescence therefore denotes a stable and long-term loss of proliferative capacity, despite continued viability and metabolic activity.
Consistent with Hayflick's proposal, we now know that, with the propagation of human cells in culture, telomeres (the protective chromosomal termini) are progressively shortened, ultimately causing cells to reach their “Hayflick limit.” This barrier has been termed replicative (cellular) senescence, since it is brought about by replication. Telomeres are subject to attrition due to the fact that DNA polymerase fails to completely replicate the lagging strands. In the early 1970s, Olovnikov (1971) and Watson (1972) independently described this so-called “end replication problem”, which contributes to telomere shortening. Thus, telomeres act as a molecular clock, reflecting the replicative history of a primary cell (Harley et al. 1990).
When telomeres reach a critical minimal length, their protective structure is disrupted. This triggers a DNA damage response (DDR), which is associated with the appearance of foci that stain positive for γ-H2AX (a phosphorylated form of the histone variant H2AX) and the DDR proteins 53BP1, NBS1, and MDC1. Moreover, the DNA damage kinases ATM and ATR are activated in senescent cells (D'Adda di Fagagna et al. 2003). After amplification of the DDR signal, these kinases activate CHK1 and CHK2 kinases. Communication between DDR-associated factors and the cell cycle machinery is brought about by phosphorylation and activation of several cell cycle proteins, including CDC25 (a family of phosphatases) and p53. In addition, differential expression of p53 isoforms has been linked to replicative senescence (Fujita et al. 2009). Together, these changes can induce a transient proliferation arrest, allowing cells to repair their damage. However, if the DNA damage exceeds a certain threshold, cells are destined to undergo either apoptosis or senescence. The factors bringing about this differential outcome have remained largely elusive, but the cell type and the intensity and duration of the signal, as well as the nature of the damage, are likely to be important determinants (D'Adda di Fagagna 2008).
In addition to p53, replicative senescence is linked to the RB tumor suppressor and its signaling partners, including p16INK4A (a cyclin-dependent kinase inhibitor acting upstream of RB). Indeed, activation of both the p53 and p16INK4A–RB pathways is essential for induction of senescence in a variety of human cell strains. The first evidence for this came from experiments employing the viral oncoprotein SV40 large T antigen (LT) and mutants thereof lacking the ability to inhibit p53 or RB. While expression of wild-type LT allowed cellular immortalization to occur, expression of either of the mutants failed to do so (Shay et al. 1991). A variety of experiments subsequently confirmed the critical roles of the p53 and p16INK4A–RB pathways (Ben-Porath and Weinberg 2005; Campisi 2005). The relative contribution of these cascades to senescence depends on the cell strain: While some are significantly delayed in their onset of senescence upon inactivation of p16INK4A alone, others require a deficiency in p53 or in p53 as well as p16INK4A for the abrogation of senescence. However, such escape from replicative senescence results in only limited further proliferation: Ultimately, cells will undergo telomeric crisis, resulting in chromosomal instability and death (Shay and Wright 2005).
The dependence of replicative senescence on telomere shortening is evident from its bypass by the ectopic expression of the catalytic subunit of the telomerase holoenzyme (hTERT), which elongates telomeres, thereby abrogating the effect of the end replication problem (Bodnar et al. 1998; Vaziri and Benchimol 1998). The limited life span of most primary human cells is explained by the fact that, in contrast to stem cells, telomerase is not expressed in human somatic cells, so they are unable to maintain telomeres at a sufficient length to suppress a DDR (Harley et al. 1990; Wright et al. 1996; Masutomi et al. 2003). Therefore, the ectopic expression of hTERT is a common practice in vitro, allowing for the immortalization of primary human cells. Likewise, tumor cells often express telomerase (Shay and Bacchetti 1997), or elongate their telomeres through a mechanism termed alternative lengthening of telomeres (ALT) (Muntoni and Reddel 2005). As a result, telomeres of human cancer cells are maintained at a length that permits continued proliferation (Shay and Wright 2006).
Premature cellular senescence
Senescence can be induced also in the absence of any detectable telomere loss or dysfunction, by a variety of conditions. This type of senescence has been termed premature, since it arises prior to the stage at which it is induced by telomere shortening. In recent years, evidence for the existence of premature senescence in vivo has been accumulating rapidly and points to a critical role in tumor suppression. We now turn to the various conditions that can induce such premature cellular senescence.
Stress-induced senescence in vitro
In vitro, premature senescence can result from inadequate culturing conditions. When cells are explanted from an organism and placed in culture, they have to adapt to an artificial environment, characterized by abnormal concentrations of nutrients and growth factors and the presence of ambient O2 levels, as well as the absence of surrounding cell types and extracellular matrix components. One or more of these conditions can induce a culture shock, resulting in stress-induced senescence (Sherr and DePinho 2000). This type of cell cycle arrest is independent of telomere length. It also occurs in mouse cells, which, in contrast to most human cells, express telomerase (Prowse and Greider 1995) and have long telomeres (Kipling and Cooke 1990). Mouse embryonic fibroblasts (MEFs) undergo senescence after a limited number of passages in culture, despite their retaining of long telomeres. Elongation of their life span can be achieved by culturing in serum-free medium supplemented with a number of defined growth factors (Loo et al. 1987) or by culturing under physiological oxygen conditions (Parrinello et al. 2003). Consistent with this, oxidative stress induces cessation of replication in cultured human cells (Packer and Fuehr 1977; Chen et al. 1995; Yuan et al. 1995), while the replicative potential of human melanocytes and epithelial cells depends largely on the composition of the culture medium used, as well as on the use of feeder layers (Ramirez et al. 2001; Bennett and Medrano 2002; Bennett 2003). Senescence of MEFs can be bypassed also by inactivation of p53 or simultaneous ablation of RB family genes (Tanaka et al. 1994; Dannenberg et al. 2000; Sage et al. 2000). Thus, the immortalization of mammalian cells requires not only telomere maintenance, but also optimal culture conditions (Mathon et al. 2001; Ramirez et al. 2001; Tang et al. 2001; Herbert et al. 2002; for review, see Wright and Shay 2002).
Oncogene-induced senescence (OIS) in vitro
Early studies on mutant HRAS (HRASV12) led to the discovery that, although it can transform most immortal mammalian cell lines and collaborate with immortalizing genes in oncogenically transforming primary cells, it induces cell cycle arrest when it is introduced alone into primary cells (and at least one immortal rat fibroblast cell line) (Land et al. 1983; Franza et al. 1986; Serrano et al. 1997). Serrano et al. (1997) noted the striking phenotypic resemblance of such nonproliferating cells to those in replicative senescence, and this phenomenon has eventually come to be known as OIS. Unlike replicative senescence, OIS cannot be bypassed by expression of hTERT, confirming its independence from telomere attrition (Wei and Sedivy 1999).
One of the hallmarks shared by cells undergoing replicative senescence and OIS is the critical involvement of the p53 and p16INK4A–RB pathways, at least in certain settings. In murine cells, functional inactivation of p53 or its direct upstream regulator, p19ARF, is sufficient to bypass RASV12-induced senescence (Kamijo et al. 1997; Serrano et al. 1997). In human cells, p16INK4A seems to play a more prominent role than p53, as some cells depend solely on p16INK4A for OIS (Ben-Porath and Weinberg 2005). Whereas p19ARF is an exquisite sensor that is activated by oncogenic signals and mediates senescence in cultured murine cells, in human cells it does not seem to play a similarly dominant role (Wei et al. 2001; Michaloglou et al. 2005). Nonetheless, specific mutations affecting human ARF (i.e., p14ARF) but not p16INK4A have been identified in some human melanoma (Freedberg et al. 2008). Indeed, OIS mechanisms do not seem to be universal across cell types and genetic contexts. This is also exemplified by the signaling routes relaying OIS by RASV12 versus BRAFE600: Whereas RASV12-induced senescence can be bypassed by abrogation of the p16INK4A–RB pathway (Serrano et al. 1997), BRAFE600-triggered senescence cannot be bypassed by functional inactivation of p16INK4A, be it alone (Michaloglou et al. 2005) or in combination with silencing of p14ARF (Haferkamp et al. 2009).
Recent evidence suggests the relevance of OIS also in the context of induced pluripotency in vitro. At least two oncoproteins, c-MYC and KLF4, are required for the generation of induced pluripotent stem (iPS) cells. As the INK4A/ARF proteins and p53 limit the efficiency of iPS cell formation, it has been suggested that cellular senescence counteracts the induced conversion of primary cells into pluripotent stem cells (Banito et al. 2009; Hong et al. 2009; Kawamura et al. 2009; Li et al. 2009; Marión et al. 2009; Utikal et al. 2009). Alternatively, increased proliferation rates associated with p53 loss may result in accelerated kinetics of iPS formation (Hanna et al. 2009). To the extent that this can be extrapolated to an in vivo setting, one could imagine that cancer stem cells arise from a similar reprogramming process (Krizhanovsky and Lowe 2009). Thus, cellular senescence might suppress tumor formation not only by inducing a persistent cell cycle arrest, but also by limiting the generation of cancer stem cells.
Tumor suppressor loss-induced senescence in vitro
Similar to oncogene mutation or overexpression, loss of a tumor suppressor can also trigger senescence in mouse and human cells. This was first illustrated for PTEN and NF1. As elaborated further below, for PTEN it was shown that fully deficient MEFs undergo senescence, which is accompanied by induction of p53. Concomitant loss of p53 allows cells to override the cytostatic effects of Pten deletions (Chen et al. 2005). Similarly, depletion of NF1 causes senescence in vitro, which is eventually accompanied by decreases in ERK and AKT activities (Courtois-Cox et al. 2006). An elegant model was proposed in which the increase in RAS activity following NF1 loss is dampened by a negative feedback loop. Of note, although loss of NF1 triggers senescence in human diploid fibroblasts (HDFs), it immortalizes MEFs. Another example within this theme is VHL, loss of which triggers senescence in an RB- and p400-dependent manner (Young et al. 2008).
Biomarkers and mechanisms of cellular senescence
While cellular senescence is induced by a wide variety of conditions, senescent cells display a number of characteristics that allow their identification both in vitro and in vivo. Some of these biomarkers reflect the activation of mechanisms (such as the induction of tumor suppressor networks) that contribute to the senescence program. For others that accompany the execution of the senescence program (like the increase in senescence-associated β-galactosidase [SA-β-GAL] activity), it is as yet unclear to what extent they contribute mechanistically.
Cell cycle arrest
Long-term exit from the cell cycle is the central and, in our view, only indispensable marker for the identification of all types of cellular senescence both in vitro and in vivo. However, it is important to realize that, although senescent cells by definition withdraw from the cell cycle, their inability to replicate is far from unique. Terminal differentiation, for example, similarly results in stable replicative arrest. An essential difference is the fact that differentiation is typically triggered by physiological cues and does not commonly involve the activation of tumor suppressor networks. Thus, although cell cycle exit constitutes an indispensable biomarker for senescence, it can by no means be used in isolation to identify senescent cells.
Is cellular senescence strictly irreversible? Early in vitro studies—for example, on p16INK4A and RAF1—suggested that it essentially is (Kato et al. 1998; Zhu et al. 1998), but subsequent studies have argued that, in fact, escape scenarios exist. In spite of the observation that stable RB-dependent heterochromatin structures and several other factors contribute to lock cells in their senescent state (see below), there are multiple ways to reverse the arrest, allowing cells to re-enter the cell cycle. For example, inactivation of the p53 pathway permits senescence reversal, while inactivation of some interleukins also abrogates the arrest (Beauséjour et al. 2003; Dirac and Bernards 2003; Coppé et al. 2008; Kuilman et al. 2008; see below). In some settings, the reversibility depends on the expression of p16INK4A prior to entering senescence (Beauséjour et al. 2003). As discussed in more detail below, there is also the possibility that, in addition to the levels of certain tumor suppressor proteins, the strength of the oncogenic signal contributes to the reversibility of senescence.
It should be noted here that strong selection exists for the small subset of cells that are endowed with the ability to exit the senescent state. While this may be a rare event in cultured cells, it is highly relevant in in vivo settings, where clonal expansion of such reverted cells likely represents a rate-limiting event on the path toward tumor progression. Indeed, activation of senescence-abrogating pathways can be seen in melanomas clonally emerging from melanocytic nevi, which carry the same driver mutation (LCW Vredeveld and DS Peeper, unpubl.). Notably, wound healing can create a microenvironment that induces regrowth in nevi (Schoenfeld and Pinkus 1958; Park et al. 1987). It will be of interest to identify the signaling pathways that apparently relax the cytostatic constraints. A variation on this theme is preventing senescence, rather than reversing it. One could imagine that this can be achieved by either a failure to engage senescence pathways or a lack of fundamental senescence mediators. An example for the first scenario would be the inability of mutant KRAS to induce a senescence response in the small intestine of mice that display evidence of senescence in the colon. In the same study, the rapid development of colon adenocarcinomas in the absence of INK4a/Arf is an example of the second scenario (Bennecke et al. 2010; see below).
Morphological transformation
Cell senescence is generally accompanied by morphological changes, which may be quite striking. Depending on the senescence trigger, cells can become large, flat, and multinucleated, or rather refractile. A flat cell phenotype is commonly seen in cells undergoing H-RASV12-induced senescence (Serrano et al. 1997; Denoyelle et al. 2006), stress-induced senescence (Parrinello et al. 2003), or DNA damage-induced senescence (Chen and Ames 1994; Chen et al. 2001). Cells senescing due to BRAFE600 expression or the silencing of p400, however, acquire a more spindle-shaped morphology (Chan et al. 2005; Michaloglou et al. 2005). Melanocytes undergoing RASV12-induced senescence display extensive vacuolization as a result of endoplasmic reticulum stress caused by the unfolded protein response (Denoyelle et al. 2006).
Activation of tumor suppressor networks
As mentioned above, the p53 and p16INK4A–RB signal transduction cascades commonly mediate the activation of the senescence program (Lowe et al. 2004). Consequently, components thereof have been used as biomarkers to identify senescent cells. In human fibroblasts undergoing replicative or premature senescence, RB accumulates in its active, hypophosphorylated form (Stein et al. 1990; Serrano et al. 1997; Lin et al. 1998), and p53 displays increased activity and/or levels (Atadja et al. 1995; Vaziri et al. 1997; Bunz et al. 1998; Wei et al. 2001). The p53 protein can also be phosphorylated on Ser 15 by ATM as part of the senescence response (Calabrese et al. 2009). p53 serves as a node, mediating prosenescence signals emerging from unscheduled oncogene activation, telomere dysfunction, DNA damage, and reactive oxygen species (ROS).
Among the pocket proteins, RB has a unique role in mediating senescence in human cells (Chicas et al. 2010). One of its primary activators, p16INK4A, is commonly induced in senescent cells in many contexts in vitro (Serrano et al. 1997; Campisi 2005). Other proteins in the p16INK4A–RB and p53 pathways, notably p21CIP1 and p15INK4B, also often accumulate in senescent cells, and have been used as markers reflecting the activation of these pathways in senescence (Alcorta et al. 1996; Hara et al. 1996; Reznikoff et al. 1996; Serrano et al. 1997; Erickson et al. 1998; Lin et al. 1998; Robles and Adami 1998; Zhu et al. 1998; Hitomi et al. 2007). Induction of p16INK4A is commonly seen in senescent mouse and human lesions in vivo also (te Poele et al. 2002; Collado et al. 2005; Michaloglou et al. 2005; Gray-Schopfer et al. 2006; Dhomen et al. 2009; Goel et al. 2009), while p53 and p21CIP1 induction can be evident, too; for example, in senescent mouse prostate tumors (Chen et al. 2005). Disruption of the p16INK4A–RB pathway collaborates with ectopic hTERT expression in the immortalization of both primary human epithelial cells (Kiyono et al. 1998) and melanocytes (Gray-Schopfer et al. 2006). At least in some in vitro settings, this can be bypassed by altering the cell culture conditions (Ramirez et al. 2001), consistent with the view discussed above that inadequate circumstances can launch the senescence program (Sherr and DePinho 2000).
Genetic disruption of the gene encoding p16INK4A predisposes mice and humans to tumorigenesis, including melanoma (Gruis et al. 1995; Krimpenfort et al. 2001; Sharpless et al. 2001). This notwithstanding, at least in melanomagenesis, genetic and immunohistochemical evidence in mice and humans suggests that p16INK4A plays a redundant role in senescence (Gruis et al. 1995; Michaloglou et al. 2005; Dhomen et al. 2009). This may be different in other settings, like human colon adenoma, in which a strict correlation is observed between p16INK4A expression and cell cycle arrest (Dai et al. 2000; Kuilman et al. 2008). In murine cells, its neighbor, p19ARF, appears to take on this dominant role as a common senescence marker. Concordantly, Arf acts as a potent tumor suppressor gene in mice (Kamijo et al. 1997) and is induced in response to oncogenic signals in vivo (Zindy et al. 2003).
Induction of SA-β-GAL activity
SA-β-GAL is a commonly used senescence biomarker (Dimri et al. 1995; Debacq-Chainiaux et al. 2009). Its increased activity in senescent cells derives from lysosomal β-D-galactosidase, which is encoded by the GLB1 gene. Its detection requires tissues to be snap-frozen to preserve enzymatic activity (Debacq-Chainiaux et al. 2009). Also, nonsenescent cells display β-galactosidase activity in the lysosomes that functions most optimally at pH 4 (Lee et al. 2006). Accordingly, the increase in SA-β-GAL activity in senescent cells is likely due to an expansion of the lysosomal compartment, giving rise to an increase in β-galactosidase activity that can be measured also at suboptimal pH 6 (hence, SA-β-GAL) (Kurz et al. 2000; Yang and Hu 2005; Lee et al. 2006). There is, however, as yet no evidence pointing to an actual involvement of this enzyme in the senescence response (Lee et al. 2006).
Senescence-associated heterochromatic foci (SAHF)
Cellular senescence can be associated with an altered chromatin structure, at least in vitro. While DNA dyes display overall homogenous staining patterns in cycling or quiescent human cells, senescent cells often show strikingly different punctate staining patterns. These DNA SAHF (Narita et al. 2003) are specifically enriched in methylated Lys 9 of histone H3 (a modification catalyzed by the histone methyltransferase Suv39h1), while histone H3-Lys 9 acetylation and Lys 4 methylation (both euchromatin markers) are excluded from SAHF. Whereas polycomb group proteins have been shown to repress the INK4A/ARF locus (Jacobs et al. 1999; Gil et al. 2004; Bracken et al. 2007), the histone H3-Lys 27 demethylase JMJD3 contributes to its transcriptional activation (Agger et al. 2009; Barradas et al. 2009), thus regulating senescence. Senescent cells display increased binding of heterochromatin-associated proteins in the promoters of several E2F target genes. SAHF formation is circumvented by interference with p16INK4A–RB pathway signaling, correlating with bypass of senescence. Depending on the experimental system, interference with expression of other genes—including those encoding p53, C/EBPβ, or interleukin-6 (IL-6) (see below)—also reduces SAHF-positivity, which is associated with abrogation of senescence (Chan et al. 2005; Ye et al. 2007; Zhang et al. 2007; Kuilman et al. 2008).
An essential step in the initiation phase of chromosome condensation appears to be the translocation of HIRA (a histone chaperone) to PML (promyelocytic leukemia nuclear) bodies (Zhang et al. 2005; Adams 2007, 2009). These subnuclear organelles are thought to serve as a staging ground for the formation of HIRA/ASF1A-containing complexes, which are subsequently incorporated into chromatin and play an essential role in instigating SAHF formation. RNAi depletion of either ASF1A or HMGA1 (a SAHF component) leads to a partial bypass of senescence (Zhang et al. 2005; Narita et al. 2006).
Secreted factors in senescence
Cells undergoing senescence—whether in response to telomere malfunction, DNA damage, or oncogenic alterations—exhibit profound changes in their transcriptomes. A major consequence of this is the secretion of many dozens of factors, including cytokines and chemokines (Campisi 2005). The first indication of changes in the secretome of human cells accompanying senescence was reported for fibroblasts undergoing replicative senescence. Microarray analysis revealed a strong inflammatory response, as seen in wound healing (Shelton et al. 1999). Subsequent work from various laboratories has revealed that cells undergoing either replicative or premature senescence display profound changes in their secretome, termed the senescence-associated secretory phenotype (SASP) (Coppé et al. 2008; Rodier et al. 2009). A recent study indicates that, for the induction of several of these SASP factors, persistent DNA damage is required. Because DNA damage accompanies some but not all senescence settings (see below), the SASP is not strictly coupled to senescence per se (Rodier et al. 2009).
Proinflammatory cytokines—when secreted by senescent cells—trigger a variety of cellular responses. In certain settings, pro-oncogenic effects result: The proliferative rate, migration, and invasion of premalignant cells are enhanced when they are cocultured with, or grown in medium conditioned by, senescent fibroblasts (Krtolica et al. 2001; Dilley et al. 2003; Parrinello et al. 2005; Yang et al. 2006). For example, a study on ovarian tumorigenesis has revealed that preneoplastic epithelial ovarian cells expressing oncogenic RAS induce expression of GRO1 (a cytokine recognized by CXCR2) (Yang et al. 2006). Once secreted, GRO1 has the potential to induce senescence in ovarian fibroblasts in vitro. In turn, these fibroblasts promote tumor growth when coinjected with preneoplastic epithelial cells into mice. Interestingly, fibroblasts surrounding human ovarian tumors express several senescence markers, suggesting that this two-way communication exists in vivo as well. Similar findings have been reported for several additional weakly oncogenic epithelial cell lines that show increased tumorigenic potential upon exposure to senescent fibroblasts (Krtolica et al. 2001).
Intriguingly, in addition to influencing their microenvironment, some inflammatory cytokines have an indispensable role in the establishment and maintenance of the senescence arrest. For example, signaling through the IL-6 and IL-8 (CXCR2) receptors is essential, in a cell-autonomous fashion, for cells to enter senescence in response to oncogenic BRAF or replicative exhaustion, respectively (Acosta et al. 2008; Kuilman et al. 2008). This is relayed by the C/EBPβ and NF-κB transcription factors and is associated with the activation of an inflammatory transcriptome. Correspondingly, elevated levels of cytokines are found in senescent human neoplasms. Likewise, the ECM regulator PAI-1 has been shown to mediate senescence (Kortlever et al. 2006), although clinical data seem to point to a more complex picture (Kuilman and Peeper 2009).
It thus appears that, while senescent cells can promote cancer by stimulating the proliferation of incipient tumor cells that reside in their microenvironment, senescence also acts as a cell-autonomous tumor suppression mechanism limiting the expansion of early malignant cells. Therefore, the name “senescence-messaging secretome” (SMS) has been proposed in order to emphasize that, next to their requirement for the senescence response (whether or not involving a DDR), many of these factors are also endowed with communicative functions (Kuilman and Peeper 2009). The SMS creates a complex signaling network in which secreted factors affect not only the cells producing them (autocrine effects), but also the microenvironment and hence neighboring cells (paracrine effects). In some cases, SMS factors can stimulate the innate immune system, triggering tumor clearance (Xue et al. 2007; see below). The ultimate effect on target cells may depend largely on their genetic constitution. A classic example is the pro- or anti-proliferative effect of TGFβ on tumor cells as a function of the stage of tumorigenesis (Massagué 2008). Also, the effect of IL-6 on melanomagenesis depends on tumor progression (Lu et al. 1992, 1996). Although in these examples it is as yet unclear to what extent this differential response is linked to the ability of cells to undergo senescence, it is conceivable that the effect of SMS factors on their target cells is influenced by the oncogenic lesions that are carried by the latter.
ROS
As already alluded to, the replicative potential of primary cells is influenced by the oxygen levels in which they are cultured. In fact, lowering the oxygen tension can prevent OIS in HDF (Lee et al. 1999) and tissue culture stress-induced senescence in MEFs (Parrinello et al. 2003). It is widely assumed that not oxygen itself, but rather ROS produced by mitochondria are involved in senescence (Lu and Finkel 2008; Moiseeva et al. 2009). While ROS levels increase in both replicative senescence and OIS (Furumoto et al. 1998; Lee et al. 1999), treatment of HDF with a sublethal concentration of H2O2 induces senescence (Chen and Ames 1994; Chen et al. 1998). ROS contribute also to induction of replicative senescence, as evidenced by its delayed or premature onset upon treatment with antioxidants or inhibitors of cellular oxidant scavengers, respectively (Chen et al. 1995; Yuan et al. 1995). A recent systems biology study has suggested that ROS mediates senescence through induction of DNA damage foci, with a contribution of p21CIP1 (Passos et al. 2010).
How do ROS relate to p53 and RB? A study on the maintenance of a senescence-like arrest upon temporary expression of SV40 LT revealed that ROS and PKCδ function in a positive feedback loop to maintain this proliferative halt (Takahashi et al. 2006). Furthermore, ROS have been suggested to impinge either directly or indirectly on the p53 and p16INK4A–RB signal transduction cascades (Itahana et al. 2003; Iwasa et al. 2003). For instance, the MINK–p38–PRAK pathway is activated in senescence and controls the activation of p16INK4A and p53, as well as expression of p21CIP1, in a p53-independent manner (Wang et al. 2002; Bulavin et al. 2003; Iwasa et al. 2003; Nicke et al. 2005; Sun et al. 2007). These results not withstanding, although ROS undoubtedly plays an important role in senescence, the nature and mechanism of this contribution remains largely unclear (Lu and Finkel 2008). Major questions include how the increased levels of ROS are generated, and what the cellular targets for ROS in senescence are.
DNA damage-induced senescence
The involvement of DNA damage in the induction of replicative senescence by telomere attrition has been established (D'Adda di Fagagna 2008). Also DNA-damaging agents such as ionizing radiation can induce cell cycle arrest with characteristics of senescence in HDFs (Di Leonardo et al. 1994; Robles and Adami 1998). Furthermore, DNA damage-inducing drugs can cause senescence of tumor cells in vitro and in vivo, a phenomenon termed drug-induced senescence, which may be exploited for the treatment of cancer (Wang et al. 1998; Chang et al. 1999; Berns 2002; Schmitt et al. 2002; te Poele et al. 2002; Roninson 2003).
Activation of a DDR has also been shown to contribute to OIS in several settings in vitro; among others, in the context of oncogene-induced DNA hyperreplication (D'Adda di Fagagna 2008). The DDR and p53 often function in a common signal transduction cascade in which interference with specific DDR components can substitute for the loss of p53 function (Bartkova et al. 2006; Di Micco et al. 2006; Moiseeva et al. 2006; Mallette et al. 2007; Kim et al. 2009; Santoriello et al. 2009). For example, a shRNA targeting ATM can serve as a proxy for HPV E6 (which inactivates p53), contributing to bypass of senescence by STAT5 (Mallette et al. 2007).
However, DDR activation is not a universal feature of OIS. For example, in mice, in the context of several types of senescent adenomas, no DDR is observed, nor is there a requirement for ATM in (oncogene-induced) senescence (Efeyan et al. 2009). Furthermore, senescence triggered by RAF1 or BRAFE600 and, in some cases, RASV12 does not require p53 (Olsen et al. 2002; Nicke et al. 2005; Kuilman et al. 2008) and fails to mount an appreciable DDR (C Lenain and DS Peeper, unpubl.). In line with this, senescence induced upon genetic loss of Skp2 in the context of Pten heterozygosity is not associated with the emergence of DDR markers and does not depend on p53 signaling (Lin et al. 2010). Shedding some light on a possible link between the DDR and senescence, an elegant study showed that, in the context of Rb loss-driven murine adenomas, the DDR preceded cellular senescence (Shamma et al. 2009; see also below). While early and late adenomas similarly expressed DDR markers, senescence was apparent only in late (arrested) lesions, suggesting that, at least in this experimental system, it is primarily senescence and not DNA damage signaling that acts cytostatically (Peeper 2009). It thus seems that DDR activation is involved in certain, but not all, OIS settings.
Autophagy
Increasing evidence points to a link between cellular senescence and autophagy. This catabolic process is mediated by the formation of double-membraned vesicles (autophagosomes) engulfing cytoplasmic content that fuse with lysosomes. Ultimately, this leads to the breakdown of the vesicles and their constituents (Levine and Kroemer 2008). Early studies have demonstrated that chaperone-mediated autophagy is decreased in senescent human cells (Cuervo and Dice 2000). Treatment of human umbilical vein endothelial cells (HUVECs) with glycated collagen I (GC) results in an increase of SA-β-GAL activity (Patschan et al. 2008). This seems to be correlated with a transient induction of the formation of autophagosomes, as evidenced by the up-regulation of the LC3-II protein. The fusion of autophagosomes with lysosomes, as measured by colocalization of LC3 and LAMP1 (a lysosomal marker), correlates with expression of LC3-II. Thus, both autophagosome formation and its fusion with lysosomes are eventually decreased compared with nonsenescent cells. Inhibition of autophagosome formation by treatment with the pharmacological inhibitor 3-methyladenine decreases the number of SA-β-GAL-positive cells upon treatment with GC (Patschan et al. 2008). This might indicate a decrease in the amount of senescent cells, although one cannot exclude that it reflects a drop in the number of lysosomes due to a decreased demand for lysosome–autophagosome fusion. However, senescence and autophagy have recently been connected more tightly. It was shown that autophagic activity increases in OIS, as monitored by the activation of LC3-II, through a delayed activation of the mTORC1 pathway. Furthermore, autophagy contributes to cell cycle arrest and production of senescence-associated interleukins (Young et al. 2009).
Identifying senescent cells
As described above, the execution of senescence programs is associated with the appearance of several markers, which are commonly used in order to identify senescent cells in vitro and in vivo. They include the loss of proliferation, morphological changes, increased SA-β-GAL activity, the production of SAHF, and a rise in the levels of DDR markers as well as the cell cycle inhibitors p16INK4A, p15INK4B, p21CIP1, and p53. DEC1, DCR2 (Collado et al. 2005), and PAI1 (Goldstein et al. 1994) have also been used as senescence biomarkers (Collado and Serrano 2010). Furthermore, a number of inflammation-linked factors have been associated with senescence. However, it should be noted that different senescent lesions may be characterized by different biomarkers.
It should be emphasized that, in isolation, none of these markers can indisputably identify senescent cells, whether in vitro or in vivo. Indeed, several of the markers used in vitro await in vivo confirmation. For example, due to the lack of appropriate antibodies, it has remained unclear whether the senescence-associated cell cycle protein p15INK4B can be used to specifically identify senescent human cells in vivo. Moreover, although recently identified markers encoded by the inflammatory transcriptome—particularly IL-6, IL-8, and CXCR2 (Acosta et al. 2008; Coppé et al. 2008; Kuilman et al. 2008)—have been demonstrated to identify senescent cells in some early murine and human tumors, it remains to be determined to what extent they can be used across different tissues and genetic contexts.
In spite of its popularity, SA-β-GAL should not be regarded as a unique identifier for senescent cells. In addition to senescent cells, contact-inhibited or serum-starved cells in tissue culture, as well as proliferating dysplastic epithelium in the gastrointestinal tract, can be positive for SA-β-GAL (Severino et al. 2000; Going et al. 2002; Yang and Hu 2005). Furthermore, one would expect that increases in the number or activity of lysosomes unrelated to senescence would also result in elevated lysosomal β-galactosidase protein levels, and thus in increased SA-β-GAL activity. Thus, employing SA-β-GAL in the absence of additional senescence markers may inappropriately classify cells as being senescent. For these reasons, SA-β-GAL can serve as senescence marker only in conjunction with additional markers.
A major challenge to the field, therefore, is to increase the number as well as the reliability of markers to identify senescent cells, especially in vivo. Ideally, one needs to uncover biomarkers that are causally involved in this unique type of proliferative arrest. For the time being, in the absence of unambiguous single markers, we would recommend that, for the identification of senescent cells, one uses, in addition to a proliferation marker such as the Ki-67 antigen (by immunostaining) or the thymidine analog bromodeoxyuridine (BrdU) (by in vivo labeling), at least two additional senescence markers, the choice of which may vary for different settings. For example, p16INK4A often correlates with senescence both in vitro and in vivo, and as such it is a common (but not universal) senescence marker. Also, tissue sections for immunostaining should be analyzed with multiple senescence markers. Ideally, this is done on consecutive sections or, even better, on single sections by double staining, if feasible. Only careful and multiparameter analyses will allow the appropriate detection of presumed senescent lesions.
Cellular senescence as a pathophysiological phenomenon
Ever since the discovery of cellular senescence in vitro, researchers have wondered whether there are in vivo correlates of this program. Hayflick (1965) described possible implications of cellular senescence for carcinogenesis and aging: “Thus the phenomenon of the alteration of a cell strain to a cell line is important because, in its simplest terms, it can be regarded as oncogenesis in vitro.” Indeed, the conversion from a mortal to an immortal cell reflects a rate-limiting step in tumorigenesis. The identification of OIS in cultured cells opened a debate on the possible role of this type of proliferation arrest in vivo. Many were quick to realize that, in principle, OIS could serve as a powerful line of defense against tumorigenesis. It would allow an incipient neoplastic cell harboring an oncogenic lesion to withdraw itself from the proliferative pool, so that tumor formation is prevented. This is consistent with the fact that p16INK4A and p53, two factors often associated with senescence, are among the most commonly mutated proteins in cancer (The Cancer Genome Atlas Gene Ranker GBM 6000, http://cbio.mskcc.org/tcga-generanker/index.jsp).
Early in vitro experiments on senescence commonly used supraphysiological expression levels of RASV12. Subsequently, several groups reported that RASV12 and mutant RAF proteins act mitogenically or, conversely, drive cells into senescence as a function of increasing expression levels (Woods et al. 1997; Guerra et al. 2003; Deng et al. 2004; Tuveson et al. 2004; Sarkisian et al. 2007; Chen et al. 2009). Some of these observations, and the fact that commonly used culturing conditions differ markedly from those in intact tissue and presumably act as a further stressor, initially caused some skepticism about a physiological role for senescence. In the last 5 years, however, a plethora of mouse models as well as human lesions have provided convincing and independent arguments in favor of OIS serving as a bona fide and effective tumor suppressor mechanism.
Although some in vitro senescence models may have been artificial, they did not at all rule out a possible role for senescence in vivo. For instance, increased expression of activated RAS genes is a common feature of human tumors (Elenbaas et al. 2001; Johnson et al. 2005; Okamura et al. 2006; Chen et al. 2009) that can be associated with the conversion from benign to malignant tumors (Quintanilla et al. 1986; Finney and Bishop 1993; Rodriguez-Puebla et al. 1999). Amplification of HRASV12 is common in human Spitz nevi, which rarely progress to malignancy (Maldonado et al. 2004), probably representing the best available evidence of high levels of a mutant RAS gene in a growth-arrested benign neoplastic lesion.
As already alluded to above, the propensity to launch a senescence program in response to an oncogenic alteration differs among tissue and cell types. In murine pulmonary tumors, for example, p19ARF is induced to relatively low levels upon expression of KRASG12D, while it is highly elevated in sarcomas (Young and Jacks 2010). Along these lines, KRAS-driven senescence is observed in several mouse tissues, including lung adenomas, pancreatic intraductal neoplasia, and colonic epithelium, but not small intestinal epithelial cells (Collado et al. 2005; Bennecke et al. 2010). Similarly, reactivation of p53 in established murine tumors causes senescence in sarcomas but apoptosis in lymphomas (Ventura et al. 2007; see below). Thus, while senescence can be considered as a pathophysiological phenomenon, several physiological factors influence its onset.
Replicative senescence in vivo
A number of studies have suggested that senescent cells accumulate in aging individuals. An increase in SA-β-GAL activity can be detected in the skin of elderly people (Dimri et al. 1995). In addition, a small but significant decrease in telomere length has been detected in aged tissue, although this is limited to certain cell types (Cristofalo et al. 2004). These studies, which relied on single senescence markers, were later supported by the finding that several DNA damage and heterochromatinization markers—including 53BP1, γ-H2AX, phospho-Ser 1981-ATM, HP-1β, and HIRA—are increased in dermal fibroblasts from aging baboons compared with young ones. DNA damage markers were shown to colocalize with telomeres, and this correlated with increased p16INK4A expression (Herbig et al. 2006), suggesting that dysfunctional telomeres can create DNA damage signals leading to the onset of senescence also in vivo. In line with the idea that replicative senescence results from telomeric attrition upon prolonged proliferation, senescence is detected mainly in tissues experiencing substantial cellular turnover (Jeyapalan et al. 2007).
Telomere dysfunction has been suggested to be connected to age-related pathology, and this warrants further study. For example, atherosclerosis is accompanied by an induction of SA-β-GAL activity (Minamino et al. 2002) and telomere shortening (Foreman and Tang 2003). Senescent cells have also been observed in osteoarthritis (Price et al. 2002). Since these studies used single senescence markers, they await confirmation. This notwithstanding, the observations are in agreement with the proposed deleterious effects of senescent cells on their microenvironment, possibly contributing to age-related disease (Campisi 2005).
Conversely, beneficial aspects of replicative senescence have also been uncovered, including some that are unrelated to cancer. In a mouse model of liver fibrosis, senescent cells were detected, as evidenced by positivity for SA-β-GAL, p16INK4A, p53, p21CIP1, and HMGA1. These senescent cells derive from activated hepatocellular stem cells and limit the progression of fibrosis (Krizhanovsky et al. 2008). In addition, two reports (Cosme-Blanco et al. 2007; Feldser and Greider 2007) have provided evidence for the proposal by Hayflick (1965) that replicative senescence limits tumorigenesis. Both studies report that mice lacking the RNA component of telomerase (mTR) display decreased tumor formation in the context of either one or two copies of mutant p53R172P replacing endogenous p53 (Cosme-Blanco et al. 2007) or Eμ-MYC/BCL2-driven lymphomagenesis (Feldser and Greider 2007). The lack of telomerase activity had been shown previously to result in an induction of apoptosis, but, in these two models, this response was abrogated owing to expression of the p53 mutant or BCL2, respectively. These studies show that cells display extensive induction of senescence in intestine, kidney, and spleen (Cosme-Blanco et al. 2007), or in microlymphomas (Feldser and Greider 2007). This has provided the first direct evidence of replicative senescence preventing tumorigenesis, at least in the context of an apoptosis block.
Consequently, a colorful picture is emerging for the role of telomeres in senescence and cancer biology. Telomere shortening or dysfunction initially triggers a robust stress response that, through the induction of cell cycle inhibitory proteins, limits the replicative potential of cells. As such, this aspect of telomere biology is likely to act as a potent anti-cancer mechanism. This is consistent with a significant drop in the tumor take of telomerase-deficient (mTR−/−) mice in the context of INK4a/Arf loss (Greenberg et al. 1999). In the absence of p53, however, telomere dysfunction instead promotes tumorigenesis (Chin et al. 1999). This could occur through the inability of cells to engage a full DDR, and through the perturbation of the apoptosis and senescence responses (Artandi and DePinho 2010).
OIS in vivo
The past 5 years have witnessed a boost in the number of studies demonstrating senescence in vivo in both murine and human lesions. Senescence markers have been demonstrated in several contexts in which oncogenes or tumor suppressor genes were perturbed (Fig. 1). Four studies that were published in concert provided the first evidence for OIS in vivo. Schmitt and colleagues (Braig et al. 2005) reported on the tumor-suppressive role of the chromatin remodeling enzyme Suv39h1 in Eμ-NRAS-driven lymphomagenesis, which correlates with bypass of OIS in vitro in Suv39h1−/− splenocytes. Serrano and coworkers (Collado et al. 2005) showed that conditional expression of KRASV12 from its endogenous locus in mice results in the emergence of lung adenomas, as well as premalignant pancreatic intraductal neoplasia, most of which fail to progress to malignancy. The adenomatous stage is specifically characterized by a low proliferative index and the appearance of several senescence markers, including SA-β-GAL, p15INK4B, p16INK4A, and several new markers. Peeper and coworkers (Michaloglou et al. 2005) showed that congenital human melanocytic nevi, which frequently harbor activating BRAF or NRAS mutations, display several characteristics of senescence (see below). The first demonstration of tumor suppressor (PTEN) loss-induced senescence in vivo (Chen et al. 2005) is discussed below.
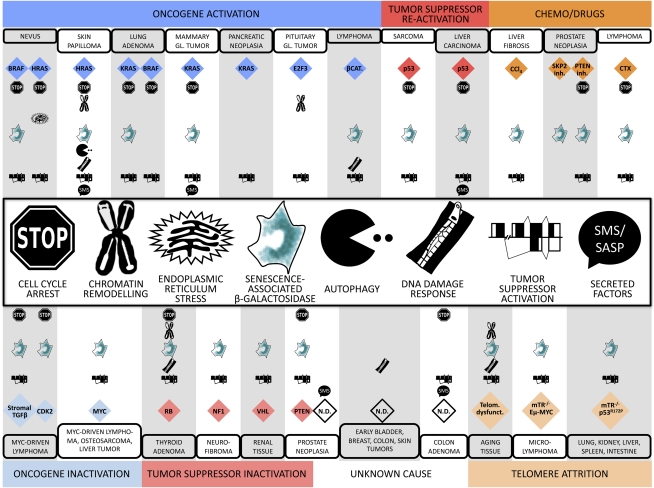
Figure 1.
The essence of senescence: biomarkers in vivo. Several markers of cellular senescence have been identified in early neoplastic lesions in both mice and humans. Representative examples are shown in the various columns, with the type of genetic lesions or other types of stress (stress categories, color-coded) that instigate senescence at the very top and very bottom, and from thereon inward: the tissue types, specific stress signals, biomarkers, and symbols legends, respectively. For instance, in BRAF mutant nevi, the stress category is oncogene activation (blue), the tissue type is nevus, the specific stress signal is BRAF, and the biomarkers reported are cell cycle arrest, increase in SA-β-GAL activity, and tumor suppressor activation. (CTX) Cyclophosphamide; (βCAT) β-catenin; (GL) gland; (N.D.) not determined.
As a sequel to this first series of observations, several other groups have further supported the view that OIS inhibits tumor formation. For example, both established and newly identified chemokine and cytokine markers suggest the presence of senescent cells in human colon adenoma and prostatic intraepithelial neoplasia (PIN) lesions (Acosta et al. 2008; Kuilman et al. 2008). In addition, murine papillomas driven by HRASV12 expression or induced upon DMBA/TPA treatment express several senescence markers (Collado et al. 2005; Acosta et al. 2008; Chen et al. 2009; Yamakoshi et al. 2009). Recent evidence indicates that Myc, known mainly for its proapoptotic function, drives a subset of murine lymphomas into senescence through stromal secretion of TGFβ (Reimann et al. 2010), providing support for the premise that senescence is not solely implemented in a cell-autonomous manner. In line with the idea that OIS represents a barrier for cancer development, a senescence index of tumor cells has been associated with better treatment outcome in high-grade colorectal cancer (Haugstetter et al. 2010). Moreover, expression of several senescence-associated genes is reduced when tumors progress beyond the senescent stage (Chen et al. 2005; Collado et al. 2005; Lazzerini Denchi et al. 2005; Acosta et al. 2008). However, particularly for cell cycle-regulating genes like p16INK4A, abundant expression may, in fact, be maintained during malignancy, which is explained by the occurrence of other (epi)genetic aberrations (including events occurring in parallel and downstream) that neutralize their functions. As such cases are expected to coincide with immunopositivity for proliferation markers, this reinstates the need for careful, multiparameter analysis of senescence in vivo.
OIS in models of nevus and melanoma formation
Melanocytic nevi, benign tumors that have a low propensity to progress toward melanoma, are a well-studied system for OIS in vivo in humans, mice, and fish. In 2002, BRAFE600 was identified as a frequent mutation in human cancer, predominantly melanoma (Davies et al. 2002). At least as remarkable was the finding that the same mutation is present in the large majority of nevi (Pollock et al. 2003). In spite of the presence of an oncogenic BRAF (or, in some cases, NRAS) allele, an important and common feature of nevi is their exceedingly low proliferative activity. This characteristic is typically maintained for decades until the lesion gradually disappears. Nevi express elevated levels of p16INK4A and display increased SA-β-GAL activity (Michaloglou et al. 2005). Arguing against a role for replicative senescence, it was found that telomere length in nevi is indistinguishable from that in normal skin (and longer than in melanoma cells). This strongly suggests that nevi undergo OIS in vivo. These findings have been confirmed by Bennett and coworkers (Gray-Schopfer et al. 2006). Secreted IGFBP7 has been reported to play a central role in the initiation and maintenance of the senescent state of nevus cells (Wajapeyee et al. 2008), but these findings were challenged recently (Schrama et al. 2010; Scurr et al. 2010; Wajapeyee et al. 2010).
The studies on senescent nevi are consistent with earlier observations that a mutant BRAF transgene in the melanocytic compartment induces the formation of nevus-like lesions in zebrafish (Patton et al. 2005). Although senescence markers were not assessed in this study, Patton et al. (2005) describe that, in combination with loss of p53, the fish develop invasive melanomas. In a similar transgenic mouse model, expression of BRAFE600 in the melanocytic lineage drives the formation of nevi with several signs of senescence (Goel et al. 2009). These animals develop melanoma with a long latency, depending on the expression of the transgene. Melanoma formation was strongly accelerated in Cdkn2a or p53-deficient backgrounds.
Recently, two advanced mouse models have been created that more closely resemble spontaneous mutation of the oncogene by conditionally expressing BRAFE600 from its endogenous promoter (Dankort et al. 2009; Dhomen et al. 2009). In these models, specific expression of mutant BRAF in the melanocytic compartment results in the formation of nevus-like benign lesions, which, depending on the model used, remain stable for several months to more than a year. Importantly, these melanocytic cell groups express several senescence markers, corroborating earlier observations on RASV12 that physiological expression levels of an activated oncogene can also give rise to senescence in neoplasms. In line with the idea that p16INK4A is not always strictly required for OIS in vivo (Michaloglou et al. 2008), nevus formation was unimpaired in a p16INK4A-deficient background, although increased melanoma penetrance and reduced latency were observed (Dhomen et al. 2009). In contrast, in combination with a mutant Braf knock-in allele, loss of Pten produced aggressive tumors much resembling human metastatic melanoma (Dankort et al. 2009). These elegant models have convincingly shown that mutation of BRAF can drive nevus formation, and that a specific secondary lesion (e.g., Pten loss) collaborates to drive melanomagenesis. Whether this classical genetic oncogenic cooperation denotes an essential role of PTEN in BRAFE600-induced senescence remains to be established.
Tumor suppressor loss-induced senescence in vivo
Pandolfi and colleagues (Chen et al. 2005) were the first to show that senescence in vivo can also be triggered by the loss of a tumor suppressor gene. They found that conditional Pten deletion in murine prostate cells results in the formation of high-grade PIN, which display characteristics of senescence. In conjunction with p53 loss, these lesions progress to malignancy. Senescence induced by Pten loss can be enhanced by inactivation of the E3 ubiquitin ligase Skp2 (Lin et al. 2010). Similarly, Cichowski and coworkers (Courtois-Cox et al. 2006) showed that, in benign dermal neurofibromas carrying NF1 mutations, several senescence markers are up-regulated, while phospho-ERK and phospho-AKT are present at low levels. Finally, kidneys from Vhl knockout mice display an increase in SA-β-GAL activity as well as induced immunostaining for p27Kip1 and the senescence marker DcR2 (Young et al. 2008).
The Takahashi laboratory (Shamma et al. 2009) used a model of senescence in vivo in which genetic loss of one allele of Rb drives thyroid adenoma formation. These lesions display enhanced isoprenylation and activation of N-Ras and express several senescence markers, as discussed above. Homozygous loss of NRas in the context of Rb heterozygosity allowed for progression to carcinomas that was accompanied by the loss of senescence markers. Together, these examples provide the first pieces of evidence that, similar to activated oncogenes, loss of expression of tumor suppressors can also cause incipient cancer lesions to activate features of senescence, serving to limit tumorigenesis in vivo.
Restoration of cellular senescence in vivo
In light of the steadily increasing evidence that senescence protects humans and other organisms against cancer, ideas are being launched to restore this process in tumor cells in which it has become deficient. Induction of apoptosis in tumor cells, whether by chemotherapeutics or signaling molecules, is successfully used therapeutically. Would reactivation of senescence be similarly rewarding clinically? In particular, for those tumors that are highly resistant to drug- or radiotherapy-induced cell death, the concept of activating senescence in (early) tumors may sound appealing. But is it feasible? To explore the viability of such an approach, the Jacks (Ventura et al. 2007) and Lowe (Xue et al. 2007) laboratories have employed conditional mouse models. In the system used by Ventura et al. (2007) a transcription–translation stop site flanked by loxP sites within the p53 gene could be excised upon expression of Cre recombinase. Upon activation of p53 in already established lymphomas and sarcomas, dramatic tumor regression was observed. While this was associated with induction of apoptosis in lymphomas, sarcomas failed to undergo apoptosis, but instead displayed several characteristics of senescence. In contrast to tumor cells, restoration of p53 function in normal tissue did not result in detectable expression of the tumor suppressor. This suggests that restoration of p53-dependent senescence occurs only in the context of stress signals (Ventura et al. 2007). In the model by Xue et al. (2007), liver progenitor cells were infected ex vivo with retrovirus encoding HRASV12 and an inducible shRNA targeting p53. Upon transplantation into the spleen of recipient mice, the hepatoblasts seeded in the liver and produced invasive hepatocarcinomas. Reactivation of p53 caused these tumors to undergo senescence. Remarkably, an innate immune response was subsequently elicited, eventually resulting in the clearance of the tumors (Xue et al. 2007). Thus, these models have established that, at least under conditions in which widespread and acute activation of senescence can be achieved, this can culminate in tumor regression. Conversely, as has been shown for Myc, oncogene inactivation can also set off a senescence program in several tumors (Wu et al. 2007) in a TGFβ-dependent manner (van Riggelen et al. 2010). These studies may therefore serve as proof of principle that reactivation of senescence is a realistic means to intervene with cancer.
In several examples above, a tumor suppressor (p53) that contributed to the tumor initiation and maintenance was restored, resulting in senescence. Since inactivation, rather than restoration, of a tumor suppressor can also induce senescence in vivo (as discussed above for PTEN and NF1), it thus appears that tumor suppressors can differentially influence senescence. These effects can be seen even for a single tumor suppressor. For example, as ectopic expression of PTEN or suppression of PI3K also causes senescence (Courtois-Cox et al. 2006), together these observations suggest that major pathways like PI3K/PTEN require fine-tuning to maintain cell proliferation: Too little or too much activity may act cytostatically. Recently, the window in which reduction in PTEN levels induces senescence (PICS) has been proposed as a means to establish a prosenescence therapy (Alimonti et al. 2010). It was shown that pharmacologic inhibition of PTEN caused increased SA-β-GAL activity along with a reduction in cell proliferation both in vitro and in tumor xenografts. Along these lines, Lin et al. (2010) reported that a Skp2–SCF inhibitor triggers senescence and inhibition of tumor growth of PTEN-deficient cancer cells. In further support of this emerging theme, Amati and colleagues (Campaner et al. 2010) observed that oncogenic stress caused by the Myc oncoprotein sensitizes Cdk2-deficient cells to undergo senescence in vitro and in vivo. Similarly, in advanced non-small-cell lung carcinoma driven by activation of oncogenic KRas, tumor progression is halted and senescence is induced upon genetic ablation of Cdk4 (Puyol et al. 2010). The rising number of examples of enforced senescence in vivo justifies further exploration of this possibility by addressing several more clinically oriented questions.
Concluding remarks
The discovery of cellular senescence in cultured cells came with exciting hypotheses about the potential roles it may have in tumorigenesis and aging. Despite intensive research on this topic, four decades have passed before solid evidence was first presented that senescence occurs not only under artificial conditions in vitro, but also under pathophysiological conditions and in several genetic settings in vivo. Attempts to increase our understanding of this process were boosted by the discovery of OIS, which strengthened the link with cancer research. In spite of this important progress, however, many challenges remain. Probably most importantly, there is an urgent need for better senescence biomarkers. It is clear that, although a plethora of markers has been proposed and in fact are commonly used, no single one can reliably identify senescent cells in vitro or in vivo. Results from genome-wide expression analyses of senescent cells could serve as a convenient starting point for the identification of new and better senescence markers. Integrating these data with systematic RNAi approaches is likely to yield biomarkers with causal relationships to senescence. The contribution to senescence in vitro and in vivo of several cellular processes—including activation of DDR, SAHF formation, and induction of ROS and autophagy—also requires further elucidation. In addition, the question remains of which factors determine whether tissues primarily undergo senescence or other stress-induced programs like apoptosis. This may be determined by the abundance of cell-intrinsic survival proteins, but other factors, perhaps of stromal origin, are likely to add to the complexity of this choice. Several of these issues can be effectively investigated in mouse models; for instance, in animals conditionally expressing activated oncogenes from their endogenous promoters, or conditional tumor suppressor genes. It is conceivable that these as well as newly generated models will prove instrumental in validating results obtained in vitro. As therapeutic exploitation of enforced cellular senescence may become a realistic goal, answers to these questions may eventually provide us with new tools to effectively treat cancer patients.
Acknowledgments
T.K., C.M., W.J.M, and D.S.P. were supported by grants from the Dutch Cancer Society, including a Queen Wilhelmina Research Award, and a Vici grant from the Netherlands Organization for Scientific Research (NWO).
Footnotes
Article is online at http://www.genesdev.org/cgi/doi/10.1101/gad.1971610.
References
- Acosta JC, O'Loghlen A, Banito A, Guijarro MV, Augert A, Raguz S, Fumagalli M, Da Costa M, Brown C, Popov N, et al. 2008. Chemokine signaling via the CXCR2 receptor reinforces senescence. Cell 133: 1006–1018 [DOI] [PubMed] [Google Scholar]
- Adams PD 2007. Remodeling of chromatin structure in senescent cells and its potential impact on tumor suppression and aging. Gene 397: 84–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams PD 2009. Healing and hurting: Molecular mechanisms, functions, and pathologies of cellular senescence. Mol Cell 36: 2–14 [DOI] [PubMed] [Google Scholar]
- Agger K, Cloos PA, Rudkjaer L, Williams K, Andersen G, Christensen J, Helin K 2009. The H3K27me3 demethylase JMJD3 contributes to the activation of the INK4A–ARF locus in response to oncogene- and stress-induced senescence. Genes Dev 23: 1171–1176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alcorta DA, Xiong Y, Phelps D, Hannon G, Beach D, Barrett JC 1996. Involvement of the cyclin-dependent kinase inhibitor p16 (INK4a) in replicative senescence of normal human fibroblasts. Proc Natl Acad Sci 93: 13742–13747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alimonti A, Nardella C, Chen Z, Clohessy JG, Carracedo A, Trotman LC, Cheng K, Varmeh S, Kozma SC, Thomas G, et al. 2010. A novel type of cellular senescence that can be enhanced in mouse models and human tumor xenografts to suppress prostate tumorigenesis. J Clin Invest 120: 681–693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Artandi SE, DePinho RA 2010. Telomeres and telomerase in cancer. Carcinogenesis 31: 9–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atadja P, Wong H, Garkavtsev I, Veillette C, Riabowol K 1995. Increased activity of p53 in senescing fibroblasts. Proc Natl Acad Sci 92: 8348–8352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banito A, Rashid ST, Acosta JC, Li S, Pereira CF, Geti I, Pinho S, Silva JC, Azuara V, Walsh M, et al. 2009. Senescence impairs successful reprogramming to pluripotent stem cells. Genes Dev 23: 2134–2139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barradas M, Anderton E, Acosta JC, Li S, Banito A, Rodriguez-Niedenfuhr M, Maertens G, Banck M, Zhou MM, Walsh MJ, et al. 2009. Histone demethylase JMJD3 contributes to epigenetic control of INK4a/ARF by oncogenic RAS. Genes Dev 23: 1177–1182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartkova J, Rezaei N, Liontos M, Karakaidos P, Kletsas D, Issaeva N, Vassiliou L-VF, Kolettas E, Niforou K, Zoumpourlis VC, et al. 2006. Oncogene-induced senescence is part of the tumorigenesis barrier imposed by DNA damage checkpoints. Nature 444: 633–637 [DOI] [PubMed] [Google Scholar]
- Beauséjour CM, Krtolica A, Galimi F, Narita M, Lowe SW, Yaswen P, Campisi J 2003. Reversal of human cellular senescence: Roles of the p53 and p16 pathways. EMBO J 22: 4212–4222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennecke M, Kriegl L, Bajbouj M, Retzlaff K, Robine S, Jung A, Arkan MC, Kirchner T, Greten FR 2010. Ink4a/Arf and oncogene-induced senescence prevent tumor progression during alternative colorectal tumorigenesis. Cancer Cell 18: 135–146 [DOI] [PubMed] [Google Scholar]
- Bennett DC 2003. Human melanocyte senescence and melanoma susceptibility genes. Oncogene 22: 3063–3069 [DOI] [PubMed] [Google Scholar]
- Bennett DC, Medrano EE 2002. Molecular regulation of melanocyte senescence. Pigment Cell Res 15: 242–250 [DOI] [PubMed] [Google Scholar]
- Ben-Porath I, Weinberg RA 2005. The signals and pathways activating cellular senescence. Int J Biochem Cell Biol 37: 961–976 [DOI] [PubMed] [Google Scholar]
- Berns A 2002. Senescence: A companion in chemotherapy? Cancer Cell 1: 309–311 [DOI] [PubMed] [Google Scholar]
- Bodnar AG, Ouellette M, Frolkis M, Holt SE, Chiu CP, Morin GB, Harley CB, Shay JW, Lichtsteiner S, Wright WE 1998. Extension of life-span by introduction of telomerase into normal human cells. Science 279: 349–352 [DOI] [PubMed] [Google Scholar]
- Bracken AP, Kleine-Kohlbrecher D, Dietrich N, Pasini D, Gargiulo G, Beekman C, Theilgaard-Monch K, Minucci S, Porse BT, Marine JC, et al. 2007. The Polycomb group proteins bind throughout the INK4A-ARF locus and are disassociated in senescent cells. Genes Dev 21: 525–530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braig M, Lee S, Loddenkemper C, Rudolph C, Peters AHFM, Schlegelberger B, Stein H, Dörken B, Jenuwein T, Schmitt CA 2005. Oncogene-induced senescence as an initial barrier in lymphoma development. Nature 436: 660–665 [DOI] [PubMed] [Google Scholar]
- Bulavin DV, Kovalsky O, Hollander MC, Fornace AJ 2003. Loss of oncogenic H-ras-induced cell cycle arrest and p38 mitogen-activated protein kinase activation by disruption of Gadd45a. Mol Cell Biol 23: 3859–3871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunz F, Dutriaux A, Lengauer C, Waldman T, Zhou S, Brown JP, Sedivy JM, Kinzler KW, Vogelstein B 1998. Requirement for p53 and p21 to sustain G2 arrest after DNA damage. Science 282: 1497–1501 [DOI] [PubMed] [Google Scholar]
- Calabrese V, Mallette FA, Deschênes-Simard X, Ramanathan S, Gagnon J, Moores A, Ilangumaran S, Ferbeyre G 2009. SOCS1 links cytokine signaling to p53 and senescence. Mol Cell 36: 754–767 [DOI] [PubMed] [Google Scholar]
- Campaner S, Doni M, Hydbring P, Verrecchia A, Bianchi L, Sardella D, Schleker T, Perna D, Tronnersjö S, Murga M, et al. 2010. Cdk2 suppresses cellular senescence induced by the c-myc oncogene. Nat Cell Biol 12: 54–59; sup pp 51–14 [DOI] [PubMed] [Google Scholar]
- Campisi J 2005. Senescent cells, tumor suppression, and organismal aging: Good citizens, bad neighbors. Cell 120: 513–522 [DOI] [PubMed] [Google Scholar]
- Chan HM, Narita M, Lowe SW, Livingston DM 2005. The p400 E1A-associated protein is a novel component of the p53 → p21 senescence pathway. Genes Dev 19: 196–201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang BD, Xuan Y, Broude EV, Zhu H, Schott B, Fang J, Roninson IB 1999. Role of p53 and p21waf1/cip1 in senescence-like terminal proliferation arrest induced in human tumor cells by chemotherapeutic drugs. Oncogene 18: 4808–4818 [DOI] [PubMed] [Google Scholar]
- Chen Q, Ames BN 1994. Senescence-like growth arrest induced by hydrogen peroxide in human diploid fibroblast F65 cells. Proc Natl Acad Sci 91: 4130–4134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Q, Fischer A, Reagan JD, Yan LJ, Ames BN 1995. Oxidative DNA damage and senescence of human diploid fibroblast cells. Proc Natl Acad Sci 92: 4337–4341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen QM, Bartholomew JC, Campisi J, Acosta M, Reagan JD, Ames BN 1998. Molecular analysis of H2O2-induced senescent-like growth arrest in normal human fibroblasts: p53 and Rb control G1 arrest but not cell replication. Biochem J 332: 43–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen QM, Prowse KR, Tu VC, Purdom S, Linskens MH 2001. Uncoupling the senescent phenotype from telomere shortening in hydrogen peroxide-treated fibroblasts. Exp Cell Res 265: 294–303 [DOI] [PubMed] [Google Scholar]
- Chen Z, Trotman LC, Shaffer D, Lin H-K, Dotan ZA, Niki M, Koutcher JA, Scher HI, Ludwig T, Gerald W, et al. 2005. Crucial role of p53-dependent cellular senescence in suppression of Pten-deficient tumorigenesis. Nature 436: 725–730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X, Mitsutake N, LaPerle K, Akeno N, Zanzonico P, Longo VA, Mitsutake S, Kimura ET, Geiger H, Santos E, et al. 2009. Endogenous expression of Hras(G12V) induces developmental defects and neoplasms with copy number imbalances of the oncogene. Proc Natl Acad Sci 106: 7979–7984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chicas A, Wang X, Zhang C, McCurrach M, Zhao Z, Mert O, Dickins RA, Narita M, Zhang M, Lowe SW 2010. Dissecting the unique role of the retinoblastoma tumor suppressor during cellular senescence. Cancer Cell 17: 376–387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin L, Artandi SE, Shen Q, Tam A, Lee SL, Gottlieb GJ, Greider CW, DePinho RA 1999. p53 deficiency rescues the adverse effects of telomere loss and cooperates with telomere dysfunction to accelerate carcinogenesis. Cell 97: 527–538 [DOI] [PubMed] [Google Scholar]
- Collado M, Serrano M 2010. Senescence in tumours: Evidence from mice and humans. Nat Rev Cancer 10: 51–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collado M, Gil J, Efeyan A, Guerra C, Schuhmacher AJ, Barradas M, Benguría A, Zaballos A, Flores JM, Barbacid M, et al. 2005. Tumour biology: Senescence in premalignant tumours. Nature 436: 642. [DOI] [PubMed] [Google Scholar]
- Coppé J-P, Patil CK, Rodier F, Sun Y, Muñoz DP, Goldstein J, Nelson PS, Desprez P-Y, Campisi J 2008. Senescence-associated secretory phenotypes reveal cell-nonautonomous functions of oncogenic RAS and the p53 tumor suppressor. PLoS Biol 6: 2853–2868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosme-Blanco W, Shen M-F, Lazar AJF, Pathak S, Lozano G, Multani AS, Chang S 2007. Telomere dysfunction suppresses spontaneous tumorigenesis in vivo by initiating p53-dependent cellular senescence. EMBO Rep 8: 497–503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtois-Cox S, Genther Williams SM, Reczek EE, Johnson BW, McGillicuddy LT, Johannessen CM, Hollstein PE, MacCollin M, Cichowski K 2006. A negative feedback signaling network underlies oncogene-induced senescence. Cancer Cell 10: 459–472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cristofalo VJ, Lorenzini A, Allen RG, Torres C, Tresini M 2004. Replicative senescence: A critical review. Mech Ageing Dev 125: 827–848 [DOI] [PubMed] [Google Scholar]
- Cuervo AM, Dice JF 2000. Age-related decline in chaperone-mediated autophagy. J Biol Chem 275: 31505–31513 [DOI] [PubMed] [Google Scholar]
- D'Adda di Fagagna F 2008. Living on a break: Cellular senescence as a DNA-damage response. Nat Rev Cancer 8: 512–522 [DOI] [PubMed] [Google Scholar]
- D'Adda di Fagagna F, Reaper PM, Clay-Farrace L, Fiegler H, Carr P, Von Zglinicki T, Saretzki G, Carter NP, Jackson SP 2003. A DNA damage checkpoint response in telomere-initiated senescence. Nature 426: 194–198 [DOI] [PubMed] [Google Scholar]
- Dai CY, Furth EE, Mick R, Koh J, Takayama T, Niitsu Y, Enders GH 2000. p16(INK4a) expression begins early in human colon neoplasia and correlates inversely with markers of cell proliferation. Gastroenterology 119: 929–942 [DOI] [PubMed] [Google Scholar]
- Dankort D, Curley DP, Cartlidge RA, Nelson B, Karnezis AN, Damsky WE, You MJ, Depinho RA, McMahon M, Bosenberg M 2009. Braf(V600E) cooperates with Pten loss to induce metastatic melanoma. Nat Genet 41: 544–552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dannenberg JH, van Rossum A, Schuijff L, te Riele H 2000. Ablation of the retinoblastoma gene family deregulates G(1) control causing immortalization and increased cell turnover under growth-restricting conditions. Genes Dev 14: 3051–3064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies H, Bignell GR, Cox C, Stephens P, Edkins S, Clegg S, Teague J, Woffendin H, Garnett MJ, Bottomley W, et al. 2002. Mutations of the BRAF gene in human cancer. Nature 417: 949–954 [DOI] [PubMed] [Google Scholar]
- Debacq-Chainiaux F, Erusalimsky JD, Campisi J, Toussaint O 2009. Protocols to detect senescence-associated β-galactosidase (SA-βgal) activity, a biomarker of senescent cells in culture and in vivo. Nat Protoc 4: 1798–1806 [DOI] [PubMed] [Google Scholar]
- Deng Q, Liao R, Wu B-L, Sun P 2004. High intensity ras signaling induces premature senescence by activating p38 pathway in primary human fibroblasts. J Biol Chem 279: 1050–1059 [DOI] [PubMed] [Google Scholar]
- Denoyelle C, Abou-Rjaily G, Bezrookove V, Verhaegen M, Johnson TM, Fullen DR, Pointer JN, Gruber SB, Su LD, Nikiforov MA, et al. 2006. Anti-oncogenic role of the endoplasmic reticulum differentially activated by mutations in the MAPK pathway. Nat Cell Biol 8: 1053–1063 [DOI] [PubMed] [Google Scholar]
- Dhomen N, Reis-Filho JS, Da Rocha Dias S, Hayward R, Savage K, Delmas V, Larue L, Pritchard C, Marais R 2009. Oncogenic Braf induces melanocyte senescence and melanoma in mice. Cancer Cell 15: 294–303 [DOI] [PubMed] [Google Scholar]
- Di Leonardo A, Linke SP, Clarkin K, Wahl GM 1994. DNA damage triggers a prolonged p53-dependent G1 arrest and long-term induction of Cip1 in normal human fibroblasts. Genes Dev 8: 2540–2551 [DOI] [PubMed] [Google Scholar]
- Dilley TK, Bowden GT, Chen QM 2003. Novel mechanisms of sublethal oxidant toxicity: Induction of premature senescence in human fibroblasts confers tumor promoter activity. Exp Cell Res 290: 38–48 [DOI] [PubMed] [Google Scholar]
- Di Micco R, Fumagalli M, Cicalese A, Piccinin S, Gasparini P, Luise C, Schurra C, Garré M, Nuciforo PG, Bensimon A, et al. 2006. Oncogene-induced senescence is a DNA damage response triggered by DNA hyper-replication. Nature 444: 638–642 [DOI] [PubMed] [Google Scholar]
- Dimri GP, Lee X, Basile G, Acosta M, Scott G, Roskelley C, Medrano EE, Linskens M, Rubelj I, Pereira-Smith OM 1995. A biomarker that identifies senescent human cells in culture and in aging skin in vivo. Proc Natl Acad Sci 92: 9363–9367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dirac AMG, Bernards R 2003. Reversal of senescence in mouse fibroblasts through lentiviral suppression of p53. J Biol Chem 278: 11731–11734 [DOI] [PubMed] [Google Scholar]
- Efeyan A, Murga M, Martinez-Pastor B, Ortega-Molina A, Soria R, Collado M, Fernandez-Capetillo O, Serrano M 2009. Limited role of murine ATM in oncogene-induced senescence and p53-dependent tumor suppression. PLoS ONE 4: e5475 doi: 10.1371/journal.pone.0005475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elenbaas B, Spirio L, Koerner F, Fleming MD, Zimonjic DB, Donaher JL, Popescu NC, Hahn WC, Weinberg RA 2001. Human breast cancer cells generated by oncogenic transformation of primary mammary epithelial cells. Genes Dev 15: 50–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erickson S, Sangfelt O, Heyman M, Castro J, Einhorn S, Grandér D 1998. Involvement of the Ink4 proteins p16 and p15 in T-lymphocyte senescence. Oncogene 17: 595–602 [DOI] [PubMed] [Google Scholar]
- Feldser DM, Greider CW 2007. Short telomeres limit tumor progression in vivo by inducing senescence. Cancer Cell 11: 461–469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finney RE, Bishop JM 1993. Predisposition to neoplastic transformation caused by gene replacement of H-ras1. Science 260: 1524–1527 [DOI] [PubMed] [Google Scholar]
- Foreman KE, Tang J 2003. Molecular mechanisms of replicative senescence in endothelial cells. Exp Gerontol 38: 1251–1257 [DOI] [PubMed] [Google Scholar]
- Franza BR, Maruyama K, Garrels JI, Ruley HE 1986. In vitro establishment is not a sufficient prerequisite for transformation by activated ras oncogenes. Cell 44: 409–418 [DOI] [PubMed] [Google Scholar]
- Freedberg DE, Rigas SH, Russak J, Gai W, Kaplow M, Osman I, Turner F, Randerson-Moor JA, Houghton A, Busam K, et al. 2008. Frequent p16-independent inactivation of p14ARF in human melanoma. J Natl Cancer Inst 100: 784–795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujita K, Mondal AM, Horikawa I, Nguyen GH, Kumamoto K, Sohn JJ, Bowman ED, Mathe EA, Schetter AJ, Pine SR, et al. 2009. p53 isoforms Δ133p53 and p53β are endogenous regulators of replicative cellular senescence. Nat Cell Biol 11: 1135–1142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furumoto K, Inoue E, Nagao N, Hiyama E, Miwa N 1998. Age-dependent telomere shortening is slowed down by enrichment of intracellular vitamin C via suppression of oxidative stress. Life Sci 63: 935–948 [DOI] [PubMed] [Google Scholar]
- Gil J, Bernard D, Martinez D, Beach D 2004. Polycomb CBX7 has a unifying role in cellular lifespan. Nat Cell Biol 6: 67–72 [DOI] [PubMed] [Google Scholar]
- Goel VK, Ibrahim N, Jiang G, Singhal M, Fee S, Flotte T, Westmoreland S, Haluska FS, Hinds PW, Haluska FG 2009. Melanocytic nevus-like hyperplasia and melanoma in transgenic BRAFV600E mice. Oncogene 28: 2289–2298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Going JJ, Stuart RC, Downie M, Fletcher-Monaghan AJ, Keith WN 2002. ‘Senescence-associated’ β-galactosidase activity in the upper gastrointestinal tract. J Pathol 196: 394–400 [DOI] [PubMed] [Google Scholar]
- Goldstein S, Moerman EJ, Fujii S, Sobel BE 1994. Overexpression of plasminogen activator inhibitor type-1 in senescent fibroblasts from normal subjects and those with Werner syndrome. J Cell Physiol 161: 571–579 [DOI] [PubMed] [Google Scholar]
- Gray-Schopfer VC, Cheong SC, Chong H, Chow J, Moss T, Abdel-Malek ZA, Marais R, Wynford-Thomas D, Bennett DC 2006. Cellular senescence in naevi and immortalisation in melanoma: A role for p16? Br J Cancer 95: 496–505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg RA, Chin L, Femino A, Lee KH, Gottlieb GJ, Singer RH, Greider CW, DePinho RA 1999. Short dysfunctional telomeres impair tumorigenesis in the INK4a(Δ2/3) cancer-prone mouse. Cell 97: 515–525 [DOI] [PubMed] [Google Scholar]
- Gruis NA, van der Velden PA, Sandkuijl LA, Prins DE, Weaver-Feldhaus J, Kamb A, Bergman W, Frants RR 1995. Homozygotes for CDKN2 (p16) germline mutation in Dutch familial melanoma kindreds. Nat Genet 10: 351–353 [DOI] [PubMed] [Google Scholar]
- Guerra C, Mijimolle N, Dhawahir A, Dubus P, Barradas M, Serrano M, Campuzano V, Barbacid M 2003. Tumor induction by an endogenous K-ras oncogene is highly dependent on cellular context. Cancer Cell 4: 111–120 [DOI] [PubMed] [Google Scholar]
- Haferkamp S, Scurr LL, Becker TM, Frausto M, Kefford RF, Rizos H 2009. Oncogene-induced senescence does not require the p16(INK4a) or p14ARF melanoma tumor suppressors. J Invest Dermatol 129: 1983–1991 [DOI] [PubMed] [Google Scholar]
- Hanna J, Saha K, Pando B, van Zon J, Lengner CJ, Creyghton MP, van Oudenaarden A, Jaenisch R 2009. Direct cell reprogramming is a stochastic process amenable to acceleration. Nature 462: 595–601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hara E, Smith R, Parry D, Tahara H, Stone S, Peters G 1996. Regulation of p16CDKN2 expression and its implications for cell immortalization and senescence. Mol Cell Biol 16: 859–867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harley CB, Futcher AB, Greider CW 1990. Telomeres shorten during ageing of human fibroblasts. Nature 345: 458–460 [DOI] [PubMed] [Google Scholar]
- Haugstetter AM, Loddenkemper C, Lenze D, Grone J, Standfuss C, Petersen I, Dorken B, Schmitt CA 2010. Cellular senescence predicts treatment outcome in metastasised colorectal cancer. Br J Cancer 103: 505–509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayflick L 1965. The limited in vitro lifetime of human diploid cell strains. Exp Cell Res 37: 614–636 [DOI] [PubMed] [Google Scholar]
- Hayflick L, Moorhead PS 1961. The serial cultivation of human diploid cell strains. Exp Cell Res 25: 585–621 [DOI] [PubMed] [Google Scholar]
- Herbert B-S, Wright WE, Shay JW 2002. p16(INK4a) inactivation is not required to immortalize human mammary epithelial cells. Oncogene 21: 7897–7900 [DOI] [PubMed] [Google Scholar]
- Herbig U, Ferreira M, Condel L, Carey D, Sedivy JM 2006. Cellular senescence in aging primates. Science 311: 1257. [DOI] [PubMed] [Google Scholar]
- Hitomi T, Matsuzaki Y, Yasuda S, Kawanaka M, Yogosawa S, Koyama M, Tantin D, Sakai T 2007. Oct-1 is involved in the transcriptional repression of the p15(INK4b) gene. FEBS Lett 581: 1087–1092 [DOI] [PubMed] [Google Scholar]
- Hong H, Takahashi K, Ichisaka T, Aoi T, Kanagawa O, Nakagawa M, Okita K, Yamanaka S 2009. Suppression of induced pluripotent stem cell generation by the p53–p21 pathway. Nature 460: 1132–1135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Itahana K, Zou Y, Itahana Y, Martinez J-L, Beausejour C, Jacobs JJL, van Lohuizen M, Band V, Campisi J, Dimri GP 2003. Control of the replicative life span of human fibroblasts by p16 and the polycomb protein Bmi-1. Mol Cell Biol 23: 389–401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwasa H, Han J, Ishikawa F 2003. Mitogen-activated protein kinase p38 defines the common senescence-signalling pathway. Genes Cells 8: 131–144 [DOI] [PubMed] [Google Scholar]
- Jacobs JJ, Kieboom K, Marino S, DePinho RA, van Lohuizen M 1999. The oncogene and Polycomb-group gene bmi-1 regulates cell proliferation and senescence through the ink4a locus. Nature 397: 164–168 [DOI] [PubMed] [Google Scholar]
- Jeyapalan JC, Ferreira M, Sedivy JM, Herbig U 2007. Accumulation of senescent cells in mitotic tissue of aging primates. Mech Ageing Dev 128: 36–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SM, Grosshans H, Shingara J, Byrom M, Jarvis R, Cheng A, Labourier E, Reinert KL, Brown D, Slack FJ 2005. RAS is regulated by the let-7 microRNA family. Cell 120: 635–647 [DOI] [PubMed] [Google Scholar]
- Kamijo T, Zindy F, Roussel MF, Quelle DE, Downing JR, Ashmun RA, Grosveld G, Sherr CJ 1997. Tumor suppression at the mouse INK4a locus mediated by the alternative reading frame product p19ARF. Cell 91: 649–659 [DOI] [PubMed] [Google Scholar]
- Kato D, Miyazawa K, Ruas M, Starborg M, Wada I, Oka T, Sakai T, Peters G, Hara E 1998. Features of replicative senescence induced by direct addition of antennapedia-p16INK4A fusion protein to human diploid fibroblasts. FEBS Lett 427: 203–208 [DOI] [PubMed] [Google Scholar]
- Kawamura T, Suzuki J, Wang YV, Menendez S, Morera LB, Raya A, Wahl GM, Belmonte JCI 2009. Linking the p53 tumour suppressor pathway to somatic cell reprogramming. Nature 460: 1140–1144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim K, Kang K, Seu Y, Baek S, Kim J 2009. Interferon-γ induces cellular senescence through p53-dependent DNA damage signaling in human endothelial cells. Mech Ageing Dev 130: 179–188 [DOI] [PubMed] [Google Scholar]
- Kipling D, Cooke HJ 1990. Hypervariable ultra-long telomeres in mice. Nature 347: 400–402 [DOI] [PubMed] [Google Scholar]
- Kiyono T, Foster SA, Koop JI, McDougall JK, Galloway DA, Klingelhutz AJ 1998. Both Rb/p16INK4a inactivation and telomerase activity are required to immortalize human epithelial cells. Nature 396: 84–88 [DOI] [PubMed] [Google Scholar]
- Kortlever RM, Higgins PJ, Bernards R 2006. Plasminogen activator inhibitor-1 is a critical downstream target of p53 in the induction of replicative senescence. Nat Cell Biol 8: 877–884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krimpenfort P, Quon KC, Mooi WJ, Loonstra A, Berns A 2001. Loss of p16Ink4a confers susceptibility to metastatic melanoma in mice. Nature 413: 83–86 [DOI] [PubMed] [Google Scholar]
- Krizhanovsky V, Lowe SW 2009. Stem cells: The promises and perils of p53. Nature 460: 1085–1086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krizhanovsky V, Yon M, Dickins RA, Hearn S, Simon J, Miething C, Yee H, Zender L, Lowe SW 2008. Senescence of activated stellate cells limits liver fibrosis. Cell 134: 657–667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krtolica A, Parrinello S, Lockett S, Desprez PY, Campisi J 2001. Senescent fibroblasts promote epithelial cell growth and tumorigenesis: A link between cancer and aging. Proc Natl Acad Sci 98: 12072–12077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuilman T, Peeper DS 2009. Senescence-messaging secretome: SMS-ing cellular stress. Nat Rev Cancer 9: 81–94 [DOI] [PubMed] [Google Scholar]
- Kuilman T, Michaloglou C, Vredeveld LCW, Douma S, van Doorn R, Desmet CJ, Aarden LA, Mooi WJ, Peeper DS 2008. Oncogene-induced senescence relayed by an interleukin-dependent inflammatory network. Cell 133: 1019–1031 [DOI] [PubMed] [Google Scholar]
- Kurz DJ, Decary S, Hong Y, Erusalimsky JD 2000. Senescence-associated β-galactosidase reflects an increase in lysosomal mass during replicative ageing of human endothelial cells. J Cell Sci 113: 3613–3622 [DOI] [PubMed] [Google Scholar]
- Land H, Parada LF, Weinberg RA 1983. Tumorigenic conversion of primary embryo fibroblasts requires at least two cooperating oncogenes. Nature 304: 596–602 [DOI] [PubMed] [Google Scholar]
- Lazzerini Denchi E, Attwooll C, Pasini D, Helin K 2005. Deregulated E2F activity induces hyperplasia and senescence-like features in the mouse pituitary gland. Mol Cell Biol 25: 2660–2672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee AC, Fenster BE, Ito H, Takeda K, Bae NS, Hirai T, Yu ZX, Ferrans VJ, Howard BH, Finkel T 1999. Ras proteins induce senescence by altering the intracellular levels of reactive oxygen species. J Biol Chem 274: 7936–7940 [DOI] [PubMed] [Google Scholar]
- Lee BY, Han JA, Im JS, Morrone A, Johung K, Goodwin EC, Kleijer WJ, DiMaio D, Hwang ES 2006. Senescence-associated β-galactosidase is lysosomal β-galactosidase. Aging Cell 5: 187–195 [DOI] [PubMed] [Google Scholar]
- Levine B, Kroemer G 2008. Autophagy in the pathogenesis of disease. Cell 132: 27–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H, Collado M, Villasante A, Strati K, Ortega S, Cañamero M, Blasco MA, Serrano M 2009. The Ink4/Arf locus is a barrier for iPS cell reprogramming. Nature 460: 1136–1139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin AW, Barradas M, Stone JC, van Aelst L, Serrano M, Lowe SW 1998. Premature senescence involving p53 and p16 is activated in response to constitutive MEK/MAPK mitogenic signaling. Genes Dev 12: 3008–3019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin H-K, Chen Z, Wang G, Nardella C, Lee S-W, Chan C-H, Yang W-L, Wang J, Egia A, Nakayama KI, et al. 2010. Skp2 targeting suppresses tumorigenesis by Arf-p53-independent cellular senescence. Nature 464: 374–379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loo DT, Fuquay JI, Rawson CL, Barnes DW 1987. Extended culture of mouse embryo cells without senescence: Inhibition by serum. Science 236: 200–202 [DOI] [PubMed] [Google Scholar]
- Lowe SW, Cepero E, Evan GI 2004. Intrinsic tumour suppression. Nature 432: 307–315 [DOI] [PubMed] [Google Scholar]
- Lu T, Finkel T 2008. Free radicals and senescence. Exp Cell Res 314: 1918–1922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu C, Vickers MF, Kerbel RS 1992. Interleukin 6: A fibroblast-derived growth inhibitor of human melanoma cells from early but not advanced stages of tumor progression. Proc Natl Acad Sci 89: 9215–9219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu C, Sheehan C, Rak JW, Chambers CA, Hozumi N, Kerbel RS 1996. Endogenous interleukin 6 can function as an in vivo growth- stimulatory factor for advanced-stage human melanoma cells. Clin Cancer Res 2: 1417–1425 [PubMed] [Google Scholar]
- Maldonado JL, Timmerman L, Fridlyand J, Bastian BC 2004. Mechanisms of cell-cycle arrest in Spitz nevi with constitutive activation of the MAP-kinase pathway. Am J Pathol 164: 1783–1787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallette FA, Gaumont-Leclerc M-F, Ferbeyre G 2007. The DNA damage signaling pathway is a critical mediator of oncogene-induced senescence. Genes Dev 21: 43–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marión RM, Strati K, Li H, Murga M, Blanco R, Ortega S, Fernandez-Capetillo O, Serrano M, Blasco MA 2009. A p53-mediated DNA damage response limits reprogramming to ensure iPS cell genomic integrity. Nature 460: 1149–1153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massagué J 2008. TGFβ in cancer. Cell 134: 215–230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masutomi K, Yu EY, Khurts S, Ben-Porath I, Currier JL, Metz GB, Brooks MW, Kaneko S, Murakami S, DeCaprio JA, et al. 2003. Telomerase maintains telomere structure in normal human cells. Cell 114: 241–253 [DOI] [PubMed] [Google Scholar]
- Mathon NF, Malcolm DS, Harrisingh MC, Cheng L, Lloyd AC 2001. Lack of replicative senescence in normal rodent glia. Science 291: 872–875 [DOI] [PubMed] [Google Scholar]
- Michaloglou C, Vredeveld LCW, Soengas MS, Denoyelle C, Kuilman T, van der Horst CMAM, Majoor DM, Shay JW, Mooi WJ, Peeper DS 2005. BRAFE600-associated senescence-like cell cycle arrest of human naevi. Nature 436: 720–724 [DOI] [PubMed] [Google Scholar]
- Michaloglou C, Vredeveld LCW, Mooi WJ, Peeper DS 2008. BRAF(E600) in benign and malignant human tumours. Oncogene 27: 877–895 [DOI] [PubMed] [Google Scholar]
- Minamino T, Miyauchi H, Yoshida T, Ishida Y, Yoshida H, Komuro I 2002. Endothelial cell senescence in human atherosclerosis: Role of telomere in endothelial dysfunction. Circulation 105: 1541–1544 [DOI] [PubMed] [Google Scholar]
- Moiseeva O, Mallette FA, Mukhopadhyay UK, Moores A, Ferbeyre G 2006. DNA damage signaling and p53-dependent senescence after prolonged β-interferon stimulation. Mol Biol Cell 17: 1583–1592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moiseeva O, Bourdeau V, Roux A, Deschênes-Simard X, Ferbeyre G 2009. Mitochondrial dysfunction contributes to oncogene-induced senescence. Mol Cell Biol 29: 4495–4507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muntoni A, Reddel R.R. 2005. The first molecular details of ALT in human tumor cells. Hum Mol Genet 14: R191–R196 doi: 10.1093/hmg/ddi266 [DOI] [PubMed] [Google Scholar]
- Narita M, Nũnez S, Heard E, Narita M, Lin AW, Hearn SA, Spector DL, Hannon GJ, Lowe SW 2003. Rb-mediated heterochromatin formation and silencing of E2F target genes during cellular senescence. Cell 113: 703–716 [DOI] [PubMed] [Google Scholar]
- Narita M, Narita M, Krizhanovsky V, Nuñez S, Chicas A, Hearn SA, Myers MP, Lowe SW 2006. A novel role for high-mobility group a proteins in cellular senescence and heterochromatin formation. Cell 126: 503–514 [DOI] [PubMed] [Google Scholar]
- Nicke B, Bastien J, Khanna SJ, Warne PH, Cowling V, Cook SJ, Peters G, Delpuech O, Schulze A, Berns K, et al. 2005. Involvement of MINK, a Ste20 family kinase, in Ras oncogene-induced growth arrest in human ovarian surface epithelial cells. Mol Cell 20: 673–685 [DOI] [PubMed] [Google Scholar]
- Okamura M, Unami A, Matsumoto M, Oishi Y, Kashida Y, Mitsumori K 2006. Gene expression analysis of urethane-induced lung tumors in ras H2 mice. Toxicology 217: 129–138 [DOI] [PubMed] [Google Scholar]
- Olovnikov AM 1971. Principle of marginotomy in template synthesis of polynucleotides. Dokl Akad Nauk SSSR 201: 1496–1499 [PubMed] [Google Scholar]
- Olsen CL, Gardie B, Yaswen P, Stampfer MR 2002. Raf-1-induced growth arrest in human mammary epithelial cells is p16-independent and is overcome in immortal cells during conversion. Oncogene 21: 6328–6339 [DOI] [PubMed] [Google Scholar]
- Packer L, Fuehr K 1977. Low oxygen concentration extends the lifespan of cultured human diploid cells. Nature 267: 423–425 [DOI] [PubMed] [Google Scholar]
- Park HK, Leonard DD, Arrington JH, Lund HZ 1987. Recurrent melanocytic nevi: Clinical and histologic review of 175 cases. J Am Acad Dermatol 17: 285–292 [DOI] [PubMed] [Google Scholar]
- Parrinello S, Samper E, Krtolica A, Goldstein J, Melov S, Campisi J 2003. Oxygen sensitivity severely limits the replicative lifespan of murine fibroblasts. Nat Cell Biol 5: 741–747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parrinello S, Coppe J-P, Krtolica A, Campisi J 2005. Stromal–epithelial interactions in aging and cancer: Senescent fibroblasts alter epithelial cell differentiation. J Cell Sci 118: 485–496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passos JF, Nelson G, Wang C, Richter T, Simillion C, Proctor CJ, Miwa S, Olijslagers S, Hallinan J, Wipat A, et al. 2010. Feedback between p21 and reactive oxygen production is necessary for cell senescence. Mol Syst Biol 6: 347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patschan S, Chen J, Polotskaia A, Mendelev N, Cheng J, Patschan D, Goligorsky MS 2008. Lipid mediators of autophagy in stress-induced premature senescence of endothelial cells. Am J Physiol Heart Circ Physiol 294: H1119–H1129 doi: 10.1152/ajpheart.00713.2007 [DOI] [PubMed] [Google Scholar]
- Patton EE, Widlund HR, Kutok JL, Kopani KR, Amatruda JF, Murphey RD, Berghmans S, Mayhall EA, Traver D, Fletcher CDM, et al. 2005. BRAF mutations are sufficient to promote nevi formation and cooperate with p53 in the genesis of melanoma. Curr Biol 15: 249–254 [DOI] [PubMed] [Google Scholar]
- Peeper DS 2009. Ras and pRb: The relationship gets yet more intimate. Cancer Cell 15: 243–245 [DOI] [PubMed] [Google Scholar]
- Pollock PM, Harper UL, Hansen KS, Yudt LM, Stark M, Robbins CM, Moses TY, Hostetter G, Wagner U, Kakareka J, et al. 2003. High frequency of BRAF mutations in nevi. Nat Genet 33: 19–20 [DOI] [PubMed] [Google Scholar]
- Price JS, Waters JG, Darrah C, Pennington C, Edwards DR, Donell ST, Clark IM 2002. The role of chondrocyte senescence in osteoarthritis. Aging Cell 1: 57–65 [DOI] [PubMed] [Google Scholar]
- Prowse KR, Greider CW 1995. Developmental and tissue-specific regulation of mouse telomerase and telomere length. Proc Natl Acad Sci 92: 4818–4822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puyol M, Martin A, Dubus P, Mulero F, Pizcueta P, Khan G, Guerra C, Santamaria D, Barbacid M 2010. A synthetic lethal interaction between K-Ras oncogenes and Cdk4 unveils a therapeutic strategy for non-small cell lung carcinoma. Cancer Cell 18: 63–73 [DOI] [PubMed] [Google Scholar]
- Quintanilla M, Brown K, Ramsden M, Balmain A 1986. Carcinogen-specific mutation and amplification of Ha-ras during mouse skin carcinogenesis. Nature 322: 78–80 [DOI] [PubMed] [Google Scholar]
- Ramirez RD, Morales CP, Herbert BS, Rohde JM, Passons C, Shay JW, Wright WE 2001. Putative telomere-independent mechanisms of replicative aging reflect inadequate growth conditions. Genes Dev 15: 398–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reimann M, Lee S, Loddenkemper C, Dörr JR, Tabor V, Aichele P, Stein H, Dörken B, Jenuwein T, Schmitt CA 2010. Tumor stroma-derived TGF-β limits myc-driven lymphomagenesis via Suv39h1-dependent senescence. Cancer Cell 17: 262–272 [DOI] [PubMed] [Google Scholar]
- Reznikoff CA, Yeager TR, Belair CD, Savelieva E, Puthenveettil JA, Stadler WM 1996. Elevated p16 at senescence and loss of p16 at immortalization in human papillomavirus 16 E6, but not E7, transformed human uroepithelial cells. Cancer Res 56: 2886–2890 [PubMed] [Google Scholar]
- Robles SJ, Adami GR 1998. Agents that cause DNA double strand breaks lead to p16INK4a enrichment and the premature senescence of normal fibroblasts. Oncogene 16: 1113–1123 [DOI] [PubMed] [Google Scholar]
- Rodier F, Coppé J-P, Patil CK, Hoeijmakers WAM, Muñoz DP, Raza SR, Freund A, Campeau E, Davalos AR, Campisi J 2009. Persistent DNA damage signalling triggers senescence-associated inflammatory cytokine secretion. Nat Cell Biol 11: 973–979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Puebla ML, LaCava M, Bolontrade MF, Russell J, Conti CJ 1999. Increased expression of mutated Ha-ras during premalignant progression in SENCAR mouse skin. Mol Carcinog 26: 150–156 [PubMed] [Google Scholar]
- Roninson IB 2003. Tumor cell senescence in cancer treatment. Cancer Res 63: 2705–2715 [PubMed] [Google Scholar]
- Sage J, Mulligan GJ, Attardi LD, Miller A, Chen S, Williams B, Theodorou E, Jacks T 2000. Targeted disruption of the three Rb-related genes leads to loss of G(1) control and immortalization. Genes Dev 14: 3037–3050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santoriello C, Deflorian G, Pezzimenti F, Kawakami K, Lanfrancone L, D'Adda di Fagagna F, Mione M 2009. Expression of H-RASV12 in a zebrafish model of Costello syndrome causes cellular senescence in adult proliferating cells. Dis Model Mech 2: 56–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkisian CJ, Keister BA, Stairs DB, Boxer RB, Moody SE, Chodosh LA 2007. Dose-dependent oncogene-induced senescence in vivo and its evasion during mammary tumorigenesis. Nat Cell Biol 9: 493–505 [DOI] [PubMed] [Google Scholar]
- Schmitt CA, Fridman JS, Yang M, Lee S, Baranov E, Hoffman RM, Lowe SW 2002. A senescence program controlled by p53 and p16INK4a contributes to the outcome of cancer therapy. Cell 109: 335–346 [DOI] [PubMed] [Google Scholar]
- Schoenfeld R, Pinkus H 1958. The recurrence of nevi after incomplete removal. AMA Arch Derm 78: 30–35 [DOI] [PubMed] [Google Scholar]
- Schrama D, Kneitz H, Willmes C, Adam C, Houben R, Becker JC 2010. Lack of correlation between IGFBP7 expression and BRAF mutational status in melanoma. J Invest Dermatol 130: 897–898 [DOI] [PubMed] [Google Scholar]
- Scurr LL, Pupo GM, Becker TM, Lai K, Schrama D, Haferkamp S, Irvine M, Scolyer RA, Mann GJ, Becker JC, et al. 2010. IGFBP7 is not required for B-RAF-induced melanocyte senescence. Cell 141: 717–727 [DOI] [PubMed] [Google Scholar]
- Serrano M, Lin AW, McCurrach ME, Beach D, Lowe SW 1997. Oncogenic ras provokes premature cell senescence associated with accumulation of p53 and p16INK4a. Cell 88: 593–602 [DOI] [PubMed] [Google Scholar]
- Severino J, Allen RG, Balin S, Balin A, Cristofalo VJ 2000. Is β-galactosidase staining a marker of senescence in vitro and in vivo? Exp Cell Res 257: 162–171 [DOI] [PubMed] [Google Scholar]
- Shamma A, Takegami Y, Miki T, Kitajima S, Noda M, Obara T, Okamoto T, Takahashi C 2009. Rb Regulates DNA damage response and cellular senescence through E2F-dependent suppression of N-ras isoprenylation. Cancer Cell 15: 255–269 [DOI] [PubMed] [Google Scholar]
- Sharpless NE, Bardeesy N, Lee KH, Carrasco D, Castrillon DH, Aguirre AJ, Wu EA, Horner JW, DePinho RA 2001. Loss of p16Ink4a with retention of p19Arf predisposes mice to tumorigenesis. Nature 413: 86–91 [DOI] [PubMed] [Google Scholar]
- Shay JW, Bacchetti S 1997. A survey of telomerase activity in human cancer. Eur J Cancer 33: 787–791 [DOI] [PubMed] [Google Scholar]
- Shay JW, Wright WE 2005. Senescence and immortalization: Role of telomeres and telomerase. Carcinogenesis 26: 867–874 [DOI] [PubMed] [Google Scholar]
- Shay JW, Wright WE 2006. Telomerase therapeutics for cancer: Challenges and new directions. Nat Rev Drug Discov 5: 577–584 [DOI] [PubMed] [Google Scholar]
- Shay JW, Pereira-Smith OM, Wright WE 1991. A role for both RB and p53 in the regulation of human cellular senescence. Exp Cell Res 196: 33–39 [DOI] [PubMed] [Google Scholar]
- Shelton DN, Chang E, Whittier PS, Choi D, Funk WD 1999. Microarray analysis of replicative senescence. Curr Biol 9: 939–945 [DOI] [PubMed] [Google Scholar]
- Sherr CJ, DePinho RA 2000. Cellular senescence: Mitotic clock or culture shock? Cell 102: 407–410 [DOI] [PubMed] [Google Scholar]
- Stein GH, Beeson M, Gordon L 1990. Failure to phosphorylate the retinoblastoma gene product in senescent human fibroblasts. Science 249: 666–669 [DOI] [PubMed] [Google Scholar]
- Sun P, Yoshizuka N, New L, Moser BA, Li Y, Liao R, Xie C, Chen J, Deng Q, Yamout M, et al. 2007. PRAK is essential for ras-induced senescence and tumor suppression. Cell 128: 295–308 [DOI] [PubMed] [Google Scholar]
- Takahashi A, Ohtani N, Yamakoshi K, Iida S-i, Tahara H, Nakayama K, Nakayama KI, Ide T, Saya H, Hara E 2006. Mitogenic signalling and the p16INK4a–Rb pathway cooperate to enforce irreversible cellular senescence. Nat Cell Biol 8: 1291–1297 [DOI] [PubMed] [Google Scholar]
- Tanaka N, Ishihara M, Kitagawa M, Harada H, Kimura T, Matsuyama T, Lamphier MS, Aizawa S, Mak TW, Taniguchi T 1994. Cellular commitment to oncogene-induced transformation or apoptosis is dependent on the transcription factor IRF-1. Cell 77: 829–839 [DOI] [PubMed] [Google Scholar]
- Tang DG, Tokumoto YM, Apperly JA, Lloyd AC, Raff MC 2001. Lack of replicative senescence in cultured rat oligodendrocyte precursor cells. Science 291: 868–871 [DOI] [PubMed] [Google Scholar]
- te Poele RH, Okorokov AL, Jardine L, Cummings J, Joel SP 2002. DNA damage is able to induce senescence in tumor cells in vitro and in vivo. Cancer Res 62: 1876–1883 [PubMed] [Google Scholar]
- Tuveson DA, Shaw AT, Willis NA, Silver DP, Jackson EL, Chang S, Mercer KL, Grochow R, Hock H, Crowley D, et al. 2004. Endogenous oncogenic K-ras(G12D) stimulates proliferation and widespread neoplastic and developmental defects. Cancer Cell 5: 375–387 [DOI] [PubMed] [Google Scholar]
- Utikal J, Polo JM, Stadtfeld M, Maherali N, Kulalert W, Walsh RM, Khalil A, Rheinwald JG, Hochedlinger K 2009. Immortalization eliminates a roadblock during cellular reprogramming into iPS cells. Nature 460: 1145–1148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Riggelen J, Muller J, Otto T, Beuger V, Yetil A, Choi PS, Kosan C, Moroy T, Felsher DW, Eilers M 2010. The interaction between Myc and Miz1 is required to antagonize TGFβ-dependent autocrine signaling during lymphoma formation and maintenance. Genes Dev 24: 1281–1294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaziri H, Benchimol S 1998. Reconstitution of telomerase activity in normal human cells leads to elongation of telomeres and extended replicative life span. Curr Biol 8: 279–282 [DOI] [PubMed] [Google Scholar]
- Vaziri H, West MD, Allsopp RC, Davison TS, Wu YS, Arrowsmith CH, Poirier GG, Benchimol S 1997. ATM-dependent telomere loss in aging human diploid fibroblasts and DNA damage lead to the post-translational activation of p53 protein involving poly(ADP-ribose) polymerase. EMBO J 16: 6018–6033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventura A, Kirsch DG, Mclaughlin ME, Tuveson DA, Grimm J, Lintault L, Newman J, Reczek EE, Weissleder R, Jacks T 2007. Restoration of p53 function leads to tumour regression in vivo. Nature 445: 661–665 [DOI] [PubMed] [Google Scholar]
- Wajapeyee N, Serra RW, Zhu X, Mahalingam M, Green MR 2008. Oncogenic BRAF induces senescence and apoptosis through pathways mediated by the secreted protein IGFBP7. Cell 132: 363–374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wajapeyee N, Serra RW, Zhu X, Mahalingam M, Green MR 2010. Role for IGFBP7 in senescence induction by BRAF. Cell 141: 746–747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Wong SC, Pan J, Tsao SW, Fung KH, Kwong DL, Sham JS, Nicholls JM 1998. Evidence of cisplatin-induced senescent-like growth arrest in nasopharyngeal carcinoma cells. Cancer Res 58: 5019–5022 [PubMed] [Google Scholar]
- Wang W, Chen JX, Liao R, Deng Q, Zhou JJ, Huang S, Sun P 2002. Sequential activation of the MEK-extracellular signal-regulated kinase and MKK3/6-p38 mitogen-activated protein kinase pathways mediates oncogenic ras-induced premature senescence. Mol Cell Biol 22: 3389–3403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson JD 1972. Origin of concatemeric T7 DNA. Nat New Biol 239: 197–201 [DOI] [PubMed] [Google Scholar]
- Wei S, Sedivy JM 1999. Expression of catalytically active telomerase does not prevent premature senescence caused by overexpression of oncogenic Ha-Ras in normal human fibroblasts. Cancer Res 59: 1539–1543 [PubMed] [Google Scholar]
- Wei W, Hemmer RM, Sedivy JM 2001. Role of p14(ARF) in replicative and induced senescence of human fibroblasts. Mol Cell Biol 21: 6748–6757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods D, Parry D, Cherwinski H, Bosch E, Lees E, McMahon M 1997. Raf-induced proliferation or cell cycle arrest is determined by the level of Raf activity with arrest mediated by p21Cip1. Mol Cell Biol 17: 5598–5611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright WE, Shay JW 2002. Historical claims and current interpretations of replicative aging. Nat Biotechnol 20: 682–688 [DOI] [PubMed] [Google Scholar]
- Wright WE, Piatyszek MA, Rainey WE, Byrd W, Shay JW 1996. Telomerase activity in human germline and embryonic tissues and cells. Dev Genet 18: 173–179 [DOI] [PubMed] [Google Scholar]
- Wu C-H, van Riggelen J, Yetil A, Fan AC, Bachireddy P, Felsher DW 2007. Cellular senescence is an important mechanism of tumor regression upon c-Myc inactivation. Proc Natl Acad Sci 104: 13028–13033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xue W, Zender L, Miething C, Dickins RA, Hernando E, Krizhanovsky V, Cordon-Cardo C, Lowe SW 2007. Senescence and tumour clearance is triggered by p53 restoration in murine liver carcinomas. Nature 445: 656–660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamakoshi K, Takahashi A, Hirota F, Nakayama R, Ishimaru N, Kubo Y, Mann DJ, Ohmura M, Hirao A, Saya H, et al. 2009. Real-time in vivo imaging of p16Ink4a reveals cross talk with p53. J Cell Biol 186: 393–407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang N-C, Hu M-L 2005. The limitations and validities of senescence associated-β-galactosidase activity as an aging marker for human foreskin fibroblast Hs68 cells. Exp Gerontol 40: 813–819 [DOI] [PubMed] [Google Scholar]
- Yang G, Rosen DG, Zhang Z, Bast RC, Mills GB, Colacino JA, Mercado-Uribe I, Liu J 2006. The chemokine growth-regulated oncogene 1 (Gro-1) links RAS signaling to the senescence of stromal fibroblasts and ovarian tumorigenesis. Proc Natl Acad Sci 103: 16472–16477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye X, Zerlanko B, Kennedy A, Banumathy G, Zhang R, Adams PD 2007. Downregulation of Wnt signaling is a trigger for formation of facultative heterochromatin and onset of cell senescence in primary human cells. Mol Cell 27: 183–196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young NP, Jacks T 2010. Tissue-specific p19Arf regulation dictates the response to oncogenic K-ras. Proc Natl Acad Sci 107: 10184–10189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young AP, Schlisio S, Minamishima YA, Zhang Q, Li L, Grisanzio C, Signoretti S, Kaelin WG 2008. VHL loss actuates a HIF-independent senescence programme mediated by Rb and p400. Nat Cell Biol 10: 361–369 [DOI] [PubMed] [Google Scholar]
- Young ARJ, Narita M, Ferreira M, Kirschner K, Sadaie M, Darot JFJ, Tavaré S, Arakawa S, Shimizu S, Watt FM, et al. 2009. Autophagy mediates the mitotic senescence transition. Genes Dev 23: 798–803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan H, Kaneko T, Matsuo M 1995. Relevance of oxidative stress to the limited replicative capacity of cultured human diploid cells: The limit of cumulative population doublings increases under low concentrations of oxygen and decreases in response to aminotriazole. Mech Ageing Dev 81: 159–168 [DOI] [PubMed] [Google Scholar]
- Zhang R, Poustovoitov MV, Ye X, Santos HA, Chen W, Daganzo SM, Erzberger JP, Serebriiskii IG, Canutescu AA, Dunbrack RL, et al. 2005. Formation of MacroH2A-containing senescence-associated heterochromatin foci and senescence driven by ASF1a and HIRA. Dev Cell 8: 19–30 [DOI] [PubMed] [Google Scholar]
- Zhang W, Chan HM, Gao Y, Poon R, Wu Z 2007. BS69 is involved in cellular senescence through the p53-p21Cip1 pathway. EMBO Rep 8: 952–958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu J, Woods D, McMahon M, Bishop JM 1998. Senescence of human fibroblasts induced by oncogenic Raf. Genes Dev 12: 2997–3007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zindy F, Williams RT, Baudino TA, Rehg JE, Skapek SX, Cleveland JL, Roussel MF, Sherr CJ 2003. Arf tumor suppressor promoter monitors latent oncogenic signals in vivo. Proc Natl Acad Sci 100: 15930–15935 [DOI] [PMC free article] [PubMed] [Google Scholar]