Abstract
Background:
Large adrenal tumors were initially believed to be a relative contraindication to laparoscopic adrenalectomy.
Methods:
Here we discuss the case of a 42-year-old female with a 12-cm adrenal mass.
Results:
The patient underwent successful laparoscopic resection, and pathology revealed a cavernous hemangioma, a rare benign tumor of the adrenal gland.
Conclusion:
The following is a discussion of the case, laparoscopic resection technique, and brief review of adrenal hemangiomas. In experienced hands, adrenal mass size should not be considered a contraindication to laparoscopic intervention.
Keywords: Adrenal mass, Hemangioma, Laparoscopic adrenalectomy
INTRODUCTION
Large adrenal tumors were initially believed to be a relative contraindication to laparoscopic adrenalectomy. Here we discuss the case of a 42-year-old female with a 12-cm adrenal mass. The patient underwent successful laparoscopic resection, and pathology revealed a cavernous hemangioma, a rare benign tumor of the adrenal gland. The following is a discussion of the case, laparoscopic resection technique, and brief review of adrenal hemangiomas.
CASE REPORT
The patient is a 42-year-old female with a past medical history significant for hypertension, osteoarthritis, and obesity who presented to her primary care physician with a 1-year history of left-sided flank pain. She had never experienced similar pain in the past, and the pain was progressive. She denied headaches, fatigue, chest pain, shortness of breath, dizziness, new onset weight gain, palpitations, or skin changes. The remainder of the review of systems was within normal limits. Her physical examination was unremarkable; the abdomen was benign and no masses were appreciated.
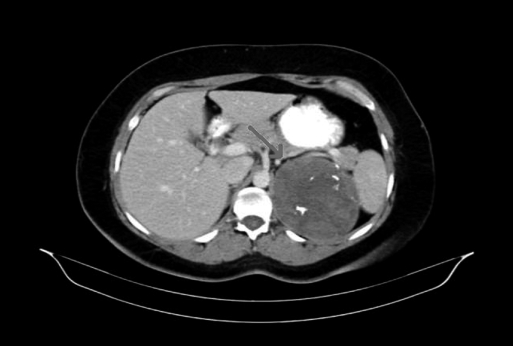
A computed tomography (CT) scan revealed a 12-cm left adrenal mass (Figure 1). The mass was noted to be heterogeneous with scattered calcifications. It was also noted to abut the tail of the pancreas and spleen as well as displace the left kidney and renal vessels inferiorly. On MRI, the mass enhanced on T2 weighted images.
Figure 1.
Computed tomographic scan of left adrenal mass.
An endocrine workup was performed to rule out a functioning tumor and was within normal limits. Urine and plasma catecholamines were unremarkable. Chromogranin A was within normal limits. Hypercorticolism and hyperaldosteronism were also ruled out.
The patient underwent an uncomplicated laparoscopic adrenalectomy. The postoperative course was uneventful; she tolerated a diet on postoperative day 1 and was discharged home on postoperative day 2. The pathology examination revealed a cavernous hemangioma with extensive hematoma.
Laparoscopic Technique
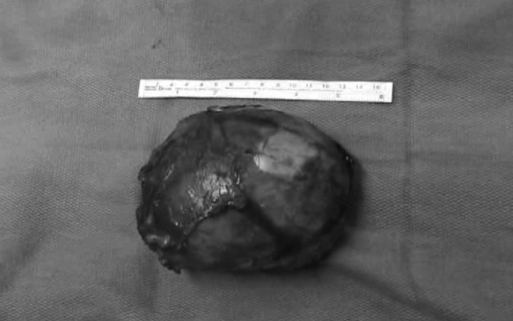
The patient was taken to the operating room and placed in the left lateral decubitus position. The open Hasson technique was used to place a 10-mm trocar in the midclavicular line of the left upper abdomen. Subsequent left flank 5-mm and 10-mm trocars were placed under direct vision. The dissection began by taking down the splenic flexure with the ultrasonic shears. Once the colon was reflected, the lateral margin of the tumor was identified and abutted the spleen and splenic vessels. The medial margin of the mass was then approached and was adjacent to the pancreas. The mass was noted to be well encapsulated and was carefully dissected off of the splenic vessels, pancreas, and Gerota's fascia. Next, the left adrenal vein was exposed. Initially, it was difficult to discern the adrenal vein from the renal vein and splenic vessels. The adrenal vein was displaced inferiorly and plastered against the mass. After careful dissection, the adrenal vein was confidently identified, taken with clips and divided. The deep attachments to the mass were then addressed. At this point in the procedure, we encountered difficulty maintaining adequate retraction on the mass while taking the posterior retroperitoneal attachments. Retraction was facilitated with the use of a fan retractor. The dissection was then continued, and the attachments of the mass to the lateral abdominal wall and diaphragm were taken. Once the mass was free, it was placed in a 15-cm endobag. The 10-mm trocar site was then extended to an approximately 6.5-cm subcostal incision to extract the mass. The mass was measured to be approximately 12cm in its longest dimension. Grossly, the opened mass had some areas of necrosis, and the tissue was extremely heterogeneous (Figure 2). Frozen sections sent intraoperatively were benign. The abdomen was then copiously irrigated and port sites closed. Operative time was 167 minutes. Estimated blood loss was 50 mL.
Figure 2.
Gross pathology of adrenal mass.
Cavernous Hemangioma
Cavernous hemangiomas are benign tumors that arise from endothelial cells that line blood vessels. They consist of multiple, large vascular channels lined by a single layer of endothelial cells and supported by collagenous walls1 Adrenal hemangiomas are rare, and the literature is limited to case reports. In 1955, Johnson and Jeppesen described the first successful surgical resection of this adrenal tumor, and since that time only approximately 50 such cases have been described in the literature.2 The majority of adrenal hemangiomas are unilateral, and nonfunctioning. Coexistence with malignant hemangioendothelioma has been reported.3 Though these tumors are predominantly nonfunctioning, in 1996 Stumvoll et al4 published a case report of a functional hemangioma.
The majority of patients presenting with this tumor are asymptomatic, and the mass is discovered incidentally on imaging. Symptomatic patients generally present with abdominal or flank pain, with or without a palpable mass. Hemangiomas may become quite large and cause symptoms secondary to compression of surrounding structures. Rarely, these tumors are associated with rupture, hypovolemia secondary to hemorrhage, acute thrombosis, and Kasabach-Merritt syndrome, which is a consumptive coagulopathy.2,3
The cause of adrenal hemangioma is not completely understood. Hemangiomas are likely congenital, and hereditary factors may play a role in the pathogenesis. Ectasia, rather than growth, is believed to contribute to hemangioma enlargement.5
CT and magnetic resonance imaging (MRI) are the most frequently utilized modalities to diagnose and characterize adrenal masses. Typical findings of adrenal hemangioma on CT include a heterogeneous, hypodense lesion with calcifications, as was seen in our patient. However, it can be difficult to distinguish these lesions from carcinomas or cysts.6 MRI may also be helpful; common findings associated with adrenal hemangiomas are hypointense inhomogeneous masses with central hyperintensity on T1-weighted images as well as peripheral enhancement after injection of Gd-DTPA.7 In our case, the patient had enhancement on T2 weighted images.
Surgical resection is recommended when tumors exceed 4cm in diameter. Several open techniques including transabdominal, flank, and posterior approaches have been described. While laparoscopic adrenalectomy has become the procedure of choice for adrenal mass, the majority of these lesions tend to be small.8 Giant adrenal masses are still considered by many to be a relative contraindication to laparoscopy. To our knowledge, there has only been one recent report of retroperitoneal endoscopic resection of a large tumor that was 6.5cm × 7cm.9
In this patient, we describe the feasibility of laparoscopic resection even in cases of giant adrenal masses. The key to performing this operation successfully is careful dissection of the mass off surrounding structures without compromising the tumor capsule or injuring abutting organs. A major disadvantage of this resection is maintenance of adequate retraction on the mass when intraabdominal space is limited. Appropriate tension is essential for safe dissection when freeing the mass from its lateral, medial, and posterior attachments. Here we used a fan retractor to gain adequate tension. Another pitfall of this procedure is the identification of the adrenal vein from surrounding vessels when displaced from proper anatomic position. Careful identification of the renal vein, and, in this circumstance, the splenic vessels is essential prior to adrenal vein ligation.
In our experience, laparoscopic resection of a giant adrenal mass is technically feasible and confers the established perioperative benefits of laparoscopy. Our patient tolerated the procedure well without complication. She was tolerating a diet by postoperative day 1 and discharged home on postoperative day 2. She is currently 24 months postsurgical resection with no evidence of recurrence. In experienced hands, adrenal mass size should not be considered a contraindication to laparoscopic intervention.
References:
- 1.Del Gaudio A, Solidoro G, Martinellu G. Adrenal hemangiomas: two case reports with a review of the literature. Surgery. 1989;105:674–681 [PubMed] [Google Scholar]
- 2.Johnson CC, Jeppesen FB. Hemangioma of the adrenal. J Urol. 74(5):573–577, 1955. November [DOI] [PubMed] [Google Scholar]
- 3.Salup R, Finegold R, Borochovitz D, Boehnke M, Posner M. Cavernous hemangioma of the adrenal gland. J Urol. 1992;147:110–112 [DOI] [PubMed] [Google Scholar]
- 4.Stumvoll M, Fritsche A, Wehrmann M, Dammann F, Becker HD, Eggstein M. A functioning adrenocortical hemangioma. J Urol. 1996;155:638. [PubMed] [Google Scholar]
- 5.Hugh TJ, Poston GJ. Benign Liver Tumours and Masses. Surgery of the Liver and Biliary Tract. 3rd ed. London: WB Saunders; 2000;1397–1422 [Google Scholar]
- 6.Deckers F, De Schepper A, Shamsi K, Hauben E, Van Marck E. Cavernous hemangioma of the adrenal gland: CT appearance. Comput Assis Tomogr. 1993;17:506. [DOI] [PubMed] [Google Scholar]
- 7.Rieber A, Brambs HJ. CT and MR imaging of adrenal hemangioma. A case report. Acta Rad. 1995;36:659. [PubMed] [Google Scholar]
- 8.Janetschek G. Surgical options in adrenalectomy: laparoscopic versus open surgery. Curr Opin Urol. 1999;9:213–218 [DOI] [PubMed] [Google Scholar]
- 9.Yagisawa T, Amano H, Ito F, Horita S, Yamaguchi Y, Toma H. Adrenal hemangioma removed by a retroperitoneoscopic procedure. Int J Uro. 2001;8:457. [DOI] [PubMed] [Google Scholar]