Abstract
Purpose
Light-induced damage can be a problem after surgery or sun exposure. Short-duration, intense light causes preferential photoreceptor death in the superior central retina of albino mice and rats and serves as a model of oxidation-induced neurodegeneration. Previous work on retinal ischemia-induced neuronal death suggests the involvement of zinc (Zn2+) toxicity in the death and collapse of many retinal cell layers and demonstrates the protective efficacy of pyruvate. Retinal pigment epithelial (RPE) cells were shown to be sensitive to oxidative stress, and zinc, causing loss of nicotinamide adenine dinucleotide (NAD+) and adenine triphosphate (ATP), which was prevented by pyruvate and nicotinamide. We previously showed similar results in cortical neurons exposed to oxidative stress or Zn2+. In vivo, Zn2+ is normally present in the inner and outer segments (associated with rhodopsin), Bruch’s membrane and sclera (elastin), RPE, and the outer plexiform layer of the eye (synaptic). In this study, we examine the role of Zn2+ in oxidative stress and light-induced damage in vitro and in vivo.
Methods
We modeled retinal toxicity in cell-culture lines derived from retinal tissue: Müller and human retinal pigment epithelial (ARPE-19) cells and a cone photoreceptor-derived line (661W). These cultures were exposed to Zn2+ and OS, and the therapeutic efficacy of pyruvate, nicotinamide, and NAD+ was determined. Sprague Dawley albino rats were exposed to 18 kLux of white fluorescent light for 1–4 h in the presence and absence of pyruvate, nicotinamide, lactate, and cyclic light. The intracellular free zinc concentration ([Zn2+]i) and cell damage were assessed 0.5 and 7 days later, respectively.
Results
We show that Zn2+ and oxidative stress results in increased [Zn2+]i and that Zn2+ therapeutic compounds (pyruvate, nicotinamide, and NAD+) and inhibitors of previously implicated pathways (sirtuin) are efficacious in vitro. Exposure to 18 kLux of cool white fluorescent light for 1 h induced a large increase in Zn2+ staining 4–14 h later, particularly in the superior outer nuclear layer and RPE of dark-maintained Sprague Dawley albino rats; 4 h of light was required to induce similar damage in cyclic light-maintained rats. Photoreceptors and RPE cells died in untreated animals at 3–7 days. However, nicotinamide and pyruvate (intraperitoneal), but not lactate, attenuated this death in treated animals, as measured using optical coherence tomography and confirmed by counting photoreceptor nuclei.
Conclusions
Zn2+ plays a role in this injury, as suggested by the increased Zn2+ staining and the efficacy of Zn2+ therapeutics. These results suggest that cyclic light maintenance, Zn2+ chelation, pyruvate, and nicotinamide promote RPE and photoreceptor survival after injury and could be effective for various forms of retinal neurodegeneration. These results could have immediate clinical applications in surgery- or sun exposure- induced light damage to the retina.
Introduction
There are many reasons to study light-induced damage to the retina: Light damage (LD) can occur under bright surgical lights if the eye patches normally used to block light are improperly placed or forgotten. Light damage also occurs during acute intense sun exposure (such as prolonged exposure over water or snow or improper solar eclipse viewing); chronic sun exposure has also been implicated in cataracts [1-5]. Furthermore, light-induced retinal damage is a physiologically relevant model for oxidation (OS)-induced retinal neurodegeneration [6,7]. Light or oxidation accelerates disease progression in many models of retinal diseases, such as retinitis pigmentosa (RP) mutant mice [8-11], Smith-Lemli- Opitz rats [12,13], and in retinal degenerations [14,15], including Royal College of Surgeons rats [16], age-related macular degeneration (AMD) [17], glaucoma [18], Tubby mice [19], and diabetic retinopathy [20]. This was reviewed in [21]. Thus, therapeutics that are efficacious against oxidation- or light-induced damage should also be effective against these retinal degenerative diseases.
Retinal ischemia-mediated neuronal death is associated with an increase in zinc (Zn2+), and pyruvate or nicotinamide attenuates this death in vitro and in vivo by restoring NAD+ levels [22,23]. Intra-ocular injection of 1–10 nanomoles of the Zn2+ chelators, EDTA-calcium salt (CaEDTA), or N,N,N'N'-tetrakis(-)[2-pyridylmethyl]-ethylenediamine (TPEN) attenuates neuronal death induced by retinal ischemia [24]. Higher levels of these chelators can induce retinal detachment [22]. Either extracellular Zn2+ uptake through voltage gated Ca2+ channels or OS-induced intracellular Zn2+ release from Zn2+ binding proteins or organelles are neurotoxic. Previous chelator, metabolic, and zinc transporter 3 (ZnT3 and slc30a3) knockout studies have demonstrated that synaptically released zinc contributes to neuronal death after global ischemia, hypoglycemia, or seizures [25-27]. Intracellular Zn2+ release contributes to focal ischemia, OS-, or trophic deprivation-induced neuronal death [28,29]. Pyruvate or nicotinamide can attenuate these zinc neurotoxicities in vitro and in vivo in part through restoration of NAD+ levels lost due to Zn2+ exposure; this NAD+ restoration restores glycolytic flux [28,30-33]. We are interested in the role of excess zinc in retinal degeneration as a result of pathologic light exposure and oxidative conditions. In ambient light, Zn2+ is present physiologically in layers of the eye, most notably in the rod inner and outer segments (RIS, ROS) of the outer nuclear layer (ONL), the outer plexiform layer (OPL), and retinal pigment epithelial (RPE) cells. However, in the dark, the RIS and ROS segmental Zn2+ disappears and Zn2+ appears in photoreceptor perikarya of the ONL. Zn2+ serves important functions, such as modulating neurotransmission [34,35], regulating intracellular metabolism, and dark-light adaptation in retina [reviewed in 36]. The “stainable, releasable” Zn2+ has been demonstrated through auto-metallographic staining [36-38] and fluorescent dye staining [22,36,39] and Zn2+ has been shown to be synaptically released in the OPL through photoreceptor activity [39,40].
The pathway we studied was that elevation of intracellular Zn2+ can cause a reduction in NAD+ and ATP levels, causing dysfunction of glycolysis and cellular metabolism [30,32]. In the experiments presented here, we used the light-induced retinal damage model in albino rats. Oxidative stress has been shown to be involved in this model in the initiation of damage after intense light exposure. In addition, endoplasmic reticulum (ER) stress has also been shown to occur after LD and in rhodopsin RP mutants, and degeneration could be attenuated by overexpression of ER chaperone proteins, perhaps reflecting excessive shedding or misfolding of ROS proteins [41,42]. Previous studies have shown that intense light-induced photoreceptor and RPE cell death is greater in the superior central retina compared to the inferior retina, as measured by ONL thickness and counting [43,44]. This damage involves specific prolonged apoptotic rod cell death and rapid necrosis cone cell death; the roles for DNA damage and repair have been established [reviewed in 21,43]. In our study, we investigated whether light- and radical-induced damage of retinal cells or cell lines causes toxic zinc accumulation, and whether pharmacologic Zn2+ therapeutics, which restore NAD+ levels, are effective in vitro and in vivo.
Methods
Cell culture
A Müller cell line and the ARPE-19 cell line were maintained in Dulbecco’s Modified Eagle Medium (DMEM) media containing 10% fetal bovine serum and penicillin/streptomycin. The 661W cone photoreceptor cell line was maintained in the same medium with supplementation of 2-mercaptoethanol, hydrocortisone 21-hemisuccinate, progesterone, and putrescine [45-47]. Some 661W cultures were preloaded and grown with an additional 10 μM Zn2+ for 2 days before toxicities (~13 μM Zn2+ total in plating medium). This Zn2+ concentration does not cause toxicity or affect growth, but does increase basal [Zn2+]i [28]. Cells were grown in 5% CO2 in 95% humidity at 37 °C for 2 days after splitting to achieve 50%–70% confluency at the time of the experiment. Cells were exposed to zinc (10–200 μM), ethacrynic acid (ETH; 15–100 μM), and H2O2 (100–400 μM) for 24 h in minimal essential medium.
Cell viability assay
The cells (50%–70% confluent) were exposed to zinc, ETH, and H2O2 in the presence of 1–10 mM pyruvate, NAD+, or nicotinamide, and 0.03–0.5 μM TPEN or 3–20 μM of the sirtuin pathway inhibitor, sirtinol. Cell viability was determined by measuring lactate dehydrogenase released into the medium after 24 h. For cells that were exposed to NAD+, cell viability was determined by MTT assay or PI staining assay [48]. Twenty-four h after exposure, cells were stained with 0.1% MTT for 30 min at 37 °C, lysed, and absorbance measured at 595 nm, or PI was added (5 μg/ml) for 30 min at 37 °C and fluorescence measured (ex 530/em 645).
Live-cell imaging
FluoZin3 AM (5 μM; Invitrogen/Life Technologies, Carlsbad, CA) was pre- or post-loaded in the cell lines for 30 min at 37 °C, washed, and exposed to toxic Zn2+, ETH, or H2O2 for 1–11 h before photomicrographs of identical duration were taken.
Rat light damage model
Sprague Dawley albino rats (Charles River, Wilmington, MA) weighing 150–175 g were acclimated for 5 days to a cyclic, dim overhead fluorescent light (30 Lux), followed by a 60 h dark adaption. At this point, one group of animals (dark) was maintained totally in the dark for the duration of the experiment, using red light illumination to dilate their eyes (1% tropicamide ophthalmic solution USP), and was returned to their cages after 1–2 h of light exposure. The second group of rats (light) had their eyes dilated in room light after the 60 h dark adaptation, were exposed to 4 h of light damage, and were returned to cyclic light after 24 h recovery in the dark. The animal chamber was rotated during the light exposure to ensure that the animals were awake with their eyes open. Rats were exposed to bright cool white fluorescent light from 8x 20W-circular fluorescent bulbs (18,000 Lux) [43] in the presence or absence of 500 mg/kg intraperitoneal (i.p.) pyruvate or nicotinamide (3×/week). This was followed by recovery in the dark for 24 h (light) or 7 days for the dark maintained animals (dark). After 24 h recovery in the dark, the (light) group was returned to the cyclic, dim overhead fluorescent light environment for 6 days. All studies were conducted within the guidelines (stated above) established by the Institutional Animal Care and Use Committee (Louisiana State University Health Sciences Center, New Orleans), and were in accordance with the PHS Guide for the Care and Use of Laboratory Animals, USDA Regulations, and the AVMA Panel on Euthanasia guidelines.
Optical coherence tomography
Optical coherence tomography (OCT) is an optical signal acquisition and processing method providing extremely high-quality, micrometer-resolution, three-dimensional images from within optical scattering media (Spectralis, Heidelberg Engineering, Heidelberg, Germany). On the 7th day after light damage, rats were anesthetized with ketamine and xylazine and OCT was performed to measure the thickness of the ONL. A real-time eye tracker was used to couple cSLO and SD-OCT scanners to position and stabilize the OCT scan on the retina. Scaling X was 3.24–3.31 µm/pixel; scaling Z was 3.87 µm/pixel. The built-in scale bar was used when performing OCT analysis. The thickness of the ONL was measured from the bottom edge of the outer plexiform layer to the top edge of the RIS.
Retinal histology
After OCT, rats were sacrificed by CO2 asphyxiation. Eyes were fixed in 2% formaldehyde/2% glutaraldehyde and cut in half along a superior-to-inferior meridian through the center of the optic nerve. After a 1 h fixation period in 1% osmium tetroxide and sequential dehydration in ethanol, eyes were embedded in plastic resin (Electron Microscopy Systems, Hatfield, PA). Retinal sections of 1.5 microns were cut, mounted on glass slides, and stained with 0.1% toluidine blue. The number of ONL nuclei was counted on sections from 6 different retinas at increasing distances from the optic nerve on the superior-to-inferior meridian. Pictures were taken in the mid-superior and mid-inferior hemispheres.
Retinal Zn2+ staining
Eyes of Sprague Dawley rats were collected 4 and 14 h after 1 or 4 h of light exposure with or without dark maintenance, respectively. For example, 4 h LD (light) + 4 h refers to an animal that had its eyes dilated in normal light (not red light) before undergoing 4 h of light damage; the animal was then sacrificed 4 h after light damage. Fresh frozen cryostat sections (10 microns) were prepared, dried, and stained with 5 μM ZinPyr-1 (ZP1, TefLabs, Galveston, TX) for 2 min, washed with PBS, and then photomicrographs were taken immediately using the exposure times indicated (ex: 480nm; em: 530nm). Note that to prevent complete saturation of the images, exposure times were varied. There was no autofluorescence at this wavelength either basally or after light damage, and staining was prevented by pretreatment with the zinc specific chelator, TPEN (data not shown).
Reagents
All materials were purchased from Sigma Chemical Co. (St. Louis, MO) unless otherwise stated.
Results
Zinc and oxidative stress induce [Zn2+]i increases in cone photoreceptors, ARPE-19 cells, or Müller cells
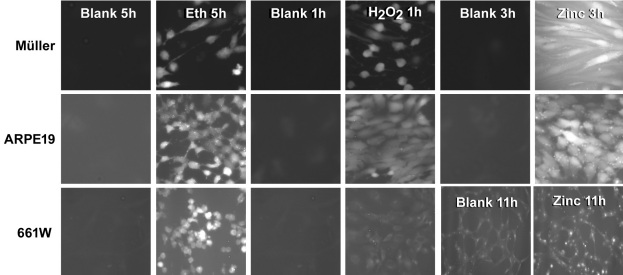
We examined whether zinc (30–200 μM), ETH (10–100 μM), and H2O2 (100–400 μM) induced a [Zn2+]i increase in Müller, ARPE-19, or 661W cone photoreceptors. Cultures were pre- or post-loaded with 5 μM FluoZin3 AM for 30 min and then washed out and exposed to oxidative stress as indicated. We found that after 1–11 h, [Zn2+]i was increased after Zn2+ or oxidative exposure in each of these cell lines (Figure 1). The increase in Fluo-Zin3 staining was specific for Zn2+ as demonstrated using the intracellular zinc chelator, TPEN. The extracellular zinc chelator, CaEDTA, was ineffective except for exogenous Zn2+ exposure, perhaps due to the intracellular release of zinc and the short 1–5 h exposure to CaEDTA (data not shown). Pyruvate, nicotinamide, or NAD+ are not expected to affect [Zn2+]i because they had no effect on [Zn2+]i in cortical neurons, but did restore NAD+, glycolytic flux, and prevented Zn2+ neurotoxicity.
Figure 1.
Zinc (Zn2+), or oxidative stress induces an increase in intracellular free zinc concentration ([Zn2+]i). Cultures of Müller, ARPE-19, and 661W cells were pre- or post-loaded with 5 μM FluoZin3 AM and exposed to 60–300 μM Zn2+, 30–60 μM ethacrynic acid, and 200–400 μM H2O2, as indicated. Representative photomicrographs (n=6) of identical exposure were taken at the times shown.
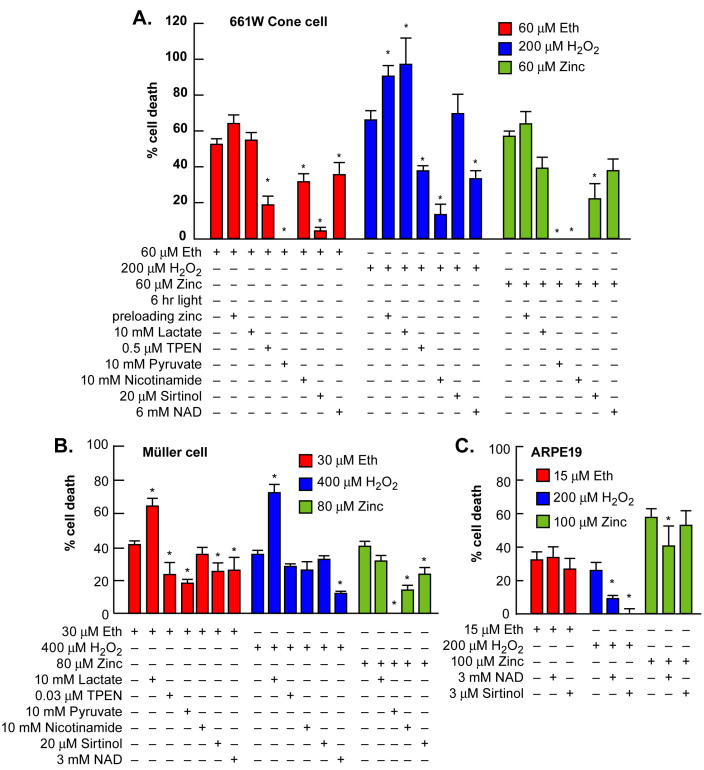
Zinc- and oxidative-stress-induced death of cone photoreceptors or Müller cells was attenuated by Zn2+ therapeutics
TPEN, pyruvate, nicotinamide, NAD+, or sirtinol (Zn2+ therapeutics) can protect cortical neurons from zinc and oxidative toxicities in vitro or in vivo [28,30,32]. Chronic addition of these Zn2+ therapeutic compounds attenuated zinc and oxidative-stress-induced death of Müller or ARPE-19 cells and 661W cone photoreceptors as measured using lactate dehydrogenase release to the media, 5 μg/ml PI staining, or 0.1% MTT staining [49]. Zn2+ preloading potentiated oxidative-stress-induced toxicity in 661W cells. The respective LD50 for zinc, ethacrynic acid, and H2O2 was 60 μM, 60 μM, and 200 μM for 661 W cells; 100 μM, 30 μM, and 600 μM for Müller cells; and 90 μM, 20 μM, and 300 μM for ARPE-19 cells. Chronic additions of 3–10 mM pyruvate or nicotinamide or 3–6 mM NAD+ were consistently efficacious across toxicities. The resultant cell death was variably attenuated by 3–20 μM sirtinol, whereas 10 mM lactate was consistently ineffective or detrimental. Zn2+ pre-loading potentiated, and 0.03–0.5 μM TPEN attenuated these injuries (Figure 2). The effective concentration of TPEN was lower in Müller cells due to their tendency to detach from the plate at higher concentrations of TPEN.
Figure 2.
Zn2+ or oxidative-stress-induced death was attenuated by Zn2+ therapeutics. A: Pyruvate, nicotinamide, NAD+, TPEN, and sirtinol variably attenuated ethacrynic acid, H2O2, or zinc toxicity in the 661 W cone photoreceptor cell line. B: The effect of these exposures on Müller glial cells is presented. C: The effect of these exposures in ARPE-19 cells is presented (n=10–15). * indicates difference from toxic exposure alone at p<0.05 by one-way ANOVA and a Bonferroni test.
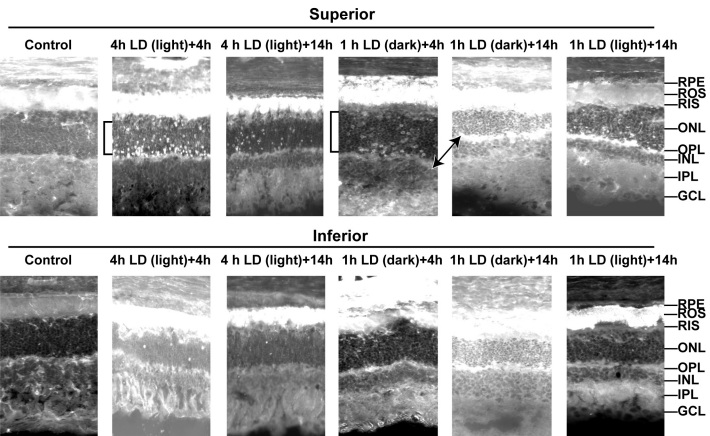
Light damage increases Zn2+ staining in photoreceptors
We performed time courses of zinc accumulation after light-induced damage using a zinc fluorescent dye (5 μM ZP1) on fresh frozen dried rat retinas. Figure 3 shows that zinc accumulated preferentially in the mid-superior RPE and the superior photoreceptors of the ONL at 4–14 h after light damage, which is before the onset of cell death induced by light (48–96 h). The two previously mentioned layers are the most sensitive to LD. Zinc staining started at 2 h, and was maintained at 24 h after LD (data not shown). More zinc-stained photoreceptors were present in the mid-superior than in the mid-inferior retina, correlating with the sensitivity of these regions to LD. The stain was specific for Zn2+ because at 480 nm excitation, there was no autofluorescence and no staining after TPEN pretreatment (data not shown). We also show that Zn2+ staining and accumulation in ROS, RIS, and photoreceptors after only 1 h of LD was much more prevalent when animals were kept dark-adapted and if the eyes were collected and frozen in the dark (note exposure times). This may be due to the depolarization of photoreceptors in the dark, which allows Zn2+ influx through voltage-gated Ca2+ channels [50]. Because Zn2+ staining must be performed on fresh frozen dried tissue sections, the morphologic preservation of the tissue was not perfect. However, the inner and outer segments, ONL, RPE, and plexiform layers were still easily discernible, and the increase in the number of superior photoreceptors and RPE cells that stained for Zn2+ at 4–14 h was greater than the increase in inferior photoreceptors and RPE cells. The entire superior ONL, ROS, RIS, and RPE layers were destroyed after 3–7 days (see below), and these were the layers that preferentially stain with Zn2+ 4–14 h after LD.
Figure 3.
Light-induced damage caused Zn2+ accumulation preferentially in superior photoreceptors, retinal pigment epithelial (RPE), rod outer segments (ROS), and outer plexiform layer (OPL). Light-induced damage (LD) was performed and fresh frozen rat retinas were analyzed at 4 or 14 h after 1 h of light damage in dark maintained conditions (dark) or after 4 h of light damage in non-dark maintained conditions (light). Zn2+ accumulation (white regions) was assessed by ZP1 staining of fresh frozen rat eye cryostat sections cut at 10 microns, which were dried and stained in 5 μM ZP1 for 2 min. Representative photomicrographs (n=4) were taken of the mid inferior and mid superior regions of the retina at 5 s exposure for: control, 4 h LD (light) + 4 h, and 1 h LD (dark) + 4 h; at 1 s exposure for: 1 h LD (dark) + 14 h; and at 2 s exposure for: 4 h LD (light) + 14 h, and 1 h LD (light) + 14 h. Layers are as marked. Notice the large increase in the number and intensity of Zn2+ stained cells in superior ONL (brackets), ROS, and RPE. Light=non-dark maintained, Dark=dark maintained.
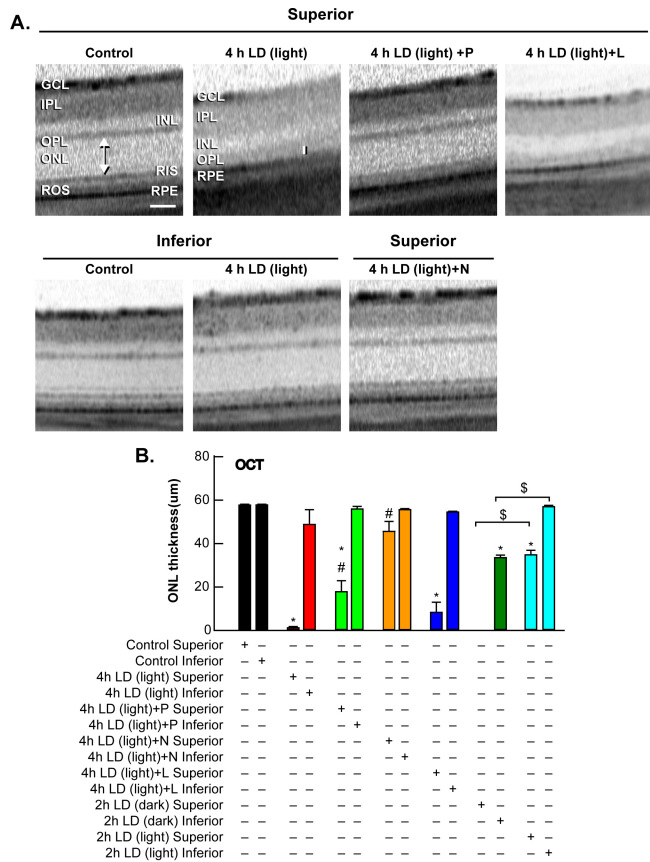
Light damage induced death of photoreceptors in vivo
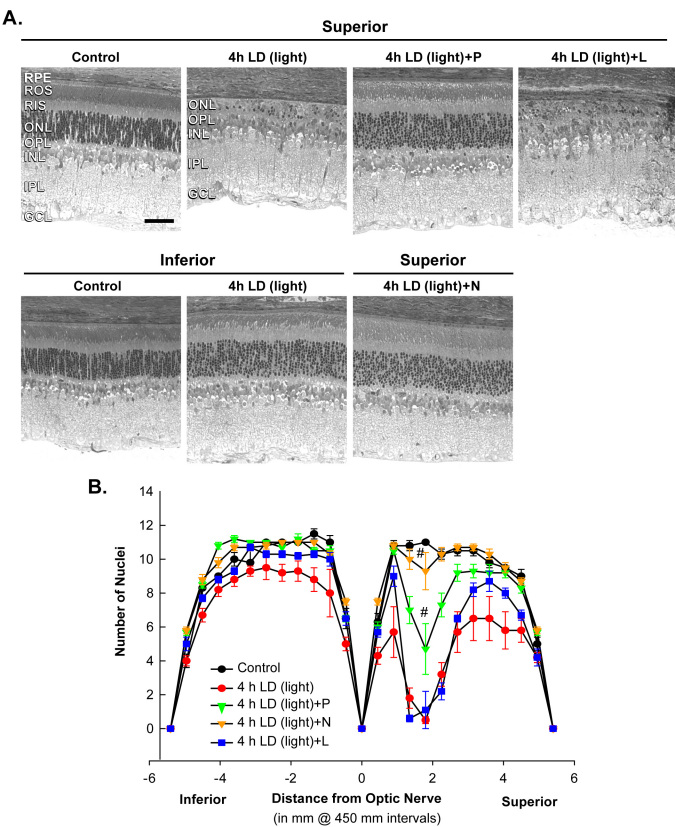
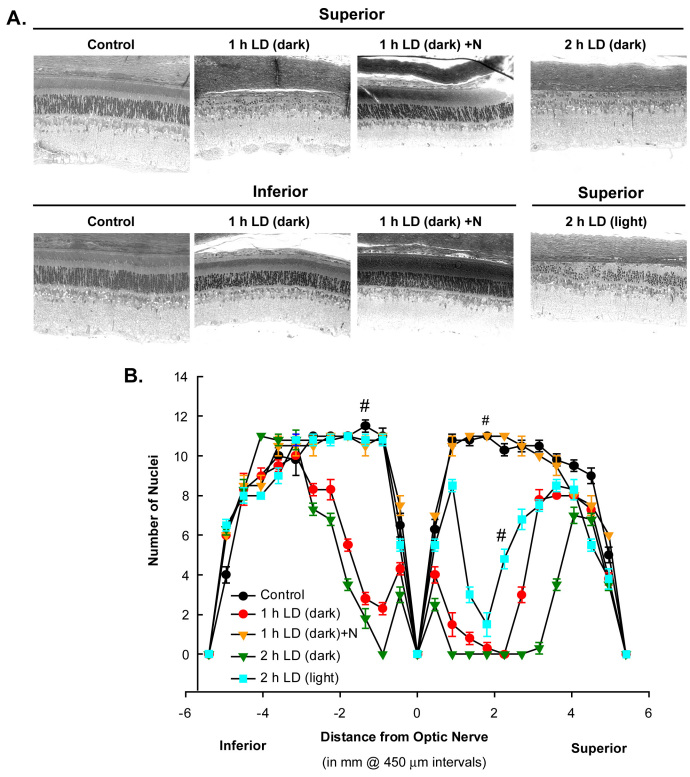
Treatment with pyruvate or nicotinamide (i.p.) attenuated damage to the superior retina, as shown 7 days post-LD by optical coherence tomography (Figure 4), and by ONL cell counting of plastic sections (Figure 5 and Figure 6). Rats exposed to 4 h of 18 kLux white fluorescent light followed by cyclic light displayed complete loss of the superior central ONL, including the RIS, ROS, and the RPE, and ~10% photoreceptor death in the inferior central ONL, as previously reported [43,44,51]. Pre-treatment with i.p. pyruvate, but not lactate, afforded substantial protection of the photoreceptors and RPE cells against light damage, and partial protection of RIS and ROS (Figure 4 and Figure 5); nicotinamide provided complete protection to photoreceptors, RIS, ROS, and RPE cells (Figure 4, Figure 5, and Figure 6). Quantitations of ONL thickness, measured as the distance between the RIS and the OPL (arrow or bar), were made by OCT, and are plotted in Figure 4B. Figure 5B presents the number of photoreceptor nuclei at increasing distances superior or inferior to the optic nerve.
Figure 4.
Optical coherence tomography (OCT) scans demonstrate protection of ONL by pyruvate and nicotinamide against LD. A: Representative ONL images were taken from OCT in control, 7 days after 4 h light damage in non-dark conditions (4 h LD (light)), 4 h LD (light) + P, 4 h LD (light) + N, and 4 h LD (light) + L, where P, N, and L refer to 500 mg/kg i.p. injection before LD and 3x/week of pyruvate, nicotinamide, or lactate, respectively. Bar represents 50 microns. B: The mean thickness in central superior and central inferior hemispheres (arrow or bar in A) of the retina in microns after these exposures is presented ± SEM (n=6). * indicates difference from control, # indicates difference from light damage, and $ indicates difference between dark maintained and non-dark maintained retinas at p<0.05 by one-way ANOVA and a Bonferroni test.
Figure 5.
Plastic sections confirm protection of ONL by pyruvate and nicotinamide against LD. A: Plastic sections were cut from eyes along a superior to inferior meridian encompassing the optic nerve and stained with 0.1% Toluidine Blue. Representative photo-micrographs were taken of the mid superior and mid inferior regions from each of the groups as designated in Figure 4. Bar represents 50 microns. B: The mean number of nuclei at increasing distance from the optic nerve on the superior and inferior sides was averaged and plotted as a function of distance from the optic nerve for each of the experimental conditions above (n=6). # signifies difference from LD at p<0.05 by one-way ANOVA and a Bonferroni test.
Figure 6.
Plastic sections confirm potentiation of ONL loss by dark maintenance and protection by nicotinamide against LD. A: Plastic sections were cut from eyes along a superior to inferior meridian encompassing the optic nerve, and were stained with 0.1% Toluidine Blue. Representative photo-micrographs were taken of the mid superior and mid inferior regions from Control group; 1 h light-induced damage dark-maintained (1 h LD (dark)) group; LD + i.p. injection of nicotinamide (1h LD (dark) + N); and 2 h of LD dark maintained (2 h LD (dark)) versus non dark maintained (2 h LD (light)) as marked. B: The mean number of nuclei at increasing distance from the optic nerve on the superior and inferior sides was averaged and plotted as a function of distance from the optic nerve for each of the experimental conditions above (n=6). # signifies difference from LD at p<0.05 by one-way ANOVA and a Bonferroni test.
Data analysis and statistics
The changes in retinal cell death were determined in cultures under the conditions stated. Means±SEM are plotted and the number is given for each experiment in the figure legends. Results were compared to sham wash or saline injection controls and toxin or injury exposure alone. A one-way ANOVA was used to assess variance in each set of experiments, followed by a Bonferroni test. Significance was achieved by a p value of less than 0.05.
Discussion
In these experiments, we show that: 1) Intense light can induce zinc accumulation in the retina, particularly in the RPE, ROS, RIS, sclera, OPL, and photoreceptors. The early, preferential accumulation of zinc in the superior photoreceptors after light-induced damage (before ONL cell death) suggests that zinc may play a role in the death of these cells in vivo. Potentiation of Zn2+ accumulation and injury by maintenance of dark adaptation/depolarization supports this notion. 2) The superior retina is more sensitive to light-induced damage compared to the inferior retina, and pyruvate or nicotinamide (i.p.) can attenuate photoreceptor cell death as shown by OCT and plastic sections. 3) In vitro, pyruvate, nicotinamide, sirtinol, NAD+, and, perhaps, TPEN can attenuate Müller, ARPE-19, and 661W cone cell death induced by zinc and oxidative stress.
We and others have previously shown that Zn2+ accumulates in cortical, thalamic, and striatal neurons exposed to extracellular Zn2+ or oxidative stress, and that Zn2+ chelators or compounds that restore NAD+ levels and glycolysis (Zn2+ therapeutics) attenuate injury [28,30,32,52,53]. We now show that these Zn2+ therapeutics were also effective in retinal cells in vitro and in vivo. These compounds have been shown to prevent Zn2+ neurotoxicity by restoring NAD+ levels and glycolytic flux; this may be their mechanism of action against light-induced damage as well. The mechanisms of Zn2+ toxicity has been shown to be multi-factorial, and they include affects on increasing autophagy [54], damaging mitochondria inducing metabolic dysfunction [55,56], inhibiting protein phosphatases causing kinase cascade activation [53,57], and inducing OS through activation of nicotinamide adenine dinucleotide phosphate oxidase [58-60]. Importantly, chelator compounds, Zn2+ reducing manipulations, and manipulations demonstrated to restore NAD+ (pyruvate, nicotinamide, poly-ADP ribose polymerase (PARP) inhibition, slow Wallerian degeneration (Wlds)) have displayed in vivo efficacy against Zn2+ neurotoxicity, but the alternate pathways described above have limited evidence for in vivo efficacy [22,28,31-33,61-64].
High levels of Zn2+ also have been found in the aggregated proteins that comprise drusen in AMD [65]. This is similar to the presence of high levels of Zn2+ in amyloid plaques of Alzheimer disease [66,67]. Zn2+ chelation has been proposed as a therapy for Alzheimer disease [68], and a chelator from DPharm (DP-b99) is being tested in phases II and III Alzheimer clinical trials. This chelator also has proven effective against stroke [69]. This is in contrast to the use of Zn2+ as a supplement in the AREDS trial against AMD. Zn2+ was used in the AREDS trial because it has been reported to be beneficial in the immune system, where it may cause an antioxidant response [reviewed in 70]. However, due to Zn2+ accumulation after ischemia, injury, and in drusen, many researchers have recently questioned the use of Zn2+ supplementation in AMD treatment.
However, it should also be noted that too little Zn2+ in the retina has been shown to be detrimental. Zn2+ deficiency in patients with chronic alcoholic cirrhosis or pancreatitis may reversibly impair dark adaptation, electroretinography, and induce structural defects in the periphery of the retina [71,72]. Also, a chronic Zn2+ deficient diet [73], or Zn2+ chelation [74], resulted in osmiophilic lipid inclusion bodies in the RPE, and ROS disruption.
In these experiments on the role of Zn2+ in retinal neurodegeneration, we used a light-induced retinal damage model for albino rats. Light damage has been shown to cause both direct DNA damage and oxidative DNA damage, both of which can activate PARP, resulting in NAD+ loss [75]. Furthermore, light damage in the eye has been shown to activate PARP, and antioxidants attenuate PARP activation and LD of photoreceptors [76]. We performed time courses of zinc accumulation after light-induced damage using a zinc fluorescent dye on fresh frozen rat retina to demonstrate the accumulation of zinc in the RPE and ONL before light-induced cell death. This Zn2+ accumulation was especially prevalent 4–14 h post-exposure in the superior versus the inferior central retina, which is where photoreceptors are most vulnerable to light damage. Zn2+ accumulation peaked more than 20 h before photoreceptor death occurred, and it was most prevalent in the ROS and in dark-maintained animals. RPE cells also accumulated significant Zn2+, which may be the result of their involvement in the clearance of shed outer segments that contain significant Zn2+ in association with rhodopsin. Zn2+ has been shown to be a structural component of rhodopsin, which is critical for its stability, cis-retinal binding, and function in the dark state [77,78]. In addition, substantial Zn2+ staining also occurred in the sclera, especially after light damage. This was likely due to the tight binding of zinc by the membrane protein elastin.
Photons are absorbed in the outer segments by rhodopsin, changing its structure and resulting in activation of the phototransduction cascade and photoreceptor hyperpolarization. Therefore, light stimulation induces hyperpolarization and dark adaptation induces photoreceptor depolarization, which potentiates Zn2+ influx through voltage-gated calcium channels [50,79,80]. A similar situation seems to occur in the retina, where LD and zinc accumulation was greatest if the retina was completely dark adapted (and therefore depolarized) before and after LD [81,82]. These data implicate Zn2+ influx into photoreceptors in LD. Also, the stainable Zn2+ pool in the retina is dramatically affected by dark adaptation. As stated previously, Zn2+ is located in specific retinal layers in adults exposed to ambient light, but Zn2+ is especially found in the inner segments of photoreceptors. Dark adaptation results in the stainable zinc pool disappearing from the RIS and appearing in the cell bodies of most photoreceptors [36]. The light-dark staining pattern in RIS can be explained by an interaction with rhodopsin (see below), but the pattern in photoreceptor perikarya suggests an unknown Zn2+ binding/translocation protein interaction. It is also interesting to note that Zn2+ deficiency results in a loss of night vision [71,83], which suggests that this dark-induced change in Zn2+ staining may be functionally relevant.
Grimm and colleagues demonstrated effective LD using only 2 h of exposure to 15 kLux white light when pigmented mice were completely dark-maintained before and after LD [84]. Mice maintained in this manner are more sensitive to LD, perhaps due to depolarization of photoreceptors in the dark state and the movement or release of Zn2+ from the inner segments to the photoreceptor cell bodies, which may potentiate injury (Figure 3B) [36]. Some researchers have not demonstrated this degeneration in pigmented mice with 2 h LD, but the dark-adapted state may not have been maintained. In Figure 4B and Figure 6, we show that 2 h of LD with dark maintenance causes substantially more injury than if the albino rats are not dark-maintained. Only 1 h of LD causes almost complete loss of superior photoreceptors in albino Sprague Dawley rats (as determined by OCT and plastic sectioning), while 4 h of light damage was required if animals were returned to light.
Where does the Zn2+ come from to induce the massive increase in Zn2+ staining observed in the ROS and ONL after LD? In the inner and outer segments, rhodopsin has been shown to bind to and require one ion of Zn2+, which stabilizes the structure and organization of rhodopsin into disc membranes [85,86]. The amino acids involved in this high-affinity, required, tetrahedral Zn2+ binding site are Glu122 (at the end of transmembrane region 3), and His211 (at the end of transmembrane region 5). This Zn2+ coordination site lies within the 11-cis-retinal binding pocket and is critical for the stability of this chromophore-receptor interaction and for proper rhodopsin folding in the inactive (dark) state. Binding of additional Zn2+ ions (> 1) to rhodopsin through lower affinity sites (His100 and His195) has been suggested to induce a destabilization that might help RPE cells (with a high basal Zn2+ content) degrade rhodopsin from shed outer segments. Many of the RP rhodopsin mutations cluster around the amino acids involved in Zn2+ binding (His100 and His195), and the His211-Pro or -Arg and the Pro23-His RP mutations have been suggested to affect Zn2+ binding and reduce rhodopsin stability [77,78]. Light activation also induces structural changes increasing the distance between TM 3 and 5 of rhodopsin, which increases the tetrahedral binding distance for Zn2+; this is inconsistent with continued Zn2+ binding [77,87]. We therefore predict Zn2+ release from rhodopsin by light exposure, which is supported by our data (Figure 3). Rhodopsin (Rho) knockout (KO) mice lack opsin synthesis, do not develop an ROS structure, and do not activate the required apoptotic AP-1/c-fos transcription factor in response to LD. Photoreceptors from Rho KO mice spontaneously degenerate starting at 3 months of age, but at 1–2 months of age Rho KO photoreceptors are resistant to LD [84,88,89]. RPE65 KO prevents re-isomerization of all-trans retinol in the visual cycle, and thereby prevents rhodopsin regeneration and rod function. RPE65 KO mice also do not show any photoreceptor death after LD [84,90]. C-fos/AP-1 KO mice were also insensitive to LD [91] and increased [Zn2+]i activates kinase cascades that activate c-fos/AP-1 [53,58,92]. A diffusible light damage-induced factor has been postulated in the literature [21,36,84], and it is possible that Zn2+ is this factor. We postulate that Zn2+ is released from rhodopsin by light and moves to the RIS and cell body, allowing Zn2+ staining and c-fos/AP-1 activation. The regenerated rhodopsin then rebinds this zinc in the ER of the RIS in the dark and RIS staining goes away, thus accounting for the RIS light-dark Zn2+ staining pattern.
Immediate post-LD treatment with these compounds is ongoing and may be effective since it has been shown that pyruvate and nicotinamide are effective for 1–2 h after ischemia, hypoglycemia, and trophic deprivation [26,28,30-33]. Studies involving eye drop application of pyruvate or nicotinamide are also ongoing, and this route of administration may be effective because topical application of pyruvate was shown to penetrate the human cornea [93]. We are also studying the efficacy of reducing retinal Zn2+ through chelators and diet to affect Zn2+ staining and LD, as well as the potentiation of LD by dark maintenance. Finally, we plan to examine the zinc staining of the Rho and RPE65 KO animals and the efficacy of pyruvate and nicotinamide against rhodopsin RP mutant models of retinal degeneration. These experiments have validated the therapeutic efficacy of pyruvate and nicotinamide against the light-induced retinal damage model in rat and have implicated an increase in retinal Zn2+ accumulation in this injury.
Acknowledgments
We would like to thank the laboratory of Dr. Nicolas Bazan for their assistance and discussions. We would like to thank Dr. Muayyad Al-Ubaidi for the 661W cells. This work was supported by a grant from NIDDK #073446 (C.T.S.), and departmental funds.
References
- 1.Zigman S, Datiles M, Torczynski E. Sunlight and human cataracts. Invest Ophthalmol Vis Sci. 1979;18:462–7. [PubMed] [Google Scholar]
- 2.Codenotti M, Patelli F, Brancato R. OCT findings in patients with retinopathy after watching a solar eclipse. Ophthalmologica. 2002;216:463–6. doi: 10.1159/000067540. [DOI] [PubMed] [Google Scholar]
- 3.Thanos S, Heiduschka P, Romann I. Exposure to a solar eclipse causes neuronal death in the retina. Graefes Arch Clin Exp Ophthalmol. 2001;239:794–800. doi: 10.1007/s004170100362. [DOI] [PubMed] [Google Scholar]
- 4.Jain A, Desai RU, Charalel RA, Quiram P, Yannuzzi L, Sarraf D. Solar retinopathy: comparison of optical coherence tomography (OCT) and fluorescein angiography (FA). Retina. 2009;29:1340–5. doi: 10.1097/IAE.0b013e3181b0da88. [DOI] [PubMed] [Google Scholar]
- 5.Vojnikovíc B, Micovic V, Coklo M, Vojnikovic D. Sun exposure and visual field damage among children on the Adriatic Island Rab–possible initial risk factor in development of age-related macular degeneration. Coll Antropol. 2009;33:747–9. [PubMed] [Google Scholar]
- 6.Organisciak DT, Darrow RM, Jiang YI, Marak GE, Blanks JC. Protection by dimethylthiourea against retinal light damage in rats. Invest Ophthalmol Vis Sci. 1992;33:1599–609. [PubMed] [Google Scholar]
- 7.Wang M, Lam TT, Fu J, Tso MO. TEMPOL, a superoxide dismutase mimic, ameliorates light-induced retinal degeneration. Res Commun Mol Pathol Pharmacol. 1995;89:291–305. [PubMed] [Google Scholar]
- 8.Wang M, Lam TT, Tso MO, Naash MI. Expression of a mutant opsin gene increases the susceptibility of the retina to light damage. Vis Neurosci. 1997;14:55–62. doi: 10.1017/s0952523800008750. [DOI] [PubMed] [Google Scholar]
- 9.Bicknell IR, Darrow R, Barsalou L, Fliesler SJ, Organisciak DT. Alterations in retinal rod outer segment fatty acids and light-damage susceptibility in P23H rats. Mol Vis. 2002;8:333–40. [PubMed] [Google Scholar]
- 10.Organisciak DT, Darrow RM, Barsalou L, Kutty RK, Wiggert B. Susceptibility to retinal light damage in transgenic rats with rhodopsin mutations. Invest Ophthalmol Vis Sci. 2003;44:486–92. doi: 10.1167/iovs.02-0708. [DOI] [PubMed] [Google Scholar]
- 11.Duncan T, Wiggert B, Whittaker N, Darrow R, Organisciak DT. Effect of visible light on normal and P23H–3 transgenic rat retinas: characterization of a novel retinoic acid derivative present in the P23H–3 retina. Photochem Photobiol. 2006;82:741–5. doi: 10.1562/2005-10-05-RA-712. [DOI] [PubMed] [Google Scholar]
- 12.Vaughan DK, Peachey NS, Richards MJ, Buchan B, Fliesler SJ. Light-induced exacerbation of retinal degeneration in a rat model of Smith-Lemli-Opitz syndrome. Exp Eye Res. 2006;82:496–504. doi: 10.1016/j.exer.2005.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Richards MJ, Nagel BA, Fliesler SJ. Lipid hydroperoxide formation in the retina: correlation with retinal degeneration and light damage in a rat model of Smith-Lemli-Opitz syndrome. Exp Eye Res. 2006;82:538–41. doi: 10.1016/j.exer.2005.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang LP, Wu LM, Guo XJ, Tso MO. Activation of endoplasmic reticulum stress in degenerating photoreceptors of the rd1 mouse. Invest Ophthalmol Vis Sci. 2007;48:5191–8. doi: 10.1167/iovs.07-0512. [DOI] [PubMed] [Google Scholar]
- 15.Sanz MM, Johnson LE, Ahuja S, Ekstrom PA, Romero J, van Veen T. Significant photoreceptor rescue by treatment with a combination of antioxidants in an animal model for retinal degeneration. Neuroscience. 2007;145:1120–9. doi: 10.1016/j.neuroscience.2006.12.034. [DOI] [PubMed] [Google Scholar]
- 16.Organisciak DT, Li M, Darrow RM, Farber DB. Photoreceptor cell damage by light in young Royal College of Surgeons rats. Curr Eye Res. 1999;19:188–96. doi: 10.1076/ceyr.19.2.188.5333. [DOI] [PubMed] [Google Scholar]
- 17.Wang AL, Lukas TJ, Yuan M, Du N, Tso MO, Neufeld AH. Autophagy and exosomes in the aged retinal pigment epithelium: possible relevance to drusen formation and age-related macular degeneration. PLoS ONE. 2009;4:e4160. doi: 10.1371/journal.pone.0004160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Munemasa Y, Ahn JH, Kwong JM, Caprioli J, Piri N. Redox proteins thioredoxin 1 and thioredoxin 2 support retinal ganglion cell survival in experimental glaucoma. Gene Ther. 2009;16:17–25. doi: 10.1038/gt.2008.126. [DOI] [PubMed] [Google Scholar]
- 19.Kong L, Zhou X, Li F, Yodoi J, McGinnis J, Cao W. Neuroprotective effect of overexpression of thioredoxin on photoreceptor degeneration in Tubby mice. Neurobiol Dis. 2010;38:446–55. doi: 10.1016/j.nbd.2010.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sasaki M, Ozawa Y, Kurihara T, Kubota S, Yuki K, Noda K, Kobayashi S, Ishida S, Tsubota K. Neurodegenerative influence of oxidative stress in the retina of a murine model of diabetes. Diabetologia. 2010;53:971–9. doi: 10.1007/s00125-009-1655-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Organisciak DT, Vaughan DK. Retinal light damage: mechanisms and protection. Prog Retin Eye Res. 2010;29:113–34. doi: 10.1016/j.preteyeres.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yoo MH, Lee JY, Lee SE, Koh JY, Yoon YH. Protection by pyruvate of rat retinal cells against zinc toxicity in vitro, and pressure-induced ischemia in vivo. Invest Ophthalmol Vis Sci. 2004;45:1523–30. doi: 10.1167/iovs.03-1315. [DOI] [PubMed] [Google Scholar]
- 23.Tam D, Tam M, Maynard KI. Nicotinamide modulates energy utilization and improves functional recovery from ischemia in the in vitro rabbit retina. Ann N Y Acad Sci. 2005;1053:258–68. doi: 10.1196/annals.1344.023. [DOI] [PubMed] [Google Scholar]
- 24.Choi JS, Kim KA, Yoon YJ, Fujikado T, Joo CK. Inhibition of cyclooxygenase-2 expression by zinc-chelator in retinal ischemia. Vision Res. 2006;46:2721–7. doi: 10.1016/j.visres.2006.02.014. [DOI] [PubMed] [Google Scholar]
- 25.Koh JY, Suh SW, Gwag BJ, He YY, Hsu CY, Choi DW. The role of zinc in selective neuronal death after transient global cerebral ischemia. Science. 1996;272:1013–6. doi: 10.1126/science.272.5264.1013. [DOI] [PubMed] [Google Scholar]
- 26.Suh SW, Aoyama K, Matsumori Y, Liu J, Swanson RA. Pyruvate administered after severe hypoglycemia reduces neuronal death and cognitive impairment. Diabetes. 2005;54:1452–8. doi: 10.2337/diabetes.54.5.1452. [DOI] [PubMed] [Google Scholar]
- 27.Suh SW, Hamby AM, Gum ET, Shin BS, Won SJ, Sheline CT, Chan PH, Swanson RA. Sequential release of nitric oxide, zinc, and superoxide in hypoglycemic neuronal death. J Cereb Blood Flow Metab. 2008;28:1697–706. doi: 10.1038/jcbfm.2008.61. [DOI] [PubMed] [Google Scholar]
- 28.Sheline CT, Cai AL, Zhu J, Shi C. Serum or target deprivation-induced neuronal death causes oxidative neuronal accumulation of Zn(2+) and loss of NAD. Eur J Neurosci. 2010;32:894–904. doi: 10.1111/j.1460-9568.2010.07372.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee JM, Zipfel GJ, Park KH, He YY, Hsu CY, Choi DW. Zinc translocation accelerates infarction after mild transient focal ischemia. Neuroscience. 2002;115:871–8. doi: 10.1016/s0306-4522(02)00513-4. [DOI] [PubMed] [Google Scholar]
- 30.Sheline CT, Behrens MM, Choi DW. Zinc-induced cortical neuronal death: contribution of energy failure attributable to loss of NAD(+) and inhibition of glycolysis. J Neurosci. 2000;20:3139–46. doi: 10.1523/JNEUROSCI.20-09-03139.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee JY, Kim YH, Koh JY. Protection by pyruvate against transient forebrain ischemia in rats. J Neurosci. 2001;21:RC171. doi: 10.1523/JNEUROSCI.21-20-j0002.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cai AL, Zipfel GJ, Sheline CT. Zinc neurotoxicity is dependent on intracellular NAD levels and the sirtuin pathway. Eur J Neurosci. 2006;24:2169–76. doi: 10.1111/j.1460-9568.2006.05110.x. [DOI] [PubMed] [Google Scholar]
- 33.Suh SW, Aoyama K, Chen Y, Garnier P, Matsumori Y, Gum E, Liu J, Swanson RA. Hypoglycemic neuronal death and cognitive impairment are prevented by poly(ADP-ribose) polymerase inhibitors administered after hypoglycemia. J Neurosci. 2003;23:10681–90. doi: 10.1523/JNEUROSCI.23-33-10681.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rosenstein FJ, Chappell RL. Endogenous zinc as a retinal neuromodulator: evidence from the skate (Raja erinacea). Neurosci Lett. 2003;345:81–4. doi: 10.1016/s0304-3940(03)00472-5. [DOI] [PubMed] [Google Scholar]
- 35.Chappell RL, Anastassov I, Lugo P, Ripps H. Zinc-mediated feedback at the synaptic terminals of vertebrate photoreceptors. Exp Eye Res. 2008;87:394–7. doi: 10.1016/j.exer.2008.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ugarte M, Osborne NN. Zinc in the retina. Prog Neurobiol. 2001;64:219–49. doi: 10.1016/s0301-0082(00)00057-5. [DOI] [PubMed] [Google Scholar]
- 37.Lee SC, Zhong YM, Li RX, Yu Z, Yang XL. Localization of zinc in the outer retina of carp: a light- and electron-microscopic study. Synapse. 2008;62:352–7. doi: 10.1002/syn.20501. [DOI] [PubMed] [Google Scholar]
- 38.Wang X, Wang ZY, Gao HL, Danscher G, Huang L. Localization of ZnT7 and zinc ions in mouse retina–immunohistochemistry and selenium autometallography. Brain Res Bull. 2006;71:91–6. doi: 10.1016/j.brainresbull.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 39.Redenti S, Chappell RL. Neuroimaging of zinc released by depolarization of rat retinal cells. Vision Res. 2005;45:3520–5. doi: 10.1016/j.visres.2005.07.039. [DOI] [PubMed] [Google Scholar]
- 40.Redenti S, Ripps H, Chappell RL. Zinc release at the synaptic terminals of rod photoreceptors. Exp Eye Res. 2007;85:580–4. doi: 10.1016/j.exer.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 41.Yang LP, Wu LM, Guo XJ, Li Y, Tso MO. Endoplasmic reticulum stress is activated in light-induced retinal degeneration. J Neurosci Res. 2008;86:910–9. doi: 10.1002/jnr.21535. [DOI] [PubMed] [Google Scholar]
- 42.Gorbatyuk MS, Knox T, LaVail MM, Gorbatyuk OS, Noorwez SM, Hauswirth WW, Lin JH, Muzyczka N, Lewin AS. Restoration of visual function in P23H rhodopsin transgenic rats by gene delivery of BiP/Grp78. Proc Natl Acad Sci USA. 2010;107:5961–6. doi: 10.1073/pnas.0911991107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gordon WC, Casey DM, Lukiw WJ, Bazan NG. DNA damage and repair in light-induced photoreceptor degeneration. Invest Ophthalmol Vis Sci. 2002;43:3511–21. [PubMed] [Google Scholar]
- 44.Cortina MS, Gordon WC, Lukiw WJ, Bazan NG. Light-induced photoreceptor damage triggers DNA repair: differential fate of rods and cones. Adv Exp Med Biol. 2003;533:229–40. doi: 10.1007/978-1-4615-0067-4_29. [DOI] [PubMed] [Google Scholar]
- 45.Kanan Y, Moiseyev G, Agarwal N, Ma JX, Al-Ubaidi MR. Light induces programmed cell death by activating multiple independent proteases in a cone photoreceptor cell line. Invest Ophthalmol Vis Sci. 2007;48:40–51. doi: 10.1167/iovs.06-0592. [DOI] [PubMed] [Google Scholar]
- 46.Tan E, Ding XQ, Saadi A, Agarwal N, Naash MI, Al-Ubaidi MR. Expression of cone-photoreceptor-specific antigens in a cell line derived from retinal tumors in transgenic mice. Invest Ophthalmol Vis Sci. 2004;45:764–8. doi: 10.1167/iovs.03-1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Krishnamoorthy RR, Crawford MJ, Chaturvedi MM, Jain SK, Aggarwal BB, Al-Ubaidi MR, Agarwal N. Photo-oxidative stress down-modulates the activity of nuclear factor-kappaB via involvement of caspase-1, leading to apoptosis of photoreceptor cells. J Biol Chem. 1999;274:3734–43. doi: 10.1074/jbc.274.6.3734. [DOI] [PubMed] [Google Scholar]
- 48.Sheline CT, Choi DW. Neuronal death in cultured murine cortical cells is induced by inhibition of GAPDH and triosephosphate isomerase. Neurobiol Dis. 1998;5:47–54. doi: 10.1006/nbdi.1998.0177. [DOI] [PubMed] [Google Scholar]
- 49.Ying H, Gottron F, Choi D. Assessment of cell viability in primary neuronal cultures. New York: John Wiley & Sons, Inc; 2000. [DOI] [PubMed] [Google Scholar]
- 50.Canzoniero LM, Turetsky DM, Choi DW. Measurement of intracellular free zinc concentrations accompanying zinc- induced neuronal death. J Neurosci. 1999;19:RC31. doi: 10.1523/JNEUROSCI.19-19-j0005.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tanito M, Li F, Anderson RE. Protection of retinal pigment epithelium by OT-551 and its metabolite TEMPOL-H against light-induced damage in rats. Exp Eye Res. 2010;91:111–4. doi: 10.1016/j.exer.2010.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Aizenman E, Stout AK, Hartnett KA, Dineley KE, McLaughlin B, Reynolds IJ. Induction of neuronal apoptosis by thiol oxidation: putative role of intracellular zinc release. J Neurochem. 2000;75:1878–88. doi: 10.1046/j.1471-4159.2000.0751878.x. [DOI] [PubMed] [Google Scholar]
- 53.Zhang Y, Aizenman E, DeFranco DB, Rosenberg PA. Intracellular zinc release, 12-lipoxygenase activation and MAPK dependent neuronal and oligodendroglial death. Mol Med. 2007;13:350–5. doi: 10.2119/2007-00042.Zhang. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lee SJ, Cho KS, Koh JY. Oxidative injury triggers autophagy in astrocytes: the role of endogenous zinc. Glia. 2009;57:1351–61. doi: 10.1002/glia.20854. [DOI] [PubMed] [Google Scholar]
- 55.Sensi SL, Yin HZ, Weiss JH. AMPA/kainate receptor-triggered Zn2+ entry into cortical neurons induces mitochondrial Zn2+ uptake and persistent mitochondrial dysfunction. Eur J Neurosci. 2000;12:3813–8. doi: 10.1046/j.1460-9568.2000.00277.x. [DOI] [PubMed] [Google Scholar]
- 56.Sensi SL, Ton-That D, Sullivan PG, Jonas EA, Gee KR, Kaczmarek LK, Weiss JH. Modulation of mitochondrial function by endogenous Zn2+ pools. Proc Natl Acad Sci USA. 2003;100:6157–62. doi: 10.1073/pnas.1031598100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Redman PT, Hartnett KA, Aras MA, Levitan ES, Aizenman E. Regulation of apoptotic potassium currents by coordinated zinc-dependent signalling. J Physiol. 2009;587:4393–404. doi: 10.1113/jphysiol.2009.176321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Noh KM, Kim YH, Koh JY. Mediation by membrane protein kinase C of zinc-induced oxidative neuronal injury in mouse cortical cultures. J Neurochem. 1999;72:1609–16. doi: 10.1046/j.1471-4159.1999.721609.x. [DOI] [PubMed] [Google Scholar]
- 59.Kim YH, Kim EY, Gwag BJ, Sohn S, Koh JY. Zinc-induced cortical neuronal death with features of apoptosis and necrosis: mediation by free radicals. Neuroscience. 1999;89:175–82. doi: 10.1016/s0306-4522(98)00313-3. [DOI] [PubMed] [Google Scholar]
- 60.Kim YH, Koh JY. The role of NADPH oxidase and neuronal nitric oxide synthase in zinc- induced poly(ADP-ribose) polymerase activation and cell death in cortical culture. Exp Neurol. 2002;177:407–18. doi: 10.1006/exnr.2002.7990. [DOI] [PubMed] [Google Scholar]
- 61.Endres M, Wang ZQ, Namura S, Waeber C, Moskowitz MA. Ischemic brain injury is mediated by the activation of poly(ADP- ribose)polymerase. J Cereb Blood Flow Metab. 1997;17:1143–51. doi: 10.1097/00004647-199711000-00002. [DOI] [PubMed] [Google Scholar]
- 62.Szabó C, Dawson VL. Role of poly(ADP-ribose) synthetase in inflammation and ischaemia-reperfusion. Trends Pharmacol Sci. 1998;19:287–98. doi: 10.1016/s0165-6147(98)01193-6. [DOI] [PubMed] [Google Scholar]
- 63.Plaschke K, Kopitz J, Weigand MA, Martin E, Bardenheuer HJ. The neuroprotective effect of cerebral poly(ADP-ribose)polymerase inhibition in a rat model of global ischemia. Neurosci Lett. 2000;284:109–12. doi: 10.1016/s0304-3940(00)00988-5. [DOI] [PubMed] [Google Scholar]
- 64.Gillingwater TH, Haley JE, Ribchester RR, Horsburgh K. Neuroprotection after transient global cerebral ischemia in Wld(s) mutant mice. J Cereb Blood Flow Metab. 2004;24:62–6. doi: 10.1097/01.WCB.0000095798.98378.34. [DOI] [PubMed] [Google Scholar]
- 65.Lengyel I, Flinn JM, Peto T, Linkous DH, Cano K, Bird AC, Lanzirotti A, Frederickson CJ, van Kuijk FJ. High concentration of zinc in sub-retinal pigment epithelial deposits. Exp Eye Res. 2007;84:772–80. doi: 10.1016/j.exer.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 66.Lee JY, Cole TB, Palmiter RD, Suh SW, Koh JY. Contribution by synaptic zinc to the gender-disparate plaque formation in human Swedish mutant APP transgenic mice. Proc Natl Acad Sci USA. 2002;99:7705–10. doi: 10.1073/pnas.092034699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lee JY, Mook-Jung I, Koh JY. Histochemically reactive zinc in plaques of the Swedish mutant beta-amyloid precursor protein transgenic mice. J Neurosci. 1999;19:RC10. doi: 10.1523/JNEUROSCI.19-11-j0002.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lee JY, Friedman JE, Angel I, Kozak A, Koh JY. The lipophilic metal chelator DP-109 reduces amyloid pathology in brains of human beta-amyloid precursor protein transgenic mice. Neurobiol Aging. 2004;25:1315–21. doi: 10.1016/j.neurobiolaging.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 69.Diener HC, Schneider D, Lampl Y, Bornstein NM, Kozak A, Rosenberg G. DP-b99, a membrane-activated metal ion chelator, as neuroprotective therapy in ischemic stroke. Stroke. 2008;39:1774–8. doi: 10.1161/STROKEAHA.107.506378. [DOI] [PubMed] [Google Scholar]
- 70.Prasad AS. Zinc: role in immunity, oxidative stress and chronic inflammation. Curr Opin Clin Nutr Metab Care. 2009;12:646–52. doi: 10.1097/MCO.0b013e3283312956. [DOI] [PubMed] [Google Scholar]
- 71.Morrison SA, Russell RM, Carney EA, Oaks EV. Zinc deficiency: a cause of abnormal dark adaptation in cirrhotics. Am J Clin Nutr. 1978;31:276–81. doi: 10.1093/ajcn/31.2.276. [DOI] [PubMed] [Google Scholar]
- 72.Toskes PP, Dawson W, Curington C, Levy NS, Fitzgerald C. Non-diabetic retinal abnormalities in chronic pancreatitis. N Engl J Med. 1979;300:942–6. doi: 10.1056/NEJM197904263001702. [DOI] [PubMed] [Google Scholar]
- 73.Leure-duPree AE, McClain CJ. The effect of severe zinc deficiency on the morphology of the rat retinal pigment epithelium. Invest Ophthalmol Vis Sci. 1982;23:425–34. [PubMed] [Google Scholar]
- 74.Leure-duPree AE. Electron-opaque inclusions in the rat retinal pigment epithelium after treatment with chelators of zinc. Invest Ophthalmol Vis Sci. 1981;21:1–9. [PubMed] [Google Scholar]
- 75.Vodenicharov MD, Ghodgaonkar MM, Halappanavar SS, Shah RG, Shah GM. Mechanism of early biphasic activation of poly(ADP-ribose) polymerase-1 in response to ultraviolet B radiation. J Cell Sci. 2005;118:589–99. doi: 10.1242/jcs.01636. [DOI] [PubMed] [Google Scholar]
- 76.Costa BL, Fawcett R, Li GY, Safa R, Osborne NN. Orally administered epigallocatechin gallate attenuates light-induced photoreceptor damage. Brain Res Bull. 2008;76:412–23. doi: 10.1016/j.brainresbull.2008.01.022. [DOI] [PubMed] [Google Scholar]
- 77.Stojanovic A, Stitham J, Hwa J. Critical role of transmembrane segment zinc binding in the structure and function of rhodopsin. J Biol Chem. 2004;279:35932–41. doi: 10.1074/jbc.M403821200. [DOI] [PubMed] [Google Scholar]
- 78.Gleim S, Stojanovic A, Arehart E, Byington D, Hwa J. Conserved rhodopsin intradiscal structural motifs mediate stabilization: effects of zinc. Biochemistry. 2009;48:1793–800. doi: 10.1021/bi800968w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sheline CT, Ying HS, Ling CS, Canzoniero LM, Choi DW. Depolarization-induced (65)zinc influx into cultured cortical neurons. Neurobiol Dis. 2002;10:41–53. doi: 10.1006/nbdi.2002.0497. [DOI] [PubMed] [Google Scholar]
- 80.Sheline CT, Takata T, Ying H, Canzoniero LM, Yang A, Yu SP, Choi DW. Potassium attenuates zinc-induced death of cultured cortical astrocytes. Glia. 2004;46:18–27. doi: 10.1002/glia.10313. [DOI] [PubMed] [Google Scholar]
- 81.Organisciak DT, Darrow RM, Barsalou L, Kutty RK, Wiggert B. Circadian-dependent retinal light damage in rats. Invest Ophthalmol Vis Sci. 2000;41:3694–701. [PubMed] [Google Scholar]
- 82.Vaughan DK, Nemke JL, Fliesler SJ, Darrow RM, Organisciak DT. Evidence for a circadian rhythm of susceptibility to retinal light damage. Photochem Photobiol. 2002;75:547–53. doi: 10.1562/0031-8655(2002)075<0547:efacro>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 83.McClain CJ, Van Thiel DH, Parker S, Badzin LK, Gilbert H. Alterations in zinc, vitamin A, and retinol-binding protein in chronic alcoholics: a possible mechanism for night blindness and hypogonadism. Alcohol Clin Exp Res. 1979;3:135–41. doi: 10.1111/j.1530-0277.1979.tb05287.x. [DOI] [PubMed] [Google Scholar]
- 84.Grimm C, Wenzel A, Hafezi F, Yu S, Redmond TM, Reme CE. Protection of Rpe65-deficient mice identifies rhodopsin as a mediator of light-induced retinal degeneration. Nat Genet. 2000;25:63–6. doi: 10.1038/75614. [DOI] [PubMed] [Google Scholar]
- 85.Shuster TA, Nagy AK, Conly DC, Farber DB. Direct zinc binding to purified rhodopsin and disc membranes. Biochem J. 1992;282:123–8. doi: 10.1042/bj2820123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Park PS, Sapra KT, Kolinski M, Filipek S, Palczewski K, Muller DJ. Stabilizing effect of Zn2+ in native bovine rhodopsin. J Biol Chem. 2007;282:11377–85. doi: 10.1074/jbc.M610341200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Patel AB, Crocker E, Reeves PJ, Getmanova EV, Eilers M, Khorana HG, Smith SO. Changes in interhelical hydrogen bonding upon rhodopsin activation. J Mol Biol. 2005;347:803–12. doi: 10.1016/j.jmb.2005.01.069. [DOI] [PubMed] [Google Scholar]
- 88.Hafezi F, Marti A, Grimm C, Wenzel A, Reme CE. Differential DNA binding activities of the transcription factors AP-1 and Oct-1 during light-induced apoptosis of photoreceptors. Vision Res. 1999;39:2511–8. doi: 10.1016/s0042-6989(98)00313-7. [DOI] [PubMed] [Google Scholar]
- 89.Hao W, Wenzel A, Obin MS, Chen CK, Brill E, Krasnoperova NV, Eversole-Cire P, Kleyner Y, Taylor A, Simon MI, Grimm C, Reme CE, Lem J. Evidence for two apoptotic pathways in light-induced retinal degeneration. Nat Genet. 2002;32:254–60. doi: 10.1038/ng984. [DOI] [PubMed] [Google Scholar]
- 90.Redmond TM, Yu S, Lee E, Bok D, Hamasaki D, Chen N, Goletz P, Ma JX, Crouch RK, Pfeifer K. Rpe65 is necessary for production of 11-cis-vitamin A in the retinal visual cycle. Nat Genet. 1998;20:344–51. doi: 10.1038/3813. [DOI] [PubMed] [Google Scholar]
- 91.Hafezi F, Steinbach JP, Marti A, Munz K, Wang ZQ, Wagner EF, Aguzzi A, Reme CE. The absence of c-fos prevents light-induced apoptotic cell death of photoreceptors in retinal degeneration in vivo. Nat Med. 1997;3:346–9. doi: 10.1038/nm0397-346. [DOI] [PubMed] [Google Scholar]
- 92.Manzerra P, Behrens MM, Canzoniero LM, Wang XQ, Heidinger V, Ichinose T, Yu SP, Choi DW. Zinc induces a Src family kinase-mediated up-regulation of NMDA receptor activity and excitotoxicity. Proc Natl Acad Sci USA. 2001;98:11055–61. doi: 10.1073/pnas.191353598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chandra P, Hegde KR, Varma SD. Possibility of topical antioxidant treatment of cataracts: corneal penetration of pyruvate in humans. Ophthalmologica. 2009;223:136–8. doi: 10.1159/000184538. [DOI] [PubMed] [Google Scholar]