Abstract
Laparoscopic cholecystectomy has been widely performed since its introduction in 1987 by Mouret. However, conversion to open cholecystectomy is common when the surgeon encounters variant anatomy. We report 2 cases of cholecystitis and cholelithiasis in patients with left-sided gallbladders that were treated with laparoscopic cholecystectomy by the same surgeon at this institution. The patient in the first case had the condition of situs inversus totalis, and the gallbladder of the second patient was located to the left of the round ligament. In both instances, successful laparoscopic cholecystectomy was performed, and the patients recovered uneventfully.
Keywords: Situs inversus totalis, Laparoscopic cholecystectomy
CASE REPORTS
Case 1
B.K. was a 43-year-old white female who experienced retrosternal chest pain 3 months prior to her presentation to the surgeon. At that time, she was admitted to the hospital to rule out any cardiac cause of her symptoms. For the next 3 months, she experienced intermittent nausea without vomiting, bloating after some meals, and occasional diarrhea. She did not associate her symptoms with greasy or fatty foods. She also denied any shoulder or back pain. In this interim period, her primary care physician obtained a cardiac stress test and upper GI series, which were both negative. She then received an abdominal ultrasound that showed abdominal situs inversus with the liver and gallbladder in the left upper quadrant and the presence of gallstones without biliary tree distention. No gallbladder wall thickening or pericholecystic fluid was present. She was then referred to the surgeon for definitive care.
Her past medical and surgical history was significant for known situs inversus with dextrocardia, a history of depression, and a dilation and curettage (D & C) following 3 miscarriages. Her obstetrical history was gravida 10, para 7.
Her physical examination demonstrated an obese white female in no apparent distress. She stood 5 feet 6 inches tall and weighed 174 pounds. Head, eye, ear, nose, throat (HEENT), cardiovascular, respiratory, genitouri-nary, and neurologic systems were all within normal limits. No jaundice or scleral icterus was present. Her abdomen was obese, soft, nontender and non-distended. Bowel sounds were present. No masses were palpated. The liver and spleen were nonpalpable. Stool was guaiac negative.
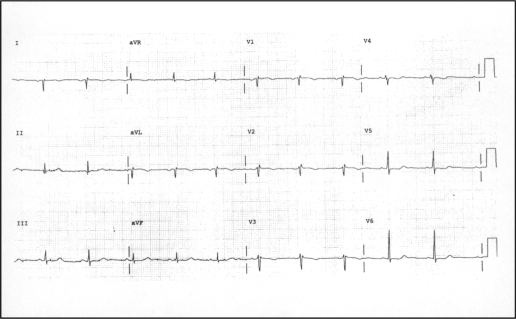
A preoperative electrocardiogram (ECG) (Figure 1) showed a right axis deviation, positive QRS complex in aVR, and a negative QRS in leads I and aVL, consistent with dextrocardia. CBC, blood chemistries, and liver function tests were all within normal limits.
Figure 1.
Preoperative ECG revealing right axis deviation, positive QRS complex in lead aVR, negative QRS in leads I and aVL, suggestive of dextrocardia.
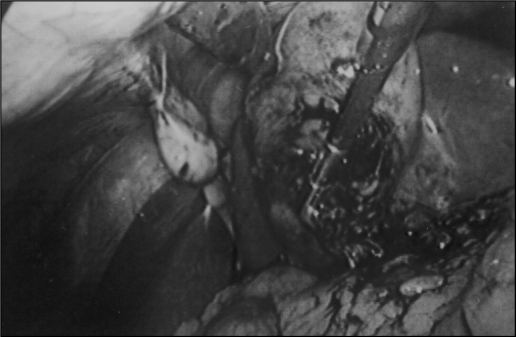
In the operating room, a 10-mm trocar was first placed in the infraumbilical position and the laparoscope was inserted. Visualization of the peritoneal cavity confirmed situs inversus. Three more 5-mm ports were introduced under direct visualization, 1 in the left anterior axillary line, 1 in the left midclavicular line, and the third in the epigastric region. The gallbladder was then visualized and dense omental adhesions were released (Figure 2). Next, the hepatoduodenal ligament was dissected, and the cystic duct and artery were identified and endo-clipped in the usual fashion. The gallbladder was then dissected from the liver bed, hemostasis was obtained, irrigation performed, and the gallbladder was removed from the umbilical port after first crushing and removing several large stones that were from 1 to 1.5 cm in diameter. The remainder of the operation concluded without incident.
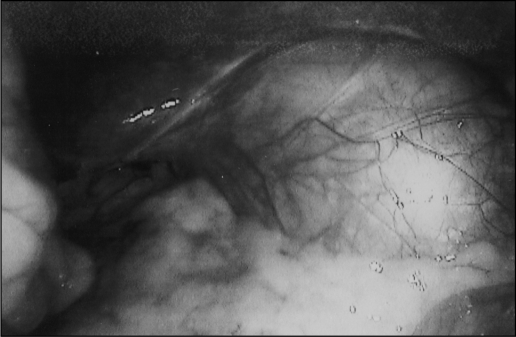
Figure 2.
Intraoperative laparoscopic photograph of the gallbladder following the release of omental adhesions. Situs inversus is apparent, as is the location of the gallbladder in the left upper quadrant
Pathologic examination of the surgical specimen revealed nonspecific chronic cholecystitis with associated cholelithiasis. The patient recovered uneventfully and had no recurrence of her symptoms.
Case 2
E.P. was a 34-year-old white female who presented with the chief complaint of intermittent epigastric pain that radiated laterally to both sides of her upper abdomen. She noted feeling bloated on occasion and also associated her discomfort with eating greasy foods. She stated that her symptoms first began about 6 weeks prior to her presentation to the office. She denied any nausea, vomiting, diarrhea, shoulder pain, jaundice, or urinary symptoms. She did admit to a lifelong history of constipation. Her past medical and surgical histories were significant for repair of a ventral septal defect at age 7. Her medications included Prilosec and FiberCon.
Her physical examination demonstrated a soft abdomen with tenderness present in the right upper quadrant. No rebound, guarding, rigidity, or hepatosplenomegaly was detected. HEENT, cardiovascular, respiratory, genitouri-nary, and neurologic systems were all within normal limits. A midline scar was present on her anterior thorax.
Abdominal ultrasound revealed cholelithiasis. No other abnormalities were noted. Preoperative ECG showed a left posterior fascicular block and an incomplete right bundle branch block. Preoperative complete blood count (CBC) and liver function tests were all within normal limits.
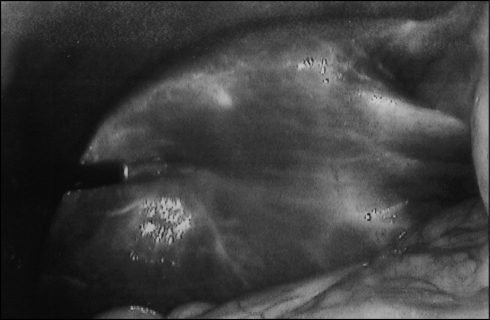
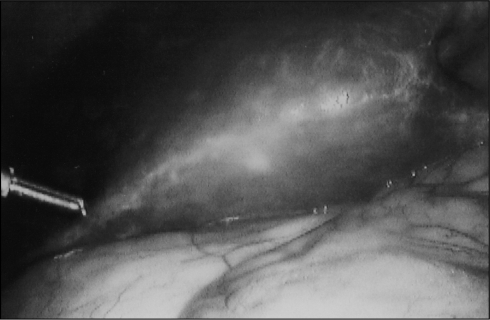
In the operating room, the laparoscope was introduced into a 10-mm infraumbilical port, followed by three 5-mm ports in the right midclavicular line, the right anterior axillary line, and the epigastric region. The liver was exposed, and the gallbladder was not seen in the usual anatomic location. Further exploration revealed the gall-bladder to lie to the left of the round ligament (Figures 3,4,5). Two additional 5-mm ports were then inserted in the left midclavicular line and the left anterior axillary line. The hepatoduodenal ligament was identified, and the cystic duct dissected out. Attempts to perform a cholangiogram were unsuccessful, as the cholangio-catheter was unable to be inserted. Based upon normal preoperative liver enzymes, further attempts were abandoned. Next, the cystic artery was identified and transected in the usual fashion. The gallbladder was then removed from the hepatic bed without much difficulty. Hemostasis was obtained and irrigation performed, and the gallbladder was removed through the epigastric port. The remainder of the operation proceeded in a normal fashion without incident.
Figure 3.
Intraoperative laparoscopic photographs taken upon initial attempt to visualize the gallbladder. Note the normally situated liver and falciform ligament and the absence of the gallbladder in its usual location.
Figure 4.
Intraoperative laparoscopic photographs taken upon initial attempt to visualize the gallbladder. Note the normally situated liver and falciform ligament and the absence of the gallbladder in its usual location.
Figure 5.
Intraoperative laparoscopic photographs showing the gallbladder lying to the left of the round and falciform ligaments
Pathologic examination of the specimen revealed chronic cholecystitis with cholelithiasis. The patient recovered uneventfully and had no recurrence of her symptoms.
DISCUSSION
We report 2 cases of left-sided gallbladders successfully treated by laparoscopic cholecystectomy by the same surgeon. The first case presented illustrates a left-sided gallbladder associated with situs inversus totalis. Situs inversus totalis is inherited as an autosomal recessive trait1–3 and occurs in approximately 1 per 10 to 20,000 live births.1–5 It is defined as the transposition of both the thoracic and abdominal viscera to the opposite side of the body.6 In our first patient, the diagnosis of situs inversus totalis had been made prior to her presentation. However, some clues to this condition in a previously undiagnosed patient include: abnormal ECG findings, particularly right axis deviation and apparent reversal of limb leads; chest x-ray revealing dextrocardia; abdominal x-rays showing the stomach bubble on the right side and the liver shadow on the left.7 On physical examination of these patients, pain may be located in the epigastrium or left upper quadrant and may radiate to the left shoulder or back,8 and heart sounds can be heard best on the right side of the thorax. Definitively, the diagnosis can be made preoperatively with an abdominal ultrasound or CT scan, which will clearly show the presence of situs inversus.
Not all cases of left-sided gallbladders are associated with situs inversus. Recently Fujita et al9 and Nagai et al10 reported in 19 cases the occurrence of round ligaments aberrantly located to the right side of normally positioned gallbladders, giving the appearance of left-sided gallbladders. In our second patient, however, the round ligament was indeed located in its normal position, and the gallbladder was located to the left of the round ligament, a type of malposition known as sinistrotorsion.11 Idu et al11 calculated a prevalence of 0.3% for sinistrotorsion of the gallbladder in a review of a series of 1764 patients who underwent laparoscopic cholecystectomy for symptomatic gallstone disease, indicating the rarity of this variant of left-sided gallbladder location.
Regardless of the etiology of the left-sided gallbladder, cholecystitis, cholelithiasis, and even empyema of the gallbladder12 in these patients can be successfully and safely treated laparoscopically. The operation is carried out in the usual manner with the trocars placed in locations on the left side of the abdomen as mirror images to their usual location on the right side. We found this port placement to be equally effective in accomplishing laparoscopic cholecystectomy when encountering left-sided gallbladders regardless of whether the cause was sinistrotorsion of the gallbladder or situs inversus totalis. Furthermore, careful dissection must be performed and an intraoperative cholangiogram, although not required, often proves helpful in verifying the biliary anatomy.
References:
- 1. Lipschutz JH, Canal DF, Hawes RH, Ruffolo TA, Besold MA, Lehman GA. Laparoscopic cholecystectomy and ERCP with sphincterotomy in an elderly patient with situs inversus. Am J Gastroenterology. 1992; 87: 218–220 [PubMed] [Google Scholar]
- 2. McDermott JP, Caushaj PF. ERCP and laparoscopic cholecystectomy for cholangitis in a 66-year-old male with situs inversus. Surg Endosc. 1994; 8: 1227–1229 [DOI] [PubMed] [Google Scholar]
- 3. Watanabe M, Ueki K, Okinaga Y, Umekawa Y, Hidaka M, Hirakawa H, Fukumoto S, Shimada Y. Laparoscopy of situs inversus totalis. Endoscopy. 1989; 21: 293–294 [DOI] [PubMed] [Google Scholar]
- 4. Huang SM, Chau GY, Lui WY. Laparoscopic cholecystectomy for cholelithiasis in a patient with situs inversus totalis. Endoscopy. 1992; 24: 802–803 [DOI] [PubMed] [Google Scholar]
- 5. Southa JA. Left-sided gallbladder: calculous cholecystitis with situs inversus. Annal Surg. 1975; 182: 135–137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Venu RP, Geenen JE, Hogan WJ, Johnson GK, Taylor AJ, Stewart ET, Jackson A. ERCP and endoscopic sphincterotomy in patients with situs inversus. Gastrointest Endosc. 1985; 31: 338–340 [DOI] [PubMed] [Google Scholar]
- 7. Takei HT, Maxwell JG, Clancy TV, Tinsley EA. Laparoscopic cholecystectomy in situs inversus totalis. J Laparoendoscopic Surg. 1992; 2: 171–176 [DOI] [PubMed] [Google Scholar]
- 8. Drover JW, Nguyen KT, Pace RF. Laparoscopic cholecystectomy in a patient with situs inversus viscerum: a case report. Canadian J Surg. 1992; 35: 65–66 [PubMed] [Google Scholar]
- 9. Fujita N, Shirai Y, Kawaguchi H, Tsukada K, Hatakeyama H. Left-sided gallbladder on the basis of a right-sided round ligament. Hepatogastroenterology. 1998; 23: 1482–1484 [PubMed] [Google Scholar]
- 10. Nagai M, Kubota K, Kawasaki S, Takayama T, Bandai Y, Makuuchi M. Are left-sided gallbladders really located on the left side?. Annal Surg. 1997; 225: 274–280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Idu M, Jakimowicz J, Iuppa A, Cushieri A. Hepatobiliary anatomy in patients with transposition of the gallbladder: implications for safe laparoscopic cholecystectomy. Br J Surg. 1996; 83: 1442–1443 [DOI] [PubMed] [Google Scholar]
- 12. Goh P, Tekant Y, Shang NS. Laparoscopic cholecystectomy in a patient with empyema of the gallbladder and situs inversus. Endoscopy. 1992; 45: 799–800 [DOI] [PubMed] [Google Scholar]