Abstract
Background
Readmissions in patients with chronic obstructive pulmonary disease (COPD) are common and costly. We examined the effect of early follow-up visit with patient’s primary care physician (PCP) or pulmonologist following acute hospitalization on the 30-day risk of an emergency department (ER) visit and readmission.
Methods
We conducted a retrospective cohort study of fee-for-service Medicare beneficiaries with an identifiable PCP who were hospitalized for COPD between 1996 and 2006. Three or more visits to a PCP in the year prior to the hospitalization established a PCP for a patient. We performed a Cox proportional hazard regression with time-dependent covariates to determine the risk of 30-day ER visit and readmission in patients with or without a follow-up visit to their PCP or pulmonologist.
Results
Of the 62 746 patients admitted for COPD, 66.9% had a follow-up visit with their PCP or pulmonologist within 30 days of discharge. Factors associated with lower likelihood of outpatient follow-up visit were longer length of hospital stay, prior hospitalization for COPD, older age, black race, lower socioeconomic status, and emergency admission. Those receiving care at nonteaching, for-profit, and smaller-sized hospitals were more likely to have a follow-up visit. In a multivariate, time-dependent analysis, patients who had a follow-up visit had a significantly reduced risk of an ER visit (hazard ratio [HR], 0.86; 95% confidence interval [CI], 0.83–0.90) and readmission (HR, 0.91; 95% CI, 0.87–0.96).
Conclusion
Continuity with patient’s PCP or pulmonologist after an acute hospitalization may lower rates of ER visits and readmission in patients with COPD.
Chronic obstructive Pulmonary disease (COPD) is the fourth leading cause of death in the United States and the only disease associated with both increasing morbidity and mortality over the past 30 years.1 Research has consistently shown that patients with COPD have exceedingly high rates of hospitalization and emergency department (ER) visits. In 2000, COPD resulted in 726 000 hospitalizations and 1.5 million ER visits in the United States.2 One in 5 patients discharged with COPD is rehospitalized within 30 days of discharge.3,4 A recent study of over 11 million Medicare beneficiaries found COPD to be the third most common cause of 30-day rehospitalization.4
In 2005, potentially preventable hospital readmissions cost Medicare $12 billion.5 This burden underscores the importance of developing strategies to reduce these early readmissions for persons with chronic conditions. Age, disease severity, functional limitation, lack of social support, length of stay, and prior hospitalization are well-known risk factors for rehospitalization.6–12 Geographic variation in readmission rates suggests that some readmissions are potentially preventable.4,13 Coordinated discharge planning and hospital at-home and self-management education have been shown to reduce both exacerbations and hospitalization among patients with chronic diseases.14–17
Despite the consistently high rates of rehospitalization among patients with COPD, limited information is available on whether follow-up care with a patient’s primary care physician (PCP) or pulmonologist after hospitalization for COPD reduces early rehospitalization (ie, within 30 days). In this study of patients hospitalized for COPD in an acute care setting, we assessed whether follow-up care within 30 days of discharge with the patient’s PCP or pulmonologist that they had seen prior to hospitalization was associated with a reduced rate of 30-day ER visits and rehospitalization. We also examined patient and hospital characteristics associated with early outpatient follow-up.
METHODS
SOURCE OF DATA
We conducted a population-based cohort study using enrollment and claims data for a 5% national sample of Medicare beneficiaries from 1995 to 2006.18 Data were obtained from annual Medicare files of patients’ demographic and enrollment characteristics (Denominator File), hospital stays (Medicare Provider and Analysis Review File [MEDPAR]), outpatient facility services (Outpatient Standard Analytical File), and physician services (Carrier Standard Analytical File).19 Hospital characteristics were obtained from the Centers for Medicare and Medicaid Services (CMS) Provider of Services (POS) File.20
DESCRIPTION OF COHORT
Our study cohort consisted of 164 041 Medicare beneficiaries 66 years or older hospitalized for COPD (Diagnosis Related Group [DRG] code 088) at least once during the period 1996 to 2006. Patients with stays longer than 18 days (n= 1777 admissions) were considered outliers (exceeding the 99th percentile) and were excluded. Also excluded were 67 992 admissions for patients with no identifiable PCP in the year prior to hospitalization and 15 559 admissions resulting in a discharge destination other than home. For patients with more than 1 admission in a given year, we randomly selected 1 admission per patient per year and excluded discharges in December 2006 (in order to have a 30-day follow-up period), resulting in 62 746 admissions for study analysis. Of these admissions based on COPD-DRG, 87.6% had a COPD-related International Classification of Diseases, Ninth Revision (ICD-9) code (491.xx, 492.xx, and 496) listed as the primary diagnosis. Asthma (ICD-9 code 493.xx) was listed as the primary diagnosis in an additional 11.2% of these admissions.
PATIENT-LEVEL CHARACTERISTICS
Medicare enrollment files were used to categorize patients by age (66–74 years, 75–84 years, and ≥85 years), sex (male or female), and race/ethnicity (non-Hispanic white, black, or other). A Medicaid indicator (state buy-in) in the enrollment file was used as a proxy for low socioeconomic status (SES). Information regarding the origin of the admission (via the ER vs other), day of admission (weekend vs other), and discharge DRG were obtained from the MEDPAR files. A patient’s place of residence was categorized by size of metropolitan area in quartiles. A comorbidity score was generated using the Elixhauser comorbidity score, using inpatient and outpatient billing data.21 Any prior claim for hospitalization with a DRG for COPD was considered a prior admission. Length of stay was categorized as 1 to 2 days, 3 to 4 days, 5 to 7 days, and more than 7 days. A patient was considered to have used intensive care unit (ICU) services if there was a claim for any ICU stay of more than 1 day.
HOSPITAL-LEVEL CHARACTERISTICS
Hospital characteristics, including total number of beds, type of hospital, medical school affiliation, and location, were obtained from data in the POS files. The total number of beds was categorized as less than 200, 200 to 349, 350 to 499, and 500 or more; the location was grouped by CMS region; the hospital type was categorized as nonprofit, for-profit, or public; and medical school affiliation was categorized as none, minor, or major.
DEFINITION OF PCP
A patient was defined as having a PCP if he or she had 3 or more visits to a PCP in a year prior to the hospitalization. There is no well-established algorithm to identify a patient’s PCP using administrative data. Having 3 or more visits to the same PCP in a year had a 76.3% concordance to the patient’s self-identified PCP.22 The Health Care Financial Administration (HCFA) Common Procedure Terminology (CPT) evaluation and management codes 99201 to 99205 (new patient encounter) and codes 99221 to 99215 (established patient encounter) were used to identify visits to the patient’s PCP. For purposes of this study, a PCP was defined as a general practitioner, family physician, internist, or geriatrician. Physician specialty was determined from hospital claims in the MEDPAR file.
ESTABLISHMENT OF THE FOLLOW-UP VISIT
An outpatient visit to the patient’s PCP or pulmonary physician (who saw the patient in the year prior to the hospitalization) within 30 days of the discharge date established follow-up care for that admission. We included pulmonary physicians in follow-up visits because 25.9% of our study patients were cotreated with a pulmonary physician (ie, had ≥1 outpatient visit to a pulmonary physician in the year prior to the hospitalization). Outpatient physician visits were captured using HCFA CPT evaluation and management codes 99221 to 99215 (established patient encounter).
OUTCOME
The primary outcomes were (1) an ER visit and (2) a rehospitalization within 30 days of the discharge date. For patients with more than 1 ER visit or rehospitalization within 30 days, only the first event for each outcome was counted. We chose a 30-day window because most preventable readmissions occur within 1 month of discharge, and Medicare uses this time interval to compare readmission rates for hospitals across the United States.
STATISTICAL ANALYSES
We compared the patient and hospital characteristics between those with and without a follow-up visit to their PCP or pulmonologist within 30 days of discharge. The cumulative percentage of follow-up visits with their PCP or pulmonologist were estimated using the Kaplan-Meier method. In this analysis, patients were censored at death or 30 days after discharge. We repeated the analysis by also censoring patients who had an ER visit or readmission prior to the follow-up visit. The Cox proportional hazard model was used to identify factors associated with a follow-up visit within 30 days. To avoid time-dependent bias, a follow-up visit was treated as a time-dependent covariate to allow it to change over time during the 30-day period. Patients were assigned to the group “without follow-up visit” until they had their first follow-up visit to their PCP or pulmonologist after discharge. The outcomes of ER visit and rehospitalization for patients with and without a follow-up visit were estimated by multistate Nelson-Aalen estimation,23–25 a nonparametric method of calculating the cumulative hazard for time-varying covariates. We used a Cox proportional hazards technique with time-dependent covariates to model the effect of follow-up visits on 30-day outcomes.26 In these Cox proportional hazard models, the multivariate-adjusted hazard ratios (HRs) with corresponding 95% confidence intervals were estimated using admissions with no follow-up with their PCP or pulmonologist as a reference group. The covariates in the models were age, sex, race/ethnicity, SES, region, comorbidity, admission day (weekend or not), year of admission, history of prior COPD hospitalization, length of stay, source of admission, hospital teaching status, metropolitan size, type of hospital, and size of hospital. Efron approximation27 in the partial likelihood function was used to handle ties for events occurring on the same day in several patients within the 30-day follow-up period. To adjust for the clustering effect at the hospital level, robust sandwich estimation was used.24 We reanalyzed the 30-day outcomes (excluding death) and focused on any emergent or urgent readmission within 30 days or any readmission related to pulmonary conditions (COPD, pneumonia, pneumothorax, lower respiratory tract infection, and pulmonary embolism). The proportional hazard assumption was examined by plotting the log of cumulative hazard rates against time for patients with and without follow-up visits. The log of cumulative hazard rates was proportional to the follow-up time, and there were no violations to the proportional hazard assumption. All reported P values were 2-sided, and P< .05 was considered statistically significant. All analyses were performed with SAS statistical software (version 9.1; SAS Inc, Cary, North Carolina).
RESULTS
A total of 62 746 hospitalizations for COPD exacerbation occurred between 1996 and 2006 for patients who had a PCP prior to hospitalization. Of these patients, 74.1% were exclusively treated by their PCP and 25.9% were cotreated with a pulmonary physician in the year prior to the hospitalization.
Table 1 presents the patient and hospital characteristics of patients who did and did not have a follow-up visit with their PCP or pulmonologist and an adjusted HR of seeing either physician. Between 1996 and 2006, 66.9% of patients with COPD had an outpatient visit with their PCP or pulmonologist within 30 days of discharge. The percentage of patients with COPD with a postdischarge follow-up with their PCP or pulmonologist increased from 65.2% in 1996 to 71.0% in 2006 (P< .001). Among patients who had a follow-up visit, 86.7% were with their PCP, 6.7% with their pulmonary physician, and 6.6% with both.
Table 1.
Comparison of Patient- and Hospital-Level Characteristic of Patients With and Without a Follow-up Visit With Their Primary Care Physician (PCP) or Pulmonologist Following Hospitalization for COPD
| No. (%) |
||||
|---|---|---|---|---|
| 30-d Follow-up With PCP or Pulmonologista |
||||
| Characteristic | All Patients | Yes | No | Adjusted HR (95% CI)b |
| Total | 62746 | 42002 (66.9) | 20744 (33.4) | |
| Year of admission | ||||
| 1996 | 5499 (8.8) | 3532 (8.4) | 1967 (9.5) | |
| 1997 | 5350 (8.5) | 3518 (8.4) | 1832 (8.8) | |
| 1998 | 5430 (8.7) | 3570 (8.5) | 1860 (9.0) | |
| 1999 | 5894 (9.4) | 3863 (9.2) | 2031 (9.8) | |
| 2000 | 5592 (8.9) | 3710 (8.8) | 1882 (9.1) | |
| 2001 | 5401 (8.6) | 3638 (8.7) | 1763 (8.5) | 1 02 (1.01–1.02) |
| 2002 | 5869 (9.4) | 3824 (9.1) | 2045 (9.9) | |
| 2003 | 6248 (10.0) | 4261 (10.1) | 1987 (9.6) | |
| 2004 | 5894 (9.4) | 4016 (9.6) | 1876 (9.0) | |
| 2005 | 5372 (10.2) | 4423 (10.5) | 1949 (9.4) | |
| 2006 | 5197 (8.3) | 3645 (8.7) | 1552 (7.5) | |
| Length of stay, d | ||||
| 1–2 | 13192 (21.0) | 8808 (21.0) | 4384 (21.1) | 1 [Reference] |
| 3–4 | 22875 (36.5) | 15458 (36.8) | 7417 (35.8) | 1.02 (0.99–1.04) |
| 5–7 | 18115 (28.9) | 12309 (29.3) | 5806 (28.0) | 1.03 (1.01–1.06) |
| >7 | 8564 (13.6) | 5427 (12.9) | 3137 (15.1) | 0.95 (0.91–0.98) |
| Prior COPD admission | ||||
| No | 34750 (55.4) | 23474 (55.9) | 11276 (54.4) | 1 [Reference] |
| Yes | 27996 (44.6) | 18528 (44.1) | 9468 (45.6) | 0.95 (0.93–0.96) |
| Age at admission, y | ||||
| 66–74 | 27677 (44.1) | 18799 (44.8) | 8878 (42.8) | 1 [Reference] |
| 75–84 | 27538 (43.9) | 18440 (43.9) | 9098 (43.9) | 0.97 (0.95–0.99) |
| >85 | 7531 (12.0) | 4763 (11.3) | 2768 (13.3) | 0.88 (0.85–0.91) |
| Sex | ||||
| Male | 25978 (41.4) | 17440 (41.5) | 8538 (41.2) | 1 [Reference] |
| Female | 36768 (58.6) | 24562 (58.5) | 12206 (58.8) | 0.98 (0.96–1.00) |
| Race/ethnicity | ||||
| White | 55914 (89.1) | 37713 (89.8) | 18201 (87.7) | 1 [Reference] |
| Black | 4287 (6.8) | 2675 (6.4) | 1612 (7.8) | 0.92 (6.89–0.96) |
| Other | 2545 (4.1) | 1614 (3.8) | 931 (4.5) | 0.97 (0.91–1.03) |
| Low SES | ||||
| No | 45416 (72.4) | 30913 (73.6) | 14503 (69.9) | 1 [Reference] |
| Yes | 17330 (27.6) | 11089 (26.4) | 6241 (30.1) | 0.90 (0.88–0.92) |
| Emergency admission | ||||
| No | 24818 (39.6) | 17222 (41.0) | 7596 (36.6) | 1 [Reference] |
| yes | 37928 (60.4) | 24780 (59.0) | 13148 (63.4) | 0.90 (0.89–0.92) |
| Elixhauser comorbidity score | ||||
| 0 | 8908 (14.2) | 6027 (14.3) | 2881 (13.9) | 1 [Reference] |
| 1 | 14295 (22.8) | 9926 (23.6) | 4369 (21.1) | 1.04 (1.01–1.08) |
| 2 | 13166 (21.0) | 8968 (21.4) | 4198 (20.2) | 1.02 (0.98–1.05) |
| ≥3 | 26377 (42.0) | 17081 (40.7) | 9296 (44.8) | 0.94 (0.91–0.97) |
| Weekend admission | ||||
| No | 47221 (75.3) | 31643 (75.3) | 15578 (75.1) | 1 [Reference] |
| Yes | 15525 (24.7) | 10359 (24.7) | 5166 (24.9) | 1.00 (0.98–1.02) |
| Geographic region of the United Statesc | ||||
| New England | 2336 (3.7) | 1556 (3.7) | 780 (3.8) | 0.88 (0.81–0.94) |
| Middle Atlantic | 8761 (14.0) | 5858 (13.9) | 2903 (14.0) | 0.90 (0.85–0.95) |
| East North Central | 11510 (18.3) | 7827 (18.6) | 3683 (17.8) | 0.93 (0.88–0.98) |
| West North Central | 4320 (6.9) | 2975 (7.1) | 1345 (6.5) | 0.91 (0.86–0.97) |
| South Atlantic | 14105 (22.5) | 9427 (22.4) | 4678 (22.6) | 0.89 (0.84–0.93) |
| East South Central | 6891 (11.0) | 4564 (10.9) | 2327 (11.2) | 0.86 (0.81–0.91) |
| West South Central | 7135 (11.4) | 4683 (11.1) | 2452 (11.8) | 0.84 (0.80–0.89) |
| Mountain | 2284 (3.6) | 1519 (3.6) | 765 (3.7) | 0.91 (0.84–0.98) |
| Pacific | 4030 (6.4) | 2789 (6.6) | 1241 (6.0) | 1 [Reference] |
| Size of metropolitan area, populationd | ||||
| ≥1000000 | 27092 (43.3) | 17893 (42.7) | 9199 (44.5) | 1 [Reference] |
| 250000–999999 | 14936 (23.9) | 10121 (24.2) | 4815 (23.3) | 1.02 (0.99–1.05) |
| 100000–249999 | 1500 (2.4) | 994 (2.4) | 506 (2.4) | 0.99 (0.91–1.07) |
| <10000 | 19065 (30.5) | 12891 (30.8) | 6174 (29.8) | 1.01 (0.97–1.04) |
| Medical school affiliationd | ||||
| Major | 9050 (14.5) | 5847 (14.0) | 3203 (15.5) | 1 [Reference] |
| Minor | 12733 (20.3) | 8436 (20.1) | 4297 (20.8) | 1.00 (0.96–1.05) |
| None | 40810 (65.2) | 27616 (65.9) | 13194 (63.8) | 1.03 (1.00–1.08) |
| Type of hospitald | ||||
| Nonprofit | 43919 (70.2) | 29446 (70.3) | 14473 (69.9) | 1 [Reference] |
| For profit | 8610 (13.8) | 5773 (13.8) | 2837 (13.7) | 1.04 (1.00–1.08) |
| Public | 10064 (16.1) | 6680 (15.9) | 3384 (16.4) | 1.00 (0.97–1.04) |
| Hospital size, No. of bedsd | ||||
| 200 | 26593 (42.5) | 17976 (42.9) | 8617 (41.6) | 1 [Reference] |
| 200–349 | 17048 (27.2) | 11493 (27.4) | 5555 (26.8) | 0.97 (0.94–1.00) |
| 350–499 | 9191 (14.7) | 6095 (14.5) | 3096 (15.0) | 0.95 (0.91–0.98) |
| ≥500 | 9761 (15.6) | 6335 (15.1) | 3426 (16.6) | 0.92 (0.89–0.96) |
| ICU use | ||||
| No | 54798 (87.3) | 36751 (87.5) | 18047 (87.0) | 1 [Reference] |
| Yes | 7948 (12.7) | 5251 (12.5) | 2697 (13.0) | 0.98 (0.95–1.01) |
Abbreviations: CI, confidence interval; COPD, chronic obstructive pulmonary disease; HR, hazard ratio; ICU, intensive care unit; SES, socioeconomic status.
Table compares baseline characteristics of all patients with a PCP (defined as ≥3 visits to the same PCP in a year prior to the hospitalization) who did or did not have a follow-up visit with their PCP or pulmonologist (who had cotreated the patient with PCP) within 30 days of discharge.
Adjusted HR indicates the factors associated with the likelihood of having a follow-up visit with their PCP or pulmonologist after discharge. Patients were censored at death or 30 days after discharge.
Puerto Rico and Guam are not shown in the geographic region (n=1221).
Data missing(n=153).
Patients who did not have a follow-up visit with their PCP or pulmonologist were more likely to have a longer length of hospital stay, be older (>85 years), be black, have a low SES, have multiple comorbidities, and be admitted through the ER compared with those who had a follow-up visit within 30 days of discharge. Patients who lived in a large metropolitan area, received care at a major teaching hospital, or received care at a large hospital were also less likely to have a postdischarge follow-up visit. There were no differences between the groups in prior admissions for COPD, geographic region, admission day of the week, or type of hospital.
Also shown in Table 1 are the multivariate analyses of patient- and hospital-level characteristics on the likelihood of an outpatient follow-up with their PCP or pulmonologist. The odds of a follow-up visit within 30 days of discharge increased 2% (95% CI, 1%–2%) per year from 1996 to 2006. Factors associated with a lower likelihood of outpatient follow-up were longer hospital stay, prior COPD hospitalization, older age, black race, lower SES, and emergency admission. Those receiving care at nonteaching, for-profit, and smaller sized hospitals were more likely to have a follow-up visit within 30 days of discharge. Censoring patients who had an ER visit or readmission prior to a follow-up visit with their PCP or pulmonologist did not change the adjusted HR for most of the variables listed in Table 1, except for low SES (HR, 0.92; 95% CI, 0.89–0.94) and 3 or more comorbidities (HR, 1.00; 95% CI, 0.97–1.03).
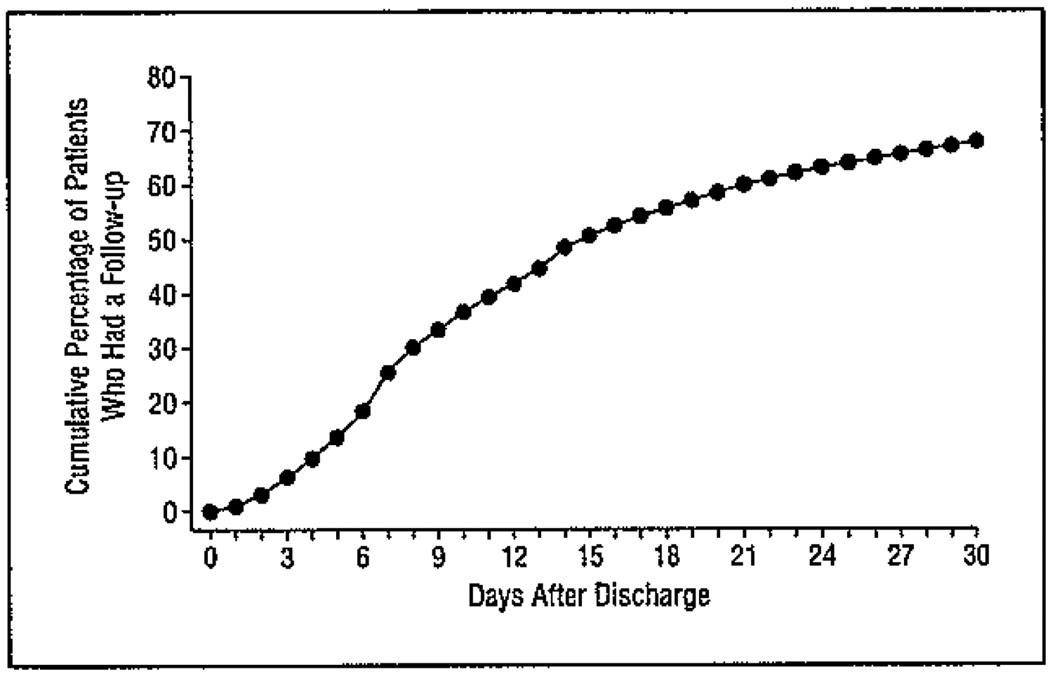
The Figure shows the lag time from the date of discharge to the patient’s first follow-up visit with his or her PCP or pulmonologist. Of those seen, 75.2% were seen within 15 days of discharge.
Figure.
Cumulative percentage of patients who had a follow-up visit with their primary care physician or pulmonologist from the day of discharge from a hospitalization for chronic obstructive pulmonary disease. Patients were censored at death (n=1419).
Patients who had a follow-up visit with their PCP or pulmonologist after discharge had fewer ER visits and lower readmission rates. The 30-day rates of postdischarge ER visits in patients with follow-up to their PCP or pulmonologist was 21.7% compared with 26.3% in those with no postdischarge follow-up (P < .001). Similarly, 30-day readmission rates were 18.9% and 21.4% for patients with and without a follow-up visit with their PCP or pulmonologist, respectively (P< .001). Of the 11 558 readmissions within 30 days, the top 3 reasons for readmission were COPD (24.1%), pneumonia or respiratory infection (12.9%), and heart failure (7.8%).
In a time-dependent analysis, controlling for patient-and hospital-level characteristics and excluding patients (n=1817) who died within 30 days of discharge, patients seen by their PCP or pulmonologist had lower 30-day adjusted rates of ER visits (HR, 0.86; 95% CI, 0.83–0.90] and readmission (HR, 0.91; 95% CI, 0.87–0.96) compared with those not seen by their PCP or pulmonologist (Table 2). The magnitude of the results did not change when we included patients who died within 30 days of discharge or restricted outcomes to hospitalization for pulmonary conditions or urgent or emergent admissions. Factors associated with increased 30-day risk of an ER visit or readmissions were length of initial hospitalization (>7 days), comorbidities, prior hospitalization for COPD, male sex, low SES, ICU stay, admission from the ER, and weekend hospital admission.
Table 2.
Hazard of ER Visit and Hospital Readmission 30 Days After Discharge in Patients With and Without a Follow-up Visit With Their PCP or a Pulmonologist
| HR (95% CI) |
|||
|---|---|---|---|
| Outcomes | Rate, % | Unadjusted | Adjusteda |
| 30-d ER visit; patients had follow-up with their PCP or pulmonologist |
|||
| Yes | 21.7 | 0.83 (0.79–0.86) | 0.86 (0.83–0.90) |
| No | 26.3 | 1 [Reference] | 1 [Reference] |
| 30-d readmission; patients had follow-up with their PCP or pulmonologist |
|||
| Yes | 18.9 | 0.88 (0.84–0.92) | 0.91 (0.87–0.96) |
| No | 21.4 | 1 [Reference] | 1 [Reference] |
Abbreviations: CI, confidence interval; ER, emergency department; HR, hazard ratio; PCP, primary care physician.
The HRs indicate the association of follow-up visit with patient's PCP or pulmonologist within 30 days of discharge with the risk of ER visit or readmission after adjusting for all the variables listed in Table 1. Deaths (n=1817) within 30 days of discharge were excluded from the analysis.
COMMENT
We found that patients with COPD who had an early follow-up with their PCP or pulmonologist after acute hospitalization had lower odds of a 30-day ER visit or hospital readmission compared with patients who had no such follow-up. In patients with COPD, a follow-up visit within 30 days of initial hospitalization was associated with 14% fewer ER visits and 9% fewer readmissions 30 days after discharge. Continuity of care with a PCP or a pulmonologist after an acute hospitalization is a potentially modifiable factor that may lower the risk of clinical relapse requiring an ER visit or readmission in patients with COPD.
Rehospitalizations among Medicare beneficiaries are common and costly.4 In 2004, 19.6% of older adults were rehospitalized within 30 days of discharge at an estimated cost of $17.4 billion. Congestive heart failure, psychosis, and COPD are the chronic conditions with the highest 30-day readmission rates (26.9%, 24.6%, and 22.6%, respectively). Our findings of COPD, pneumonia, and congestive heart failure as the most frequent cause for readmission in patients hospitalized for COPD are similar to those in a recent study by Jencks et al.4
We used the follow-up visit as a time-dependent covariate in our analyses. A prior study using follow-up visit as a fixed variable showed a large effect of follow-up visit on reducing repeated ER visits within 90 days of an initial ER visit.28 The bias in these analyses results from the fact that patients who are readmitted earlier will not have a chance to see their physicians and hence are included in the “no follow-up” group; this makes the “no follow-up” group seem worse and thus overestimates the benefit of a follow-up visit. For example, when we analyzed the effect of a 30-day follow-up visit as a fixed variable, we found a large reduction in 30-day risk of readmission (HR, 0.48; 95% CI, 0.47–0.50) compared with when the follow-up visit was analyzed as a time-dependent variable (HR, 0.91; 95% CI, 0.87–0.96). Time-dependent bias can artificially inflate effects and is common in articles published in medical journals.29
Patients who were black and those with low SES had higher rates of rehospitalization and were less likely to follow up with their PCP or pulmonologist. These findings are consistent with those of previous studies that found substantially lower use of screening and preventive care among these subgroups. Efforts to improve early follow-up are necessary, especially in these vulnerable populations. It will be particularly important to examine the specific socioeconomic barriers and behavioral factors that underlie the reduced access to outpatient care in these patient subgroups. Similarly, older adults and those with multiple comorbidities were less likely to have an outpatient follow-up visit.
Patients receiving care at teaching hospitals were less likely to follow up with their PCP or pulmonologist than those treated at community hospitals. Patients are more likely to see their outpatient health care provider during hospitalization in community settings,30 and this continuity across transition may also increase the likelihood that they will follow up with their PCP after discharge.
Chronic obstructive pulmonary disease is designated an ambulatory care sensitivity condition (ACSC) by the Agency for Healthcare Research and Quality, among others; ACSCs are medical conditions for which timely access to outpatient care can obviate the need for hospitalization. However, a randomized controlled trial of improving access to primary care after discharge in male veterans hospitalized for COPD, congestive heart failure, or diabetes mellitus-related complications found increased rehospitalization rates in patients with increased access to care over 6 months after discharge.31 This study included only veterans who did not have a PCP, and the negative findings may be explained by the fact that assigning chronically ill patients to a PCP with no prior relationship may not translate into immediate reduction in hospitalizations.
Readmission rates can be lowered by postdischarge follow-up.32,33 Patients who follow up with their outpatient physicians after hospitalization may have fewer ER visits and readmissions for various reasons. Most patients are discharged with their symptoms improving but not completely resolved. Early follow-up with their PCP or pulmonologist can help intervene by adjusting medications to potentially avoid an ER visit or hospitalization. In patients with advanced disease, early referral to a pulmonary specialist, or cotreatment34 can raise the quality of care and improve survival.
Our study has several limitations. We examined only follow-up visits with the patient’s own PCP or pulmonologist. Some patients may have had follow-up visits with other physicians or mid-level health care providers after discharge. This would have led to an underestimation of postdischarge follow-up. However, this change would affect the magnitude but not the direction of the association between follow-up and 30-day ER visits or readmission. We did not have information on the quality of care during the index hospitalization. Substandard care during hospitalization is associated with early relapse and readmission.35 In addition, information on outpatient treatment of COPD prior to the hospitalization and COPD-specific disease severity measures are not available in the administrative data set. Patients with more severe disease are likely to have recurrent exacerbations and frequent hospitalization. As a surrogate for severity of COPD, we controlled for prior COPD hospitalization in our analyses. Physician practice patterns can influence the decision to admit a patient independent of a patient’s clinical status and were not examined in the present study.36 Our study did not examine care coordination, such as early discharge to pulmonary rehabilitation, home-hospital (in which the patient is treated by his or her PCP or other health care provider at home; this type of care is common in Europe), home visits from a respiratory therapist, or nurse or self-management education, all beneficial in reducing COPD exacerbations.16,37,38 This may have lowered our estimate of the true benefits of follow-up care. We included 1 admission per patient per year in our analyses. Theoretically, a patient can have a maximum of 11 admissions (once per year during the entire study period), which can result in clustering at the patient level. We did not adjust for clustering at the patient level, and this may have resulted in a small bias in our estimates. Our results may not be applicable to non-Medicare patients or those enrolled in managed care. Finally, given the observational design of the study, we cannot exclude unmeasured or residual confounding as a possible explanation for the observed associations.
In summary, an early follow-up visit with a patient’s PCP or pulmonologist is associated with decreased likelihood of an ER visit and hospital readmission within 30 days of discharge in patients hospitalized for COPD. Discharge planning that emphasizes early outpatient follow-up may reduce hospital readmissions in patients with COPD.
Acknowledgments
Funding/Support: This study was supported by grants K05 CA 134923, K08 AG 031583, R01 AG 033134, and P30 AG 024832 from the National Institutes of Health.
Additional Contributions: Sarah Toombs Smith, PhD, provided help in preparation of the manuscript.
Footnotes
Author Contributions: Study concept and design: Sharma, Kuo, Freeman, and Goodwin. Acquisition of data: Zhang and Goodwin. Analysis and interpretation of data: Sharma and Kuo. Drafting of the manuscript: Sharma, Kuo, Freeman, and Zhang. Critical revision of the manuscript for important intellectual content: Sharma, Kuo, Freeman, and Goodwin. Statistical analysis: Kuo and Zhang. Obtained funding: Sharma and Goodwin, Study supervision: Goodwin.
Financial Disclosure: None reported.
REFERENCES
- 1.Centers for Disease Control and Prevention (CDC) Deaths from chronic obstructive pulmonary disease--United States, 2000–2005. MMWR Morb Mortal Wkly Rep. 2008;57(45):1229–1232. [PubMed] [Google Scholar]
- 2.Centers for Disease Control. [Accessed March 1, 2009];Chronic Obstructive Pulmonary Disease (COPD) http://www.edc.gov/copd/copdfaq.htm.
- 3.Camberg LC, Smith NE, Beaudet M, Daley J, Cagan M, Thibault G. Discharge destination and repeat hospitalizations. Med Care. 1997;35(8):756–767. doi: 10.1097/00005650-199708000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 5.Payment policy for inpatient readmissions: report to the Congress, promoting greater efficiency in Medicare. [Accessed November 1, 2009];2007 June; http://www.medpac.gov/documents/jun07_EntireReport.pdf.
- 6.Holloway JJ, Medendorp SV, Bromberg J. Risk factors for early readmission among veterans. Health Serv Res. 1990;25(1, pt 2):213–237. [PMC free article] [PubMed] [Google Scholar]
- 7.Reed RL, Pearlman RA, Buchner DM. Risk factors for early unplanned hospital readmission in the elderly. J Gen Intern Med. 1991;6(3):223–228. doi: 10.1007/BF02598964. [DOI] [PubMed] [Google Scholar]
- 8.Weissman JS, Stern RS, Epstein AM. The impact of patient socioeconomic status and other social factors on readmission: a prospective study in four Massachusetts hospitals. Inquiry. 1994;31(2):163–172. [PubMed] [Google Scholar]
- 9.Krumholz HM, Parent EM, Tu N, et al. Readmission after hospitalization for congestive heart failure among Medicare beneficiaries. Arch Intern Med. 1997;157(1):99–104. [PubMed] [Google Scholar]
- 10.Chin MH, Goldman L. Factors contributing to the hospitalization of patients with congestive heart failure. Am J Public Health. 1997;87(4):643–648. doi: 10.2105/ajph.87.4.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sin DD, Tu JV. Are elderly patients wish obstructive airway disease being prematurely discharged? Am J Respir Crit Care Med. 2000;161(5):1513–1517. doi: 10.1164/ajrccm.161.5.9907031. [DOI] [PubMed] [Google Scholar]
- 12.Friedman B, Jiang HJ, Elixhauser A. Costly hospital readmissions and complex chronic illness. Inquiry. 2008–2009;45(4):408–421. doi: 10.5034/inquiryjrnl_45.04.408. [DOI] [PubMed] [Google Scholar]
- 13.Fisher ES, Wennberg JE, Stukel TA, Sharp SM. Hospital readmission rates for cohorts of Medicare beneficiaries in Boston and New Haven. N Engl J Med. 1994;331(15):989–995. doi: 10.1056/NEJM199410133311506. [DOI] [PubMed] [Google Scholar]
- 14.Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004;52(5):675–684. doi: 10.1111/j.1532-5415.2004.52202.x. [DOI] [PubMed] [Google Scholar]
- 15.Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 16.Effing T, Monninkhof EM, van der Valk PD, et al. Self-management education for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2007;(4) doi: 10.1002/14651858.CD002990.pub2. CD002990. [DOI] [PubMed] [Google Scholar]
- 17.Peikes D, Chen A, Schore J, Brown R. Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries: 15 randomized trials. JAMA. 2009;301(6):603–618. doi: 10.1001/jama.2009.126. [DOI] [PubMed] [Google Scholar]
- 18.Research Data Assistance Center. [Accessed March 1, 2009];Differences in how the Medicare 5% Files are generated. http://www.resdac.umn.edu/Tools/TBs/TN-011_How5percentMedicarefilescreated_508.pdf.
- 19.Centers for Medicare and Medicaid Services. [March 1, 2009];Identifiable data files: standard analytical files. http://www.cms.gov/IdentifiableDataFiles/02_StandardAnalyticalFiles.asp#TopOfPage.
- 20.Centers for Medicare and Medicaid Services. [Accessed March 1, 2009];Nonidentifiable data files: provider of service files. http://www.cms.gov/NonIdentifiableDataFiles/04_ProviderofServicesFile.asp#TopOfPage. [Google Scholar]
- 21.Weinhandl ED, Snyder JJ, Israni AK, Kasiske BL. Effect of comorbidity adjustment on CMS criteria for kidney transplant center performance. Am J Transplant. 2009;9(3):506–516. doi: 10.1111/j.1600-6143.2008.02527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shah BR, Hux JE, Laupacis A, Zinman B, Cauch-Dudek K, Booth GL. Administrative data algorithms can describe ambulatory physician utilization. Health Serv Res. 2007;42(4):1783–1796. doi: 10.1111/j.1475-6773.2006.00681.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aalen O. Non-parametric inference for a family of counting processes. Ann Statist. 1978;6(4):701–726. [Google Scholar]
- 24.Anderson P, Borgan O, Gill R, Keiding N. Statistical Models Based on Counting Processes. New York, NY: Springer; 2003. chaps IV.1–IV.4. [Google Scholar]
- 25.Snapinn S, Jiang Q, Iglewicz B. Illustrating the impact a time-varying covariate with an extended Kaplan-Meier estimator. Am Stat. 2005;59:301–307. [Google Scholar]
- 26.van Walraven C, Mamdani M, Fang J, Austin PC. Continuity of care and patient outcomes after hospital discharge. J Gen Intern Med. 2004;19(6):624–631. doi: 10.1111/j.1525-1497.2004.30082.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hertz-Picciotto I, Rockhill B. Validity and efficiency of approximation methods for tied survival times in Cox regression. Biometrics. 1997;53(3):1151–1156. [PubMed] [Google Scholar]
- 28.Sin DD, Bell NR, Svenson LW, Man SF. The impact of follow-up physician visits on emergency readmissions for patients with asthma and chronic obstructive pulmonary disease: a population-based study. Am J Med. 2002;112(2):120–125. doi: 10.1016/s0002-9343(01)01079-8. [DOI] [PubMed] [Google Scholar]
- 29.van Walraven C, Davis D, Forster AJ, Wells GA. Time-dependent bias was common in survival analyses published in leading clinical journals. J Clin Epidemiol. 2004;57(7):672–682. doi: 10.1016/j.jclinepi.2003.12.008. [DOI] [PubMed] [Google Scholar]
- 30.Sharma G, Fletcher KE, Zhang D, Kuo YF, Freeman JL, Goodwin JS. Continuity of outpatient and inpatient care by primary care physicians for hospitalized older adults. JAMA. 2009;301(16):1671–1680. doi: 10.1001/jama.2009.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weinberger M, Oddone EZ, Henderson WG. Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. Does increased access to primary care reduce hospital readmissions? N Engl J Med. 1996;334(22):1441–1447. doi: 10.1056/NEJM199605303342206. [DOI] [PubMed] [Google Scholar]
- 32.Emerman CL, Cydulka RK. Factors associated with relapse after emergency department treatment for acute asthma. Ann Emerg Med. 1995;26(1):6–11. doi: 10.1016/s0196-0644(95)70230-x. [DOI] [PubMed] [Google Scholar]
- 33.Ettner SL. The relationship between continuity of care and the health behaviors of patients: does having a usual physician make a difference? Med Care. 1999;37(6):547–555. doi: 10.1097/00005650-199906000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Nie JX, Wang L, Upshur RE. Mortality of elderly patients in Ontario after hospital admission for chronic obstructive pulmonary disease. Can Respir J. 2007;14(8):485–489. doi: 10.1155/2007/425248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ashton CM, Kuykendall DH, Johnson ML, Wray NP, Wu L. The association between the quality of inpatient care and early readmission. Ann Intern Med. 1995;122(6):415–421. doi: 10.7326/0003-4819-122-6-199503150-00003. [DOI] [PubMed] [Google Scholar]
- 36.O’Malley AS, Pham HH, Schrag D, Wu B, Bach PB. Potentially avoidable hospitalizations for COPD and pneumonia: the role of physician and practice characteristics. Med Care. 2007;45(6):562–570. doi: 10.1097/MLR.0b013e3180408df8. [DOI] [PubMed] [Google Scholar]
- 37.Lawlor M, Kealy S, Agnew M, et al. Early discharge care with ongoing follow-up support may reduce hospital readmissions in COPD. Int J Chron Obstruct Pulmon Dis. 2009;4(1):55–60. [PMC free article] [PubMed] [Google Scholar]
- 38.Bourbeau J, Julien M, Maltais F, et al. Chronic Obstructive Pulmonary Disease axis of the Respiratory Network Fonds de la Recherche en Santé du Québec. Reduction of hospital utilization in patients with chronic obstructive pulmonary disease: a disease-specific self-management intervention. Arch Intern Med. 2003;163(5):585–591. doi: 10.1001/archinte.163.5.585. [DOI] [PubMed] [Google Scholar]