Abstract
Objectives:
This study aimed to determine whether advanced age or sex was predictive of adverse outcomes after Roux-en-Y gastric bypass.
Methods:
The Pennsylvania State Discharge Database was searched for records of morbidly obese patients who underwent Roux-en-Y gastric bypass. The SASs MIXED Procedure was used to test whether mortality alone or adverse outcomes (postoperative complications, nonroutine hospital transfer and mortality) were significantly related to sex or advanced age (>50 years). The presence of comorbidities was used as a blocking variable.
Results:
Between 1999 and 2001, 4,685 patients underwent Roux-en-Y gastric bypass in Pennsylvania, of which 82% were female and 20% were older than 50 years of age. Comorbidities were present in 71% of patients. Twenty-eight deaths (0.6%) and 813 adverse outcomes (17.4%) occurred. Mortality was greater in males than in females (1.2% vs. 0.47%, P<0.05) without comorbid interaction. Mortality did not increase with age. Adverse outcomes were related to both sexes (24% male, 16% female, P<0.05) and age (≤50, 16% vs. >50, 23%, P<0.05) with a small comorbid interaction.
Conclusion:
Adverse outcomes are more frequent among males and older patients and are influenced by comorbidities. Male patients have a higher mortality that was not affected by the presence of comorbidities.
Keywords: Gastric bypass, Age, Sex, Adverse outcome
INTRODUCTION
Obesity has reached epidemic proportions in the United States and has become a major health problem estimated to account for approximately 280,000 deaths per year.1 Bariatric surgery has been proven to be the most effective treatment of refractory morbid obesity. Roux-en-Y gastric bypass (RYGB) appears to offer the best long-term results, and the demand for this procedure has increased dramatically the last decade.2 The elective nature of this procedure mandates a low risk/benefit ratio. Identification of risk factors that predict adverse outcomes after RYGB and preoperative risk stratification is an integral part of patient education and selection and ultimately leads to improved patient satisfaction. Hypertension, sleep apnea, advanced age, sex, and surgeon's experience have all been associated with adverse outcome after RYGB in recent studies.3–5 The main limitation of these studies is that they represent a single institution's experience. Our population-based study includes all patients who underwent RYGB in the State of Pennsylvania over a 3-year period and aims to determine whether age or sex is predictive of adverse outcomes and mortality.
METHODS
All hospitals in the state of Pennsylvania are required to review all in-patient hospital medical records and submit data regarding patients' age, sex, race, principal and all secondary diagnoses, principal and all secondary procedures, length of stay, illness severity, discharge status, unique hospital and surgeon identifier, and insurance status to the Pennsylvania Health Care Cost Containment Council (PHC4) on a quarterly basis. Data are abstracted from medical records and collection is made by trained personnel in each hospital and is based on standardized requirements. The principal procedure code for RYGB (44.31 or 44.39) and the principal diagnosis code for obesity (diagnostic-related group 288) were used to search the PHC4 database and identify patients who underwent RYGB for obesity between January 1, 1999 and December 31, 2001.
Data regarding age, sex, race, comorbid medical conditions, illness severity, in-hospital mortality, in-hospital adverse outcome, and insurance status for all appropriately selected patients were obtained from the database. Prevalences were computed, and subsequent analysis with the MIXED Procedure6 (SAS Institute Inc., Cary, NC) was used to assess whether advanced age (>50 years) or sex significantly increase mortality or adverse outcomes after RYGB for obesity while controlling for any comorbid medical conditions. The dependent variables were inhospital mortality and adverse outcome. In-hospital adverse outcome was defined as a combined variable (one or more postoperative complications, nonroutine hospital transfer, and in-hospital mortality). Complications or deaths that occurred after discharge from the original hospitalization for surgery could not be identified based on the collected data and therefore are not reported. Nonroutine hospital transfer is defined as any disposition other than discharge to home. The independent variables included patient age, sex, race, comorbid medical conditions, insurance status, and illness severity. Co-morbidities included the secondary diagnoses of all the obesity-related medical conditions, such as sleep apnea, hypercholesterolemia, cirrhosis, history of thrombophlebitis, coronary artery disease, diabetes mellitus, hypertension, osteoarthritis, benign intracranial hypertension, esophageal reflux, depression, and congestive heart failure. Patient's preoperative illness severity was categorized as catastrophic, major, moderate, or minor, according to the Ohio Refined DRG Grouper, a Severitized DRG Report.7
RESULTS
Between 1999 and 2001, 4685 patients in Pennsylvania underwent RYGB for obesity. Of the 4685 patients, 82% were females and the remaining were males. Ages ranged from 16 to 74 years with a mean and median of 42 years. Included were 3076 (80%) patients 50 years or younger (mean age, 38 years) and 609 patients older than 50 years (mean age, 55 years). No change occurred in the annual ratios of female/male and younger/older patients between 1999 and 2001. Seventy percent of patients were white and 10% were black. The race was not coded in the remaining 20%. Patient's preoperative illness severity was categorized as catastrophic in 4.5%, major in 16.3%, moderate in 16.2%, and minor in 63% of cases. Seventy-one percent of patients had one or more comorbid medical conditions (Table 1).
Table 1.
Incidence of Comorbid Medical Conditions
| Condition | % |
|---|---|
| Hypertension | 41% |
| Sleep apnea | 25% |
| Gastroesophageal reflux disease | 23% |
| Diabetes mellitus | 19% |
| Osteoarthritis | 12% |
| Depression | 11% |
| Hypercholesterolemia | 9% |
| Coronary artery disease | 2.6% |
| Congestive heart failure | 1.6% |
| Cirrhosis | 0.5% |
| Benign intracranial hypertension | 0.5% |
| Venous stasis | 0.1% |
The median length of stay was 4 days (range, 1 to 83). An in-hospital adverse outcome occurred in 813 of 4685 (17.4%) patients who underwent RYGB. Of the 813 patients with adverse outcomes, 756 (93%) had postoperative complications, 29 (3.6%) required a nonroutine hospital transfer, and 28 (3.4%) died in the immediate postoperative period. The overall complication and mortality rates were 16.1% (756/4685) and 0.6% (28/4685), respectively. Respiratory complications were the most common (7.7%) followed by cardiac events (3.4%), intestinal obstruction (2.7%), urinary complications (2.6%), hemorrhage (2.4%), sepsis (1.9%), renal failure (0.8%), pulmonary embolism (0.2%), clostridium difficile colitis (0.2%) and fascial dehiscence (0.1%). Patients with major or catastrophic illness severity preoperatively had the highest prevalence (71.5%) of adverse outcome, while patients with Medicaid insurance had the highest mortality rate (1.6%). Age >50 years, male sex, black race, and presence of comorbidities were also associated with an increased prevalence of adverse outcomes and mortality (Table 2).
Table 2.
Patient Characteristics With Increased Prevalence of Adverse Outcome and Mortality
| Patient Characteristics | Adverse Outcome (%) | Mortality (%) |
|---|---|---|
| Major or catastrophic illness severity | 71.5% (696/973) | 0.6% (6/973) |
| Medicaid insurance | 24.7% (94/381) | 1.6% (6/381) |
| Male sex | 23.9% (199/833) | 1.2% (10/833) |
| Age > 50 years | 23.2% (222/957) | 0.6% (6/957) |
| Black race | 18.2% (82/451) | 1.3% (6/451) |
| Comorbid medical conditions | 18.2% (608/3340) | 0.5% (17/3340) |
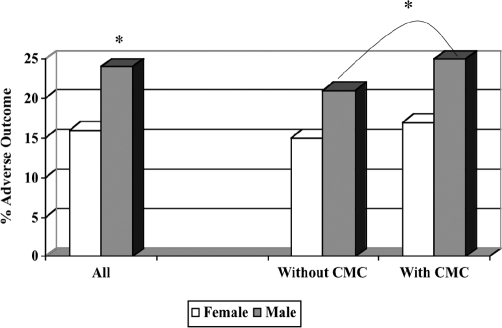
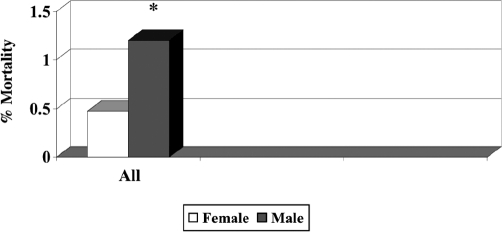
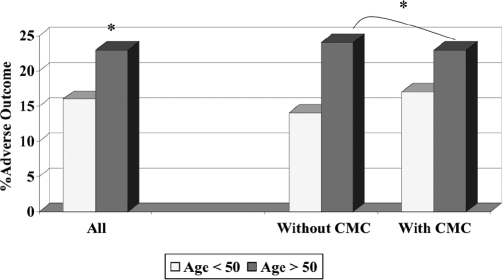
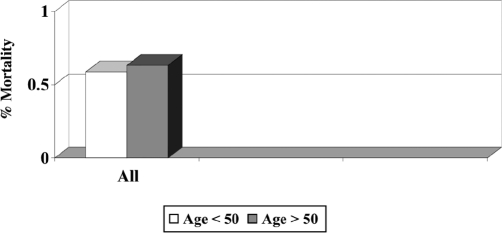
Male patients had a significantly higher prevalence of adverse outcomes (males, 24% vs. females, 16%, P<0.05) and mortality (males, 1.2% vs. females, 0.47%, P<0.05) (Figures 1 and 2). The likelihood of an adverse outcome in males was further increased (P<0.05) when the groups were controlled for the presence of comorbid medical conditions (Figure 1). Older patients had a significantly higher adverse outcome rate (>50, 23% vs. ≤50, 16%, P<0.05) as well. Adverse outcome rates were higher (P<0.05) in older patients who had no other comorbid medical conditions (Figure 3). Age had no significant effect on mortality rates (Figure 4). The presence of comorbidities had no significant effect on mortality rate in relation to sex or age.
Figure 1.
Prevalence of adverse outcome in relation to sex, with or without comorbidity interaction. CMC = Comorbid medical conditions, *P<0.05.
Figure 2.
Mortality rate in relation to sex. *P<0.05.
Figure 3.
Prevalence of adverse outcome in relation to age, with, or without comorbidity interaction. CMC = Comorbid medical conditions, *P<0.05.
Figure 4.
Mortality rate in relation to age.
DISCUSSION
Statewide data from Pennsylvania confirmed the national trend of an increasing demand for bariatric procedures.8 In this study, the annual number of patients undergoing RYGB almost doubled each year (672 in 1999, 1322 in 2000, 2691 in 2001). In accordance with the literature,9 the majority of patients in this study undergoing RYGB were females less than 50 years old and of white origin. Approximately 2/3 of patients had additional obesity-related comorbidities and 1/5 was considered severely ill preoperatively. In addition, the 16.1% and 0.6% complication and mortality rates reported in this study fall within the range of rates reported in previous open9 and laparoscopic10 RYGB series.
According to our results, men carry a higher risk for postoperative complications and death after RYGB. The complication rate in male patients undergoing RYGB was further increased when additional comorbid medical conditions were present. Mortality rate in male patients however was not related to pre-existing medical conditions. Recent studies have also shown that male sex is an independent risk factor for complications and anastomotic leaks.4,10–12 Livingston et al12 showed in his series of 1067 patients that adverse outcomes after RYGB occurred more frequently in men (men, 13.1% vs. women, 6%).
This study confirmed previous reports4,11 that advanced age significantly increased the likelihood of complications after RYGB. In addition, as previously reported,4 the presence of comorbid medical conditions in older patients undergoing RYGB did not have a negative impact on the morbidity of the procedure. Our finding, however, that mortality rates were similar in younger and older patients, is in contrast with the study by Livingston et al11 that showed that mortality of patients 55 years of age and older was 3.5% compared with 1.1% in patients younger than 55 years (P=0.05). It is possible that the different cut-off values used in the 2 studies to dichotomize the age variable may have affected the ultimate results of the analysis.
This study has certain advantages. Contrary to most of the published series that represent a single institution's experience, this is a large, population-based study including surgeons and institutions from the entire State of Pennsylvania. Therefore, the applicability of the findings is more likely to be generalizable to all practice settings. The inclusion of nonroutine hospital transfers to the in-hospital adverse outcomes allowed the identification of all patients who experienced a less than routine outcome after elective surgery. Furthermore, in this study, the effect of comorbid medical conditions on the relationship of age and sex to the morbidity and mortality of RYGB was statistically controlled. Previous studies, such as that by Nguyen and colleagues,4 have not done so.
This study also has several limitations. Body mass index (BMI) was not included in the data reported to the PHC4 by each hospital. Therefore, the effect of the BMI-age, or BMI-sex interaction on the morbidity and mortality rates is not known. Nevertheless, BMI was not a significant risk factor for an adverse outcome after RYGB in any of the previously published reports.3,4,11,12 Similarly, the anastomotic leak rate was not separately recorded and therefore could not be assessed.
In addition, laparoscopic and open RYGB could not be distinguished in the state database and could not be analyzed separately. As a result, the effect of type of approach on the increased morbidity and mortality of RYGB in patients of advanced age or male sex cannot be investigated. A recent study showed that the laparoscopic approach did not ameliorate the increased risk of men for postoperative complications. In his series of 150 laparoscopic RYGB, Nguyen et al4 demonstrated that men had a greater risk of developing complications (adjusted odds ratio, 5.2, P=0.03) than did women. In contrast, another recent study of 188 laparoscopic RYGB by Perugini et al3 showed that of 9 variables examined by univariate and multivariate analysis, including age and sex, only surgeon's experience, sleep apnea, and hypertension were predictive of complications. Further studies on larger patient populations are needed to delineate the effect, if any, of the type of approach on the increased morbidity and mortality of RYGB in older men.
It was also impossible to distinguish primary and revision RYGB in the database. Major complications following revision operations have been more frequent than in primary RYGB in most reported series.13,14 Others however found no significant increase in the complication rates after revision RYGB.12 Nevertheless, it is possible that the inclusion of revision operations in this study may have affected the reported morbidity and mortality rate. Another limitation of this study is that the complication and mortality rates represent events that occurred within the initial in-hospital course from the day of surgery until the date of discharge. Discharge data collection and entry did not allow the identification of events that occurred during the 30-day postoperative period but after the initial discharge. Therefore, it is likely that the complication and mortality rates reported herein might have been underestimated. Finally, the coding of data for these databases may lead to systematic over- or underreporting.15
CONCLUSION
In summary, this study clearly suggests that male patients are at increased risk for complications and death after RYGB and should be monitored closely during the immediate postoperative period. Careful preoperative patient assessment for any comorbid medical conditions is important for risk stratification purposes, especially for men, because their presence increases the morbidity of the procedure. Older patients require close perioperative monitoring as well because advanced age (>50 years) has a negative impact on morbidity rates after RYGB. Despite the fact that the morbidity and mortality rates after RYGB remain within acceptable limits for both subgroups, older patients and men should be counseled regarding their higher perioperative risk.
Footnotes
Presented at the 12th International Congress and Endo Expo 2003, SLS Annual Meeting, Las Vegas, Nevada, September 22–25, 2003.
References:
- 1. Allison DB, Fontaine KR, Manson JE, Stevens J, Vanltallie TB. Annual deaths attributable to obesity in the United States. JAMA. 1999;282:1530–1538 [DOI] [PubMed] [Google Scholar]
- 2. Capella JF, Capella RF. The weight reduction operation of choice: vertical banded gastroplasty or gastric bypass? Am J Surg. 1996;171:74–79 [DOI] [PubMed] [Google Scholar]
- 3. Perugini RA, Mason R, Czerniach DR, et al. Predictors of complication and suboptimal weight loss after laparoscopic Roux-en-Y gastric bypass. Arch Surg. 2003;138:541–546 [DOI] [PubMed] [Google Scholar]
- 4. Nguyen NT, Rivers R, Wolfe BM. Factors associated with operative outcomes in laparoscopic gastric bypass. J Am Coll Surg. 2003;197:548–557 [DOI] [PubMed] [Google Scholar]
- 5. Livingston EH, Ko CY. Assessing the relative contribution of individual risk factors on surgical outcome for gastric bypass surgery: a baseline probability analysis. J Surg Res. 2002;105:48–52 [DOI] [PubMed] [Google Scholar]
- 6. Littell RC, Milliken GA, Stroup WW, Wolfinger RD. SAS system for mixed models. Cary, NC: SAS Institute Inc; 1996 [Google Scholar]
- 7. Smith E. Diagnosis-related group refinement with diagnosis and procedure specific comorbidities and complications. Med Care. 1995;3:8–12 [DOI] [PubMed] [Google Scholar]
- 8. MacDonald KG., Jr Overview of the epidemiology of obesity and the early history of procedures to remedy morbid obesity. Arch Surg. 2003;138:357–360 [DOI] [PubMed] [Google Scholar]
- 9. Cottam DR, Mattar SG, Schauer PR. Laparoscopic era of operations for morbid obesity. Arch Surg. 2003;138:367–375 [DOI] [PubMed] [Google Scholar]
- 10. Gentileschi P, Kini S, Catarci M, Gagner M. Evidence-based medicine: open and laparoscopic bariatric surgery. Surg Endosc. 2002;16:736–744 [DOI] [PubMed] [Google Scholar]
- 11. Fernandez AZ, Jr., DeMaria EJ, Tichansky DS, et al. Experience with over 3,000 open and laparoscopic bariatric procedures: multivariate analysis of factors related to leak and resultant mortality. Surg Endosc. 2004;18(2):193–197 [DOI] [PubMed] [Google Scholar]
- 12. Livingston EH, Huerta S, Arthur D, Lee S, De Shields S, Heber D. Male gender is a predictor of morbidity and age a predictor of mortality for patients undergoing gastric bypass surgery. Ann Surg. 2002;236:576–582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Buckwalter JA, Herbst CA, Jr., Khouri RK. Morbid obesity. Second gastric operations for poor weight loss. Am Surg. 1985; 51:208–211 [PubMed] [Google Scholar]
- 14. Sugerman HJ, Wolper JL. Failed gastroplasty for morbid obesity. Revised gastroplasty versus Roux-Y gastric bypass. Am J Surg. 1984;148:331–336 [DOI] [PubMed] [Google Scholar]
- 15. Hannan EL, Radzyner JD, Rubin D, Dougherty J, Brennan MF. The influence of hospital and surgeon volume on in-hospital mortality for colectomy, mastectomy, and lung lobectomy in patients with cancer. Surg. 2002;131:6–15 [DOI] [PubMed] [Google Scholar]