Abstract
Objectives:
This study was undertaken to determine the actual amount of time a dynamic fluoroscopic intraoperative cholangiogram adds to a laparoscopic cholecystectomy. A secondary objective was to define the information gained from this procedure.
Methods:
A consecutive case study of 52 patients undergoing laparoscopic cholecystectomy was used. Time was recorded from placement of a laparoscopic hemoclip across the cystic duct at its junction with the gallbladder until successful completion of the intraoperative cholangiogram. The mean, median, and range of times for these cases, as well as the results and false-negative rates, were determined.
Results:
Cholangiography was successfully completed in 96% of patients. The mean time added to laparoscopic cholecystectomy by the addition of dynamic fluoroscopic intraoperative cholangiography was 4.3 minutes. The median time was 3.0 minutes. The times ranged from 2.0 minutes to 16.0 minutes. Choledocholithiasis was present in 15.4% of these patients. The false-positive rate was zero in this study.
Conclusions:
Dynamic fluoroscopic intraoperative cholangiogram was fast and efficient. The information gained was significant in that 15% of patients proceeded on to laparoscopic common bile duct exploration. We conclude that intraoperative cholangiography should be a routine addition to laparoscopic cholecystectomy.
Keywords: Laparoscopic cholecystectomy, Intraoperative cholangiogram, Laparoscopic common bile duct exploration, Choledocholithiasis
INTRODUCTION
The advent of laparoscopic cholecystectomy (LC) revolutionized the care of patients with cholelithiasis. However, after its early introduction, it became clear that LC had its own unique complications. The most significant complication was that the rates of common bile duct (CBD) injuries were 2 times to 15 times higher than those identified in the era of open cholecystectomy.1,2 Unfortunately, despite the widespread application of LC, it appears that the rate of injury continues to remain about 1.4%.3 Injury to the CBD is an important source of patient morbidity, and it is associated with a mortality of 11%.4 It is also the leading cause of malpractice suits against general surgeons.5,6 The median jury award for a CBD injury is $500,000.7
Intraoperative cholangiography (IOC), which was first introduced into clinical practice by Mirizzi8 in the 1930s, is thought to prevent CBD injury during cholecystectomy. In the era of open cholecystectomy, it was used to detect CBD stones. However, in the era of laparoscopy, it acts to provide valuable anatomical delineation of the biliary system. It can assist in providing an early clue to prevent surgical misperception of the CBD as the cystic duct.9,10 The application of IOC has been debated extensively in the literature with some surgeons advocating its routine use.11,12 However, other surgeons advocate only selective use of cholangiography.13,14 We undertook this study to determine the actual time that dynamic fluoroscopic intraoperative cholangiography (DFIOC) adds to an LC.
METHODS
This prospective study was conducted at Eastern New Mexico Medical Center in Roswell, New Mexico. Fifty-two consecutive LCs were performed with DFIOC. These cases were cataloged and time values were recorded. The time was recorded from the placement of the laparoscopic hemoclip across the junction of the gallbladder with the cystic duct until the successful completion of the DFIOC by adequate imaging of the entire biliary system. We calculated the mean, median, and range of times required for successful completion of the DFIOC. All procedures were performed by 1 of 3 experienced laparoscopic surgeons. Surgical residents did not participate in any of these studies. Procedures were done in the surgeon's routine fashion with the only change to our technique being the addition of a stopwatch to time the procedure. The technologists from the radiology department who provide 24-hour coverage to the operating room were responsible for timing the procedure and collecting data. Data collected included the presence or absence of choledocholithiasis, the actual amount of fluoroscopy time used in each procedure, and whether the procedure was an urgent or elective case. Urgent cases were defined as those patients admitted directly to the hospital with acute symptoms and having their surgery during that admission. Elective cases were patients scheduled for surgery through our medical office. Additionally, we determined whether any of the cases of choledocholithiasis represented false-positive results. No internal review board approval was sought for this study.
Technique for Dynamic Fluoroscopic Intraoperative Cholangiogram
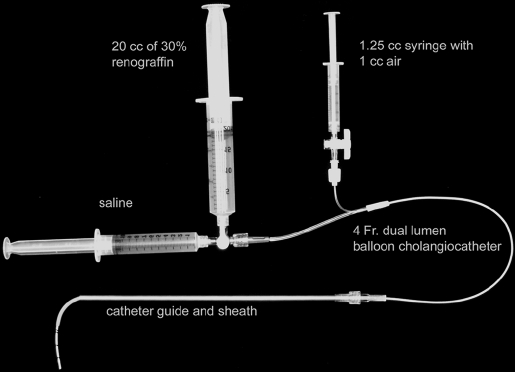
A standard technique was adopted by all surgeons participating in the study. The cystic duct at its junction with the gallbladder was first identified. A laparoscopic hemoclip was placed across this junction. We started timing from this point onward. A cystic ductotomy was then performed by using sharp disposable laparoscopic scissors. The operating room technician had already prepared a 4-French dual lumen Arrow Karlan balloon cholangiocatheter. A 1.25-mL syringe filled with 1 mL of air was connected to the balloon lumen with a 2-way stopcock. A 3-way stopcock was connected to the open lumen of the cholangiocatheter. A 20-mL syringe filled with saline was connected to the straight end of the stopcock and a 20-mL syringe filled with 30% renografin contrast was connected to the 90-degree side of the stopcock. The catheter was preflushed with saline to eliminate any air bubbles, and the stopcock was turned off toward the open lumen to prevent any air bubbles from entering the cholangiocatheter (Figure 1). The cholangiocatheter was then threaded through the curved American Catheter guide. The guide was deployed through a 5-mm stainless steel sheath. The assembly of the catheter, guide, and sheath was then introduced into the peritoneal cavity through a 10-mm laparoscopic port positioned in the epigastrium. The curved guide was withdrawn into the sheath for insertion through the laparoscopic port. The guide was then extended from the sheath to allow introduction of the cholangiocatheter into the cystic duct at any angle between 0 and 90 degrees (Figure 2). At this point in time, a brief inflation-deflation cycle of the balloon at the tip of the cholangiocatheter was often done to help the catheter traverse the spiral valves. If stones were lodged in the cystic duct, these were milked out through the cystic ductotomy. If the cholangiocatheter could not be introduced into the cystic duct at the point of initial cystic ductotomy, further dissection of the cystic duct toward the CBD was carried out, and a second cystic ductotomy was made closer to the junction of the cystic and CBD. The cholangiogram was performed with a balloon holding the catheter in position, either in the cystic duct or more commonly in the CBD. Flow was checked by first infusing saline. The C arm was positioned over the CBD by using the hemoclip placed at the junction of the gallbladder and cystic duct as a reference for initial positioning of the C arm. Fluoroscopy was begun as the contrast medium was injected and a dynamic study of the hepatobiliary tree obtained. The images were interpreted real time by the surgeons performing the procedure. Timing was stopped when the surgeons deemed that an adequate study had been obtained. An adequate study was defined as imaging the Ampulla of Vater, the CBD, the common hepatic duct (CHD), and the confluence of the right and left hepatic ducts with sufficient detail to define the anatomy and to identify any stones.
Figure 1.
Cholangiocatheter set-up standardized for dynamic fluoroscopic intraoperative cholangiography.
Figure 2.
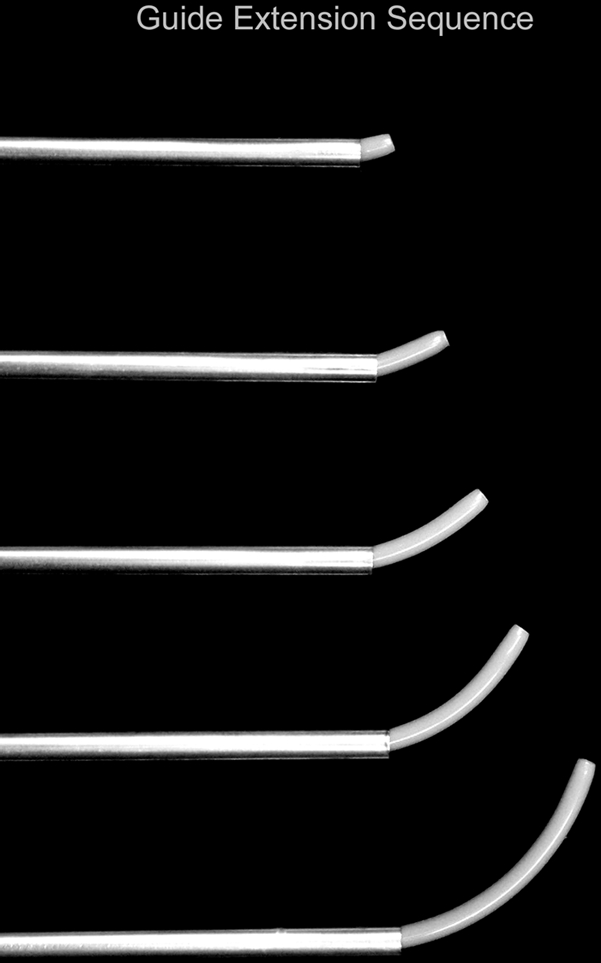
Guide extension sequence showing changing angle of guide tip as guide is extended from sheath.
RESULTS
The study showed that the mean time added by DFIOC to the procedure was 4.3 minutes. The median time was 3 minutes. The times ranged from 2.0 minutes to 17 minutes. Average fluoroscopy time was 39 seconds. Of note, in 15.4% of the cases (8/52), the study identified stones within the CBD. No false-positive studies existed. All cases of choledocholithiasis were successfully treated with LCBDE techniques. A successful DFIOC was obtained in 50/52 patients for a 96% success rate. The 2 failures were attributed to an excessively narrow cystic duct that would not allow the cholangiocatheter to advance into the cystic duct. No cases of bile duct injury occurred during this study. No complications associated with the performance of the DFIOC occurred. The actual cost to the hospital for the balloon cholangiocatheter used in this study was $39.90, and the catheter guide and sheath cost $19.60.
DISCUSSION
A previous study estimated that cholangiography added 10 minutes to the operating room time and $675 in cost.15 The protective effect of cholangiography in preventing CBD injury is significant. Kullman and associates16 showed in their series of 513 cholangiograms that 98 (19%) had anatomical aberrations. Performing IOC may prevent the errors of cognition that lead to CBD injury.17 A cohort analysis of Medicare patients undergoing cholecystectomy from 1992 to 1999 showed that not using an IOC during cholecystectomy was associated with a 50% to 70% increase in CBD injury.18 Interestingly enough, a study done in Western Australia during the early 1990s, also found a reduction close to 50%.19 The use of IOC in the prevention of CBD injury has also been evaluated by using a cost-effectiveness analysis.20 This study showed that the routine use of IOC would add about $100 more per case. However, it would also prevent 2.5 deaths for every 10,000 patients at a savings of almost $400,000 per life saved.
Preoperative liver function tests and ultrasound have only a 30% predictive value in identifying cases of choledocholithiasis.21 Rather than exposing 70% of these patients to an unnecessary ERCP, it is our practice to identify patients with choledocholithiasis by DFIOC. We use LCBDE at the same time as LC to remediate this problem. This has been shown to be the most cost-effective approach to choledocholithiasis.22
CONCLUSION
We have found DFIOC to be fast and efficient, adding a mean time of 4.3 minutes to the LC procedure. DFIOC provided valuable information by identifying choledocholithiasis in 15% of our patients. Patient management was influenced by the DFIOC as patients with choledocholithiasis proceeded on to LCBDE. Another worrisome finding was the fact that we had several additional patients in whom stones were extracted from the cystic duct in the process of performing the DFIOC. These stones would have been left behind in the cystic duct remnant if cholangiography had not been attempted. The long-term consequence of these retained cystic duct stones is unknown. Our study design did not rigorously quantitate these numbers. No cases of bile duct injury occurred during our series; however, the relatively small number of cases52 and the infrequency of this complication do not allow us to draw any conclusions about DFIOC, enhancing the safety of LC. We had no cases of a false-positive DFIOC leading to an unnecessary LCBDE. We had no complications resulting from the performance of the DFIOC.
It is our contention that the benefits of routine DFIOC far outweigh its drawbacks. We feel the information gained from DFIOC is well worth the 4.3-minute mean time that DFIOC takes.
Contributor Information
Donald E. Wenner, Eastern New Mexico Medical Center, Roswell, New Mexico, USA..
Paul Whitwam, Eastern New Mexico Medical Center, Roswell, New Mexico, USA..
David Turner, Eastern New Mexico Medical Center, Roswell, New Mexico, USA..
Kathy Kennedy, Radiology Practitioner Assistant Student, Weber State University, Ogden, Utah, USA..
Syed Hashmi, Lincoln County Medical Center, Ruidoso, New Mexico, USA..
References:
- 1. Bernard HR, Hartman TW. Complications after laparoscopic cholecystectomy. Am J Surg. 1993;165:533–535 [DOI] [PubMed] [Google Scholar]
- 2. Gouma DJ, Go PM. Bile duct injury during laparoscopic and conventional cholecystectomy. J Am Coll Surg. 1994;178:229–233 [PubMed] [Google Scholar]
- 3. Calvete J, Sabater L, Camps B, et al. Bile duct injury during laparoscopic cholecystectomy: myth or reality of the learning curve? Surg Endosc. 2000;14:608–611 [DOI] [PubMed] [Google Scholar]
- 4. Kern KA. Medicolegal analysis of bile duct injury during open cholecystectomy and abdominal surgery. Am J Surg. 1994; 168:217–222 [DOI] [PubMed] [Google Scholar]
- 5.Physicians Insurers Association of America Exhibit 6. In: Risk Management Review for General Surgery 2000. Rockville, MD: Physician Insurers Association of America; 2000:15 [Google Scholar]
- 6.Physicians In surers Association of America Table 4. In: Laparoscopic Injury Study 2000. Rockville, MD: Physician Insurers Association of America; 2000:11 [Google Scholar]
- 7. Carroll BJ, Birth M, Phillips EH. Common bile duct injuries during laparoscopic cholecystectomy that result in litigation. Surg Endosc. 1998;12:310–314 [DOI] [PubMed] [Google Scholar]
- 8. Mirrizzi PL. Operative cholangiography. Surg Gynecol Obstet. 1937;65:702–710 [Google Scholar]
- 9. Woods MS, Traverso LW, Kozarek RA, et al. Characteristics of biliary tract complications during laparoscopic cholecystectomy: a multi-institutional study. Am J Surg. 1994;167:27–33 [DOI] [PubMed] [Google Scholar]
- 10. Woods MS, Traverso LW, Kozarek RA, et al. Biliary tract complications of laparoscopic cholecystectomy are detected more frequently with routine intraoperative cholangiography. Surg Endosc. 1995;9:1076–1080 [DOI] [PubMed] [Google Scholar]
- 11. Soper NJ, Brunt LM. The case for routine operative cholangiography during laparoscopic cholecystectomy. Surg Clin North Am. 1994;74:953–959 [PubMed] [Google Scholar]
- 12. Vezakis A, Davides P, Ammori BJ, Martin IG, Larvin M, McMahon MJ. Intraoperative cholangiography during laparoscopic cholecystectomy. Surg Endosc. 2000;14:118–122 [DOI] [PubMed] [Google Scholar]
- 13. Ladosci LT, Benitz LD, Filippone DR, Nance FC. Intraoperative cholangiography and laparoscopic cholecystectomy: a review of 734 consecutive cases. Am Surg. 1997;63:150–156 [PubMed] [Google Scholar]
- 14. Wright KD, Wellwood JM. Bile duct injury during laparoscopic cholecystectomy without operative cholangiography. Br J Surg 1998;85:191–194 [DOI] [PubMed] [Google Scholar]
- 15. Podnos YD, Gelfand DV, Dulkanchainun TS. Is intraoperative cholangiography during laparoscopic cholecystectomy cost effective? Am J Surg. 2001;182:663–669 [DOI] [PubMed] [Google Scholar]
- 16. Kullman E, Borch K, Lindstrom J, Svanik J, Anderberg B. Value of routine intraoperative cholangiography in detecting aberrant bile ducts and bile duct injuries during laparoscopic cholecystectomy. Br J Surg. 1996;83:171–175 [PubMed] [Google Scholar]
- 17. Way LW, Stewart L, Gantert W, et al. Causes and prevention of laparoscopic bile duct injuries: an analysis of 252 from a human factors and cognitive psychology perspective. Ann Surg. 2003;237:460–469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Flum DR, Dellinger EP, Cheadle A, Chan L, Koepsell T. Intraoperative cholangiography and risk of common bile duct injury during cholecystectomy. JAMA. 2003;289:1639–1644 [DOI] [PubMed] [Google Scholar]
- 19. Fletcher DR, Hobbs MS, Tan P, et al. Complications of cholecystectomy: risks of the laparoscopic approach and the protective effects of operative cholangiography: a population-based study. Ann Surg. 1999;229:449–457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Flum DR, Flowers C, Veenstra DL. A cost-effectiveness analysis of intraoperative cholangiography in the prevention of bile duct injury due to laparoscopic cholecystectomy. J Am Coll Surg. 2003;196:385–393 [DOI] [PubMed] [Google Scholar]
- 21. Koo K, Traverso LW. Do preoperative indicators predict the presence of common bile duct stones during laparoscopic cholecystectomy? Am J Surg. 1996;171:495–499 [DOI] [PubMed] [Google Scholar]
- 22. Urbach DR, Khajanchee YS, Jobe BA, et al. Cost effective analysis of common bile duct stones: a decision analysis of the use of endoscopic retrograde cholangiopancreatography (ERCP), intraoperative cholangiography, and laparoscopic bile duct exploration. Surg Endosc. 2001;15:4–13 [DOI] [PubMed] [Google Scholar]