Abstract
Adult intussusception is uncommon and requires a surgical approach. Malignancy is associated with 31% (43/137) of small bowel intussusception and 70% (74/106) of large bowel intussusception. Computerized tomography (CT) findings are pathognomonic for this condition. Often, the patient presents with long-standing, nonspecific complaints. A 63-year-old man presented with sudden onset of abdominal pain. CT demonstrated colonic inflammation. A laparoscopic right hemicolectomy for ileocecal intussusception was performed. The pathology report revealed a lipoma of the cecum. The postoperative course was uneventful, and he was discharged the fifth postoperative day. Despite a high incidence of malignancy, colonic or ileocecal intussusception can be successfully treated by laparoscopic resection. Review of the literature and treatment options are discussed.
Keywords: Laparoscopic hemicolectomy, Ileocecal, Adult intussusception
INTRODUCTION
Intussusception of the bowel in adults is uncommon.1 Unlike intussusception in the pediatric population, the classical triad of palpable sausage, current jelly stools, and pain are rarely evident.2–4 Adults generally present with nonspecific findings of variable duration.1,5–8 Diagnosis is based on radiologic or surgical findings. Computerized tomography (CT) results are pathognomonic9,10 and can diagnose intussusception in approximately 72% (23/32) of cases.3–5
Series from major centers report an incidence of adult intussusception of 1.86 cases/year (313/168).2–8,11 Intussusception of the large bowel in adults was associated with malignancy in 70% (74/106) of patients.5–8 Small bowel intussusception,12–15 as well as proven ileocecal and colon benign lesions,16–18 have been successfully resected laparoscopically. Recent trials have shown the efficacy of laparoscopic surgery for resection of colon cancer.19
CASE REPORT
A 63-year-old man presented to the Emergency Department with a 1-day history of mid abdominal pain. The pain was exacerbated by movement and radiated to the right abdomen. He was passing flatus and experiencing nausea, but no vomiting. One week before presentation, he experienced a single episode of hematochezia.
His past medical history was significant for peptic ulcer disease and colonic polyps, which were treated by colonoscopic polypectomy 3 years prior. He had severe coronary artery disease, chronic obstructive pulmonary disease (COPD), and hypertension.
Physical examination revealed a distended abdomen and a tender right lower quadrant, with voluntary guarding. Laboratory studies disclosed a slightly elevated white blood cell count of 11.3 thousand/UL. All other studies, including electrolytes and urinalysis, were within normal limits. A computerized tomography (CT) scan of the abdomen and pelvis revealed a thickened, inflamed cecum, from the ascending colon to the hepatic flexure.
The patient underwent a laparoscopy. The cecum and ascending colon were hemorrhagic and thickened. The appendix was not visible. Because of the ischemic colon secondary to the intussusception, a laparoscopic right hemicolectomy was performed, taking the vessels at the root of the mesentery. Since the colon was compromised, the intussusception was not reduced intraoperatively. Pathology of the cecum revealed hemorrhage, acute inflammation, and ulceration. A lipoma of the ileocecal valve was identified as the lead point.
The postoperative course was uneventful. Bowel function returned, and the patient was passing flatus by his second postoperative day; he was discharged on the fifth postoperative day.
DISCUSSION
In 1956, Dean et al6 classified adult intussusception as enteric; colocolic; ileocecal, with the ileocecal valve as lead point; and ileocolic, with the ileum through the ileocecal valve. The most common type is enteric, occurring in 43% of patients (Table 1).1,4,6,7,8
Table 1.
| Type | Percent |
|---|---|
| Enteric | 43% (331/775) |
| Colocolic | 22% (172/775) |
| Ileocecal | 21% (162/775) |
| Ileocolic | 14% (110/775) |
Although some series classified intussusception as a small bowel versus a large bowel etiology, Dean's classification best defined location and possible etiology. Gupta11 and Azar5 reported that 76% (78/103) of cases were small bowel lesions.
Intussusception in adults has been reported in patients as young as 13 and as old as 90 years of age,5,7,8,11 the highest incidence occurred in the 30- to 50-year-old age group.1,4,8 The male to female ratio was approximately 2:1.1,4,5
The incidence of adult intussusception in 8 worldwide centers is 1.86 cases/year (313/168)2–8,11 (range 1 case/ year/center, 34/368 to 4 cases/year/center 45/1111). Five series from major centers in the United States report an incidence of 1.7 cases/year (249/146).2,5–8
Adults commonly presented with nonspecific signs and symptoms similar to a bowel obstruction (Table 2). The pediatric signs and symptoms, which included a classic triad of palpable sausage, current jelly stools, and pain, occurred infrequently in adults.4 Our patient presented with an acute onset of nausea and abdominal pain, as well as a recent gastrointestinal bleed.
Table 2.
Signs and Symptoms Associated With Adult Intussusception
Symptoms could be acute or chronic. The duration was reported as less than 7 days in 34% (30/88) of patients and between 7 days and 3 months in 48% (42/88).3,8,11 Gupta11 and Steubenbord8 reported 22% (18/79) experienced symptoms of more than 3 months’ duration; some patients have reported symptoms lasting up to one year.5
Laboratory studies were nonspecific for adult intussusception, unless bowel perforation or compromise occurred.7 Contrast studies were rarely used in adults and not utilized to reduce the intussusception, as in the pediatric population. Ultrasound could demonstrate a target or donut sign, but ultrasounds were difficult to interpret because of increased intestinal gas.9,10 Ultrasound diagnosed intussusception in 33% (1/3) of cases3; barium enema in 36% (8/22)3,5; plain radiographs in 60%9; and CT scan in 72% (23/32).3–5
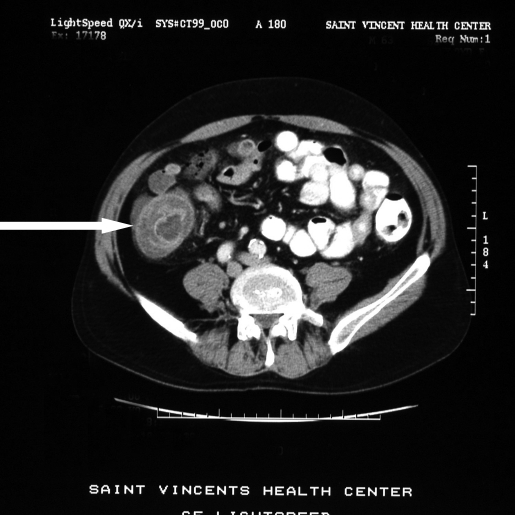
On CT, intussusception appeared as one of 3 patterns: a target lesion; a sausage mass with layers; or a reniform mass caused by edema, mural thickening, and vascular compromise.9,10 In our case, though a target sign was present, it was not identified preoperatively (Figures 1 and 2).
Figure 1.
Computed tomographic scan demonstrating the target sign in an ileocecal intussusception.
Figure 2.
Computed tomographic scan demonstrating reniform mass secondary to edema, mural thickening, and vascular compromise.
Although a positive CT scan was diagnostic, CT often failed to establish the cause.10 Occasionally, a lipoma, metastatic disease, as well as bowel obstruction and air fluid levels could also be identified.9,10
The cause of intussusception in adults varied by location. Large bowel lead points were more frequently malignant than small bowel lead points. The incidence of either primary or metastatic malignancy in the small bowel was 31% (43/137)5–8 compared with 70% (74/106) in colon lesions.5–8 Benign lesions, including lipomas that cause intussusception were predominantly found in the cecum and terminal ileum.5,20 The most common benign lesions of the colon causing intussusception were lipomas.20 Postoperative mortality was 5% (10/191) and was related to sepsis or metastatic disease.3,5,7,8,11
Laparoscopic management of intussusception in adults has been described for small12–16 and large bowel.15,17,18 Reports have identified a benign cecal lipoma as the lead point, before laparoscopic resection.15,17 Anastomoses were performed extracorporeally. Recent studies describing outcomes of laparoscopic resection of colon cancer19 support a similar approach for ileocecal or colocolic intussusception, regardless of the pathology.
CONCLUSION
Adult intussusception is very rare; most surgeons will encounter only 1 or 2 cases in their entire careers.2 With advances in laparoscopic surgical techniques and outcomes, the experienced surgeon can approach this disease laparoscopically. The presence of malignancy should be considered and proximal vascular pedicle ligation should be performed. Reduction of the intussusception may be performed in enteric lesions, but the risk of perforation and dissemination of malignant cells exists. Primary resection using oncologic principles presents the best option.
Acknowledgments
The author acknowledges Phyllis J. Kuhn, PhD, Lake Erie Research Institute for her review and comments.
References:
- 1. Donhauser JL, Kelly EC. Intussusception in the adult. Am J Surg. 1950; 79: 673– 677 [DOI] [PubMed] [Google Scholar]
- 2. Begos DG, Sandor A, Modin IM. The diagnosis and management of adult intussusception. Am J Surg. 1997; 173: 88– 94 [DOI] [PubMed] [Google Scholar]
- 3. Tan KY, Tan SM, Tan AG, Chen CY, Chng HC, Hoe MN. Adult intussusception: experience in Singapore. Aust N Z J Surg. 2003; 73: 1044– 1047 [DOI] [PubMed] [Google Scholar]
- 4. Toso C, Erne M, Lenzlinger PM, et al. Intussusception as a cause of bowel obstruction in adults. Swiss Med Weekly. 2005; 135: 87– 90 [DOI] [PubMed] [Google Scholar]
- 5. Azar T, Berger DL. Adult intussusception. Ann Surg. 1997; 226: 134– 138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dean DL, Ellis FH, Sauer WG. Intussusception in adults. Arch Surg. 1956; 73: 6– 11 [DOI] [PubMed] [Google Scholar]
- 7. Nagorney DM, Sarr MG, McIlrath DC. Surgical management of intussusception in the adult. Ann Surg. 1981; 193: 230– 236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Stubenbord WT, Thorbjarnarson B. Intussusception in adults. Ann Surg. 1970; 172: 306– 310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Byrne AT, Goeghegan T, Govender P, Lyburn ID, Colhoun E, Torreggiani WC. The imaging of intussusception. Clin Radiol. 2005; 60: 39– 46 [DOI] [PubMed] [Google Scholar]
- 10. Gayer G, Zissin R, Apter S, Papa M, Hertz M. Adult intussusception—a CT diagnosis. Br J Radiol. 2002; 75: 185– 190 [DOI] [PubMed] [Google Scholar]
- 11. Gupta S, Udupa KN, Gupa S. Intussusception in adults. Int Surg. 1976; 61: 231– 233 [PubMed] [Google Scholar]
- 12. Alonso V, Targarona EM, Bendahan GE, et al. Laparoscopic treatment for intussusception of the small intestine in the adult. Surg Laparosc Endosc Percutan Tech. 2003; 13: 394– 396 [DOI] [PubMed] [Google Scholar]
- 13. El-Sherif OF. Laparoscopy in the management of an adult case of small bowel intussusception. Surg Laparos Endosc. 1998; 8: 21– 25 [PubMed] [Google Scholar]
- 14. Harrison LE, Kim SH. Images in clinical medicine. Intussusception of the small bowel. N Engl J Med. 2004; 351: 379. [DOI] [PubMed] [Google Scholar]
- 15. Park KT, Kim SH, Sony TJ, Moon HY. Laparoscopic-assisted resection of ileal lipoma causing ileo-ileo-colic intussusception. J Korean Med Sci. 2001; 16: 119– 122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chiu CC, Wei PL, Huang MT, Wang W, Chen TC, Lee WJ. Laparoscopic treatment of iIleocecal intussusception caused by primary ileal lymphoma. Surg Laparosc Endosc Percutan Tech. 2004; 14: 93– 95 [DOI] [PubMed] [Google Scholar]
- 17. Hacham DJ, Saibil F, Wilson S, Litwin D. Laparoscopic management of intussusception caused by colonic lipomata: a case report and review of the literature. Surg Laparosc Endosc. 1996; 6: 155– 159 [PubMed] [Google Scholar]
- 18. Yamaguchi S, Fujii S, Ike H, Shimada H. Laparoscopic reduction of appendicocecal intussusception due to mucinous cystadenoma in an adult. JSLS. 2004; 8: 279– 282 [PMC free article] [PubMed] [Google Scholar]
- 19. Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004; 350: 2050– 2059 [DOI] [PubMed] [Google Scholar]
- 20. Hozo I, Perkovic D, Grandic L, Klaudije G, Simunic M, Piplovic T. Colonic lipoma intussusception: a case report. Med Arh. 2004; 58: 382– 383 [PubMed] [Google Scholar]