Abstract
Background:
Tube thoracostomy remains the standard of care for the treatment of pneumothoraces and simple effusions. This report describes a favorable experience with the 8.3 French pigtail catheter as a less invasive alternative to traditional chest tube insertion.
Methods:
We retrospectively reviewed 109 consecutive pigtail catheter placements. Catheters were inserted under local anesthesia at the bedside without radiographie guidance. Pre- and post-insertion chest radiographs were reviewed to determine efficacy of drainage.
Results:
Fifty-one of 109 patients (47%) were mechanically ventilated and 26 patients (24%) had a coagulopathy. There were no complications related to pigtail catheter insertion. Seventy-seven pigtail catheters were placed for pleural effusion and 32 for pneumothorax. Mean effusion volume decreased from 43 to 9 percent, and drainage averaged 2899 ml over 97 hours. Mean pneumothorax size diminished from 38 to 1 percent during an average 71-hour placement. Clinical success rates in the effusion and pneumothorax groups were 86 and 81 percent, respectively.
Conclusion:
The pigtail catheter offers reliable treatment of pneumothoraces and simple effusions and is a safe and less invasive alternative to tube thoracostomy.
Keywords: Pneumothorax, Pleural effusion, Catheter, Drainage
INTRODUCTION
Tube thoracostomy remains the standard of care for the treatment of pneumothorax and simple effusions in most hospitals.1 The 8.3 French pigtail catheter (Cook Inc., Bloomington, IN) was designed for pericardial drainage but was first applied as an alternative to chest tube placement for the treatment of postoperative pleural effusions on the liver transplant service at our institution. A favorable initial experience stimulated broader application of this technique, and the pigtail catheter now enjoys acceptance for chest drainage in a variety of clinical settings. The objective of this study was to evaluate the efficacy of the pigtail catheter as an alternative to tube thoracostomy for pneumothoraces and simple effusions.
MATERIALS AND METHODS
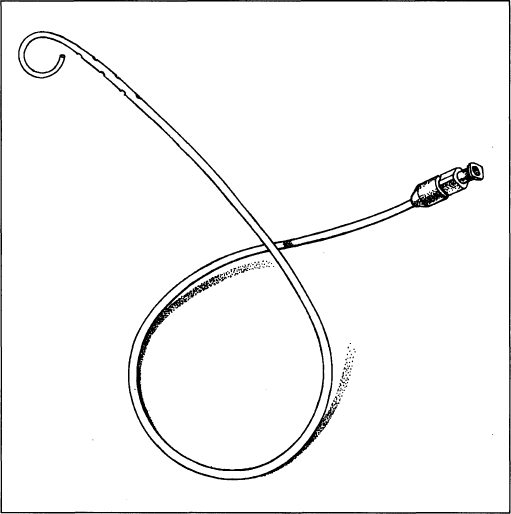
We reviewed all consecutive inpatient pigtail catheter insertions performed between January and October 1996 at the University of Pittsburgh Medical Center. The 8.3 French pigtail catheter (C-PCS-830-LOCK) is constructed of radiopaque polyethylene and is 40 centimeters in length (Figure 1). There are six side holes at the distal end of the catheter. It is packaged with a needle, guidewire, and dilator for insertion using the modified Seldinger technique as well as a serrated, tapered catheter connector which allows easy attachment of the catheter to a standard thoracic drainage system.
Figure 1.
The 8.3 French pigtail catheter (Cook Inc., Bloomington, IN; C-PCS-830-LOCK). The catheter is constructed of polyethylene and has six sideholes at the distal end.
All procedures were done at the bedside under local anesthesia and without radiologie guidance. Salient technical aspects of pigtail catheter insertion include appropriate use of local anesthetic and needle insertion that barely “walks over” the top of the rib to avoid the intercostal bundle. We typically employ a small (22 gauge) “finder needle” before inserting the larger needle provided with the kit. Air or pleural fluid should be easily withdrawn with the needle, and passage of the guidewire into the pleural space should be virtually effortless. Development of an adequate tract with the dilator and insertion of the pigtail so that the sideholes are well within the pleural cavity are important for proper function. The pigtail catheter is attached to a standard thoracic drainage system and suction applied for pneumothoraces.
Pre- and post-placement radiographs were reviewed by a thoracic radiologist (CRF) who determined effusion or pneumothorax volume before and after catheter placement. Pneumothorax and effusion volumes were calculated by determining the average intrapleural distance [AID; AID = (A + B + C) / 3, where A = maximum apical interpleural distance, B = interpleural distance at mid-point of upper half of lung, and C = interpleural distance at midpoint of lower half of lung] and applying a nomo-gram to calculate the percent pneumothorax/effusion volume.2 Therapeutic success was defined as freedom from a second intervention (repeat pigtail placement, tube thoracostomy, or operation) within 72 hours after removal of the pigtail catheter.
RESULTS
One hundred and nine pigtail catheters were placed in 86 patients during the nine-month study period. Mean age was 56.3 years (range 16 to 80 years). There were 50 females and 36 males. Fifty-one of 109 insertions (47%) were performed on mechanically ventilated patients. Coagulopathies (defined as an international normalized ratio greater than 1.5 and/or a platelet count below 80,000/mm3 ) were present at the time of 26/109 (24%) insertions. Seventy-seven effusions and 32 pneumothoraces were treated with pigtail catheters.
Etiologies of effusions included: postoperative (3D, sympathetic (26), congestive heart failure (7), empyema (5), and other (8). The pneumothorax group included: central line-related (10), trauma (9), spontaneous (7), and postoperative (6). Treatment details are outlined in Table 1. Therapeutic success rates in the pneumothorax and effusion groups were 81 and 86%, respectively. There were no major complications related to pigtail catheter insertion. The clinical history and description of failures in the effusion and pneumothorax groups are detailed in Table 2. Among initial failures in the pneumothorax group, one was associated with malposition of the catheter four days after placement (and initial resolution of the pneumothorax). In three additional placements (in two patients), severe underlying parenchymal disease (severe emphysema in one case and diffuse pulmonary abscesses in another) likely predisposed the pig-tail catheter (and in one case multiple chest tubes) to failure. Exclusion of the two patients (three catheter placements) with severe underlying parenchymal disease and prevention of pigtail migration in the fourth would have yielded a success rate of 30/32, or 94% for pneumotho-races.
Table 1.
Treatment details of patients undergoing insertion of pigtail catheters for pneumothorax or simple effusion.
| Effusion (N = 77) | Pneumothorax (N = 32) | |
|---|---|---|
| Duration of drainage (mean ± SD): | 97 ± 15 hours | 71 ± 46 hours |
| Size pre-placementa (mean ± SD): | 43 ± 23% | 38 ± 26% |
| Size post-placement (mean ± SD): | 9 ± 16% | 1 ± 4% |
| Drainage (mean ± SD): | 2899 ± 3782 ml | 145 ± 224 ml |
| Success rate: | 66/77 (86%) | 26/32 (81%) |
Volume of effusion or pneumothorax based on average interpleural distance. SD = standard deviation
Table 2.
Clinical details of patients not responding to initial pigtail catheter placement (therapeutic failures).
| Pneumothoraces: | ||
|---|---|---|
| Pt.# | History | Resolution |
| 1 | s/p lung transplant, OB, PTX after TBBx | Persistent PTX after 72 hours, resolved with CT |
| 2 | s/p OLTX, diffuse pulmonary abscesses | Ongoing air leak/PTX at 48 hours, 2nd pigtail unsuccessful, 2 Cts placed: persistent air leak; ARDS, death |
| 3 | advanced COPD, pneumonia, PTX after central line | Persistent PTX/air leak at 48 hours; required 3 Cts / 19 days to resolve PTX |
| 4 | anorectal cancer, PTX after central line placement | Initial success; recurrent PTX at 96 hours (pigtail sideholes migrated outside thorax); resolved with CT |
| 5 | 3 days s/p CABG; bilat PTX after CT removal | Left pigtail successful; right pigtail failed; CT successful |
| Effusions: | ||
| 1 | 13 days s/p CABG; nonlayering effusion | Pigtail # drained 550 cc/24hrs, then displaced to chest wall Pigtail #2: minimal drainage; CT & CAT-guided pigtail successful |
| 2 | 29 days s/p OLTX | Pigtail successful, removed with 1 liter/day output; 2nd pigtail successful |
| 3 | metastatic breast cancer: bilateral effusions | Left pigtail successful; Right failed: loculated collection required ultrasound-guided drainage w/ 8F catheter |
| 4 | 10 days s/p OLTX | Effusion drained: persistent air leak resolved with 2nd pigtail |
| 5 | 1 day s/p OLTX: opacified hemithorax | Minimal drainage with pigtail; CT also failed: thoracotomy for large hemothorax |
| 6 | 11 days s/p OLTX: right effusion | Pigtail sideholes extrapleural; CT unsuccessful; U/S guided thoracentesis fails: death from sepsis |
| 7 | 14 days s/p AVR: R effusion | Effusion resolved with pigtail: removed 48 hours after placement; pneumothorax 24 hours later resolved w/ CT |
| 8 | 1 month s/p hepatic lobectomy: R effusion | U/S catheter drainage failed; pigtail->partial drainage; CAT-guided 10F catheters x 2 failed (loculated collection); VATS successful |
| 9 | 2 years s/p OLTX: R effusion | Pigtail successful × 72 hours: pulled out on bedrail; residual fluid removed with thoracentesis |
| 10 | Ascites (ESLD): R effusion | Pigtail successful, removed with 1600 cc/day output; second pigtail successful |
OB = obliterative bronchiolitis PTX = pneumothorax TBBx = trans-bronchial biopsy ESLD = end-stage liver disease CT = chest tube OLTX = orthotopic liver transplant ARDS = adult respiratory distress syndrome COPD = chronic obstructive pulmonary disease CABG = coronary artery bypass grafting CAT = computed tomography AVR = aortic valve replacement U/S = ultrasound VATS = video-assisted thoracoscopic surgery
Eleven of 77 catheter placements for pleural effusions were not successful. Four failures were associated with loculated (non-layering) fluid collections that required either operation or radiographically-guided drainage for resolution. In two cases, pigtail catheters were removed when they were draining in excess of 1000 ml of fluid per day, and the underlying effusions re-accumulated. Exclusion of patients with pre-placement evidence of loculated non-layering effusions and postponement of pigtail removal in the face of excess drainage would have yielded a success rate of 94% for effusions treated by pig-tail catheter drainage.
COMMENT
Tube thoracostomy is the gold standard for drainage of pleural fluid and air at most medical centers in the United States. Experience on the liver transplant service at our institution suggested that pneumothoraces and simple effusions could be successfully treated with the 8.3 F pigtail catheter. The current study reviews our experience with 109 catheters inserted in 86 patients over a nine-month period. The high clinical success rate combined with the absence of insertion-related complications strongly supports broader use of the pigtail catheter for drainage of simple effusions and pneumothoraces.
Although sporadic reports supporting the use of small-bore catheters for thoracic drainage have appeared in the literature, this technique has not enjoyed widespread application in clinical practice. Sargent reported using a 9 F catheter to treat pneumothoraces in 1970.3 Lawless and colleagues from the University of Pittsburgh used an 8.5 F pigtail catheter for the treatment of pneumothorax in 16 neonates and small children with a high success rate.4 Robinson applied Tenckhoff catheters for palliative drainage of malignant pleural effusion in nine patients.5 Martin reported the use of a small-bore 13 F catheter with an integral one-way valve for the treatment of simple pneumothoraces in 84 patients.6 All catheters were placed in the second intercostal space in the midclavicular line. No patients were mechanically ventilated. The success rate of 85% in this series was similar to our experience. Conces et al. treated small, asymptomatic, iatrogenic pneumothoraces with a 9 F catheter inserted in the second intercostal space under fluoroscopic guidance with a success rate of 87%.7 A recent extensive review of techniques of thoracic drainage mentions small-bore catheters only in the context of the treatment of spontaneous or post-needle biopsy pneumothoraces in neonates.1 A similar review does not include the small-bore catheter as a therapeutic option.8
The 8.3 F pigtail catheter is now our method of choice for draining air and free-flowing simple effusions from the pleural space. The utility and advantages of the pig-tail catheter for thoracic drainage are supported by the results of this study, with no associated complications in over 100 consecutive insertions. These patients were quite ill: one-half were on mechanical ventilation, and one-quarter had a significant coagulopathy. In general, we do not attempt to correct coagulopathies before inserting the pigtail catheter, and this feature alone makes this technique an attractive alternative to tube thoracostomy for the critically ill, coagulopathic patient. Clinical success rates were high and comparable to previously reported rates for tube thoracostomy.9 For effusions in the current series, 86 percent of initial pigtail placements were clinically successful. Similarly, 81 percent of pigtails inserted for pneumothoraces were successful. Review of failures in both groups (Table 2) suggests that refinement of patient selection and management strategies would yield even higher success rates for the treatment of both pneumothoraces and effusions.
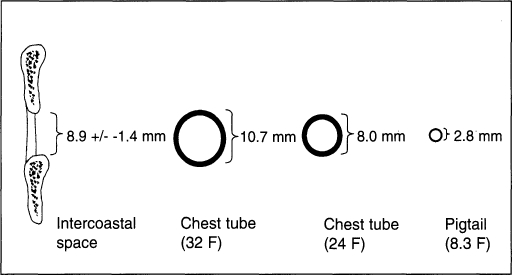
Among physicians at our institution, there is wide acceptance of the pigtail catheter for thoracic drainage on a variety of clinical services. We strongly believe that the pigtail catheter causes substantially less pain than traditional tube thoracostomy, by virtue of its size in relation to the normal intercostal space. The average intercostal space in an adult (measured at the 5th intercostal space in the mix-axillary line) is 8.8 ±1.4 millimeters. A 24 F chest tube (the smallest size commonly used for the described indications) has an outer diameter of 8 mm, while a 32 F chest tube has an outer diameter of just under 11 mm. Chest tubes, with their excessive size, cause pain by compressing the neurovascular bundle at the top of the interspace, as well as by levering open the interspace. In contrast, the 8.3 F pigtail catheter has a diameter of only 2.8 mm and does not impinge on the neurovascular bundle or alter the geometry of the intercostal space (Figure 2). It has previously been shown that routine chest tube placement is frequently associated with an unacceptable pain level.10
Figure 2.
Relative sizes of the average intercostal distance in the adult (fifth intercostal space, mid-axillary line), two commonly used chest tube sizes (24 F and 32 F), and the 8.3 F pigtail catheter.
Success using the pigtail catheter demands adherence to proper patient selection and attention to details at the time of insertion. A lateral decubitus chest radiograph is a rapid and simple way of assuring that an effusion is free-flowing and, therefore, likely to respond to pigtail drainage. Nonlayering effusions should be drained with radiographie guidance. Classic teaching mandates placement of a thoracic drainage tube high in the chest for evacuation of air, and low for evacuation of fluid. In practice, however, with free-flowing effusions and pneumothoraces (in which there is free communication throughout the pleural space), we have not found the site of placement of the pigtail catheter to have any bearing on procedural success. Therefore, we place most pigtail catheters in the 4th-6th intercostal space in the mid-axillary line for maximum patient comfort and ease of insertion. Because the diaphragm can be elevated well into the pleural space (particularly in the presence of effusion and parenchymal collapse), we advise insertion of the catheter in a “safe zone” above the sixth intercostal space to avoid subdiaphragmatic catheter placement with its attendant complications.
We restrict the use of the pigtail catheter for patients with pneumothoraces and for those with nonloculated simple effusions. We do not use the pigtail catheter on newly postoperative patients, trauma patients, or patients with suspected hemorrhagic effusions. The pigtail catheter may have utility for exudative (stage I, American Thoracic Society) empyemas, although our limited experience treating this entity with small-bore catheter drainage precludes a definitive conclusion; stage II (fibrinopurulent) and stage III (organized) empyemas require more invasive management. The pigtail catheter probably also has limited utility in the treatment of malignant pleural effusions, as the ability to perform talc pleurodesis through the catheter is restricted.
In our hands, the pigtail catheter yielded rapid radiographie resolution of both pneumothoraces and pleural effusions. Failure to produce radiographie improvement should prompt insertion of either a second pigtail or a chest tube. One should have a low threshold for additional radiographie study of a pleural fluid collection that does not respond to initial drainage maneuvers.
In conclusion, our enthusiasm for application of the pig-tail catheter for thoracic drainage is substantiated by the findings of this study. The pigtail catheter provides safe, reliable, and effective drainage of pneumothoraces and free-flowing simple effusions and is a reasonable alternative to tube thoracostomy when applied to appropriate patients. Adoption of this technique will provide the clinician with a valuable addition to his/her armamentarium that allows effective pleural drainage with minimal patient discomfort.
Footnotes
We thank Michael Holbert, MD for assistance reading radiographs
References:
- 1. Munnell ER. Thoracic drainage. Ann Thome Surg. 1997;63:1497–1502 [DOI] [PubMed] [Google Scholar]
- 2. Rhea JT, DeLuca SA, Greene RE. Determining the size of pneumothorax in the upright patient. Radiology. 1982;144:733–736 [DOI] [PubMed] [Google Scholar]
- 3. Sargen EN, Turner AF. Emergency treatment of pneumothorax: a simple catheter technique for use in the radiology department. AJR 1970;109:531–535 [PubMed] [Google Scholar]
- 4. Lawless S, Orr R, Killian A, et al. New pigtail catheter for pleural drainage in pediatrie patients. Crit Care Med. 1989;17:173–175 [DOI] [PubMed] [Google Scholar]
- 5. Robinson RD, Fullerton DA, Albert JD, et al. Use of pleural Tenckhoff catheter to palliate malignant pleural effusion. Ann Thorac Surg. 1994;57:286–288 [DOI] [PubMed] [Google Scholar]
- 6. Martin T, Fontana G, Olak J, et al. Use of a pleural catheter for the management of simple pneumothorax. Chest. 1996;110:1169–1172 [DOI] [PubMed] [Google Scholar]
- 7. Gonces DJ, Tarver RD, Gray WC, Pearcy EA. Treatment of pneumothoraces utilizing small caliber chest tubes. Chest. 1988;94:55–57 [DOI] [PubMed] [Google Scholar]
- 8. Quigley RL. Thoracentesis and chest tube drainage. Crit Care Clinics. 1995;11:111–126 [PubMed] [Google Scholar]
- 9. Miller KS, Sahn SA. Chest tubes: indications, techniques, management and complications. Chest. 1987;91:258–263 [DOI] [PubMed] [Google Scholar]
- 10. Luketich JD, Kiss M, Herstery J, et al. Chest tube insertion: a prospective evaluation of pain management. Accepted with revisions to: Clinical Journal of Pain. 1998;14(2):152–154 [DOI] [PubMed] [Google Scholar]