Abstract
Background
Mitral annular calcification (MAC) is a fibrous, degenerative calcification of the mitral valve. The relationship between MAC and cardiovascular disease (CVD) risk factors is not well defined. Thus, we performed a cross-sectional study to determine which CVD risk factors are independently associated with MAC in the Multi-Ethnic Study of Atherosclerosis (MESA).
Methods
MESA includes 6,814 women and men ages 45–84 years old without apparent CVD in 4 ethnic groups (12% Chinese, 38% Caucasian, 22% Hispanic, and 28% African-American). MAC was defined by presence of calcium in the mitral annulus by cardiac computed tomography at enrollment. Multivariable logistic regression was used to evaluate relationships between MAC and CVD risk factors.
Results
The overall prevalence of MAC was 9%. The prevalence of MAC was highest in Caucasians (12%), followed by Hispanics (10%), African Americans (7%) and was lowest in Chinese (5%). Characteristics associated with MAC included age (p<0.01), female gender (p<0.01), increased body mass index (BMI) (p=0.03), and former smoking status (p<0.008). The MAC group had a higher prevalence of hypertension, diabetes mellitus (DM), and family history of heart attack (all p<0.001). After adjusting for all variables, age, female gender, diabetes mellitus, and increased BMI remained strongly associated with MAC.
Conclusions
Age, female gender, DM, and increased BMI were significantly associated with MAC. Prevalence of MAC was strongly associated with female gender and increasing age in all ethnicities.
Keywords: Mitral annular calcification, MESA, Cardiac CT, risk factors
Introduction
Mitral annular calcification (MAC) is a chronic degenerative non-inflammatory process characterized by calcification of the surrounding fibrous support of the mitral valve.1–3 Several studies demonstrated that MAC was associated with atherosclerotic risk factors4–8 and different forms of atherosclerotic cardiovascular disease including carotid stenosis, coronary artery disease, and aortic atheroma.1–3,9–11 The relationship between MAC and cardiovascular disease (CVD) risk factors is not well defined. Cardiac CT is a well-established tool for the detection of arterial calcium in the coronary vasculature and valvular calcification such as MAC.12–13 In the current study we assess the relationship between cardiovascular disease (CVD) risk factors and MAC using cardiac computed tomography (CT) by analyzing data from a multi-ethnic population based cohort of asymptomatic individuals.
Methods
The Multi-Ethnic Study of Atherosclerosis (MESA) was initiated in July 2000 to investigate the prevalence, correlates, and progression of subclinical cardiovascular disease in individuals without known cardiovascular disease.6 This prospective cohort study includes 6,814 women and men ages 45–84 years old recruited from six U.S. communities (Baltimore, MD; Chicago, IL; Forsyth County, NC; Los Angeles County, CA; Northern Manhattan, NY; and St. Paul, MN). The cohort is comprised of 38% Caucasian (N=2,624), 28% African-American (N=1,895), 22% Hispanic (N=1,492) and 12% Chinese (N=803).
Medical history, anthropometric measurements, and laboratory data for the present study were taken from the first examination of the MESA cohort (July 2000 to August 2002). Information about age, gender, race/ethnicity, and medical history were obtained by questionnaires. Current smoking was defined as having smoked a cigarette in the last 30 days. Former smoking was defined as previous smoking who was not met the criteria of current smoking. Diabetes mellitus was defined as a fasting glucose > 126 mg/dL or use of hypoglycemic medications.
Resting blood pressure was measured three times in the seated position using a Dinamap model Pro 100 automated oscillometric sphygmomanometer (Critikon, Tampa, FL) and the average of the second and third readings was recorded. Hypertension was defined as a systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, or use of prescribed medications for hypertension. Body mass index (BMI) was calculated from the equation weight (kg)/height (m2).
Total and high-density lipoprotein (HDL) cholesterol were measured from blood samples obtained after a 12 hour fast. Low-density lipoprotein (LDL) cholesterol was calculated with the Friedewald equation. C-reactive protein (CRP) was measured usuing the BNII nephelometer (N High Sensitity CRP; Dade Behring Inc., Deerfield, IL) at the Laboratory for Clinical Biochemistry Research (University of Vermont, Burlington, VT). Analytical intra-assay CVs ranged from 2.3 to 4.4% and inter-assay CVs ranged from 2.1 to 5.7%.
After signing informed consent, all participants underwent two CT scans at the same time for evaluation of coronary artery calcium and MAC. This study was approved by the Institutional Review Board at all participating centers. Three sites used an Imatron C-150XL CT scanner (GE-Imatron, San Francisco, CA) and three sites used a multidetector CT scanner (four slice). This method has been reported previously8. Image slices were obtained in the supine position with no couch angulation. A minimum of 35 contiguous images with a 2.5 or 3mm slice thickness were obtained starting above the left main coronary artery to the bottom of both ventricles. Each scan was obtained in a single breath hold. Section thickness of 3 mm, field of view of 35 cm, and matrix of 512 × 512 were used to reconstruct raw image data. The nominal section thickness was 3.0 mm for electron beam CT and 2.5 mm for four-detector row CT. Spatial resolution can be described by the smallest volume element, or voxel, for the protocol for each system: 1.15 mm3 for four-detector row CT (0.68 mm × 0.68 mm × 3.00 mm). MAC was defined by presence of calcium on mitral valve by CT scan at the enrollment.
Statistical Methods
Demographics and CVD risk factors were compared between those with and without MAC. Differences in characteristics were compared using ANOVA for continuous variables and χ2 tests for categorical variables. We used logistic regression models to assess the relationship between each risk factor and the presence of calcium and adjusted for all other risk factors in the model. The odds ratios we estimate approximate relative risks because our endpoint is quite rare (prevalence of 9%). The following covariates were used in the multivariable adjustment: age, gender, body mass index, HDL, LDL, lipid lowering medications, smoking status, family history of heart attack, hypertension, and diabetes mellitus.
Among those with detectable MAC, the relationship between risk factors and the quantity of calcification [(ln)Agatston score] was assessed with multi-variable linear regression. The relationship was expressed as a percent difference in calcification for a given increment in the risk factor. The ‘Relative Difference’ is the anti-log of the regression coefficient using log-transformed calcium score as the dependent variable in each multiple linear regression analysis. Statistical analyses were performed with SPSS 13.0.1 software for Windows (SPSS Inc, Chicago, Ill) and STATA 10.0 for Windows (Stata Corp, College Station, Tx).
Results
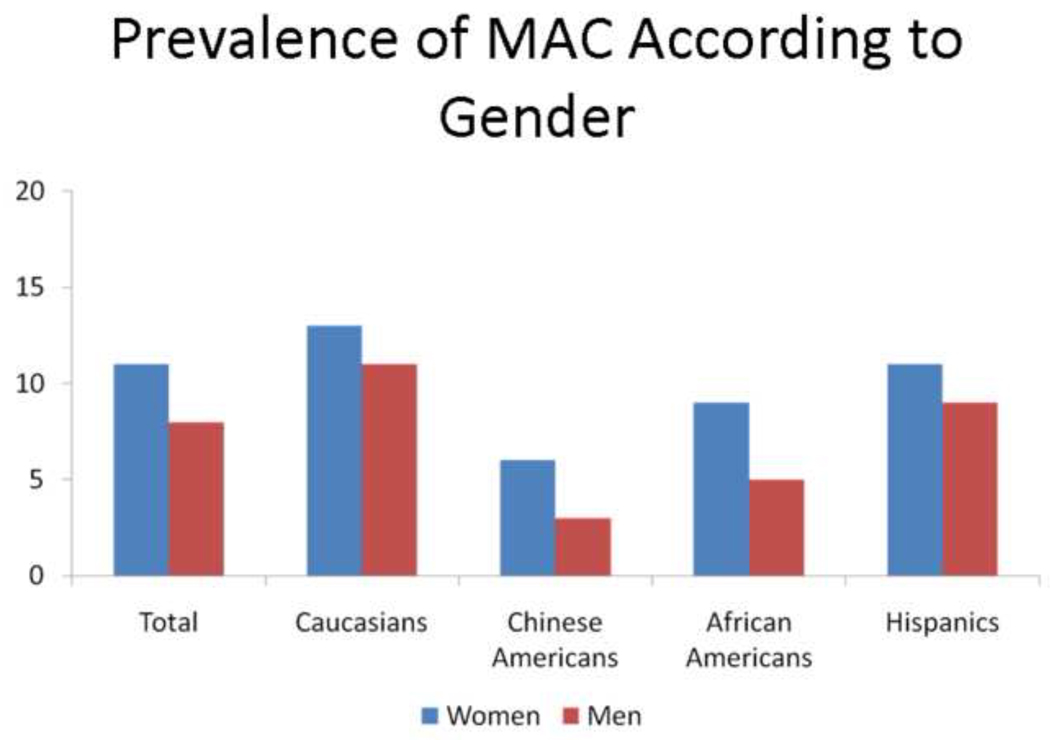
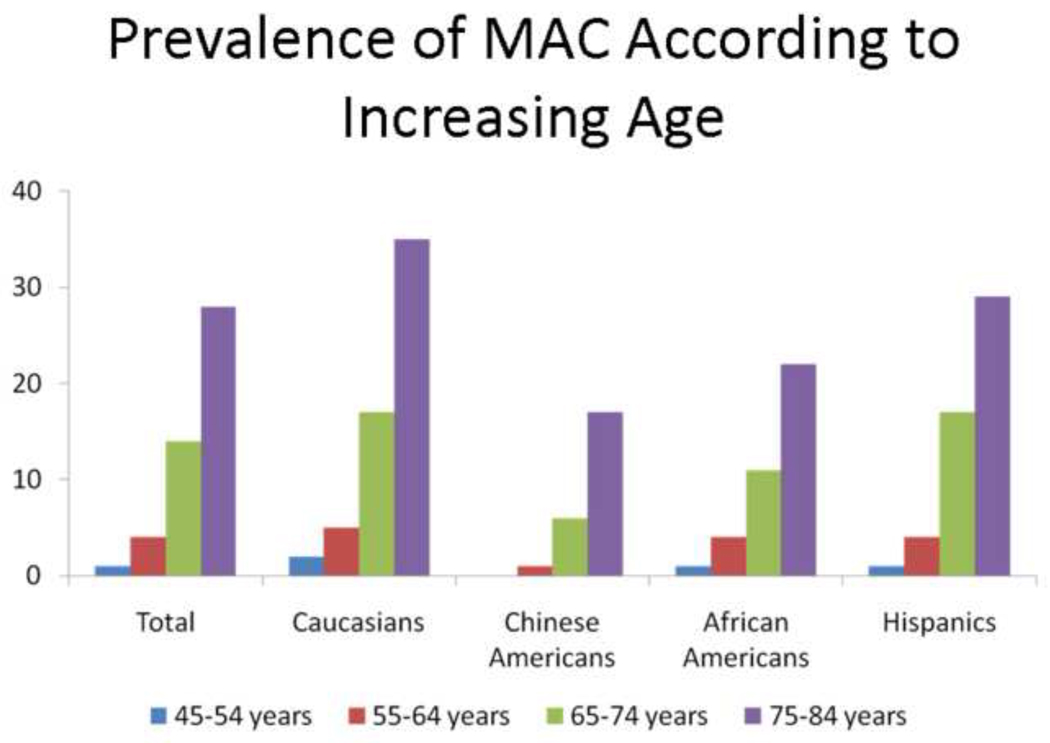
Overall in our study, 644 individuals had MAC (MAC >0) and 6,170 individuals did not have MAC (MAC =0). The overall prevalence of MAC was 9%. The prevalence of MAC was highest in Caucasians (12%), followed by Hispanics (10%), African Americans (7%) and was lowest in Chinese (5%). Table 1 demonstrates the baseline characteristics of the study population according to absence and presence of MAC. Individuals with MAC were more likely to be older and women, as seen in figure 1 and 2. Characteristics associated with MAC included age (p<0.01), female gender (p<0.01), increased BMI (p=0.03), and former smoking status (p<0.08).
Table 1.
Characteristics of MESA absence/presence of MAC
| MAC=0 | MAC>0 | p-value | |
|---|---|---|---|
| N | 6170 (91) | 644 (9) | |
| Age † | 61±10 | 72±9 | <0.001 |
| Men | 2955 (48) | 258 (40) | <0.001 |
| Race | |||
| Caucasian | 2309 (38) | 315 (49) | |
| Chinese | 766 (12) | 37 (6) | <0.001 |
| African American | 1753 (28) | 141 (22) | |
| Hispanic | 1342 (22) | 151 (23) | |
| Smoking | |||
| Former | 2234 (36) | 253 (39) | <0.008 |
| Current | 828 (13) | 59 (9) | |
| BMI† | 28±5 | 29±6 | 0.003 |
| Systolic BP† | 126±21 | 135±23 | <0.001 |
| Hypertension | 2655 (43) | 403 (63) | <0.001 |
| Diabetes Mellitus | 827 (13) | 144 (22) | <0.001 |
| Family history of heart attack | 2438 (40) | 296 (46) | <0.001 |
| Total cholesterol (mg/dl)† | 194±35 | 195±38 | 0.439 |
| LDL (mg/dl)† | 117±31 | 115±33 | 0.09 |
| HDL (mg/dl)† | 51±15 | 52±15 | 0.08 |
| Lipid lowering meds | 479 (8) | 165 (15) | <0.001 |
| CRP | 1.88 [0.83,4.25] | 2.21 [0.94,4.40] | 0.02 |
Numbers of patients are indicated for each group and numbers given in parentheses indicate percentages.
are given in mean±SD.
Figure 1.
Prevalence of MAC according to gender.
Figure 2.
Prevalence of MAC according to increasing age
The MAC group had a higher prevalence of hypertension, diabetes mellitus (DM), and family history of heart attack (all p<0.001) when compared with the absence of MAC group. There were no statistically significant differences in total cholesterol, LDL cholesterol, or HDL cholesterol between those with and without MAC. However, lipid lowering medications were used more in the MAC group. In addition, CRP level was significantly higher in the MAC group when compared with the absence of the MAC group (p = 0.02).
Table 2 demonstrates the univariate and multivariable adjusted association of risk factors with presence of MAC. Increasing age (per 10 year) was associated with a 3-fold increase in the odds of presence of MAC in unadjusted as well as multivariate adjusted analyses. Men had 29% lower likelihood for MAC than women. As compared to Caucasians, all ethnic groups had a lower odds ratio for presence of MAC, however a statistical significance was not observed among Hispanics.
Table 2.
Association of Risk Factors with Presence of MAC in unadjusted and multivariate analyses using logistic regression
| Unadjusted | Adjusted† | |
|---|---|---|
| OR (95% CI) | OR (95% CI) | |
| Age (per 10 year) | 3.34 (3.01–3.71) | 3.58 (3.18–4.03)* |
| Men vs. Women | 0.72 (0.62–0.86) | 0.71 (0.57–0.87)* |
| Race | ||
| Caucasian | Ref group | Ref group |
| Chinese | 0.35 (0.24–0.50) | 0.36 (0.24–0.54)* |
| African American | 0.59 (0.47–0.72) | 0.47 (0.37–0.59)* |
| Hispanic | 0.82 (0.67–1.01) | 0.82 (0.65–1.03) |
| Smoking | ||
| Former | 1.07 (0.90–1.27) | 1.01 (0.83–1.23) |
| Current | 0.67 (0.50–0.89) | 1.45 (1.05–1.99)* |
| BMI (per SD increase) | 1.13 (1.04–1.21) | 1.32 (1.19–1.47)* |
| Hypertension | 2.21 (1.87–2.62) | 1.14 (0.94–1.39) |
| Diabetes Mellitus | 1.86 (1.52–2.27) | 1.58 (1.25–1.99)* |
| Family history of heart attack | 1.30 (1.10–1.53) | 1.09 (0.91–1.31) |
| LDL (mg/dl) per SD increase | 0.93 (0.85–1.01) | 1.01 (0.92–1.310 |
| HDL (mg/dl) per SD increase | 1.07 (0.99–1.16) | 1.02 (0.92–1.13) |
| Lipid lowering meds | 1.93 (1.59–2.33) | 1.32 (1.06–1.64)* |
| CRP (log transformation) per unit | 1.08 (1.00–1.16) | 0.96 (0.88–1.05) |
All variables adjusted simultaneously
Indicates statistically significance
Among the traditional risk factors, current smoking, increased BMI, and DM remained significantly associated with presence of MAC in multivariable adjusted analyses (all p<0.05). In multivariable adjusted analyses, the association of hypertension and family history of premature heart attack were no longer statistically significant. Additionally, LDL, HDL, and CRP were also not significantly associated with presence of MAC after taking into account other risk factors.
Table 3 represents the relative change in calcium between various risk factors and MAC severity among those prevalent MAC>0. In our study, aging (per 10 years) represented a 65% increase in a unit of log calcium score (RD=1.65, 95% CI 1.34, 2.05), whereas males were significantly less likely to have an increase in MAC scores (table 3). In addition, a higher BMI and hypertension represented increased risk of calcium score among those with MAC>0, whereas no significant association was noted with other risk factors
Table 3.
Unadjusted and Multivariable estimates of relative difference in calcification associated with each unit difference in risk factors among people with detectable calcium (i.e. MAC > 0).
| Unadjusted | Adjusted* | |
|---|---|---|
| Exp(β) (95% CI) | Exp(β) (95% CI) | |
| N=644 | ||
| Age (per 10 year) | 1.41 (1.16, 1.72)* | 1.65 (1.34, 2.05)* |
| Men vs. Women | 0.75 (0.55, 1.02) | 0.66 (0.48, 0.93)* |
| Race | ||
| White | Ref group | Ref group |
| Chinese | 0.66 (0.34, 1.27) | 0.69 (0.35, 1.39) |
| Black | 0.92 (0.63, 1.35) | 0.67 (0.45, 1.00) |
| Hispanic | 1.34 (0.92, 1.93) | 1.11 (0.76, 1.62) |
| Smoking | ||
| Former | 0.94 (0.68, 1.30) | 1.03 (0.90, 1.19) |
| Current | 0.87 (0.52, 1.51) | 1.31 (0.76, 2.25) |
| BMI (per SD increase) | 1.28 (1.12, 1.48)* | 1.34 (1.12, 1.58)* |
| Hypertension | 1.88 (1.39, 2.56)* | 1.60 (1.16, 2.20)* |
| Diabetes Mellitus | 1.55 (1.07, 2.20)* | 0.23 (0.15, 0.60) |
| Family history of heart attack | 1.11 (0.82, 1.49) | 1.26 (0.86, 1.82) |
| LDL (mg/dl) per SD increase | 0.99 (0.86, 1.14) | 0.98 (0.85, 1.14) |
| HDL (mg/dl) per SD increase | 0.83 (0.71, 0.96) | 0.84 (0.71, 0.99) |
| Lipid lowering meds | 0.91 (0.65, 1.28) | 0.77 (0.54, 1.11) |
| CRP (log transformation) per unit | 1.03 (0.90, 1.19) | 0.90 (0.78, 1.03) |
For continuous variables, Exp(β) = relative difference in geometric mean MAC score per SD higher level.
For categorical variables, Exp(β) = relative difference in geometric mean MAC score for yes vs no categorical variable.
Indicates statistically significance
Discussion
In this prospective cohort study of 6,814 men and women without apparent CVD, the overall prevalence of MAC was 9%. In prior studies, the prevalence of MAC detected through transthoracic echocardiography has varied greatly ranging from 4.6% up to 36%.9,11,14–16 However, echocardiography is probably not an ideal method for detection of valvular calcification because of its relatively low specificity in distinguishing between calcification and dense collagen. Recent studies have used cardiac CT to determine valvular calcification including MAC.12,13Allison et al15 used cardiac CT and reported a similar MAC prevalence to our study, despite the differences in population size and race/ethnicity.
Racial/Ethnic differences in MAC
Caucasians had the highest prevalence of MAC (12%). Caucasians also had the highest prevalence of coronary artery calcification (CAC) in prior MESA studies17,18 and non-MESA studies.19,20 Conversely, Chinese had the lowest prevalence of MAC (5%) but had the second highest prevalence of CAC in MESA.18 Caucasians had higher MAC prevalence than Hispanics, but both ethnicities did not have statistical difference in association with MAC (Table 2). Chinese and African Americans were less likely to be associated with MAC when compared to Caucasians. Racial differences were not only observed in MAC but also in other valvular calcifications in a prior study.21
Age and Gender difference in MAC
Regarding age, we found that MAC had a higher prevalence in older age groups which has been observed in previous studies.4–6This finding was observed in all races/ethnicities (Figure 2) and can be explained by MAC having an underlying component of chronic degenerative changes associated with age apart from atherosclerosis. Since both processes increase with aging, we observed a higher prevalence of MAC in the elderly.
As far as gender is concerned, female gender was strongly associated with MAC. Previous studies also reported that MAC occurs more often in women.4,10In addition MAC is independently associated with CVD risk factors which were correlated with a higher prevalence of CAC10,21,22 and cardiovascular mortality.2,23,24 The underlying mechanism associated with the gender differences observed in various arterial beds is poorly understood, and further studies are needed to explain this phenomenon.
Other risk factors in MAC
In addition to age and female gender, other risk factors included DM, increased BMI, current smoking status and use of lipid lowering medications were significantly associated with MAC after adjusting for all variables simultaneously. Our study findings are consistent with prior reports that DM and obesity have been shown to be associated with MAC.4–6However conflicting data exists regarding the association with other risk factors.
Prior studies have shown that smoking tobacco was not associated with MAC.2,9,11 However, we showed that current smoking status was significantly associated with MAC after adjusting all risk factors simultaneously. Interestingly, there were no statistically differences in LDL, HDL, and total cholesterol between those with and without MAC. However, the MAC group tended to take lipid lowering medications more than the absence of MAC group did. It is likely that most of patients in MAC group with hyperlipidemia were taking lipid lowering medications which resulted in controlled lipid profiles. Thus, we did not find the difference in levels of LDL, HDL, and total cholesterol between MAC and absence of MAC groups. Conversely, previous studies have observed that hyperlipidemia4–6 and family hypercholesterolemia25 were associated with MAC but did not mention about taking lipid lowering medications.
Conflicting results regarding association of hypertension and MAC exist. Several studies have shown that hypertension was associated with MAC2,4–6,15, but some studies did not reach the same conclusion.9–11 These conflicting findings were not observed in aortic valvular calcification (AVC) and thoracic aortic wall calcification (TAC) which have shown to be significantly associated with hypertension in all races/ethnicities.21
We had hypothesized that the development of AVC and TAC were affected with higher pressure load unlike the development of MAC. Although, the relationship of MAC and hypertension was not statistically significant in our study, the direction of association was still in a positive direction. This may be due to our study population being healthier and having a lower prevalence of hypertension than in previous studies.
Multiple studies documented that atherosclerosis was associated with inflammation.26,27High levels of various inflammatory markers such as CRP28 and interleukin-629 were associated with increased risk of future atherosclerotic disease. Takasu et al, recently described that IL-6 was related to the presence and extent of descending thoracic aortic calcification in MESA.30 In our study, CRP was not significantly elevated in the MAC group after adjusting for all CVD risk factors. This can be explained by the fact that development of MAC, apart from potential underlying atherosclerotic process, is also due to chronic degenerative non-inflammatory process characterized by calcification of the surrounding fibrous support of the mitral valve.
Overall, the present study has shown that MAC was associated with the majority of CVD risk factors. We indirectly conclude that MAC could relate to increase burden of risk factors and we should emphasize the aggressive primary prevention of CVD in those patients who have MAC. Interestingly, MAC was strongly associated with female than male gender. We postulate that MAC could be the important risk factors in addition to conventional risk factors to predict CVD events especially in female gender, but the future studies are needed to confirm this conclusion.
Our study findings need to be interpreted in light of the following limitations. As noted earlier, the MESA sample may not be completely generalizable to the entire population, with MESA participants tending to be healthier overall than the general population.7Also, overall, only 12% of our cohort were Chinese, so these estimates are associated with more variance than those for the other race/ethnicities. Another limitation is we do not have lipid profile before being on lipid lowering agents. It would be interesting to compare those values between MAC and non-MAC group instead of using random lipid profiles (with or without on lipid lowering agents). We may have seen a positive relationship of hyperlipidemia and MAC if we had those values.
In conclusion, our study suggested that risk factors of MAC were largely similar to CVD risk factors in multi-ethnic groups. After adjusting for all variables, age, female gender, DM, and obesity remained strongly associated with MAC. Whether MAC has prognostic implications incremental or independent to CAC is being actively investigated in the Multi-Ethnic Study of Atherosclerosis.
Acknowledgements
This research was supported by R01–HL–071739 and contracts N01–HC–95159 through N01–HC–95165 and N01–HC–95169 from the National Heart, Lung, and Blood Institute, Bethesda, MD. The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesanhlbi.org
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Adler Y, Koren A, Fink N, et al. Association between mitral annulus calcification and carotid atherosclerotic disease. Stroke. 1998;29:1833–1837. doi: 10.1161/01.str.29.9.1833. [DOI] [PubMed] [Google Scholar]
- 2.Fox CS, Vasan RS, Parise H, et al. Mitral annular calcification predicts cardiovascular morbidity and mortality: the Framingham Heart Study. Circulation. 2003;107:1492–1496. doi: 10.1161/01.cir.0000058168.26163.bc. [DOI] [PubMed] [Google Scholar]
- 3.Adler Y, Vaturi M, Fink N, et al. Association between mitral annulus calcification and aortic atheroma: a prospective transesophageal echocardiographic study. Atheroslerosis. 2000;152:451–456. doi: 10.1016/s0021-9150(99)00497-9. [DOI] [PubMed] [Google Scholar]
- 4.Savage DD, Garrison RJ, Castelli WP, et al. Prevalence of submitral (annular) calcium and its correlates in a general population-based sample (the Framingham study) Am J Cardiol. 1983;51:1375–1378. doi: 10.1016/0002-9149(83)90315-6. [DOI] [PubMed] [Google Scholar]
- 5.Nair CK, Sudhakaran C, Aronow WS, et al. Clinical characteristics of patients younger than 60 years with mitral annular calcium: comparison with age- and sexmatched control subjects. Am J Cardiol. 1984;54:1286–1287. doi: 10.1016/s0002-9149(84)80082-x. [DOI] [PubMed] [Google Scholar]
- 6.Boon A, Cheriex E, Lodder J, et al. Cardiac valve calcification: characteristics of patients with calcification of the mitral annulus or aortic valve. Heart. 1997;78:472–474. doi: 10.1136/hrt.78.5.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bild DE, Bluemke DA, Burke GL, et al. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 8.Carr JJ, Nelson JC, Wong ND, et al. Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of multi-ethnic study of atherosclerosis (MESA) and coronary artery risk development in young adults (CARDIA) study. Radiology. 2005;234:35–43. doi: 10.1148/radiol.2341040439. [DOI] [PubMed] [Google Scholar]
- 9.Fox E, Harkins D, Taylor H, et al. Epidemiology of mitral annular calcification and its predictive value for coronary events in African Americans: The Jackson Cohort of the Atherosclerotic Risk in Communities Study. Am Heart J. 2004;148:979–984. doi: 10.1016/j.ahj.2004.05.048. [DOI] [PubMed] [Google Scholar]
- 10.Adler Y, Herz I, Vaturi M, et al. Mitral annular calcium detected by transthoracic echocardiography is a marker for high prevalence and severity of coronary artery disease in patients undergoing coronary angiography. Am J Cardiol. 1998;82:1183–1186. doi: 10.1016/s0002-9149(98)00596-7. [DOI] [PubMed] [Google Scholar]
- 11.Atar S, Jeon DS, Luo H, et al. Mitral annular calcification: a marker of severe coronary artery disease in patients under 65 years old. Heart. 2003;89:161–164. doi: 10.1136/heart.89.2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adler Y, Fisman EZ, Shemesh J, et al. Usefulness of helical computed tomography in detection of mitral annular calcification as a marker of coronary artery disease. Int J Cardiol. 2005;101:371–376. doi: 10.1016/j.ijcard.2004.03.044. [DOI] [PubMed] [Google Scholar]
- 13.Budoff MJ, Katz R, Wong ND, et al. Effect of scanner type on the reproducibility of extracoronary measures of calcification: the multi-ethnic study of atherosclerosis. Acad Radiol. 2007;14:1043–1049. doi: 10.1016/j.acra.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 14.Benjamin EJ, Plehn JF, D'Agostino RB, et al. Mitral annular calcification and the risk of stroke in an elderly cohort. N Engl J Med. 1992;327:374–379. doi: 10.1056/NEJM199208063270602. [DOI] [PubMed] [Google Scholar]
- 15.Allison MA, Cheung P, Criqui MH, et al. Mitral and aortic annular calcification are highly associated with systemic calcified atherosclerosis. Circulation. 2006;113:861–866. doi: 10.1161/CIRCULATIONAHA.105.552844. [DOI] [PubMed] [Google Scholar]
- 16.Maher ER, Yong G, Smyth-Walsh B, et al. Aortic and mitral valve calcification in patients with end-stage renal disease. Lancet. 1987;2:875–877. doi: 10.1016/s0140-6736(87)91370-5. [DOI] [PubMed] [Google Scholar]
- 17.Takasu J, Budoff MJ, O'Brien KD, et al. Relationship between coronary artery and descending thoracic aortic calcification as detected by computed tomography: The Multi-Ethnic Study of Atherosclerosis. Atherosclerosis. 2009;204:440–446. doi: 10.1016/j.atherosclerosis.2008.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bild DE, Detrano R, Peterson D, et al. Ethnic differences in coronary calcification: The Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2005;111:1313–1320. doi: 10.1161/01.CIR.0000157730.94423.4B. [DOI] [PubMed] [Google Scholar]
- 19.Budoff MJ, Nasir K, Mao S, et al. Ethnic differences of the presence and severity of coronary atherosclerosis. Atherosclerosis. 2006;187:343–350. doi: 10.1016/j.atherosclerosis.2005.09.013. [DOI] [PubMed] [Google Scholar]
- 20.Budoff MJ, Yang TP, Shavelle RM, et al. Ethnic differences in coronary atherosclerosis. J Am Coll Cardiol. 2002;39:408–412. doi: 10.1016/s0735-1097(01)01748-x. [DOI] [PubMed] [Google Scholar]
- 21.Nasir K, Katz R, Takasu J, et al. Ethnic differences between extra-cornary measures on cardiac computed tomography: Multi-ethnic study of atherosclerosis (MESA) Atherosclerosis. 2008;198:104–114. doi: 10.1016/j.atherosclerosis.2007.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tenenbaum A, Shemesh J, Fisman EZ, et al. Advanced mitral annular calcification is associated with severe coronary calcification on fast dual spiral computed tomography. Invest Radiol. 2000;35:193–198. doi: 10.1097/00004424-200003000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Kamensky G, Lisy L, Polak E, et al. Mitral annular calcification and aortic plaques as predictors of increased cardiovascular mortality. J Cardiol. 2001;37 Suppl 1:21–26. [PubMed] [Google Scholar]
- 24.Willens HJ, Chirinos JA, Schob A, et al. The relation between mitral annular calcification and mortality in patients undergoing diagnostic coronary angiography. Echocardiography. 2006;23:717–722. doi: 10.1111/j.1540-8175.2006.00300.x. [DOI] [PubMed] [Google Scholar]
- 25.Sprecher DL, Schaefer EJ, Kent KM, et al. Cardiovascular features of homogous familial hypercholesterolemia: analysis of 16 patients. Am J Cardiol. 1984;54:20–30. doi: 10.1016/0002-9149(84)90298-4. [DOI] [PubMed] [Google Scholar]
- 26.Ross R. Atherosclerosis – an inflammatory disease. N Engl J Med. 1999;340:115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 27.Pearson TA, Mensah GA, Alexander RW, et al. Centers for Disease Control and Prevention; American Heart Association. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003;107:499–511. doi: 10.1161/01.cir.0000052939.59093.45. [DOI] [PubMed] [Google Scholar]
- 28.Ridker PM, Hennekens CH, Buring JE, et al. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med. 2000;342:836–843. doi: 10.1056/NEJM200003233421202. [DOI] [PubMed] [Google Scholar]
- 29.Ridker PM, Rifai N, Stampfer MJ, et al. Plasma concentration of interleukin-6 and the risk of future myocardial infarction among apparently healthy men. Circulation. 2000;101:1767–1772. doi: 10.1161/01.cir.101.15.1767. [DOI] [PubMed] [Google Scholar]
- 30.Takasu J, Katz R, Shavelle DM, et al. Inflammation and descending thoracic aortic calcification as detected by computed tomography: The Multi-Ethnic Study of Atherosclerosis. Atherosclerosis. 2008;199:201–206. doi: 10.1016/j.atherosclerosis.2007.11.005. [DOI] [PubMed] [Google Scholar]