Abstract
We randomized 332 women, 18–24 years old who were not explicitly seeking treatment for their marijuana use, to either a two-session motivationally-focused intervention or an assessment only condition. Assessed by time-line follow-back methodology, participants reported using marijuana 57 % of days in the three months prior to study entry. Intervention effects on the likelihood of marijuana use were not statistically significant at 1-month (OR = 0.77, p = .17), significant at 3-months (OR = 0.53, p=.01), and no longer significant at 6-months (OR = .74; p = .20). Among the 61% of participants endorsing any desire to quit using marijuana at baseline, significant intervention effects on the likelihood of marijuana use days were observed at 1- (OR = 0.42, p = .03), 3- (OR = 0.31, p = .02), and 6-months (OR = 0.35, p = .03). A two-session brief motivational intervention reduced marijuana use among young women not seeking treatment. Women with a desire to quit showed a greater and more durable response.
Keywords: marijuana, motivational interviewing, women, motivation to change, clinical trial
1. Introduction
Recent estimates suggest that 16.5% of young persons between the ages of 18–25 have used marijuana in the past month (Substance Abuse and Mental Health Services Administration, 2009), and over half have used marijuana in their lifetime (Substance Abuse and Mental Health Services Administration, 2007). In this age group, men and women differ in their quantity, frequency and symptoms of use, as well as endorsement of marijuana-related problems (Agrawal & Lynskey, 2007; Grant, et al., 2006). Rates of past month use have generally increased in the past two decades among females, especially adolescents (Wallace, et al., 2003). Women are often “early initiators” (Flory, Lynam, Milich, Leukefeld, & Clayton, 2004), beginning marijuana use earlier than men, putting them at increased risk of developing a marijuana use disorder (Substance Abuse and Mental Health Services Administration, 2008).
Marijuana use is associated with accidents and injuries (Dennis, Babor, Roebuck, & Donaldson, 2002; Hall & Babor, 2000), executive dysfunction (Lundqvist, Jonsson, & Warkentin, 2001), respiratory disease (Taylor, et al., 2002), polysubstance use (Magill, Barnett, Apodaca, Rohsenow, & Monti, 2009). Depressive disorders are more common in women with cannabis disorders than men (Harder, Morral, & Arkes, 2006). Several researchers have argued that females carry a heightened risk for the adverse physical, mental and social consequence of substance use (Brady & Randall, 1999; Greenfield, Manwani, & Nargiso, 2003). As such, young females constitute a particularly high-risk marijuana-using group who require attention.
Psychosocial interventions effective in decreasing use and promoting abstinence for marijuana-dependent adults have included cognitive behavioral therapy (CBT) and contingency management (CM) treatments (Budney, Roffman, Stephens, & Walker, 2007). A brief motivational intervention (MI), with its limited contact time, cost effectiveness, and client-centered approach, may be particularly promising for the great majority of marijuana users who don‘t seek treatment but may have interest in reducing or quitting (Miller & Rollnick, 2002). Using a single session of a brief motivational intervention , one study found a significant effect on reducing marijuana use at 3 months among 16–20 year olds who reported smoking marijuana at least weekly (McCambridge & Strang, 2004). In a second study, a brief “Marijuana Check-Up” MI decreased use among 97 adolescents at 3 months (Walker, et al., 2006). The largest brief motivational intervention study targeting adult non-treatment seekers, advertised for persons interested in receiving “objective feedback about marijuana use” (Stephens, Roffman, Fearer, Williams, & Burke, 2007). The 188 participants with a mean age of 33 were near-daily marijuana users, 93% of whom met criteria for marijuana abuse or dependence. Participants were also relatively homogenous: predominantly male, white, and employed. Persons assigned to a single 90-minute MI session reported fewer marijuana use days at 12 months (though not significantly different at 2 or 6 months) with an effect size of .45, compared to either a delayed feedback or an educational control condition. In summary, these brief motivational intervention studies focused on non-treatment-seekers, the predominant population of marijuana users in the United States, but did not specifically target 18–24 year olds, the age group with the highest prevalence, enroll persons with lower levels of use, or focus on women.
Among variables that influence treatment efficacy, willingness to alter one‘s substance use behaviors seems central. In the opiate dependence treatment literature, higher levels of motivation to change are associated with reductions in drug use (Nosyk, et al., 2010). In the alcohol literature however, the predictive value of readiness to change measures has been mixed. Some work has found that lower readiness-to-change predicts reduced intervention efficacy among young adult alcohol users (Carey, Henson, Carey, & Maisto, 2007; Fromme & Corbin, 2004). However, other studies have reported that readiness was not predictive of subsequent alcohol consumption (Bertholet, Cheng, Palfai, Samet, & Saitz, 2009; Forsberg, Ekman, Halldin, & Ronnberg, 2004; Reed, et al., 2005; Williams, Horton, Samet, & Saitz, 2007). Among non-treatment-seeking marijuana users followed naturalistically, initial change goal was a poor predictor of outcome (Hughes, Peters, Callas, Budney, & Livingston, 2008). Yet among incarcerated adolescents, motivation to change predicted severity of use 3 months after release (Slavet, et al., 2006), and among adolescents attending an intensive outpatient treatment program for marijuana, motivation to abstain predicted fewer days of use in the following month (King, Chung, & Maisto, 2009). Whether readiness or desire to change or abstain is a requisite condition for marijuana use reduction during MI interventions among young adults remains unexplored.
Previous intervention studies have enrolled few women and have not targeted young adults, the age group that reports the highest marijuana use prevalence(De Dios, et al., 2010). The current randomized trial addresses these unexplored groups, and tests the hypothesis that among non-treatment-seeking women aged 18–24 who are engaging in marijuana use, a brief motivational marijuana intervention (MI) will result in less marijuana use relative to assessment only (AO), as indexed by lower percentage of marijuana use days.
2. Methods and Materials
2.1 Study Design and Procedure
The study sample was recruited from the community through newspaper and radio advertisements for a “research study about the health behaviors of young adult women.” Women responding to the ads were screened for eligibility with a brief phone interview, and if interested were scheduled for a comprehensive assessment.
Inclusion criteria included: 1) smoking marijuana at least 3 times in the past three months, 2) aged 18–24, 3) living within 20 miles of Providence RI and planning to remain in the geographic area for the next 6 months, 4) speaking English, 5) not pregnant, and 6) not meeting criteria for substance dependence other than marijuana, alcohol, or nicotine within the past year. Although the consent form indicated that participants could be randomized to an intervention condition in which they would receive two sessions with a clinician to discuss their health behaviors, an explicitly stated commitment to reduce or quit marijuana use was not an enrollment criterion. The trial protocol was approved by the Institutional Review Board of Butler Hospital. In addition, a federal Certificate of Confidentiality was obtained to ensure participant privacy.
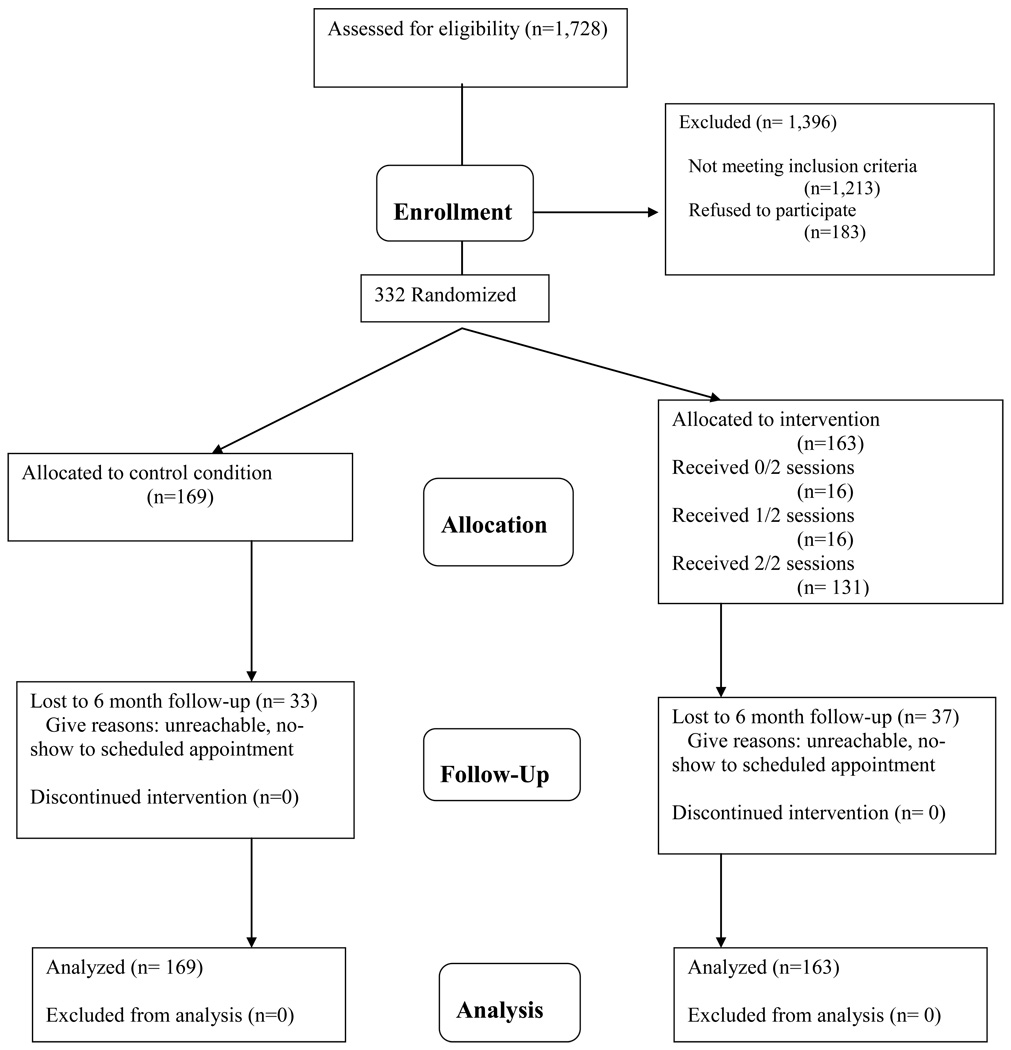
Between January 2005 and May 2009, 1,728 individuals were screened by phone and 1,213 were excluded for not meeting eligibility criteria (see Figure 1) for the following reasons: had not smoked marijuana in the last 3 months (n=958) or marijuana use frequency was too low (n=60); did not meet secondary criteria (e.g., were pregnant, non-English speaking, older than 24, lived too far from the study site or were drug dependent, n=140); did not provide enough information to determine eligibility (n=55). Of the 515 eligible women, 183 refused or were unable to enroll. A total of 332 women were enrolled in the trial. Eligible persons provided informed consent and were enrolled in a randomized clinical trial to reduce marijuana use comparing a 2-session motivationally-focused intervention (MI) to assessment only (AO). Women were compensated for all assessment visits.
Figure 1.
Recruitment flowchart
2.2 Schedule of the Intervention
Following the baseline assessment, participants were randomized to the MI condition or the assessment only (AO) condition. Research staff performing the assessments was blinded to assigned condition. All women were scheduled for follow-up assessment at 1-, 3-, and 6-months following the baseline assessment. All interviews and intervention sessions were completed at a hospital-based research site.
For each MI participant, two individual sessions were scheduled, each lasting approximately 45 minutes. The initial MI session was conducted on the same day immediately following the baseline assessment. The second MI session was scheduled for one month later, and occurred on the same day immediately following the 1-month assessment. Participants assigned to AO completed baseline, 1-, 3-, and 6-month assessment visits only. Participants were compensated $30 for the baseline, $20 for the 1-month, $40 for the 3-month, and $50 for the 6-month assessments.
2.3 Manual Development and Therapist Training
The manual for MI intervention was adapted from the MI approach of Miller & Rollnick (Miller & Rollnick, 2002). Training consisted of reviewing five basic principles, 1) expressing empathy; 2) developing discrepancy; 3) avoiding argumentation; 4) rolling with resistance; 5) supporting self-efficacy. All sessions were audiotaped and reviewed in biweekly supervision sessions.
A modification of the Motivational Interviewing Skill Code 1.0 (MISC) (Miller, 2000) was used both to train the five female study interventionists (four clinical psychologists and one masters‘ level clinician) and to monitor their MI skills during biweekly supervision. The MISC 1.0 allowed for an assessment of threshold competence for interventionists and provided measures for feedback during supervision.
To quantify the integrity of the MI sessions, the MITI 3.1 coding form was used (Moyers, Martin, Manuel, Miller, & Ernst, 2009). Three raters, trained in MI, developed inter-rater reliability (mean intraclass coefficient for behavioral scales = .83; for global scales = .72) by coding a set of sessions from this study. The Direction global scale was not counted in this mean global scale ICC because there was very little variability in scores (all coders rated the sessions with a 4 or a 5), invalidating the ICC statistic. Because this level of reliability fell into the “good” and “excellent” categories of reliability (Cicchetti, 1994), it was decided that the 3 raters met the threshold of independent coding. A random sample of sessions, separate from those used to establish reliability, was created for the 3 raters to code in pairs, in order to determine whether the intervention sessions met a threshold of MI competence. These independently coded sessions were coded on the 5-point MITI scale; global scores above 4 are considered to be reflective of MI competence. Mean scores for the three raters across the scales were 4.31 (SD .74; Evocation), 4.15 (SD .72; Collaboration), 4.24 (SD .68; Autonomy/Support), 4.73 (SD .52; Direction), 4.25 (SD .68; Empathy).
2.4 Initial MI Session
Participants were told at the onset that the intervention sessions were an opportunity to learn more about themselves, and that while there would be discussion about their marijuana use, there was no ’hidden agenda‘ about having to quit. Rather, the goals of this session—raising awareness of the pros and cons of marijuana use, exploring any conflicting motivation governing the decision to change, and organizing strategies to deal with internal or external obstacles to achieving change goals—could apply to any type of health behavior the participant was interested in changing, or could simply be an exercise in how to make such changes should she be interested at some time in the future. Interventionists engaged participants in a discussion of values and goals, thoughts about cutting back/quitting, state of readiness to make changes, and provided feedback from the research assessment materials. This discussion led to the option of generating a change plan, should the participant choose to do so. Participants were told that the Change Plan form could be used for any goal, such as a health behavior goal (such as increasing exercise) or a general life goal (such as completing an education degree), in addition to or instead of a marijuana-related goal. If participants were unable to generate an idea for a goal, and did not explicitly state they did not want to set a goal, common goals were offered as examples, such as increased exercise, change in diet, or change in money or time management. At the end of the session, change plan sheets and an assessment feedback report were given to participants and the next appointment date was set. If the participant set a non-marijuana goal (e.g., quit cigarette use), the end of the session focused on generation of a change plan to achieve this goal.
2.5 Follow-up MI Session
The follow-up session was based on the participants‘ goals and change plans from the initial session. For participants with a marijuana use change plan, the follow-up session focused on progress, assessment of barriers, and developing concrete strategies for meeting new goals. Recovery strategies were also discussed, with an emphasis on identifying situations with high risk for relapse and developing effective strategies for coping with these situations.
If the participant set a non-marijuana goal, the session focused on progress and barriers in achieving this goal. MI techniques were used to review the information from the first session in order to re-evaluate the interest in setting a marijuana-related goal. Participants were also offered suggestions about interim steps which they might consider prior to setting an abstinence goal, such as gaining knowledge about trigger situations, and/or beginning to increase quality of life activities such as exercising, or using stress management techniques.
For those participants who did not set any goals in the first session, MI techniques were used to review the information from the first session in order to re-evaluate the interest for setting a health-related, marijuana-related risk behavior, and/or marijuana- related risk behavior goal.
2.6 Measures
During the baseline assessment, staff collected general demographic information, and a 90-day time-line follow-back (TLFB) report on marijuana, alcohol and other substance use (Sobell & Sobell, 1992). Other measures included the Marijuana Problem Scale (Stephens, Roffman, & Curtin, 2000). This 19-item summated three-point rating scale measures the number and severity of problems associated with marijuana use during the past 90 days; internal-consistency reliability in this cohort was .84. Marijuana abuse and dependence was assessed by the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) (First, Spitzer, Gibbon, & Williams, 2002). A 3-month time frame was used to assess current level of dependence. Desire to quit marijuana was measured as a single item change ladder (Amodei & Lamb, 2004; Biener & Abrams, 1991) with wording adapted from the Thoughts About Abstinence scale (Marlatt, Curry, & Gordon, 1988). Participants were asked to rate their current desire to quit with the question: On a scale from 1 to ten, with one representing no desire to quit, give yourself a rating. Choose the number between 1 and 10 that best describes your own desire to stop using marijuana at this time. Remember, the higher the number, the greater your desire. Because this indicator was very skewed with 39.6% of participants reporting no desire to quit, we compared those endorsing any desire to quit to those with no desire to quit using marijuana.
At 1-, 3-, and 6-month follow-up assessments the TLFB was used to assess marijuana, alcohol and other substance use since the date of a participant‘s last interview.
2.7 Analysis Plan
We present descriptive statistics to summarize the baseline characteristics of this cohort; t-tests for differences in means and the χ2-test of independence are used to compare groups with respect to background characteristics and study retention. Logistic regression analysis was used to determine if study attrition was systematically associated with demographic characteristics or baseline indicators of marijuana use frequency and problem severity. Our primary outcome, marijuana use, was assessed using the TLFB assessments. Preliminary analysis indicated that summary measures of use frequency resulted in bimodal distributions at each assessment that were not appropriate for analysis with normal theory methods. Additionally, these distributions were not well approximated by Poisson or negative binomial distributions that would be appropriate for analyzing count data. Therefore, we used random intercept logistic regression to estimate the effect of intervention on the likelihood of using marijuana on any TLFB day. This approach has the advantage of using all available data while using a binomial error distribution to model dichotomous outcomes.
Our initial step was to estimate models describing the growth process. Alternatives considered included linear change over time, quadratic change over time, and unconstrained change in which separate parameters are estimated to describe differences in the likelihood of marijuana use at each time point. The relative fit of models is compared using the Satorra-Bentler (Satorra & Bentler, 2001) scaled χ2-test.
Our next step was to determine if change in marijuana use over time was conditioned on treatment assignment. Here, intervention effects were estimated as the treatment by time interaction. To determine if the effect of intervention was moderated by baseline desire to quit using marijuana, we estimated models including the treatment by time by desire to quit interaction.
In all of these models, the random intercept represents the joint effect of all time-invariant subject specific characteristics influencing individuals‘ overall propensity to use to marijuana. To describe the fixed part of the model we present exponentiated coefficients giving the effect on the odds of using marijuana on any day during the period assessed and 95% confidence interval estimates. All confidence interval estimates and tests of significance are based on robust sandwich standard error estimators adjusted for within-subject clustering (Satorra & Bentler, 2001). To facilitate interpretation, we also present line graphs comparing the estimated probability of marijuana use by treatment and time of assessment. The estimated probabilities were subject-specific and depended on individuals‘ initial propensities to use marijuana. However, the pattern and relative magnitude of differences in probabilities were functions of the fixed parameters. Here, we evaluated the expected probability by setting the random intercept at the mean of 0 (e.g., subjects with an average initial propensity to use marijuana).
As an ancillary analysis we also estimated the effect of intervention on marijuana problem severity which was assessed only at baseline, 3-, and 6-months. The analytic strategy paralleled that described for the primary outcome but random intercept linear regression was used to model the continuous outcome. Models were estimated using the generalized linear latent and mixed models module (Rabe-Hesketh & Skrondal, 2008) in Stata 10.1 (StataCorp, 2008).
3. Results
Participants were ethnically diverse (Table 1). Almost 70% reported attending some college or had completed a college degree. On average, participants had used marijuana for 3.9 (SD = 2.6) years, and 39.5% met SCID diagnostic criteria for marijuana dependence. The mean proportion of days on which participants used marijuana prior to baseline was .57 (SD = .34). There was no evidence of statistically significant between group differences on demographic characteristics or baseline measures of marijuana use or problems. Study attrition during follow-up was not associated significantly with age (OR = 1.11, z = 1.02, p = .306), ethnicity (OR = .83, z = −0.98, p = .327), education (OR = 1.15, z = 1.10, p = .270), years of regular marijuana use (OR = 1.07, z = .090, p = .369), proportion of days using marijuana (OR = 0.51, z = −1.20, p = .232), marijuana problem severity index scores (OR = 0.99, z = −0.14, p = .887), meeting criteria for marijuana abuse (OR = 0.62, z = −1.21, p = .226), meeting criteria for marijuana dependence (OR = 1.34, z = −1.21, p = .226) or treatment condition (OR = 0.91, z = −0.67, p = .503).
Table 1.
Baseline Characteristics by Intervention (n = 332)
| Total (n = 332) |
Control (n = 169) |
MI (n = 163) |
t (p = ) | |
|---|---|---|---|---|
| Age (Yrs) | 20.5 (±1.8) | 21.0 (±1.8) | 20.5 (±1.7) | 0.50 (.617) |
| Prop. Days Used MJ | .57 (±.34) | .55 (±.34) | .59 (±.34) | −1.07 (.285) |
| Years Regular MJ Use | 3.92 (±2.58) | 4.05 (±2.48) | 3.79 (±2.67) | 0.95 (.345) |
| Marijuana Problem Severity (range 0–24) |
4.90 (±4.68) | 4.99 (±4.71) | 4.82 (±4.66) | 0.33 (.738) |
|
χ2 (p =) |
||||
| Ethnicity | ||||
| Caucasian | 225 (67.8%) | 107 (63.3%) | 118 (72.4%) | 4.35 (.226) |
| African-American | 35 (10.5%) | 18 (10.7%) | 17 (10.4%) | |
| Hispanic | 38 (11.5%) | 22 (13.0%) | 16 (9.8%) | |
| Other | 34 (10.2%) | 22 (13.0%) | 12 (7.4%) | |
| Some College or Degree | 232 (69.9%) | 121 (71.6%) | 111 (68.1%) | 0.48 (.487) |
| Met MJ Dependence | 131 (39.6%) | 67 (39.6%) | 64 (39.5%) | 0.00 (.979) |
| Any Desire to Quit Using | 200 (60.2%) | 108 (63.5%) | 92 (56.8%) | 1.57 (.210) |
| n (%) 1-Mo. Assessment | 283 (85.2%) | 149 (88.2%) | 134 (82.2%) | 2.34 (.126) |
| n (%) 3-Mo. Assessment | 264 (79.5%) | 138 (81.7%) | 126 (77.3%) | 0.97 (.325) |
| n (%) 6-Mo. Assessment | 262 (78.9%) | 136 (80.5%) | 126 (77.3%) | 0.50 (.479) |
| n (%) At Least 1 FU | 302 (90.1%) | 159 (94.1%) | 143 (87.7%) | 4.07 (.044) |
MJ=marijuana
FU=follow-up
A quadratic time model fit the observed marijuana use over time data significantly better than a linear time model (S-B Scaled χ2 = 13.54, df = 1, p < .001), and an unconstrained time model estimating a separate parameter comparing the likelihood of marijuana use at each follow-up to baseline fit the observed data significantly better than the quadratic time model (S- B Scaled χ2 = 19.18, df = 1, p < .001). Coefficients indicated that relative to baseline, the odds of marijuana use was significantly lower at 1-month (OR = 0.55, z = −6.22, p < .001), 3-months (OR = 0.56, z = −4.76, p < .001), and 6-months (OR = 0.54, z = −5.23, p < .001). Based on these analyses, we next estimated a model in which the separate effects of intervention were estimated for each follow-up assessment.
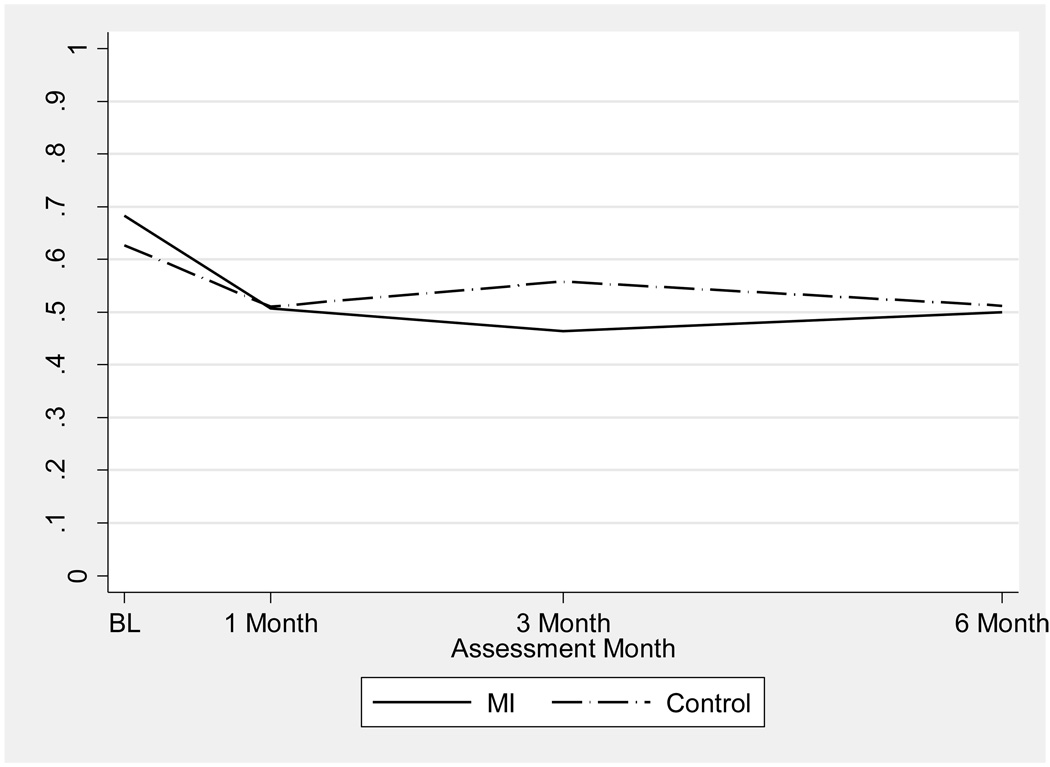
Based on the analysis of change in marijuana use, the primary outcomes analysis estimated separate effects of intervention for each follow-up assessment (see Model 1 in Table 2). The coefficients for time give the estimated change in the odds of marijuana use at 1-, 3-, and 6-months, relative to baseline, among controls. Compared to baseline, the expected odds of marijuana use among controls was about 62% (OR = .62, z = −3.80, p < .001), 75% (OR = .75, z = −1.96, p = .051), and 63% (OR = .63, z = −3.05, p = .002) as large at 1-, 3-, and 6-months, respectively. The effect of intervention is represented by the coefficients for the treatment by time interaction; these indicate that MI participants had larger reductions in the odds of marijuana use at all three time points. The between group differences in the reduction of marijuana were not significant at 1-month (OR = 0.77, z = −1.36, p = .174) or at 6-months (OR = 0.74, z = −1.28), p = .202). However, the effect of intervention was statistically significant at 3-months (OR = 0.53, z = −2.59, p = .010). For individuals with an average initial propensity to use marijuana (random intercept = 0), the estimated probability of marijuana use decline from .683 at baseline to .464 at 3 months; among corresponding controls, the estimated probabilities of marijuana use were .627 and .558 respectively. Converted to rates of use per 30 days, these differences represent a 2.07 day reduction among controls and a 6.58 day reduction among women randomized to MI. The estimated conditional probabilities of marijuana use at all assessments as specified by Model 1 in Table 2 are shown in Figure 2, illustrating the pattern of between group differences over time.
Table 2.
Mixed Linear Logistic Regression Models Estimating the Effective of Motivational Interviewing on the Likelihood of Marijuana Use at Follow-Up (n = 332 subjects observed on 83,052 person days).
| Model 1 | Model 2 | ||||
|---|---|---|---|---|---|
| Fixed Effects | OR | 95%CI | OR | 95%CI | |
| Treatment (MI = 1) | 1.28 | (0.76 – 2.17) | 1.15 | (0.49 – 2.70) | |
| Any Desire To Quit (Yes = 1) | 0.32** | (0.15 – 0.68) | |||
| Time | |||||
| Month 1 | 0.62** | (0.49 – 0.79) | 0.43** | (0.30 – 0.62) | |
| Month 3 | 0.75 | (0.57 – 1.00) | 0.44** | (0.26 – 0.74) | |
| Month 6 | 0.63** | (0.46 – 0.85) | 0.41** | (0.24 – 0.72) | |
| Treatment by Time | |||||
| Month 1 | 0.77 | (0.53 – 1.12) | 1.41 | (0.77 – 2.58) | |
| Month 3 | 0.53** | (0.33 – 0.86) | 1.17 | (0.54 – 2.52) | |
| Month 6 | 0.74 | (0.47 – 1.17) | 1.44 | (0.65 – 3.22) | |
| Treatment by Quit Desire | 0.96 | (0.33 – 2.73) | |||
| Quit Desire by Time | |||||
| Month 1 | 1.64* | (1.02 – 2.63) | |||
| Month 3 | 2.19* | (1.18 – 4.07) | |||
| Month 6 | 1.78 | (0.94 – 3.37) | |||
|
Treatment by Quit Desire by Time |
|||||
| Month 1 | 0.42* | (0.20 – 0.90) | |||
| Month 3 | 0.31* | (0.12 – 0.83) | |||
| Month 6 | 0.35* | (0.13 – 0.91) | |||
|
Random Effects |
|||||
| Subject (Variance) | 4.99** | 4.56** | |||
| Log L | - | - | |||
| 36908.8 | 36257.6 | ||||
p < .05,
p < .01
Model 2 includes n=328; 4 persons missing Quit Desire response
Figure 2.
Estimated Probabilitya of Marijuana Use by Time and Intervention.
a The presented probabilities are conditional on a subject specific random intercept equal to 0.
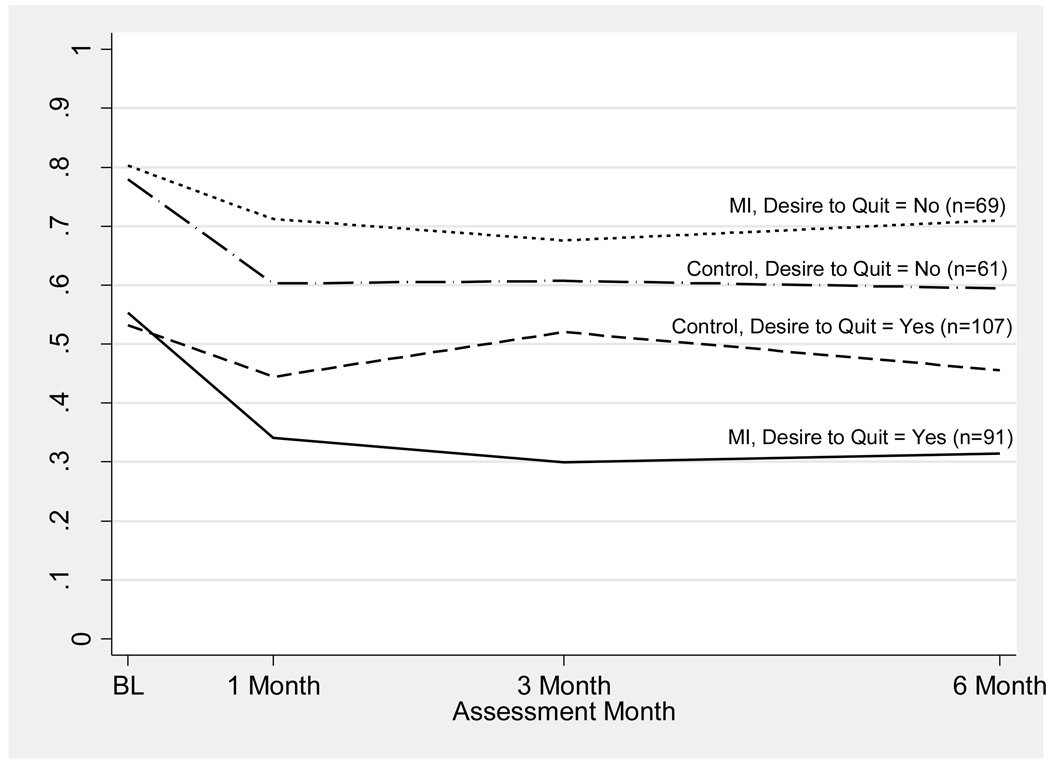
Model 2 (Table 2) extends the primary outcomes analysis by including the treatment by time by desire to quit using marijuana at baseline as an interaction term. Model 2 also includes all implied lower order interaction terms and tests the hypothesis that the effect of intervention on change in marijuana use is moderated by desire to quit using marijuana at baseline. Here, statistically significant treatment by desire to quit using marijuana are observed at 1- (OR = 0.42, z = −2.25, p = .025), 3- (OR = 0.31, z = −2.33, p = .020), and 6-months (OR = 0.35, z = −2.15, p = .032). The nature of this interaction and the estimated probabilities as specified in this model are shown in Figure 3.
Figure 3.
Estimated Probabilitya of Marijuana Use by Time, Intervention., and Any Desire to Quit Using Marijuana at Baseline (n = 328b).
a Estimated probabilities are conditional on a subject specific random intercept equal to 0.
b Data on quit desire were missing for 4 participants.
The two top line graphs in Figure 3 reflect treatment group differences among participants expressing no desire to quit using marijuana at baseline. At baseline, 91 (56.9%) participants randomized to MI and 107 (63.7%) controls endorsed any desire to quit using marijuana. Among those with no motivation to quit the effects of intervention did not approach statistically significant levels at any time point. For controls with no desire to quit using marijuana and an average baseline propensity to use marijuana, the estimated probability of use decreased from .80 at baseline, to .60, .61, and .59 at 1-, 3-, and 6-months, respectively. Among comparable participants randomized to MI the estimated probabilities of marijuana use were .80 at baseline, .71 at 1-month, .67 at 3-months, and .71 at 6-months.
A very different pattern is observed among those who expressed a desire to quit using marijuana at baseline; the estimated conditional probabilities are shown in the two lower line graphs in Figure 3. For those randomized to MI, the expected probability of marijuana use decreases sharply from baseline to 1-month and remains relatively stable through the 6-month follow-up. Among controls who endorsed any desire to quit using marijuana, the expected probability of marijuana remained near the baseline levels through the 6-month assessment.
Of the 163 women assigned to the brief motivational intervention, 79 (49%) set a marijuana change goal at baseline. Setting a marijuana change goal was significantly associated with endorsing any desire to quit (χ2 = 14.17, p<.001), but 40% of women who endorsed any desire to quit did not set a marijuana change goal. Relative to baseline, marijuana use at 1- (OR = 0.82, z = −0.67, p = .501), 3- (OR = 0.75, z = −0.75, p = .455), or 6-months (OR = 1.37, z = 0.88, p = .378) did not differ significantly between participants who did or did not set a marijuana change goal during intervention.
As an auxiliary analysis, we also used random intercept linear regression to estimate the effect of intervention on marijuana problem severity. Relative to baseline, MI did not significantly reduce marijuana problem severity at either 3- (b = −.40, z = −.93, p = .353) or 6-months (b = −.10, z = −.14, p = .890).
4. Discussion
We found that this two-session brief motivational intervention reduced marijuana use among young women during the 3 months following the baseline assessment. The subgroup of women who had a desire to quit at study entry had a greater and more durable response to MI out to six months.
There is evidence supporting a variety of effective intervention approaches for adult marijuana users who are interested in treatment to cease or reduce use (Budney, et al., 2007). These treatment programs typically enroll marijuana dependent persons who are willing to receive longer, more intensive treatment protocols than the one offered here. Yet among the 25.8 million Americans aged 12 years or older who have used marijuana in the past year, fewer than 2% seek formal drug treatment (Substance Abuse and Mental Health Services Administration, 2009). These non-treatment-seekers are often not ready to stop using, cannot afford the cost of specialty drug treatment, may be experiencing or perceiving few negative consequences from marijuana use, or may be ambivalent about stopping because seeking treatment implies that they have a “drug problem.” Still, previous work suggests that many users may, upon review, decide to change their marijuana use even if they are initially ambivalent (Stephens, et al., 2007).
There have been several earlier reports of brief interventions to reduce marijuana use among persons not ready to approach formal treatment (McCambridge & Strang, 2004; Stephens, et al., 2007; Walker, et al., 2006). Our sample was demographically quite different from these earlier studies which enrolled predominantly males and Caucasians, often including persons with daily marijuana smoking histories of 10 or more years. Our female cohort reported using marijuana on average 3 out of 5 days at baseline, but included women with a wide range of use, from infrequent to multiple times per day.
While our overall effect size was similar to that reported by Stephens et al., (Stephens, et al., 2007), we found larger reductions in marijuana use among the 61% who reported a desire to quit at study entry which accounted for the intervention efficacy prediction. In the current study at baseline, the subgroup that expressed a desire to quit had a significantly lower frequency of marijuana use than the subgroup with no desire to quit (see Figure 3). Perhaps MI received by those with an intrinsic desire to quit prompted a more facile change in social-contextual variables (substance-free activities, new social networks) that led to greater reductions in marijuana use.
Interestingly, setting a marijuana change goal was not associated with significant reductions in marijuana use among those randomized to the brief motivational intervention. This suggests that response to a desire to change questionnaire and goal-setting in the presence of a clinician are cognitively different. “Readiness to change” is not monolithic; measures designed to predict change may be capturing different concepts such as importance of change or confidence in change, and “readiness” may be dependent on a variety of internal and external influences.
The mechanisms underlying MI‘s efficacy across a variety of substances remain obscure (Apodaca & Longabaugh, 2009; Dunn, Deroo, & Rivara, 2001). MI treatment here clearly increased self-regulation, particularly those with a desire to make changes at study entry, and we speculate that our decisional balance exercise may have increased perceived cons of marijuana use or allowed for the exploration of rewards provided by activities other than substance use. However this was not an MI dismantling study and there is no attention-control comparison condition; our intervention may have had non-specific effects.
The significant effect of MI at 3 months but not 6 months is consistent with results of meta-analyses of MI for substance use (Hettema, Steele, & Miller, 2005; Vasilaki, Hosier, & Cox, 2006). How to maintain marijuana use reduction beyond 3 months, and determining the optimal timing and number of MI sessions to enhance treatment effects for this population remain open to further study. The effect at 3 months, as noted, was achieved mainly through moderation of use rather than cessation, although cessation could be a goal over longer follow-up periods for those who successfully reduce in the shorter term. Because abstinence was not the goal of MI in this trial of non-treatment seekers, we were not surprised that few participants stopped using marijuana entirely during the 6 months of follow-up (n=3).
Of note, the significant treatment effect on marijuana use at 3 months was not associated with a parallel reduction in marijuana-related problems, most likely due to the low level of problems reported by this cohort at baseline, a floor effect. The baseline problem scale score of our cohort was considerably lower than that reported in sample of treatment seekers, and lower also than that reported in Stephens et al‘s samples of non-treatment seekers (Stephens, et al., 2007; Stephens, et al., 2004). Perhaps the specifics of our sample (younger participants with shorter marijuana use histories, women, lower average of days-per-week used) limited accumulation of problems. Stephens et al also did not find a reduction in marijuana-related problems despite a reduction in marijuana use (Stephens, et al., 2007).
This trial had limitations. Marijuana use outcomes were based on self-report, although they were assessed by trained staff using validated instruments and procedures to aid recall and minimize bias. Second, we did not measure other potential moderating variables (e.g., social support). Third, we had broader a marijuana use inclusion criterion than other studies, enrolling even infrequent marijuana users in the belief that some participants would become abstinent, but also with the understanding that lower frequency users might have less problematic use, fewer reasons to quit, and little room to reduce use. Because of the inclusion of infrequent users, we did not require biological verification of marijuana use at baseline or follow-ups. Fourth, interventionists were clinicians experienced in MI, which may limit generalizability to settings where clinicians have less MI training. Finally, these findings may not pertain to older women or to men.
Young adults have a high prevalence of marijuana use frequently contributing to negative life consequences. While this group typically doesn‘t seek help for marijuana-related problems, our findings suggest that a brief motivational interviewing intervention for marijuana use, if applied in primary care or behavioral health settings, may have a positive impact. This type of approach may appeal to a wider range of users in terms of age, frequency of use, and readiness to change or quit than more formal treatments. If the effects demonstrated here can be replicated and extended, MI could add to the continuum of care for young adult marijuana users.
Acknowledgements
This study was supported by NIDA grant R01 DA018954. Dr. Stein is a recipient of NIDA Award K24 DA000512. The authors thank Dr. Alan Budney for his early critique of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Trial registered at clinicaltrials.gov; Clinical Trial #NCT00227864
No author on this manuscript has any personal or financial interest that would influence the results.
References
- Agrawal A, Lynskey MT. Does gender contribute to heterogeneity in criteria for cannabis abuse and dependence? Results from the national epidemiological survey on alcohol and related conditions. Drug and Alcohol Dependence. 2007;88(2–3):300–307. doi: 10.1016/j.drugalcdep.2006.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amodei N, Lamb RJ. Convergent and concurrent validity of the Contemplation Ladder and URICA scales. Drug and Alcohol Dependence. 2004;73(3):301–306. doi: 10.1016/j.drugalcdep.2003.11.005. [DOI] [PubMed] [Google Scholar]
- Apodaca TR, Longabaugh R. Mechanisms of change in motivational interviewing: a review and preliminary evaluation of the evidence. Addiction. 2009;104(5):705–715. doi: 10.1111/j.1360-0443.2009.02527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertholet N, Cheng DM, Palfai TP, Samet JH, Saitz R. Does readiness to change predict subsequent alcohol consumption in medical inpatients with unhealthy alcohol use? Addictive Behaviors. 2009;34(8):636–640. doi: 10.1016/j.addbeh.2009.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biener L, Abrams DB. The contemplation ladder: Validation of a measure of readiness to consider smoking cessation. Health Psychology. 1991;10(5):360–365. doi: 10.1037//0278-6133.10.5.360. [DOI] [PubMed] [Google Scholar]
- Brady KT, Randall CL. Gender differences in substance use disorders. The Psychiatric Clinics of North America. 1999;22(2):241–252. doi: 10.1016/s0193-953x(05)70074-5. [DOI] [PubMed] [Google Scholar]
- Budney A, Roffman R, Stephens R, Walker D. Marijuana dependence and its treatment. Addiction Science and Clinical Practice. 2007;4(1):4–16. doi: 10.1151/ascp07414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Henson JM, Carey MP, Maisto SA. Which heavy drinking college students benefit from a brief motivational intervention? Journal of Consulting and Clinical Psychology. 2007;75(4):663–669. doi: 10.1037/0022-006X.75.4.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological Assessment. 1994;6(4):284–290. [Google Scholar]
- De Dios MA, Anderson BJ, Herman DS, Hagerty CE, Caviness CM, Budney AJ, et al. Marijuana use subtypes in a community sample of young adult females. Women's Health Issues. 2010;20(3):201–210. doi: 10.1016/j.whi.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M, Babor TF, Roebuck MC, Donaldson J. Changing the focus: The case for recognizing and treating cannabis use disorders. Addiction. 2002;97(Suppl 1):4–15. doi: 10.1046/j.1360-0443.97.s01.10.x. [DOI] [PubMed] [Google Scholar]
- Dunn C, Deroo L, Rivara F. The use of brief interventions adapted from motivational interviewing across behavioral domains: a systematic review. Addiction. 2001;96(12):1725–1742. doi: 10.1046/j.1360-0443.2001.961217253.x. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Flory K, Lynam D, Milich R, Leukefeld C, Clayton R. Early adolescent through young adult alcohol and marijuana use trajectories: Early predictors, young adult outcomes, and predictive utility. Development and Psychopathology. 2004;16:193–213. doi: 10.1017/s0954579404044475. [DOI] [PubMed] [Google Scholar]
- Forsberg L, Ekman S, Halldin J, Ronnberg S. The readiness to change questionnaire: reliability and validity of a Swedish version and a comparison of scoring methods. Br J Health Psychol. 2004;9(Pt 3):335–346. doi: 10.1348/1359107041557084. [DOI] [PubMed] [Google Scholar]
- Fromme K, Corbin W. Prevention of heavy drinking and associated negative consequences among mandated and voluntary college students. Journal of Consulting and Clinical Psychology. 2004;72(6):1038–1049. doi: 10.1037/0022-006X.72.6.1038. [DOI] [PubMed] [Google Scholar]
- Grant JD, Scherrer JF, Neuman RJ, Todorov AA, Price RK, Bucholz KK. A comparison of the latent class structure of cannabis problems among adult men and women who have used cannabis repeatedly. Addiction. 2006;101(8):1133–1142. doi: 10.1111/j.1360-0443.2006.01463.x. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Manwani SG, Nargiso JE. Epidemiology of substance use disorders in women. Obstetrics and Gynecology Clinics of North America. 2003;30(3):413–446. doi: 10.1016/s0889-8545(03)00072-x. [DOI] [PubMed] [Google Scholar]
- Hall W, Babor T. Cannabis use and public health: assessing the burden. Addiction. 2000;95(4):485–490. doi: 10.1046/j.1360-0443.2000.9544851.x. [DOI] [PubMed] [Google Scholar]
- Harder VS, Morral AR, Arkes J. Marijuana use and depression among adults: Testing for causal associations. Addiction. 2006;101(10):1463–1472. doi: 10.1111/j.1360-0443.2006.01545.x. [DOI] [PubMed] [Google Scholar]
- Hettema J, Steele J, Miller W. Motivational Interviewing. Annual Review of Clinical Psychology. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- Hughes J, Peters E, Callas P, Budney A, Livingston A. Attempts to stop or reduce marijuana use in non-treatment seekers. Drug and Alcohol Dependence. 2008;97(1–2):180–184. doi: 10.1016/j.drugalcdep.2008.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King KM, Chung T, Maisto SA. Adolescents' thoughts about abstinence curb the return of marijuana use during and after treatment. Journal of Consulting and Clinical Psychology. 2009;77(3):554–565. doi: 10.1037/a0015391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundqvist T, Jonsson S, Warkentin S. Frontal lobe dysfunction in long-term cannabis users. Neurotoxicol Teratol. 2001;23(5):437–443. doi: 10.1016/s0892-0362(01)00165-9. [DOI] [PubMed] [Google Scholar]
- Magill M, Barnett NP, Apodaca TR, Rohsenow DJ, Monti PM. The role of marijuana use in brief motivational intervention with young adult drinkers treated in an emergency department. Journal of Studies on Alcohol and Drugs. 2009;70:409–413. doi: 10.15288/jsad.2009.70.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt GA, Curry S, Gordon JR. A longitudinal analysis of unaided smoking cessation. Journal of Consulting and Clinical Psychology. 1988;56(5):715–720. doi: 10.1037//0022-006x.56.5.715. [DOI] [PubMed] [Google Scholar]
- McCambridge J, Strang J. The efficacy of single-session motivational interviewing in reducing drug consumption and perceptions of drug-related risk and harm among young people: results from a multi-site cluster randomized trial. Addiction. 2004;99(1):39–52. doi: 10.1111/j.1360-0443.2004.00564.x. [DOI] [PubMed] [Google Scholar]
- Miller W. Motivational Interviewing Skill Code (MISC): Coder's Manual. 2000. Available at http://casaa.unm.edu/codinginst.html.
- Miller W, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd ed. New York, NY: Guilford Press; 2002. [Google Scholar]
- Moyers T, Martin T, Manuel J, Miller W, Ernst D. [Retrieved Accessed 11/2/09];Revised Global Scales: Motivational Interviewing Treatment Integrity 3.1 (MITI 3.1) 2009 [Google Scholar]
- Nosyk B, Geller J, Guh DP, Oviedo-Joekes E, Brissette S, Marsh DC, et al. The effect of motivational status on treatment outcome in the North American Opiate Medication Initiative (NAOMI) study. Drug and Alcohol Dependence. 2010 doi: 10.1016/j.drugalcdep.2010.03.019. in press. [DOI] [PubMed] [Google Scholar]
- Rabe-Hesketh S, Skrondal A. Multilevel and Longitudinal Modeling Using Stata (Second Edition) College Station, TX: Stata Press; 2008. [Google Scholar]
- Reed DN, Jr, Wolf B, Barber KR, Kotlowski R, Montanez M, Saxe A, et al. The stages of change questionnaire as a predictor of trauma patients most likely to decrease alcohol use. J Am Coll Surg. 2005;200(2):179–185. doi: 10.1016/j.jamcollsurg.2004.10.020. [DOI] [PubMed] [Google Scholar]
- Satorra A, Bentler P. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66(4):507–514. doi: 10.1007/s11336-009-9135-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavet J, Stein L, Colby S, Barnett N, Monti P, Golembeske C, et al. The marijuana ladder: measuring motivation to change marijuana use in incarcerated adolescents. Drug and Alcohol Dependence. 2006;83:42–48. doi: 10.1016/j.drugalcdep.2005.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell L, Sobell M. Timeline follow-back: a technique for assessing self-reported alcohol consumption. In: Allen L, editor. Measuring Alcohol Consumption. New York: The Humana Press; 1992. pp. 41–72. [Google Scholar]
- StataCorp. Stata Statistical Software: Release 10.1. College Station, TX: StataCorp LP; 2008. [Google Scholar]
- Stephens R, Roffman R, Curtin L. Comparison of extended versus brief treatments for marijuana use. Journal of Consulting and Clinical Psychology. 2000;68(5):898–908. [PubMed] [Google Scholar]
- Stephens R, Roffman R, Fearer S, Williams C, Burke R. The marijuana check-up: promoting change in ambivalent marijuana users. Addiction. 2007;102(6):947–957. doi: 10.1111/j.1360-0443.2007.01821.x. [DOI] [PubMed] [Google Scholar]
- Stephens R, Roffman R, Fearer S, Williams C, Picciano J, Burke R. The marijuana check-up: reaching users who are ambivalent about change. Addiction. 2004;99(10):1323–1332. doi: 10.1111/j.1360-0443.2004.00832.x. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2006 National Survey on Drug Use and Health: National Findings. Rockville, MD: 2007. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2007 National Survey on Drug Use and Health: National findings. Rockville, MD: 2008. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2008 National Survey on Drug Use and Health: National Findings. Rockville, MD: 2009. [Google Scholar]
- Taylor D, Fergusson D, Milne B, Horwood L, Moffitt T, Sears M, et al. A longitudinal study of the effects of tobacco and cannabis exposure on lung function in young adults. Addiction. 2002;97(8):1055–1061. doi: 10.1046/j.1360-0443.2002.00169.x. [DOI] [PubMed] [Google Scholar]
- Vasilaki EI, Hosier SG, Cox WM. The efficacy of motivational interviewing as a brief intervention for excessive drinking: a meta-analytic review. Alcohol Alcohol. 2006;41(3):328–335. doi: 10.1093/alcalc/agl016. [DOI] [PubMed] [Google Scholar]
- Walker D, Roffman R, Stephens R, Wakana K, Berghuis J, Kim W. Motivational enhancement therapy for adolescent marijuana users: a preliminary randomized controlled trial. Journal of Consulting and Clinical Psychology. 2006;74(3):628–632. doi: 10.1037/0022-006X.74.3.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace JM, Jr, Bachman JG, O'Malley PM, Schulenberg JE, Cooper SM, Johnston LD. Gender and ethnic differences in smoking, drinking and illicit drug use among American 8th, 10th and 12th grade students, 1976–2000. Addiction. 2003;98(2):225–234. doi: 10.1046/j.1360-0443.2003.00282.x. [DOI] [PubMed] [Google Scholar]
- Williams EC, Horton NJ, Samet JH, Saitz R. Do brief measures of readiness to change predict alcohol consumption and consequences in primary care patients with unhealthy alcohol use? Alcoholism: Clinical and Experimental Research. 2007;31(3):428–435. doi: 10.1111/j.1530-0277.2006.00324.x. [DOI] [PubMed] [Google Scholar]