Abstract
Background
Despite the high prevalence of pacemakers and implantable cardioverter-defibrillators, little is known about physician views surrounding the ethical and legal aspects of managing these devices at the end-of-life.
Objective
To identify physician experiences and views surrounding the ethical and legal aspects of managing cardiac devices at the end-of-life.
Methods
Survey questions were administered to internal medicine physicians and subspecialists at a tertiary care center. Physicians were surveyed about their clinical experience, legal knowledge, and ethical beliefs relating to the withdrawal of PM and ICD therapy in comparison to other life-sustaining therapies.
Results
Responses were obtained from 185 physicians. Compared to PMs and ICDs, physicians more often reported having participated in the withdrawal or removal of mechanical ventilation (86.1% vs. 33.9%, P<0.0001), dialysis (60.6% vs. 33.9%, P<0.001), and feeding tubes (73.8% vs. 33.9%, P<0.0001). Physicians were consistently less comfortable discussing cessation of PMs and ICDs compared to other life-sustaining therapies (P<0.005). Only 65% of physicians correctly identified the legal status of euthanasia in the US, and 20% accurately reported the legal status of physician-assisted suicide in the US. Compared to deactivation of an ICD, physicians more often characterized deactivation of a PM in a pacemaker-dependent patient as physician-assisted suicide (19% vs. 10%, P=0.027) or euthanasia (9% vs. 1%, P<0.001).
Conclusions
In this single-center study, internists were less comfortable discussing cessation of PM and ICD therapy compared to other life-sustaining therapies and lacked experience with this practice. Education regarding the legal and ethical parameters of device deactivation is needed.
Keywords: Pacemakers, implantable-cardioverter defibrillators, ethics, end-of-life care
Introduction
Navigating end-of-life care for patients who require life-sustaining devices can be clinically and ethically challenging.(1) Physicians have reported a lack of confidence in approaching end-of-life care decisions involving therapies such as dialysis and mechanical ventilation.(2–6) Patients have reported an interest in participating in these decisions, though comfort and understanding varies considerably according to the setting and complexity of the intervention.(7–9) Withdrawal of life-sustaining therapies has even led to significant public controversy and debate in cases such as the legal battle to remove Terri Schiavo's feeding tube.(10–11)
Permanent heart rhythm devices such as pacemakers (PM) and implantable cardioverterdefibrillators (ICD) prolong patients' lives across a wide spectrum of cardiovascular diseases.(12–14) Currently, over 2 million patients have these devices,(15) a number that will continue to grow due to an aging US population and expanding clinical indications.(16–17) Despite the effectiveness of heart rhythm devices, clinical studies demonstrate 5–20% annual mortality rates for recipients, meaning that tens of thousands of deaths occur annually among these patients.(12–14, 18) Therefore, physicians caring for this broadening population of device recipients will inevitably be confronted with the possibility of device deactivation.
Little research is available to guide physician decision-making with these devices at the patients' end-of-life despite the challenges involved in management.(1, 19–24) Immediate death or acute cardiovascular symptoms may follow deactivation of devices treating heart rhythm abnormalities or heart failure; these outcomes may be unpredictable and beyond the experience of some physicians.(21) Many physicians are uncertain about the experience of clinical arrhythmias or ICD shocks, making communication with patients more difficult.(23–26) A study of heart rhythm specialists with substantial personal experience deactivating devices suggested that, despite frequently performing deactivations, many remained uncomfortable with the practice and favored involvement of psychiatric and/or ethics consultation.(22) The specific reasons for these views, however, are not clear.
Similarly, though studies have suggested that many physicians view PM and ICD deactivation differently than other life-sustaining therapies, the underlying basis for those views remains poorly understood.(20, 22–24, 27) Physicians may have legal, ethical, or other objections to PM and ICD deactivation. Reluctance to withdraw these therapies may be related to attitudes and knowledge surrounding end-of-life care generally. In particular, the views of physicians apart from arrhythmia specialists, have not been adequately explored, despite their frequent responsibilities managing these patients at the end-of-life.(16)
To shed more light on this complex and increasingly common area of health care delivery, we surveyed internal medicine physicians and subspecialists about their specific ethical beliefs and legal knowledge relating to the withdrawal of PM and ICD therapy in end-of-life patients. We then compared these results to their views on withdrawing other life-sustaining therapies.
Methods
Study Population and Recruitment
All internal medicine physicians and internal medicine subspecialists at Beth Israel Deaconess Medical Center, an academic tertiary care center in Boston, Massachusetts, were eligible for study participation. These 746 physicians included 471 clinical attendings, 158 residents, and 117 subspecialty fellows. Physicians were recruited to participate by email through an anonymous link (no honorarium offered). Research was conducted with approval of the Beth Israel Deaconess Medical Center Institutional Review Board.
Survey Instrument
Survey questions were developed with input from collaborators with ethics and legal expertise, Questions and definitions were pilot tested in a convenience sample of potential respondents for comprehension prior to administration to the study population.
The survey was divided into five parts. First, we obtained basic physician demographic information, including specialty training and practice level. Next, we assessed physicians' subjective comfort with patient discussions about withdrawal of life-sustaining devices. Physicians were asked to rate on a five-point Likert scale their comfort in discussing withdrawal of five different devices in their patients (mechanical ventilation, feeding tubes, dialysis, PM, and ICD). Third, we asked physicians to report whether they had previous objective experience with withdrawing life-sustaining therapy from each of the five devices. In the case of PM or ICD deactivation, we also asked physicians to report whether they had sought official hospital legal or ethical consultations.
The fourth section of the survey assessed physicians' legal knowledge and ethical views regarding aspects of withdrawal of care at the end of life. Physicians were provided with a set of standard definitions (see FIGURE 1)(28) and queried about the legal status of euthanasia or physician-assisted suicide. We also asked physicians whether they were concerned about malpractice liability for decisions made about deactivating life-sustaining cardiac devices.
Figure 1. Definitions provided to study participants.
Physicians were asked whether or not they believed deactivation of a PM or and ICD was morally equivalent to turning off or stopping chest compressions, mechanical ventilation, dialysis, or feeding tubes. Physicians were then asked to provide their ethical perspectives on whether the deactivation of an ICD or a PM in a pacemaker-dependent patient should be considered euthanasia, physician-assisted suicide, or palliative care. To further characterize areas of ethical concern surrounding cardiac device deactivation, we asked physicians to rate their level of concern regarding specific aspects of the informed consent process for withdrawal of a life-sustaining cardiac device and situations involving disagreements regarding the appropriateness of withdrawal among caregivers for an end-of-life patient. On a 0 – 10 scale, a score of 0 was defined as “no concerns” and a score of 10 was defined as “very concerned”. Scores ≥8 were pre-specified by the investigators to indicate a substantial expression of ethical concern.
The final section of the survey involved assessing physicians' reactions to a series of clinical scenarios. We presented two descriptions of patients at end-of-life with different life-sustaining devices or therapies: an inpatient with life-threatening sepsis and an outpatient with terminal cancer. Physicians were asked their comfort withdrawing ventilator, dialysis, feeding tube, pressors, CPR, and antibiotics, as well as cardiac devices (PM or ICD). Subsequent scenarios involving cardiac devices presented the patients as pacemaker-dependent or non-pacemaker-dependent, and as having previously received or not received ICD treatment for life-threatening arrhythmias. Physicians rated their comfort on a 10-point Likert scale, with scores ≥8 pre-specified as indicative of strong comfort.
Data Analysis
Statistical calculations were performed using SAS statistical software (Version 9.1, SAS Institute, Cary, NC, USA). Student t-tests and chi-square tests were used to compare continuous and discrete outcomes, respectively. A P value of <0.05 was considered to be statistically significant.
Results
We received responses from 185 (25%) physicians (see TABLE 1). Among the 153 responders who provided professional training data, nearly all were trained as internists (150, 98%) and most practiced at the level of clinical attending (119, 69%). Among the physicians reporting additional subspecialty training, the most common fields were cardiology (13, 8.5%), pulmonary critical care (13, 8.5%), and geriatrics (8, 5.2%).
Table 1.
Subject Characteristics
| Demographics | Total N = 185* |
|---|---|
| Male, N (%) | 101 (54.9) |
| White, N (%) | 140 (76.5) |
| Age <35, N (%) | 72 (39.1) |
| Age >65, N (%) | 17 (9.2) |
| Professional Experience | |
| Clinical Attending, N (%) | 119 (69.2) |
| Fellows, N (%) | 25 (14.5) |
| Residents, N (%) | 28 (16.3) |
| Specialty Training | |
| Internists, N (%) | 150 (98.0) |
| Subspecialists, N (%) | 36 (23.5) |
| Cardiologists, N (%) | 13 (8.5) |
| Pulmonary/Critical Care, N (%) | 13 (8.5) |
| Geriatrics, N (%) | 8 (5.2) |
Percentages refer to proportion of physicians who responded to each question.
Comfort and Clinical Experience with Withdrawing Life-Sustaining Devices
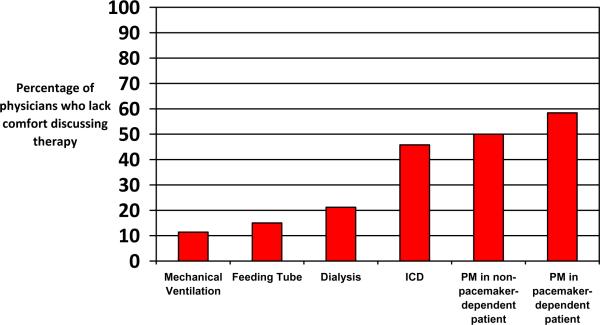
Though the vast majority of physicians (149 of 167, 89%) conveyed comfort discussing end-of-life care in general with their patients, physicians reported being significantly less comfortable discussing deactivation of PMs or ICDs as compared to three more familiar clinical scenarios (ventilation, feeding tube, dialysis; P<0.005 for all comparisons, see FIGURE 2). Physicians were least comfortable participating in a decision to deactivate a PM in a pacemaker-dependent patient who was critically or terminally ill; this task was the most problematic for physicians with less clinical experience (P<0.005 for comparison of trainees vs. clinical attendings). Compared to PMs and ICDs, physicians in our sample more often reported having participated in the withdrawal or removal of mechanical ventilation (86.1% vs. 33.9%, P<0.0001), dialysis (60.6% vs. 33.9%, P<0.001), and feeding tubes (73.8% vs. 33.9%, P<0.0001). Few had personally deactivated either type of cardiac device in end-of-life patients (10% PMs; 11% ICDs).
FIGURE 2. PHYSICIANS' LACK OF COMFORT DISCUSSING WITHDRAWAL OF SPECIFIC LIFE-SUSTAINING THERAPIES*.
*P<0.005 for comparison of mechanical ventilation, feeding tubes, and dialysis vs. each of three cardiac device options.
Despite widespread discomfort, few physicians (<2% for both PMs and ICDs) had requested legal consultation to guide patient management decisions and fewer than 1% had requested ethics consultation.
Legal Knowledge
Physicians displayed a greater understanding of local legal issues related to end-of-life care than of national policy. Physicians correctly identified that euthanasia and physician-assisted suicide are not legal in Massachusetts (98% for both). However, only 65% of physicians (106 of 163) were able to correctly identify that euthanasia is illegal everywhere in the US. Similarly, only 20% (33 of 164) could identify that physician-assisted suicide is legal in more than one US state.
Deficiencies in physicians' legal knowledge were more pronounced for questions related to cardiac devices. Fifty-one of 163 (31%) correctly responded that the presence of an underlying rhythm (i.e., pacemaker dependence) does not influence the legal status of PM deactivation. In addition, 59 of 163 (36%) and 89 of 161 (55%) correctly indicated that presence of a terminal illness does not influence the legal status of PM or ICD deactivation, respectively. On the other hand, 42 of 161 physicians (26%) thought the presence of an underlying rhythm should influence legality of PM deactivation, while slightly fewer thought that presence of a terminal illness should influence the legality of device deactivation (27 of 161, 17%, for PMs and 22 of 161, 14%, for ICDs). A substantial minority of physicians were concerned that PM (30 of 149, 20%) or ICD (29 of 149, 20%) deactivation could expose them to legal liability.
Ethical Views
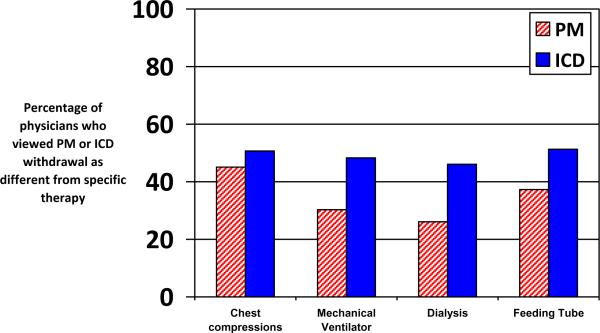
Respondents viewed deactivation of PMs and ICDs in end-of-life patients differently from withdrawal of other life sustaining devices (see FIGURE 3). For example, 73 of 151 (48%) and 46 of 152 (30%) of physicians felt that ICD and PM deactivation, respectively, were not morally equivalent to cessation of mechanical ventilation. Compared to deactivation of an ICD, physicians more often characterized deactivation of a PM in a pacemaker-dependent patient as physician-assisted suicide (30 of 161, 19% vs. 16 of 160, 10%, P=0.027) or euthanasia (151 of 161, 9% vs. 2 of 160, 1%, P<0.001).
FIGURE 3. PHYSICIANS' VIEWS ON PACEMAKER AND IMPLANTABLE DEFIBRILLATOR DEACTIVATION COMPARED TO WITHDRAWAL OF OTHER THERAPIES.
The percentage of physicians who viewed withdrawal of PM (RED-HATCHED bars) or ICD (BLUE-SOLID bars) therapy to be morally different compared to withdrawal of each therapy additional therapy are shown.
*P<0.001 for ICD vs. PM for mechanical ventilation, dialysis
P=0.016 for ICD vs. PM for feeding tube
P=NS for ICD vs. PM for chest compressions
Physicians pointed to potentially problematic ethical issues in their experiences with cardiac device deactivation. A substantial minority of physicians did not believe that the informed consent process prior to implantation adequately addressed the possibility of device deactivation (31 of 146, 21%) for PM and 27 of 145, 19% for ICDs). Physicians frequently viewed discord among patients' family members (102 of 145, 70%) or the patient care team (83 of 144, 58%) as points of concern in the management of cardiac devices at end-of-life. Nearly half (68 of 148, 46%) strongly agreed that patient care would be improved by national guidelines addressing the appropriate time for cardiac device deactivation in end-of-life patients.
Clinical Vignettes
In the hypothetical scenarios presented, physicians consistently expressed strong comfort with withdrawal of mechanical ventilation (130 of 144, 90%), dialysis (132 of 144, 92%), and feeding tubes (131 of 144, 91%) for a critically-ill patient with a very poor prognosis. Physicians also supported withholding these therapies for a stable outpatient with terminal cancer (mechanical ventilation 141 of 144, 98%; dialysis 141 of 144, 98%; feeding tube 139 of 144, 97%).
Among cardiac devices, for a patient who was pacemaker-dependent, nearly all physicians supported deactivation of a PM in the cases of brain death (141 of 143, 99%) or a coma with very poor prognosis (133 of 142, 94%). For a patient who was not pacemaker-dependent, there was also widespread support for deactivation of a pacemaker (99% for brain death vs. 95% for a coma). In contrast, for stable outpatients with terminal cancer requesting deactivation of their pacemaker, support for withdrawal of PM therapy was not as strong though still indicated by over half of the respondents. Specifically, PM deactivation was supported less often for pacemaker-dependent patients than for non-pacemaker-dependent patients (73 of 141, 52% vs. 126 of 141, 83%, P<0.0001).
In contrast to withdrawal of PM therapy, there was general agreement about withdrawing a secondary-prevention ICD in brain dead patients (140 of 142, 99%), comatose inpatients (135 of 141, 96%), and stable but terminally ill cancer patients who request this course of action (125 of 141, 89%). Responses were similar for a patient with a primary-prevention ICD (139 of 141, 99%; 138 of 141, 98%; and 130 of 140, 93%, respectively).
Discussion
This study expands the understanding of internal medicine physician practices, knowledge, and beliefs regarding PM and ICD deactivation. Though most physicians expressed confidence in discussing end-of-life care generally, some lack experience and comfort in managing cardiac devices specifically at the end-of-life, and have important gaps and inconsistencies in their legal and ethical knowledge pertaining to cessation of PM and ICD therapy. Notably, twenty-five to fifty percent of physicians considered deactivation of PMs and ICDs to be morally distinct from withdrawal of other life-sustaining therapies, and cessation of these devices was less frequently supported in clinical scenarios involving stable ambulatory patients with terminal illnesses.
Recent consensus guidelines have emphasized the importance of thoughtful, multi-disciplinary care of patients with PMs and ICDs, whose care frequently involves multiple specialties apart from cardiac electrophysiologists.(1) There is a broad consensus in the health care field that patients with decision-making capacity have the right to request withdrawal of life-sustaining therapies and that physicians have an obligation to respect those wishes.(1, 29–31) Even if such actions lead to a patient's death, it is considered neither euthanasia nor assisted-suicide to respect a patient's right to refuse treatment or request treatment withdrawal. No medical therapy is mandatory, and there is no meaningful distinction in the law or among ethicists between different life-sustaining therapies such as mechanical ventilation, feeding tubes, dialysis, or cardiac devices.(1, 20, 32)
The results of this study, however, demonstrate that some physicians do draw such boundaries. Physicians described wide experience and comfort with general management of end-of-life care and in withdrawing interventions such as mechanical ventilation and dialysis. Yet physicians had less far less experience participating in decisions to deactivate PMs and ICDs, and many were less comfortable discussing withdrawal of these therapies compared with other life-sustaining treatments.
Many physicians were unaware of different laws that may guide discontinuation of life-sustaining therapies both generally and specifically with regard to PMs and ICDs. Physicians characterized PM and ICD deactivation as physician-assisted suicide substantially more frequently than previously reported.(22) This is particularly important as nearly all physicians correctly identified that physician-assisted suicide is illegal in Massachusetts (the location of the study center), implying that for these caregivers device deactivation would not be viewed as legal in their state, which is not the case. While these differences may reflect the greater expertise with cardiac devices in previous study populations, inevitably, physicians apart from electrophysiologists will encounter these clinical situations, and therefore will need to be familiar with the relevant laws guiding treatment options.
Notably, many physicians were less familiar with the legality of physician-assisted suicide in states other than Massachusetts. Though knowledge of local laws is undoubtedly more important for direct clinical care, the status of physician-assisted suicide nationally has led to broad public debate and legal challenges involving the U.S. Supreme Court. Given the prominence of end-of-life care in national discussions on health care reform, we consider it essential for physicians caring for patients receiving life-sustaining therapies to maintain a working understanding of the national context for these debates.
Importantly, many physicians viewed deactivation of PMs and ICDs as morally distinct from each other as well as from withdrawal of other life sustaining therapies. The specific reasons for these distinctions require further investigation, although our results suggest that variability in legal knowledge may contribute to the difference in perception. Additionally, the actual clinical experience of deactivating different therapies – including PMs and ICDs – varies in ways that may influence perceptions. Even patients who are “dependent” on mechanical ventilation, dialysis, vasopressors or pacemakers may not necessarily die immediately when those therapies are withdrawn, and this unpredictability (perhaps heightened with regard to devices that are less familiar) may contribute to moral unease. Similarly, while mechanical ventilation or the shocks from an ICD are obviously intrusive or painful, the burdens of pacing therapy from a patient's perspective may not be as readily apparent.
Our study has several limitations. Subjects included were drawn from a single tertiary care center, and the response rate for our survey was limited. Despite the anonymous nature of the survey, there is a potential for response bias with physicians reporting themselves as having an elevated sense of comfort with complex ethical situations.
These data suggest that efforts are required to better educate physicians regarding the legal and ethical underpinnings of life-sustaining therapy. Because less-experienced physicians are particularly uncomfortable with device deactivation, initiatives directed at medical students and residents may be particularly important. Adding cessation of PMs and ICDs alongside training on withdrawal of other therapies may provide a foundation for a broader experience with these modalities and allow non-electrophysiologists to engage patients and families in these discussions more effectively. At a minimum, health care facilities need clear policies regarding management of life-sustaining therapies, including cardiac devices, particularly in facilities where immediate electrophysiology consultation may not be available.(16) Additionally, physicians caring for patients with PMs and ICDs should include discussion of these devices in conversations regarding goals of care, code status, and advance care planning.
All physicians should understand that patients with decision-making capacity have the right to refuse interventions, or to ask that therapies be withheld or withdrawn, regardless of the therapy in question or the consequences of stopping treatment.(10, 20) Though some may view PMs or ICDs as unique,(25) there is no identifiable medical, legal, or ethical basis for this distinction.(1, 27) It is understood, however, that some physicians may object to device deactivation or moral or other grounds, even when provided with additional teaching and guidance.(25) While these physicians cannot be forced to perform actions they deem unethical or otherwise unacceptable, they do have an obligation to provide an alternative means for patients to have their wishes respected.(1) This may include transfer of care to another facility or a different provider within the same setting, but in all cases respects the rights of patients as well as providers. Given the multidisciplinary nature of caring for many patients with heart rhythm devices, cardiac electrophysiologists must work with clinicians from other specialties to ensure consistent, coordinated, and compassionate care for these patients.
Conclusion
In this single-center study, internists were less comfortable discussing cessation of PM and ICD therapy compared to other life-sustaining therapies and lacked experience with this practice. Efforts to better educate health care providers about the methods, clinical implications, ethics, and legality of device deactivation should be undertaken.
Supplementary Material
Acknowledgments
Funding: This research was conducted with the support of a pilot grant from Harvard Catalyst | The Harvard Clinical and Translational Science Center (NIH Grant #1 UL1 RR 025758-02 and financial contributions from participating institutions). Dr. Kesselheim is supported by a career development award from the Agency for Healthcare Research & Quality (K08HS18465-01).
Abbreviations
- PM
pacemaker
- ICD
implantable cardioverter-defibrillator
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts: There are no potential conflicts of interest to disclose for any of the authors.
References
- 1.Lampert R, Hayes DL, Annas GJ, et al. HRS Expert Consensus Statement on the Management of Cardiovascular Implantable Electronic Devices (CIEDs) in patients nearing end of life or requesting withdrawal of therapy This document was developed in collaboration with the American College of Cardiology (ACC), the American Geriatrics Society (AGS), the American Academy of Hospice and Palliative Medicine (AAHPM); the American Heart Association (AHA), and the European Heart Rhythm Association (EHRA) Heart Rhythm. 2010 May 13; doi: 10.1016/j.hrthm.2010.04.033. [DOI] [PubMed] [Google Scholar]
- 2.Sulmasy DP, Sood JR, Ury WA. Physicians' confidence in discussing do not resuscitate orders with patients and surrogates. J Med Ethics. 2008 Feb;34(2):96–101. doi: 10.1136/jme.2006.019323. [DOI] [PubMed] [Google Scholar]
- 3.Perry E, Swartz R, Smith-Wheelock L, Westbrook J, Buck C. Why is it difficult for staff to discuss advance directives with chronic dialysis patients? J Am Soc Nephrol. 1996 Oct;7(10):2160–8. doi: 10.1681/ASN.V7102160. [DOI] [PubMed] [Google Scholar]
- 4.Holley JL, Foulks CJ, Moss AH. Nephrologists' reported attitudes about factors influencing recommendations to initiate or withdraw dialysis. J Am Soc Nephrol. 1991 Jun;1(12):1284–8. doi: 10.1681/ASN.V1121284. [DOI] [PubMed] [Google Scholar]
- 5.Farber NJ, Simpson P, Salam T, et al. Physicians' decisions to withhold and withdraw life-sustaining treatment. Arch Intern Med. 2006 Mar 13;166(5):560–4. doi: 10.1001/archinte.166.5.560. [DOI] [PubMed] [Google Scholar]
- 6.Solomon MZ, O'Donnell L, Jennings B, et al. Decisions near the end of life: professional views on life-sustaining treatments. Am J Public Health. 1993 Jan;83(1):14–23. doi: 10.2105/ajph.83.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heyland DK, Frank C, Groll D, et al. Understanding cardiopulmonary resuscitation decision making: perspectives of seriously ill hospitalized patients and family members. Chest. 2006 Aug;130(2):419–28. doi: 10.1378/chest.130.2.419. [DOI] [PubMed] [Google Scholar]
- 8.Heyland DK, Tranmer J, O'Callaghan CJ, Gafni A. The seriously ill hospitalized patient: preferred role in end-of-life decision making? J Crit Care. 2003 Mar;18(1):3–10. doi: 10.1053/jcrc.2003.YJCRC2. [DOI] [PubMed] [Google Scholar]
- 9.Schulman-Green DJ, Naik AD, Bradley EH, McCorkle R, Bogardus ST. Goal setting as a shared decision making strategy among clinicians and their older patients. Patient Educ Couns. 2006 Oct;63(1–2):145–51. doi: 10.1016/j.pec.2005.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Annas GJ. “Culture of life” politics at the bedside--the case of Terri Schiavo. N Engl J Med. 2005 Apr 21;352(16):1710–5. doi: 10.1056/NEJMlim050643. [DOI] [PubMed] [Google Scholar]
- 11.Quill TE. Terri Schiavo--a tragedy compounded. N Engl J Med. 2005 Apr 21;352(16):1630–3. doi: 10.1056/NEJMp058062. [DOI] [PubMed] [Google Scholar]
- 12.Cleland JG, Daubert JC, Erdmann E, et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005 Apr 14;352(15):1539–49. doi: 10.1056/NEJMoa050496. [DOI] [PubMed] [Google Scholar]
- 13.Bristow MR, Saxon LA, Boehmer J, et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med. 2004 May 20;350(21):2140–50. doi: 10.1056/NEJMoa032423. [DOI] [PubMed] [Google Scholar]
- 14.Moss AJ, Zareba W, Hall WJ, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002 Mar 21;346(12):877–83. doi: 10.1056/NEJMoa013474. [DOI] [PubMed] [Google Scholar]
- 15.Epstein AE, DiMarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices): developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. Circulation. 2008 May 27;117(21):e350–408. doi: 10.1161/CIRCUALTIONAHA.108.189742. [DOI] [PubMed] [Google Scholar]
- 16.Goldstein N, Carlson M, Livote E, Kutner JS. Brief communication: Management of implantable cardioverter-defibrillators in hospice: A nationwide survey. Ann Intern Med. 2010 Mar 2;152(5):296–9. doi: 10.1059/0003-4819-152-5-201003020-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hlatky MA, Sanders GD, Owens DK. Evidence-based medicine and policy: the case of the implantable cardioverter defibrillator. Health Aff (Millwood) 2005 Jan–Feb;24(1):42–51. doi: 10.1377/hlthaff.24.1.42. [DOI] [PubMed] [Google Scholar]
- 18.Lamas GA, Lee KL, Sweeney MO, et al. Ventricular pacing or dual-chamber pacing for sinus-node dysfunction. N Engl J Med. 2002 Jun 13;346(24):1854–62. doi: 10.1056/NEJMoa013040. [DOI] [PubMed] [Google Scholar]
- 19.Berger JT. The ethics of deactivating implanted cardioverter defibrillators. Ann Intern Med. 2005 Apr 19;142(8):631–4. doi: 10.7326/0003-4819-142-8-200504190-00012. [DOI] [PubMed] [Google Scholar]
- 20.Zellner RA, Aulisio MP, Lewis WR. Should implantable cardioverter-defibrillators and permanent pacemakers in patients with terminal illness be deactivated? Deactivating permanent pacemaker in patients with terminalillness. Patient autonomy is paramount. Circ Arrhythm Electrophysiol. 2009 Jun;2(3):340–4. doi: 10.1161/CIRCEP.109.848523. discussion. [DOI] [PubMed] [Google Scholar]
- 21.Goldstein NE, Mehta D, Teitelbaum E, Bradley EH, Morrison RS. “It's like crossing a bridge” complexities preventing physicians from discussing deactivation of implantable defibrillators at the end of life. J Gen Intern Med. 2008 Jan;23(Suppl 1):2–6. doi: 10.1007/s11606-007-0237-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mueller PS, Jenkins SM, Bramstedt KA, Hayes DL. Deactivating implanted cardiac devices in terminally ill patients: practices and attitudes. Pacing Clin Electrophysiol. 2008 May;31(5):560–8. doi: 10.1111/j.1540-8159.2008.01041.x. [DOI] [PubMed] [Google Scholar]
- 23.Kelley AS, Reid MC, Miller DH, Fins JJ, Lachs MS. Implantable cardioverterdefibrillator deactivation at the end of life: a physician survey. Am Heart J. 2009 Apr;157(4):702–8. e1. doi: 10.1016/j.ahj.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 24.Sherazi S, Daubert JP, Block RC, et al. Physicians' preferences and attitudes about endof-life care in patients with an implantable cardioverter-defibrillator. Mayo Clin Proc. 2008 Oct;83(10):1139–41. doi: 10.4065/83.10.1139. [DOI] [PubMed] [Google Scholar]
- 25.Kay GN, Bittner GT. Should implantable cardioverter-defibrillators and permanent pacemakers in patients with terminal illness be deactivated? Deactivating implantable cardioverter-defibrillators and permanent pacemakers in patients with terminal illness. An ethical distinction. Circ Arrhythm Electrophysiol. 2009 Jun;2(3):336–9. doi: 10.1161/CIRCEP.108.821975. discussion 9. [DOI] [PubMed] [Google Scholar]
- 26.Goldstein N, Bradley E, Zeidman J, Mehta D, Morrison RS. Barriers to conversations about deactivation of implantable defibrillators in seriously ill patients: results of a nationwide survey comparing cardiology specialists to primary care physicians. J Am Coll Cardiol. 2009 Jul 21;54(4):371–3. doi: 10.1016/j.jacc.2009.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sulmasy DP. Within you/without you: biotechnology, ontology, and ethics. J Gen Intern Med. 2008 Jan;23(Suppl 1):69–72. doi: 10.1007/s11606-007-0326-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Beauchamp TL, Childress JF. Principles of Biomedical Ethics. 6th Edition ed. NOUP; New York: [Google Scholar]
- 29.Annas GJ. The Rights of Patients: The Authoritative ACLU Guide to the Rights of Patients TEeNYNYUP [Google Scholar]
- 30.Pellegrino ED. Decisions to withdraw life-sustaining treatment: a moral algorithm. JAMA. 2000 Feb 23;283(8):1065–7. doi: 10.1001/jama.283.8.1065. [DOI] [PubMed] [Google Scholar]
- 31.AMA 1996 . AMA Code of Medical Ethics: Policy on End of Life Care: Opinion E-2.20. IAMA; Chicago: 1996. [Google Scholar]
- 32.Wilkoff BL, Auricchio A, Brugada J, et al. HRS/EHRA expert consensus on the monitoring of cardiovascular implantable electronic devices (CIEDs): description of techniques, indications, personnel, frequency and ethical considerations. Heart Rhythm. 2008 Jun;5(6):907–25. doi: 10.1016/j.hrthm.2008.04.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.