Abstract
Background:
Suturing and knot tying are basic skills for surgeons. Performing these tasks laparoscopically can be a tedious, time-consuming endeavor associated with much frustration. We evaluated a mechanically assisted suture and pretied knot device (Quik-Stitch) for performing the basic tasks of suturing and knot tying.
Methods:
We performed a time study using 1) intracorporeal suturing and knot tying, 2) intracorporeal suturing and extracorporeal knot tying, and 3) a mechanically assisted suture and pretied knot device (Quik-Stitch). From September 2000 through March 2001, time trials were conducted using each of the different techniques. Three attending surgeons, one with much experience and 2 with less experience, and 2 chief residents, with the least experience, participated in the study.
Results:
For the experienced surgeon, the average times for intracorporeal knot tying, extracorporeal knot tying, and knot tying with Quik-Stitch were 97.3, 103.9, and 67.7 seconds, respectively. For the less experienced surgeons, the times were 237.2, 224.3, and 92.5 seconds, respectively. For the least experienced group, the times were 265.3, 263.0, and 128.7 seconds, respectively.
Conclusions:
The mechanically assisted suture device and pretied knot (Quik-Stitch by PARE Surgical, Inc, Englewood, CO, USA) provides significant time-saving to surgeons regardless of experience and thus reduces operating room costs. Less experienced surgeons and surgeons in training benefited the most by the use of this device.
Keywords: Quik-Stitch, Suture, Laparoscopic suturing
INTRODUCTION
Because laparoscopic surgery is considered the standard of care for many surgical conditions, residents are expected to learn advanced laparoscopic skills by the time they graduate. Many courses are offered to teach advanced laparoscopic techniques and provide an opportunity for the surgeon to practice outside the operating room. Laparoscopic suturing and knot tying are among the most basic, but also the most challenging, skills required of the laparoscopic surgeon.
Currently, many laparoscopic suturing and knot tying methods are used by surgeons. The oldest technique is intracorporeal suturing and knot tying. Two laparoscopic needle drivers and a curved needle are used to tie a series of half-hitch knots inside the body. This technique requires skill to manipulate the needle, pass it from 1 needle driver to the next, and execute a series of knots.
Intracorporeal suturing and extracorporeal knot tying techniques were later introduced as an alternative to intracorporeal knot tying. Two needle drivers and a curved needle were used to suture, but the knot was tied extracorporeally using a series of half-hitch knots that were advanced into the abdomen through a port by using a knot pusher.
Recently, a number of devices have been introduced into the market in an attempt to simplify and expedite the process of laparoscopic suturing and knot tying. In terms of suturing, a straight needle eliminates the necessity of orienting a curved needle in 2-dimensional space. The EndoStitch (United States Surgical Corporation, Norwalk, CT, USA) allows transfer of a straight needle within 2 jaws of the same instrument. A straight needle can also be passed between 2 traditional needle drivers.
In terms of knot tying, certain instruments have pretied knots that can be deployed after suturing is completed. The Quik-Stitch (PARE Surgical, Inc., Englewood, CO, USA) incorporates a straight ski needle attached to a pretied knot.
The literature comparing different methods is difficult to interpret because no prospective, randomized controlled trials on human subjects have been conducted. Of the studies that have been reported about in the literature, most compare only 2 different methods. Studies are available on knot strength, suture choice, physician preference in terms of time, ease of use, and cost analysis.1–5
We present a comparison of conventional instruments versus a mechanical assist device, the Quik-Stitch.
METHODS
Data were gathered between September 2000 and March 2001. All surgical procedures were done at either Exempla Saint Joseph Hospital or Presbyterian Saint Lukes Hospital in Denver, Colorado.
We compared 3 different surgical skill levels: experienced (1 advanced laparoscopic surgeon), less experienced (2 general surgeons), and least experienced (2 surgical chief residents). Three different techniques were evaluated: intracorporeal suturing and knot tying, intracorporeal suturing and extracorporeal knot tying, and the Quik-Stitch for both suturing and knot tying.
For each patient, 6 knots were tied. Two time trials were conducted for each suture method. Nine patients were in the experienced group, and 5 patients were in each of the other 2 groups.
To assure that no significant difference existed between the knot tying times of the surgeons within a skill level, a Wilcoxon rank sum test was done for both the less and least experienced groups. Because sample sizes were small, statistical analyses were performed using the Kruskal-Wallis test (one-way ANOVA for nonparametric data) to compare the different methods of knot tying in each surgeon skill level.
RESULTS
No statistically significant difference was found in the knot tying times between surgeons within the same group (P >0.14). For the experienced surgeon, the average times for intracorporeal knot tying, extracorporeal knot tying, and knot tying with Quik-Stitch were 97.3 seconds, 103.9 seconds, and 67.7 seconds, respectively. For the less experienced surgeons, the average times were 237.2 seconds, 224.3 seconds, and 92.5 seconds, respectively. For the chief surgical residents, the average times were 265.3 seconds, 263.0 seconds, and 128.7 seconds, respectively. Table 1 reports the average knot tying times for each surgeon experience group, as well as the minimum and maximum times per group because sample sizes are small.
Table 1.
Average Knot Tying Times by Surgeon Skill Level
| Skill Level | Intracorporeal* | Extracorporeal* | Quik-Stitch* |
|---|---|---|---|
| Experienced | 97.3 (80, 124) | 103.9 (96, 113) | 67.7 (38, 86) |
| Less experienced | 237.2 (233, 244) | 224.3 (219, 229) | 92.5 (91, 94) |
| Surgical chief residents | 265.3 (216, 299) | 263.0 (233, 285) | 128.7 (109, 144) |
Seconds (minimum, maximum).
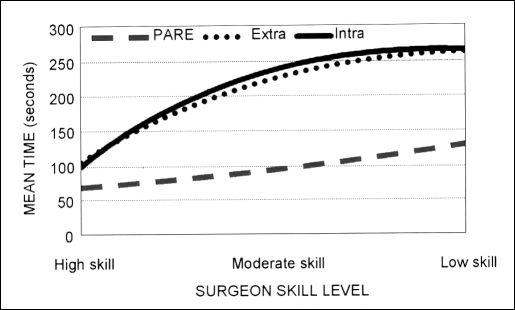
Using the Kruskal-Wallis test, we found a statistically significant difference between the knot tying times for each of the 3 surgeon skill levels (P<0.01). However, the Quik-Stitch was the fastest technique regardless of skill of the surgeon, as evidenced by Figure 1.
Figure 1.
Mean knot tying time by skill level.
CONCLUSION
The use of the mechanically assisted suture device and pretied knot device (Quik-Stitch) took less time than either the intra- or extracorporeal methods. For the experienced surgeon, the average time difference between the Quik-Stitch and intracorporeal knot tying was approximately 30 seconds per stitch. For the least experienced surgeons, the average time difference was greater than 2 minutes.
Less experienced surgeons and surgeons in training benefited the most by the use of the Quik-Stitch. In addition, time saved in the operating room can decrease cost. Randomized, controlled trials would be needed to further evaluate this issue, but our data suggest that the Quik-Stitch is the fastest knot tying technique regardless of surgeon skill level.
References:
- 1. Kadirkamanathan SS, Shelton JC, Hepworth CC, Laufer JG, Swain CP. A comparison of the strength of knots tied by hand and at laparoscopy J Am Coll Surg. 1996;182:46–54 [PubMed] [Google Scholar]
- 2. Nguyen NT, Mayer KL, Bold RJ, et al. Laparoscopic suturing evaluation among surgical residents. J Surg Res. 2000;93:133–136 [DOI] [PubMed] [Google Scholar]
- 3. Pattaras JG, Smith GS, Landman J, Moore RG. Comparison and analysis of laparoscopic intracorporeal suturing devices: Preliminary results. J Endourol. 2001;15(2);187–192 [DOI] [PubMed] [Google Scholar]
- 4. Sedlack JD, Willliams VM, DeSimone J, Page D, Ghosh BC. Laparoscopic knot security. Surg Laparosc Endosc. 1996;6(2):144–146 [PubMed] [Google Scholar]
- 5. Risucci D, Geiss A, Gellman L, Pinard B, Rossner J. Surgeon-specific factors in the acquisition of laparoscopic surgical skill. Am J Surg. 2001;181:289–293 [DOI] [PubMed] [Google Scholar]