Abstract
Objective:
We reviewed the long-term results and patient survival for laparoscopic-assisted resection of colorectal malignancies. The place of laparoscopic colectomy for colorectal carcinomas is controversial. The techniques and expected surgical outcomes for patients undergoing laparoscopic and laparoscopic-assisted colectomies are being defined as these procedures become more acceptable and reach parity with, or even surpass, results of traditional operations. Anecdotal reports in the literature describe port-site and incisional tumor implantation in patients undergoing laparoscopic-assisted colectomies for colorectal malignancies. This raises concerns about whether these incisional tumor sites are more common in these patients and whether their survival is compromised by the laparoscopic technique.
Methods:
The authors reviewed data from 110 patients who underwent laparoscopic-assisted colectomies for colorectal cancer to determine the long-term results and survival and to compare the safety and efficacy of laparoscopic-assisted colectomy to the safety and efficacy of open colectomy. Between July 1991 and June 1999, 350 patients underwent laparoscopic-assisted colectomies. Of these, 110 patients had colorectal malignancies. Survival rates and patterns of recurrence were compared within the various TNM stages and compared with conventional data after open surgery. The American Joint Committee on Cancer staging for colorectal carcinomas and the Kaplan-Meier method were used to determine the survival curves.
Results:
Laparoscopic-assisted colon resections for colorectal malignancies were performed in 110 patients. Fifty-one percent of the patients were women, and 49% percent were men, with a mean age of 78.17 years. The mean follow-up was 43 months. Thirteen patients were converted to open operation due to various difficulties encountered during the procedure. Mean operative time was 128.16 minutes, and mean hospital stay was 6.91 days. Perioperative mortality was 2.77%. There were 4 local recurrences. The ten-year survival rates for the various stages were 78% for stage I, 33% for stage II, 30% for stage III, and 0% for stage IV. No port-site implantations occurred.
Conclusion:
Laparoscopic-assisted colon resection of colorectal carcinomas is technically feasible and safe. It allows earlier postoperative recovery and a shorter hospital stay. The long-term survival is also satisfactory. The incidence of port-site implants is no more than that with the conventional open technique. Determination of any benefits over the conventional open technique, however, still await prospective randomized trials.
Keywords: Laparoscopic colon resections, Laparoscopic-assisted colon resections, Colorectal malignancies
INTRODUCTION
In recent years, laparoscopic surgery has become a matter of growing interest.1 Since its introduction in the late 1980s and the subsequent recognition of its potential advantages, minimally invasive surgery has been applied to almost all areas of abdominal surgery.2 Laparoscopic techniques have been applied to a variety of benign colorectal conditions, including inflammatory and diverticular disease.3 These successes have prompted the development of laparoscopic techniques for the resection of colorectal malignancies.3
Fowler et al4 reported one of the earliest laparoscopic sigmoid resections in 1991. Since then, numerous authors have demonstrated the feasibility and safety of laparoscopic colon surgery.2 Techniques range from full laparoscopic procedures including intracorporeal resection and anastomosis, to laparoscopic-assisted procedures, where a portion of the procedure is done extracorporeally.3 Potential short-term benefits of laparoscopic colectomies include faster recovery of pulmonary function, less pain from smaller incisions, reduced ileus, lower rate of wound complications, and more rapid mobilization of patients leading to a shorter hospital stay and quicker return to normal activities–to which has been added lower hospital costs and improved cosmesis.3,5 These benefits make laparoscopic colectomy a very attractive option. However, the surgical community has not accepted it in the same way as it has accepted laparoscopic cholecystectomy. Acceptance in colorectal malignancies, especially for operations with curative intent, is controversial.6 This controversy has been fueled by the well-publicized anecdotal reports of port-site tumor implantations.7 Other controversies include long-term survival and adequacy of re-section.1 Further, it has been suggested that cancer cells can be spread at the time of the laparoscopic resection, through the misuse of instruments, detrimental effects of CO2 pneumoperitoneum, or movement of cell laden fluid.7 However, emerging data show benefits for patients treated laparoscopically for colon and rectal adenocarcinomas.7
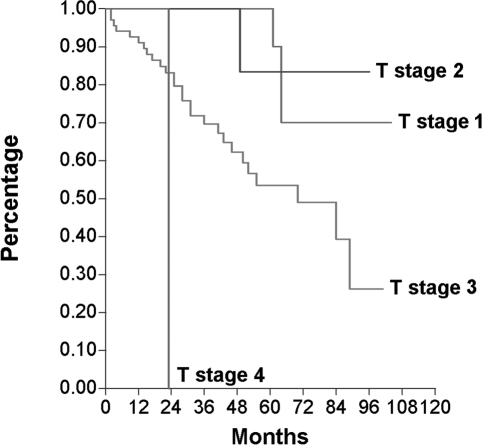
Figure 1.
Kaplan-Meier survival curves per tumor stage.
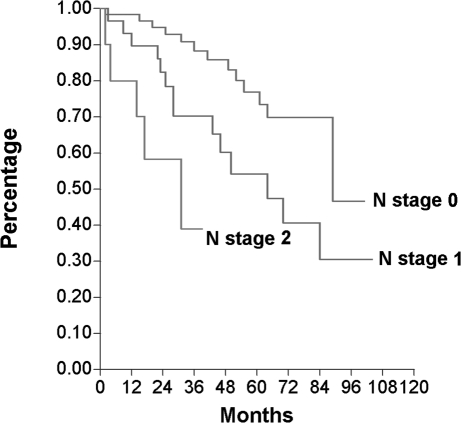
Figure 2.
Kaplan-Meier survival curves per node status.
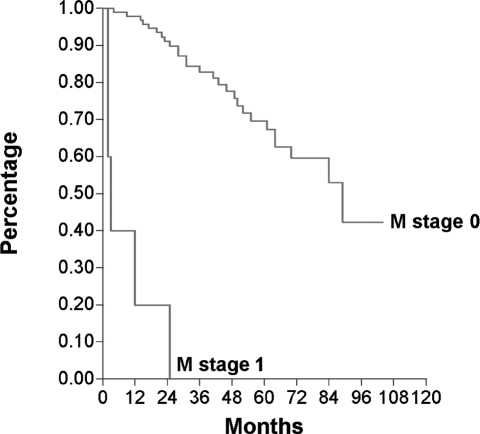
Figure 3.
Kaplan-Meier survival curves per metastasis stage.
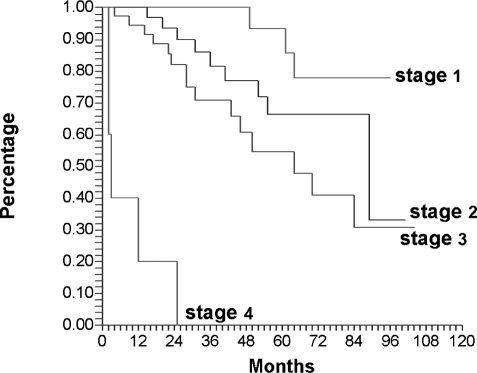
Figure 4.
Kaplan-Meier survival curves per AJCC stage. Stage 1 range, 72–74%; stage 2 range 54 – 63%; stage 3 range, 39 – 46%; stage 4 range, 6 –7%. Adapted from Beart RW, Steele GD Jr, Menck HR, Chmiel JS, Ocwieja KE, Winchester DP. Management and survival of patients with adenocarcinoma of the colon and rectum: a national survey of the Commission on Cancer. J Am Coll Surg. 1995;181:225–236.
Several recent reports exist describing wound tumor implantations after open colectomies, but only 2 large series report an incidence of 1% and 1.5%.8,9 Very limited reports exist on long-term survival for these patients. The purpose of our study was to define the survival curves in a cohort of consecutive patients who underwent laparoscopic resection of colorectal malignancies and to review the literature.
METHODS
The charts of 350 consecutive patients who underwent laparoscopic-assisted colon resections for both benign and malignant disease of the colon between July 1991 and June 1999 were reviewed retrospectively. These charts also included attempted laparoscopic procedures that were converted to open operations. Inpatient and outpatient records were reviewed for patient demographics, (including age, sex, and associated co-morbidities) as well as the details of the operation, (including procedure performed, indication and duration of operation, intraoperative and postoperative complications, conversion to open procedure, time taken to resumption of diet and length of hospital stay). The follow-up was also reviewed including complications and recurrences. All these data were then compared with our open colectomy data obtained from our database for colorectal carcinomas accrued before we started performing laparoscopic-assisted colectomies.
All patients underwent laparoscopic-assisted resections, with the mobilization performed laparoscopically, and the resection and anastomosis accomplished extracorporeally. No special precaution was taken to remove the specimen. Total operative time was defined as the time from initial incision to completion of closure. Operative records were reviewed for total blood loss and the need for blood transfusion. Diet was initiated on return of bowel function, starting from fluids, and advancing as tolerated. The patients were discharged home when they were passing flatus or stool, or both, tolerating a soft or regular diet, and receiving adequate relief from oral pain medications. Discharge criteria however were not strictly enforced, and patients were sometimes allowed to stay longer, even after achieving these goals.
All patients were staged postoperatively, using the American Joint Committee of Cancer staging system (TNM classification) as stage I, II, III, and IV. The TNM classification for cancer of the colon and rectum was modified in 1988 to correspond directly to the Dukes classification, which is often used to estimate the prognosis of the disease (8/15). The survival rates for all stages were determined using the Kaplan-Meier curve. Estimates for overall 2-year, 5-year, and 10-year survival were calculated from the values used to determine the Kaplan-Meier curves.
RESULTS
Starting from July 1991, 350 laparoscopic-assisted colon resections were performed. Of these, 240 were for benign disease, while 110 were for malignant disease. Of the 110 patients with malignancy, 50.9% were female. The mean age was 78.17(standard deviation of 11.3 years; range, 54 to 91 years). There were 4 abdominoperineal resections, 6 low anterior resections, 5 transverse colectomies, 8 left hemicolectomies, 25 sigmoid resections, and 62 right hemicolectomies.
The margins and lymph nodes obtained were also reviewed in this study. The mean proximal margin was 8.57 cm (SD, 5.52 cm; range, 1 cm to 31 cm), while the distal margin was 8.23 cm (SD, 5.5 cm; range, 1cm to 33cm). The mean number of lymph nodes obtained were 10.75 (SD, 6.8; range, 0 to 37), and the number of positive lymph nodes was mean 1.46 (SD, 2.93; range, 0 to 21).
The conversion rate was 11.81% (13 patients). Conversion was defined as inability to mobilize the colon laparoscopically. The reason for conversion included adhesions (6 patients), technical difficulty (5 patients), and unexpected findings (2 patients). The mean operative time was 128.16 minutes (SD, 69.9; range, 35 to 495). In our open colectomy database, the mean operative time was 155 minutes.
The mean time for resumption of a clear fluid diet was 2.28 days (SD, 1.37; range, 1 to 8 days); while a regular diet was tolerated in 4.21 days (SD, 2.34; range, 2 to 15 days). Mean length of hospital stay was 6.91 days (SD, 4.24; range, 2 to 25 days). In our open colectomy database, the mean time to starting a clear diet was 3.9 days, and mean hospital stay was 12.5 days.
The perioperative mortality was 2.77% (3 patients). Two patients succumbed to their metastatic disease, while 1 patient died of complications of pneumonia. Table 1 lists the 23 complications that occurred. Of these, 7 necessitated surgical intervention. One had intraabdominal bleeding, requiring return to the operating room, while 1 bladder injury and 3 small bowel injuries were identified and repaired laparoscopically at the same time as the primary surgery. Two patients had intraabdominal abscesses and required a re-exploration.
Table 1.
Complications
| Complication | Number | Comments | Due to LAC* |
|---|---|---|---|
| Deaths† | 3 | No | |
| Bleeding | 1 | Required reoperation | Yes |
| Bladder injury | 1 | Repaired intraoperatively | Yes |
| Small bowel injury | 3 | Repaired intraoperatively | Yes |
| Pneumonia | 1 | No | |
| Wound infection | 1 | No | |
| Hypotension | 1 | No | |
| Small bowel obstruction | 1 | Unknown | |
| Intraabdominal abscesses | 2 | Required reoperation | No |
| Urinary tract infection | 4 | No | |
| Ileus | 8 | Unknown |
LAC = laparoscopic assisted colectomy.
Two patients succumbed to their metastatic disease; 1 patient died of complications of pneumonia.
There were 4 local recurrences, 3 after right colectomies and 1 after a left colectomy. No port-site recurrences were observed.
Follow-up data were available for 104 patients. Twenty-six patients had Stage I disease, 34 had Stage II, 35 had Stage III, and 9 had Stage IV disease. The mean follow-up for all patients was 43 months (SD 36.5; range, 1 to 104). As determined by the Kaplan-Meier curves, the 2-year, 5-year, and 8-year survival for these patients was stage I (100%, 94%, 78%), stage II (94%, 66%, 33%), stage III (82%, 55%, 30%), and stage IV (20%, 0%, 0%). For the TNM staging, the 5- and 8-year survival for the lesion was T1 (100% and 82%), T2 (84% and 70%), T3 (54% and 26%); there were no 5- or 8-year survivors for T4 lesions. For nodal disease, the 5- and 8-year survival was N0 (70% and 46%), N1 (44% and 30%) with no survivors for N2. Similarly, the 5- and 8-year survival for patients with no metastatic disease was 70% and 42%, respectively. There were no survivors of metastatic disease.
DISCUSSION
Laparoscopic cholecystectomy has been widely accepted by surgeons because of its minimally invasive nature and physiologic, perioperative benefits. However, the application of laparoscopic surgery for colorectal malignancies is still controversial because for any malignancy the long-term benefits are more important than the benefits obtained in the immediate postoperative period. If we can demonstrate that the long-term survival achieved by laparoscopic procedures is no less than that achieved by the conventional open technique, that result in itself should be sufficient to establish the advantage of laparoscopic and laparoscopic-assisted resections of colorectal malignancies.
Like other laparoscopic operations, laparoscopic colectomies offer many short-term benefits to patients. These include less pain, reduced ileus with earlier resumption of diet, shorter hospital stay, and more rapid return to a functional status. In our series of 110 patients, the patients were started on a diet earlier in the laparoscopic group, with an earlier discharge from the hospital.
Our overall conversion rate of 11.81% was comparable to conversion rates reported in other series. Our operative time was less than that for open colectomies. Of 3 perioperative mortalities, none was directly related to the laparoscopic procedure itself. The complications, of small bowel injury in 3 patients and bladder injury in 1 patient, though directly related to the laparoscopic procedure, was recognized immediately and repaired laparoscopically.
On follow-up, the 5-year survival for each stage is no different in the laparoscopic data as compared to the data obtained from open series.10 They compare stage-to-stage, Stage I (94% vs 72% to 74%), Stage II (66% vs 54% to 63%), Stage III (55% vs 39% to 46%), and Stage IV (0% vs 6% to 7%).
Port-site tumor implantations have been a matter of much concern with laparoscopic and laparoscopic-assisted colectomies. However, this may just represent an underestimation of wound implants in open techniques or an overestimation in laparoscopic surgery, wherein port-site “recurrences” just represent a part of widespread metastases. In our series, we had no trocar-site or incisional implants. This correlates well with other series that report port-site implants of approximately 1% or less, which is about the same as the wound tumor implantation rate of 0.6% to 1.5% reported for open procedures.
Despite a few contradictory reports, most clinical and experimental studies support the view that laparoscopic surgery is associated with better preservation of immune function.11 The minimal access technique is believed to produce an attenuated metabolic stress response and represents a milder challenge to the immune response.11,12 This beneficial trait is purportedly related to the smaller incision. Theoretically, in the long-term, the better immune status in the early postoperative period will translate into longer survival for patients with cancer.6
CONCLUSION
Laparoscopic-assisted colectomy for colorectal malignancies is a technically feasible procedure that can be performed effectively and safely, with a superior quality of life outcome. The learning curve is still an ongoing process and depends on the level of competence of the surgeon and operating room staff. In our review of 110 operations performed at our institution during the study period, we have demonstrated an acceptable outcome concerning conversion rates, mortality, morbidity, and hospital stay. Also, the survival curves for patients with colorectal malignancies undergoing laparoscopic-assisted resections do not differ negatively from the results of conventional open surgery. Short-term results are favorable to those of laparoscopic-assisted colectomies; however, final answers await longer follow-up and results of prospective randomized trials.
References:
- 1. Gibson M, Byrd C, Pierce C, et al. Laparoscopic colon resections: a five-year retrospective review. Am Surg. 2000;66:245–249 [PubMed] [Google Scholar]
- 2. Faynsod M, Stamos MJ, Arnell T, Borden C, Udani S, Vargas H. A case-control study of laparoscopic versus open sigmoid colectomy for diverticulitis. Am Surg. 2000;66(9):841–843 [PubMed] [Google Scholar]
- 3. Chapman A, Levitt MD, Hewett P, Woods R, Sheiner H, Maddern GJ. Laparoscopic-assisted resection of colorectal malignancies. Ann Surg. 2001;234(5):590–600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fowler DL, White SA, Anderson CA. Surg Laparosc Endosc. 5(6):468–471, 1996 [PubMed] [Google Scholar]
- 5. Hoffman GC, Baker JW, Doxey JB, Hubbard W, Ruffin WK, Wishner JA. Minimally invasive surgery for colorectal cancer: Initial follow-up. Ann Surg. 1996;223(6):790–798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Leung KL, Yiu RYC, Lai BS, Lee JFY, Thung KH, Lau WY. Laparoscopic-assisted resection of colorectal carcinoma: Five-year audit. Dis Colon Rectum. 1999;42(3):327–333 [DOI] [PubMed] [Google Scholar]
- 7. Paulin EC, Mamozza J, Schlachta C, Gregoire R, Roy N. Laparoscopic resection does not adversely affect early survival curves in patients undergoing surgery for colorectal adenocarcinoma. Ann Surg. 1999;229(4):487–492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hughes ES, McDermott FT, Polglase AL, Johnson WR. Tumor recurrence in the abdominal wall scar tissue after large-bowel cancer surgery. Dis Colon Rectum. 1983;26:571–572 [DOI] [PubMed] [Google Scholar]
- 9. Reilly WT, Nelson H, Schroeder G, Wieand HS, Bolton J, O'Connell MJ. Wound recurrence following conventional treatment of colorectal cancer: a rare but perhaps underestimated problem. Dis Colon Rectum. 1996;39:200–207 [DOI] [PubMed] [Google Scholar]
- 10. Beart RW, Steele GD, Jr., Menck HR, Chmiel JS, Ocwieja KE, Winchester DP. Management and survival of patients with adenocarcinoma of the colon and rectum: a national survey of the Commission on Cancer. J Am Coll Surg. 1995;181(3):225–236 [PubMed] [Google Scholar]
- 11. Vittemberga FJ, Jr, Foley DP, Meyers WC, Callery MP. Laparoscopic surgery and the systemic immune response. Ann Surg. 1998;227(3):326–334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gupta A, Watson DI. Effect of laparoscopy on immune function. Br J Surg. 2001;88:1296–1306 [DOI] [PubMed] [Google Scholar]