Abstract
Background:
The urachus is a vestigial structure between the dome of the bladder and the umbilicus. Tumors may develop from the remnants, most of which are well-differentiated, mucinous adenocarcinomas. Urachal adenocarcinoma is an exceedingly rare type of tumor.
Methods:
We present a case of a 51-year-old female presenting to our institution with complaints of abdominal pain for 36 hours. The patient was taken to the operating room for an acute appendicitis. Laparoscopy was performed, and gross purulence and appendiceal perforation were noted as well as a mass on the anterior abdominal wall. Based on the location of the mass, we converted to an open midline laparotomy to treat both the perforated appendicitis and to remove the mass.
Results:
Pathology confirmed the diagnosis of perforated appendicitis and a mucinous-producing urachal adeno-carcinoma.
Discussion:
Data support both open and laparoscopic approaches for appendicitis. This case, although rare, highlights the importance of laparoscopy in a complete and thorough examination of the abdominal cavity. A standard right lower quadrant incision for an open technique would likely have resulted in omission of this lesion, and the patient would have presented at a more typical late stage of her cancer development with significantly more morbidity.
Keywords: Urachal adenocarcinoma, Ruptured appendicitis, Laparoscopy
INTRODUCTION
The urachus is a vestigial structure between the dome of the bladder and the umbilicus. It represents the apical attachment of the bladder to the allantois during human fetal development.1 It usually retracts from the bladder before birth, but its lumen, which is lined by transitional or columnar epithelium, may persist within the bladder wall and be continuous with the bladder cavity even in adults. Tumors may develop from the remnants, most of which are well-differentiated mucinous adenocarcinomas.2 Urachal adenocarcinoma is an exceedingly rare type of tumor. These tumors account for less than 1% of all bladder tumors.3–8
CASE REPORT
We present the case of a 51-year-old white female who presented to our institution with complaints of abdominal pain for approximately 36 hours. The pain was described in her history as more localized to the epigastrium, but she was more tender in the right lower quadrant. She described this pain as achy and constant with positive nausea and emesis. She noted a decreased appetite and diarrhea for approximately 1 week. She denied any fever or chills at home over that time. She also described a straining sensation on urination but no associated dysuria or blood. All other system reviews were noncontributory. The patient denied any significant past medical, social, or family history.
On physical examination, her temperature was 101.2° with other vital signs being stable. Her abdominal examination indicated that the abdomen was quiescent, soft, hot to the touch, and nondistended. McBurney's sign, Rovsing's sign, Merkel's sign, and rebound throughout were positive. The only significant laboratory value was an elevated white blood cell count of 15.8x109. A CT scan ordered in the emergency department was interpreted as showing the presence of fluid in the RLQ with pericecal haziness and fluid in the paracolic gutter. Fluid was noted in the pelvis as well as a left ovarian cyst approximately 2.5 cm in size. Another cyst was identified in the right lobe of the liver approximately 1.5 cm in size (Figure 1).
Figure 1.
Computed tomographic scan showing pericecal fluid consistent with acute appendicitis.
The decision was made to perform a laparoscopic appendectomy. The patient was taken to the operating room where a diagnostic laparoscopy was performed. On entry into the abdomen, gross purulence was noted in the pelvis (Figure 2) and subhepatic space. A mass was found on the anterior abdominal wall in the midline to which the omentum was adherent (Figure 3). Once the inflammatory mass was moved laterally, we noted a perforated appendix and the anterior abdominal wall mass was clearly a separate entity (Figures 4 and 5). At this point, we converted to an open midline laparotomy so as to clearly remove the midline mass. After performing our standard open appendectomy, we turned our attention to the midline mass. We were able to dissect it free with grossly clear margins, but on the inferior surface were obligated to remove a small portion of the bladder. Postoperatively, the pathology of the mass came back as a primary urachal adenocarcinoma. The patient did well postoperatively, and a positron emission tomographic (PET) scan done 6 weeks postoperatively was negative for any further evidence of tumor spread. A colonoscopy done at that time also was completely normal. The patient did not follow up with her medical oncologist until 6 months later at which time she underwent a computed tomographic (CT) scan of the chest, abdomen, and pelvis. No evidence of recurrent disease was present. Because of the length of time after surgery and her follow-up with medical oncology, she is not a candidate for chemotherapy.
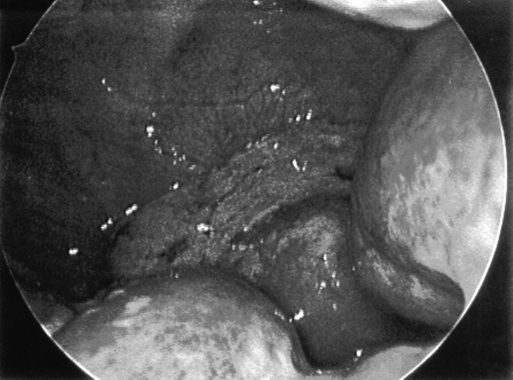
Figure 2.
Purulent drainage in pelvis.
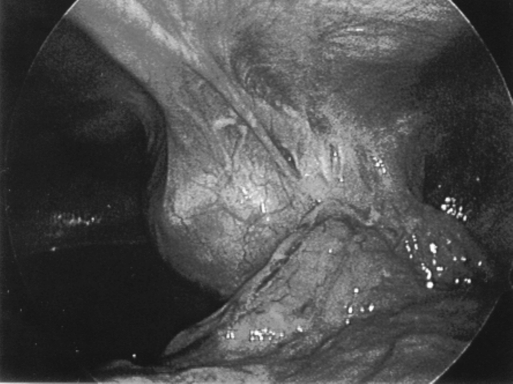
Figure 3.
Gross appearance of anterior abdominal wall mass with adherent appendix.
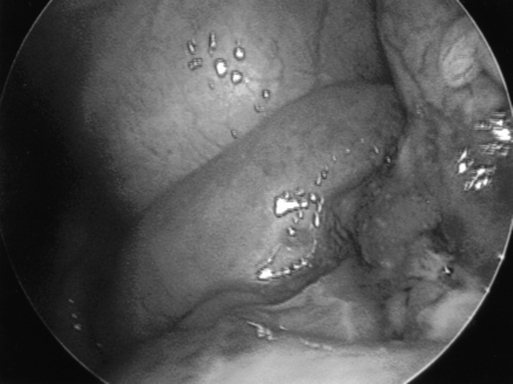
Figure 4.
Perforated appendix.
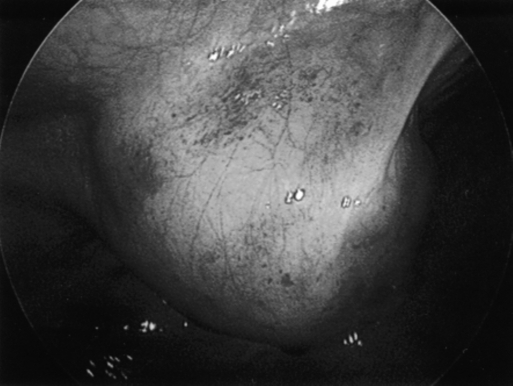
Figure 5.
Anterior wall abdominal mass.
RESULTS
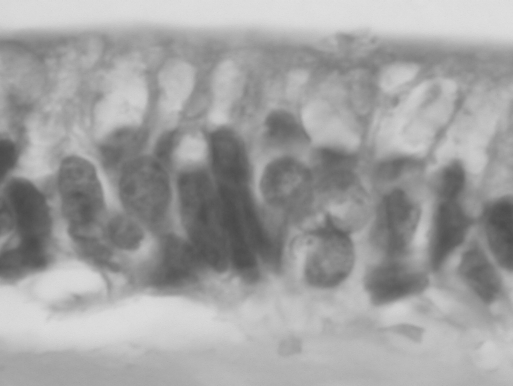
The specimen consisted of a 33-gram circumscribed, bosselated red-tan mass, measuring 5.0 x4.5x3.8 cm. A cut section revealed multiple locules filled with a viscid, pale gelatinous fluid. Microscopic sections revealed a mucinous neoplasm arising external to the muscularis propria of the bladder. The urothelium showed reactive features but was not directly involved by the mass. High-power examination revealed that the mucinous pools were lined by a columnar epithelium with malignant features (Figure 6).
Figure 6.
High-power view of specimen revealing pools of mucin.
The accompanying appendix was completely examined and showed acute appendicitis. No evidence was present of a mucinous neoplasm within the appendix. Clinical and radiographic evaluation of the ovaries and gastrointestinal tract revealed no evidence of a neoplasm. The lack of involvement by ovaries, appendix, and other gastrointestinal organs served to rule out a metastatic lesion from those locations. Accordingly, the bladder mass was diagnosed as a mucin-producing adenocarcinoma, consistent with urachal adenocarcinoma.
DISCUSSION
Primary urachal adenocarcinoma is exceedingly rare accounting for less than 1% of all bladder malignancies. Urachal adenocarcinoma is more common in men and typically presents in the fifth or sixth decade of life.9 Common presenting symptoms are hematuria, pain, irritative symptoms, and mucosuria. Late findings include mucinous or serous drainage from a tract in the umbilicus. Histologically, these tumors are most commonly the mucinous type.10 Currently, no absolute consensus exists regarding diagnostic criteria. Several authors agree that the important clinicopathologic features of a primary urachal adenocarcinoma include1 location of the tumor in the bladder wall,2 evidence of a sharp demarcation between the tumor and surface epithelium,3 exclusion of a primary tumor located elsewhere that has spread to the bladder, and4 a urachal remnant associated with the tumor.11–13
Because of the typical late presentation of these tumors, the prognosis is poor. The 5-year survival rate reported by several authors is between 16% and 45%.14,15 Complete resection improves overall survival as does early diagnosis and surgical intervention. The role for chemotherapy in urachal adenocarcinoma is not well established. The most recent study addressing this issue from The University of Texas M.D. Anderson Cancer Center advocates the use of 5-flourouracil and cisplatin with either α-interferon or gemcitabine and leucovorin.16
CONCLUSION
It is our hope that with the early finding of the urachal mass and complete resection that we have provided a long-term cure. Our expectation is that this case report will add to the body of literature supporting a laparoscopic approach to evaluation of abdominal pathology. We believe that had this patient been treated with a standard open approach for appendicitis on initial exploration, the urachal mass would not have been found. Furthermore, diagnostic laparoscopy allowed us to fully evaluate the abdominal cavity as well as plan our more appropriate surgical incision without compromising the integrity of the mass, allowing us to remove it in its entirety. Currently, this patient remains disease free after 12 months of follow-up.
Contributor Information
Richard M. Peterson, Department of Surgery, St. Agnes Hospital, Baltimore, Maryland, USA..
Curtis Ollayos, Department of Pathology, St. Agnes Hospital, Baltimore, Maryland, USA..
Deepak Merchant, Department of Surgery, St. Agnes Hospital, Baltimore, Maryland, USA..
References:
- 1. Minevich E, Sheldon CA. In: Greenfield LJ, et al. ed. Surgery: Scientific Principles & Practice. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2001; 2047 [Google Scholar]
- 2. Ohira S, Shiohara S, Itoh K, Ashida T, Fukushima M, Konishi I. Urachal Adenocarcinoma metastatic to the ovaries: case report and literature review. Int J Gynelcol Pathol. 2003; 22 (2): 189–193 [DOI] [PubMed] [Google Scholar]
- 3. Ichikawa T. Remote results of bladder tumors. Jpn J Urol. 1958; 49: 602–610 [Google Scholar]
- 4. Jacobo E, Loening S, Schmidt JD, et al. Primary adenocarcinoma of the bladder: a retrospective study of 20 patients. J Urol. 1977; 117: 54–56 [DOI] [PubMed] [Google Scholar]
- 5. Thomas DG, Ward AM, Williams JL. A study of 52 cases of adenocarcinoma of the bladder. Br J Urol. 1971; 43: 4–15 [DOI] [PubMed] [Google Scholar]
- 6. Jakse G, Schneider J, Jacobi GH. Urachal signet-ring carcinoma, a rare variant of vesical adenocarcinoma: Incidence and pathological criteria. J Urol. 1978; 120: 764–766 [DOI] [PubMed] [Google Scholar]
- 7. Yu HH, Leon CH. Carcinoma of the urachus: report of one case and review of the literature. Surgery. Urology. 1975; 77: 726. [PubMed] [Google Scholar]
- 8. Henley DR, Farrow GM, Zincke H. Urachal cancer: role of conservative surgery. Urology. 1993; 42: 635. [DOI] [PubMed] [Google Scholar]
- 9. Besarani D, Purdie CA, Townell NH. Recurrent urachal adenocarcinoma. J Clin Pathol. 2003; 56: 882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Grignon DJ, Ro JY, Ayala AG, et al. Primary adenocarcinoma of the urinary bladder. A clinicopathologic analysis of 72 cases. Cancer. 1991; 67: 2165–2172 [DOI] [PubMed] [Google Scholar]
- 11. Wheeler JD, Hill WT. Adenocarcinoma involving the urinary bladder. Cancer. 1954; 7: 199–135 [DOI] [PubMed] [Google Scholar]
- 12. Mostofi FK, Thompson RV, Dean AL., Jr Mucinous adenocarcinoma of the urinary bladder. Cancer. 1955; 8: 741–758 [DOI] [PubMed] [Google Scholar]
- 13. Johnson DE, Hodge GB, Abdul-Karim FW, Ayala AG. Urachal carcinoma. Urology. 1985; 26: 218–221 [DOI] [PubMed] [Google Scholar]
- 14. Cirillo RL. Urachal carcinoma. eMedicine. Available at: http://www.emedicine.com/radio/topic727.htm Last updated July 29, 2004 [Google Scholar]
- 15. Herr HW. Urachal carcinoma: the case for extended partial cystectomy. J Urol. 1994; 151: 365–366 [DOI] [PubMed] [Google Scholar]
- 16. Siefker-Radtke AO, Gee J, Shen Y, et al. Multimodality management of urachal carcinoma: the MD Anderson cancer center experience. J Urol. 2003; 169: 1295–1298 [DOI] [PubMed] [Google Scholar]