Abstract
Although vaccines against influenza A virus are the most effective method to combat infection, it is clear that their production needs to be accelerated and their efficacy improved. We generated live attenuated human influenza A vaccines (LAIVs) by rationally engineering mutations directly into the genome of a pandemic-H1N1 virus. Two LAIVs (NS1-73 and NS1-126) were based on the success of LAIVs for animal influenza A viruses. A third candidate (NSΔ5) is a unique NS-mutant that has never been used as a LAIV. The vaccine potential of each LAIV was determined through analysis of attenuation, interferon production, immunogenicity, and their ability to protect mice and ferrets. This study demonstrates that NSΔ5 is an ideal LAIV candidate, provides important information on the effects that different NS mutations have on the pandemic-H1N1 virus and shows that LAIVs can be engineered directly from the genomes of emerging/circulating influenza A viruses.
Keywords: Influenza A virus, live attenuated vaccine, Nonstructural protein
1. Introduction
Influenza A viruses are highly contagious human and animal pathogens in the family Orthomyxoviridae. Annual influenza A epidemics result in 250-500 million infections, which cause 250,000-500,000 fatalities worldwide [1]. The influenza A viral genome is composed of eight negative sense single-stranded RNA segments (vRNAs) that together encode 10-11 proteins [2]. Influenza A virus vaccines have to be updated frequently because of “antigenic drift” variants that escape antibody neutralization and rapidly displace the previously circulating strains. We also need to swiftly generate vaccines to combat unpredictable intermittent influenza A virus pandemics (e.g., 1918 (H1N1), 1957 (H2N2), and 1968 (H3N2)), which are caused by “antigenic shift” viruses that can emerge from animal reservoirs [3]. An error-prone RNA-dependent RNA polymerase, large and diverse viral reservoirs, frequent interspecies transmission, and reassortment of the segmented RNA genome during co-infections are powerful evolutionary mechanisms that make influenza A viruses extremely challenging pathogens to predict or to control with antivirals or vaccines.
The unique influenza A virus responsible for the 2009 pandemic provides the most recent example of the evolution and rapid dissemination of a pandemic virus. In late April 2009, the first H1N1 pandemic (H1N1pdm) isolate was identified at the Centers for Disease Control and Prevention (CDC) in the United States, and sequence analysis indicated it to be a quadruple reassortant virus. The genomic vRNAs of the H1N1pdm virus were originally derived from North American classical swine viruses (HA, NP, NS), North American human H3N2 viruses (PB1), North American avian viruses (PB2, PA), and Eurasian avian-like swine viruses (NA, M) [4]. Because the H1N1pdm was antigenically distinct from the seasonal H1N1 virus that has circulated in humans since its re-introduction in 1977, there was little pre-existing immunity to the H1N1pdm in the human population, particularly among individuals born after 1950 [5]. Thus, the H1N1pdm virus spread globally, resulting in millions of infections and tens of thousands of deaths [6]. Prior investments in pandemic preparedness provided an increased global capacity for production of large quantities of H1N1pdm vaccines, and the extraordinary efforts of many health care professionals yielded a safe and fairly effective vaccine by the fall of 2009. However, the lack of H1N1pdm vaccine for the first 2009 winter season in the Southern hemisphere and the shortage of vaccine early in the 2009/2010 influenza season in the Northern hemisphere illustrate the need to develop methods to improve influenza A virus vaccine production.
The H1N1pdm vaccines approved for human use by the United States Food and Drug Administration are either inactivated split vaccines, which represent the majority of the vaccines currently administered, or live attenuated influenza virus vaccines (LAIVs). Both the inactivated vaccines and LAIVs are produced by creating reassortant viruses that generally contain six vRNAs (PB2, PB1, PA, NP, M and NS) from a master donor strain, plus the two glycoprotein vRNAs (HA and NA) from a virus that antigenically matches the strain predicted to circulate in upcoming influenza season (e.g. A/CA/07/2009). The reassortant vaccine seed stocks are prepared using both classical reassortment techniques and increasingly by the use of plasmid-based reverse-genetics. Although reverse genetics has enhanced our ability to generate influenza virus vaccines, the current LAIV and inactivated approaches both require significant lead time for vaccine production, and it is clear that innovative strategies need to be developed and tested in animal models [7;8].
In the present study we used multi-segment reverse transcription polymerase chain reaction (M-RTPCR) and accelerated reverse-genetics technology [9] to rapidly engineer interferon (IFN)-inducing and attenuating phenotypes into the natural gene constellation of the novel H1N1pdm virus. The NS1 protein of influenza A virus is a multifunctional protein that plays important roles in virus replication and as potent type I IFN antagonist [10;11]. Mutations and/or deletions in NS1 typically induce stronger IFN responses by the host; those in turn suppress the replication of influenza virus [10-14] and can enhance immune recognition [15-18]. Carboxy terminal deletions in the influenza A NS1 protein have been successfully exploited to create experimental LAIVs for avian, equine, and swine influenza A viruses [19-24]. However, some of the ideal NS-based LAIVs (NS-LAIVs) for these animal viruses have different NS1 deletions due to the influence of strain specific variation in the NS gene, virus lineage, and gene constellation. The H1N1pdm is a novel reassortant, and its NS1 protein has unique properties that distinguish it from the NS1 proteins of typical influenza A viruses (e.g., it lacks 11 residues at the C-terminus), so the mutations required to generate the optimal H1N1pdm NS-LAIV candidate were unknown. Therefore, we created a panel of experimental H1N1pdm NS-LAIV candidates that have different deletions in the NS vRNA and analyzed the vaccine potential of each NS-LAIV in vitro and in vivo to identify the best candidate(s).
2. Materials and Methods
2.1 Biosafety and Animal Care
All experiments with infectious virus were performed using procedures and facilities that met or exceeded the requirements set forth by the U.S. Department of Health and Human Services for propagation of influenza A viruses. In vitro experiments with infectious H1N1pdm viruses were conducted using enhanced biosafety level 2 laboratory practices and procedures as described by the Centers for Disease Control and Prevention interim biosafety guidelines. Experiments involving animals were performed in a biosafety level 3 containment laboratory approved for such use by the Centers for Disease Control and Prevention and the U.S. Department of Agriculture.
The animal studies were conducted under approved animal care and use protocols at the Wadsworth Center, NYSDOH, and at the U.S. Centers for Disease Control and Prevention. All animal experiments were conducted in compliance with the requirements of federal and state regulatory agencies and used husbandry and procedures to limit discomfort, distress, pain or injury.
2.2. Cell Culture
Human embryonic kidney (293T) cells were maintained in Dulbecco's modified Eagle's medium (DMEM) supplemented with 10% fetal bovine serum (FBS). Madin-Darby canine kidney (MDCK) cells and human lung adenocarcinoma (A549) cells were maintained in Eagle's minimum essential medium (EMEM), supplemented with FBS (5% for MDCK and 10% for A549).
2.3 Generation and Propagation of Recombinant Viruses
WT H1N1pdm influenza A virus A/New York/1682/2009 (NY1682) was created by reverse-genetics directly from a human swab specimen collected in New York state in April 2009 [9]. Deletions were introduced into the NY1682 NS plasmid to generate the three mutant NS segments: NS1-73, NS1-126, and NSΔ5 (Fig. 1A). Nucleotides 246 to 482 (cDNA of NS segment) were replaced by stop codons to generate NS1-73; nucleotides 405 to 482 were replaced by stop codons to generate NS1-126; nucleotides 612 to 626 were deleted and the open reading frames for NS1 and NEP were maintained to generate NSΔ5. Recombinant viruses NY1682 WT, NS1-73, NS1-126, and NSΔ5 were generated by co-transfection of eight reverse-genetics plasmids carrying the cDNA of each gene segment into 293T/MDCK co-cultured monolayer adapted from Hoffmann et al. [25]. Briefly, 0.6 μg of plasmid for each gene segment was mixed and incubated with 15 μl of lipofectamine 2000 (Invitrogen, Carlsbad, CA) at 20°C for 20 min. The lipofectamine-DNA mixture was transferred to 90% confluent 293T/MDCK cell co-cultures in a 35mm tissue culture dish and incubated at 33°C with 5% CO2 for 8h. Transfection supernatant was replaced with 3 ml of Opti-MEM I medium (Invitrogen) supplemented with 0.3% BSA fraction V (Invitrogen), 3 μg/ml TPCK-trypsin (Worthington, Lakewood, NJ) and 1% antibiotic-antimycotic (Invitrogen). Three days post transfection, supernatant was collected and viruses were propagated in MDCK cells at 33°C (P1 stock). Viral stocks (P2 stock) for animal studies were generated by propagation of the P1 stocks at a multiplicity of infection (MOI) of 0.01 TCID50/cell, in MDCK cells, at 33°C. Titers of the viruses used in this study were determined by 50% tissue culture infectious dose (TCID50) or plaque assay in MDCK cells. The TCID50 assay was more accurate and consistent for determination of the titer of NS-mutants; because they have a small-plaque phenotype.
Fig. 1. Engineering NS-LAIV candidates and controls.
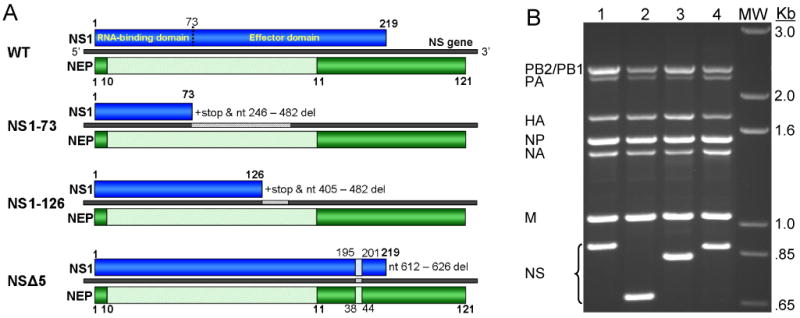
(A) Schematic diagram NS antigenomic RNA (positive sense, cRNA) depicting the WT H1N1pdm and the attenuating NS mutations designed to create NS-LAIV candidates. NS1 protein is directly translated from the full length mRNA and is shown on the top of the gene; NEP protein is translated from spliced mRNA and is illustrated below the gene. Selected amino acid positions are labeled for NS1 and NEP. LAIV candidates NS1-73, NS1-126 express truncated NS1 but intact NEP; NSΔ5 expresses NS1 and NEP proteins each having a five amino acid in-frame deletion. (B) Genomic amplification of the WT and NS-LAIV candidates. The viral genomes were amplified by M-RTPCR and the length of the NS vRNA amplicons was examined by subsequent agarose gel electrophoresis and staining with ethidium bromide. Lane 1, WT; Lane 2, NS1-73; Lane 3, NS1-126; Lane 4, NSΔ5; lane MW, 1Kb+ DNA ladder (Invitrogen). The viral gene segment amplified is listed to the left and length of DNA marker ladder is shown on the right.
2.4 Replication Kinetics in Cell Cultures
Confluent monolayers of MDCK cells were infected at an MOI of 0.002 TCID50/cell with recombinant NY1682 wild-type (WT) or any of the NS-LAIV candidates at 33°C in triplicate. One hour post infection (hpi), inocula were removed, and cells were washed twice and EMEM supplemented with 0.15% BSA fraction V, 3 μg/ml TPCK-trypsin, and 1% antibiotic-antimycotic was added. Supernatants were collected at 2, 12, 24, 48, and 72 hpi. Infection of A549 cells was performed similarly, except that a MOI of 0.01 TCID50/cell was used, and the virus growth medium was EMEM supplemented with 0.3% BSA fraction V, 2 μg/ml TPCK-trypsin and 1% antibiotic-antimycotic.
2.5 Assays for Type I IFN and IFN Stimulated Genes
For the VSV-GFP virus mediated bioassay, A549 cells were inoculated with one of the recombinant influenza viruses at an MOI of 4 TCID50/cell, or were mock-inoculated; supernatants were then collected at 8, 16 and 24 hpi. Supernatants were treated with UV-irradiation to inactivate viruses and were then transferred to naïve A549 cells. Following 24 h of incubation at 37°C, supernatants were removed, and the cells were inoculated with VSV-GFP virus [26], at a MOI of 2 TCID50/cell. GFP expression in the cells was examined by fluorescence microscopy 4 hpi with VSV-GFP.
RT-PCR detection of IFN-β mRNA in cells inoculated with the various influenza A viruses at 24 hpi. Total RNA was purified using TRIzol reagent (Invitrogen) and 80 ng was used as template for RT-PCR using the Qiagen OneStep RT-PCR kit (Qiagen, Valencia, CA). The primers for IFN-β were hIFNBF1 (5′-GGCCATGACCAACAAGTGTCTCCTCC-3′) and hIFNBR1 (5′-GCGCTCAGTTTCGGAGGTAACCTGT-3′) [27]; for GAPDH were G3P-279 (5′-CATCACCATCTTCCAGGAGC-3′) and G3P-1069R (5′-CTTACTCCTTGGAGGCCATG-3′) [28]. For both targets, RT-PCR parameters were: 50°C for 30 min, 95°C for 15 min, and then 28 cycles of 94°C for 30 s, 54°C for 30 s, and 72°C for 1 min, followed by a final extension at 72°C for 10min.
Quantitative RT-PCR assays for mRNA of IFN-β and IFN stimulated genes (ISGs) in A549 cells inoculated with one of the recombinant viruses at MOI of 4 TCID50/cell. At 4, 8, 12, and 16 hpi, total RNA was extracted from cells using TRIzol reagent (Invitrogen). 3-5 μg of total RNA was used to generate cDNA with RevertAid reverse transcriptase (Fermentas, Glen Burnie, MD) and oligo-dT primers in a total volume of 20 μl, according to the manufacturer's protocol. 0.25 μl of cDNA, 0.5μl of 10μM gene specific primer mix, and 5 μl of Brilliant II SYBR Green qPCR Mastermix (Agilent, Santa Clara, CA) were used as template for qPCR in a total volume of 10 μl. Reaction and analysis were performed on a LightCycler 480 (Roche, Indianapolis, IN). The mRNA levels were normalized to 18S rRNA levels, and were expressed as the fold increase relative to the average level for that RNA in the mock-inoculated samples collected at all time points. The N-fold expression values were calculated according to the 2−ΔΔCT method [29]. Each of three biological replicates was measured in technical triplicates. The primers used for the analysis were IFNBfw (5′-TCTGGCACAACAGGTAGTAGGC-3′), IFNBrev (5′GAGAAGCACAACAGGAGAGCAA-3′), IL29fw (5′-GCCCCCAAAAAGGAGTCCG-3′), IL29rev (5′-AGGTTCCCATCGGCCACATA-3′), MXAfw (5′-GTTTCCGAAGTGGACATCGCA-3′), MXArev(5′-GAAGGGCAACTCCTGACAGT-3′), IP10fw (5′-GGAACCTCCAGTCTCAGCACCA-3′), IP10rev (5′-AGACATCTCTTCTCACCCTTC-3′), and 18SrRNAfw (5′-GTAACCCGTTGAACCCCATT-3′), 18SrRNArev (5′-CCATCCAATCGGTAGTAGCG-3′).
2.6 Mouse Studies
Virus attenuation was studied in 6-week-old female BALB/cJ mice (Jackson Laboratory, Bar Harbor, ME), that had been separated into microisolator cages at 5-weeks of age and allowed to acclimate to the ABSL3 laboratory for 6-8 days prior to the studies. Groups of 6-week-old female BALB/cJ were anesthetized with isoflurane and inoculated intranasally with 105 TCID50 of each recombinant virus in 20 μl of PBS diluent, or mock inoculated with PBS to serve as controls. Body weights and clinical symptoms of the mice were monitored daily for 10 days. Nine mice in each group were euthanized on 1, 2 and 5 days post inoculation (dpi). Nasal washes (9 mice/group) were collected by insertion of a 26-gauge needle into the trachea and washing of the nasal turbinates with 1 ml of virus collection medium (VCM: EMEM supplemented with 0.15% BSA fraction V and 1% antibiotic-antimycotic), which was collected from the nostrils. Lungs from 6 mice/group were homogenized using a 5 mm stainless steel BB in a Tissue Lyser II (Qiagen) in 1 ml of VCM for virus titration, and lungs from 3 mice/group were fixed in 10% buffered formalin for 24 hours, stored in 70% ethanol for 3-7 days, and embedded in paraffin for histopathological examination.
Histopathological evaluation and immunohistochemical (IHC) assays were done using routine hematoxylin-eosin (H+E) stains of the lung tissues for histopathological changes. IHC assays were performed on 3μm sections of tissue using a monoclonal antibody against the nucleoprotein (NP) of influenza A virus [30]. The antibody/polymer conjugate was visualized by applying UltraVision LP system with napthol phosphate substrate (Thermo Scientific/Lab Vision) to tissue sections. Negative controls consisted of sequential tissue sections incubated with an isotype control monoclonal antibody.
For vaccination, microneutralization assay, and virus challenge studies, groups of ABSL3 acclimatized 6-week-old female BALB/cJ mice (Jackson Laboratory) were anesthetized with isoflurane and intranasally inoculated with 105 TCID50 of one of the 5 viruses in 20 μl of PBS diluent, or else inoculated with PBS, to serve as a control (n=12/group). Serum was isolated from blood samples obtained from mouse tail veins at 21 dpi. The levels of neutralizing antibodies present in sera were assessed by microneutralization assay. Briefly, serum was 1:100 diluted prior to serial 1:2 dilutions in PBS, and mixed with 200 TCID50 of NY1682 virus, incubated at 33°C for 1 h and transferred to MDCK cells in 96-well plates. At 4 dpi, the plates were stained with crystal violet and neutralizing titers were determined.
At 30 dpi, 12 mice per group were challenged intranasally with 5 × 104 TCID50 (100 LD50 in 6-week-old mice) of a mouse-adapted variant of NY1682 (A/NY/1682/2009-MA7) created by serial lung passage in BALB/cJ mice. This mouse-adapted variant of NY1682 was created by intranasal inoculation of 6-to-8 week-old naïve BALB/cJ, and lungs were harvested 4 days post inoculation, homogenized, clarified, and used to inoculate naïve mice for a total of seven passages (Submitted, Journal of Virology). Disease symptoms and weights of the vaccinated mice were monitored for 10 days and four mice from each virus group were euthanized at 3 and 6 days post challenge. Lungs were homogenized in 1 ml of VCM and titers were determined by TCID50 assay. A/NY/1682/2009-MA7 causes dramatic morbidity in naïve mice and animals that became moribund or lost greater than 25% of their starting body weight were euthanized for humane reasons.
2.7 Ferret Experiments
Male Fitch ferrets (Triple F Farms, Sayre, PA), 7 to 10 months of age and serologically negative by hemagglutination inhibition (HI) assay for currently circulating influenza viruses, were used in this study. Ferrets were housed for the duration of each experiment in a Duo-Flow Bioclean mobile clean room (Lab Products, Inc., Seaford, DE). Groups of 3 or 4 ferrets were inoculated intranasally with 106.5 TCID50 of one of the viruses: NY1682 WT (n=4), NS1-73 (n=3), NS1-126 (n=4), or NSΔ5 (n=4). Ferrets were monitored for clinical signs through 14 dpi as previously described [31]. Nasal washes were collected on 1, 3, 5, and 7 dpi and were titrated in MDCK cells by TCID50 assay. Serum was isolated from blood collected 6.5 weeks after immunization/infection and used for neutralization assays. The ferrets were challenged with 106 PFU of A/Mexico/4482/2009 [32] 6.5 weeks post-immunization and monitored for clinical signs of disease through 14 dpi. Nasal washes were collected on 1, 3, 5, and 7 dpi, and were titrated in MDCK cells by plaque assay.
3. Results
3.1 Generation of experimental live attenuated influenza vaccines (LAIVs)
We created four recombinant H1N1pdm viruses (Fig. 1A) derived from A/New York/1682/2009 (NY1682) directly from an original clinical specimen using M-RTPCR genomic amplification and cloning techniques [9]. LAIV candidates NS1-73 and NS1-126 were designed to produce C-terminally truncated NS1 proteins that respectively retain the N-terminal 73 and 126 amino acids (Fig. 1A). These C-terminal truncations were selected based upon the success of prior studies using a laboratory-adapted virus and animal viruses [12;19]. The NSΔ5-LAIV candidate was engineered to have an in-frame deletion of 15 nucleotides that affects both the NS1 (residues 196-200) and NEP (residues 39-43) proteins (Fig. 1A); this mutation has never been used to create a LAIV. NSΔ5 was designed because an analogous deletion occurred naturally in an H5N1 virus (A/SW/FJ/03) isolated from a pig; that deletion attenuated a normally highly pathogenic H5N1 virus (SW/FJ/01) in chickens [33]. Thus, the panel of viruses created consists of WT NY1682, and three NS-LAIVs composed entirely of vRNAs from NY1682.
To confirm that the desired mutations were present in the panel of viruses rescued by reverse-genetics, we used M-RTPCR to amplify the genome of each virus and then analyzed the amplicons by agarose gel electrophoresis (Fig. 1B). M-RTPCR amplicons of NS-vRNA from the WT (lane 1) and NSΔ5-LAIV (lane 4) migrate at similar positions (∼890 bp), whereas the deletions present in NS-vRNA of NS-73 (lane 2), and NS1-126 (lane 3) lead to accelerated migration of the NS amplicons (Fig. 1B). The NS vRNAs of the recombinant viruses were subsequently confirmed by sequencing of the M-RTPCR amplicons (data not shown).
3.2 Attenuation of NS-LAIV candidates in vitro
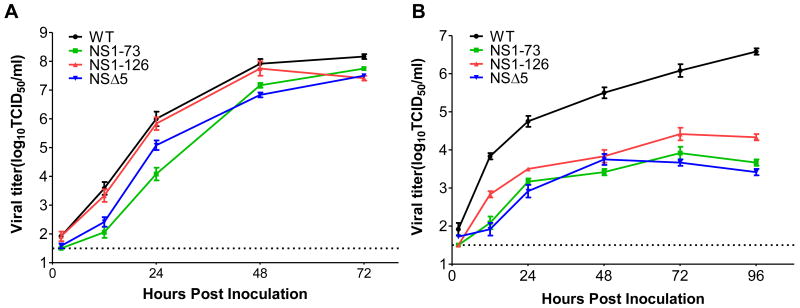
The replication kinetics of the recombinant NS-LAIV candidates were compared to the kinetics of recombinant WT virus in Madin Darby canine kidney (MDCK) cell cultures (Fig. 2A). The WT virus replicated rapidly and reached the highest titer (108.2 TCID50/ml, at 72 h). The NS1-126 replicated with kinetics very similar to that of the WT virus in MDCK cells, and also achieved very high titers (107.8 TCID50/ml at 48 h) (Fig. 2A). The NS1-73 and NSΔ5 viruses showed delayed replication rates compared to the WT rate (Fig. 2A, 12 & 24 h); however, both eventually reach peak titers similar to that of the WT virus (107.5 TCID50/ml, at 72h) (Fig. 2A). All of the NS-LAIV candidates showed more pronounced attenuation, 100-fold to 1000-fold reduction compared to WT, in the A549 human lung epithelial cell line, which was statistically significant (p < 0.05) at all of the time points examined (Fig. 2B). These results indicate that the NY1682 (H1N1pdm) NS-LAIVs are attenuated in human lung epithelial cells, but they can be propagated efficiently in MDCK cells.
Fig. 2. Replication of NS-LAIV candidates is inhibited under IFN competent culture conditions.
(A) MDCK cells were inoculated with an MOI of 0.002 TCID50/cell and the culture supernatants were collected at 2, 12, 24, 48 and 72 hpi. (B) A549 cells were inoculated with an MOI of 0.01 TCID50/cell, the culture supernatants were collected at 2, 12, 24, 48, 72 and 96 hpi. The viral titer in culture supernatants was determined by TCID50 assay using MDCK cells. The limit of detection (LOD) of these assays is indicated by the dotted line. The error bars were calculated using standard error of the mean (SEM) of triplicate assays.
3.3. H1N1pdm NS-LAIV candidates induce IFN and IFN-stimulated genes in human lung cells
A VSV-GFP virus [26] mediated IFN bioassay was used to determine whether the H1N1pdm NS-LAIV candidates induced elevated levels of type I IFN, relative to induction by the WT virus. Human A549 cells were inoculated with one of the recombinant influenza A viruses or were mock-inoculated. A multiplicity of infection (MOI) of 4 was used to ensure efficient infection of the A549 cells, regardless of the relative replication kinetics of the NS-LAIVs in this cell line. Supernatants from cells mock-inoculated with influenza A virus didn't inhibit the GFP expression from VSV-GFP virus, indicating that INF-α/β was not present at high levels in those supernatants (Fig. 3A). In contrast, supernatants from cells infected by NS1-126, or NSΔ5, inhibited GFP expression as early as 16 hpi (Fig. 3A). Supernatants from the NS1-73 infected cells contained lower levels of IFN, since GFP expression by VSV-GFP was only inhibited by the supernatant harvested at 24 hpi (Fig. 3A). Supernatants from the cells infected with the WT H1N1pdm virus didn't show any inhibition of GFP expression up to 24 hpi (Fig. 3A).
Fig. 3. NS-LAIVs Induce IFN and ISGs in Human Cells.
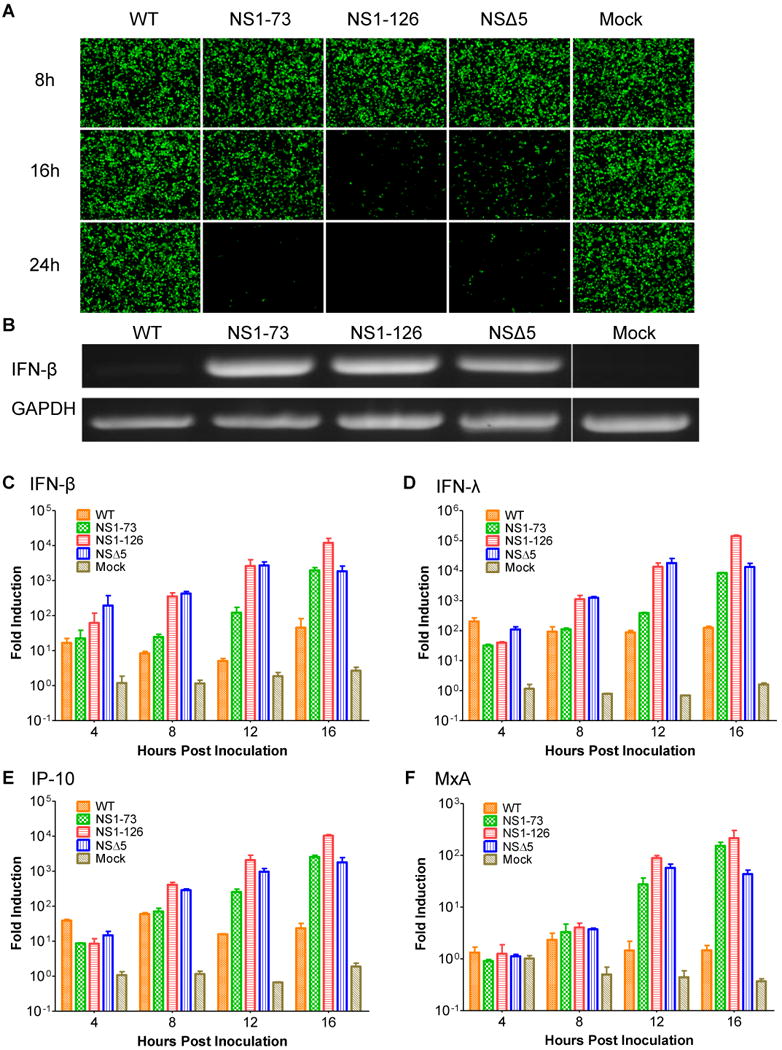
(A) Confluent A549 cells were inoculated with the recombinant viruses at an MOI of 4 TCID50/cell. Supernatants were collected at 8, 16 and 24 hpi, UV-inactivated, transferred to naive A549 cells, and incubated for 24h. The treated A549 cells were subsequently inoculated with VSV-GFP (MOI=2) and GFP expression in cells was visualized by fluorescence microscopy at 4 hpi. (B) RT-PCR analysis of IFN-β and GAPDH mRNAs in virus infected cells at 24hpi. (C-F) Confluent A549 cells were inoculated with the recombinant viruses at MOI of 4. Total cellular RNA was extracted from the inoculated cells at 4, 8, 12, 16 hpi and the levels of IFN-β (C), IL-29 (IFN-λ (D)), IP-10 (E) and MxA (F) mRNA were determined by quantitative RT-PCR. Error bars indicate the SEM of triplicate assays.
The VSV-GFP bioassay results were verified by RT-PCR amplification of the IFN-β mRNA from the cells inoculated with the WT virus or each one of the NS-LAIV candidates at 24 hpi. All of the NS-LAIV candidates induced high levels of INF-β mRNA production, whereas WT induced only low levels of mRNA; the mock-inoculated cells had no detectable mRNA (Fig. 3B). Quantitative RT-PCR (qRTPCR) was used to further investigate the production of mRNA for type I and III IFNs and IFN-stimulated genes (ISGs) in A549 cells. Compared to the mock-inoculated cells, the WT virus infection induced a 10-fold increase in IFN-β mRNA by 12 hpi, while the NS-LAIV candidates induced 100- (NS1-73) to 3,000-fold (NS1-126, and NSΔ5) increases (Fig 3C). qRTPCR analysis of the type III IFN, IFN-λ1 (IL-29) mRNA indicated that the NS-LAIV candidates induced 10,000-to 100,000-fold increases in mRNA by 16 hpi, whereas the WT virus showed only a 100-fold increase (Fig. 3D). Although WT virus induced a 60-fold increase in the chemokine IP10 (CXCL10), the vaccine candidates induced 1,800- to 10,000-fold increases in IP-10 mRNA (Fig. 3E). The ISG Mx is important in host resistance to influenza viruses and the production of human MxA was blocked in WT virus-infected cells. In contrast, ∼100-fold induction of MxA mRNA was observed in cells infected with anyone of the NS-LAIV candidates by 12 hpi (Fig. 3F). The qRTPCR data (Fig. 3C-F) correlate with the results of the IFN bioassay (Fig. 3A) and with the attenuation of the NS-LAIV candidates seen in a human lung cell line (Fig. 2B). Nevertheless, the qRTPCR results help to delineate differences in the host response to the various NS-LAIVs. NS1-126 and NSΔ5 consistently induced the greatest host antiviral response. While the induction of IFN and ISG mRNAs by NS1-73 lagged behind the induction by the other NS-LAIVs (Fig. 3C-F, 12 hpi), it was considerably greater than that of the WT virus.
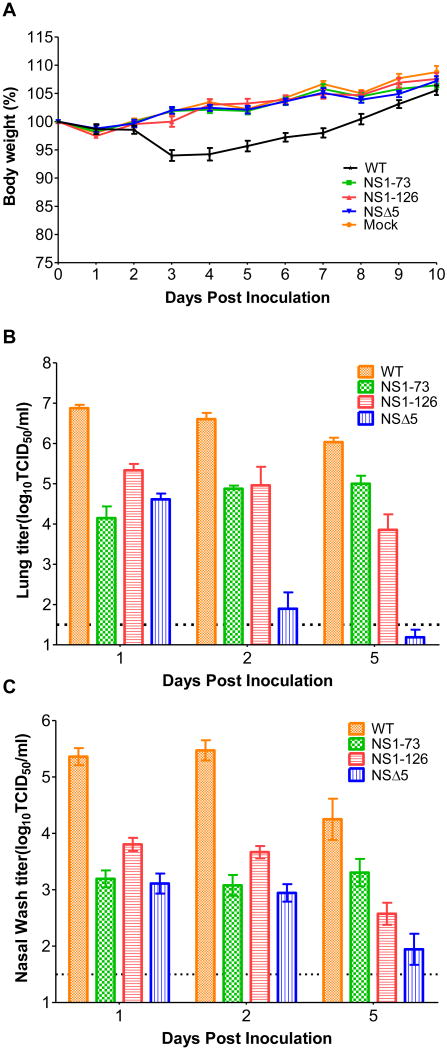
3.4 H1N1pdm NS-LAIV candidates are attenuated in mice
Mice were also used to examine the level of attenuation of the NS-LAIV candidates in vivo. Mice were inoculated intranasally with 105 TCID50 of the WT, NS1-73, NS1-126, or NSΔ5 viruses, or were mock-inoculated. Clinical signs of disease such as ruffled fur were observed in mice inoculated with WT virus as early as 2 days post inoculation (dpi) (data not shown). Weight loss became evident at 3 dpi and the mice did not recover until 9 dpi (Fig. 4A). In contrast, mice inoculated with any one of the vaccine candidates showed no clinical signs of disease and continued to gain weight at the same rate as did the mock-inoculated mice (Fig. 4A). Students t-test showed that the weight loss caused by WT virus was statistically different from NSΔ5 and the other NS-LAIVs from days 3-to-8 (p < 0.05). Viral titers in the lungs of NS1-73, and NS1-126 infected mice were approximately 100-fold lower than titers from WT virus-infected mice, at all the time points analyzed (1, 2, and 5 dpi) (Fig. 4B). The titer of the WT virus was significantly higher than any of the NS-LAIVs at 1, 2, and 5 dpi (p < 0.05, students t-test). Notably, the NSΔ5 LAIV was cleared from the mouse lungs very rapidly and the average titers were approximately 100-fold and 50,000-fold lower than the titers of the WT virus at 1 and 2 dpi, respectively (Fig. 4B). Although there was an average of 106 TCID50/lung in mice infected by WT virus on day 5 pi, the average NSΔ5-LAIV titer was below the limit of detection. The NS-LAIV candidates also showed 10- to 100-fold lower titers in the upper respiratory tract (Fig. 4C). The differences observed between the titer of WT virus and the NS-LAIVs in the upper respiratory tract were also statistically significant. For example, comparison of the titers of WT with NS1-126 by students t-test showed that they were significantly different (p ≤ 0.001) at all of the time points examined (Fig. 4C). Nevertheless, all of the vaccine candidates were detectable through 5 dpi (Fig. 4C), and this could promote a strong adaptive immune response.
Fig. 4. NS-LAIV candidates have different levels of attenuation in mice.
6 week-old female BALB/cJ mice were inoculated intranasally with 105 TCID50 of WT, the NS-LAIVs, or were mock inoculated. (A) Body weight of inoculated mice (n=12/group) was recorded daily and is represented as the percent of the animals weight on the day of inoculation (day 0). (B) Viral titers in the lung homogenates of inoculated mice (n=6/group) were determined for each mouse by TCID50 assay at 1, 2, and 5 dpi. (C) Viral titers from nasal airway of inoculated mice (n=9/group). The average of each group is shown with error bars determined by SEM, and the limit of detection for virus titration is indicated by the dotted line (B, C).
Histopathological analysis of lungs from mice euthanized on 1, 2, and 5 dpi showed lesions typical of influenza A virus infection; the severity of histopathology observed in mice inoculated with recombinant WT or any of the NS-LAIVs directly correlated with the amount of virus present in the animals' lungs. Mice inoculated with WT virus had the most severe pathological changes, while mice inoculated with the NSΔ5-LAIV showed the least severe pathology. Beginning at 1 dpi, epithelial necrosis and sloughing into the bronchioles was evident in WT infected mice (data not shown). Peribronchiolar and interstitial inflammation were also evident at 2 and 5 dpi in WT infected mice (data not shown). Immunohistochemistry of the lung tissues collected 2 dpi from mice inoculated with the WT virus or any of the NS-LAIVs indicated that viral NP was present in the nuclei and cytoplasm of infected cells (red staining), including epithelial cells in the bronchioles (arrows) and in pneumocytes, either detached or lining the alveoli (Fig. 5). The number of antigen positive cells varied depending on the virus strain, and corresponded to the extent of histopathology observed and the amount of virus present in the lungs (compare Figs. 4B and 5). Intriguingly, virus antigen was detected in all lobes of the lungs of mice inoculated with all of the recombinant viruses except in mice inoculated with NSΔ5. At 2 and 5 dpi NP antigen positive cells that are depicted in Fig. 5D were infrequently detected in mice infected with NSΔ5.
Fig 5. NS-LAIV candidates show similar cell tropism but reduced pathogenesis in mouse lungs.
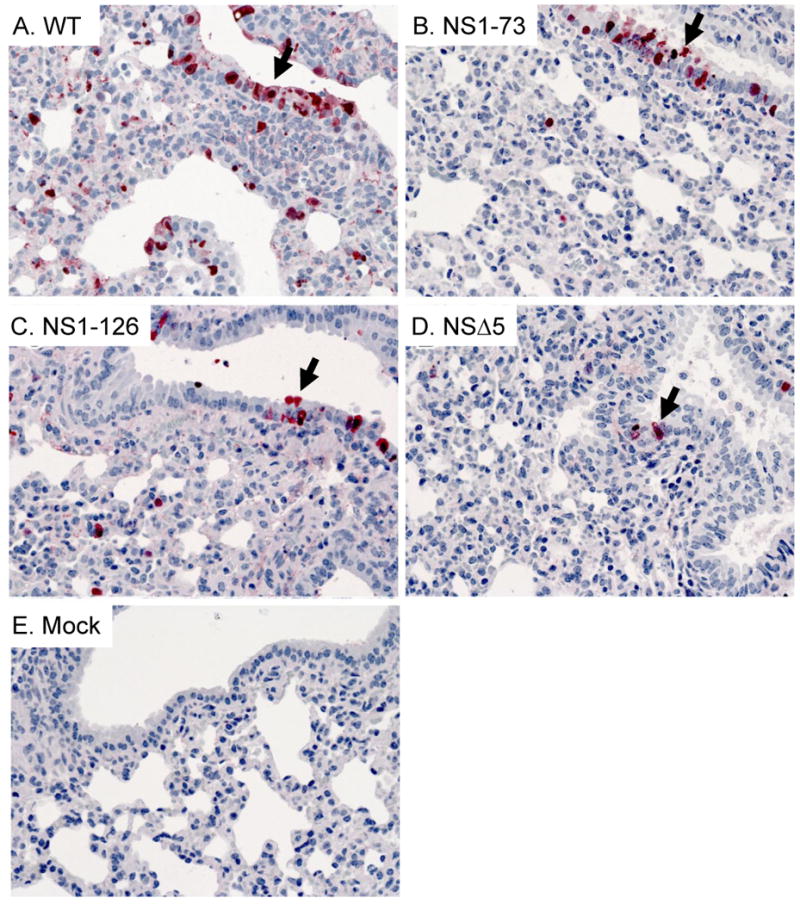
Viral NP antigens are detected in infected bronchiolar epithelial cells (upper right in each panel) and alveolar lining cells in mice inoculated with A) WT, B) NS1-73, C) NS1-126, D) NSΔ5, or E) mock (arrows indicate infected epithelial cells in the bronchioles) at 2 dpi. All images, except D, are representative of observations from sections obtained from multiple animals (n=3/group). NP antigen was less abundant in mice inoculated with NSΔ5, so an image (D) illustrating some antigen positive cells was selected.
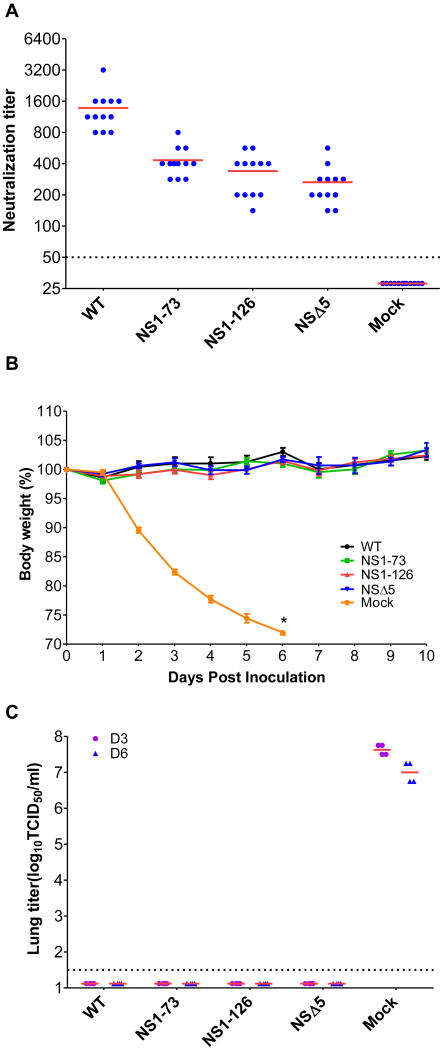
3.5 The H1N1pdm NS-LAIV candidates protect mice from lethal challenge
Groups of mice were inoculated intranasally with 105 TCID50 of the H1N1pdm NS-LAIV candidates or either of the controls (WT or mock). Microneutralization assays demonstrated that the vaccine candidates elicited neutralizing antibodies in all of the NS-LAIV immunized mice, with the average antibody titer of each group ranging from 300 to 500 at 21 dpi (Fig. 6A). When the mice were challenged with a lethal mouse-adapted variant of NY1682 (NY1682-MA7) at 30 dpi, each of the NS-LAIV candidates or prior infection by the WT virus protected the mice from the challenge. No disease symptoms were observed in the mice immunized by any of the NS-LAIV candidates or the WT control. In contrast, disease symptoms including ruffled fur, hunched posture, and weight loss were observed in the mock-immunized mice as early as 2 days post challenge (dpc); the symptoms progressed to severe disease, and the animals showed statistically significant (p<0.001, students t-test) weight loss compared to the WT or NS-LAIV immunized mice (Fig. 6B). The mice became moribund, and succumbed to infection by 5-6 dpc. High titers of virus were also present in the mock-immunized mice at 3 dpc (4×107 TCID50/ml) and at 6 dpc (1×107 TCID50/ml) (Fig. 6C). In contrast, virus was not detected in the lungs of mice immunized with NS1-73, NS1-126, NSΔ5, or the WT control, at 3 and 6 dpc (Fig. 6C). This mouse challenge data demonstrates that all of the NS-LAIV candidates, including the highly attenuated NSΔ5, induced sterilizing immunity to challenge with a lethal variant of NY1682 H1N1pdm.
Fig 6. NS-LAIV candidates protect mice from lethal infection.
Groups of mice (n=12/group) were immunized by intranasal inoculation with the wild-type (WT), the NS-LAIVs (NS1-73, NS1-126, or NSΔ5) or inoculation media alone (Mock). (A) Neutralizing antibody levels in serum collected at 21 days post-immunization were determined by microneutralization assay (each dot represents an individual mouse). (B) Mice were challenged intranasally, 30 days post-immunization, with 5×104 TCID50 (∼100 LD50) of a lethal mouse adapted variant of NY1682, and their weight was monitored for 10 days post challenge, error bars represent ± SEM (days 1-3, n=12; days 4-6, n=8; days 7-10 n=4). * Only 4/8 mice remained in the mock immunized group on day 6 post challenge because 4 mice were euthanized for humane reasons on day 5, and the remaining animals were euthanized on day 6. (C) Viral titers in the lungs were determined at 3 and 6 days post challenge. Each dot represents the virus titer of an individual mouse (n=4/group). Mock indicates animals that were mock-immunized and subsequently challenged. The LOD of the assays is indicated by the dotted line (A, & C). The graphs are representative of two independent experiments.
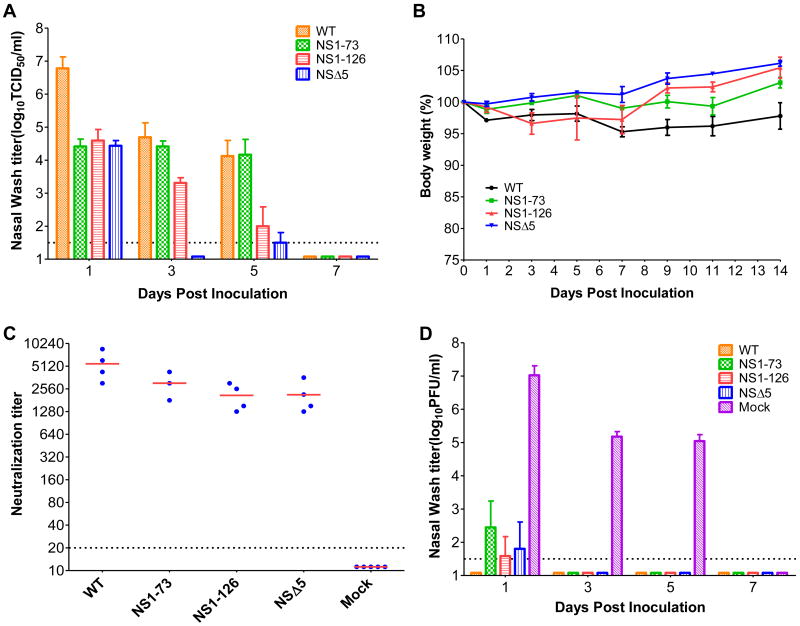
3.6 H1N1pdm NS-LAIV candidates were attenuated in ferrets and protective against homosubtypic challenge
The ferret is a well established animal model which generally recapitulates the severity and outcome of disease observed in humans infected with influenza A virus. To assess attenuation of the NS-LAIV candidates, we inoculated groups of ferrets intranasally with 106.5 TCID50 of each vaccine candidate or the WT virus. The titers of viruses recovered from nasal washes ranged from 106.8 to 104.5 TCID50/ml through day 5 in the WT virus-infected group, while the NS-LAIVs were attenuated to various degrees (Fig. 7A). Relative to WT, all of the NS-LAIVs showed at least 100-fold reduction in titer at 1 dpi (Fig. 7A). The NS1-73 LAIV was the least attenuated in ferrets (Fig. 7A), which was similar to that observed in mice. Relative to the WT virus, the NS1-126 LAIV showed 100-fold reduction in titer and the NSΔ5 LAIV was below the limit of detection (at least 1000-fold reduction) at 3 dpi (Fig. 7A).
Fig 7. NS-LAIV candidates are attenuated in ferrets and protect from challenge.
Ferrets were inoculated intranasally with 106.5 TCID50 of the various recombinant viruses. (A) Virus shedding from the nasal airway of the infected ferrets was determined by TCID50 assay of nasal washes collected at 1, 3, 5 and 7 dpi. (B) Body weight of the inoculated ferrets (n=3-4/group) was recorded on alternate days and is represented as the mean percent of initial body weight (day 0). (C) Neutralizing antibody levels in sera isolated 6.5 weeks post immunization was determined by micro-neutralization assay. (D) 6.5 weeks post immunization, ferrets were challenged with 106 PFU of A/Mexico/4482/2009 (H1N1pdm). Virus shedding from the nasal airway was determined by plaque assay of nasal washes collected at 1, 3, 5 and 7 dpc. The average of each group is shown and the error bars represent SEM. If virus titers were below the LOD (1.5 log10) they are shown as 1 log10, however they lack error bars (A, & D).
Disease symptoms and weights were also monitored through 14 dpi. Ferrets in all groups, including animals inoculated with the WT virus, remained alert and playful for the duration of the 14-day observation period. Clinical symptoms such as sustained fever, sneezing, nasal discharge, and diarrhea or other gastrointestinal symptoms were not consistently observed in infected animals. Infection with the WT virus caused modest weight loss in the ferrets (Fig. 7B). Student's t-test showed that WT infection caused weight loss that was significantly different at every time point post infection compared to infection by the NSΔ5 LAIV (p < 0.05); the WT weight loss was also significantly different at 1 dpi, and at 7 dpi compared to weight loss caused by NS1-73, and significantly different at 9, 11, 14 dpi compared to weight change of NS1-126 infected animals (p < 0.05) (Fig. 7B).
Sera from blood collected 6.5 weeks after immunization/infection were analyzed for the presence of neutralizing antibody (Fig. 7C). The NS-LAIV candidates all induced very strong neutralizing antibody responses (1280-5120) that were similar to the titer elicited by WT virus infection (Fig. 7C). The virus neutralization data illustrate that although the NS1-126 and NSΔ5 H1N1pdm LAIVs are highly attenuated and readily cleared by the host, they nevertheless induce a potentially protective antibody response.
To determine whether the NS-LAIV candidates protect ferrets from infection by a homosubtypic virus, we challenged ferrets 6.5 weeks post immunization with 106 PFU of the H1N1pdm virus A/Mexico/4482/2009, which was isolated from a 29-year-old female patient with severe respiratory disease [32]. Little disease or weight loss were observed in the naïve ferrets, and the ferrets immunized by infection with WT virus or the NS-LAIV candidates didn't show any disease symptoms or weight loss (data not shown). In contrast to the high titer of virus detected in the naïve ferrets through 5 dpc, the NS-LAIV immunized ferrets had very low levels of A/Mexico/4482/2009 in their nasal washes at 1 dpc (Fig. 7D). The ferrets immunized with the NY1682 NS-LAIVs had ∼10,000- to 100,000-fold lower viral titers than did the naïve animals (Fig. 7D). In summary, the NS-LAIV candidates dramatically inhibited initial replication of the H1N1pdm virus under stringent challenge conditions (106 PFU), and the vaccinated animals rapidly cleared the infection (to below the limit of detection, at 3 dpc).
4. Discussion
This study demonstrates that recombinant NS-LAIV(s) created directly from human swab material are effective experimental vaccines against H1N1pdm viruses. In vitro, the NS-LAIV candidates replicated efficiently in canine MDCK cells, which produce type I IFN but lack the ISG Mx [34]. Efficient replication in MDCK cells has important practical implications because this is an approved cell line for production of influenza A virus vaccines. Importantly, pronounced attenuation was observed in the human lung epithelial cell line A549, correlating with the induction of type I IFN and ISGs by the NS-LAIVs, and this is consistent with previous studies showing that influenza A viruses with deleted or truncated NS1 proteins are attenuated in IFN-competent cells [35;36]. The results from the IFN bioassays and RT-PCR analysis show the host innate immune response was induced at much higher levels in the human lung epithelial cells infected with NS1-126 and NSΔ5 than in those infected with the WT H1N1pdm virus. This data also indicates that NS1-126 and NSΔ5 are likely to be strong inducers of IFNs and ISGs in humans and other primates. Stimulation of the innate immune system is a major advantage to the NS-LAIV strategy because this acts as a natural adjuvant and enhances the adaptive immune response of the host [15-18;37].
Mice immunized with the NS-LAIVs were asymptomatic, and the tissue titers of NS1-126 and NSΔ5 viruses were dramatically lower than the titers of WT virus, indicating that they were significantly attenuated in vivo. Histopathological and immunohistochemical analysis also showed that the NS-LAIVs were severely attenuated and rapidly cleared in mice; lesions in the lungs were the smallest and most sporadic in mice inoculated with the NSΔ5, and this correlated with the level of virus replication observed for this NS-LAIV candidate. Although both NS1-126 and NSΔ5 were highly attenuated, they generated complete immune protection from lethal challenge with a mouse-adapted variant of NY1682.
Examination of the NS-LAIVs in ferrets substantiated the pronounced attenuation phenotype of the NSΔ5 candidate that was observed in mice. For example, the NSΔ5 LAIV was severely attenuated and rapidly cleared by the two hosts (Fig. 4B and Fig. 7A). Although NS1-126 and NSΔ5 LAIV candidates were markedly attenuated in ferrets, both elicited strong neutralizing antibody responses that dramatically inhibited replication in the face of a high-titer challenge, and results in rapid clearance of the challenge virus (by 3 dpc), A/Mexico/4482/2009 (H1N1pdm).
Collectively, the data from the in vitro and in vivo (mice, and ferrets) studies show that NS1-73 was the least attenuated LAIV candidate; and NSΔ5 was the most attenuated LAIV. NSΔ5 is a new type of NS-LAIV that has a subtle in-frame deletion (15 nt), which affects both the NS1 (residues 196-200) and NEP (residues 39-43). The NSΔ5 H1N1pdm LAIV was designed to be analogous to a naturally attenuated variant (A/SW/FJ/03) of a normally highly pathogenic H5N1 virus [33]. The NS1 deletion in A/SW/FJ/03 (NS1 residues 191-195) was shown to reduce binding of NS1 to host cleavage and polyadenylation specificity factor (CPSF), reduce NS1 protein stability, and enhance the type I IFN response of an H5N1 virus [33]. Our data prove that deletion of these 15nt in the NS vRNA of the quadruple reassortant H1N1pdm virus also stimulates the host innate immune response (specifically, IFN-ß, IFN-λ1, IP10, and MxA), and attenuates this virus. The fact that NSΔ5 attenuates two distantly related influenza A viruses suggests that this region of the NS gene/protein(s) is a good target for NS-LAIVs against many diverse influenza A viruses and potentially for the development of anti-viral compounds. The role of the deletion of residues 39-43 from NEP has not been elucidated, but the induction of IFN and ISGs by NSΔ5 was similar to, or slightly lower than their induction by NS-126, suggesting that the NEP mutation may also have an attenuating effect, which warrants future investigation.
LAIV safety and the potential problems associated with reassortment of LAIVs with other circulating influenza A viruses are also of paramount importance, and are challenges for the experimental approach described in this study. The currently licensed LAIVs have six internal-protein encoding vRNAs derived from the cold-adapted temperature sensitive A/Ann Arbor/6/1960 master donor strain (ca A/AA/6/60), which is an H2N2 virus that was originally isolated in 1960 and then subjected to many serial passages in vitro [38;39]. This licensed vaccine has many point mutations in multiple vRNAs (e.g., PB1, PB2, NP) [40-42] that both attenuate the virus and enhance its safety by inhibiting the rapid generation of revertants and/or single-gene reassortants that have lost the attenuating temperature sensitive phenotype, but contain wild-type HA and NA vRNAs. Although the NS-deletions used in this study are large enough so that rapid reversion to a wild-type phenotype via point mutation is highly unlikely, substitution of the NS vRNA segment via reassortment with either wild-type H1N1pdm viruses or other seasonal viruses would remove the single attenuating vRNA. This is a very serious concern, particularly in situations where the emerging strains have pandemic potential but have not yet become widespread. Therefore, we envision swapping the cis-acting segment-specific packaging signals in the vRNA segments such as the HA and NS, which was recently effective with A/PR/8/1934 (H1N1) [44], in order to prevent reassortment and enhance safety of future NS-based LAIVs. Additional animal studies and human trials with specific NS-LAIVs such as the recent study by Wacheck et. al. [43] are needed to help to define safety parameters for NS-LAIVs in humans.
A drawback of using the 6 internal-protein encoding vRNAs of ca A/AA/6/60 is that the cytotoxic T lymphocyte epitopes present in influenza A virus have mutated because of host immune pressure, which reduces immune recognition of the internal proteins expressed by currently circulating strains [45-48]. Additionally, many immune evading amino acid substitutions are present when novel reassortants like the H1N1pdm virus emerge from animal reservoirs. Our strategy can be accomplished with equal, or greater, speed than typical reverse-genetics based vaccine approaches, which often require virus isolation prior to RT-PCR amplification with HA and NA specific primers. Most importantly, the LAIV approach outlined in this study has the advantage of stimulating the host's innate and adaptive immune system with the entire repertoire of proteins expressed by circulating or new emerging strains.
In summary, we rapidly generated a panel of recombinant LAIVs, directly from a patient specimen, by introducing attenuating mutations into the NS gene of an emerging pandemic influenza A virus. Our results demonstrate that two deletion mutations (NS1-126 and NSΔ5) in the NS vRNA in the unique gene constellation of the H1N1pdm virus attenuate this virus in a human lung epithelial cell line, in mice and in ferrets. A new type of NS-LAIV (NSΔ5) was designed and shown to be highly attenuated, and to elicit strong innate and adaptive immune responses, resulting in protection of mice from subsequent challenge with a lethal mouse-adapted variant of NY1682, and ferrets from challenge with A/Mexico/4482/2009. The creation of LAIVs by the rational introduction of attenuating mutations to the genome of emerging or currently circulating strains of influenza A virus could be integrated with current and future vaccine production scheme(s) and it has important potential advantages over the reassortant-based vaccine seed stock production strategies that are currently used.
Acknowledgments
We thank Chrystal Chadwick, Scott Speer, and Amanda Mercer for their expert assistance with the mouse studies, Matthew Shudt in the Wadsworth Center Applied Genomic Technologies Core for his assistance in the sequencing of plasmids and RT-PCR amplicons, Noel Espina, Jianzhong Tang and Richard Cadagan for tissue culture support, Elizabeth White for histological support, and Dr. Susan Wong for Luminex analysis of antibody titers. We are grateful to Dr. Peter Palese for providing the pDZ reverse-genetics plasmid and the NDV-GFP used in preliminary studies, and to Dr Sean P. Whelan for providing the VSV-GFP reporter virus. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention, the Wadsworth Center, NYSDOH, or the Mount Sinai School of Medicine.
These studies were supported in part by Health Research Inc., the Wadsworth Center, NYSDOH Directors office, and NIH/NIAID Northeast Biodefense Center's animal core award 2 U54 AI057178-06. D.E.W. was also supported NIH/NIAID P01AI059576-05. Work in the A.G.-S. laboratory was partly supported by NIAID grant U01AI070469. A.G.-S. owns equity and receives financial compensation for providing consulting services and for serving on the advisory board of Vivaldi BioScience, a biotechnology company that develops influenza vaccines based on NS-1-modification technology. Mount Sinai School of Medicine has received compensation from Vivaldi in return for a license to certain technology, the value of which may be affected by the outcome of this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.World Health Organization. Influenza (Seasonal) Fact sheet 211. 2009 April 1; Available from: URL: http://www.who.int/mediacentre/factsheets/fs211/en/
- 2.Palese P, Shaw ML. Orthomyxoviridae: The Viruses and Their Replication. In: Knipe DM, Howley PM, Griffin DE, Lamb RA, Straus SE, Martin MA, et al., editors. Fields Virology. 5. Philadelpha, PA: Lippincott Williams and Wilkins; 2007. pp. 1647–90. [Google Scholar]
- 3.Wright PF, Neumann G, Kawaoka Y. Orthomyxoviruses. In: Knipe DM, Howley PM, Griffin DE, Lamb RA, Straus SE, Martin MA, et al., editors. Fields Virology. 5. Philadelpha, PA: Lippincott Williams and Wilkins; 2007. pp. 1691–740. [Google Scholar]
- 4.Neumann G, Noda T, Kawaoka Y. Emergence and pandemic potential of swine-origin H1N1 influenza virus. Nature. 2009 Jun 18;459(7249):931–9. doi: 10.1038/nature08157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hancock K, Veguilla V, Lu X, et al. Cross-reactive antibody responses to the 2009 pandemic H1N1 influenza virus. N Engl J Med. 2009 Nov 12;361(20):1945–52. doi: 10.1056/NEJMoa0906453. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. Pandemic (H1N1) 2009 - update 97. 2010 April 18; Available from: URL: http://www.who.int/csr/don/2010_04_23a/en/index.html.
- 7.Salomon R, Webster RG. The influenza virus enigma. Cell. 2009 Feb 6;136(3):402–10. doi: 10.1016/j.cell.2009.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Collin N, de Radiguès X. Vaccine production capacity for seasonal and pandemic (H1N1) 2009 influenza. Vaccine. 2009 Aug 20;27(38):5184–6. doi: 10.1016/j.vaccine.2009.06.034. [DOI] [PubMed] [Google Scholar]
- 9.Zhou B, Donnelly ME, Scholes DT, et al. Single-Reaction Genomic Amplification Accelerates Sequencing and Vaccine Production for Classical and Swine Origin Human Influenza A Viruses. J Virol. 2009 Oct 1;83(19):10309–13. doi: 10.1128/JVI.01109-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hale BG, Randall RE, Ortin J, Jackson D. The multifunctional NS1 protein of influenza A viruses. J Gen Virol. 2008 Oct;89(Pt 10):2359–76. doi: 10.1099/vir.0.2008/004606-0. [DOI] [PubMed] [Google Scholar]
- 11.Hsiang TY, Zhao C, Krug RM. Interferon-induced ISG15 conjugation inhibits influenza A virus gene expression and replication in human cells. J Virol. 2009 Jun;83(12):5971–7. doi: 10.1128/JVI.01667-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Talon J, Salvatore M, O'Neill RE, et al. Influenza A and B viruses expressing altered NS1 proteins: A vaccine approach. Proc Natl Acad Sci U S A. 2000 Apr 11;97(8):4309–14. doi: 10.1073/pnas.070525997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kochs G, Garcia-Sastre A, Martinez-Sobrido L. Multiple anti-interferon actions of the influenza A virus NS1 protein. J Virol. 2007 Jul;81(13):7011–21. doi: 10.1128/JVI.02581-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haye K, Burmakina S, Moran T, Garcia-Sastre A, Fernandez-Sesma A. The NS1 protein of a human influenza virus inhibits type I interferon production and the induction of antiviral responses in primary human dendritic and respiratory epithelial cells. J Virol. 2009 Jul;83(13):6849–62. doi: 10.1128/JVI.02323-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fernandez-Sesma A. The influenza virus NS1 protein: inhibitor of innate and adaptive immunity. Infect Disord Drug Targets. 2007 Dec;7(4):336–43. doi: 10.2174/187152607783018754. [DOI] [PubMed] [Google Scholar]
- 16.Iwasaki A, Medzhitov R. Regulation of Adaptive Immunity by the Innate Immune System. Science. 2010 Jan 15;327(5963):291–5. doi: 10.1126/science.1183021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koyama S, Aoshi T, Tanimoto T, et al. Plasmacytoid Dendritic Cells Delineate Immunogenicity of Influenza Vaccine Subtypes. Science Translational Medicine. 2010 Mar 31;2(25):25ra24. doi: 10.1126/scitranslmed.3000759. [DOI] [PubMed] [Google Scholar]
- 18.Mueller SN, Langley WA, Carnero E, Garcia-Sastre A, Ahmed R. Immunization with live attenuated influenza viruses that express altered NS1 proteins results in potent and protective memory CD8+ T-cell responses. J Virol. 2010 Feb;84(4):1847–55. doi: 10.1128/JVI.01317-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Quinlivan M, Zamarin D, Garcia-Sastre A, Cullinane A, Chambers T, Palese P. Attenuation of equine influenza viruses through truncations of the NS1 protein. J Virol. 2005 Jul;79(13):8431–9. doi: 10.1128/JVI.79.13.8431-8439.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Solorzano A, Webby RJ, Lager KM, Janke BH, Garcia-Sastre A, Richt JA. Mutations in the NS1 protein of swine influenza virus impair anti-interferon activity and confer attenuation in pigs. J Virol. 2005 Jun;79(12):7535–43. doi: 10.1128/JVI.79.12.7535-7543.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Richt JA, Lekcharoensuk P, Lager KM, et al. Vaccination of pigs against swine influenza viruses by using an NS1-truncated modified live-virus vaccine. J Virol. 2006 Nov;80(22):11009–18. doi: 10.1128/JVI.00787-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vincent AL, Ma W, Lager KM, et al. Efficacy of intranasal administration of a truncated NS1 modified live influenza virus vaccine in swine. Vaccine. 2007 Nov 19;25(47):7999–8009. doi: 10.1016/j.vaccine.2007.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chambers TM, Quinlivan M, Sturgill T, et al. Influenza A viruses with truncated NS1 as modified live virus vaccines: pilot studies of safety and efficacy in horses. Equine Vet J. 2009 Jan;41(1):87–92. doi: 10.2746/042516408x371937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Steel J, Lowen AC, Pena L, et al. Live attenuated influenza viruses containing NS1 truncations as vaccine candidates against H5N1 highly pathogenic avian influenza. J Virol. 2009 Feb;83(4):1742–53. doi: 10.1128/JVI.01920-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hoffmann E, Webster RG. Unidirectional RNA polymerase I-polymerase II transcription system for the generation of influenza A virus from eight plasmids. J Gen Virol. 2000 Dec;81(Pt 12):2843–7. doi: 10.1099/0022-1317-81-12-2843. [DOI] [PubMed] [Google Scholar]
- 26.Chandran K, Sullivan NJ, Felbor U, Whelan SP, Cunningham JM. Endosomal proteolysis of the Ebola virus glycoprotein is necessary for infection. Science. 2005 Jun 10;308(5728):1643–5. doi: 10.1126/science.1110656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang X, Li M, Zheng H, et al. Influenza A virus NS1 protein prevents activation of NF-kappaB and induction of alpha/beta interferon. J Virol. 2000 Dec;74(24):11566–73. doi: 10.1128/jvi.74.24.11566-11573.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gillim-Ross L, Taylor J, Scholl DR, Ridenour J, Masters PS, Wentworth DE. Discovery of novel human and animal cells infected by the severe acute respiratory syndrome coronavirus by replication-specific multiplex reverse transcription-PCR. J Clin Microbiol. 2004 Jul;42(7):3196–206. doi: 10.1128/JCM.42.7.3196-3206.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001 Dec;25(4):402–8. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 30.Guarner J, Shieh WJ, Dawson J, et al. Immunohistochemical and in situ hybridization studies of influenza A virus infection in human lungs. Am J Clin Pathol. 2000 Aug;114(2):227–33. doi: 10.1309/HV74-N24T-2K2C-3E8Q. [DOI] [PubMed] [Google Scholar]
- 31.Maines TR, Lu XH, Erb SM, et al. Avian influenza (H5N1) viruses isolated from humans in Asia in 2004 exhibit increased virulence in mammals. J Virol. 2005 Sep;79(18):11788–800. doi: 10.1128/JVI.79.18.11788-11800.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maines TR, Jayaraman A, Belser JA, et al. Transmission and Pathogenesis of Swine-Origin 2009 A(H1N1) Influenza Viruses in Ferrets and Mice. Science. 2009 Jul 2; doi: 10.1126/science.1177238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhu Q, Yang H, Chen W, et al. A naturally occurring deletion in its NS gene contributes to the attenuation of an H5N1 swine influenza virus in chickens. J Virol. 2008 Jan;82(1):220–8. doi: 10.1128/JVI.00978-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Seitz C, Frensing T, Hoper D, Kochs G, Reichl U. High yields of Influenza A virus in MDCK cells are promoted by an insufficient IFN-induced antiviral state. J Gen Virol. 2010 Mar 31; doi: 10.1099/vir.0.020370-0. [DOI] [PubMed] [Google Scholar]
- 35.Egorov A, Brandt S, Sereinig S, et al. Transfectant influenza A viruses with long deletions in the NS1 protein grow efficiently in Vero cells. J Virol. 1998 Aug;72(8):6437–41. doi: 10.1128/jvi.72.8.6437-6441.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Garcia-Sastre A, Egorov A, Matassov D, et al. Influenza A virus lacking the NS1 gene replicates in interferon-deficient systems. Virology. 1998 Dec 20;252(2):324–30. doi: 10.1006/viro.1998.9508. [DOI] [PubMed] [Google Scholar]
- 37.Fernandez-Sesma A, Marukian S, Ebersole BJ, et al. Influenza virus evades innate and adaptive immunity via the NS1 protein. J Virol. 2006 Jul;80(13):6295–304. doi: 10.1128/JVI.02381-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maassab HF. Adaptation and growth characteristics of influenza virus at 25 degrees c. Nature. 1967 Feb 11;213(5076):612–4. doi: 10.1038/213612a0. [DOI] [PubMed] [Google Scholar]
- 39.Maassab HF, Bryant ML. The development of live attenuated cold-adapted influenza virus vaccine for humans. Rev Med Virol. 1999 Oct;9(4):237–44. doi: 10.1002/(sici)1099-1654(199910/12)9:4<237::aid-rmv252>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 40.Chan W, Zhou H, Kemble G, Jin H. The cold adapted and temperature sensitive influenza A/Ann Arbor/6/60 virus, the master donor virus for live attenuated influenza vaccines, has multiple defects in replication at the restrictive temperature. Virology. 2008 Oct 25;380(2):304–11. doi: 10.1016/j.virol.2008.07.027. [DOI] [PubMed] [Google Scholar]
- 41.Jin H, Zhou H, Lu B, Kemble G. Imparting temperature sensitivity and attenuation in ferrets to A/Puerto Rico/8/34 influenza virus by transferring the genetic signature for temperature sensitivity from cold-adapted A/Ann Arbor/6/60. J Virol. 2004 Jan;78(2):995–8. doi: 10.1128/JVI.78.2.995-998.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jin H, Lu B, Zhou H, et al. Multiple amino acid residues confer temperature sensitivity to human influenza virus vaccine strains (FluMist) derived from cold-adapted A/Ann Arbor/6/60. Virology. 2003 Feb 1;306(1):18–24. doi: 10.1016/s0042-6822(02)00035-1. [DOI] [PubMed] [Google Scholar]
- 43.Wacheck V, Egorov A, Groiss F, et al. A novel type of influenza vaccine: safety and immunogenicity of replication-deficient influenza virus created by deletion of the interferon antagonist NS1. J Infect Dis. 2010 Feb 1;201(3):354–62. doi: 10.1086/649428. [DOI] [PubMed] [Google Scholar]
- 44.Gao Q, Palese P. Rewiring the RNAs of influenza virus to prevent reassortment. Proc Natl Acad Sci U S A. 2009 Sep 15;106(37):15891–6. doi: 10.1073/pnas.0908897106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rimmelzwaan GF, Kreijtz JH, Bodewes R, Fouchier RA, Osterhaus AD. Influenza virus CTL epitopes, remarkably conserved and remarkably variable. Vaccine. 2009 Oct 23;27(45):6363–5. doi: 10.1016/j.vaccine.2009.01.016. [DOI] [PubMed] [Google Scholar]
- 46.Boon AC, de MG, Graus YM, et al. Sequence variation in a newly identified HLA-B35-restricted epitope in the influenza A virus nucleoprotein associated with escape from cytotoxic T lymphocytes. J Virol. 2002 Mar;76(5):2567–72. doi: 10.1128/jvi.76.5.2567-2572.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rimmelzwaan GF, Boon AC, Voeten JT, Berkhoff EG, Fouchier RA, Osterhaus AD. Sequence variation in the influenza A virus nucleoprotein associated with escape from cytotoxic T lymphocytes. Virus Res. 2004 Jul;103(1-2):97–100. doi: 10.1016/j.virusres.2004.02.020. [DOI] [PubMed] [Google Scholar]
- 48.Berkhoff EG, Geelhoed-Mieras MM, Verschuren EJ, et al. The loss of immunodominant epitopes affects interferon-gamma production and lytic activity of the human influenza virus-specific cytotoxic T lymphocyte response in vitro. Clin Exp Immunol. 2007 May;148(2):296–306. doi: 10.1111/j.1365-2249.2007.03340.x. [DOI] [PMC free article] [PubMed] [Google Scholar]