Abstract
Background and Objectives:
A history of a prior abdominal operation is common among patients presenting for laparoscopic colorectal surgery, and its impact on conversion and complication rates has been insufficiently studied. This study compares the conversion rates of patients with and without a prior abdominal operation (PAO).
Methods:
We analyzed 1000 consecutive laparoscopic colorectal resection cases.
Results:
Complete data on past surgical history were available on 820 of 1000 patients. The overall conversion rate was 14.8% (122/820). A history of PAO was present in 347 patients (42.3%). These patients experienced a higher conversion rate compared with non-PAO patients (68/ 347, 19.6% versus 54/473, 11.4%; P<0.001; OR 1.9). Patients with PAO had a significantly higher rate of inadvertent enterotomy (5/347, 1.4% vs. 1/473, 0.2%; P=0.04; OR 6.9), a higher incidence of postoperative ileus (23/347, 6.6% vs 14/473% 3.0; P=0.012; OR 2.3), and higher reoperative rates (8/347, 2.3% vs 1/473, 0.2%; P=0.006; OR 11.1). The incidence of other complications and mortality (total 6/820, 0.7%) was similar regardless of PAO status.
Conclusion:
Having a prior abdominal operation represents a risk factor for conversion in laparoscopic colon and rectal surgery. The incidence of a successfully completed laparoscopic operation, however, remains high in previously operated on patients.
Keywords: Laparoscopy, Intraoperative complications, Postoperative complications, Ileus
INTRODUCTION
Laparoscopic surgery of the colon and rectum has gained acceptance as the minimally invasive counterpart of traditional open resections. It was first accepted for benign conditions; however, a recent prospective trial demonstrated the noninferiority of laparoscopic resection of the colon and rectum for malignant diseases.1
A history of previous abdominal operations is not considered an absolute contraindication to laparoscopic colorectal surgery.2 Common sequelae of prior abdominal operations include adhesions,3,4 increased operative time,5 and a higher rate of complications.5,6 The conversion rate to an open procedure might also be affected, with resultant increased operative time and cost.7 Thus, if a high-risk patient group for conversion can be identified based on preoperative data, these patients might be counseled about the possible increased conversion risk.
Previous studies have not identified PAO as a risk factor for conversion in laparoscopic colorectal operations8,9; however, numbers were small and higher conversion rates were seen in previously operated on patients. Thus, we decided to conduct a larger study with adequate statistical power to analyze the influence of prior abdominal operations on the conversion rate and complication risk in patients undergoing laparoscopic colon and rectal surgery.
METHODS
The records of 1000 consecutive patients who underwent laparoscopic colon or rectal resection between 1997 and 2004 were analyzed.
All operations took place in 2 community hospitals, one teaching (ie, had resident physicians) and one nonteaching hospital. Most operations in the teaching hospital were performed with the assistance of a surgical resident, who depending on the level of his or her training and skills, performed some or all of the procedure under the supervision of a fellowship-trained colon and rectal surgeon with laparoscopic expertise (SAF and DMZ).
Data Collection
A prospectively collected database of a single colorectal surgical group in both hospitals was reviewed. An electronic medical record system was available in the teaching hospital. Prior abdominal operation (PAO) was defined as previous surgical intervention involving the peritoneal cavity, whether by celiotomy or laparoscopy. Inguinal and femoral hernia repairs were not included as PAO.
Operative Procedure and Conversion
For the purpose of this study, conversion was defined as the change in operative strategy requiring exsufflation of capnoperitoneum and elongation of the surgical incision to allow direct visualization for continued dissection. Hand-assisted cases were included in the laparoscopic group. Anastomosis was fashioned extracorporeally in right-sided procedures and intracorporeally via the rectum in left-sided procedures. Conversion and its indication, demographic characteristics, complication rate, operative time, and estimated blood loss were analyzed.
Complications
Intraoperative and early postoperative complications were recorded. Intraoperative complications included bleeding, enterotomy, ureteral and bladder injury, and injury to any other structure, such as the large vessels, spleen, or liver.
Early postoperative complications included surgical and medical complications, both diagnosed during the postoperative in-hospital stay. No differentiation between postoperative ileus and early small bowel obstruction was made because of the lack of exact criteria. Ileus was defined as the inability to tolerate any diet combined with abdominal distension beyond the third postoperative day. Mortality rates were analyzed separately.
Statistical Analysis
The Mann-Whitney test, Kruskal-Wallis ANOVA, χ2-test, and Fisher exact test were used as appropriate. Significance was defined at P<0.05 or less as indicated.
RESULTS
The most common operation performed in our group of patients was right hemicolectomy (n=337, 41%), followed by sigmoid colectomy (n=214, 26%), left hemicolectomy (n=205, 25%), and rectal procedure (n=64, 8%). Invasive cancer was the most common indication (n=277, 34%), followed by polyps (n=246, 30%), and diverticulitis (n=224, 27%).
History of Prior Abdominal Operation and Conversion Rate
Of 1000 consecutive patients, the data on past surgical history were available on 820 patients, representing a data collection rate of 82%. The remaining 180 patients with missing data were excluded from the study. A history of PAO was present in 347 patients (42.3%) (Table 1). The overall conversion rate was 14.8% (122 of 820 patients) (Table 2) in the analyzed subgroup with known PAO status. When the entire prospective database was analyzed, 132 of 1000 (13.2%) patients were converted. Loss of data was not significant.
Table 1.
Demographic Characteristics and Prior Abdominal Operation Status (PAO)
| Characteristic | No. of Patients (%) | Conversion Rate (%) | P |
|---|---|---|---|
| Sex | |||
| Male | 528 (52.8) | 12.7 | |
| Female | 472 (47.2) | 14.2 | 0.485 |
| ASA Score | |||
| ASA 1 | 50 (14.0) | 14.0 | |
| ASA 2 | 199 (57.6) | 16.6 | |
| ASA 3 | 86 (24.9) | 15.1 | |
| ASA 4 | 10 (2.9) | 20.0 | 0.947 |
| History of PAO | |||
| Without PAO | 473 (57.7) | 11.4 | |
| With PAO | 347 (42.3) | 19.6 | 0.001 |
| PAO status unknown | 180 (−) | ||
| History of Appendectomy (APE) | |||
| APE+ | 102 (12.4) | 11.8 | |
| APE− | 718 (87.6) | 15.3 | 0.345 |
| History of Cholecystectomy (CHE) | |||
| CHE+ | 27 (3.3) | 18.5 | |
| CHE− | 793 (96.7) | 14.8 | 0.589 |
| History of Prior Pelvic Surgery | |||
| Pelvic surgery+ | 77 (9.4) | 26.0 | |
| Pelvic surgery− | 743 (90.6) | 13.7 | 0.004 |
Table 2.
Indications for Conversion
| Indication | Frequency | Percent |
|---|---|---|
| Anatomic reason | 78 | 63.9 |
| Tumor-related reason | 9 | 7.4 |
| Intraoperative complications | 24 | 19.7 |
| Other | 11 | 9.0 |
| Total | 122 | 100.0 |
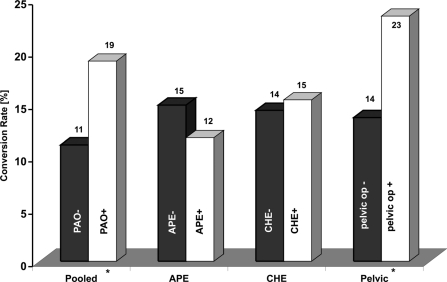
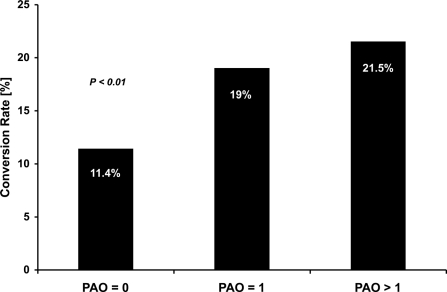
Patients with PAO experienced a higher conversion rate compared with the patients with no PAO (68/347, 19.6% versus 54/473, 11.4%; P<0.001; OR 1.9; 95% CI for OR 1.3–2.8) (Figure 1). Because some patients had multiple PAOs (n=79, 9.6%), the influence of the number of PAOs on the conversion rate was also analyzed. The conversion rate was significantly lower in the group without PAO (11.4%, 54/473; P<0.01) compared with both the group with 1 PAO (19.0%, 51/268) and the group with more than 1 PAO (21.5%, 17/79). There was no statistically significant difference when a group with one PAO was compared with the group with multiple PAOs (P=0.624) (Figure 2).
Figure 1.
Conversion rates (%). Patients without and with PAO (PAO-, PAO+); patients without and with prior appendectomy (APE-, APE+); patients without and with prior cholecystectomy (CHE-, CHE+); patients without and with prior pelvic surgery (pelvic-, pelvic+). Note that patients without prior appendectomy (or cholecystectomy or pelvic surgery) could still have some other prior abdominal operation. *Statistically significant difference.
Figure 2.
Conversion rate depending on number of PAOs. Patients without a history of PAOs (PAO=0) have significantly lower conversion rates than those with a history of at least of 1 PAO (P<0.01). There is no statistically significant difference in conversion rates between patients with 1 (PAO=1) and more than 1 PAO (PAO>1).
An increased risk of conversion was noted in patients with a history of prior pelvic surgery (20/77, 26.0% versus 102/743, 13.7%; P=0.004; OR 2.2, 95% CI 1.3–3.8). A history of prior appendectomy or cholecystectomy had no statistically significant effect on conversion rates (Table 1, Figure 1).
Effect of History of PAO on Estimated Blood Loss and Operative time
Estimated blood loss was nonsignificantly lower in the group without PAO than in the group with PAO (153±136mL vs. 180±279 mL, P=0.95). Operating time was similar between the groups without and with PAO (158±89 min vs 159±130 min, P=0.24).
History of PAO and Incidence of Complications
Patients with PAO had a higher incidence of ileus (23/347, 6.6% vs. 14/473% 3.0; P=0.012, OR 2.3, 95% CI 1.2– 4.6). Inadvertent enterotomy was significantly more common in patients with PAO (5/347, 1.4% vs 1/473, 0.2%; P=0.04, OR 6.9). Reoperative rates were also higher in patients with PAO (8/347, 2.3% vs 1/473, 0.2%; P=0.006, OR 11.1). Rates of frank bowel obstruction, readmission, leak, abscess, wound infection, intraoperative bladder or ureter injury, significant iatrogenic intraoperative bleed, and death were not statistically significantly different (Table 3).
Table 3.
Rate of Intraoperative and Postoperative Complications
| Complication | PAO− (%) | PAO+ (%) | Significance |
|---|---|---|---|
| Intraoperative | |||
| Bleeding | 7/473 (1.5) | 9/347 (2.6) | 0.255 |
| Enterotomy | 1/473 (0.2) | 5/347 (1.4) | 0.041 |
| Ureter injury | 0/473 (0.0) | 1/347 (0.3) | 0.423 |
| Bladder injury | 2/473 (0.4) | 0/347 (0.0) | 0.511 |
| Early Postoperative | |||
| Wound infection | 7/473 (1.5) | 2/347 (0.6) | 0.315 |
| Overt leak & abscess | 8/473 (1.7) | 7/347 (2.0) | 0.731 |
| Ileus | 14/473 (3.0) | 23/347 (6.6) | 0.012 |
| Myocardial infarction | 3/473 (0.6) | 3/347 (0.9) | 0.702 |
| Other complications (stroke, TIA) | 4/473 (0.8) | 2/347 (0.6) | 1.000 |
| Readmission | 9/473 (1.9) | 13/347 (3.7) | 0.106 |
| Reoperation | 1/473 (0.2) | 8/347 (2.3) | 0.006 |
Mortality
In-hospital mortality occurred in 6 patients for a total mortality of 0.7%. A history of PAO had no statistically significant impact on in-hospital mortality (4/473, 0.8% versus 2/347, 0.6%; P=1.0, NS).
DISCUSSION
Laparoscopic resection of the colon and rectum has become established as a minimally invasive alternative for a variety of benign diseases,2,10 but its applicability for curative treatment of carcinoma of the colon and rectum was initially questioned because of such factors as suspected high local and trocar wound site recurrence and dubious clearance of the nodal basin.
Several large retrospective analyses,11–13 as well as the COST clinical trial,1 have reported favorable oncologic outcomes in patients treated with laparoscopic colon re-section.
Conversion of a laparoscopic procedure to an open one should not be viewed as a failure of technique, but rather as a safer means to accomplish the same therapeutic goal. The quality of an operation cannot be compromised by a selected technique.1,2 Traditionally accepted benefits of laparoscopic operations include a shorter hospital stay and recovery, decreased rate of pulmonary complications, less pain, lower wound infection rates, and superior cosmesis.1,14 Oncologic outcome is believed to be equal for both open and laparoscopic procedures.1,2,13 Some evidence, however, suggests a poorer oncologic outcome in patients, who underwent conversion versus patients with laparoscopically completed resection of colon cancer.2,15,16
A prior abdominal operation leads to formation of adhesions in over 80% of patients with a history of PAO.3,4 On the other hand, adhesions are uncommon in patients without PAO and are seen in less than 10% of the population in the same studies. Inadvertent intestinal injury during laparotomy is more common in patients with multiple PAOs and leads to significant morbidity.6 Ellis et al5 reported a 21% increase in the inadvertent enterotomy rate in patients undergoing repeated laparotomy and estimated 24 minute increase in total operative time caused by intraabdominal adhesions from prior abdominal surgery.5 The magnitude of adhesion-related morbidity is supported by Medicare data, as analyzed by Beck et al4 on almost 19,000 patients, who observed a 14% rate of clinically evident small bowel obstruction and a 2.6% reoperative rate within 2 years after an intestinal operation.
In an analysis of a recent large data set, Tekkis et al17 reported that laparoscopic conversion rates are dependent on multiple factors, including body mass index, American Society of Anesthesiologists score, type of re-section, and the presence of abscess. Patients with multiple PAOs, however, were excluded from this analysis, and data on prior surgical history were available in only approximately 40% of the cases.17
Since the prevalence of PAO in the population presenting to colon and rectal surgeons can reach 30% to 50%,11,18 it is only reasonable to ask the following question: is laparoscopy indicated for everyone? Generally, the presence of PAO is not considered an absolute contraindication,2 but rather a relative one.
The influence of prior surgical history on the conversion rate has been studied mostly in patients undergoing laparoscopic cholecystectomy. Although this procedure was found to be “more difficult” in patients with PAO,19 it is still considered safe in patients with PAO. Upper abdominal surgery, however, increases the need for adhesiolysis, prolongs operative time, increases wound infection and hospital stay, and leads to a significantly higher conversion rate.20
Two recent studies8,9 examined the effect of PAO on the outcome of laparoscopic colorectal surgery. Hamel et al8 studied 85 patients undergoing laparoscopic right hemicolectomy. Conversions due to adhesions were more common in those who had a previous operation, but this did not reach statistical significance. Nonetheless, their P value (P=0.078) approached statistical significance, and one can speculate that a higher number of patients might have changed the outcome of the study. A larger study by Law et al9 examined almost 300 patients and found similar conversion rates to our results: 11.4% in patients with no PAO, and 17.8% for PAO patients. Again, no statistically significant increase in conversion rates in PAO patients was demonstrated. On the other hand, those patients whose operations were converted because of adhesions were more likely to have undergone PAO.9 Pandya and associates18 concluded that a history of PAO does not increase the conversion risk, but their data were not formally analyzed for this factor.
Our data represent the largest study available to date. We hypothesize that by achieving adequate statistical power we were able to demonstrate the significant impact of PAO on the conversion rate. In this report, we found the conversion risk to be almost doubled in patients with PAO. Interestingly, we found this risk is not increased in patients with multiple PAO beyond the risk of patients with just one PAO. Thus, we conclude that an increased number of PAOs does not increase the risk of conversion beyond the risk acquired by the first PAO.
Nevertheless, even patients with multiple PAOs have a rather high success rate of laparoscopic colon resection (>80%). In our practice, we do not use a history of PAO as a contraindication for a laparoscopic approach, but we counsel patients appropriately regarding the possibility of increased technical difficulty and possible inadvertent complications.
It has been well established that the operative time in laparoscopic surgery tends to be longer than that of conventional open colectomy. Operative time, however, decreases with accumulating experience.2,18 Significantly less blood loss was documented in laparoscopic procedures.21 Based on our data, operative time as well as estimated blood loss was similar in both groups. Thus, we agree with others,8,9 that a history of PAO does not significantly affect operative time or blood loss.
It is clear that patients who undergo conversion of the procedure do not derive the same benefits as patients whose procedure was completed via a laparoscopic approach. Besides the increased costs associated with conversion in multiple studies,7 the risk of intraoperative injuries must be considered. Laparoscopic colon resection has been found comparable to open resection with regards to ureteral or other organ injury.1,2,13 A recent meta-analysis14 of published trials in the English literature comparing laparoscopic and open colon resection for cancer suggests a statistically significantly decreased morbidity after laparoscopic colon resection. Short-term mortality did not appear statistically different, although it was lower in the laparoscopic group.
Reported incidence of iatrogenic bowel injury during laparoscopy ranges from 0.2% to 5%22,23 and is dependent on experience.24 We found an almost 7 times higher risk of inadvertent injury to the intestine in the cohort of patients with PAO. It is unclear how this compares to the risk of inadvertent enterotomy in patients with PAO undergoing open colectomy. This substantial increase in the risk of inadvertent enterotomy appears to be much higher than the reported 21% increased risk in the open intestinal cases.5 More comparative studies are needed to further elucidate this question, both for open and laparoscopic abdominal procedures.
Postoperative ileus is known to be of significantly shorter duration in patients undergoing laparoscopic resection of the colon and rectum.2,7 Interestingly, incidence of postoperative ileus was more than doubled in our patients with a history of PAO compared with those with no PAO. The comparison of length of postoperative ileus in patients with laparoscopic versus open colon and rectal resection was not an objective of this study.
CONCLUSION
Prior abdominal surgery is a risk factor for conversion of laparoscopic surgery of the colon and rectum. Nonetheless, the incidence of successfully completed laparoscopic operations on the colon and rectum remains high in previously operated on patients. Inadvertent enterotomy and postoperative ileus are more common in patients with a history of PAO.
References:
- 1. Clinical Outcomes of Surgical Therapy Study Group A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004; 350: 2050– 2059 [DOI] [PubMed] [Google Scholar]
- 2. Veldkamp R, Gholghesaei M, Bonjer HJ, et al. Laparoscopic resection of colon Cancer: consensus of the European Association of Endoscopic Surgery (EAES). Surg Endosc. 2004; 18: 1163– 1185 [DOI] [PubMed] [Google Scholar]
- 3. Weibel MA, Majno G. Peritoneal adhesions and their relation to abdominal surgery. A postmortem study. Am J Surg. 1973; 126: 345– 353 [DOI] [PubMed] [Google Scholar]
- 4. Beck DE, Opelka FG, Bailey HR, Rauh SM, Pashos CL. Incidence of small-bowel obstruction and adhesiolysis after open colorectal and general surgery. Dis Colon Rectum. 1999; 42: 241– 248 [DOI] [PubMed] [Google Scholar]
- 5. Ellis H, Moran BJ, Thompson JN, et al. Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet. 1999; 353: 1476– 1480 [DOI] [PubMed] [Google Scholar]
- 6. Van Der Krabben AA, Dijkstra FR, Nieuwenhuijzen M, Reijnen MM, Schaapveld M, Van Goor H. Morbidity and mortality of inadvertent enterotomy during adhesiotomy. Br J Surg. 2000; 87: 467– 471 [DOI] [PubMed] [Google Scholar]
- 7. Pikarsky AJ. Update on prospective randomized trials of laparoscopic surgery for colorectal cancer. Surg Oncol Clin N Am. 2001; 10: 639– 653 [PubMed] [Google Scholar]
- 8. Hamel CT, Pikarsky AJ, Weiss E, Nogueras J, Wexner SD. Do prior abdominal operations alter the outcome of laparoscopically assisted right hemicolectomy? Surg Endosc. 2000; 14: 853– 857 [DOI] [PubMed] [Google Scholar]
- 9. Law W, Lee Y, Chu K. Previous abdominal operations do not affect the outcomes of laparoscopic colorectal surgery. Surg Endosc. 2005; 19: 326– 330 [DOI] [PubMed] [Google Scholar]
- 10. Rose J, Schneider C, Yildirim C, Geers P, Scheidbach H, Kockerling F. Complications in laparoscopic colorectal surgery: results of a multicentre trial. Tech Coloproctol. 2004; 8 Suppl 1: s25– 28 [DOI] [PubMed] [Google Scholar]
- 11. Lumley J, Stitz R, Stevenson A, Fielding G, Luck A. Laparoscopic colorectal surgery for cancer: intermediate to long-term outcomes. Dis Colon Rectum. 2002; 45: 867– 872; discussion 872–875 [DOI] [PubMed] [Google Scholar]
- 12. Lujan HJ, Plasencia G, Jacobs M, Viamonte M, 3rd, Hartmann RF. Long-term survival after laparoscopic colon resection for cancer: complete five-year follow-up. Dis Colon Rectum. 2002; 45: 491– 501 [DOI] [PubMed] [Google Scholar]
- 13. Patankar SK, Larach SW, Ferrara A, et al. Prospective comparison of laparoscopic vs. open resections for colorectal adenocarcinoma over a ten-year period. Dis Colon Rectum. 2003; 46: 601– 611 [DOI] [PubMed] [Google Scholar]
- 14. Abraham NS, Young JM, Solomon MJ. Meta-analysis of short-term outcomes after laparoscopic resection for colorectal cancer. Br J Surg. 2004; 91: 1111– 1124 [DOI] [PubMed] [Google Scholar]
- 15. Moloo H, Mamazza J, Poulin EC, et al. Laparoscopic resections for colorectal cancer: does conversion survival? Surg Endosc. 2004; 18: 732– 735 [DOI] [PubMed] [Google Scholar]
- 16. Lacy AM, Garcia-Valdecasas JC, Delgado S, et al. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002; 359: 2224– 2229 [DOI] [PubMed] [Google Scholar]
- 17. Tekkis PP, Senagore AJ, Delaney CP. Conversion rates in laparoscopic colorectal surgery: a predictive model with, 1253 patients. Surg Endosc. 2005; 19: 47– 54 [DOI] [PubMed] [Google Scholar]
- 18. Pandya S, Murray JJ, Coller JA, Rusin LC. Laparoscopic colectomy: indications for conversion to laparotomy. Arch Surg. 1999; 134: 471– 475 [DOI] [PubMed] [Google Scholar]
- 19. Schrenk P, Woisetschlager R, Rieger R, Wayand WU. A diagnostic score to predict the difficulty of a laparoscopic cholecystectomy from preoperative variables. Surg Endosc. 1998; 12: 148– 150 [DOI] [PubMed] [Google Scholar]
- 20. Karayiannakis AJ, Polychronidis A, Perente S, Botaitis S, Simopoulos C. Laparoscopic cholecystectomy in patients with previous upper or lower abdominal surgery. Surg Endosc. 2004; 18: 97– 101 [DOI] [PubMed] [Google Scholar]
- 21. Kiran RP, Delaney CP, Senagore AJ, Millward BL, Fazio VW. Operative blood loss and use of blood products after laparoscopic and conventional open colorectal operations. Arch Surg. 2004; 139: 39– 42 [DOI] [PubMed] [Google Scholar]
- 22. Bishoff JT, Allaf ME, Kirkels W, Moore RG, Kavoussi LR, Schroder F. Laparoscopic bowel injury: incidence and clinical presentation. J Urol. 1999; 161: 887– 890 [DOI] [PubMed] [Google Scholar]
- 23. Wexner SD, Reissman P, Pfeifer J, Bernstein M, Geron N. Laparoscopic colorectal surgery: analysis of 140 cases. Surg Endosc. 1996; 10: 133– 136 [DOI] [PubMed] [Google Scholar]
- 24. Larach SW, Patankar SK, Ferrara A, Williamson PR, Perozo SE, Lord AS. Complications of laparoscopic colorectal surgery. Analysis and comparison of early vs. latter experience. Dis Colon Rectum. 1997; 40: 592– 596 [DOI] [PubMed] [Google Scholar]