Abstract
This article focuses on drug targeting to specific cellular organelles for therapeutic purposes. Drugs can be delivered to all major organelles of the cell (cytosol, endosome/lysosome, nucleus, nucleolus, mitochondria, endoplasmic reticulum, Golgi apparatus, peroxisomes and proteasomes) where they exert specific effects in those particular subcellular compartments. Delivery can be achieved by chemical (e.g., polymeric) or biological (e.g., signal sequences) means. Unidirectional targeting to individual organelles has proven to be immensely successful for drug therapy. Newer technologies that accommodate multiple signals (e.g., protein switch and virus-like delivery systems) mimic nature and allow for a more sophisticated approach to drug delivery. Harnessing different methods of targeting multiple organelles in a cell will lead to better drug delivery and improvements in disease therapy.
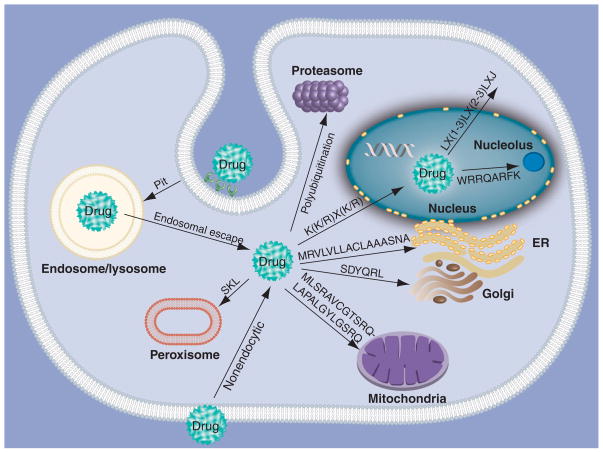
The 1975 discovery of the ‘signal hypothesis’ led Gunter Blobel to win a Nobel Prize [1–3]. Blobel predicted that ‘zip codes’ were responsible for targeting certain proteins to subcellular compartments such as the cytoplasm, nucleus, nucleolus, mitochondria, endoplasmic reticulum (ER), Golgi and peroxisomes (Figure 1). The intracellular delivery of a pharmaceutical agent can have a dramatic impact on its therapeutic efficacy. Indeed, precise compartmentalization of certain drugs is necessary for their biological effect. For example, agents intended for gene therapy must be eventually delivered to the nucleus in order for the therapeutic protein to be expressed. Some drugs, such as RNAi, must target the cytosol in order to block the cells’ mRNA. In other cases, pro-apoptotic drugs can be selectively targeted to the mitochondria where they exert their actions.
Figure 1. Drug targeting to cellular organelles.
Text on arrows indicate consensus targeting sequence (if available), example of targeting signal or mode of targeting.
ER: Endoplasmic reticulum.
Our previous work has shown that an oncogene can be targeted to a different cellular compartment to completely alter its function. The causative agent of chronic myelogenous leukemia (CML), Bcr-Abl, is normally found in the cytoplasm where it acts as an oncogene. However, when targeted to the nucleus (by attaching four nuclear localization signals [NLSs]) it acts as an apoptotic factor [4]. In this case, targeting a protein to a single organelle can be used to elicit a desired effect such as apoptosis. Further work in our laboratory focuses on controlled localization of proteins to alter function. We have described our ‘protein switch’ technology that allows controlled translocation from the cytoplasm to the nucleus upon addition of a ligand [5–7]. One of the main goals of our research is to imitate the function of proteins found in nature. Many proteins in signal transduction pathways are localized to one compartment initially, bind to protein partners in the cell (or are signaled by other proteins) and change their location in the cell, leading to an alteration in function. Ultimately we seek not only targeting of a specific organelle, but also a further level of sophistication, where multiple signals can be used to target multiple organelles. Indeed, the ability to precisely target drugs to different organelles is changing the way therapeutics are developed. This article will focus on therapeutic targeting to specific cellular organelles (Figure 1). Each organelle will be briefly described, followed by methods to reach and target the organelle for therapy. Finally, future perspectives for therapeutic delivery will be discussed.
Cytosolic delivery
Typically, drugs targeting cellular organelles have to be initially delivered to the cytosol, which in some cases is the site of action, where drugs (e.g., glucocorticoids, proteins or siRNA) bind to their receptors or act on other targets. There are three main barriers that must be overcome to facilitate cytosolic delivery:
Evading detection by the reticuloendothelial system (RES)
Interaction with the cell membrane and internalization
Intracellular trafficking and endosomal escape
Evading RES detection
In order for cytosolic delivery to occur when the drug is delivered into the bloodstream, the drug first has to evade detection by the RES prior to interacting with cell membranes. The endothelial layers of the liver, spleen and bone marrow comprising the RES contain mononuclear macrophages that filter the blood of foreign pathogenic particles [8]. Aggregation of foreign particles in the presence of plasma proteins and cell adhesion molecules facilitates rapid clearance from the bloodstream [9–12]. To lengthen the circulatory time and decrease macrophage detection, several approaches have been attempted. Liposomes have been one of the most common drug delivery agents used to evade RES detection. Regular liposomes undergo rapid opsonization via the RES cells, followed by lysosomal degradation. Strategies to evade RES detection have included use of targeted liposomes (for accumulation in target organs) and/or using ‘stealth’ liposomes [13]. Long-circulating liposomes (stealth) can be prepared by including amphiphilic stabilizers (e.g., cholesterol) [14–16], phosphatidylinositol and gangliosides [17], or a hydrophilic surface by grafting with polyethylene glycol (PEG) [18]. The combination of long-circulating and targeted liposomes has been extremely popular in the last decade (e.g., antibody targeting and PEG) [13].
Cell membrane interaction
Subsequently, therapeutics interact with cell membranes (plasma membranes), which are lipid bilayers composed of phospholipids (phosphatidylcholine, phosphatidylethanolamine, phosphatidylserine and sphingomyelin are common phospholipids), cholesterol, glycolipids and proteins (including proteoglycans, which contain a core protein with one or more glycosaminoglycans attached) [19]. Proteoglycans are important for delivery of drugs via cationic polymers [20,21]. For example, an ionic interaction occurs between cationic polyethyleneimine (PEI) and the cell membrane, which has negatively charged sulfated proteoglycans on the cell surface [20].
Conjugation with cell-penetrating peptides can also overcome the barrier of the cell membrane [22,23]. In the late 1980s and early 1990s many groups ([24–26] and others) found that a protein transduction domain of 9–16 cationic (polyarginine like) amino acid residues had cell membrane-penetrating capability, including the ability to cross the nucleus. Several other groups [27] showed that peptides and proteins attached to cell-penetrating peptides can cross cell membranes (reviewed in [28]). Many therapeutics have been delivered to cells in this manner [29–33].
Internalization may occur by endocytosis (initiated by electrostatic or hydrophobic interactions with the cell membrane, or interaction with a cell-surface receptor) followed by endosomal escape, or by other means, such as macropinocytosis, or combinations of these [13]. After traf-ficking into the cytosol, the drug may either exert its action or traverse to a subcellular compartment (e.g., nucleus, mitochondria and peroxisome). For example, for delivery of genes, the cytoplasmic barrier is only the first step before delivery to the nucleus can occur. Table 1 depicts various agents designed to target the cytosol and their corresponding cargo (drug).
Table 1.
Cytosolic targeting of drug therapeutics (includes endosomal/lysosomal escape, in some cases).
| Class of targeting agent | Targeting agent composition | Drug delivered (trade name if available) | Ref. |
|---|---|---|---|
| Liposomes | Liposome composed of lipid bilayer neutral lipids, DPPC and cholesterol | Amikacin (Arikace™) | [347] |
| Liposomal includes soybean oil and phospholipids | Cyclosporin | [348] | |
| Doxorubicin STEALTH® liposome containing MPEG–DSPE, HSPC and cholesterol | Doxorubicin (Doxil®) | [349] | |
| pH-sensitive liposomes | Liposomes composed of CHEMS and DOPE | Diptheria toxin A chain | [38] |
| DOPE, N-succinyl–DOPE and PEG–ceramide | Gentamycin | [350] | |
| Thermosensitive liposomes | DPPC, HSPC and cholesterol liposomes surface modified with DSPE-PEG-2000:PNIPAM-AAM17 | Doxorubicin | [351] |
| Targeted thermal magnetic liposomes | DPPC, cholesterol, DSPE–PEG(2000) and DSPE–PEG(2000)–folate | Doxorubicin | [352,353] |
| Polymeric micelles | PEG–poly(aspartic acid) block copolymer | Doxorubicin (Adriamycin®) | [354] |
| pH-sensitive micelles | PEG-block-poly(aspartate-hydrazide) or PEG–p(Asp-Hyd) was modified using either levulinic acid or 4-acetyl benzoic acid attached via hydrazone bonds | Doxorubicin (Adriamycin) | [355] |
| pH-sensitive micelles with cell surface targeting | Amphiphilic block copolymers that self-assemble into spherical micelles, folate–PEG–poly(aspartate-hydrazone-adriamycin) with γ-carboxylic acid-activated folate | Doxorubicin (Adriamycin) | [356] |
| Thermosensitive micelles/polymers | Micellar cyclotriphosphazenes | Human growth hormone | [43] |
| Biodegradable triblock copolymer of PLGA–PEG–PLGA (ReGel®) | Paclitaxel | [357] | |
| Cell-penetrating peptides | Doxorubicin bound to HPMA-based polymer with the cell-penetrating peptide Tat | Doxorubicin | [358] |
| Cationic polymers and cationic lipids | Polyethyleneimine | Genes (DNA) | [61,359] |
| Virus mimetic | Hydrophobic polymer core (poly(L-histidine-co-phenylalanine)(poly(His32-co-Phe6) and two layers of hydrophilic shell (one PEG end linked to core polymer; other end to BSA) | Doxorubicin | [346] |
| NES | NES (LQLPPLERLTL) encoded in a plasmid | Genes (DNA) | [6,7,60] |
| NES (ALPPLERLTL) conjugated to DNA | Antisense oligonucleotide | [360] |
BSA: Bovine serum albumin; CHEMS: Cholesterylhemisuccinate; DOPE: Dioleoylphosphatidylethanolamine; DPPC: Dipalmitoylphosphatidylcholine; DSPE: Distearoylphosphatidylethanolamine; HPMA: N-(2-hydroxypropyl)methacrylamide; HSPC: Fully hydrogenated soy phosphatidylcholine; MPEG: Methoxypolyethylene glycol; NES: Nuclear export signal; PEG: Polyethylene glycol; PLGA: Poly(lactide-co-glycolide).
Liposomes, cationic lipid DNA and polymer complexes have been used as nonviral delivery carriers by complexing with DNA [34,35]. Nanoparticles can encapsulate various types of therapeutics including low-molecular-weight drugs [36,37] and macromolecules (e.g., proteins and DNA). Liposomes bind to cell membranes and are internalized via endocytosis with pH- sensitive liposomes being more efficient [38,39]. The formulation of pH-sensitive liposomes with phosphatidylethanolamine increases affinity to adhere to cell membranes due to the poor hydration of its head groups leading to aggregate formation [40,41]. Other liposome examples include thermosensitive liposomes, which allow temperature-sensitive release of drug [42–50]. Development of drug carriers is still in progress to overcome cytosolic barriers, including biodegradable polymeric carriers for controlled release [51,52].
Conjugating antibodies to either liposomes or polymers increases internalization via a receptor-mediated endocytotic process [53,54]. Others have targeted ligands to their respective cell-surface receptors (folate receptor [55], transferrin receptor [56], low-density lipoprotein receptor [57] and many other ligand-receptor-mediated methods [58]) for endocytosis and eventual release into the cytoplasm.
It may be desirable to retain a protein or peptide, once inside a cell, in the cytoplasm, where it may interact with its target (e.g., a signal transduction protein or receptor). Proteins smaller than approximately 45 kDa can passively diffuse into the nucleus; exclusion from the nucleus (hence cytoplasmic localization) can also be conferred by increasing the size of the gene therapy protein to over 60 kDa [59]. Such large proteins cannot traverse the nuclear pore complex (NPC) passively, and require NLSs for entry into the nucleus via the NPC. Proteins, peptides and DNA may be tagged with amino acid sequences that confer nuclear export (using a nuclear export signal [NES]) to achieve this goal, or in the case of a gene, the NES may be encoded by plasmid DNA and genetically engineered to the therapeutic gene. Our laboratory uses the latter to confer cytoplasmic localization to engineered proteins (Table 1) [5–7,60]. NESs are composed of sequences that are leucine rich, approximately 10–12 amino acids in length. Proteins with NESs are exported out of the nucleus by the classical export receptor, CRM-1 or exportin-1 (Figure 2A) [59]. A common consensus NES is LX (1–3) LX (2–3) LXJ where L is leucine, X is a spacer (numbers in parenthesis indicate number of amino acids in the spacer) and J is leucine, valine or isoleucine [6,7, 60].
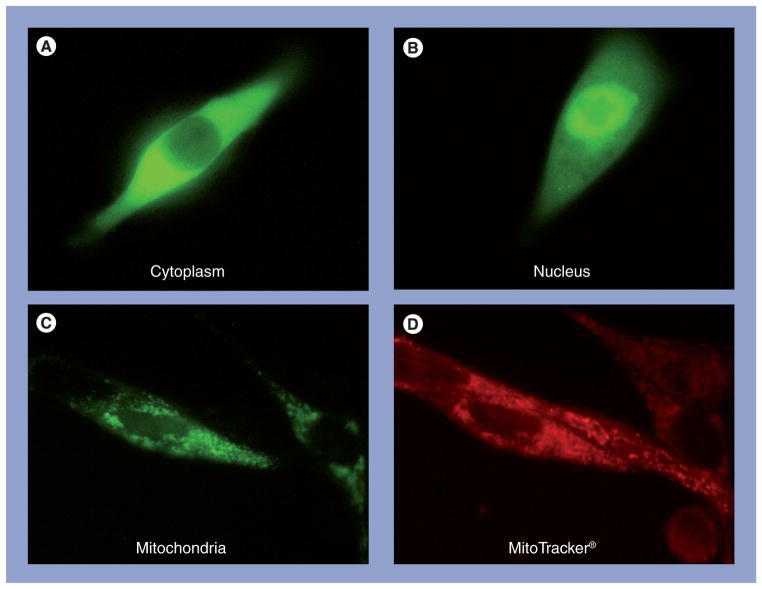
Figure 2. Enhanced green fluorescence protein fused to different targeting signals and transfected into 1471.1 murine adenocarcinoma cells.
(A) Nuclear export signal (HIV NES) delivers enhanced green fluorescence protein (EGFP) to cytoplasm. (B) Nuclear localization signal (MycA8 NLS) delivers EGFP to nucleus. (C) Mitochondrial targeting signal (orthinine transcarbamylase MTS) delivers EGFP to mitochondria. (D) MitoTracker® (Invitrogen) stains mitochondria in live cells.
The endosome/lysosome
Endosomal/lysosomal barriers
Drugs that have entered cells via endocytosis (and need to be delivered to the cytosol) are faced with a third obstacle: late endosomal/lysosomal degradation. The process of endocytosis starts at the cell surface. The material to be internalized gets encapsulated by a small portion of the plasma membrane (clathrin-coated pit formation), followed by a pinching off to form an endocytic vesicle. In the case of pinocytosis, some vesicles may originate at caveolae (instead of clathrin). Receptor-mediated endocytosis is a common mechanism for endocytosis of drugs/drug carriers. Endocytosed material that is not retrieved from endosomes (in the case of recycled receptors, for example) is destined for the lysosome [19]. Lysosomes contain hydrolytic enzymes for digestion of phagocytosed materials, and macromolecules (derived intra- or extra-cellular), and even for production of nutrients [19].
The classic example uses PEI for endosomal escape [61]. PEI’s secondary and tertiary amines are protonated in the acidic environment of the endosomes. The ‘proton sponge effect’ causes osmotic swelling and rupture of the endosomes [62]. The main drawback of PEI is its toxicity [63,64], but many modifications of PEI have been made in an attempt to circumvent this [65–69].
Many other techniques to escape the endosome (hence bypassing degradation) have been investigated. These include the development of pH-sensitive liposomes and polymers, where they switch from a membrane-inert (pH 7.4) to a membrane-disruptive (under acidic conditions) conformation [70]. This facilitates a destabilization of the endosomal membranes, resulting in release of the encapsulated therapeutic in the cytoplasm (reviewed in [37]). Furthermore, membrane-disruptive polymers masked by PEG via disulfide groups and acid-degradable acetal groups disrupt the endosomal membrane when the acidic pH of the endosome degrades the acetal groups unmasking the membrane-disruptive backbone [71]. Subsequently, the disulfide groups are reduced in the cytoplasm releasing the conjugated drug. Another strategy is to use membrane-disruptive peptides mimicking the viral mechanism of endosomal escape. These peptides contain acidic residues that prevent the formation of an α-helix when unprotonated, but under slightly acidic pH the peptide forms an α-helix that allows multi-merization and protein interaction, leading to endosomal escape.
Endosomal/lysosomal targeting
A drug may also be targeted to the endosome/lysosome directly for a therapeutic effect. There are over 40 lysosomal storage diseases that occur as a result of lysosomal enzyme deficiency, which allow various proteins, lipids and carbohydrates to accumulate in the lysosomes. These diseases usually manifest as neurodegenerative, but can be treated with enzyme-replacement therapy (reviewed in [72]). Drug delivery to endosomes has been achieved by targeting cell-surface receptors (mannose-6 receptor, reviewed in [73] and the IGF-II/cation-independent mannose 6-phosphate receptor [74]) for receptor-mediated endocytosis.
Nucleus
Transport through the NPC
Nucleocytoplasmic exchange occurs via pores formed by NPCs embedded in the nuclear envelope [75]. The 125-MDa NPC is the gatekeeper for nuclear entry, and the central role of this complex is confirmed by the high level of conservation among all eukaryotes [76–78]. This complex regulates all trafficking into and out of the nucleus, including passive diffusion of molecules smaller than 9 nm in diameter (<40 kDa) and active transport of molecules between 9 and 40 nm in diameter (40 kDa to 60 MDa), and has an estimated ability to translocate 1000 molecules per second [79–81]. Cytoplasmic filaments, a central channel and a nuclear basket give the NPC a tripartite structure constructed from approximately 100 nucleoporins (Nups) [82–84] (reviewed in [5]). The long cytoplasmic filaments project into the cytoplasm and interact with karyopherins (family of transport receptors) and deflect nonshuttling proteins [85–88]. The central channel is a cylindrical intramembrane transporter (central aqueous channel) with a 9 nm diameter pore [89–91] and is anchored to the nuclear membrane via eight spokes. The nuclear basket consists of eight long filaments projecting into the nucleoplasm, which are connected distally by a ring.
While molecules that are small enough to fit through the 9-nm pore in the central channel can enter the nucleus passively, larger molecules must be escorted through the NPC by karyopherins. Karyopherins, such as importin α, recognize and bind specific amino acid sequences termed NLSs [59,92–95]. Classical NLSs are monopartite with a single stretch of amino acids similar to the NLS found in SV-40 large tumor antigen (PKKKRKV; critical residues underlined) [96], or a consensus of K(R/K)X(R/K) [97] (Figure 2B). Bipartite NLSs (two short amino acid sequences with a spacer in between) have also been identified in proteins such as nucleoplasmin (KRPAATKKAGQAKKKKLDK) [98]. Classical NLS sequences are recognized by importin α [99,100], which binds to the HEAT repeats (helical repeats of histidine, glutamic acid, alanine and threonine) of importin β [101] through an importin β binding domain [102]. Once this ternary complex is formed, importin β mediates the translocation of the complex into the nucleus through interactions with FG (F: Phe; G: Gly) amino acid repeats of Nups in the NPC [103]. Inside the nucleus the complex dissociates when RanGTP binds to importin β [104], and both importin α and importin β are escorted separately back to the cytoplasm by RanGTP [100,105,106]. In the cytoplasm, RanGAP catalyzes the conversion of RanGTP to RanGDP, and importin α and importin β are ready for another cycle of import.
Challenges of nuclear trafficking
It is not a simple task to diffuse through the highly viscous cytosolic fluid. DNA over 2 kb is almost immobile in the cytosol, and DNA over 250 bp has reduced lateral mobility [107,108]. Nevertheless, a mechanism to overcome the challenge of diffusing through the cytosol is demonstrated by viruses that use active transport along the microtubule cytoskeleton [109–112]. Another challenge in nuclear targeting is the translocation through the nuclear envelope, which has been described as one of the limiting steps for nonviral gene delivery [113]. The midplane of the pore in the NPC is the narrowest and is estimated to be approximately 40 nm in diameter [114]. Thus, the largest molecule able to fit through this pore and enter the nucleus is roughly 40 nm, an estimate that has been confirmed (39 nm) using gold nanoparticles coated with NLSs [115]. The 36-nm capsid from hepatitis B can also transport through the NPC into the nucleus without dissociating [115], further demonstrating the capabilities of the NPC and validating the 40-nm size limitation. However, plasmid DNA in complex with polylysine crosslinked with NLSs, 60 nm in diameter, has been shown to enter the nucleus [116,117], likely due to the increased flex-ibility of this complex versus the more rigid gold nanoparticles. Molecules larger than 40–60 nm in diameter, regardless of containing a NLS, will be unable to enter the nucleus [116,117].
Methods of NLS incorporation
Various methods of incorporating a NLS into the therapeutic have been attempted (reviewed in [113,118]). For peptide/protein therapeutics, genetic engineering provides a facile method of incorporating the NLS as we have recently demonstrated with the oncoprotein Bcr-Abl, which causes CML [4]. However, for nonpeptide/protein therapeutics, the attachment of the NLS is no trivial matter and can result in drastically different results. As gene therapy is one of the most extensively researched areas in nuclear targeting, Table 2 provides examples of various methods of linking NLSs to DNA for gene therapy.
Table 2.
Methods to link nuclear localization signals to DNA-based therapeutic agents.
| Type of association | Description | Ref. |
|---|---|---|
| Electrostatic | NLS in complex with DNA | [361–365] |
| Electrostatic | NLS–PLy in complex with DNA | [366] |
| Electrostatic | M9–ScT in complex with DNA | [367] |
| Electrostatic | NLS–PNA in complex with DNA | [134,368–371] |
| Electrostatic | Triplex formation between padlock oligonucleotide with NLS and DNA | [372] |
| Electrostatic | NLS–streptavidin bound to biotinylated DNA | [373] |
| Covalent (random) | N3–adenine adduct via CPI–NLS | [120] |
| Covalent (random) | Photoactivation of p-azido-tetrafluoro-benzyl–NLS | [121] |
| Covalent (random) | Diazo coupling to increasing lengths of PEG–NLS | [122] |
| Covalent (specific) | Crosslinked triple helix with psoralen-oligonucleotide | [124] |
| Covalent (specific) | Attachment to hairpin of linear DNA | [125,126,128] |
| Covalent (specific) | Attachment to PCR primer | [126,127] |
CPI: Cyclopropapyrroloindole; NLS: Nuclear localization signal; PEG: Polyethylene glycol; PLy: Polylysine; PNA: Peptide nucleic acid; ScT: SV40 T-antigen consensus NLS.
Of these approaches, electrostatic interactions are the simplest, but are not without drawbacks. One potential problem is the dissociation of the complex in the cytosol, leaving the DNA without the nuclear targeting signal. Furthermore, as most electrostatic interactions with DNA are not sequence specific, the interactions may interfere with the transcription of the gene after being delivered to the nucleus. To circumvent this problem, peptide nucleic acid with a NLS has been used to interact with the DNA in a sequence-specific manner in a region other than the gene of interest [119], but only achieved modest improvements. Numerous attempts to improve efficiency through covalent attachment of the NLS have been attempted, but many have failed to demonstrate improved nuclear translocation and gene expression [120–123]. However, initial attempts to covalently attach the NLS to the DNA did not control where on the DNA strand the NLS was attached and may have resulted in the NLS preventing the efficient transcription of the gene of interest.
Further attempts were then made to attach the NLS to DNA upstream or downstream from the gene of interest to avoid interference with transcription, but did not achieve the anticipated results. The triple helix with photoactivation attempted by Neves et al. [124], the conjugation to the hairpin attempted by Tanimoto et al. [125] and linear DNA amplified via PCR with NLS-conjugated primers [126,127] all demonstrated a lack of transfection efficiency, and even a lack of nuclear tanslocation. However, one study has shown that covalent attachment of a NLS to a hairpin at the 3′-end of linear DNA can enhance transfection anywhere from 10- to 1000-fold depending on the cell type [128], but similar schemes did not achieve the same result by others.
Therapeutics targeting the nucleus
Pharmacological agents that alter the nuclear translocation (either inhibit or induce translocation) also provides a means for therapeutic intervention [129]. Inhibition of the NPC through binding FG amino acid repeats by antibodies has been used to prevent nuclear accumulation [130] but is not specific and inhibits all protein translocation into the nucleus. These antibodies, RL2 and mAb414, are further limited by complications with delivery of an antibody inside a cell. Wheat germ agglutinin is a lectin that binds to N-acetylglucosamine common to certain Nups and also inhibits general nuclear transport through the NPC [131,132]. Kosugi et al. have also demonstrated that nuclear translocation can be inhibited through two peptides, bimax1 and bimax2, that bind to importin α [133]. The inhibition of the NPC reduces nuclear transport and results in reduced nuclear localization, while the inhibition of nuclear export can increase the nuclear accumulation of proteins. Leptomycin B (LMB) is a general nuclear export inhibitor that binds to CRM-1 [134–136], a protein that escorts other proteins with NESs from the nucleus to the cytoplasm. Although LMB has antitumor properties, it was also found to be highly toxic and cannot be used clinically. Recently, Mutka et al. have identified LMB analogs that retain the potency of LMB, are better tolerated and have shown potential as cancer therapeutics in mouse xenograft models [137]. Still, inhibiting the general nuclear import or export of all proteins may be limited as a therapeutic approach and methods to target specific proteins would be a better alternative.
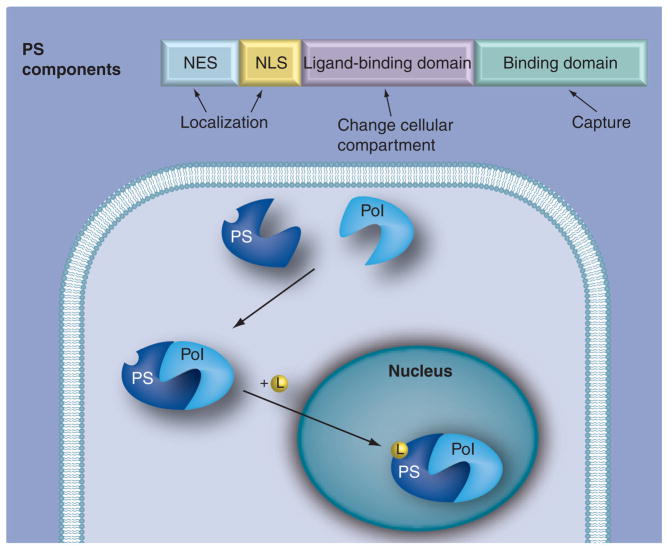
An example of therapeutic intervention through altering the nuclear localization of a specific protein is the use of peptides that bind nuclear factor-κB (NF-κB) and prevent its nuclear translocation [138,139]. The misregulation of the transcription factor NF-κB has been associated with cancer and autoimmune diseases, both of which potentially could be treated by inhibiting the nuclear accumulation of NF-κB [140]. A similar approach of inhibiting nuclear translocation through binding with a peptide has been demonstrated for nuclear factor of activated T cells [141]. Moving proteins from the cytoplasm into the nucleus has also been demonstrated through the use of protein aptamers containing a NLS [142]. We have also developed a sophisticated chimeric protein we have termed a protein switch (Figure 3), for controlled nuclear transport [6,7, 60]. This protein switch (containing both a NES and an inducible NLS) localizes to the cytoplasm, but upon the addition of a ligand, it translocates into the nucleus. This controlled nuclear translocation can be used to alter nuclear localization of endogenous proteins; attempts to do so are currently underway in our laboratory.
Figure 3. Protein switch mechanism.
The PS, shown schematically (top diagram), consists of a NES, NLS, ligand-binding domain and dimerization domain. When PS plasmid is transfected into cells, the expressed PS captures a PoI in the cytoplasm. Upon addition of ligand, the PS–PoI complex translocates to the nucleus. L: Ligand; NES: Nuclear export signal; NLS: Nuclear localization signal; Pol: Protein of interest; PS: Protein switch.
Targeting the nucleolus
A subcellular compartment such as the nucleolus presents additional challenges in identifying specific targeting sequences as it exists in a highly dynamic equilibrium with the nucleoplasm and is not enclosed by a membrane. The nucleolus has been described as a machine for ribosome production and is a dense area composed of nucleolar organizer regions (loops of DNA containing genes encoding rRNA), rRNA, ribosomal proteins, ribosomal-binding proteins, small ribonucleprotein particles and RNA polymerase I. The nucleolus typically exhibits fibrillar centers, fibrillar components and granular components. The fibrillar centers are regions where transcription does not take place, whereas the fibrillar components are more dense regions where transcription is underway. The granular components are regions where the ribosomal precursor particles are undergoing maturation.
Various sequences (reviewed elsewhere [143]) with as few as seven amino acids [144] have been identified that can be used to direct a protein to the nucleolus. The nucleolus localization signals (NoLSs) are very similar to the arginine/lysine-rich NLS sequences, which is easy to conceive owing to the necessity to first be transported into the nucleus before targeting the nucleolus. However, there is a distinction between NLSs and NoLSs as demonstrated through deletion analysis of the NoLS in the ORF57 protein (among others), resulting in diminished nucleolar localization while retaining nuclear localization [145]. Through alignment of various proteins containing NoLSs, Weber et al. identified a common NoLS motif (R/K)(R/K)X(R/K) [146]. This highly conserved sequence was also noted by Horke et al. after finding it to be important for nucleolar localization in the human La protein [147]. Although there is still not a consensus NoLS and nucleolar targeting is not as well characterized as other signals, the addition of short NoLS sequences has been demonstrated to direct proteins to the nucleolus [144,148], validating their use in targeting the nucleolus.
Proteins without an identifiable NoLS have been shown to localize to the nucleolus via interactions with other molecules at the nucleolus. One such example is nucleolin, a protein that may localize to the nucleolus partially due to RNA binding. However, the RNA binding domains are not sufficient to cause nucleolar localization of chimeric proteins [149]. Additionally, NoLS-containing proteins, such as NPM [150] and NOM1 [151], have been shown to bind and cause nucleolar localization of proteins that do not contain a NoLS, further expanding the mechanisms for nucleolar localization. Emmott and Hiscox have recently proposed that nucleolar hub proteins play an essential role in nucleolar localization [145]. Thus, nucleolar targeting can be achieved through NoLSs, by being dragged by a NoLS-containing protein, or potentially by binding to a nucleolar hub protein.
There are relatively few drugs that target the nucleolus or nucleolar components specifically, but actinomycin D has been shown to induce nucleolar localization due to the inhibition of rDNA transcription [152,153]. Phosphorylation is a critical modification in the regulation of nucleolar proteins; indeed, kinase inhibitors have drastic effects on the nucleolus [154–156]. One such inhibitor, the casein kinase inhibitor 5,6-dichloro-1-ribo-furanosylbenzimidazole, causes the nucleolus to disassemble [157]. An example of a more specific interaction involving a potential nucleolar targeting therapeutic is the peptide consisting of amino acids 26–46 of the p19ARF protein [158]. This peptide, modified with additional arginine residues to increase cellular uptake, has been shown to bind Foxm1b and send it to the nucleolus where it is unable to function as a transcription factor. Foxm1b has been shown to have a key role in the development of hepatocellular carcinoma [159], and the nucleolar sequestration of Foxm1b presents a novel therapeutic intervention.
Mitochondria
Mitochondria contain a double membrane composed of phospholipid bilayers with proteins embedded in them. This results in two aqueous spaces; the matrix and the intermembrane space. The inner membrane contains the proteins involved in the respiratory chain complex, ATP synthase and protein import machinery. The human mitochondrial matrix encloses a small genome (mtDNA) coding for 13 hydrophobic proteins, 22 tRNAs and two rRNAs [160,161]. The 13 hydrophobic proteins encoded in the matrix are all involved in the electron transfer system. The matrix is also the site for the citric acid cycle, urea cycle and fatty acid oxidation. Therefore, mitochondrial dysfunction contributes to a range of human diseases including obesity, diabetes and cancer. Mitochondrial targeting is mainly performed to interrupt mitochondrial function including energy production, oxidative stress and the apoptotic pathway.
Mitochondrial function
Mitochondria maintain an acidic inner space and an electrochemical potential across the inner membrane, which are utilized by the electron transport system to transfer electrons to oxygen. The electron transport chain passes electrons from the reducing equivalents (flavin adenine dinucleotide and nicotinamide adenine dinucleotide) to oxygen. During this process, protons are pumped from the matrix to the intermembrane space via NADH dehydrogenase, cytochrome c reductase and cytochrome c oxidase. As a result, an electrochemical gradient is established, which activates ATP synthase to pump protons back in and activates ADP to ATP conversion as the energy source for the cell [162].
In the mitochondrial respiratory chain, oxygen is partially reduced to form reactive oxygen species (ROS), which activate proton leak uncoupling proteins that pump protons back into the matrix without forming ATP [163–165]. Superoxides are also converted to other ROS such as hydroxyl radicals, which contribute to a number of degenerative diseases [166–170]. The oxidative damage, which increases with aging, also affects lipids, proteins and DNA, leading to a decline in the efficiency of oxidative phosphorylation [167,171]. Mitochondria destroy the free radicals using antioxidants (e.g., vitamin E, ascorbate and ubiquinol), which scavenge ROS converting them to less reactive species or prevent oxidative damage. Therefore, antioxidants have been used as supplements to specifically target the mitochondria (reviewed elsewhere [172]).
Apoptosis is frequently triggered through the mitochondria after collapse of the inner transmembrane potential, disruption of electron transport and ATP production, oxidative stress, permeability transition pore opening or mitochondrial swelling with outer membrane rupture. When the outer mitochondrial membrane undergoes permeabilization, cytochrome c is released from the intermembranous space into the cytosol activating caspase-3 via the Apaf-1 pathway [173–175]. Mitochondrial outer membrane permeabilization is commonly disabled in cancer cells and hence its pharmacological induction constitutes a therapeutic goal [176]. Bcl-2 and Bcl-XL are mitochondrial proteins that inhibit apoptosis by inhibiting Bax and Bak oligomerization [177–181].
Mitochondrial import machinery
Drugs targeting mitochondria are necessary to induce apoptosis in cancer cells as well as to protect cells from oxidative damage and to repair defects. The outer membrane of the mitochondria allows diffusion of small molecules through pores formed by the spanning β-barrel protein porin. Simple ions with localized charge such as Cl+, Na+ or Ca2+ require translocators or energy-dependent transporters to allow them to cross into the matrix (reviewed in [182]). However, ions with delocalized charge and cationic hydrophobic molecules such as triphenylphosphonium (TPP) can diffuse across the mitochondrial membrane taking advantage of the hydrophobic nature of the membrane [183–185]. Conjugating antioxidants to TPP or a methyl derivative increases their accumulation within the mitochondria and selectively blocks mitochondrial oxidative damage (Table 3). TPP cation has been covalently attached to antioxidants such as ubiquinol (MitoQ®) [186–188] and α-tocopherol (MitoE®) [189]. The same concept has been utilized to target DNA to the mitochondria using dequalinium, a delocalized cationic lipid [190]. It crosses the plasma membrane by endocytosis, and then DNA is released upon interacting with the mitochondrial membrane [191].
Table 3.
Mitochondria targeting signals/motifs and delivered therapeutic agents.
| Targeting motif | Therapeutic | Ref. |
|---|---|---|
| (2-oxo-ethyl)-triphenyl-phosphonium | Nitroxide (4-amino-2,2,6,6-tetramethyl-piperidine-1-oxyl) | [374] |
| Rhodamine β | Porphyrin | [375] |
| Stearyltriphenyl phosphonium | Liposome-based nanocarrier containing ceramide | [376] |
| Triphenylphosphonium | Ubiquinol antioxidant | [183] |
| Dequalinium | DNA | [190] |
| MLSCTSPLLRGACHNMGAAKALRLRWTVPPAVLIALG SGALYTTSGQTLYYKNSVQQTD | Phospholipase A ortholog (AoPlaA) | [377] |
| MLSRAVCGTSRQLAPALGYLGSRQ | Protein transduction domain of HIV-1 TAT protein | [378] |
| MSATRMQLLSPRNVRLLSRGRSELFAGGSGGGPRVRSLISP PLSSSSPGRALSSVSATRRGLPKEKMTENGVSSRAKVLT IDT | Alanine aminotransferase | [379] |
| MLFNLRILLNNAAFRNGHNFMVRNFRCGQPLQ | Tumor suppressor p53 | [212] |
| MLFNLRILLNNAAFRNGHNFMVRNFRCGQPLQ | Dihydrofolate reductase | [213] |
Large molecules (e.g., proteins) exploit the mitochondrial protein import apparatus to cross the outer and inner membrane. The TOM complex (translocase of the outer membrane of mitochondria) is the molecular machine responsible for translocating proteins across the mitochondrial outer membrane. The TOM complex contains receptor subunits, Tom70 and Tom20, which recognize proteins destined for import [192,193]. Other TOM complex components, Tom40, Tom22, Tom7, Tom6 and Tom5, assist the transfer of the protein into the intermembrane space [194–196]. The TIM complex (translocase of the inner membrane of mitochondria) binds to proteins destined for localization to the inner membrane and the matrix through TIM22 and TIM23, respectively [194,197]. The TIM22 complex translocates proteins depending on the electrochemical potential across the inner membrane. However, the TIM23 complex drives the protein trafficking via a motor complex built around a mitochondrial heat shock cognate protein 70 [193]. Mitochondrial targeting signals (MTSs) are mainly N-terminal cleavable amino acids 15–40 residues in length, which are positively charged with a notable absence of negatively charged residues [198]. These MTSs forming amphipathic α-helices are thought to be important for their recognition by the translocation machineries in the mitochondrial outer (TOM complex) and inner (TIM complex) membranes [193,197,199–202]. Once the protein is translocated into the matrix, the targeting signal is proteolytically removed by mitochondria processing peptidase [203,204]. Nevertheless, a significant fraction of mitochondrial proteins, especially proteins of the outer membrane, the inner membrane space and the inner membrane, lack typical N-terminal sequences and are targeted to the mitochondria by means of internal, noncleavable signals known as ‘carrier sequence motifs’ [205,206]. These internal signals resemble the N-terminal sequence and are recognized by the TOM machinery [207–209]. The internal signals function in combination with a preceding hydrophobic region [210].
Attaching MTSs to essentially any protein, DNA or RNA enables mitochondrial targeting [211–215] (Figure 2C & D). MTS has also been fused to restriction enzymes such as Sma1 endonuclease to degrade mutant mtDNA in neuropathy, ataxia and retinitis pigmentosa (NARP) disease [216]. Targeting proteins such as p53 to the mitochondria induces apoptosis by complexing with Bcl-XL proteins. The inactivation of Bcl-XL induces conformation change and oligomerization of the BH1,2,3 effector protein Bak and Bax, which then forms a pore in the outer membrane facilitating the release of cytochrome c [217–219]. We are currently investigating the fusion of a strong NES to small proteins tagged with MTS to reduce nuclear localization and increase their availability in the cytoplasm to target the mitochondria [Mossalam M, Opper K, Lim CS, Unpublished Data]. The effect of the different subcellular signals in a protein and the outcome of having multiple signals is a largely unexplored area, and warrants attention. Table 3 lists examples of chemical (TPP) and biological (MTS) means to target therapeutics to the mitochondria.
Endoplasmic reticulum
The ER is an organelle found in all eukaryotic cells. Its membrane represents as much as half of the total membrane of an average animal cell. It is continous with the nuclear envelope and extends to the cell periphery intertwining with most cellular organelles, including the mitochondria, peroxisome and the Golgi apparatus [220]. Regions of the ER that are coated with ribosomes are called rough ER, where proteins are imported into the ER in a cotranslational process. In cotranslational transport, one end of the protein is translocated into the ER while the rest of the protein is being assembled in the ribosome. Smooth ER is the region that lacks bound ribosomes. An essential function of the ER is the biosynthesis of proteins and lipids that are destined for intracellular organelles and the cell surface [221]. It also controls Ca2+ signaling via its Ca2+-binding proteins and homeostasis [222].
ER targeting
The cotranslational targeting of proteins to the ER membrane (transmembrane proteins) and lumen (water-soluble proteins) is mediated by cytosolic ribonucleoproteins called signal recognition particles (SRPs) and their cognate membrane-associated receptors [223–225]. One end of the SRP binds to the ER signal sequence as they emerge from ribosomes, while the other end of the SRP blocks the translational elongation in the ribosome halting protein synthesis [226–229]. The signal sequence consists of 7–12 large hydrophobic residues that presumably form an α-helix [229–233]. The SRP–ribosome complex is then directed to the ER membrane by binding to the SRP receptor, which is an integral membrane protein complex embedded in the rough ER membrane [224,234–237]. This binding releases the ribosome complex to the integral membrane protein Sec61 translocation complex (translocon), allows the translational elongation to continue and recycles the SRP back to the cytosol [238,239].
The ribosomal exit tunnel is aligned to a water-filled pore in the translocon through which the protein is translocated and continues being translated. Subsequently, the signal sequence is cleaved via an ER signal peptidase and released into the membrane, where they get degraded by other proteases. The translocon also allows a translocating protein lateral access into the hydrophobic core of the membrane for both integration of membrane proteins into the bilayers (via either a stop-transfer sequence or a signal-anchored sequence) and the release of the cleaved signal peptide into the membrane (for reviews see [240,241]). The ER is not limited to cotranslational targeting of proteins; some post-translational proteins are imported into the ER in a SRP-independent mechanism, where they depend on the hydrolysis of ATP and the binding to cis-acting molecular chaperones such as heat shock cognate protein 70 [242–247]. The signal sequences in this category are no more than 70 amino acid residues in length [245,248].
The ER signal sequences have substrate-specific differences, which may have functional consequences [249,250]. The signal sequences may differ in their gating of the translocation complex [251,252], dependency on the translocon-associated proteins [253,254], translocation efficiency of proteins [255–257] or sensitivity to translocation inhibitors [258,259]. Table 4 lists examples of ER signal sequences fused to therapeutic proteins.
Table 4.
Endoplasmic reticulum targeting signals/motifs and delivered therapeutic agents.
| Targeting motif | Therapeutic | Ref. |
|---|---|---|
| MDSKGSSQKAGSRLLLLL VVSNLLLCQGVVSTP | Mammalian prion protein | [380] |
| ALAAALAAAAA | G-protein-coupled receptors | [381] |
| MRVLVLLACLAAASNA | Recombinant proteins in baculovirus expression vector system | [382] |
| MLLPVPLLLGLLGLAAAL and KDEL (ER retention) | Human papilloma virus-16 E7 antigen | [383] |
| MRYMILGLLALAAVCSAA | Vesicular somatic virus nucleocapsid protein and influenza virus nucleoprotein | [384,385] |
| MKFTVTFLLIICTLSAFC | Adenovirus type 5 E3 14.5-kD protein | [386] |
| METDTLLLWV LLLWVPGSTGD | TGF-β2 and -β3 | [387] |
ER: Endoplasmic reticulum.
ER function
Nearly a third of the eukaryotic genome is processed through the ER [260]. The transferred transmembrane proteins either function in the ER or reside in the membrane of other organelles or the plasma membrane. Similarly, the water-soluble proteins are either secreted to the cytosol or transferred into the lumen of other organelles. Transmembrane proteins directed to the ER include plasma and organelle membrane receptors and channels that regulate metabolic pathways, regulate cell-to-cell communication and flow of ions and solutes, and mediate protein and lipid uptake from the surrounding cellular environment. In addition, secreted proteins and enzymes are required for cell communication with its surroundings and to support sorting, metabolic and catabolic activities [261]. Therefore, a wide range of diseases occur owing to mistakes in protein handling in the ER such as cystic fibrosis, liver failure, Alzheimer’s disease, Parkinson’s disease and diabetes mellitus [262–270] (for a list of diseases see elsewhere [261]).
The Golgi apparatus
The Golgi apparatus is known typically for post-translational modifications and shipping macromolecules to the plasma membrane, lysosomes or outside of the cell in secretory vesicles. Thus, the Golgi apparatus ships molecules in the opposite direction to drug delivery. Major players in this process, such as mannose 6-phosphate receptors, are recycled back to the trans-Golgi network in a retrograde fashion [271–273], demonstrating the potential for use in therapeutic targeting of the Golgi apparatus. However, this recycling pathway involves late endosomes [271,274,275] with the associated low pH and degradative enzymes that therapeutic delivery systems may want to avoid. However, retrograde delivery to the Golgi apparatus directly from early endosomes or recycling endosomes has been characterized with the nontoxic targeting subunit of toxic proteins such as Shiga and cholera toxins [276,277]. The receptor for these toxins is a glycolipid (globotriaosyl ceramide) that uses a pH-independent pathway [277] to target the Golgi apparatus and may have therapeutic potential. While clathrin is critical for efficient transport of Shiga toxin [278], ricin has been shown to transport to the Golgi apparatus independent of clathrin and Rab9-GTPase [279] in a process regulated by cholesterol [280]. Other proteins have also been shown to shuttle between the plasma membrane and the Golgi apparatus. One such example is a protein commonly used as a marker for the trans-Golgi network named TGN38/41, a receptor for p61 protein complexes and GTP-binding proteins, important in the formation of exocytic vesicles [281]. Other examples are furin [282] and carboxypeptidase D [283].
The signaling sequences used by these proteins to target the Golgi apparatus are not well characterized, and no specific consensus sequence has been proposed. However, tyrosine-containing motifs such as that found in TGN38/41 (SDYQRL) is one signal responsible for Golgi apparatus localization. Attachment of this signal to the low-density lipoprotein receptor has resulted in localization to the Golgi apparatus [284]. It has been shown that furin has two specific signals that target the Golgi apparatus: the acidic sequence CPSDSEEDEG, which is sufficient to cause localization to the Golgi apparatus; and the tyrosine-containing sequence YKGL, which has been proposed to function as a retrieval signal through targeting of endosomes [285,286]. The localization of furin to the Golgi apparatus, and its shuttling to and from endosomes, is further dependent on phosphorylation by casein kinase II at serine residues in the acidic cluster motif, and dephosphorylation by protein phosphatase 2A [287,288], highlighting the role of post-translational modifications on localization and not just specific amino acid sequences. A similar mechanism for targeting the Golgi apparatus via a tyrosine motif and a phosphorylation site has been demonstrated for the varicella-zoster virus glycoprotein I [289]. While sequences targeting the Golgi apparatus have been studied and identified, little effort has been put forth to harness these signals for therapeutic delivery to the Golgi apparatus, leaving much to be explored.
Although the Golgi apparatus may not be the target of the therapeutic, delivery of therapeutics via the B subunit of Shiga toxin, which enters the cell through the retrograde pathway involving the Golgi apparatus, have been studied for vaccination, targeted killing of cancer cells and imaging of cancer cells. Although the mechanism has not been delineated entirely, the MHC class I pathway involves the retrograde pathway through the Golgi apparatus, and Shiga toxin subunit B (STB) or Shiga-like toxin subunit B (SLTB) thus has been conjugated to various antigens for tumor protection [290–294]. The receptor that binds ST/SLT is the globotriaosylceramide receptor found to be overexpressed on many tumor cells, allowing the retrograde pathway with ST/SLT or STB/SLTB to be used for tumor imaging [295] and targeted delivery of cytotoxic agents for colon [296], ovarian [297] and breast cancer [298], as well as lymphoma [298,299], astrocytoma [300] and meningoma [301]. Finally, since the Golgi apparatus has been described to exhibit a mechanism for stress-induced initiation of apoptosis [302], this validates future attempts at targeting therapeutics to the Golgi as a mechanism for specific induction of apoptosis in malignant cells.
Peroxisomes
The peroxisomes are multifunctional, single-membrane enclosed, spherical vesicles distributed throughout the cytoplasm [303]. Their numbers vary in different cell types and under different stimuli. The term ‘peroxisome’ was coined due to the fact that hydrogen peroxide is formed and degraded in the organelle. Peroxisomes are responsible for a wide variety of biochemical and metabolic pathways, with implications for human health. Aging and several diseases are associated with dysfunction of the peroxisomes, which has made it an interesting pharmaceutical target.
Peroxisomal function
A major function of the peroxisome is the breakdown of a variety of fatty acids via α- and β-oxidation reactions. Similar to mitochondrial β-oxidation, fatty acids are broken down two carbons at a time in the form of acetyl-CoA. However, fatty acids containing a methyl group at the three-carbon position must be modified before entering the peroxisomal β-oxidation pathway [304]. Many of the metabolic pathways in the peroxisomes lead to hydrogen peroxide production, which is subsequently metabolized by the peroxidase catalase. Peroxisomes also play a role in the production of bile acids, docosahexanenoic acids and ether phospholipids.
Peroxisomal import machinery
The import machinery to the peroxisomal matrix requires:
Cargo containing specific targeting signals
Receptors that recognize specific signals
Membrane-associated import via docking and translocating proteins
Cargo release (reviewed elsewhere [305])
Cytosolic proteins require specific targeting signals recognized by receptors for peroxisomal targeting. Two types of peroxisomal targeting signals exist: type I (PTS1) and type 2 (PTS2). PTS1 is the most abundant, which consists of a tripeptide (SKL) or a conserved biochemical variant (consensus S/A/C-K/R/H-L/M) at the extreme C-terminus of the protein [306–308]. An additional adjacent upstream region to the PTS also influences the interaction between receptor and PTS [308–310]. By contrast, PTS2 consists of a less conserved consensus sequence (R/K-L/I/V-X5-Q/H-L/A, where X may be any amino acid) and is coded close to the N-terminus [311–313]. For a list of bona fide peroxisomal proteins and their PTSs, see [314].
Specific proteins called receptor peroxins (Pex5p and Pex7p) bind to the proteins harboring PTS in the cytosol, which then target the peroxisomal membrane as a receptor–cargo complex. PTS1 is recognized by Pex5p while Pex7p recognizes PTS2 [311,315–317]. Pex5p is retained in the cytosol in the tetramer form. Upon binding to proteins containing PTS1, Pex5p disaggregates into dimers [318]. Each dimer carrying two cargo proteins is then transported to the peroxisome. Subsequently, the receptor–cargo complex binds to membrane-associated peroxins (docking proteins), in particular Pex8p, Pex13p, Pex14p and Pex17p [319]. The remaining membrane-associated peroxins (Pex2p, Pex10p and Pex12p) form the RING–finger subcomplex. Both the docking proteins and the RING–finger complex form the putative import complex (importomer), which is thought to support translocation [320]. The precise mechanism for the peroxisomal protein import machinery remains ambiguous. The uniqueness in this mechanism is highlighted in its ability to transport folded, cofactor-bound and oligomeric proteins [321]. There are two proposed models on the receptor’s cycle between the cytosol and the peroxisome. The model of shuttling receptors states that the cargo dissociates from the receptor upon binding to the docking proteins [311,322]. The cargo is then translocated across the peroxisomal membrane while the receptor is released back to the cytosol. Alternatively, the extended shuttle hypothesis assumes that the dissociation between the cargo and receptor takes place in the peroxisomal matrix allowing the unloaded receptors to transport back to the cytosol [323–325].
Targeting the peroxisomal membrane (without translocating to the matrix) follows a different import mechanism. Peroxisomal membrane proteins (PMPs) require membrane protein targeting signals. These signals contain a cluster of basic amino acids in conjunction with one or more transmembrane regions downstream from it [326–329]. The membrane protein targeting signal is recognized by the Pex19p receptor in the cytosol, which then binds to Pex3p on the peroxisomal membrane. However, the exact mechanism on how PMPs are transported to the peroxisomal membrane is still unknown. There is also a possible but controversial involvement of the ER in PMP trafficking [305,330–332]. The importomer plays an important role for matrix targeting but not for membrane protein import.
Peroxisomal disorders are due to either mutations in peroxins (peroxisomal biogenesis disorder [PBD]) or deficiencies in peroxisomal enzymes (reviewed in [333]). PBDs are categorized by means of clinical severity into the Zellweger spectrum of disease (Zellweger syndrome, neonatal adrenoleukodystrophy) and infantile Refsum’s disease or rhizomelic chondrodysplasia punctata (RCDP) type I. For example, a defect in the Pex7p disrupts enzymatic pathways for enzymes containing PTS2 causing RCDP type I. In addition to peroxin mutations that affect enzymes delivery to the peroxisome, single peroxisomal enzyme deficiencies have been linked to a number of human diseases such as adult Refsum’s disease, X-linked adrenoleukodystrophy, RCDP type II and III, primary hyperoxaluria type I and acatalasemia (for a full list of diseases, see elsewhere [333]).
Peroxisomal targeting
Specific targeting to the peroxisome is of great clinical value to restore, alter or complement peroxisomal function. It could be used in the treatment of single enzyme deficiencies, PBD, as well as diseases associated with altered ROS [333]. Tagging protein therapeutics or peroxisomal enzymes to a PTS is required to achieve peroxisomal targeting. The carboxy-terminal PTS1 (SKL or related sequence mentioned previously) is better characterized and is easily tagged onto a protein of interest using standard recombinant molecular cloning techniques. The adjacent upstream region influences the receptor/PTS interaction and can be evaluated using a computer program [401], which can also predict the relative strength of a PTS1. To be recognized by Pex5p, accessibility of the PTS1 (not buried in the folded protein) is also crucial. Therefore, a spacer between the PTS1 on the carboxy terminal and the protein could be introduced. Table 5 lists therapeutic proteins delivered to the peroxisome via PTS1.
Table 5.
Peroxisomal targeting signals and therapeutics delivered.
Proteasomal function, inhibition & potential drug delivery
The proteasome is an ATP-dependent prote-ase that functions to remove (degrade) abnormal proteins found in the cytosol, nucleus or ER. The entire proteasome (26S proteasome) consists of the 20S proteasomal core, capped by two 19S regulatory subunits on each end. Polyubiquitination of proteins triggers degradation by the 26S proteasome complex [19]. The proteasome has become a popular target for drug therapy, since inhibiting the proteasome can be used for treatment of inflammatory diseases and cancer [334]; on the other hand, activation of the proteasome has therapeutic use in neurodegenerative diseases and cancer [335].
Synchronized synthesis and degradation of regulatory proteins is necessary for cells to function and progress through the cell cycle. In the case of tumor development, if the degradation of these proteins can be blocked, apoptosis will ensue. Rapidly dividing cancer cells are more susceptible to proteasomal inhibition since they have more disruptions in their normal regulatory pathways than noncancerous cells [336]. Bortezomib is the first small-molecule inhibitor of the ubiquitin-protease system to be approved for treatment of multiple myeloma [337,338]. While bortezomib targets the 20S subunit of the proteasome, many other drugs are being developed to target other components of the proteasome [339,340] and other components (ubiquitin ligases, ubiquitin-activating and -conjugating enzymes) of the proteasomal degradation pathway [341]. In addition, aberrant proteins could be sent to the proteasome for degradation. One focus of our laboratory is a gene therapy approach to capture oncogenic proteins and send them to the proteasome for degradation.
Conclusion & future perspective
Protein subcellular localization is behind a wide range of diseases including cancer (for a list of diseases and proteins that require specific intracellular targeting, see [5]). While unidirectional targeting of a therapeutic agent to single organelles has been well studied and utilized, multidirectional drug targeting, utilizing multiple signals, represents a more sophisticated level of targeting that mimics the complexity of nature. In nature, many signal-transducing proteins are not simply directed to one compartment of a cell. They may interact with other proteins in multiple compartments of a cell. For example, the p14/19 ARF protein can bind Mdm2 (a nucleocytoplasmic shuttling protein) to inhibit degradation of p53 by Mdm2. The p14/19 ARF protein also contains a nucleolar signal, which can re-direct the p14/19 ARF–Mdm2 complex to the nucleolus [342–344].
While we have already demonstrated that unidirectional targeting of an oncogene can dramatically alter its function [4], our ultimate goal is to utilize our protein switch technology to capture an endogenous protein in one compartment, and move it to another compartment [6,7]. Our laboratory is pursuing this approach for treatment of CML. Bcr-Abl, the causative agent of CML, is found in the cytoplasm of CML cells, where it sends oncogenic signals to other proteins in the cytoplasm. If endogenous Bcr-Abl can be captured and dragged to the nucleus of cells, apoptosis will ensue owing to loss of oncogenic signaling in the cytoplasm and gain of apoptotic function in the nucleus. Like nature, the protein switch was designed to regulate cellular proteins by changing their location and hence their function. The protein switch has the advantage of being regulated by an externally added ligand. The protein switch contains a dimerization domain (to capture the endogenous protein of interest), a NES (conferring cytoplasmic localization) and a ligand-regulated nuclear import signal. Upon addition of the ligand, the protein switch is designed to translocate from the cytoplasm to the nucleus and drag its dimerization partner with it.
Other groundbreaking studies have included the concept of delivering drugs to multiple compartments (across multiple barriers) by mimicking viral delivery. A review by Wagner discusses mimicking viral delivery of DNA to the cytoplasm, and into the nucleus [345]. There are even virus-mimetic nanogels that can deliver drugs to not only targeted cells, but also to neighboring cells [346].
The future of drug delivery to organelles lies in our ability to more closely mimic, or even improve on, nature. Spatial placement of signaling sequences in a protein, balancing the strengths of different signals against each other and the masking/unmasking of signals due to conformational changes in an engineered protein or therapeutic have not been fully explored or understood. The ability to harness genetic codes, signal sequences, targeting motifs or protein–protein interactions will lead to enormous complexity and diversity for drug delivery.
Executive summary.
For maximum therapeutic effect and minimal side effects, drugs need to be delivered to the appropriate location within the cell.
The cytoplasm and nucleus are the most widely targeted and well-studied organelles.
Cytosolic targeting is crucial before most drugs can reach any organelle within the cell.
Development of drug carriers to overcome barriers for cytosolic delivery and endosomal escape is still in progress.
Localization and export of proteins to and from the nucleus can also be blocked using molecules that inhibit either the import or export mechanism.
Gene delivery mainly targets the nucleus, while a few studies are targeting DNA to the mitochondria.
Targeting specific organelles is under investigation, especially the mitochondria owing to its role in oxidative stress and apoptosis.
Manipulating current therapeutics with specific targeting signals ensures accumulation in certain compartments within the cell.
Capturing and sending oncogenic proteins to the proteasome is a promising approach for cancer therapy.
Proteins synthesized at the endoplasmic reticulum are destined for intracellular organelles and the cell membrane.
Newer technologies (e.g., protein switch and virus-like delivery systems) mimic nature and allow for a more sophisticated approach to drug delivery. Harnessing different methods of targeting multiple organelles in a cell will lead to better drug delivery and improvements in disease therapy.
Key Terms
- Signal hypothesis
Proteins destined for movement across biological membranes contain amino acid sequences that may/may not be present in the mature protein
- Stealth liposomes
Liposomes designed with a surface coating, intended for prevention of liposome binding with serum components (hence long circulation)
- Proton sponge effect
Polymers (e.g., polyethyleneimine) with buffering capacities between 5 and 7.2 can potentially rupture the endosome
- Nups
Abbreviation for nucleoporins, a family of proteins that compose the main component of the nuclear pore complex
- Protein aptamer
Engineered protein that is soluble and stable inside of cells and binds to another macromolecule. It is composed of a peptide binding sequence attached at both ends to a scaffolding protein such as thioredoxin-A
- Hub protein
A protein that interacts with a large number of other proteins
- Bcl-XL proteins
B-cell lymphoma-extra large’ is a member of the Bcl-2 family of proteins. It is an anti-apoptotic protein found in the transmembrane of the mitochondria
Footnotes
For reprint orders, please contact reprints@future-science.com
Financial & competing interests disclosure
The authors are funded by NIH grants R01 CA129528 and DOD 55900381. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
Bibliography
Papers of special note have been highlighted as:
■ of interest
■■ of considerable interest
- 1.Heemels MT. Medicine Nobel goes to pioneer of protein guidance mechanisms. Nature. 1999;401(6754):625. doi: 10.1038/44200. [DOI] [PubMed] [Google Scholar]
- 2.Hagmen M. Protein zip codes make Nobel journey. Science. 1999;286(5440):666. doi: 10.1126/science.286.5440.666. [DOI] [PubMed] [Google Scholar]
- 3.Shields D. Gunter Blobel – still passionate after all these years. Trends Cell Biol. 2001;11(8):349–350. doi: 10.1016/s0962-8924(01)02065-7. [DOI] [PubMed] [Google Scholar]
- 4■■.Dixon AS, Kakar M, Schneider KM, Constance JE, Paullin BC, Lim CS. Controlling subcellular localization to alter function: sending oncogenic Bcr–Abl to the nucleus causes apoptosis. J Control Release. 2009;140(3):245–249. doi: 10.1016/j.jconrel.2009.06.026. Discusses how mislocalized proteins can lead to disease, and suggests that altering localization of proteins can be used for therapeutic purposes. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davis JR, Kakar M, Lim CS. Controlling protein compartmentalization to overcome disease. Pharm Res. 2007;24(1):17–27. doi: 10.1007/s11095-006-9133-z. [DOI] [PubMed] [Google Scholar]
- 6.Kakar M, Davis JR, Kern SE, Lim CS. Optimizing the protein switch: altering nuclear import and export signals and ligand binding domain. J Control Release. 2007;120(3):220–232. doi: 10.1016/j.jconrel.2007.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7■■.Kanwal C, Mu S, Kern SE, Lim CS. Bidirectional on/off switch for controlled targeting of proteins to subcellular compartments. J Control Release. 2004;98(3):379–393. doi: 10.1016/j.jconrel.2004.05.008. Discusses the protein switch technology, which allows translocation of a cytoplasmic protein to the nucleus upon addition of a ligand. [DOI] [PubMed] [Google Scholar]
- 8.Yaseen MA, Yu J, Jung B, Wong MS, Anvari B. Biodistribution of encapsulated indocyanine green in healthy mice. Mol Pharm. 2009;6(5):1321–1332. doi: 10.1021/mp800270t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li SD, Huang L. Pharmacokinetics and biodistribution of nanoparticles. Mol Pharm. 2008;5(4):496–504. doi: 10.1021/mp800049w. [DOI] [PubMed] [Google Scholar]
- 10.Alexis F, Pridgen E, Molnar LK, Farokhzad OC. Factors affecting the clearance and biodistribution of polymeric nanoparticles. Mol Pharm. 2008;5(4):505–515. doi: 10.1021/mp800051m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Owens DE, 3rd, Peppas NA. Opsonization, biodistribution, and pharmacokinetics of polymeric nanoparticles. Int J Pharm. 2006;307(1):93–102. doi: 10.1016/j.ijpharm.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 12.Connor J, Norley N, Huang L. Biodistribution of pH-sensitive immunoliposomes. Biochim Biophys Acta. 1986;884(3):474–481. doi: 10.1016/0304-4165(86)90197-2. [DOI] [PubMed] [Google Scholar]
- 13■.Torchilin VP. Recent approaches to intracellular delivery of drugs and DNA and organelle targeting. Annu Rev Biomed Eng. 2006;8:343–375. doi: 10.1146/annurev.bioeng.8.061505.095735. Excellent review on delivery of drugs to various cellular organelles. [DOI] [PubMed] [Google Scholar]
- 14.Liu D, Huang L. Role of cholesterol in the stability of pH-sensitive, large unilamellar liposomes prepared by the detergent–dialysis method. Biochim Biophys Acta. 1989;981(2):254–260. doi: 10.1016/0005-2736(89)90035-7. [DOI] [PubMed] [Google Scholar]
- 15.Liu D, Huang L. pH-sensitive, plasma-table liposomes with relatively prolonged residence in circulation. Biochim Biophys Acta. 1990;1022(3):348–354. doi: 10.1016/0005-2736(90)90284-u. [DOI] [PubMed] [Google Scholar]
- 16.Collins D, Litzinger DC, Huang L. Structural and functional comparisons of pH-sensitive liposomes composed of phosphatidylethanolamine and three different diacylsuccinylglycerols. Biochim Biophys Acta. 1990;1025(2):234–242. doi: 10.1016/0005-2736(90)90102-t. [DOI] [PubMed] [Google Scholar]
- 17.Liu D, Mori A, Huang L. Large liposomes containing ganglioside GM1 accumulate effectively in spleen. Biochim Biophys Acta. 1991;1066(2):159–165. doi: 10.1016/0005-2736(91)90182-8. [DOI] [PubMed] [Google Scholar]
- 18.Kono K, Igawa T, Takagishi T. Cytoplasmic delivery of calcein mediated by liposomes modified with a pH-sensitive poly(ethylene glycol) derivative. Biochim Biophys Acta. 1997;1325(2):143–154. doi: 10.1016/s0005-2736(96)00244-1. [DOI] [PubMed] [Google Scholar]
- 19.Alberts B, Johnson A, Lewis J, Raff M, Roberts K, Walter P. Molecular Biology of the Cell. 5. Garland Science; NY, USA: 2008. [Google Scholar]
- 20.Guillem VM, Alino SF. Transfection pathways of nonspecific and targeted PEI-polyplexes. Gene Ther Mol Biol. 2004;8:369–384. [Google Scholar]
- 21.Poon GM, Gariepy J. Cell-surface proteoglycans as molecular portals for cationic peptide and polymer entry into cells. Biochem Soc Trans. 2007;35(Pt 4):788–793. doi: 10.1042/BST0350788. [DOI] [PubMed] [Google Scholar]
- 22.Nitin N, Santangelo PJ, Kim G, Nie S, Bao G. Peptide-linked molecular beacons for efficient delivery and rapid mRNA detection in living cells. Nucleic Acids Res. 2004;32(6):e58. doi: 10.1093/nar/gnh063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ziegler A, Nervi P, Durrenberger M, Seelig J. The cationic cell-penetrating peptide CPP(TAT) derived from the HIV-1 protein TAT is rapidly transported into living fibroblasts: optical, biophysical, and metabolic evidence. Biochemistry. 2005;44(1):138–148. doi: 10.1021/bi0491604. [DOI] [PubMed] [Google Scholar]
- 24.Green M, Loewenstein PM. Autonomous functional domains of chemically synthesized human immunodeficiency virus tat transactivator protein. Cell. 1988;55(6):1179–1188. doi: 10.1016/0092-8674(88)90262-0. [DOI] [PubMed] [Google Scholar]
- 25.Frankel AD, Pabo CO. Cellular uptake of the tat protein from human immunodeficiency virus. Cell. 1988;55(6):1189–1193. doi: 10.1016/0092-8674(88)90263-2. [DOI] [PubMed] [Google Scholar]
- 26.Futaki S, Suzuki T, Ohashi W, et al. Arginine-rich peptides. An abundant source of membrane-permeable peptides having potential as carriers for intracellular protein delivery. J Biol Chem. 2001;276(8):5836–5840. doi: 10.1074/jbc.M007540200. [DOI] [PubMed] [Google Scholar]
- 27.Schwarze SR, Ho A, Vocero-Akbani A, Dowdy SF. In vivo protein transduction: delivery of a biologically active protein into the mouse. Science. 1999;285(5433):1569–1572. doi: 10.1126/science.285.5433.1569. [DOI] [PubMed] [Google Scholar]
- 28.Heitz F, Morris MC, Divita G. Twenty years of cell-penetrating peptides: from molecular mechanisms to therapeutics. Br J Pharmacol. 2009;157(2):195–206. doi: 10.1111/j.1476-5381.2009.00057.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nori A, Jensen KD, Tijerina M, Kopeckova P, Kopecek J. Tat-conjugated synthetic macromolecules facilitate cytoplasmic drug delivery to human ovarian carcinoma cells. Bioconjug Chem. 2003;14(1):44–50. doi: 10.1021/bc0255900. [DOI] [PubMed] [Google Scholar]
- 30.Sethuraman VA, Bae YH. Tat peptide-based micelle system for potential active targeting of anti-cancer agents to acidic solid tumors. J Control Release. 2007;118(2):216–224. doi: 10.1016/j.jconrel.2006.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wadia JS, Stan RV, Dowdy SF. Transducible TAT-HA fusogenic peptide enhances escape of TAT-fusion proteins after lipid raft macropinocytosis. Nat Med. 2004;10(3):310–315. doi: 10.1038/nm996. [DOI] [PubMed] [Google Scholar]
- 32.Richard JP, Melikov K, Vives E, et al. Cell-penetrating peptides. A re-evaluation of the mechanism of cellular uptake. J Biol Chem. 2003;278(1):585–590. doi: 10.1074/jbc.M209548200. [DOI] [PubMed] [Google Scholar]
- 33.Jarver P, Langel U. The use of cell-penetrating peptides as a tool for gene regulation. Drug Discov Today. 2004;9(9):395–402. doi: 10.1016/S1359-6446(04)03042-9. [DOI] [PubMed] [Google Scholar]
- 34.Zhang C, Tang N, Liu X, Liang W, Xu W, Torchilin VP. siRNA-containing liposomes modified with polyarginine effectively silence the targeted gene. J Control Release. 2006;112(2):229–239. doi: 10.1016/j.jconrel.2006.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bengali Z, Pannier AK, Segura T, et al. Gene delivery through cell culture substrate adsorbed DNA complexes. Biotechnol Bioeng. 2005;90(3):290–302. doi: 10.1002/bit.20393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Panyam J, Labhasetwar V. Biodegradable nanoparticles for drug and gene delivery to cells and tissue. Adv Drug Deliv Rev. 2003;55(3):329–347. doi: 10.1016/s0169-409x(02)00228-4. [DOI] [PubMed] [Google Scholar]
- 37.Vasir JK, Labhasetwar V. Biodegradable nanoparticles for cytosolic delivery of therapeutics. Adv Drug Deliv Rev. 2007;59(8):718–728. doi: 10.1016/j.addr.2007.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chu CJ, Dijkstra J, Lai MZ, Hong K, Szoka FC. Efficiency of cytoplasmic delivery by pH-sensitive liposomes to cells in culture. Pharm Res. 1990;7(8):824–834. doi: 10.1023/a:1015908831507. [DOI] [PubMed] [Google Scholar]
- 39.Schroit AJ, Madsen J, Nayar R. Liposome–cell interactions: in vitro discrimination of uptake mechanism and in vivo targeting strategies to mononuclear phagocytes. Chem Phys Lipids. 1986;40(2–4):373–393. doi: 10.1016/0009-3084(86)90080-0. [DOI] [PubMed] [Google Scholar]
- 40.Liu DX, Huang L. Small, but not large, unilamellar liposomes composed of dioleoylphosphatidylethanolamine and oleic acid can be stabilized by human plasma. Biochemistry. 1989;28(19):7700–7707. doi: 10.1021/bi00445a027. [DOI] [PubMed] [Google Scholar]
- 41.llens H, Bentz J, Szoka FC. pH-induced destabilization of phosphatidylethanolamine-containing liposomes: role of bilayer contact. Biochemistry. 1984;23(7):1532–1538. doi: 10.1021/bi00302a029. [DOI] [PubMed] [Google Scholar]
- 42.Wei H, Zhang XZ, Chen WQ, Cheng SX, Zhuo RX. Self-assembled thermosensitive micelles based on poly(L-lactide-star block-n-isopropylacrylamide) for drug delivery. J Biomed Mater Res A. 2007;83(4):980–989. doi: 10.1002/jbm.a.31295. [DOI] [PubMed] [Google Scholar]
- 43.Toti US, Moon SH, Kim HY, et al. Thermosensitive and biocompatible cyclotriphosphazene micelles. J Control Release. 2007;119(1):34–40. doi: 10.1016/j.jconrel.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 44.Zhou Y, Yan D, Dong W, Tian Y. Temperature-responsive phase transition of polymer vesicles: real-time morphology observation and molecular mechanism. J Phys Chem B. 2007;111(6):1262–1270. doi: 10.1021/jp0673563. [DOI] [PubMed] [Google Scholar]
- 45.Yang M, Ding Y, Zhang L, Qian X, Jiang X, Liu B. Novel thermosensitive polymeric micelles for docetaxel delivery. J Biomed Mater Res A. 2007;81(4):847–857. doi: 10.1002/jbm.a.31129. [DOI] [PubMed] [Google Scholar]
- 46.Wei H, Zhang X, Cheng C, Cheng SX, Zhuo RX. Self-assembled, thermosensitive micelles of a star block copolymer based on PMMA and PNIPAAm for controlled drug delivery. Biomaterials. 2007;28(1):99–107. doi: 10.1016/j.biomaterials.2006.08.030. [DOI] [PubMed] [Google Scholar]
- 47.Rangelov S, Dimitrov P, Tsvetanov CB. Mixed block copolymer aggregates with tunable temperature behavior. J Phys Chem B. 2005;109(3):1162–1167. doi: 10.1021/jp046118+. [DOI] [PubMed] [Google Scholar]
- 48.Bae KH, Choi SH, Park SY, Lee Y, Park TG. Thermosensitive pluronic micelles stabilized by shell cross-linking with gold nanoparticles. Langmuir. 2006;22(14):6380–6384. doi: 10.1021/la0606704. [DOI] [PubMed] [Google Scholar]
- 49.Soga O, Van Nostrum CF, Fens M, et al. Thermosensitive and biodegradable polymeric micelles for paclitaxel delivery. J Control Release. 2005;103(2):341–353. doi: 10.1016/j.jconrel.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 50.Jeong B, Bae YH, Kim SW. Drug release from biodegradable injectable thermosensitive hydrogel of PEG–PLGA–pPEG triblock copolymers. J Control Release. 2000;63(1–2):155–163. doi: 10.1016/s0168-3659(99)00194-7. [DOI] [PubMed] [Google Scholar]
- 51.Yockman JW, Kastenmeier A, Erickson HM, et al. Novel polymer carriers and gene constructs for treatment of myocardial ischemia and infarction. J Control Release. 2008;132(3):260–266. doi: 10.1016/j.jconrel.2008.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mossalam M, Jeong JH, Abel ED, Kim SW, Kim YH. Reversal of oxidative stress in endothelial cells by controlled release of adiponectin. J Control Release. 2008;130(3):234–237. doi: 10.1016/j.jconrel.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 53.Ho RJ, Rouse BT, Huang L. Target-sensitive immunoliposomes: preparation and characterization. Biochemistry. 1986;25(19):5500–5506. doi: 10.1021/bi00367a023. [DOI] [PubMed] [Google Scholar]
- 54.Straubinger RM, Duzgunes N, Papahadjopoulos D. pH-sensitive liposomes mediate cytoplasmic delivery of encapsulated macromolecules. FEBS Lett. 1985;179(1):148–154. doi: 10.1016/0014-5793(85)80210-6. [DOI] [PubMed] [Google Scholar]
- 55.Leamon CP, Low PS. Delivery of macromolecules into living cells: a method that exploits folate receptor endocytosis. Proc Natl Acad Sci USA. 1991;88(13):5572–5576. doi: 10.1073/pnas.88.13.5572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Thorstensen K, Romslo I. The transferrin receptor: its diagnostic value and its potential as therapeutic target. Scand J Clin Lab Invest. 1993;215(Suppl):113–120. doi: 10.3109/00365519309090703. [DOI] [PubMed] [Google Scholar]
- 57.Chung NS, Wasan KM. Potential role of the low-density lipoprotein receptor family as mediators of cellular drug uptake. Adv Drug Deliv Rev. 2004;56(9):1315–1334. doi: 10.1016/j.addr.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 58.Vyas SP, Singh A, Sihorkar V. Ligand–receptor-mediated drug delivery: an emerging paradigm in cellular drug targeting. Crit Rev Ther Drug Carrier Syst. 2001;18(1):1–76. [PubMed] [Google Scholar]
- 59■.Gorlich D, Kutay U. Transport between the cell nucleus and the cytoplasm. Annu Rev Cell Dev Biol. 1999;15:607–660. doi: 10.1146/annurev.cellbio.15.1.607. Excellent review on nuclear import and export, including all of the key players (proteins and cofactors) [DOI] [PubMed] [Google Scholar]
- 60.Kakar M, Cadwallader AB, Davis JR, Lim CS. Signal sequences for targeting of gene therapy products to subcellular compartments: the role of CRM1 in nucleocytoplasmic shuttling of the protein switch. Pharm Res. 2007;24(11):2146–2155. doi: 10.1007/s11095-007-9333-1. [DOI] [PubMed] [Google Scholar]
- 61.Boussif O, Lezoualc’h F, Zanta MA, et al. A versatile vector for gene and oligonucleotide transfer into cells in culture and in vivo: polyethylenimine. Proc Natl Acad Sci USA. 1995;92(16):7297–7301. doi: 10.1073/pnas.92.16.7297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62■.Akinc A, Thomas M, Klibanov AM, Langer R. Exploring polyethylenimine-mediated DNA transfection and the proton sponge hypothesis. J Gene Med. 2005;7(5):657–663. doi: 10.1002/jgm.696. Discusses the mechanism of DNA transfection by polyethyleneimine. [DOI] [PubMed] [Google Scholar]
- 63.Chollet P, Favrot MC, Hurbin A, Coll JL. Side-effects of a systemic injection of linear polyethylenimine–DNA complexes. J Gene Med. 2002;4(1):84–91. doi: 10.1002/jgm.237. [DOI] [PubMed] [Google Scholar]
- 64.Park TG, Jeong JH, Kim SW. Current status of polymeric gene delivery systems. Adv Drug Deliv Rev. 2006;58(4):467–486. doi: 10.1016/j.addr.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 65.Masotti A, Moretti F, Mancini F, et al. Physicochemical and biological study of selected hydrophobic polyethylenimine-based polycationic liposomes and their complexes with DNA. Bioorg Med Chem. 2007;15(3):1504–1515. doi: 10.1016/j.bmc.2006.10.066. [DOI] [PubMed] [Google Scholar]
- 66.Neu M, Fischer D, Kissel T. Recent advances in rational gene transfer vector design based on poly(ethylene imine) and its derivatives. J Gene Med. 2005;7(8):992–1009. doi: 10.1002/jgm.773. [DOI] [PubMed] [Google Scholar]
- 67.Wang Y, Chen P, Shen J. The development and characterization of a glutathione-sensitive cross-linked polyethylenimine gene vector. Biomaterials. 2006;27(30):5292–5298. doi: 10.1016/j.biomaterials.2006.05.049. [DOI] [PubMed] [Google Scholar]
- 68.Zintchenko A, Philipp A, Dehshahri A, Wagner E. Simple modifications of branched PEI lead to highly efficient siRNA carriers with low toxicity. Bioconjug Chem. 2008;19(7):1448–1455. doi: 10.1021/bc800065f. [DOI] [PubMed] [Google Scholar]
- 69.Yu JH, Quan JS, Huang J, et al. α,β-poly(L-aspartate-graft-PEI): a pseudo-branched PEI as a gene carrier with low toxicity and high transfection efficiency. Acta Biomater. 2009;5(7):2485–2494. doi: 10.1016/j.actbio.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 70.Duvall CL, Convertine A, Benoit DS, Hoffman AS, Stayton P. Intracellular delivery of a proapoptotic peptide via conjugation to a raft synthesized endosomolytic polymer. Mol Pharm. 2009;7(2):468–476. doi: 10.1021/mp9002267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Murthy N, Campbell J, Fausto N, Hoffman AS, Stayton PS. Bioinspired pH-responsive polymers for the intracellular delivery of biomolecular drugs. Bioconjug Chem. 2003;14(2):412–419. doi: 10.1021/bc020056d. [DOI] [PubMed] [Google Scholar]
- 72.Bareford LM, Swaan PW. Endocytic mechanisms for targeted drug delivery. Adv Drug Deliv Rev. 2007;59(8):748–758. doi: 10.1016/j.addr.2007.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gary-Bobo M, Nirde P, Jeanjean A, Morere A, Garcia M. Mannose 6-phosphate receptor targeting and its applications in human diseases. Curr Med Chem. 2007;14(28):2945–2953. doi: 10.2174/092986707782794005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lebowitz JH, Grubb JH, Maga JA, Schmiel DH, Vogler C, Sly WS. Glycosylation-independent targeting enhances enzyme delivery to lysosomes and decreases storage in mucopolysaccharidosis type VII mice. Proc Natl Acad Sci USA. 2004;101(9):3083–3088. doi: 10.1073/pnas.0308728100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Feldherr CM. The nuclear annuli as pathways for nucleocytoplasmic exchanges. J Cell Biol. 1962;14:65–72. doi: 10.1083/jcb.14.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mans BJ, Anantharaman V, Aravind L, Koonin EV. Comparative genomics, evolution and origins of the nuclear envelope and nuclear pore complex. Cell Cycle. 2004;3(12):1612–1637. doi: 10.4161/cc.3.12.1316. [DOI] [PubMed] [Google Scholar]
- 77.Jekely G. Glimpsing over the event horizon: evolution of nuclear pores and envelope. Cell Cycle. 2005;4(2):297–299. [PubMed] [Google Scholar]
- 78.Feldherr C, Akin D, Littlewood T, Stewart M. The molecular mechanism of translocation through the nuclear pore complex is highly conserved. J Cell Sci. 2002;115(Pt 14):2997–3005. doi: 10.1242/jcs.115.14.2997. [DOI] [PubMed] [Google Scholar]
- 79.Harel A, Forbes DJ. Importin β: conducting a much larger cellular symphony. Mol Cell. 2004;16(3):319–330. doi: 10.1016/j.molcel.2004.10.026. [DOI] [PubMed] [Google Scholar]
- 80.Wente SR. Gatekeepers of the nucleus. Science. 2000;288(5470):1374–1377. doi: 10.1126/science.288.5470.1374. [DOI] [PubMed] [Google Scholar]
- 81.Ribbeck K, Gorlich D. Kinetic analysis of translocation through nuclear pore complexes. EMBO J. 2001;20(6):1320–1330. doi: 10.1093/emboj/20.6.1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Akey CW, Radermacher M. Architecture of the xenopus nuclear pore complex revealed by three-dimensional cryo-electron microscopy. J Cell Biol. 1993;122(1):1–19. doi: 10.1083/jcb.122.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Allen TD, Cronshaw JM, Bagley S, Kiseleva E, Goldberg MW. The nuclear pore complex: mediator of translocation between nucleus and cytoplasm. J Cell Sci. 2000;113(Pt 10):1651–1659. doi: 10.1242/jcs.113.10.1651. [DOI] [PubMed] [Google Scholar]
- 84.Stoffler D, Fahrenkrog B, Aebi U. The nuclear pore complex: from molecular architecture to functional dynamics. Curr Opin Cell Biol. 1999;11(3):391–401. doi: 10.1016/S0955-0674(99)80055-6. [DOI] [PubMed] [Google Scholar]
- 85.Seedorf M, Damelin M, Kahana J, Taura T, Silver PA. Interactions between a nuclear transporter and a subset of nuclear pore complex proteins depend on Ran GTPase. Mol Cell Biol. 1999;19(2):1547–1557. doi: 10.1128/mcb.19.2.1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Shah S, Tugendreich S, Forbes D. Major binding sites for the nuclear import receptor are the internal nucleoporin Nup153 and the adjacent nuclear filament protein Tpr. J Cell Biol. 1998;141(1):31–49. doi: 10.1083/jcb.141.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Iovine MK, Wente SR. A nuclear export signal in Kap95p is required for both recycling the import factor and interaction with the nucleoporin GLFG repeat regions of Nup116p and Nup100p. J Cell Biol. 1997;137(4):797–811. doi: 10.1083/jcb.137.4.797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Iovine MK, Watkins JL, Wente SR. The GLFG repetitive region of the nucleoporin Nup116p interacts with Kap95p, an essential yeast nuclear import factor. J Cell Biol. 1995;131(6 Pt 2):1699–1713. doi: 10.1083/jcb.131.6.1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lyman SK, Guan T, Bednenko J, Wodrich H, Gerace L. Influence of cargo size on ran and energy requirements for nuclear protein import. J Cell Biol. 2002;159(1):55–67. doi: 10.1083/jcb.200204163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Turpin P, Ossareh-Nazari B, Dargemont C. Nuclear transport and transcriptional regulation. FEBS Lett. 1999;452(1–2):82–86. doi: 10.1016/s0014-5793(99)00533-5. [DOI] [PubMed] [Google Scholar]
- 91.Paine PL, Moore LC, Horowitz SB. Nuclear envelope permeability. Nature. 1975;254(5496):109–114. doi: 10.1038/254109a0. [DOI] [PubMed] [Google Scholar]
- 92.Talcott B, Moore MS. Getting across the nuclear pore complex. Trends Cell Biol. 1999;9(8):312–318. doi: 10.1016/s0962-8924(99)01608-6. [DOI] [PubMed] [Google Scholar]
- 93.Poon IK, Jans DA. Regulation of nuclear transport: central role in development and transformation? Traffic. 2005;6(3):173–186. doi: 10.1111/j.1600-0854.2005.00268.x. [DOI] [PubMed] [Google Scholar]
- 94.Feldherr CM, Akin D. The location of the transport gate in the nuclear pore complex. J Cell Sci. 1997;110(Pt 24):3065–3070. doi: 10.1242/jcs.110.24.3065. [DOI] [PubMed] [Google Scholar]
- 95.Weis K. Regulating access to the genome: nucleocytoplasmic transport throughout the cell cycle. Cell. 2003;112(4):441–451. doi: 10.1016/s0092-8674(03)00082-5. [DOI] [PubMed] [Google Scholar]
- 96.Kalderon D, Richardson WD, Markham AF, Smith AE. Sequence requirements for nuclear location of simian virus 40 large-T antigen. Nature. 1984;311(5981):33–38. doi: 10.1038/311033a0. [DOI] [PubMed] [Google Scholar]
- 97.Hodel MR, Corbett AH, Hodel AE. Dissection of a nuclear localization signal. J Biol Chem. 2001;276(2):1317–1325. doi: 10.1074/jbc.M008522200. [DOI] [PubMed] [Google Scholar]
- 98.Efthymiadis A, Shao H, Hubner S, Jans DA. Kinetic characterization of the human retinoblastoma protein bipartite nuclear localization sequence (NLS) in vivo and in vitro. A comparison with the SV40 large T-antigen NLS. J Biol Chem. 1997;272(35):22134–22139. doi: 10.1074/jbc.272.35.22134. [DOI] [PubMed] [Google Scholar]
- 99.Gorlich D, Prehn S, Laskey RA, Hartmann E. Isolation of a protein that is essential for the first step of nuclear protein import. Cell. 1994;79(5):767–778. doi: 10.1016/0092-8674(94)90067-1. [DOI] [PubMed] [Google Scholar]
- 100.Conti E, Uy M, Leighton L, Blobel G, Kuriyan J. Crystallographic analysis of the recognition of a nuclear localization signal by the nuclear import factor karyopherin α. Cell. 1998;94(2):193–204. doi: 10.1016/s0092-8674(00)81419-1. [DOI] [PubMed] [Google Scholar]
- 101.Chook YM, Blobel G. Karyopherins and nuclear import. Curr Opin Struct Biol. 2001;11(6):703–715. doi: 10.1016/s0959-440x(01)00264-0. [DOI] [PubMed] [Google Scholar]
- 102.Gorlich D, Henklein P, Laskey RA, Hartmann E. A 41 amino acid motif in importin-α confers binding to importin-β and hence transit into the nucleus. EMBO J. 1996;15(8):1810–1817. [PMC free article] [PubMed] [Google Scholar]
- 103.Bayliss R, Littlewood T, Stewart M. Structural basis for the interaction between FxFG nucleoporin repeats and importin-β in nuclear trafficking. Cell. 2000;102(1):99–108. doi: 10.1016/s0092-8674(00)00014-3. [DOI] [PubMed] [Google Scholar]
- 104.Azuma Y, Dasso M. The role of Ran in nuclear function. Curr Opin Cell Biol. 2000;12(3):302–307. doi: 10.1016/s0955-0674(00)00093-4. [DOI] [PubMed] [Google Scholar]
- 105.Vetter IR, Nowak C, Nishimoto T, Kuhlmann J, Wittinghofer A. Structure of a Ran-binding domain complexed with Ran bound to a GTP analogue: implications for nuclear transport. Nature. 1999;398(6722):39–46. doi: 10.1038/17969. [DOI] [PubMed] [Google Scholar]
- 106.Kohler M, Speck C, Christiansen M, et al. Evidence for distinct substrate specificities of importin α family members in nuclear protein import. Mol Cell Biol. 1999;19(11):7782–7791. doi: 10.1128/mcb.19.11.7782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lukacs GL, Haggie P, Seksek O, Lechardeur D, Freedman N, Verkman AS. Size-dependent DNA mobility in cytoplasm and nucleus. J Biol Chem. 2000;275(3):1625–1629. doi: 10.1074/jbc.275.3.1625. [DOI] [PubMed] [Google Scholar]
- 108.Dauty E, Verkman AS. Actin cytoskeleton as the principal determinant of size-dependent DNA mobility in cytoplasm: a new barrier for non-viral gene delivery. J Biol Chem. 2005;280(9):7823–7828. doi: 10.1074/jbc.M412374200. [DOI] [PubMed] [Google Scholar]
- 109.Dohner K, Nagel CH, Sodeik B. Viral stop-and-go along microtubules: taking a ride with dynein and kinesins. Trends Microbiol. 2005;13(7):320–327. doi: 10.1016/j.tim.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 110.Greber UF, Way M. A superhighway to virus infection. Cell. 2006;124(4):741–754. doi: 10.1016/j.cell.2006.02.018. [DOI] [PubMed] [Google Scholar]
- 111.Welte MA. Bidirectional transport along microtubules. Curr Biol. 2004;14(13):R525–R537. doi: 10.1016/j.cub.2004.06.045. [DOI] [PubMed] [Google Scholar]
- 112.Mastrobattista E, van der Aa MA, Hennink WE, Crommelin DJ. Artificial viruses: a nanotechnological approach to gene delivery. Nat Rev Drug Discov. 2006;5(2):115–121. doi: 10.1038/nrd1960. [DOI] [PubMed] [Google Scholar]
- 113.van der Aa MA, Mastrobattista E, Oosting RS, Hennink WE, Koning GA, Crommelin DJ. The nuclear pore complex: the gateway to successful nonviral gene delivery. Pharm Res. 2006;23(3):447–459. doi: 10.1007/s11095-005-9445-4. [DOI] [PubMed] [Google Scholar]
- 114.Lim RY, Fahrenkrog B. The nuclear pore complex up close. Curr Opin Cell Biol. 2006;18(3):342–347. doi: 10.1016/j.ceb.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 115.Pante N, Kann M. Nuclear pore complex is able to transport macromolecules with diameters of about 39 nm. Mol Biol Cell. 2002;13(2):425–434. doi: 10.1091/mbc.01-06-0308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Chan CK, Senden T, Jans DA. Supramolecular structure and nuclear targeting efficiency determine the enhancement of transfection by modified polylysines. Gene Ther. 2000;7(19):1690–1697. doi: 10.1038/sj.gt.3301275. [DOI] [PubMed] [Google Scholar]
- 117.Chan CK, Jans DA. Using nuclear targeting signals to enhance non-viral gene transfer. Immunol Cell Biol. 2002;80(2):119–130. doi: 10.1046/j.1440-1711.2002.01061.x. [DOI] [PubMed] [Google Scholar]
- 118■■.Pouton CW, Wagstaff KM, Roth DM, Moseley GW, Jans DA. Targeted delivery to the nucleus. Adv Drug Deliv Rev. 2007;59(8):698–717. doi: 10.1016/j.addr.2007.06.010. Compilation of nuclear import, nuclear localization signals, and considerations, approaches and applications of nuclear targeting. [DOI] [PubMed] [Google Scholar]
- 119.Branden LJ, Mohamed AJ, Smith CI. A peptide nucleic acid–nuclear localization signal fusion that mediates nuclear transport of DNA. Nat Biotechnol. 1999;17(8):784–787. doi: 10.1038/11726. [DOI] [PubMed] [Google Scholar]
- 120.Sebestyen MG, Ludtke JJ, Bassik MC, et al. DNA vector chemistry: the covalent attachment of signal peptides to plasmid DNA. Nat Biotechnol. 1998;16(1):80–85. doi: 10.1038/nbt0198-80. [DOI] [PubMed] [Google Scholar]
- 121.Ciolina C, Byk G, Blanche F, Thuillier V, Scherman D, Wils P. Coupling of nuclear localization signals to plasmid DNA and specific interaction of the conjugates with importin α. Bioconjug Chem. 1999;10(1):49–55. doi: 10.1021/bc980061a. [DOI] [PubMed] [Google Scholar]
- 122.Nagasaki T, Myohoji T, Tachibana T, Futaki S, Tamagaki S. Can nuclear localization signals enhance nuclear localization of plasmid DNA? Bioconjug Chem. 2003;14(2):282–286. doi: 10.1021/bc025602h. [DOI] [PubMed] [Google Scholar]
- 123.Carriere M, Escriou V, Savarin A, Scherman D. Coupling of importin β binding peptide on plasmid DNA: transfection efficiency is increased by modification of lipoplex’s physico–chemical properties. BMC Biotechnol. 2003;3:14. doi: 10.1186/1472-6750-3-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Neves C, Byk G, Scherman D, Wils P. Coupling of a targeting peptide to plasmid DNA by covalent triple helix formation. FEBS Lett. 1999;453(1–2):41–45. doi: 10.1016/s0014-5793(99)00674-2. [DOI] [PubMed] [Google Scholar]
- 125.Tanimoto M, Kamiya H, Minakawa N, Matsuda A, Harashima H. No enhancement of nuclear entry by direct conjugation of a nuclear localization signal peptide to linearized DNA. Bioconjug Chem. 2003;14(6):1197–1202. doi: 10.1021/bc034075e. [DOI] [PubMed] [Google Scholar]
- 126.van der Aa MA, Koning GA, D’oliveira C, et al. An NLS peptide covalently linked to linear DNA does not enhance transfection efficiency of cationic polymer based gene delivery systems. J Gene Med. 2005;7(2):208–217. doi: 10.1002/jgm.643. [DOI] [PubMed] [Google Scholar]
- 127.Johansson P, Lindgren T, Lundstrom M, Holmstrom A, Elgh F, Bucht G. PCR-generated linear DNA fragments utilized as a hantavirus DNA vaccine. Vaccine. 2002;20(27–28):3379–3388. doi: 10.1016/s0264-410x(02)00265-7. [DOI] [PubMed] [Google Scholar]
- 128.Zanta MA, Belguise-Valladier P, Behr JP. Gene delivery. A single nuclear localization signal peptide is sufficient to carry DNA to the cell nucleus. Proc Natl Acad Sci USA. 1999;96(1):91–96. doi: 10.1073/pnas.96.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129■■.Chahine MN, Pierce GN. Therapeutic targeting of nuclear protein import in pathological cell conditions. Pharmacol Rev. 2009;61(3):358–372. doi: 10.1124/pr.108.000620. Review of nuclear trafficking of proteins, the role of dysregulated nuclear import in disease and pharmacological approaches of targeting nuclear import. [DOI] [PubMed] [Google Scholar]
- 130.Snow CM, Senior A, Gerace L. Monoclonal antibodies identify a group of nuclear pore complex glycoproteins. J Cell Biol. 1987;104(5):1143–1156. doi: 10.1083/jcb.104.5.1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Finlay DR, Newmeyer DD, Price TM, Forbes DJ. Inhibition of in vitro nuclear transport by a lectin that binds to nuclear pores. J Cell Biol. 1987;104(2):189–200. doi: 10.1083/jcb.104.2.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Adam EJ, Adam SA. Identification of cytosolic factors required for nuclear location sequence-mediated binding to the nuclear envelope. J Cell Biol. 1994;125(3):547–555. doi: 10.1083/jcb.125.3.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Kosugi S, Hasebe M, Entani T, Takayama S, Tomita M, Yanagawa H. Design of peptide inhibitors for the importin α/β nuclear import pathway by activity-based profiling. Chem Biol. 2008;15(9):940–949. doi: 10.1016/j.chembiol.2008.07.019. [DOI] [PubMed] [Google Scholar]
- 134.Wolff B, Sanglier JJ, Wang Y. Leptomycin B is an inhibitor of nuclear export: inhibition of nucleo-cytoplasmic translocation of the human immunodeficiency virus type 1 (HIV-1) Rev protein and Rev-dependent mRNA. Chem Biol. 1997;4(2):139–147. doi: 10.1016/s1074-5521(97)90257-x. [DOI] [PubMed] [Google Scholar]
- 135.Ossareh-Nazari B, Bachelerie F, Dargemont C. Evidence for a role of CRM1 in signal-mediated nuclear protein export. Science. 1997;278(5335):141–144. doi: 10.1126/science.278.5335.141. [DOI] [PubMed] [Google Scholar]
- 136.Kudo N, Wolff B, Sekimoto T, et al. Leptomycin B inhibition of signal-mediated nuclear export by direct binding to CRM1. Exp Cell Res. 1998;242(2):540–547. doi: 10.1006/excr.1998.4136. [DOI] [PubMed] [Google Scholar]
- 137.Mutka SC, Yang WQ, Dong SD, et al. Identification of nuclear export inhibitors with potent anticancer activity in vivo. Cancer Res. 2009;69(2):510–517. doi: 10.1158/0008-5472.CAN-08-0858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Pieper GM, Riaz Ul H. Activation of nuclear factor-κb in cultured endothelial cells by increased glucose concentration: prevention by calphostin C. J Cardiovasc Pharmacol. 1997;30(4):528–532. doi: 10.1097/00005344-199710000-00019. [DOI] [PubMed] [Google Scholar]
- 139.Shoji S, Furuishi K, Ogata A, et al. An allosteric drug, o,o′-bismyristoyl thiamine disulfide, suppresses HIV-1 replication through prevention of nuclear translocation of both HIV-1 Tat and NF-κB. Biochem Biophys Res Commun. 1998;249(3):745–753. doi: 10.1006/bbrc.1998.9221. [DOI] [PubMed] [Google Scholar]
- 140.Wong ET, Tergaonkar V. Roles of NF-κB in health and disease: mechanisms and therapeutic potential. Clin Sci (Lond) 2009;116(6):451–465. doi: 10.1042/CS20080502. [DOI] [PubMed] [Google Scholar]
- 141.Hallhuber M, Burkard N, Wu R, et al. Inhibition of nuclear import of calcineurin prevents myocardial hypertrophy. Circ Res. 2006;99(6):626–635. doi: 10.1161/01.RES.0000243208.59795.d8. [DOI] [PubMed] [Google Scholar]
- 142.Colas P, Cohen B, Ko Ferrigno P, Silver PA, Brent R. Targeted modification and transportation of cellular proteins. Proc Natl Acad Sci USA. 2000;97(25):13720–13725. doi: 10.1073/pnas.97.25.13720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Emmott E, Hiscox JA. Nucleolar targeting: the hub of the matter. EMBO Rep. 2009;10(3):231–238. doi: 10.1038/embor.2009.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Birbach A, Bailey ST, Ghosh S, Schmid JA. Cytosolic, nuclear and nucleolar localization signals determine subcellular distribution and activity of the NF-κB inducing kinase NIK. J Cell Sci. 2004;117(Pt 16):3615–3624. doi: 10.1242/jcs.01224. [DOI] [PubMed] [Google Scholar]
- 145.Boyne JR, Whitehouse A. Nucleolar trafficking is essential for nuclear export of intronless herpesvirus mRNA. Proc Natl Acad Sci USA. 2006;103(41):15190–15195. doi: 10.1073/pnas.0604890103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Weber JD, Kuo ML, Bothner B, et al. Cooperative signals governing ARF–mdm2 interaction and nucleolar localization of the complex. Mol Cell Biol. 2000;20(7):2517–2528. doi: 10.1128/mcb.20.7.2517-2528.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Horke S, Reumann K, Schweizer M, Will H, Heise T. Nuclear trafficking of La protein depends on a newly identified nucleolar localization signal and the ability to bind RNA. J Biol Chem. 2004;279(25):26563–26570. doi: 10.1074/jbc.M401017200. [DOI] [PubMed] [Google Scholar]
- 148.Reed ML, Dove BK, Jackson RM, Collins R, Brooks G, Hiscox JA. Delineation and modelling of a nucleolar retention signal in the coronavirus nucleocapsid protein. Traffic. 2006;7(7):833–848. doi: 10.1111/j.1600-0854.2006.00424.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Ginisty H, Sicard H, Roger B, Bouvet P. Structure and functions of nucleolin. J Cell Sci. 1999;112(Pt 6):761–772. doi: 10.1242/jcs.112.6.761. [DOI] [PubMed] [Google Scholar]
- 150.Korgaonkar C, Hagen J, Tompkins V, et al. Nucleophosmin (B23) targets ARF to nucleoli and inhibits its function. Mol Cell Biol. 2005;25(4):1258–1271. doi: 10.1128/MCB.25.4.1258-1271.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Gunawardena SR, Ruis BL, Meyer JA, Kapoor M, Conklin KF. NOM1 targets protein phosphatase I to the nucleolus. J Biol Chem. 2008;283(1):398–404. doi: 10.1074/jbc.M706708200. [DOI] [PubMed] [Google Scholar]
- 152.Junera HR, Masson C, Geraud G, Hernandez-Verdun D. The three-dimensional organization of ribosomal genes and the architecture of the nucleoli vary with G1, S and G2 phases. J Cell Sci. 1995;108(Pt 11):3427–3441. doi: 10.1242/jcs.108.11.3427. [DOI] [PubMed] [Google Scholar]
- 153.Puvion-Dutilleul F, Puvion E, Bachellerie JP. Early stages of pre–rRNA formation within the nucleolar ultrastructure of mouse cells studied by in situ hybridization with a 5′ETS leader probe. Chromosoma. 1997;105(7–8):496–505. doi: 10.1007/BF02510486. [DOI] [PubMed] [Google Scholar]
- 154.Sirri V, Hernandez-Verdun D, Roussel P. Cyclin-dependent kinases govern formation and maintenance of the nucleolus. J Cell Biol. 2002;156(6):969–981. doi: 10.1083/jcb.200201024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Rubbi CP, Milner J. Disruption of the nucleolus mediates stabilization of p53 in response to DNA damage and other stresses. EMBO J. 2003;22(22):6068–6077. doi: 10.1093/emboj/cdg579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.David-Pfeuty T, Nouvian-Dooghe Y, Sirri V, Roussel P, Hernandez-Verdun D. Common and reversible regulation of wild-type p53 function and of ribosomal biogenesis by protein kinases in human cells. Oncogene. 2001;20(42):5951–5963. doi: 10.1038/sj.onc.1204741. [DOI] [PubMed] [Google Scholar]
- 157.Louvet E, Junera HR, Le Panse S, Hernandez-Verdun D. Dynamics and compartmentation of the nucleolar processing machinery. Exp Cell Res. 2005;304(2):457–470. doi: 10.1016/j.yexcr.2004.11.018. [DOI] [PubMed] [Google Scholar]
- 158.Kalinichenko VV, Major ML, Wang X, et al. Foxm1b transcription factor is essential for development of hepatocellular carcinomas and is negatively regulated by the p19ARF tumor suppressor. Genes Dev. 2004;18(7):830–850. doi: 10.1101/gad.1200704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Wang X, Kiyokawa H, Dennewitz MB, Costa RH. The Forkhead Box m1b transcription factor is essential for hepatocyte DNA replication and mitosis during mouse liver regeneration. Proc Natl Acad Sci USA. 2002;99(26):16881–16886. doi: 10.1073/pnas.252570299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.McFarland R, Taylor RW, Turnbull DM. Mitochondrial disease – its impact, etiology, and pathology. Curr Top Dev Biol. 2007;77:113–155. doi: 10.1016/S0070-2153(06)77005-3. [DOI] [PubMed] [Google Scholar]
- 161.Taylor RW, Turnbull DM. Mitochondrial DNA mutations in human disease. Nat Rev Genet. 2005;6(5):389–402. doi: 10.1038/nrg1606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Newmeyer DD, Ferguson-Miller S. Mitochondria: releasing power for life and unleashing the machineries of death. Cell. 2003;112(4):481–490. doi: 10.1016/s0092-8674(03)00116-8. [DOI] [PubMed] [Google Scholar]
- 163.Trushina E, McMurray CT. Oxidative stress and mitochondrial dysfunction in neurodegenerative diseases. Neuroscience. 2007;145(4):1233–1248. doi: 10.1016/j.neuroscience.2006.10.056. [DOI] [PubMed] [Google Scholar]
- 164.Orrenius S, Gogvadze V, Zhivotovsky B. Mitochondrial oxidative stress: implications for cell death. Annu Rev Pharmacol Toxicol. 2007;47:143–183. doi: 10.1146/annurev.pharmtox.47.120505.105122. [DOI] [PubMed] [Google Scholar]
- 165.Droge W. Free radicals in the physiological control of cell function. Physiol Rev. 2002;82(1):47–95. doi: 10.1152/physrev.00018.2001. [DOI] [PubMed] [Google Scholar]
- 166.Raha S, Robinson BH. Mitochondria, oxygen free radicals, disease and aging. Trends Biochem Sci. 2000;25(10):502–508. doi: 10.1016/s0968-0004(00)01674-1. [DOI] [PubMed] [Google Scholar]
- 167.Beckman KB, Ames BN. The free radical theory of aging matures. Physiol Rev. 1998;78(2):547–581. doi: 10.1152/physrev.1998.78.2.547. [DOI] [PubMed] [Google Scholar]
- 168.Wallace DC. Mitochondrial diseases in man and mouse. Science. 1999;283(5407):1482–1488. doi: 10.1126/science.283.5407.1482. [DOI] [PubMed] [Google Scholar]
- 169.Finkel T. Oxygen radicals and signaling. Curr Opin Cell Biol. 1998;10(2):248–253. doi: 10.1016/s0955-0674(98)80147-6. [DOI] [PubMed] [Google Scholar]
- 170.Finkel T, Holbrook NJ. Oxidants, oxidative stress and the biology of aging. Nature. 2000;408(6809):239–247. doi: 10.1038/35041687. [DOI] [PubMed] [Google Scholar]
- 171.Shigenaga MK, Hagen TM, Ames BN. Oxidative damage and mitochondrial decay in aging. Proc Natl Acad Sci USA. 1994;91(23):10771–10778. doi: 10.1073/pnas.91.23.10771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Ross MF, Kelso GF, Blaikie FH, et al. Lipophilic triphenylphosphonium cations as tools in mitochondrial bioenergetics and free radical biology. Biochemistry (Mosc) 2005;70(2):222–230. doi: 10.1007/s10541-005-0104-5. [DOI] [PubMed] [Google Scholar]
- 173.Green DR, Reed JC. Mitochondria and apoptosis. Science. 1998;281(5381):1309–1312. doi: 10.1126/science.281.5381.1309. [DOI] [PubMed] [Google Scholar]
- 174.Reed JC. Cytochrome c: can’t live with it – can’t live without it. Cell. 1997;91(5):559–562. doi: 10.1016/s0092-8674(00)80442-0. [DOI] [PubMed] [Google Scholar]
- 175.Green DR, Evan GI. A matter of life and death. Cancer Cell. 2002;1(1):19–30. doi: 10.1016/s1535-6108(02)00024-7. [DOI] [PubMed] [Google Scholar]
- 176.Galluzzi L, Morselli E, Kepp O, Tajeddine N, Kroemer G. Targeting p53 to mitochondria for cancer therapy. Cell Cycle. 2008;7(13):1949–1955. doi: 10.4161/cc.7.13.6222. [DOI] [PubMed] [Google Scholar]
- 177.Matsuyama S, Reed JC. Mitochondria-dependent apoptosis and cellular pH regulation. Cell Death Differ. 2000;7(12):1155–1165. doi: 10.1038/sj.cdd.4400779. [DOI] [PubMed] [Google Scholar]
- 178.Galluzzi L, Larochette N, Zamzami N, Kroemer G. Mitochondria as therapeutic targets for cancer chemotherapy. Oncogene. 2006;25(34):4812–4830. doi: 10.1038/sj.onc.1209598. [DOI] [PubMed] [Google Scholar]
- 179.Antignani A, Youle RJ. How do Bax and Bak lead to permeabilization of the outer mitochondrial membrane? Curr Opin Cell Biol. 2006;18(6):685–689. doi: 10.1016/j.ceb.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 180.Green DR, Kroemer G. The pathophysiology of mitochondrial cell death. Science. 2004;305(5684):626–629. doi: 10.1126/science.1099320. [DOI] [PubMed] [Google Scholar]
- 181.Ruffolo SC, Shore GC. BCL-2 selectively interacts with the BID-induced open conformer of BAK, inhibiting BAK auto-oligomerization. J Biol Chem. 2003;278(27):25039–25045. doi: 10.1074/jbc.M302930200. [DOI] [PubMed] [Google Scholar]
- 182.Mukhopadhyay A, Weiner H. Delivery of drugs and macromolecules to mitochondria. Adv Drug Deliv Rev. 2007;59(8):729–738. doi: 10.1016/j.addr.2007.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Adlam VJ, Harrison JC, Porteous CM, et al. Targeting an antioxidant to mitochondria decreases cardiac ischemia-reperfusion injury. FASEB J. 2005;19(9):1088–1095. doi: 10.1096/fj.05-3718com. [DOI] [PubMed] [Google Scholar]
- 184.James AM, Sharpley MS, Manas AR, et al. Interaction of the mitochondria-targeted antioxidant MitoQ with phospholipid bilayers and ubiquinone oxidoreductases. J Biol Chem. 2007;282(20):14708–14718. doi: 10.1074/jbc.M611463200. [DOI] [PubMed] [Google Scholar]
- 185.Filipovska A, Kelso GF, Brown SE, Beer SM, Smith RA, Murphy MP. Synthesis and characterization of a triphenylphosphonium-conjugated peroxidase mimetic. Insights into the interaction of ebselen with mitochondria. J Biol Chem. 2005;280(25):24113–24126. doi: 10.1074/jbc.M501148200. [DOI] [PubMed] [Google Scholar]
- 186.Smith RA, Kelso GF, James AM, Murphy MP. Targeting coenzyme Q derivatives to mitochondria. Meth Enzymol. 2004;382:45–67. doi: 10.1016/S0076-6879(04)82003-2. [DOI] [PubMed] [Google Scholar]
- 187.Kelso GF, Porteous CM, Coulter CV, et al. Selective targeting of a redox-active ubiquinone to mitochondria within cells. Antioxidant and antiapoptotic properties. J Biol Chem. 2001;276(7):4588–4596. doi: 10.1074/jbc.M009093200. [DOI] [PubMed] [Google Scholar]
- 188.Asin-Cayuela J, Manas AR, James AM, Smith RA, Murphy MP. Fine-tuning the hydrophobicity of a mitochondria-targeted antioxidant. FEBS Lett. 2004;571(1–3):9–16. doi: 10.1016/j.febslet.2004.06.045. [DOI] [PubMed] [Google Scholar]
- 189.Smith RA, Porteous CM, Coulter CV, Murphy MP. Selective targeting of an antioxidant to mitochondria. Eur J Biochem. 1999;263(3):709–716. doi: 10.1046/j.1432-1327.1999.00543.x. [DOI] [PubMed] [Google Scholar]
- 190.D’souza GG, Boddapati SV, Weissig V. Mitochondrial leader sequence-plasmid DNA conjugates delivered into mammalian cells by DQAsomes co-localize with mitochondria. Mitochondrion. 2005;5(5):352–358. doi: 10.1016/j.mito.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 191.D’souza GG, Rammohan R, Cheng SM, Torchilin VP, Weissig V. DQAsome-mediated delivery of plasmid DNA toward mitochondria in living cells. J Control Release. 2003;92(1–2):189–197. doi: 10.1016/s0168-3659(03)00297-9. [DOI] [PubMed] [Google Scholar]
- 192.Endo T, Kohda D. Functions of outer membrane receptors in mitochondrial protein import. Biochim Biophys Acta. 2002;1592(1):3–14. doi: 10.1016/s0167-4889(02)00259-8. [DOI] [PubMed] [Google Scholar]
- 193.Dolezal P, Likic V, Tachezy J, Lithgow T. Evolution of the molecular machines for protein import into mitochondria. Science. 2006;313(5785):314–318. doi: 10.1126/science.1127895. [DOI] [PubMed] [Google Scholar]
- 194.Rehling P, Brandner K, Pfanner N. Mitochondrial import and the twin-pore translocase. Nat Rev Mol Cell Biol. 2004;5(7):519–530. doi: 10.1038/nrm1426. [DOI] [PubMed] [Google Scholar]
- 195.Meisinger C, Ryan MT, Hill K, et al. Protein import channel of the outer mitochondrial membrane: a highly stable Tom40–Tom22 core structure differentially interacts with preproteins, small tom proteins, and import receptors. Mol Cell Biol. 2001;21(7):2337–2348. doi: 10.1128/MCB.21.7.2337-2348.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Herrmann JM, Neupert W. Protein transport into mitochondria. Curr Opin Microbiol. 2000;3(2):210–214. doi: 10.1016/s1369-5274(00)00077-1. [DOI] [PubMed] [Google Scholar]
- 197.Koehler CM. New developments in mitochondrial assembly. Annu Rev Cell Dev Biol. 2004;20:309–335. doi: 10.1146/annurev.cellbio.20.010403.105057. [DOI] [PubMed] [Google Scholar]
- 198.Von Heijne G. Mitochondrial targeting sequences may form amphiphilic helices. EMBO J. 1986;5(6):1335–1342. doi: 10.1002/j.1460-2075.1986.tb04364.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Roise D, Schatz G. Mitochondrial presequences. J Biol Chem. 1988;263(10):4509–4511. [PubMed] [Google Scholar]
- 200.Neupert W, Herrmann JM. Translocation of proteins into mitochondria. Annu Rev Biochem. 2007;76:723–749. doi: 10.1146/annurev.biochem.76.052705.163409. [DOI] [PubMed] [Google Scholar]
- 201.Mokranjac D, Neupert W. Protein import into mitochondria. Biochem Soc Trans. 2005;33(Pt 5):1019–1023. doi: 10.1042/BST20051019. [DOI] [PubMed] [Google Scholar]
- 202.Wiedemann N, Frazier AE, Pfanner N. The protein import machinery of mitochondria. J Biol Chem. 2004;279(15):14473–14476. doi: 10.1074/jbc.R400003200. [DOI] [PubMed] [Google Scholar]
- 203.Bohni PC, Daum G, Schatz G. Import of proteins into mitochondria. Partial purification of a matrix-located protease involved in cleavage of mitochondrial precursor polypeptides. J Biol Chem. 1983;258(8):4937–4943. [PubMed] [Google Scholar]
- 204.Schmidt B, Wachter E, Sebald W, Neupert W. Processing peptidase of neurospora mitochondria. Two-step cleavage of imported ATPase subunit 9. Eur J Biochem. 1984;144(3):581–588. doi: 10.1111/j.1432-1033.1984.tb08505.x. [DOI] [PubMed] [Google Scholar]
- 205.Folsch H, Guiard B, Neupert W, Stuart RA. Internal targeting signal of the BCS1 protein. A novel mechanism of import into mitochondria. EMBO J. 1996;15(3):479–487. [PMC free article] [PubMed] [Google Scholar]
- 206.Sirrenberg C, Endres M, Folsch H, Stuart RA, Neupert W, Brunner M. Carrier protein import into mitochondria mediated by the intermembrane proteins Tim10/Mrs11 and Tim12/Mrs5. Nature. 1998;391(6670):912–915. doi: 10.1038/36136. [DOI] [PubMed] [Google Scholar]
- 207.Rodriguez-Cousino N, Nargang FE, Baardman R, Neupert W, Lill R, Court DA. An import signal in the cytosolic domain of the neurospora mitochondrial outer membrane protein Tom22. J Biol Chem. 1998;273(19):11527–11532. doi: 10.1074/jbc.273.19.11527. [DOI] [PubMed] [Google Scholar]
- 208.Keil P, Pfanner N. Insertion of MOM22 into the mitochondrial outer membrane strictly depends on surface receptors. FEBS Lett. 1993;321(2–3):197–200. doi: 10.1016/0014-5793(93)80107-6. [DOI] [PubMed] [Google Scholar]
- 209.Mayer A, Lill R, Neupert W. Translocation and insertion of precursor proteins into isolated outer membranes of mitochondria. J Cell Biol. 1993;121(6):1233–1243. doi: 10.1083/jcb.121.6.1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Pfanner N, Hoeben P, Tropschug M, Neupert W. The carboxyl-terminal two-thirds of the ADP/ATP carrier polypeptide contains sufficient information to direct translocation into mitochondria. J Biol Chem. 1987;262(31):14851–14854. [PubMed] [Google Scholar]
- 211.Vestweber D, Schatz G. DNA–protein conjugates can enter mitochondria via the protein import pathway. Nature. 1989;338(6211):170–172. doi: 10.1038/338170a0. [DOI] [PubMed] [Google Scholar]
- 212.Marchenko ND, Zaika A, Moll UM. Death signal-induced localization of p53 protein to mitochondria. A potential role in apoptotic signaling. J Biol Chem. 2000;275(21):16202–16212. doi: 10.1074/jbc.275.21.16202. [DOI] [PubMed] [Google Scholar]
- 213.Horwich AL, Kalousek F, Mellman I, Rosenberg LE. A leader peptide is sufficient to direct mitochondrial import of a chimeric protein. EMBO J. 1985;4(5):1129–1135. doi: 10.1002/j.1460-2075.1985.tb03750.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Seibel M, Bachmann C, Schmiedel J, et al. Processing of artificial peptide–DNA-conjugates by the mitochondrial intermediate peptidase (MIP) Biol Chem. 1999;380(7–8):961–967. doi: 10.1515/BC.1999.119. [DOI] [PubMed] [Google Scholar]
- 215.Mukhopadhyay A, Ni L, Yang CS, Weiner H. Bacterial signal peptide recognizes HeLa cell mitochondrial import receptors and functions as a mitochondrial leader sequence. Cell Mol Life Sci. 2005;62(16):1890–1899. doi: 10.1007/s00018-005-5178-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Srivastava S, Moraes CT. Manipulating mitochondrial DNA heteroplasmy by a mitochondrially targeted restriction endonuclease. Hum Mol Genet. 2001;10(26):3093–3099. doi: 10.1093/hmg/10.26.3093. [DOI] [PubMed] [Google Scholar]
- 217.Tomita Y, Marchenko N, Erster S, et al. WT p53, but not tumor-derived mutants, bind to Bcl2 via the DNA binding domain and induce mitochondrial permeabilization. J Biol Chem. 2006;281(13):8600–8606. doi: 10.1074/jbc.M507611200. [DOI] [PubMed] [Google Scholar]
- 218.Mihara M, Erster S, Zaika A, et al. p53 has a direct apoptogenic role at the mitochondria. Mol Cell. 2003;11(3):577–590. doi: 10.1016/s1097-2765(03)00050-9. [DOI] [PubMed] [Google Scholar]
- 219.Erster S, Mihara M, Kim RH, Petrenko O, Moll UM. In vivo mitochondrial p53 translocation triggers a rapid first wave of cell death in response to DNA damage that can precede p53 target gene activation. Mol Cell Biol. 2004;24(15):6728–6741. doi: 10.1128/MCB.24.15.6728-6741.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Palade G. Intracellular aspects of the process of protein synthesis. Science. 1975;189(4200):347–358. doi: 10.1126/science.1096303. [DOI] [PubMed] [Google Scholar]
- 221.Pahl HL. Signal transduction from the endoplasmic reticulum to the cell nucleus. Physiol Rev. 1999;79(3):683–701. doi: 10.1152/physrev.1999.79.3.683. [DOI] [PubMed] [Google Scholar]
- 222.Borgese N, Francolini M, Snapp E. Endoplasmic reticulum architecture: structures in flux. Curr Opin Cell Biol. 2006;18(4):358–364. doi: 10.1016/j.ceb.2006.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Egea PF, Stroud RM, Walter P. Targeting proteins to membranes: structure of the signal recognition particle. Curr Opin Struct Biol. 2005;15(2):213–220. doi: 10.1016/j.sbi.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 224.Keenan RJ, Freymann DM, Stroud RM, Walter P. The signal recognition particle. Annu Rev Biochem. 2001;70:755–775. doi: 10.1146/annurev.biochem.70.1.755. [DOI] [PubMed] [Google Scholar]
- 225.Eichler J, Moll R. The signal recognition particle of archaea. Trends Microbiol. 2001;9(3):130–136. doi: 10.1016/s0966-842x(01)01954-0. [DOI] [PubMed] [Google Scholar]
- 226.Zopf D, Bernstein HD, Johnson AE, Walter P. The methionine-rich domain of the 54 kD protein subunit of the signal recognition particle contains an RNA binding site and can be crosslinked to a signal sequence. EMBO J. 1990;9(13):4511–4517. doi: 10.1002/j.1460-2075.1990.tb07902.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Lutcke H, High S, Romisch K, Ashford AJ, Dobberstein B. The methionine-rich domain of the 54 kDa subunit of signal recognition particle is sufficient for the interaction with signal sequences. EMBO J. 1992;11(4):1543–1551. doi: 10.1002/j.1460-2075.1992.tb05199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Keenan RJ, Freymann DM, Walter P, Stroud RM. Crystal structure of the signal sequence binding subunit of the signal recognition particle. Cell. 1998;94(2):181–191. doi: 10.1016/s0092-8674(00)81418-x. [DOI] [PubMed] [Google Scholar]
- 229.Brodsky JL. Post-translational protein translocation: not all hsc70s are created equal. Trends Biochem Sci. 1996;21(4):122–126. [PubMed] [Google Scholar]
- 230.Stroud RM, Walter P. Signal sequence recognition and protein targeting. Curr Opin Struct Biol. 1999;9(6):754–759. doi: 10.1016/s0959-440x(99)00040-8. [DOI] [PubMed] [Google Scholar]
- 231.Brodsky JL, Goeckeler J, Schekman R. BiP and Sec63p are required for both co- and post-translational protein translocation into the yeast endoplasmic reticulum. Proc Natl Acad Sci USA. 1995;92(21):9643–9646. doi: 10.1073/pnas.92.21.9643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Chirico WJ, Waters MG, Blobel G. 70K heat shock related proteins stimulate protein translocation into microsomes. Nature. 1988;332(6167):805–810. doi: 10.1038/332805a0. [DOI] [PubMed] [Google Scholar]
- 233.von Heijne G. The signal peptide. J Membr Biol. 1990;115(3):195–201. doi: 10.1007/BF01868635. [DOI] [PubMed] [Google Scholar]
- 234.Doudna JA, Batey RT. Structural insights into the signal recognition particle. Annu Rev Biochem. 2004;73:539–557. doi: 10.1146/annurev.biochem.73.011303.074048. [DOI] [PubMed] [Google Scholar]
- 235.Shan SO, Walter P. Cotranslational protein targeting by the signal recognition particle. FEBS Lett. 2005;579(4):921–926. doi: 10.1016/j.febslet.2004.11.049. [DOI] [PubMed] [Google Scholar]
- 236.Egea PF, Shan SO, Napetschnig J, Savage DF, Walter P, Stroud RM. Substrate twinning activates the signal recognition particle and its receptor. Nature. 2004;427(6971):215–221. doi: 10.1038/nature02250. [DOI] [PubMed] [Google Scholar]
- 237.Focia PJ, Shepotinovskaya IV, Seidler JA, Freymann DM. Heterodimeric GTPase core of the SRP targeting complex. Science. 2004;303(5656):373–377. doi: 10.1126/science.1090827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Menetret JF, Neuhof A, Morgan DG, et al. The structure of ribosome–channel complexes engaged in protein translocation. Mol Cell. 2000;6(5):1219–1232. doi: 10.1016/s1097-2765(00)00118-0. [DOI] [PubMed] [Google Scholar]
- 239.Beckmann R, Spahn CM, Eswar N, et al. Architecture of the protein-conducting channel associated with the translating 80s ribosome. Cell. 2001;107(3):361–372. doi: 10.1016/s0092-8674(01)00541-4. [DOI] [PubMed] [Google Scholar]
- 240.High S, Dobberstein B. Mechanisms that determine the transmembrane disposition of proteins. Curr Opin Cell Biol. 1992;4(4):581–586. doi: 10.1016/0955-0674(92)90075-n. [DOI] [PubMed] [Google Scholar]
- 241.Higy M, Junne T, Spiess M. Topogenesis of membrane proteins at the endoplasmic reticulum. Biochemistry. 2004;43(40):12716–12722. doi: 10.1021/bi048368m. [DOI] [PubMed] [Google Scholar]
- 242.Klappa P, Mayinger P, Pipkorn R, Zimmermann M, Zimmermann R. A microsomal protein is involved in ATP-dependent transport of presecretory proteins into mammalian microsomes. EMBO J. 1991;10(10):2795–2803. doi: 10.1002/j.1460-2075.1991.tb07828.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Hansen W, Walter P. Prepro-carboxypeptidase γ and a truncated form of pre-invertase, but not full-length pre-invertase, can be post-translationally translocated across microsomal vesicle membranes from Saccharomyces cerevisiae. J Cell Biol. 1988;106(4):1075–1081. doi: 10.1083/jcb.106.4.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Schlenstedt G, Gudmundsson GH, Boman HG, Zimmermann R. A large presecretory protein translocates both cotranslationally, using signal recognition particle and ribosome, and post-translationally, without these ribonucleoparticles, when synthesized in the presence of mammalian microsomes. J Biol Chem. 1990;265(23):13960–13968. [PubMed] [Google Scholar]
- 245.Schlenstedt G, Gudmundsson GH, Boman HG, Zimmermann R. Structural requirements for transport of preprocecropina and related presecretory proteins into mammalian microsomes. J Biol Chem. 1992;267(34):24328–24332. [PubMed] [Google Scholar]
- 246.Zimmermann R, Sagstetter M, Lewis MJ, Pelham HR. Seventy-kilodalton heat shock proteins and an additional component from reticulocyte lysate stimulate import of M13 procoat protein into microsomes. EMBO J. 1988;7(9):2875–2880. doi: 10.1002/j.1460-2075.1988.tb03144.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Wilkinson BM, Regnacq M, Stirling CJ. Protein translocation across the membrane of the endoplasmic reticulum. J Membr Biol. 1997;155(3):189–197. doi: 10.1007/s002329900171. [DOI] [PubMed] [Google Scholar]
- 248.Wiech H, Stuart R, Zimmermann R. Role of cytosolic factors in the transport of proteins across membranes. Semin Cell Biol. 1990;1(1):55–63. [PubMed] [Google Scholar]
- 249.Martoglio B, Dobberstein B. Signal sequences: more than just greasy peptides. Trends Cell Biol. 1998;8(10):410–415. doi: 10.1016/s0962-8924(98)01360-9. [DOI] [PubMed] [Google Scholar]
- 250.Hegde RS, Bernstein HD. The surprising complexity of signal sequences. Trends Biochem Sci. 2006;31(10):563–571. doi: 10.1016/j.tibs.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 251.Rutkowski DT, Lingappa VR, Hegde RS. Substrate-specific regulation of the ribosome–translocon junction by N-terminal signal sequences. Proc Natl Acad Sci USA. 2001;98(14):7823–7828. doi: 10.1073/pnas.141125098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Kim SJ, Mitra D, Salerno JR, Hegde RS. Signal sequences control gating of the protein translocation channel in a substrate-specific manner. Dev Cell. 2002;2(2):207–217. doi: 10.1016/s1534-5807(01)00120-4. [DOI] [PubMed] [Google Scholar]
- 253.Voigt S, Jungnickel B, Hartmann E, Rapoport TA. Signal sequence-dependent function of the tram protein during early phases of protein transport across the endoplasmic reticulum membrane. J Cell Biol. 1996;134(1):25–35. doi: 10.1083/jcb.134.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Fons RD, Bogert BA, Hegde RS. Substrate-specific function of the translocon-associated protein complex during translocation across the ER membrane. J Cell Biol. 2003;160(4):529–539. doi: 10.1083/jcb.200210095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Belin D, Bost S, Vassalli JD, Strub K. A two step recognition of signal sequences determines the translocation efficiency of proteins. EMBO J. 1996;15(3):468–478. [PMC free article] [PubMed] [Google Scholar]
- 256.Levine CG, Mitra D, Sharma A, Smith CL, Hegde RS. The efficiency of protein compartmentalization into the secretory pathway. Mol Biol Cell. 2005;16(1):279–291. doi: 10.1091/mbc.E04-06-0508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Shaffer KL, Sharma A, Snapp EL, Hegde RS. Regulation of protein compartmentalization expands the diversity of protein function. Dev Cell. 2005;9(4):545–554. doi: 10.1016/j.devcel.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 258.Besemer J, Harant H, Wang S, et al. Selective inhibition of cotranslational translocation of vascular cell adhesion molecule 1. Nature. 2005;436(7048):290–293. doi: 10.1038/nature03670. [DOI] [PubMed] [Google Scholar]
- 259.Garrison JL, Kunkel EJ, Hegde RS, Taunton J. A substrate-specific inhibitor of protein translocation into the endoplasmic reticulum. Nature. 2005;436(7048):285–289. doi: 10.1038/nature03821. [DOI] [PubMed] [Google Scholar]
- 260.Kelly JW, Balch WE. The integration of cell and chemical biology in protein folding. Nat Chem Biol. 2006;2(5):224–227. doi: 10.1038/nchembio0506-224. [DOI] [PubMed] [Google Scholar]
- 261.Aridor M. Visiting the ER: the endoplasmic reticulum as a target for therapeutics in traffic related diseases. Adv Drug Deliv Rev. 2007;59(8):759–781. doi: 10.1016/j.addr.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 262.Kopito RR. Biosynthesis and degradation of cftr. Physiol Rev. 1999;79(Suppl 1):S167–S173. doi: 10.1152/physrev.1999.79.1.S167. [DOI] [PubMed] [Google Scholar]
- 263.Peters KW, Qi J, Watkins SC, Frizzell RA. Mechanisms underlying regulated CFTR trafficking. Med Clin North Am. 2000;84(3):633–640. doi: 10.1016/s0025-7125(05)70246-7. [DOI] [PubMed] [Google Scholar]
- 264.Brennan SO, Wyatt J, Medicina D, Callea F, George PM. Fibrinogen brescia: hepatic endoplasmic reticulum storage and hypofibrinogenemia because of a γ284 Gly-->Arg mutation. Am J Pathol. 2000;157(1):189–196. doi: 10.1016/s0002-9440(10)64530-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Niwa M, Sidrauski C, Kaufman RJ, Walter P. A role for presenilin-1 in nuclear accumulation of IRE1 fragments and induction of the mammalian unfolded protein response. Cell. 1999;99(7):691–702. doi: 10.1016/s0092-8674(00)81667-0. [DOI] [PubMed] [Google Scholar]
- 266.Nogalska A, Engel WK, McFerrin J, Kokame K, Komano H, Askanas V. Homocysteine-induced endoplasmic reticulum protein (Herp) is up-regulated in sporadic inclusion-body myositis and in endoplasmic reticulum stress-induced cultured human muscle fibers. J Neurochem. 2006;96(5):1491–1499. doi: 10.1111/j.1471-4159.2006.03668.x. [DOI] [PubMed] [Google Scholar]
- 267.Sai X, Kawamura Y, Kokame K, et al. Endoplasmic reticulum stress-inducible protein, herp, enhances presenilin-mediated generation of amyloid β-protein. J Biol Chem. 2002;277(15):12915–12920. doi: 10.1074/jbc.M112372200. [DOI] [PubMed] [Google Scholar]
- 268.Cooper AA, Gitler AD, Cashikar A, et al. α-synuclein blocks ER–Golgi traffic and Rab1 rescues neuron loss in Parkinson’s models. Science. 2006;313(5785):324–328. doi: 10.1126/science.1129462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Taylor SI. Lilly lecture: molecular mechanisms of insulin resistance. Lessons from patients with mutations in the insulin-receptor gene. Diabetes. 1992;41(11):1473–1490. doi: 10.2337/diab.41.11.1473. [DOI] [PubMed] [Google Scholar]
- 270.Kadowaki T, Kadowaki H, Accili D, Yazaki Y, Taylor SI. Substitution of arginine for histidine at position 209 in the α-subunit of the human insulin receptor. A mutation that impairs receptor dimerization and transport of receptors to the cell surface. J Biol Chem. 1991;266(31):21224–21231. [PubMed] [Google Scholar]
- 271.Goda Y, Pfeffer SR. Selective recycling of the mannose 6-phosphate/IGF-II receptor to the trans Golgi network in vitro. Cell. 1988;55(2):309–320. doi: 10.1016/0092-8674(88)90054-2. [DOI] [PubMed] [Google Scholar]
- 272.Ghosh P, Dahms NM, Kornfeld S. Mannose 6-phosphate receptors: new twists in the tale. Nat Rev Mol Cell Biol. 2003;4(3):202–212. doi: 10.1038/nrm1050. [DOI] [PubMed] [Google Scholar]
- 273.Duncan JR, Kornfeld S. Intracellular movement of two mannose 6-phosphate receptors: return to the Golgi apparatus. J Cell Biol. 1988;106(3):617–628. doi: 10.1083/jcb.106.3.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Griffiths G, Hoflack B, Simons K, Mellman I, Kornfeld S. The mannose 6-phosphate receptor and the biogenesis of lysosomes. Cell. 1988;52(3):329–341. doi: 10.1016/s0092-8674(88)80026-6. [DOI] [PubMed] [Google Scholar]
- 275.Geuze HJ, Stoorvogel W, Strous GJ, Slot JW, Bleekemolen JE, Mellman I. Sorting of mannose 6-phosphate receptors and lysosomal membrane proteins in endocytic vesicles. J Cell Biol. 1988;107(6 Pt 2):2491–2501. doi: 10.1083/jcb.107.6.2491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Mallard F, Antony C, Tenza D, Salamero J, Goud B, Johannes L. Direct pathway from early/recycling endosomes to the Golgi apparatus revealed through the study of shiga toxin B-fragment transport. J Cell Biol. 1998;143(4):973–990. doi: 10.1083/jcb.143.4.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Schapiro FB, Lingwood C, Furuya W, Grinstein S. pH-independent retrograde targeting of glycolipids to the Golgi complex. Am J Physiol. 1998;274(2 Pt 1):C319–C332. doi: 10.1152/ajpcell.1998.274.2.C319. [DOI] [PubMed] [Google Scholar]
- 278.Lauvrak SU, Torgersen ML, Sandvig K. Efficient endosome-to-Golgi transport of shiga toxin is dependent on dynamin and clathrin. J Cell Sci. 2004;117(11):2321–2331. doi: 10.1242/jcs.01081. [DOI] [PubMed] [Google Scholar]
- 279.Iversen TG, Skretting G, Llorente A, Nicoziani P, Van Deurs B, Sandvig K. Endosome to Golgi transport of ricin is independent of clathrin and of the Rab9- and Rab11-GTPases. Mol Biol Cell. 2001;12(7):2099–2107. doi: 10.1091/mbc.12.7.2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Grimmer S, Iversen TG, Van Deurs B, Sandvig K. Endosome to Golgi transport of ricin is regulated by cholesterol. Mol Biol Cell. 2000;11(12):4205–4216. doi: 10.1091/mbc.11.12.4205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Stanley KK, Howell KE. Tgn38/41. A molecule on the move. Trends Cell Biol. 1993;3(8):252–255. doi: 10.1016/0962-8924(93)90046-4. [DOI] [PubMed] [Google Scholar]
- 282.Molloy SS, Anderson ED, Jean F, Thomas G. Bi-cycling the furin pathway. From TGN localization to pathogen activation and embryogenesis. Trends Cell Biol. 1999;9(1):28–35. doi: 10.1016/s0962-8924(98)01382-8. [DOI] [PubMed] [Google Scholar]
- 283.Varlamov O, Fricker LD. Intracellular trafficking of metallocarboxypeptidase D in AtT-20 cells. Localization to the trans-Golgi network and recycling from the cell surface. J Cell Sci. 1998;111(7):877–885. doi: 10.1242/jcs.111.7.877. [DOI] [PubMed] [Google Scholar]
- 284.Bos K, Wraight C, Stanley KK. Tgn38 is maintained in the trans-Golgi network by a tyrosine-containing motif in the cytoplasmic domain. EMBO J. 1993;12(5):2219–2228. doi: 10.1002/j.1460-2075.1993.tb05870.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Schafer W, Stroh A, Berghofer S, et al. Two independent targeting signals in the cytoplasmic domain determine trans-Golgi network localization and endosomal trafficking of the proprotein convertase furin. EMBO J. 1995;14(11):2424–2435. doi: 10.1002/j.1460-2075.1995.tb07240.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Voorhees P, Deignan E, Van Donselaar E, et al. An acidic sequence within the cytoplasmic domain of furin functions as a determinant of trans-Golgi network localization and internalization from the cell surface. EMBO J. 1995;14(20):4961–4975. doi: 10.1002/j.1460-2075.1995.tb00179.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Molloy SS, Thomas L, Kamibayashi C, Mumby MC, Thomas G. Regulation of endosome sorting by a specific pp2a isoform. J Cell Biol. 1998;142(6):1399–1411. doi: 10.1083/jcb.142.6.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Dittie AS, Thomas L, Thomas G, Tooze SA. Interaction of furin in immature secretory granules from neuroendocrine cells with the AP-1 adaptor complex is modulated by casein kinase II phosphorylation. EMBO J. 1997;16(16):4859–4870. doi: 10.1093/emboj/16.16.4859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Alconada A, Bauer U, Hoflack B. A tyrosine-based motif and a casein kinase II phosphorylation site regulate the intracellular trafficking of the varicella-zoster virus glycoprotein I, a protein localized in the trans-Golgi network. EMBO J. 1996;15(22):6096–6110. [PMC free article] [PubMed] [Google Scholar]
- 290.Smith DC, Lord JM, Roberts LM, Tartour E, Johannes L. 1st class ticket to class I. Protein toxins as pathfinders for antigen presentation. Traffic. 2002;3(10):697–704. doi: 10.1034/j.1600-0854.2002.31001.x. [DOI] [PubMed] [Google Scholar]
- 291.Lee RS, Tartour E, van der Bruggen P, et al. Major histocompatibility complex class I presentation of exogenous soluble tumor antigen fused to the B-fragment of Shiga toxin. Eur J Immunol. 1998;28(9):2726–2737. doi: 10.1002/(SICI)1521-4141(199809)28:09<2726::AID-IMMU2726>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 292.Haicheur N, Bismuth E, Bosset S, et al. The B subunit of Shiga toxin fused to a tumor antigen elicits CTL and targets dendritic cells to allow MHC class I-restricted presentation of peptides derived from exogenous antigens. J Immunol. 2000;165(6):3301–3308. doi: 10.4049/jimmunol.165.6.3301. [DOI] [PubMed] [Google Scholar]
- 293.Haicheur N, Benchetrit F, Amessou M, et al. The B subunit of shiga toxin coupled to full-size antigenic protein elicits humoral and cell-mediated immune responses associated with a Th1-dominant polarization. Int Immunol. 2003;15(10):1161–1171. doi: 10.1093/intimm/dxg118. [DOI] [PubMed] [Google Scholar]
- 294.Vingert B, Adotevi O, Patin D, et al. The Shiga toxin B-subunit targets antigen in vivo to dendritic cells and elicits anti-tumor immunity. Eur J Immunol. 2006;36(5):1124–1135. doi: 10.1002/eji.200535443. [DOI] [PubMed] [Google Scholar]
- 295.Janssen KP, Vignjevic D, Boisgard R, et al. In vivo tumor targeting using a novel intestinal pathogen-based delivery approach. Cancer Res. 2006;66(14):7230–7236. doi: 10.1158/0008-5472.CAN-06-0631. [DOI] [PubMed] [Google Scholar]
- 296.Kovbasnjuk O, Mourtazina R, Baibakov B, et al. The glycosphingolipid globotriaosylceramide in the metastatic transformation of colon cancer. Proc Natl Acad Sci USA. 2005;102(52):19087–19092. doi: 10.1073/pnas.0506474102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Arab S, Russel E, Chapman WB, Rosen B, Lingwood CA. Expression of the verotoxin receptor glycolipid, globotriaosylceramide, in ovarian hyperplasias. Oncol Res. 1997;9(10):553–563. [PubMed] [Google Scholar]
- 298.Lacasse EC, Bray MR, Patterson B, et al. Shiga-like toxin-1 receptor on human breast cancer, lymphoma, and myeloma and absence from CD34+ hematopoietic stem cells: implications for ex vivo tumor purging and autologous stem cell transplantation. Blood. 1999;94(8):2901–2910. [PubMed] [Google Scholar]
- 299.Lacasse EC, Saleh MT, Patterson B, Minden MD, Gariepy J. Shiga-like toxin purges human lymphoma from bone marrow of severe combined immunodeficient mice. Blood. 1996;88(5):1561–1567. [PubMed] [Google Scholar]
- 300.Arab S, Murakami M, Dirks P, et al. Verotoxins inhibit the growth of and induce apoptosis in human astrocytoma cells. J Neurooncol. 1998;40(2):137–150. doi: 10.1023/a:1006010019064. [DOI] [PubMed] [Google Scholar]
- 301.Salhia B, Rutka JT, Lingwood C, Nutikka A, Van Furth WR. The treatment of malignant meningioma with verotoxin. Neoplasia. 2002;4(4):304–311. doi: 10.1038/sj.neo.7900243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Hicks SW, Machamer CE. Golgi structure in stress sensing and apoptosis. Biochim Biophys Acta. 2005;1744(3):406–414. doi: 10.1016/j.bbamcr.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 303.De Duve C, Baudhuin P. Peroxisomes (microbodies and related particles) Physiol Rev. 1966;46(2):323–357. doi: 10.1152/physrev.1966.46.2.323. [DOI] [PubMed] [Google Scholar]
- 304.Jansen GA, Wanders RJ. α-oxidation. Biochim Biophys Acta. 2006;1763(12):1403–1412. doi: 10.1016/j.bbamcr.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 305.Heiland I, Erdmann R. Biogenesis of peroxisomes. Topogenesis of the peroxisomal membrane and matrix proteins. FEBS J. 2005;272(10):2362–2372. doi: 10.1111/j.1742-4658.2005.04690.x. [DOI] [PubMed] [Google Scholar]
- 306.Gould SG, Keller GA, Subramani S. Identification of a peroxisomal targeting signal at the carboxy terminus of firefly luciferase. J Cell Biol. 1987;105(6 Pt 2):2923–2931. doi: 10.1083/jcb.105.6.2923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Gould SJ, Keller GA, Hosken N, Wilkinson J, Subramani S. A conserved tripeptide sorts proteins to peroxisomes. J Cell Biol. 1989;108(5):1657–1664. doi: 10.1083/jcb.108.5.1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Lametschwandtner G, Brocard C, Fransen M, Van Veldhoven P, Berger J, Hartig A. The difference in recognition of terminal tripeptides as peroxisomal targeting signal 1 between yeast and human is due to different affinities of their receptor Pex5p to the cognate signal and to residues adjacent to it. J Biol Chem. 1998;273(50):33635–33643. doi: 10.1074/jbc.273.50.33635. [DOI] [PubMed] [Google Scholar]
- 309.Brocard C, Hartig A. Peroxisome targeting signal 1: is it really a simple tripeptide? Biochim Biophys Acta. 2006;1763(12):1565–1573. doi: 10.1016/j.bbamcr.2006.08.022. [DOI] [PubMed] [Google Scholar]
- 310.Bongcam V, Macdonald-Comber Petetot J, Mittendorf V, et al. Importance of sequences adjacent to the terminal tripeptide in the import of a peroxisomal candida tropicalis protein in plant peroxisomes. Planta. 2000;211(1):150–157. doi: 10.1007/s004250000312. [DOI] [PubMed] [Google Scholar]
- 311.Marzioch M, Erdmann R, Veenhuis M, Kunau WH. PAS7 encodes a novel yeast member of the WD-40 protein family essential for import of 3-oxoacyl-CoA thiolase, a PTS2-containing protein, into peroxisomes. EMBO J. 1994;13(20):4908–4918. doi: 10.1002/j.1460-2075.1994.tb06818.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Reumann S. Specification of the peroxisome targeting signals type 1 and type 2 of plant peroxisomes by bioinformatics analyses. Plant Physiol. 2004;135(2):783–800. doi: 10.1104/pp.103.035584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Swinkels BW, Gould SJ, Bodnar AG, Rachubinski RA, Subramani S. A novel, cleavable peroxisomal targeting signal at the amino-terminus of the rat 3-ketoacyl-CoA thiolase. EMBO J. 1991;10(11):3255–3262. doi: 10.1002/j.1460-2075.1991.tb04889.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Wanders RJ, Waterham HR. Peroxisomal disorders I: biochemistry and genetics of peroxisome biogenesis disorders. Clin Genet. 2005;67(2):107–133. doi: 10.1111/j.1399-0004.2004.00329.x. [DOI] [PubMed] [Google Scholar]
- 315.McCollum D, Monosov E, Subramani S. The pas8 mutant of Pichia pastoris exhibits the peroxisomal protein import deficiencies of Zellweger syndrome cells – the PAS8 protein binds to the COOH-terminal tripeptide peroxisomal targeting signal, and is a member of the TPR protein family. J Cell Biol. 1993;121(4):761–774. doi: 10.1083/jcb.121.4.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Terlecky SR, Nuttley WM, McCollum D, Sock E, Subramani S. The Pichia pastoris peroxisomal protein PAS8p is the receptor for the C-terminal tripeptide peroxisomal targeting signal. EMBO J. 1995;14(15):3627–3634. doi: 10.1002/j.1460-2075.1995.tb00032.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Keller GA, Gould S, Deluca M, Subramani S. Firefly luciferase is targeted to peroxisomes in mammalian cells. Proc Natl Acad Sci USA. 1987;84(10):3264–3268. doi: 10.1073/pnas.84.10.3264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Goth L. Lipid and carbohydrate metabolism in acatalasemia. Clin Chem. 2000;46(4):564–566. [PubMed] [Google Scholar]
- 319.Fransen M, Terlecky SR, Subramani S. Identification of a human pts1 receptor docking protein directly required for peroxisomal protein import. Proc Natl Acad Sci USA. 1998;95(14):8087–8092. doi: 10.1073/pnas.95.14.8087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Rayapuram N, Subramani S. The importomer – a peroxisomal membrane complex involved in protein translocation into the peroxisome matrix. Biochim Biophys Acta. 2006;1763(12):1613–1619. doi: 10.1016/j.bbamcr.2006.08.035. [DOI] [PubMed] [Google Scholar]
- 321.Leon S, Goodman JM, Subramani S. Uniqueness of the mechanism of protein import into the peroxisome matrix: transport of folded, cofactor-bound and oligomeric proteins by shuttling receptors. Biochim Biophys Acta. 2006;1763(12):1552–1564. doi: 10.1016/j.bbamcr.2006.08.037. [DOI] [PubMed] [Google Scholar]
- 322.Dodt G, Gould SJ. Multiple PEX genes are required for proper subcellular distribution and stability of Pex5p, the PTS1 receptor: evidence that PTS1 protein import is mediated by a cycling receptor. J Cell Biol. 1996;135(6 Pt 2):1763–1774. doi: 10.1083/jcb.135.6.1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.van der Klei IJ, Veenhuis M. Peroxisome biogenesis in the yeast hansenula polymorpha: a structural and functional analysis. Ann NY Acad Sci. 1996;804:47–59. doi: 10.1111/j.1749-6632.1996.tb18607.x. [DOI] [PubMed] [Google Scholar]
- 324.Nair DM, Purdue PE, Lazarow PB. Pex7p translocates in and out of peroxisomes in Saccharomyces cerevisiae. J Cell Biol. 2004;167(4):599–604. doi: 10.1083/jcb.200407119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Dammai V, Subramani S. The human peroxisomal targeting signal receptor, Pex5p, is translocated into the peroxisomal matrix and recycled to the cytosol. Cell. 2001;105(2):187–196. doi: 10.1016/s0092-8674(01)00310-5. [DOI] [PubMed] [Google Scholar]
- 326.Dyer JM, McNew JA, Goodman JM. The sorting sequence of the peroxisomal integral membrane protein PMP47 is contained within a short hydrophilic loop. J Cell Biol. 1996;133(2):269–280. doi: 10.1083/jcb.133.2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Pause B, Saffrich R, Hunziker A, Ansorge W, Just WW. Targeting of the 22 kDa integral peroxisomal membrane protein. FEBS Lett. 2000;471(1):23–28. doi: 10.1016/s0014-5793(00)01332-6. [DOI] [PubMed] [Google Scholar]
- 328.Honsho M, Fujiki Y. Topogenesis of peroxisomal membrane protein requires a short, positively charged intervening-loop sequence and flanking hydrophobic segments. Study using human membrane protein PMP34. J Biol Chem. 2001;276(12):9375–9382. doi: 10.1074/jbc.M003304200. [DOI] [PubMed] [Google Scholar]
- 329.Honsho M, Hiroshige T, Fujiki Y. The membrane biogenesis peroxin Pex16p. Topogenesis and functional roles in peroxisomal membrane assembly. J Biol Chem. 2002;277(46):44513–44524. doi: 10.1074/jbc.M206139200. [DOI] [PubMed] [Google Scholar]
- 330.Hoepfner D, Schildknegt D, Braakman I, Philippsen P, Tabak HF. Contribution of the endoplasmic reticulum to peroxisome formation. Cell. 122(1):85–95. 20050. doi: 10.1016/j.cell.2005.04.025. [DOI] [PubMed] [Google Scholar]
- 331.Voorn-Brouwer T, Kragt A, Tabak HF, Distel B. Peroxisomal membrane proteins are properly targeted to peroxisomes in the absence of COPI- and COPII-mediated vesicular transport. J Cell Sci. 2001;114(11):2199–2204. doi: 10.1242/jcs.114.11.2199. [DOI] [PubMed] [Google Scholar]
- 332.South ST, Sacksteder KA, Li X, Liu Y, Gould SJ. Inhibitors of COPI and COPII do not block PEX3-mediated peroxisome synthesis. J Cell Biol. 2000;149(7):1345–1360. doi: 10.1083/jcb.149.7.1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Terlecky SR, Koepke JI. Drug delivery to peroxisomes: employing unique trafficking mechanisms to target protein therapeutics. Adv Drug Deliv Rev. 2007;59(8):739–747. doi: 10.1016/j.addr.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 334.Nalepa G, Rolfe M, Harper JW. Drug discovery in the ubiquitin-proteasome system. Nat Rev Drug Discov. 2006;5(7):596–613. doi: 10.1038/nrd2056. [DOI] [PubMed] [Google Scholar]
- 335.Dahlmann B. Role of proteasomes in disease. BMC Biochem. 2007;8(1):S3. doi: 10.1186/1471-2091-8-S1-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Elliott PJ, Ross JS. The proteasome: a new target for novel drug therapies. Am J Clin Pathol. 2001;116(5):637–646. doi: 10.1309/44HW-5YCJ-FLLP-3R56. [DOI] [PubMed] [Google Scholar]
- 337.Richardson PG, Barlogie B, Berenson J, et al. A Phase 2 study of bortezomib in relapsed, refractory myeloma. N Engl J Med. 2003;348(26):2609–2617. doi: 10.1056/NEJMoa030288. [DOI] [PubMed] [Google Scholar]
- 338.Kyle RA, Rajkumar SV. Multiple myeloma. N Engl J Med. 2004;351(18):1860–1873. doi: 10.1056/NEJMra041875. [DOI] [PubMed] [Google Scholar]
- 339.Adams J. The development of proteasome inhibitors as anticancer drugs. Cancer Cell. 2004;5(5):417–421. doi: 10.1016/s1535-6108(04)00120-5. [DOI] [PubMed] [Google Scholar]
- 340.Burger AM, Seth AK. The ubiquitin-mediated protein degradation pathway in cancer: therapeutic implications. Eur J Cancer. 2004;40(15):2217–2229. doi: 10.1016/j.ejca.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 341.Robinson PA, Ardley HC. Ubiquitin-protein ligases – novel therapeutic targets? Curr Protein Pept Sci. 2004;5(3):163–176. doi: 10.2174/1389203043379800. [DOI] [PubMed] [Google Scholar]
- 342.Honda R, Yasuda H. Association of p19(ARF) with Mdm2 inhibits ubiquitin ligase activity of Mdm2 for tumor suppressor p53. EMBO J. 1999;18(1):22–27. doi: 10.1093/emboj/18.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Lowe SW, Sherr CJ. Tumor suppression by Ink4a-Arf: progress and puzzles. Curr Opin Genet Dev. 2003;13(1):77–83. doi: 10.1016/s0959-437x(02)00013-8. [DOI] [PubMed] [Google Scholar]
- 344.Harris SL, Levine AJ. The p53 pathway: positive and negative feedback loops. Oncogene. 2005;24(17):2899–2908. doi: 10.1038/sj.onc.1208615. [DOI] [PubMed] [Google Scholar]
- 345■.Wagner E. Strategies to improve DNA polyplexes for in vivo gene transfer: will “artificial viruses” be the answer? Pharm Res. 2004;21(1):8–14. doi: 10.1023/b:pham.0000012146.04068.56. Discusses the use of concepts borrowed from viruses for improved DNA delivery. [DOI] [PubMed] [Google Scholar]
- 346.Lee ES, Kim D, Youn YS, Oh KT, Bae YH. A virus-mimetic nanogel vehicle. Angew Chem Int Ed Engl. 2008;47(13):2418–2421. doi: 10.1002/anie.200704121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Li Z, Zhang Y, Wurtz W, et al. Characterization of nebulized liposomal amikacin (arikace) as a function of droplet size. J Aerosol Med Pulm Drug Deliv. 2008;21(3):245–254. doi: 10.1089/jamp.2008.0686. [DOI] [PubMed] [Google Scholar]
- 348.Venkataram S, Awni WM, Jordan K, Rahman YE. Pharmacokinetics of two alternative dosage forms for cyclosporine: liposomes and intralipid. J Pharm Sci. 1990;79(3):216–219. doi: 10.1002/jps.2600790307. [DOI] [PubMed] [Google Scholar]
- 349.James ND, Coker RJ, Tomlinson D, et al. Liposomal doxorubicin (Doxil): an effective new treatment for Kaposi’s sarcoma in aids. Clin Oncol (R Coll Radiol) 1994;6(5):294–296. doi: 10.1016/s0936-6555(05)80269-9. [DOI] [PubMed] [Google Scholar]
- 350.Lutwyche P, Cordeiro C, Wiseman DJ, et al. Intracellular delivery and antibacterial activity of gentamicin encapsulated in pH-sensitive liposomes. Antimicrob Agents Chemother. 1998;42(10):2511–2520. doi: 10.1128/aac.42.10.2511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Han HD, Shin BC, Choi HS. Doxorubicin-encapsulated thermosensitive liposomes modified with poly(n-isopropylacrylamide-co-acrylamide): drug release behavior and stability in the presence of serum. Eur J Pharm Biopharm. 2006;62(1):110–116. doi: 10.1016/j.ejpb.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 352.Pradhan P, Banerjee R, Bahadur D, Koch C, Mykhaylyk O, Plank C. Targeted magnetic liposomes loaded with doxorubicin. Methods Mol Biol. 2010;605:279–293. doi: 10.1007/978-1-60327-360-2_19. [DOI] [PubMed] [Google Scholar]
- 353.Pradhan P, Giri J, Rieken F, et al. Targeted temperature sensitive magnetic liposomes for thermo-chemotherapy. J Control Release. 2009;142(1):108–121. doi: 10.1016/j.jconrel.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 354.Yokoyama M, Miyauchi M, Yamada N, et al. Characterization and anticancer activity of the micelle-forming polymeric anticancer drug adriamycin-conjugated poly(ethylene glycol)-poly(aspartic acid) block copolymer. Cancer Res. 1990;50(6):1693–1700. [PubMed] [Google Scholar]
- 355.Alani AW, Bae Y, Rao DA, Kwon GS. Polymeric micelles for the pH-dependent controlled, continuous low dose release of paclitaxel. Biomaterials. 2010;31(7):1765–1772. doi: 10.1016/j.biomaterials.2009.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Bae Y, Nishiyama N, Kataoka K. In vivo antitumor activity of the folate-conjugated pH-sensitive polymeric micelle selectively releasing adriamycin in the intracellular acidic compartments. Bioconjug Chem. 2007;18(4):1131–1139. doi: 10.1021/bc060401p. [DOI] [PubMed] [Google Scholar]
- 357.Masaki T, Rathi R, Zentner G, et al. Inhibition of neointimal hyperplasia in vascular grafts by sustained perivascular delivery of paclitaxel. Kidney Int. 2004;66(5):2061–2069. doi: 10.1111/j.1523-1755.2004.00985.x. [DOI] [PubMed] [Google Scholar]
- 358.Nori A, Jensen KD, Tijerina M, Kopeckova P, Kopecek J. Subcellular trafficking of HPMA copolymer–Tat conjugates in human ovarian carcinoma cells. J Control Release. 2003;91(1–2):53–59. doi: 10.1016/s0168-3659(03)00213-x. [DOI] [PubMed] [Google Scholar]
- 359.Jeong JH, Song SH, Lim DW, Lee H, Park TG. DNA transfection using linear poly(ethylenimine) prepared by controlled acid hydrolysis of poly(2-ethyl-2-oxazoline) J Control Release. 2001;73(2–3):391–399. doi: 10.1016/s0168-3659(01)00310-8. [DOI] [PubMed] [Google Scholar]
- 360.Meunier L, Mayer R, Monsigny M, Roche AC. The nuclear export signal-dependent localization of oligonucleopeptides enhances the inhibition of the protein expression from a gene transcribed in cytosol. Nucleic Acids Res. 1999;27(13):2730–2736. doi: 10.1093/nar/27.13.2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Collas P, Alestrom P. Nuclear localization signal of SV40 T antigen directs import of plasmid DNA into sea urchin male pronuclei in vitro. Mol Reprod Dev. 1996;45(4):431–438. doi: 10.1002/(SICI)1098-2795(199612)45:4<431::AID-MRD4>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 362.Collas P, Husebye H, Alestrom P. The nuclear localization sequence of the SV40 T antigen promotes transgene uptake and expression in zebrafish embryo nuclei. Transgenic Res. 1996;5(6):451–458. doi: 10.1007/BF01980210. [DOI] [PubMed] [Google Scholar]
- 363.Ritter W, Plank C, Lausier J, et al. A novel transfecting peptide comprising a tetrameric nuclear localization sequence. J Mol Med. 2003;81(11):708–717. doi: 10.1007/s00109-003-0483-2. [DOI] [PubMed] [Google Scholar]
- 364.Aronsohn AI, Hughes JA. Nuclear localization signal peptides enhance cationic liposome-mediated gene therapy. J Drug Target. 1998;5(3):163–169. doi: 10.3109/10611869808995871. [DOI] [PubMed] [Google Scholar]
- 365.Keller M, Harbottle RP, Perouzel E, et al. Nuclear localisation sequence templated nonviral gene delivery vectors. Investigation of intracellular trafficking events of LMD and LD vector systems. Chembiochem. 2003;4(4):286–298. doi: 10.1002/cbic.200390049. [DOI] [PubMed] [Google Scholar]
- 366.Chan CK, Jans DA. Enhancement of polylysine–mediated transferrinfection by nuclear localization sequences: polylysine does not function as a nuclear localization sequence. Hum Gene Ther. 1999;10(10):1695–1702. doi: 10.1089/10430349950017699. [DOI] [PubMed] [Google Scholar]
- 367.Subramanian A, Ranganathan P, Diamond SL. Nuclear targeting peptide scaffolds for lipofection of nondividing mammalian cells. Nat Biotechnol. 1999;17(9):873–877. doi: 10.1038/12860. [DOI] [PubMed] [Google Scholar]
- 368.Cutrona G, Boffa LC, Mariani MR, et al. The peptide nucleic acid targeted to a regulatory sequence of the translocated c-myc oncogene in Burkitt’s lymphoma lacks immunogenicity: follow-up characterization of PNAEmu-NLS. Oligonucleotides. 2007;17(1):146–150. doi: 10.1089/oli.2007.9999. [DOI] [PubMed] [Google Scholar]
- 369.Rasmussen FW, Bendifallah N, Zachar V, et al. Evaluation of transfection protocols for unmodified and modified peptide nucleic acid (PNA) oligomers. Oligonucleotides. 2006;16(1):43–57. doi: 10.1089/oli.2006.16.43. [DOI] [PubMed] [Google Scholar]
- 370.Cogoi S, Codognotto A, Rapozzi V, Xodo LE. Antigene property of PNA conjugated to the nuclear localization signal peptide. Nucleosides Nucleotides Nucleic Acids. 2005;24(5–7):971–974. doi: 10.1081/ncn-200059333. [DOI] [PubMed] [Google Scholar]
- 371.Cogoi S, Codognotto A, Rapozzi V, Meeuwenoord N, van der Marel G, Xodo LE. Transcription inhibition of oncogenic KRAS by a mutation-selective peptide nucleic acid conjugated to the PKKKRKV nuclear localization signal peptide. Biochemistry. 2005;44(31):10510–10519. doi: 10.1021/bi0505215. [DOI] [PubMed] [Google Scholar]
- 372.Roulon T, Helene C, Escude C. Coupling of a targeting peptide to plasmid DNA using a new type of padlock oligonucleotide. Bioconjug Chem. 2002;13(5):1134–1139. doi: 10.1021/bc025551o. [DOI] [PubMed] [Google Scholar]
- 373.Ludtke JJ, Zhang G, Sebestyen MG, Wolff JA. A nuclear localization signal can enhance both the nuclear transport and expression of 1 kb DNA. J Cell Sci. 1999;112(Pt 12):2033–2041. doi: 10.1242/jcs.112.12.2033. [DOI] [PubMed] [Google Scholar]
- 374.Jiang J, Stoyanovsky DA, Belikova NA, et al. A mitochondria-targeted triphenylphosphonium-conjugated nitroxide functions as a radioprotector/mitigator. Radiat Res. 2009;172(6):706–717. doi: 10.1667/RR1729.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375.Ngen EJ, Rajaputra P, You Y. Evaluation of delocalized lipophilic cationic dyes as delivery vehicles for photosensitizers to mitochondria. Bioorg Med Chem. 2009;17(18):6631–6640. doi: 10.1016/j.bmc.2009.07.074. [DOI] [PubMed] [Google Scholar]
- 376.Boddapati SV, D’souza GG, Erdogan S, Torchilin VP, Weissig V. Organelle-targeted nanocarriers: specific delivery of liposomal ceramide to mitochondria enhances its cytotoxicity in vitro and in vivo. Nano Lett. 2008;8(8):2559–2563. doi: 10.1021/nl801908y. [DOI] [PubMed] [Google Scholar]
- 377.Takaya K, Higuchi Y, Kitamoto K, Arioka M. A cytosolic phospholipase A2-like protein in the filamentous fungus aspergillus oryzae localizes to the intramembrane space of the mitochondria. FEMS Microbiol Lett. 2009;301(2):201–209. doi: 10.1111/j.1574-6968.2009.01818.x. [DOI] [PubMed] [Google Scholar]
- 378.Shokolenko IN, Alexeyev MF, Ledoux SP, Wilson GL. Tat-mediated protein transduction and targeted delivery of fusion proteins into mitochondria of breast cancer cells. DNA Repair (Amst) 2005;4(4):511–518. doi: 10.1016/j.dnarep.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 379.Meton I, Egea M, Fernandez F, Eraso MC, Baanante IV. The N-terminal sequence directs import of mitochondrial alanine aminotransferase into mitochondria. FEBS Lett. 2004;566(1–3):251–254. doi: 10.1016/j.febslet.2004.04.051. [DOI] [PubMed] [Google Scholar]
- 380.Rane NS, Chakrabarti O, Feigenbaum L, Hegde RS. Signal sequence insufficiency contributes to neurodegeneration caused by transmembrane prion protein. J Cell Biol. 2010;188(4):515–526. doi: 10.1083/jcb.200911115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381.Angelotti T, Daunt D, Shcherbakova OG, Kobilka B, Hurt CM. Regulation of G-protein coupled receptor traffic by an evolutionary conserved hydrophobic signal. Traffic. 2010;11(4):560–578. doi: 10.1111/j.1600-0854.2010.01033.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Futatsumori-Sugai M, Tsumoto K. Signal peptide design for improving recombinant protein secretion in the baculovirus expression vector system. Biochem Biophys Res Commun. 2010;391(1):931–935. doi: 10.1016/j.bbrc.2009.11.167. [DOI] [PubMed] [Google Scholar]
- 383.Loera-Arias MJ, Martinez-Perez AG, Barrera-Hernandez A, et al. Targeting and retention of HPV16 E7 to the endoplasmic reticulum enhances immune tumor protection. J Cell Mol Med. 2009 doi: 10.1111/j.1582-4934.2009.00934.x. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 384.Snyder HL, Yewdell JW, Bennink JR. Trimming of antigenic peptides in an early secretory compartment. J Exp Med. 1994;180(6):2389–2394. doi: 10.1084/jem.180.6.2389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.Levelt CN, De Jong YP, Mizoguchi E, et al. High- and low-affinity single-peptide/MHC ligands have distinct effects on the development of mucosal CD8αα and CD8αβ T lymphocytes. Proc Natl Acad Sci USA. 1999;96(10):5628–5633. doi: 10.1073/pnas.96.10.5628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386.Krajcsi P, Tollefson AE, Anderson CW, Wold WS. The adenovirus E3 14.5-kilodalton protein, which is required for down-regulation of the epidermal growth factor receptor and prevention of tumor necrosis factor cytolysis, is an integral membrane protein oriented with its C terminus in the cytoplasm. J Virol. 1992;66(3):1665–1673. doi: 10.1128/jvi.66.3.1665-1673.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387.Zou Z, Sun PD. An improved recombinant mammalian cell expression system for human transforming growth factor-β2 and -β3 preparations. Protein Expr Purif. 2006;50(1):9–17. doi: 10.1016/j.pep.2006.06.022. [DOI] [PubMed] [Google Scholar]
- 388.Wood CS, Koepke JI, Teng H, et al. Hypocatalasemic fibroblasts accumulate hydrogen peroxide and display age–associated pathologies. Traffic. 2006;7(1):97–107. doi: 10.1111/j.1600-0854.2005.00358.x. [DOI] [PubMed] [Google Scholar]
- 389.Koepke JI, Nakrieko KA, Wood CS, et al. Restoration of peroxisomal catalase import in a model of human cellular aging. Traffic. 2007;8(11):1590–1600. doi: 10.1111/j.1600-0854.2007.00633.x. [DOI] [PubMed] [Google Scholar]
- 390.Lisenbee CS, Lingard MJ, Trelease RN. Arabidopsis peroxisomes possess functionally redundant membrane and matrix isoforms of monodehydroascorbate reductase. Plant J. 2005;43(6):900–914. doi: 10.1111/j.1365-313X.2005.02503.x. [DOI] [PubMed] [Google Scholar]
- 391.Mizuno T, Ito K, Uchida C, et al. Analyses in transfected cells and in vitro of a putative peroxisomal targeting signal of rat liver serine: pyruvate aminotransferase. Histochem Cell Biol. 2002;118(4):321–328. doi: 10.1007/s00418-002-0455-6. [DOI] [PubMed] [Google Scholar]
- 392.Horiguchi H, Yurimoto H, Goh T, Nakagawa T, Kato N, Sakai Y. Peroxisomal catalase in the methylotrophic yeast Candida boidinii: transport efficiency and metabolic significance. J Bacteriol. 2001;183(21):6372–6383. doi: 10.1128/JB.183.21.6372-6383.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Website
- 401.PTS1 Predictor. http://mendel.imp.ac.at/pts1/