Abstract
Objective:
Primary cysts constitute 25% of all masses in the mediastinum. Because radiological investigations are often inconclusive, many adults require mediastinoscopy, thoracotomy, video-assisted thoracic surgery, or computed tomography-guided transbronchial, transesophageal, or transcutaneous aspiration to confirm the cystic nature of these lesions. Minimally invasive procedures fail when the cyst contents are gelatinous and mucoid (failure to aspirate) or when the cyst wall continues to secrete fluid. Though Pursel reported mediastinoscopic extirpation of benign cysts 35 years ago, it remains a “therapeutic curiosity” with sporadic reports of its usage. We report 2 successful mediastinal cyst extirpations performed as out-patient procedures and review the literature with regards to its management.
Methods:
A rigid, 8-mm mediastinoscope was inserted into the anterior mediastinum following the creation of a 2-cm suprasternal incision and dissection along the anterior surface of the trachea. After aspiration, cytology of the contents revealed their benign nature. Right paratracheal cysts in 2 adult males were successfully removed mediastinoscopically by blunt and sharp dissection.
Results:
Histopathology revealed benign mesothelial cysts in both instances. Both patients had an uncomplicated procedure and were discharged within 23 hours. No other pathology was detected on mediastinoscopy, and follow-up at 3 months and 6 months has revealed no recurrence.
Conclusion:
Mediastinoscopic cyst removal is a minimally invasive procedure with a very low morbidity and mortality rate. Morbidity, recovery, and discharge times are much less than those of more invasive procedures (video-assisted thoracic surgery / thoracotomy). We suggest that it should be the first-choice procedure for the excision of appropriately located benign mediastinal cysts.
Keywords: Mediastinal cysts, Resection
INTRODUCTION
The mediastinum is the extrapleural space within the thorax, lying between the pleural cavities. It is a mobile partition that extends superiorly to the thoracic inlet and the root of the neck and inferiorly to the diaphragm. Anteriorly, it extends to the sternum and posteriorly to the thoracic vertebrae. An imaginary plane from the sternal angle to the lower border of the fourth thoracic vertebra divides it into superior and inferior portions. The inferior mediastinum is subdivided into anterior mediastinum (between the pericardium and sternum), middle mediastinum (contains the heart and pericardium) and posterior mediastinum (between pericardium and vertebral column).1 Important structures in the mediastinum include the thymus, trachea, heart within the pericardium, esophagus, large arteries and veins, thoracic duct, sympathetic trunk, and the phrenic nerves. Primary cysts constitute 25% of all masses in the mediastinum.2 Mediastinal cysts can be differentiated into foregut cysts (bronchogenic, esophageal, gastroenteric, and nonspecific), pericardial cysts, thymic cysts, dermoid cysts (teratomatous cysts), and other rare variants (cystic mediastinal tuberculosis and cystic schwannoma).3
ETIOLOGY, PATHOLOGY, AND CLINICAL FEATURES OF MEDIASTINAL CYSTS
Foregut cysts are the most common mediastinal cysts with an incidence of nearly 50% of all cysts encountered. The gastroenteric type arises from adherence of the primitive endodermal tube to the notochord, with a traction diver-ticulum or a duplication cyst developing due to differential growth of the vertebral column (Neurenteric theory of Fallon). They are often associated with vertebral abnormalities like spina bifida or split vertebrae.4–6 Esophageal cysts are characterized by a double layer of smooth muscle in their wall and arise from sequestration of isolated vacuoles, the normal fusion of which leads to canalization of the solid embryonic foregut tube.7 At approximately the fourth week of embryonic life, the respiratory diverticulum appears as an outgrowth from the ventral wall of the foregut. Two longitudinal ridges develop as the diverticulum grows caudally separating it from the foregut. The bronchial buds develop as 2 lateral outpocketings from this diverticulum. Bronchogenic cysts arise from abnormal budding of the bronchial tree8,9 and are characterized by their ciliated epithelial lining with focal areas of hyaline cartilage, smooth muscle, and bronchial glands in their wall.10–14 Maier15 classified bronchogenic cysts based on location into paratracheal, carinal, hilar, paraesophageal, and miscellaneous and found that they were most common at the hilar location. Recent studies however have found them most commonly in the paratracheal or subcarinal regions.16–18
Foregut cysts occur equally in male and female subjects.17 Cysts may be discovered incidentally in asymptomatic patients; however, a majority eventually cause aerodigestive compressive symptoms by enlargement secondary to bleeding, infection, or retained epithelial secretions. Airway obstruction and pneumonia are common presenting features in infants and children.19,20 Rupture of a bronchogenic cyst into the bronchus,21 pericardium,22 and pleura has been reported. Neurologic symptoms may occur in patients who have intraspinal extension of neurenteric cysts.23 Heterotopic, gastric, or pancreatic rests in esophageal duplication cysts may cause ulceration, hemorrhage, or rupture due to their secretions. A few reports of malignant transformation in foregut cysts24–26 and bronchogenic cysts27–30 exist. Due to the high incidence of complications, operative removal is the standard treatment for foregut cysts.22
Percardial cysts, also known as “spring water cysts,” are thought to arise from persistent ventral parietal recesses of the pericardium and rarely communicate with the pericardial cavity.31,32 They are uncommon asymptomatic lesions detected in the fourth or fifth decades of life. They are most commonly located in the right (70%) or left (22%) cardiophrenic angles.33 They are unilocular masses composed of fibrous connective tissue and lined by a single layer of mesothelial cells. A majority of these cysts need only radiological and clinical follow-up with surgical resection being performed to exclude a foregut cyst or a cystic neoplasm.34
Thymic cysts are classified as unilocular or multilocular. While unilocular cysts are considered congenital (arising from the remnants of the thymopharyngeal ducts),35 multilocular cysts are considered to form as a reaction to inflammation36 and are reported in patients with HIV, congenital syphilis (Dubois' abscess), and in congenital rubella syndrome. Subscribing to this hypothesis are pathology reports that have shown thin-walled unilocular cysts and pericystic fibrosis with inflammatory changes in the walls of multilocular cysts. Unilocular cysts cause symptoms when they enlarge, and surgical excision is recommended. Multilocular cysts can rarely transform into malignant lesions,37 but surgery is usually needed due to compressive symptoms from increasing cyst size.
Dermoid cysts are benign teratomas. Malignant teratomas are less common and are usually solid with a cystic component. Components from all 3 germ layers are encountered in a dermoid cyst while malignant lesions exhibit fewer well-differentiated structures. The mediastinum is the second most common site after the ovary or testis as the primary location for a teratoma. Common symptoms include chest pain, productive cough, and hemoptysis. Complications include cystobronchial and cystocutaneous fistulae, compressive symptoms, lipoid granulomatosis, or pneumonia from discharge of cystic contents into the bronchial tree. Malignant transformation of benign teratomas has been reported.38 Malignant teratomas often metastasize to bone. Ideal treatment for mediastinal teratomas is extirpation using a posterolateral thoracotomy approach.39
Miscellaneous cystic lesions encountered in the mediastinum include undifferentiated cysts, cystic schwannomas, cystic mediastinal tuberculous lymphadenitis, and lateral thoracic meningoceles.3 Lateral thoracic meningoceles are the most common cause of posterior mediastinal masses in patients with neurofibromatosis.31 They are usually followed up radiologically and clinically with surgical excision being indicated only if symptoms develop.40 Undifferentiated cysts share in common the location and clinical features of a bronchogenic cyst and are unilocular. Indications for excision include compressive symptoms.
EVALUATION
Mediastinal cysts present as masses on plain radiographs performed for symptoms described above. In asymptomatic individuals, they are often detected incidentally on routine chest radiographs or barium swallows.41 Air fluid levels on plain radiographs indicate communication of the cyst with a bronchus. A computed tomographic (CT) scan is however the most useful noninvasive investigation to confirm the cystic nature of a mediastinal lesion. A presumptive diagnosis of benign mediastinal cyst is based on the following CT findings: 1) a smooth, oval, or tubular mass with well-defined margins and no evidence of a thick and irregular wall; 2) homogenous CT attenuation usually but not invariably in the range of water density (0H to 20H); 3) no vascular enhancement; 4) no infiltration of adjacent mediastinal structures; and 5) characteristic location in the paratracheal, carinal, subcarinal, or paraesophageal region.42
Because radiological investigations are often inconclusive, many adults require mediastinoscopy, thoracotomy, video-assisted thoracic surgery (VATS), or CT-guided transbronchial, transesophageal, or transcutaneous aspiration to confirm the cystic nature of these lesions. Although the latter procedures are minimally invasive, their long-term efficacy is debatable because the cyst wall is not removed and is likely to continue to secrete fluid, resulting in recurrence unless sclerosants can be injected into the cyst.43 Further high-density mediastinal cysts, with high computed tomography coefficients (120H), containing gelatinous and highly mucoid contents cannot be aspirated successfully.42 Pursel et al44 nearly 35 years ago reported 2 cases of successful mediastinoscopic extirpation of benign mediastinal cysts. They offered this option as a “therapeutic curiosity” in subjects at poor risk for thoracotomy or in cases incidentally detected during mediastinoscopy. Since that time, sporadic reports have been made of successful mediastinoscopic removal of benign cysts as day surgery procedures.45,46 Davis and colleagues1 noted that nearly 65% of all mediastinal cysts presented in the middle or anterosuperior mediastinum, areas readily accessible to the mediastinoscope. However, many recent series continue to use this technique sparingly, preferring to perform thoracoscopic or surgical (thoracotomy) removal.12,47,48 These are associated with prolonged hospital stay, (2.1 days average length of stay in Hazelrigg et al's series48 after thoracoscopy; 12.4±12 days after muscle sparing or conventional thoracotomy incisions), and increased morbidity.49 Ashbaugh50 in his review of 9543 mediastinoscopies reported a morbidity of 1.5% and a mortality of 0.09%. We report 2 successful medastinoscopic cyst extirpations with follow-ups at 3 months and one year and recommend a more aggressive use of this procedure in the removal of anterosuperior and middle mediastinal benign cysts.
CASE REPORT 1
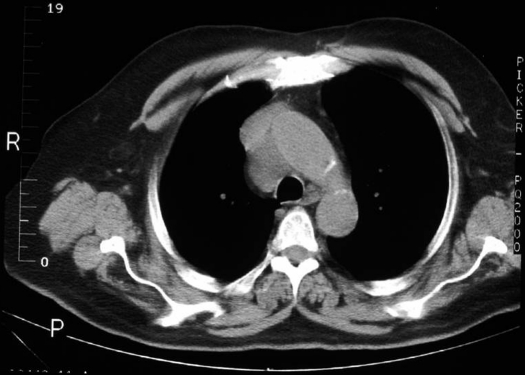
A 54-year-old man was noted to have a mediastinal mass revealed on a chest X-ray performed for an annual medical examination. A CT scan (Figure 1) showed a large right paratracheal mass (3x2x3 cm). The patient did not have a history of fever, chills, night sweats, weight loss, cough, or hemoptysis. His past medical history was significant for a stroke with some difficulty in communication thereof. He was a smoker (35 packs/year) and a retired army veteran. On physical examination, no significant lymphadenopathy was found, and the lung fields were clear to auscultation bilaterally. Bronchoscopy and Wang needle aspiration of the mass was attempted initially with no success in establishing a diagnosis, and hence the patient was referred for surgical evaluation. An 8-mm rigid mediastinoscope was inserted into the anterior mediastinum following the creation of a 2-cm suprasternal skin crease incision and dissection along the anterior surface of the trachea. A large, soft ballotable mass was noted in the right paratracheal region, and aspiration with a 19-gauge needle produced 50 mL of clear fluid. The cyst was entered with the mediastinoscope, and the smooth nature of its wall was noted. The cyst wall was removed through the mediastinoscope by using blunt and sharp dissection. No other mediastinal abnormality was noted. The patient had an uncomplicated 4-hour stay in the hospital. The pathology report described the lesion as a benign mediastinal cyst. No recurrence has been noted at the third month follow-up. A CT scan performed at 1 year (Figure 2) showed no evidence of recurrence.
Figure 1.
Preoperative computed tomographic scan shows right paratracheal mediastinal cyst in patient 1.
Figure 2.
Follow-up computed tomographic scan at 12 months shows no recurrence.
CASE REPORT 2
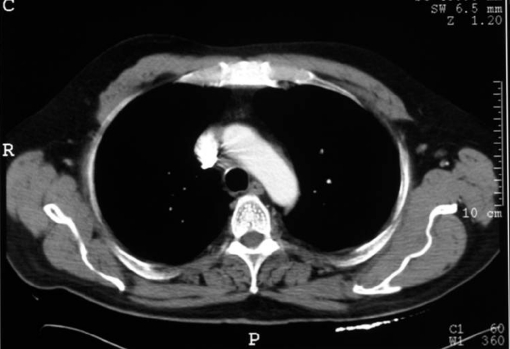
A 73-year-old man had been diagnosed with a mediastinal mass on routine chest x-rays performed at his diabetes clinic. On serial x-rays performed over a 3-year period, an increase was noted in the size of this lesion, and he was referred to the thoracic surgery clinic to exclude a neoplastic process. A CT scan (Figure 3) demonstrated a right paratracheal lesion. His past medical history was significant for a Greenfield filter placement for deep vein thrombosis with pulmonary emboli. He had significant ischemic heart disease and had undergone PTCA 8 years earlier. He was a reformed smoker with a 30-pack/year history. On physical examination, no significant cervical or axillary adenopathy was found, and he had bilateral, normal vesicular breath sounds on auscultation. On mediastinos-copy, a cystic lesion was found and aspiration revealed 45 mL of clear fluid, cytology revealing a few small lymphocytes but no malignant cells. Subtotal excision of the cyst was performed by using blunt and sharp dissection. Histopathology showed a benign mesothelial cyst with a simple cuboidal epithelial lining. No other pathology was identified on mediastinoscopy. No recurrence was noted in 3 months of follow-up (Figure 4).
Figure 3.
Preoperative computed tomographic scan shows large right paratracheal cyst.
Figure 4.
Follow-up computed tomographic scan shows no evidence of recurrence.
DISCUSSION
Mediastinoscopic cyst removal is a minimally invasive method of cyst extirpation. Mediastinoscopy can be performed with a very low morbidity and mortality rate (less than 0.5% in several large series). Standard cervical mediastinoscopy (SCM) as performed by us allows access to the right and left paratracheal areas, the hilar areas, and the carina. These are the most common sites of mediastinal cysts. Malignant mediastinal cysts are extremely rare. Clinical features of infiltration and compression of surrounding structures and the radiological findings alluded to earlier should avoid the potential for a piecemeal extirpation of malignant cysts. Extended cervical mediastinoscopy (ECM) carried out in a prevascular plane in contrast to standard cervical mediastinoscopy (SCM), which is carried out in a pretracheal plane, carries with it a higher risk of recurrent laryngeal nerve and vascular injury. In more than 100 cases of mediastinoscopy performed by the senior author (JMA), we encountered only one vascular injury to the azygos vein. In patients with lesions in the aorto-pulmonary (AP) window, we perform an anterior mediastinotomy, as described by Chamberlain,51 rather than ECM. This allows access to the pleural cavity and allows visualization of the lung at the same time. Cysts in this location are extremely rare. Bronchogenic cysts have been dealt with successfully by mediastinoscopic resections, other foregut cysts including esophageal duplication cysts, more common in the posterior mediastinum, are best dealt with by VATS. A review of recent English literature in the management of mediastinal cysts is shown in Table 1. Though sporadic reports occur in the literature of successful mediastinoscopic cyst removal, dating back to the 1950s, it remains a second-choice procedure to VATS/thoracotomy. Morbidity, recovery times, and discharge times are all prolonged with more invasive procedures vis-à-vis mediastinoscopy. Pursel et al,44 Ginsberg et al,45 and Smythe et al46 in different eras have performed mediastinoscopic cyst excision with success. It however remains an underperformed procedure for what is a fairly common condition (20% of all mediastinal masses). Because most mediastinal cysts occur in the anterosuperior/ middle mediastinum, areas easily accessible to the mediastinoscope, we advocate that mediastinoscopy be attempted for excision of cysts at these locations with more invasive procedures (VATS/thoracotomy) being used for failed mediastinoscopic removal; cysts not accessible to the mediastinoscope; or in situations where mediastinoscopy would be contraindicated (previous mediastinoscopic procedures or suspected malignant cysts with adhesion to surrounding structures). We agree with Smythe and colleagues46 that total excision of the cyst wall might not be accomplished, but removal of greater than 90% of the wall will enable the surrounding tissues to absorb the small amount of fluid secreted by the “marsupialized” cyst wall remnant. It behooves the operating surgeon to perform cytology on the aspirated fluid to exclude occult malignancy before attempting excision. Further, careful follow-up would be indicated to detect and treat a recurrence. All studies to date have not shown any recurrence in follow-ups over periods ranging from 3 months to 2 years.
Table 1.
Management of Mediastinal Cysts: Majority Still Managed by Video-assisted Thoracic Surgery or Thoracotomy
| Series | Year | Technique | N | Location in Mediastinum | Complication | Recurrence |
|---|---|---|---|---|---|---|
| Urschel52 | 1994 | Mediastinoscopy | 3 | Middle | None | none |
| St. George12 | 1991 | Open 65 | 66 | Middle 23 | Vagal injury, Esophageal | |
| Mediastinoscopy 1 | Posterior 43 | laceration, Bronchial laceration | ||||
| Ribet47 | 1995 | Open 68 | 69 | Middle 50 | 1 thoracoscopy converted to open | none |
| Mediastinoscopy 1 | Anterior 19 | |||||
| Roviaro53 | 2000 | VATS | 9 | Middle 5 | Bleeding | none |
| Anterior 4 | ||||||
| Hazelrigg48 | 1993 | VATS | 9 | Anterior 1 | None | none |
| Middle 1 | ||||||
| Posterior 7 | ||||||
| Zambudino54 | 2002 | 4 VATS | 20 | Anterior 17 | Phrenic nerve injury, hemothorax | none |
| 16 Open | Middle 3 | |||||
| Demmy55 | 1998 | VATS | 14 | Middle 7 | Hemorrhage (converted to open) | 1 |
| Posterior 7 | ||||||
| Smythe46 | 1998 | Mediastinoscopy | 3 | Anterior | None | None |
| Cohen56 | 1991 | Open | 45 | Middle and Posterior | NA | NA |
| Cirino57 | 2000 | VATS | 11 | Middle and Posterior | Air leak, Phrenic nerve injury, stellate ganglion injury, diaphragm injury | None |
| Martinod58 | 2000 | VATS | 20 | Middle and Posterior | Bleeding Convert to open in 7 | NA |
| Takeda59 | 2002 | 19 VATS | 105 | All | 3/19 VATS converted to open | NA |
| 81 Open | compartments | |||||
| Davis1 | 1987 | NA | 101 | Anterior 7 | NA | NA |
| Middle 60 | ||||||
| Posterior 34 |
Transcutaneous, transesophageal, and transbronchial aspiration have been attempted in the treatment of benign mediastinal cysts with varied success. While Kuhlman et al42 treated 5 patients successfully with transbronchial/ transesophageal aspiration, Van Beers et al43 noted a symptomatic recurrence of a transbronchially aspirated cyst. If future reports from larger series confirm good results with low recurrence rates, one might adopt this technique to initially treat benign cysts, with mediastinos-copy being used to treat recurrences or failed aspirations due to viscid fluid collections. Until such time, mediastinoscopy should remain the first-choice procedure in the treatment of benign cysts.
References:
- 1. Burkell CC, Cross JM, Kent HP, Nanson EM. Mass lesions of mediastinum. Curr Probl Surg. June 1969;2–57 [PubMed] [Google Scholar]
- 2. Davis RD, Oldham HN, Sabiston DC. Primary cysts and neoplasms of the mediastinum: Recent changes in clinical presentation, methods of diagnosis, management, and results. Ann Thorac Surg. 1987;44:229–237 [DOI] [PubMed] [Google Scholar]
- 3. Petkar M, Vaideeswar P, Deshpande JR, et al. Surgical pathology of cystic lesions of the mediastinum. J Postgrad Med. 2001;47(4):235–239 [PubMed] [Google Scholar]
- 4. Kirwan WO, Walbaum PR, McCormack JM. Cystic intrathoracic derivatives of the foregut and their complications. Thorax. 1973;28:424–428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Salyer DC, Salyer WR, Eggleston JC. Benign developmental cysts of the mediastinum. Arch Pathol Lab Med. 1977;101:136–139 [PubMed] [Google Scholar]
- 6. Fallon M, Gordon ARG, Lendrum AC. Mediastinal cysts of foregut origin associated with vertebral abnormalities. Br J Surg. 1954;41:520–533 [DOI] [PubMed] [Google Scholar]
- 7. Bremer JL. Diverticula and duplications of the intestinal tract. Arch Pathol. 1944;38:132 [Google Scholar]
- 8. O'Rahgilly R, Muller F. Respiratory and alimentary relations in staged human embryos. New embryological data and congenital anomalies. Ann Oto Rhinol Laryngol. 1984;93:421–429 [DOI] [PubMed] [Google Scholar]
- 9. Luck SR, Reynolds M, Raffensburger JG. Congenital broncho-pulmonary malformations. Curr Probl Surg. 1986;23:247–313 [DOI] [PubMed] [Google Scholar]
- 10. Ferguson TB, Jr., Ferguson TB. Congenital lesions of the lung and emphysema. In: Sabiston DC, Jr., Spencer FC. eds. Surgery of the Chest. Vol 1 5th ed. Philadelphia, PA: WB Saunders, 1990;785–789 [Google Scholar]
- 11. Duranceau ACH, Deslauriers J. Foregut cysts of the mediastinum and lung in the adult. In: Shields TW. ed. Mediastinal Surgery. Philadelphia, PA: Lea & Febiger; 1991;305–313 [Google Scholar]
- 12. St. Georges R, Deslauriers J, Duranceau A, et al. Clinical spectrum of bronchogenic cysts of the mediastinum and lung in the adult. Ann Thorac Surg. 1991;52:6–13 [DOI] [PubMed] [Google Scholar]
- 13. Coselli MP, de Ipolyi P, Bloss RS, Diaz RF, Fitzgerald JB. Bronchogenic cysts above and below the diaphragm: report of eight cases. Ann Thorac Surg. 1987;44:491–494 [DOI] [PubMed] [Google Scholar]
- 14. Lapily TC. Cysts and cystic tumors of the mediastinum. Arch Pathol. 1945;127:476–502 [Google Scholar]
- 15. Maier HC. Bronchogenic cysts of mediastinum. Ann Surg. 1948;127:476–502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Snyser ME, Luck SR, Hernandez R, et al. Diagnostic dilemmas of mediastinal cysts. J Pediatr Surg. 1985;90:776–782 [DOI] [PubMed] [Google Scholar]
- 17. Salyer DC, Salyer WR, Eggleston JC. Benign developmental cysts of the mediastinum. Arch Pathol Lab Med. 1977;101:136–139 [PubMed] [Google Scholar]
- 18. Reed JC, Sobonya RE. Morphologic analysis of foregut cysts in the thorax. AJR Am J Roentgenol. 1974;120:851–860 [DOI] [PubMed] [Google Scholar]
- 19. DiLorenzo M, Colin PP, Villancourt R, et al. Bronchogenic cysts. J Pediatr Surg. 1989;24:988–991 [DOI] [PubMed] [Google Scholar]
- 20. Eraklis AJ, Griscom NT, McGovern JB. Bronchogenic cysts of the mediastinum in infancy. N Engl J Med. 1969;281:1150–1154 [DOI] [PubMed] [Google Scholar]
- 21. Bergstrom JF, Yost RV, Ford KT, et al. Unusual roentgen manifestations of bronchogenic cysts. Radiology. 1973;107:49–54 [DOI] [PubMed] [Google Scholar]
- 22. Kirwan WO, Walbaum PR, McCormack RJM. Cystic intrathoracic derivatives of the foregut and their complications. Thorax. 1973;28:424–428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Superina RA, Ein SH, Humphreys RP. Cystic duplications of the esophagus and neurenteric cysts. J Pediatr Surg. 1984;19:527–530 [DOI] [PubMed] [Google Scholar]
- 24. Olsen JB, Clemmensen O, Andersen K. Adenocarcinoma arising in a foregut cyst of the mediastinum. Ann Thorac Surg. 1991;51:497–499 [DOI] [PubMed] [Google Scholar]
- 25. Chuang MT, Barba FA, Kanako M, Teirstein AS. Adenocarcinoma arising in an intrathoracic duplication cyst of foregut origin: a case report and review of literature. Cancer. 1981;47:1887–1890 [DOI] [PubMed] [Google Scholar]
- 26. Tapia RH, White VA. Squamous cell carcinoma arising in a duplication cyst of the esophagus. Am J Gastroenterol. 1985;80:325–329 [PubMed] [Google Scholar]
- 27. Bauer S. Carcinoma arising in a congenital lung cyst. Report of a case. Dis Chest. 1961;40:552–555 [DOI] [PubMed] [Google Scholar]
- 28. Miralles LF, Gonzalez-Martinez B, Luna MS, et al. Carcinoma arising in a calcified bronchogenic cyst. Respiration. 1981;42:135–137 [DOI] [PubMed] [Google Scholar]
- 29. Bernheim J, Griffel B, Versano S, et al. Mediastinal leiomy-osarcoma in the wall of a bronchial cyst [letter]. Arch Pathol Lab Med. 1980;104:221. [PubMed] [Google Scholar]
- 30. Greenfield LJ, Howe JS. Bronchial adenoma within the wall of a bronchogenic cyst. Report of a case. J Thorac Cardioovasc Surg. 1965;49:398–404 [PubMed] [Google Scholar]
- 31. Abell MR. Mediastinal cysts. Arch Pathol. 1956;61:360–379 [PubMed] [Google Scholar]
- 32. Lillie WI, McDonald LR, Clagett OT. Pericardial celomic cysts and pericardial diverticula: a concept of etiology and report of cases. J Thorac Surg. 1950;20:494. [PubMed] [Google Scholar]
- 33. Feigin D, Fenoglio JJ, McAllister HA, et al. Pericardial cysts: a radiologic –pathologic correlation and review. Radiology. 1977;125:15–20 [DOI] [PubMed] [Google Scholar]
- 34. Prader E, Kirschner PA. Pericardial diverticulum. Dis Chest. 1969;55:344–346 [DOI] [PubMed] [Google Scholar]
- 35. Bleger RC, McAdams AJ. Thymic cysts. Arch Pathol. 1966; 82:535–541 [PubMed] [Google Scholar]
- 36. Suster S, Rosai J. Multilocular thymic cyst-An acquired reactive process. Study of eighteen cases. Am J Surg Pathol. 1991; 15:388–398 [PubMed] [Google Scholar]
- 37. Leong AS-Y, Brown JH. Malignant transformation in a thymic cyst. Am J Surg Pathol. 1984;8:471–475 [DOI] [PubMed] [Google Scholar]
- 38. Morinaga S, Nomori H, Kobayashi R, et al. Well differentiated adenocarcinoma arising from mature cystic teratoma of the mediastinum (teratoma with malignant transformation). Report of a surgical case. Am J Clin Pathol. 1994;101:531–534 [DOI] [PubMed] [Google Scholar]
- 39. Wychulis AR, Payne WS, Clagett OT, et al. Surgical treatment of mediastinal tumors. A 40 year experience. J Thorac Cardiovasc Surg. 1971;62:379–392 [PubMed] [Google Scholar]
- 40. Canvasser DA, Naunheim KS. Thoracoscopic management of posterior mediastinal tumors. Chest Surg Clin N Am. 1996;6:53–67 [PubMed] [Google Scholar]
- 41. Kirwan WO, Walbaum PR, McCormack RM. Cystic intrathoracic derivatives of the foregut and their complications. Thorax. 1973;28:424–428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kuhlman JE, Fishman EK, Wang KP, et al. Mediastinal cysts: diagnosis by CT and needle aspiration. AJR Am J Roentgenol. 1988;150:75–78 [DOI] [PubMed] [Google Scholar]
- 43. Van Be, ers B, Trigaux J-P, Weynants P, et al. Foregut cyst of the mediastinum: fluid reaccumulation after transbronchial needle aspiration. Br J Radiol. 1989;62:558–560 [DOI] [PubMed] [Google Scholar]
- 44. Pursel SE, Hershey EA, Day JC, et al. An approach to cystic lesions of the mediastinum via the mediastinoscope. Ann Thorac Surg. 1966;2:752–754 [DOI] [PubMed] [Google Scholar]
- 45. Ginsberg RJ, Atkins RW, Paulson DL. A bronchogenic cyst successfully treated by mediastinoscopy. Ann Thorac Surg. 1972;13:266–268 [DOI] [PubMed] [Google Scholar]
- 46. Smythe WR, Bavaria JE, Kaiser LR. Mediastinoscopic subtotal removal of mediastinal cysts. Chest. 1998;114:614–617 [DOI] [PubMed] [Google Scholar]
- 47. Ribet ME, Copin MC, Gosselin B. Bronchogenic cysts of the mediastinum. J Thorac Cardiovasc Surg. 1995;109:1003–1010 [DOI] [PubMed] [Google Scholar]
- 48. Hazelrigg SR, Landreneau RJ, Mack MJ, et al. Thoracoscopic resection of mediastinal cysts. Ann Thorac Surg. 1993;56:659–660 [DOI] [PubMed] [Google Scholar]
- 49. Landreneau RJ, Pigula F, Luketich JD, et al. Acute and chronic morbidity differences between muscle sparing and standard lateral thoracotomies. J Thorac Cardiovasc Surg. 1996;112:1346–1351 [DOI] [PubMed] [Google Scholar]
- 50. Ashbaugh DG. Mediastinoscopy. Arch Surg. 1970;100:568–573 [DOI] [PubMed] [Google Scholar]
- 51. Olak J. Parasternal mediastinotomy (Chamberlain procedure). Chest Surg Clin N Am. 1996;6:31–40 [PubMed] [Google Scholar]
- 52. Urschel JD, Horan TA. Mediastinoscopic treatment of mediastinal cysts. Ann Thorac Surg. 1994;58(6):1698–1700 [DOI] [PubMed] [Google Scholar]
- 53. Roviaro G, Varoli F, Nucca O, et al. Videothoracoscopic approach to primary mediastinal pathology. Chest. 2000;117:1179–1183 [DOI] [PubMed] [Google Scholar]
- 54. Zambudino AR, Lanzas JT, Calvo MJ, et al. Eur J Cardiothoracic Surg. 22:712–716, 2002 [DOI] [PubMed] [Google Scholar]
- 55. Demmy TL, Krasna MJ, Detterbeck FC, et al. Multicenter VATS experience with mediastinal tumors. Ann Thorac Surg. 1998;66:187–192 [DOI] [PubMed] [Google Scholar]
- 56. Cohen AM, Thompson L, Edwards FH. Primary cysts and tumors of the mediastinum. Ann thorac Surg. 1991;51:378–386 [DOI] [PubMed] [Google Scholar]
- 57. Cirino LM, Campos JR, Fernandez A, et al. Diagnosis and treatment of mediastinal tumors by thoracoscopy. Chest. 2000; 117:1787–1792 [DOI] [PubMed] [Google Scholar]
- 58. Martinod E, Pons F, Azorin J, et al. Thoracoscopic excision of mediastinal cysts: Results in 20 cases. Ann Thorac Surg. 2000; 69:1525–1528 [DOI] [PubMed] [Google Scholar]
- 59. Takeda S, Miyoshi S, Minami M, et al. Clinical spectrum of mediastinal cysts. Chest. 2003;124:125–132 [DOI] [PubMed] [Google Scholar]