Abstract
Thoracic pedicle screws have superior anchoring strength compared with other available fixation techniques. However, these are not universally accepted in many developing countries because of the concerns regarding safety and complications. In addition, there is evidence that pedicle morphology is unique in Chinese patients. The goal of this study was to analyze the complications seen at our institution, while using thoracic pedicle screws for the treatment of thoracic deformity, and to determine the safety of our techniques for the treatment of thoracic deformity in a Chinese population. From 1998 to 2005, there were 208 thoracic deformity patients treated at our institution, 70 of whom were male and 138 were female. Their age ranged from 11 to 55 years (mean of 14.9 years). All of them underwent corrective deformity surgery using posterior pedicle screw systems and follow-up was available for at least 3 years. Etiologic diagnoses included adolescent idiopathic scoliosis in 119 patients, congenital kyphoscoliosis in 38, adult scoliosis in 37 and undetermined in 14. Screw positions were evaluated using intraoperative and postoperative radiographs and a CT scan was performed when a concern for screw malposition was present. All radiographic evaluations were carried out in a double-blinded fashion. A total of 1,123 thoracic pedicle screws were inserted (5.4 thoracic screws/patient). The deformity correction rate was 81, 65 and 62% for idiopathic, congenital and adult scoliosis patients, respectively. The overall complication rate was 16.5% at the final follow-up. Complication rates directly and indirectly related to pedicle screws were 7.2 and 9.3%, respectively. There were no significant screw-related neurologic or visceral complications that adversely affected long-term results. The complications seen with thoracic pedicle screws in a Chinese population were similar to other populations and could be utilized safely for the treatment of thoracic deformity in this population.
Keywords: Complication, Spinal deformity, Surgical treatment, Pedicle screw instrumentation
Introduction
The use of thoracic pedicle screws has gained popularity in many developing countries [1]. Thoracic pedicle screws provide stronger biomechanical anchoring strength compared to the use of hooks and wire fixation [2–7]. At our institution, the use of pedicle screws for the treatment of thoracic deformity has recently been adopted as the standard of care for the treatment of thoracic deformity. However, technical difficulties and concern over the development of severe complications has limited the widespread usage of such instrumentation in China. Thoracic pedicle diameters and vertebral bodies are smaller in the thoracic spine relative to the lumbar region, thus complicating their insertion [8–10]. Additionally, difference in the pedicle morphology of the Chinese population remains a concern.
Complications associated with the use of thoracic pedicle screws and the accuracy of screw insertion have been reviewed in a small number of previous studies, many of which were in a small number of patients [11–16]. Several earlier reports found high rates of pedicle wall violations, ranging from 15.9 to 54.7% [4, 17, 18]. However, in recent series, more promising results have been obtained. In their report on 4,600 thoracic screws used in deformity cases, Suk et al. [19] reported that only 1.5% of screws were malpositioned. Other complications were infrequent and included pedicle fractures (0.24%), infections (1.9%), screw loosening (0.76%) and a single case of transient paraparesis. Using a freehand technique, Kim et al. [20] found a cortical perforation rate of 6.9%, but no cases of neurologic, vascular or visceral complications as a result were reported.
In this study, we analyze the complications and related risk factors associated with the use of thoracic pedicle screws in a large cohort of Chinese patients that were treated at our institution for spinal deformities. This information will help demonstrate thoracic pedicle screw instrumentation to be safe and effective for use in this population, which to our knowledge has not been previously reported.
Methods
We searched the spine database of our department for patients who had undergone spinal deformity corrective surgery with the use of thoracic pedicle screws from 1 March 1998 to 1 March 2005. A total 242 patients who were treated for spinal deformities were identified and their charts and radiographs were retrospectively analyzed. Of these 242 thoracic deformity patients, 208 (70 males and 138 females) with an age ranging from 11 to 55 years (mean, 14.9 years) were included in this study. All 208 patients underwent corrective deformity surgery exclusively with posterior pedicle screw constructs. Clinical and radiographic follow-up for a minimum of 3 years was available for all patients. Etiologic diagnoses included adolescent idiopathic scoliosis (AIS) in 119 patients, congenital kyphoscoliosis in 38, adult scoliosis in 37 (including 30 idiopathic adult scoliosis and 7 de Novo scoliosis), Marfan syndrome combined with scoliosis in 7, neurofibromatosis in 6 and unspecified in 1 patient (Table 1). The positions of the screws were evaluated using intraoperative fluoroscopy and postoperative radiographs as well as postoperative CT scans for 19 patients in whom the accuracy of the pedicle screw placement was questionable. All radiographic evaluations were read in a double-blind fashion.
Table 1.
Demography of spinal deformity patients
| Etiology of scoliosis diagnosis | Patient (n) | Percentage correction |
|---|---|---|
| Sex (female) | 138 | |
| Adolescent idiopathic | 119 | 81 |
| Congenital | 38 | 65 |
| Adult | 37 | 62 |
| Marfan syndrome, combined | 7 | 61 |
| Neurofibromatosis, combined | 6 | 59 |
| Other | 1 | 45 |
All the patients had a minimum of 3 years of postoperative follow-up (range 3–5 years, mean 4.1 years). The medical records and radiographs were reviewed by independent observers in a double-blind fashion. The operative, postoperative and follow-up reports were reviewed to identify any complications associated with pedicle screw insertion. In cases where the instrumentation was combined with a decompression (8 patients), the position of the screw was assessed by palpating the medial and inferior wall of the pedicle, which was possible after decompression. Insertion in these cases was thought to be more accurate.
Surgical techniques
All the surgeries were performed at a single spine center and consisted of correction of deformity using posterior segmental pedicle screw fixation. Nine patients underwent posterior vertebral column resection because of rigid scoliotic and kyphotic deformities [19]. All the pedicle screws were inserted using the following technique.
Incision and exposure
Pedicle screws were inserted using the freehand technique as described by Lenke [20]. The bony landmarks were exposed, including the facet and transverse process out to its tip. The entry point for pedicle screw insertion was determined as follows:
Proximal thoracic spine (T1–T3): junction of the proximal transverse process and lamina medial to the lateral pars.
Middle thoracic spine (T4–T9): junction of the down-slope of the proximal transverse process and lamina of the base of the superior facet medial to the lateral pars.
Lower thoracic spine (T10–T12): down-slope of the bisected transverse process at the junction of the transverse process and lamina at the level of the lateral pars.
Pedicle hole preparation and screw insertion
After the proposed pedicle screw insertion, the dorsal cortex was removed with a rongeur, revealing the pedicle “blush”. A blunt, flexible, narrow probe (2-mm diameter) was then advanced down to the pedicle. The trajectory hole was then palpated to determine the integrity of the pedicle walls and bottom, followed by tapping and screw insertion [20]. The position of the screws was verified using intraoperative fluoroscopy. Transcranial motor and somatosensory evoked potential spinal cord monitoring was used in all the cases. Electromyographic nerve root recordings from the rectus abdominus muscle were recorded only for levels T7 and caudal.
Strategy of deformity correction
After insertion of pedicle screws in the proposed position, deformity correction was carried out using a rod rotation maneuver [21–23]. The inserted rods were contoured to conform to the normal sagittal profile of the instrumented spinal segments and to some modifications depending on the nature of the deformity. All the screws were locked into the corrected position and arthrodesis was carried out using autogenous iliac and or rib bone graft. In cases with vertebral column resection, the resected bone was also used for spinal fusion.
Results
A total of 1,123 thoracic pedicle screws (average: 9.2 screws/patient and 5.4 thoracic screws/patient) were inserted in 208 patients undergoing primary thoracic deformity correction. The diameter of the thoracic pedicle screws ranged from 4.5 to 6.5 mm. A diameter of 4.5 mm was used for the proximal thoracic spine (T1–T3), 5.5 mm for the middle thoracic spine (T4–T9) and 6.5 mm for the lower thoracic spine (T10–T12). The mean preoperative Cobb angle of the thoracic curvature was 68.8° (range 35°–120°). The curvatures were corrected to a mean of 19.5° (range 3°–45°) postoperatively, with a mean correction rate of 72% (P < 0.001). When separated based on diagnosis, the deformity correction rates at the final follow-up were 81% for AIS, 65% for congenital scoliosis, 62% for adult scoliosis, 61% for Marfan’s syndrome, 59% for neurofibromatosis type 1 and 45% for the remaining cases. The C7 plumb line (C7PL) distance to the midsacral line ranged from 28 to 81 mm (average 55.5 mm) preoperatively and was corrected to 21.5 mm postoperatively with a mean correction rate of 61% (P < 0.001) (Tables 1, 2). The postoperative CT scan was used in 19 patients. At a mean follow-up of 4.1 years, 19 screws were found to be aberrant (19/1,123, 1.7%) in 15 patients.
Table 2.
Global balance at pre- and postoperation
| Global balance | Preoperation | Postoperation | Correction rate (%) | P value |
|---|---|---|---|---|
| Main Cobb angle | 68.8° | 19.5° | 72 | <0.001 |
| C7PL for adult scoliosis group | 55.5 mm | 21.5 mm | 61 | <0.001 |
The postoperative complications were divided into two general categories based on Brown’s method [24]: (1) Those that were related to the use of instrumentation, but not specific to pedicle screw (e.g., instrumentation failure, pseudarthroses, infection, loss of correction and pneumothorax and effusion, etc.) and (2) those directly related to aberrant pedicle screw trajectory (e.g., screw malposition or medial pedicle wall penetration with nerve root impingement, screw loosening and dural tear, etc.).
Complications related to instrumentation, but not specific to thoracic pedicle screw
Infection
Infection was seen in eight patients (3.8%) who presented in the second postoperative week with drainage from the surgical incision. The infection was treated immediately with incision, drainage and thorough debridement without removing instrumentation. Infection resolved in all the cases and prolonged antibiotic therapy was used, extended for 1.5 months after the wound had healed.
Pneumothorax and pleural effusion
One patient with scoliosis developed a spontaneous pneumothorax postoperatively, which was treated by chest tube insertion and subsequent removal after 1 week with no recurrence later. Two patients developed small pleural effusions, without any fever or respiratory compromise and subsequently did not require thoracocentesis. The healing of the wound in these patients was uneventful and did not require removal of the implant. The total rate of pneumothorax and pleural effusion was 1.6%.
Complications directly related to incorrect pedicle screw placement
Screw malposition
Aberrant screw position was documented by the review of postoperative radiographs. Based on the attending doctor’s practice experience, when viewed on the standard AP and lateral X-rays, an apparent abnormal angle of a screw from the other screws was considered as an indication of malposition and a postoperative CT scan was performed. Postoperative CT was performed in only 19 of the 208 patients (9.1%) when radiographic evaluation showed possibility of aberrant trajectory in 23 screws. The total number of screws examined by CT was 219. CT scans were done using established 2-mm increments (intrapedicular, 0 or <2-mm pedicle breach, 2–4 mm of breach, >4 mm breach) [25].
Nineteen (1.7%; 19/1,123) thoracic screws in 15 patients having an aberrant position trajectory on CT scans were found. CT scan evaluation thus confirmed the aberrant position suspected on radiographs in 19 screws, while rest of the 200 screws confirmed by CT scan in those 19 patients had trajectory in line with the corresponding pedicles. The positions of these 19 malpositioned screws were: 2 screws in T3, 1 in T4, 7 in T5, 3 in T6, 3 in T7, and 3 in T9. Aberrant positioning was more common in severe curves: 15 screws in 10 patients with curves >90° and 4 screws in 3 patients with curves <90°. In our group of 208 patients, 21 patients’ curves were greater than 90°. Not significantly, but an obvious trend was that more aberrant positioning screws were present on the concave side. In these series, 14 misplaced screws were observed on the concave side, while 5 were found on the convex side. Of the 15 patients with aberrant screws, 5 presented with AIS, 5 with congenital curves, 3 were adult idiopathic scoliosis cases and 2 were scoliosis patients associated with Marfan syndrome.
The aberrant trajectory was medial in five (5 of 19, 26%), with medial pedicle lateral breach between 1.0 and 2.0 mm, and lateral in seven screws (7 of 19, 37%) (Figs. 1, 2), of which five were inserted on the concavity of the curve and two on the convexity of the curve with a mean pedicle breach of 2.1 mm (range 1.0–3.3 mm). The aberrant trajectory was superiorly directed in four screws and inferiorly in three (Fig. 3), with pedicle breach between 1.5 and 2.2 mm. Two of the screws had an anterior cortex penetration verified by CT scan; thereafter, one screw was immediately removed without any complications during follow-up (Table 1; Figs. 1, 2, 3, 4).
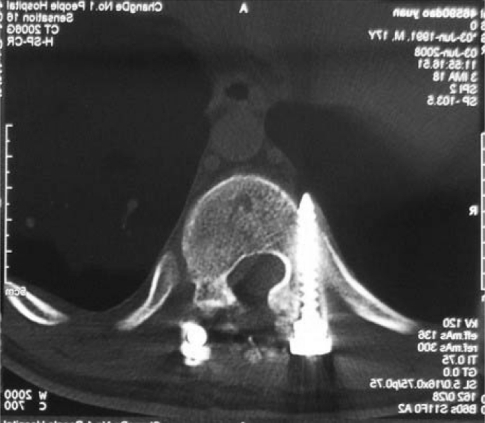
Fig. 1.
Pedicle screw placement in the thoracic spine. Note the right screw tip breached the cortical bone of the thoracic vertebrae anteriorly. As the screw tip is far away from the vascular structures, it can be left in place
Fig. 2.
Postoperative CT scan demonstrating medial placement of a left thoracic pedicle screw. This patient experienced postoperative radicular pain and required revision surgery for screw removal
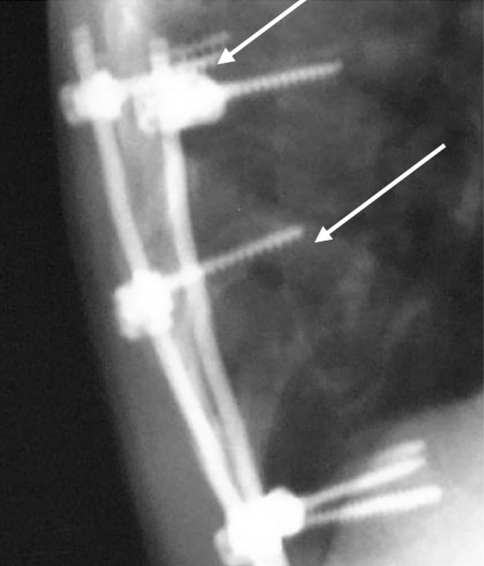
Fig. 3.
Post-operative X-ray shows rostral aberrant placement of a screw (lower arrow) and loss of fixation and screw pull out of a thoracic screw (upper arrow)
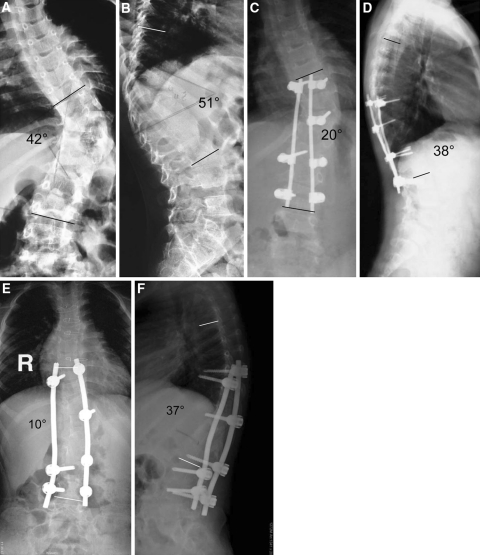
Fig. 4.
An 11-year- old boy with a congenital hemivertebra at T11. The angulation of the coronal and sagittal plane was 42 and 51, respectively. The sagittal view shows a hyperkyphosis at the thoracolumbar junctional region (a and b). Postoperative 3 months follow-up radiographs demonstrated that the angulation of the coronal and sagittal views was corrected to 20 and 38, respectively. However, the anterioposterior and lateral view (c and d) shows loosening and pullout of two screws and this patient underwent revision surgery. Four-year follow-up image (e and f). The shoulder and pelvis achieved good balance during follow-up
Only one patient (0.5%) had symptoms in the postoperative period, which were attributable to the aberrant trajectory of the screw. One patient presented with fever 4 days after surgery. CT imaging showed pleural effusion and lateral aberration in the trajectory of the left screw in T6, and the right screw also showed moderate lateral violation. In the other 18 patients, aberrant screw trajectory did not produce any clinical symptoms. These malpositioned screws presented a mild lateral cortical perforation and were not in direct contact with the aorta (at least 5 mm away) and, therefore, left the misplaced screws alone. At a mean follow-up of 3 years (range 2–5 years), there were no typical changes in the radiograph control and no symptoms.
Dural tear
Dural tear was seen in three patients (1.4%), evidenced by leakage of cerebrospinal fluid while preparing the screw holes. All dural tears were seen while preparing the concave side of the thoracic pedicles for screw insertion using a small curette. Dural tear was seen at T5, T6 or T9 in these three patients. The scoliotic curves in these three cases were more than 90°. The dural tears were immediately repaired by performing a hemilaminectomy for direct visualization of the tear and repair using suture material and fibrin glue. All the dural tears healed postoperatively with no postoperative CSF leak.
Pedicle fracture
Intraoperative pedicle fractures were seen in two patients (0.9%) and attributed to repeated attempts to position the screw in the concavity of the curvature in the presence of significant vertebral rotation. These fractures were recognized immediately during screw insertion in both cases with the whisker probe palpating a defect in the medial wall of the pedicle. The holes were then sealed with bone wax, and the pedicle screw was not inserted. In the other three cases, a pedicle fracture occurred during the rod derotational maneuver. The screws were subsequently removed and the holes sealed with bone wax. No fractures occurred in the immediate postoperative or subsequent follow-up periods.
Transient paraparesis
One patient (0.4%) developed transient paraparesis in the first postoperative month that was attributed to the loosening of the screw. Such screw was initially malpositioned and subsequently migrated further into the spine canal resulting in spinal cord compression. This patient experienced complete recovery following removal of the screw.
Screw loosening
Three cases had radiographic evidence of screw loosening because of malposition in the absence of clinical symptoms. These screws were removed at 1 year postoperatively. One case developed transient paraparesis due to screw loosening and migration, as discussed above.
At the final follow-up, the deformity correction rate (Table 1) was 81% for AIS, 65% for congenital scoliosis, 62% for adult scoliosis, 61% for Marfan’s syndrome, 59% in cases with neurofibromatosis and 45% in other cases. The complication rate was 8.6% for the perioperative period and 1.6% at the final follow-up. Pedicle screw was thought to be responsible for the complication in 7.2% patients. There were no significant screw-related neurologic or visceral complications that adversely affected the long-term outcome. As much as 78.8% (164/208) of patients showed radiographic evidence of solid fusion at the follow-up examinations. In the remaining 21.2% (44/208) patients, solid fusion was not observed, but revision surgery was not necessary. Loss of correction was not obvious in this group, since most of them did not have a very long-term follow-up.
Discussion
Thoracic pedicle screw for deformity correction has become a common method of instrumentation in developed countries [1], as it provides a stronger biomechanical anchoring strength compared to the hook and wire construct [7, 26]. However, the concern of potentially life-threatening complications from thoracic pedicle screw fixation has yet limited its widespread use. Recent studies have brought more light to this issue and showed that the complication rate of posterior instrumentations using pedicle screws is not higher that that of other instrumentations, such as Luque’s, hooks or hybrids, in the treatment of thoracic spinal deformity [3, 20, 23, 27, 28]. The purpose of our study was to analyze the complications and risk factors associated with thoracic pedicle screw fixation in a large cohort of Chinese patients with spinal deformity operated in a single spine center.
Historically, complications that result from thoracic pedicle screw instrumentation have been divided into three categories based on the time that they occur during the surgical procedure [19]. However, certain complications can occur either intraoperatively or postoperatively. In addition, some complications that develop are not directly related to the implantation of pedicle screws. Therefore, in this study, we chose to categorize our complications according to the system proposed by Brown et al. [24].
Category I complications were related to instrumentation but not specific to thoracic pedicle screws, such as infection (3.8%), pneumothorax and or pleural effusion (1.4%) can be observed specifically after pedicle screw insertion if the path of the screw had been outside the pedicle. There were eight cases of wound infection with fever and discharge, which were treated immediately with incision and drainage and healed without any consequences. None of the cases required instrumentation removal. The rate of this complication was according to that reported in literature, i.e., 1.9% for Suk et al. [19] and 1.7% for Di Silvestre et al. [29]. The incidence of infection was higher in our series (3.8%) compared to both. After retrospective analysis, poor preoperative nutritional balance and hygiene were thought to contribute to a higher rate of infection in these patients, as most of them belonged to the lower socioeconomic strata. Prolonged antibiotic therapy for 2 months after healing of infection was considered necessary.
In our series of 208 consecutive Chinese patients, low rates of neurological complications were seen, which were similar to other large series of patients with scoliosis who were treated with thoracic pedicle screws [1, 20, 29–31]. Among the 19 patients who developed clinical complications in our series, only one neurologic complication was observed. This was a case of congenital kyphoscoliosis, in which the patient developed transient paraparesis related to a misplaced pedicle screw at T10. Neurological complications in the treatment of thoracic scoliosis with pedicle screws have infrequently been reported in literature. Papin et al. [32] reported on a 15-year-old girl, at the postoperative 6 months, with an unusual presentation of spinal cord compression, epigastric pain, tremor of the right foot at rest and abnormal feelings in her legs. Her symptoms were attributed to two pedicle screws (one at T8 and one at T10), which had penetrated the spinal canal by 4 mm. The symptoms did not resolve spontaneously and she eventually required screw revision surgery. Complete recovery occurred 1 month later. In a large series of 4,604 thoracic pedicle screws inserted in 462 patients, Suk et al. [19] reported only one patient, with an associated diagnosis of neurofibromatosis, who presented with transitory paraparesis due to medial perforation of the pedicle resulting in the development of a delayed epidural hematoma. These rates of neurological complications in the thoracic spine seem counterintuitive, but may be related to less obvious clinical presentation of thoracic nerve root irritation.
Pneumothorax and pleural effusion have been previously reported in thoracic pedicle screw instrumentation. One patient in a series of Suk et al. [19] had spontaneous pneumothorax, which was subsequently treated by chest tube insertion, while one patient in the series of Di Silvestre et al. [29] developed pleural effusion with fever postoperatively, which was thought to be related to the lateral position of a left T5 screw that was inside the thoracic cavity. The pleural effusion resolved completely after screw removal. Liljenqvist et al. [3] reported one case with laterally aberrant screw that led to a small hematoma, but with no clinical consequences. In this study, two patients (one in Marfan syndrome combined and one in AIS) developed small pleural effusion and one pneumothorax (congenital), directly related to instrumentation and vertebral resection, respectively, but no fever, hematoma or respiratory compromise was seen. In both the patients with pleural effusions, healing was complete and they did not require removal of screw.
Category II complications were directly related to the aberrant screw trajectory. The screw malposition (7.2%), dural tear (1.4%), thoracic pedicle fracture (0.9%), transient paraparesis (0.4%) and screw loosening (1.4%) were found to be related to screw insertion (Table 3).
Table 3.
Classification of thoracic pedicle screw complications and comparison
| Types | Current study | Percentage of complications reported by (no. of patients) | |||
|---|---|---|---|---|---|
| Definition | No. of patients (n = 208) | Percentage of complications | Study of Suk et al. (n = 462) | Study of Di Silvestre et al. (n = 115) | |
| Category I | Infection | 8 | 3.8 | 1.9 | 1.7 |
| Effusion | 3 | 1.4 | 0.2 | 0.8 | |
| Category II | Screw malposition | 15 | 7.2 | 10.4 | 5.7 |
| Dural tear | 3 | 1.4 | 0.6 | 12.1 | |
| Pedicle fracture | 2 | 0.9 | 0.2 | 13.0 | |
| Transient paraparesis | 1 | 0.4 | 0.2 | 0.0 | |
| Screw loosening | 3 | 1.4 | 0.8 | 0.8 | |
| Overall | 35 | 16.5 | 14.3 | 34.1 | |
Few major complications have been attributed to thoracic pedicle screw insertion for scoliosis correction [33, 34]. The complications involve impingement of the descending thoracic aorta by a T5 pedicle screw, detected by postoperative CT, pseudoaneurysm formation due to an aberrant T6 pedicle screw and warranted removal of the respective screw. On retrospective analysis of CT scans of 19 patients in our series, none of the screws was found to cause aortic impingement or penetration.
The incidence of asymptomatic aberrant thoracic pedicle screws has been found to be 16.6–29% [4, 25] on postoperative CT scan evaluation. Only few of these screws were prophylactically removed and such asymptomatic screws have been shown to pose a potential risk of subsequent vascular lesions and erosion of aorta and warrant prophylactic removal [29, 35]. Malpositioned screws causing lateral cortical breach of 3.0–6.0 mm may be safely left in place without causing complications [3, 20]. Nonetheless, insertion of long screws should always be avoided, as they pose a potential for penetrating the azygos vein and the parietal pleura on the right and the thoracic aorta and esophagus on the left [17, 36–39]. To preserve the anterior vertebral cortex of the upper thoracic spine, pedicle screw insertion should be more convergent at this level and the screw length less than 25–30 mm for safe insertion [29]. None of the screws in our study had lateral cortical breach significant enough to abut against the aorta.
Medial cortical breach has been commonly reported, although it still remains controversial [25]. Medial cortical breach of ≤2 mm is considered to be acceptable. The lateral cortical breach has been shown to have a marginally higher complication rate (0.5%) than the medial cortical breach (0.3%) [4]. However, Gerbsten et al. [40] studied postoperative CT scans of 71 thoracic screws used in thoracolumbar fractures and found an incidence of 26% for medial cortical penetration and penetration of up to 8 mm. He concluded that a 4-mm breach was a “safe zone” of medial encroachment (2 mm of epidural space and 2 mm of subarachnoid space). Kim et al. [20] hypothesized on a “definite safe zone” within 2 mm, “probable safe zone” within 2–4 mm and a “questionable safe zone” of 4–8 mm for medial cortical breach. Schizas et al. [41] inserted pedicle screws in the upper thoracic spine using anatomical landmarks with an accuracy comparable to that of previous studies with navigation system at the thoracic spine. Liljenqvist et al. [3] found that the width of the epidural space was <1 mm with magnetic resonance imaging at the thoracic apical level on the concave side, which means that there was no safety zone on the concavity.
Di Silvestre et al. [29], in their series of 115 consecutive patients using 1,035 transpedicular thoracic screws with posterior fusion, reported dural tears (without neurologic complications) in 14 cases (12.1%). Suk et al. [19] reported three cases of dural tear in a larger cohort of patients with thoracic pedicle screw insertion. In our series, dural tear was seen in three cases (1.4%), all while inserting a pedicle screw on the concave side of a severe scoliotic curve using a small curette for the preparation of the hole. Dural tear was seen while inserting a screw at the T5 vertebra in two patients and at the T6 vertebra in one patient. All of the three dural tears happened laterally and not posteriorly. Since the scoliotic curves in these three cases were more than 90°, a small laminotomy was performed for safe insertion of the screws. The dural tears were treated by enlarging the laminectomy and direct suturing of the dura, and all three patients had an uneventful recovery. Commonly, it is not necessary to repair the dural tear and plugging the pedicle hole with bone wax is all that is needed when the decompression is not planned to be done before the operation.
Pedicle blowout fracture was seen in two patients (0.9%) due to repeated attempts to insert the screw in the concavity of the scoliosis curve. The resulting hole was sealed with bone without the inserting screw. In another patient, the pedicle fracture occurred during the rod rotation maneuver. The screw was removed and the hole sealed with bone wax. The incidence of pedicle screw fracture in our series was (0.9%) slightly higher than that in Suk et al. [19] (0.2%), but significantly lower than in the series of Di Silvestre et al. [29] (13%). We feel that pedicle fracture during screw insertion is not related to the pedicle diameter, though the pedicle diameter in the Chinese people is less than that in Caucasians [2, 42].
Transient paraparesis as a complication has rarely been reported in the treatment of thoracic scoliosis with pedicle screws. One patient (0.4%) developed transient paraparesis in our study. In a large series of 462 patients with 4,604 thoracic pedicle screw insertions, Suk et al. [19] reported only 1 patient (with neurofibromatosis) who developed transient paraparesis due to medial perforation of the pedicle resulting in a delayed epidural hematoma, which resolved following screw removal and decompression by laminectomy. In our series of 208 consecutive patients, none of the patients developed permanent neurological complications as was seen in other large series of scoliosis patients who were treated with thoracic pedicle screw insertion [1, 20, 29–31].
There are several limitations to this study. The rate of misplaced screws; however, has been found to increase up to 14% when all inserted screws are evaluated by CT in the postoperative period [1, 20, 25, 31, 43]. It has been shown that conventional radiographs may indicate the correct placement of a screw that is actually incorrectly placed and vice versa [37, 44]. The rate of such occurrences is generally low, however, and diminishes with the level of experience. In addition, due to concerns regarding radiation exposure and expense, CT scans were not performed on all patients involved in this study. A second limitation to this study is the lack of a control group, other than historical. Finally, despite the application of blinding among investigators in this study, the retrospective nature limits its ability to eliminate bias.
It is our conclusion that using thoracic pedicle screws for the treatment of spinal deformities of the thoracic spine is a safe procedure in the Chinese patient population. At the same time, it allows satisfactory correction of the deformity and maintenance of this correction. Future studies with direct comparison between pedicle screw instrumentation and other instrumentation are needed.
Acknowledgments
No Funding was received for this project.
Contributor Information
Gang Li, Email: li.gang@mgh.harvard.edu.
Youwen Deng, Email: drywdeng3@gmail.com.
References
- 1.Kuklo TR, Lenke LG, O’Brien MF, Lehman RA, Jr, Polly DW, Jr, Schroeder TM. Accuracy and efficacy of thoracic pedicle screws in curves more than 90 degrees. Spine. 2005;30:222–226. doi: 10.1097/01.brs.0000150482.26918.d8. [DOI] [PubMed] [Google Scholar]
- 2.Hou S, Hu R, Shi Y. Pedicle morphology of the lower thoracic and lumbar spine in a Chinese population. Spine. 1993;18:1850–1855. doi: 10.1097/00007632-199310000-00021. [DOI] [PubMed] [Google Scholar]
- 3.Liljenqvist U, Lepsien U, Hackenberg L, Niemeyer T, Halm H. Comparative analysis of pedicle screw and hook instrumentation in posterior correction and fusion of idiopathic thoracic scoliosis. Eur Spine J. 2002;11:336–343. doi: 10.1007/s00586-002-0415-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liljenqvist UR, Halm HF, Link TM. Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine. 1997;22:2239–2245. doi: 10.1097/00007632-199710010-00008. [DOI] [PubMed] [Google Scholar]
- 5.Ruofu Z, Huilin Y, Xiaoyun H, et al. CT evaluation of cervical pedicle in a Chinese population for surgical application of transpedicular screw placement. Surg Radiol Anat. 2008;30:389–396. doi: 10.1007/s00276-008-0339-0. [DOI] [PubMed] [Google Scholar]
- 6.Tan SH, Teo EC, Chua HC. Quantitative three-dimensional anatomy of cervical, thoracic and lumbar vertebrae of Chinese Singaporeans. Eur Spine J. 2004;13:137–146. doi: 10.1007/s00586-003-0586-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yuksel KZ, Adams MS, Chamberlain RH, et al. Pullout resistance of thoracic extrapedicular screws used as a salvage procedure. Spine J. 2007;7:286–291. doi: 10.1016/j.spinee.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 8.Panjabi MMOHJ, Crisco JJ, III, et al. Complexity of the thoracic spine pedicle anatomy. Eur Spine J. 1997;6:19–24. doi: 10.1007/BF01676570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rampersaud YRPJ, Salonen D, Farooq S. Clinical accuracy of fluoroscopic computer-assisted pedicle screw fixation: a CT analysis. Spine. 2005;30:E183–E190. doi: 10.1097/01.brs.0000157490.65706.38. [DOI] [PubMed] [Google Scholar]
- 10.Vaccaro ARRS, Allardyce TJ, et al. Placement of pedicle screws in the thoracic spine. Part I: Morphometric analysis of the thoracic vertebrae. J Bone Joint Surg Am. 1995;77:1193–1199. doi: 10.2106/00004623-199508000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Halm H, Niemeyer T, Link T, Liljenqvist U. Segmental pedicle screw instrumentation in idiopathic thoracolumbar and lumbar scoliosis. Eur Spine J. 2000;9:191–197. doi: 10.1007/s005860000139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lonstein JE, Denis F, Perra JH, Pinto MR, Smith MD, Winter RB. Complications associated with pedicle screws. J Bone Joint Surg Am. 1999;81:1519–1528. doi: 10.2106/00004623-199911000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Hamill CL, Lenke LG, Bridwell KH, Chapman MP, Blanke K, Baldus C. The use of pedicle screw fixation to improve correction in the lumbar spine of patients with idiopathic scoliosis. Is it warranted? Spine. 1996;21:1241–1249. doi: 10.1097/00007632-199605150-00020. [DOI] [PubMed] [Google Scholar]
- 14.Esses SI, Sachs BL, Dreyzin V. Complications associated with the technique of pedicle screw fixation. A selected survey of ABS members. Spine. 1993;18:2231–2238. doi: 10.1097/00007632-199311000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Davne SH, Myers DL. Complications of lumbar spinal fusion with transpedicular instrumentation. Spine. 1992;17:S184–S189. doi: 10.1097/00007632-199206001-00021. [DOI] [PubMed] [Google Scholar]
- 16.West JL, 3rd, Ogilvie JW, Bradford DS. Complications of the variable screw plate pedicle screw fixation. Spine. 1991;16:576–579. doi: 10.1097/00007632-199105000-00016. [DOI] [PubMed] [Google Scholar]
- 17.Vaccaro AR, Rizzolo SJ, Balderston RA, et al. Placement of pedicle screws in the thoracic spine. Part II: An anatomical and radiographic assessment. J Bone Joint Surg Am. 1995;77:1200–1206. doi: 10.2106/00004623-199508000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Xu REN, Ou Y, et al. Anatomical considerations of pedicle screw placement in the thoracic spine: Roy-Camille technique versus open-lamina technique. Spine. 1998;23:1065–1068. doi: 10.1097/00007632-199805010-00021. [DOI] [PubMed] [Google Scholar]
- 19.Suk SI, Kim WJ, Lee SM, Kim JH, Chung ER. Thoracic pedicle screw fixation in spinal deformities: are they really safe? Spine. 2001;26:2049–2057. doi: 10.1097/00007632-200109150-00022. [DOI] [PubMed] [Google Scholar]
- 20.Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD. Freehand pedicle screw placement in the thoracic spine: is it safe? Spine. 2004;29:333–342. doi: 10.1097/01.BRS.0000109983.12113.9B. [DOI] [PubMed] [Google Scholar]
- 21.Cotrel Y, Dubousset J, Guillaumat M. New universal instrumentation in spinal surgery. Clin Orthop Relat Res. 1988;227:10–23. [PubMed] [Google Scholar]
- 22.Suk SI, Lee SM, Chung ER, Kim JH, Kim SS. Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis: more than 5-year follow-up. Spine. 2005;30:1602–1609. doi: 10.1097/01.brs.0000169452.50705.61. [DOI] [PubMed] [Google Scholar]
- 23.Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995;20:1399–1405. [PubMed] [Google Scholar]
- 24.Brown CA, Lenke LG, Bridwell KH, Geideman WM, Hasan SA, Blanke K. Complications of pediatric thoracolumbar and lumbar pedicle screws. Spine. 1998;23:1566–1571. doi: 10.1097/00007632-199807150-00012. [DOI] [PubMed] [Google Scholar]
- 25.Belmont PJ, Jr, Klemme WR, Dhawan A, Polly DW., Jr In vivo accuracy of thoracic pedicle screws. Spine. 2001;26:2340–2346. doi: 10.1097/00007632-200111010-00010. [DOI] [PubMed] [Google Scholar]
- 26.Wood KB, Wentorf FA, Ogilvie JW, Kim KT. Torsional rigidity of scoliosis constructs. Spine (Phila Pa 1976) 2000;25:1893–1898. doi: 10.1097/00007632-200008010-00006. [DOI] [PubMed] [Google Scholar]
- 27.Storer SK, Vitale MG, Hyman JE, Lee FY, Choe JC, Roye DP., Jr Correction of adolescent idiopathic scoliosis using thoracic pedicle screw fixation versus hook constructs. J Pediatr Orthop. 2005;25:415–419. doi: 10.1097/01.mph.0000165134.38120.87. [DOI] [PubMed] [Google Scholar]
- 28.Suk SI, Lee CK, Min HJ, Cho KH, Oh JH. Comparison of Cotrel-Dubousset pedicle screws and hooks in the treatment of idiopathic scoliosis. Int Orthop. 1994;18:341–346. doi: 10.1007/BF00187077. [DOI] [PubMed] [Google Scholar]
- 29.Di Silvestre M, Parisini P, Lolli F, Bakaloudis G. Complications of thoracic pedicle screws in scoliosis treatment. Spine. 2007;32:1655–1661. doi: 10.1097/BRS.0b013e318074d604. [DOI] [PubMed] [Google Scholar]
- 30.Ain MC, Browne JA. Spinal arthrodesis with instrumentation for thoracolumbar kyphosis in pediatric achondroplasia. Spine. 2004;29:2075–2080. doi: 10.1097/01.brs.0000138411.14588.47. [DOI] [PubMed] [Google Scholar]
- 31.Kuklo TR, Potter BK, Polly DW, Jr, Lenke LG. Monaxial versus multiaxial thoracic pedicle screws in the correction of adolescent idiopathic scoliosis. Spine. 2005;30:2113–2120. doi: 10.1097/01.brs.0000179260.73267.f4. [DOI] [PubMed] [Google Scholar]
- 32.Papin P, Arlet V, Marchesi D, Rosenblatt B, Aebi M. Unusual presentation of spinal cord compression related to misplaced pedicle screws in thoracic scoliosis. Eur Spine J. 1999;8:156–159. doi: 10.1007/s005860050147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Minor ME, Morrissey NJ, Peress R, et al. Endovascular treatment of an iatrogenic thoracic aortic injury after spinal instrumentation: case report. J Vasc Surg. 2004;39:893–896. doi: 10.1016/j.jvs.2003.10.056. [DOI] [PubMed] [Google Scholar]
- 34.Choi JB, Han JO, Jeong JW. False aneurysm of the thoracic aorta associated with an aorto-chest wall fistula after spinal instrumentation. J Trauma. 2001;50:140–143. doi: 10.1097/00005373-200101000-00029. [DOI] [PubMed] [Google Scholar]
- 35.Jendrisak MD. Spontaneous abdominal aortic rupture from erosion by a lumbar spine fixation device: a case report. Surgery. 1986;99:631–633. [PubMed] [Google Scholar]
- 36.Rampersaud YR, Lee KS. Fluoroscopic computer-assisted pedicle screw placement through a mature fusion mass: an assessment of 24 consecutive cases with independent analysis of computed tomography and clinical data. Spine. 2007;32:217–222. doi: 10.1097/01.brs.0000251751.51936.3f. [DOI] [PubMed] [Google Scholar]
- 37.Lehman RA, Jr, Lenke LG, Keeler KA, Kim YJ, Cheh G. Computed tomography evaluation of pedicle screws placed in the pediatric deformed spine over an 8-year period. Spine. 2007;32:2679–2684. doi: 10.1097/BRS.0b013e31815a7f13. [DOI] [PubMed] [Google Scholar]
- 38.Heary RF, Bono CM, Black M. Thoracic pedicle screws: postoperative computerized tomography scanning assessment. J Neurosurg. 2004;100:325–331. doi: 10.3171/spi.2004.100.4.0325. [DOI] [PubMed] [Google Scholar]
- 39.Youkilis AS, Quint DJ, McGillicuddy JE, Papadopoulos SM. Stereotactic navigation for placement of pedicle screws in the thoracic spine. Neurosurgery. 2001;48:771–778. doi: 10.1097/00006123-200104000-00015. [DOI] [PubMed] [Google Scholar]
- 40.Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine. 1990;15:11–14. doi: 10.1097/00007632-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 41.Schizas C, Theumann N, Kosmopoulos V. Inserting pedicle screws in the upper thoracic spine without the use of fluoroscopy or image guidance: is it safe? Eur Spine J. 2007;16:625–629. doi: 10.1007/s00586-006-0262-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zindrick MR, Wiltse LL, Doornik A, et al. Analysis of the morphometric characteristics of the thoracic and lumbar pedicles. Spine. 1987;12:160–166. doi: 10.1097/00007632-198703000-00012. [DOI] [PubMed] [Google Scholar]
- 43.Smorgick Y, Millgram MA, Anekstein Y, Floman Y, Mirovsky Y. Accuracy and safety of thoracic pedicle screw placement in spinal deformities. J Spinal Disord Tech. 2005;18:522–526. doi: 10.1097/01.bsd.0000154448.90707.a8. [DOI] [PubMed] [Google Scholar]
- 44.Lee CS, Kim MJ, Ahn YJ, Kim YT, Jeong KI, Lee DH. Thoracic pedicle screw insertion in scoliosis using posteroanterior C-arm rotation method. J Spinal Disord Tech. 2007;20:66–71. doi: 10.1097/01.bsd.0000211248.75200.3f. [DOI] [PubMed] [Google Scholar]