Abstract
Background:
To develop an evidence-based protocol for the management of perforated sigmoid diverticular disease.
Methods:
A search of the literature was undertaken. All publications pertaining to perforated sigmoid diverticular disease were analyzed and then categorized according to their level of evidence. Recommendations were then made on the basis of this.
Results:
Multiple case reports suggest that primary closure of perforation of sigmoid diverticula is safe in the absence of peritoneal contamination.
Conclusions:
A 2-stage laparoscopic approach incorporating the principles of damage limitation surgery may be a safe strategy in the management of perforated diverticular disease.
Keywords: Sigmoid colon, Diverticulitis, Perforation, Laparoscopy
INTRODUCTION
The management of acute diverticulitis complicated by perforation traditionally has been the Hartmann's procedure, which may be associated with significant morbidity and mortality and the unpleasantness of a colostomy. Experience in minimal access surgery has increased, and an established place now exists for laparoscopic management of perforated sigmoid diverticular disease (PDD). We present a case study of a patient presenting with perforated acute diverticulitis managed with laparoscopic oversewing, present a systematic review of the literature, and suggest a management protocol for the laparoscopic management of this surgical emergency.
CASE REPORT
A 50-year-old male patient presented with a 24-hour history of central abdominal pain localized to the right iliac fossa. This was his first hospital attendance with this complaint. Past medical and family history were not of note. The patient appeared flushed and was afebrile. His vital signs were normal, and his right iliac fossa was tender when palpated. His white cell count was 8600 mL-1 (normal range, 4300 to 10 800) and serum C-reactive peptide level was 129 mgL-1 (normal range, <3). Diagnostic laparoscopy was performed at which a localized perforation of a sigmoid diverticulum with surrounding abscess cavity adherent to the anterior abdominal wall was seen (Figure 1).
Figure 1.
Intraoperative photograph of small perforation in sigmoid colon.
Copious lavage of the peritoneal cavity was carried out followed by laparoscopic suture repair of the perforation and insertion of a peritoneal drain. A course of broadspectrum antibiotics was completed. The patient's postoperative course was uneventful. His bowels returned to normal function by the fourth postoperative day when the peritoneal drain was removed. He was discharged from the hospital on day 5.
The patient subsequently underwent a barium enema study 6 weeks following his in-patient episode, which confirmed the presence of sigmoid diverticular disease. No extravasation of contrast was seen on the study. Risk and benefit of elective surgery were discussed, and definitive surgery was deferred.
METHODS
A literature search of Medline from 1950 to September 2007 using the OVID interface combined with manual cross-referencing was performed by using the following strategy:
Limit (sigmoid.mp. or Colon, Sigmoid/ AND Intestinal Perforation/or perforation.mp. AND laparoscopy.mp. or Laparoscopy/) to (humans and English language)
All publications pertaining to the laparoscopic management of perforated sigmoid diverticular disease were analyzed and then categorized according to their level of evidence. Further manual cross-referencing of cited papers was performed. Individual case reports were not included. Data were then categorized by management strategy and recommendations were then made on the basis of the available data.
RESULTS
Forty-two publications were found, 25 of which were of sufficient quality and relevance to be included in this review.
Classification of Perforated Sigmoid Diverticular Disease
The modified Hinchey system is a well-recognized method of classifying acute diverticulitis. Hinchey described 2 distinct evolutionary processes of perforated diverticular disease: first, where the neck of the diverticulum is obliterated and the peritonitis is purulent, and second where the neck fails to seal and feculent perforation occurs.1
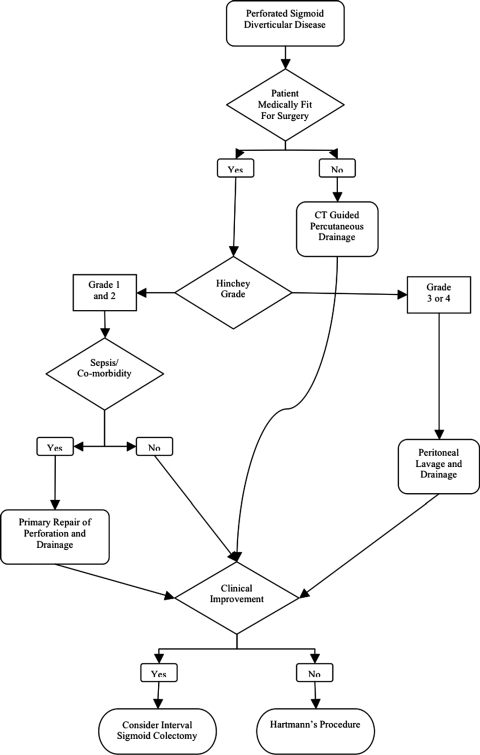
Classification is important to both select appropriate management and also to compare and pool outcome data from the experience of different surgeons. We suggest that management should be along the lines of a classification based on the Hinchey system (Table 1, Figure 2).
Table 1.
Modified Hinchey Classification of Acute Diverticulitis [modified from (9) and (26)]
| Stage | Characteristics |
|---|---|
| 0 | Mild clinical diverticulitis (left lower quadrant abdominal pain, low-grade fever, leukocytosis, no imaging information) |
| 1a | Confined pericolic inflammation, no abscess |
| 1b | Confined pericolic abscess (abscess or phlegmon may be palpable; fever; severe, localized abdominal pain) |
| 2a | Distant abscess amenable to percutaneous drainage |
| 2b | Complex abscess associated with/without fistula |
| 3 | Generalized purulent peritonitis, no communication with bowel lumen |
| 4 | Feculent peritonitis, open communication with bowel lumen |
| Complications | Fistula, obstruction (large bowel or small bowel) |
Figure 2.
Proposed laparoscopic management algorithm for perforated sigmoid diverticular disease.
Management Once Perforated Sigmoid Diverticular Disease Is Confirmed
Although optimum treatment for perforated diverticular disease is resection, a trend now exists towards “down staging” surgery prior to definitive resection.2 A study from Germany suggests that obesity, cardiac risk factors, and most significantly immunosuppression are predictive of morbidity and mortality.3 Hence, the rationale for a “damage limitation” approach to the initial operation to pave the way for resection when the patient is systemically improved.
Two-Stage Laparoscopic Management of Perforated Sigmoid Diverticular Disease
A retrospective review from Australia4 reports on researchers' experience with 14 patients with PDD managed laparoscopically. Ten patients had Hinchey grade 3 purulent peritonitis, 2 had grade 2 contamination, and 2 had grade 4 feculent peritonitis. All patients were treated initially with laparoscopic lavage and drainage. Eleven patients (79%) improved and were discharged following a median of 6.5 days (range, 5 to 32), whereas 3 patients did not improve and underwent acute resection. Of the 11 that settled, 8 patients subsequently underwent elective resection (7 laparoscopic) without a stoma at a mean interval of 6 weeks.
Faranda et al5 report on a series of 18 patients with peritonitis secondary to perforated acute diverticulitis successfully managed with emergency laparoscopy. Patients had extensive peritoneal lavage, the sigmoid lesion was stuck with biologic glue, the peritoneum was drained, and antibiotic therapy was given. No patient had a wound abscess or residual deep collections, and mean postoperative stay was 8 days. Fourteen patients underwent elective sigmoid resection (13 laparoscopic).
A series of 29 patients6 with purulent perforated sigmoid diverticulitis successfully initially managed with laparoscopic lavage and peritoneal drain insertion reported no serious complications, and all cases resolved without further intervention.
More recently, in a prospective trial from Ireland7 of 92 patients with perforated diverticular disease (Hinchey grades 2 and 3) managed by laparoscopic lavage, peritoneal drainage and antibiotics showed favorable results. The authors report that 89% of patients made an uneventful recovery; morbidity and mortality rates were 4% and 3%, respectively. Two instances of persistent pelvic abscesses, one managed by percutaneous drainage and one by an open Hartmann's procedure, were reported; and 2 patients re-presented with diverticulitis during the mean follow-up period of 36 months.
Two-Stage Management of Perforated Diverticular Disease in Patients Medically Unfit for Surgery
With patients in whom the risk of anesthesia is prohibitively high due to comorbidity, computerized tomography (CT) may be performed to confirm the diagnosis of PDD and establish percutaneous peritoneal drainage under CT control. A number of small series8–10 of between 10 and 16 patients report on short-term successes of radiological placement of peritoneal drains for PDD.
Single-Stage Laparoscopic Surgery for Perforated Sigmoid Diverticular Disease
Hinchey Class 0—Postcolonoscopy.
Several studies report that direct closure of the perforation has been successfully used. Lovisetto et al11 report laparoscopic suture repair and creation of diverting loop colostomy of an iatrogenic perforated sigmoid diverticulum following colonoscopy. Their patient was discharged following 8 uneventful postoperative days. Other papers12–14 reports on a successful laparoscopic suture repair of an iatrogenic postcolonoscopy sigmoid perforation without diverting colostomy.
A study15 of a recent case series of laparoscopic repair of iatrogenic postcolonoscopic sigmoid diverticular perforation reports on 11 attempted (6 successful) laparoscopic repairs, with a mean perforation size of 2.7cm. Three patients were immediately converted to open repair; one patient who underwent repair of a 4-cm perforation leaked and had a further open repair. Laparoscopy of one patient who underwent a delayed laparotomy for sepsis had an initially nondiagnostic laparoscopy.
A case report16 of laparoscopic repair of an iatrogenic sigmoid diverticular perforation in which the Endostich device was used following colonoscopy resulted in reoperation at day 8 following repair. The authors suggest that the nature of the Endostich device may have lead to inadequate bites of the bowel being taken in the closure.
A review17 of 197 laparoscopic colonic wall biopsies for slow motility in children reported 8 patients (2 not recognized at index operation) requiring closure of mucosal perforations using endoloops. All 8 recovered well with no complications.
In a gynecological series of 262 women undergoing pelvic laparoscopy, Nezhat et al18 describe a technique to identify iatrogenic sigmoid perforation. Rigid sigmoidoscopy and air insufflation into the colon is performed whilst the pelvis filled with saline is observed for air bubbles. They report that 4 bowel injuries as well as one incomplete repair were identified using this technique and repaired with laparoscopic suturing with no adverse events.
The successful use of the laparoscopic linear stapler to repair postcolonoscopy diverticular perforation was described by Hayashi et al.19 Yamamoto et al20 report a series of 5 patients with iatrogenic postcolonoscopy perforated sigmoid diverticula who were successfully treated laparoscopically by application of a linear stapler after the edges of the perforations had been aligned by passing stay sutures through each side of the perforations. Hinchey Class 1 and 2.
A report21 of a series of 18 patients from the Cleveland clinic undergoing laparoscopic sigmoid colectomy for diverticulitis suggests that resection is feasible for class 1 disease with no morbidity, mortality, or conversion to open surgery necessary. However, half of those operated on for class 2 disease necessitated conversion to open surgery, and the incidence of morbidity was 33.3%.21 Reports22,23 of other single-center series of laparoscopic sigmoid colectomy for class 1 and 2 diverticulitis have reported low conversion and complication rates.
A multicenter study24 of laparoscopic resections for diverticulitis revealed a high rate of conversion to open surgery and a high rate of complications, 18.2% and 28.9% (31.8% following conversion), respectively. The authors conclude that such difficult cases be the preserve of highly experienced surgeons. This view is further supported by the results of a multi-center study showing that more experienced surgeons performed laparoscopic sigmoid colectomy for more complicated cases and had fewer complications than did less experienced surgeons.25 Hinchey Class 4.
A few reports26,27 exist in the literature of favorable results with resection and primary anastomosis for class 4 diverticulitis in open surgery. The authors stress that absence of comorbidity, good response to resuscitation, and availability of intensive care facilities were key to success in these highly selected cases.
Secondary Management of Perforated Diverticular Disease
In 1999, a consensus conference28 held by the European Association of Endoscopic Surgery concluded that after 2 attacks of diverticulitis, sigmoid colectomy should be considered and that laparoscopic sigmoid colectomy should be performed for either uncomplicated cases or after abscess had been drained percutaneously. However, these and similar North American recommendations have recently been called into question by investigators29 studying 150 patients with diverticulitis who found that having more than 2 episodes of diverticulitis does not increase risk of presenting with perforated diverticular disease or of surgical morbidity or mortality. We feel that currently contemporary data are insufficient to change management in this respect.
CONCLUSION
Avoiding need for colostomy is a very attractive prospect for patients and surgeons. Current evidence on the 2-staged laparoscopic approach to PDD consists of case series (level 2).
Additional larger case series and controlled trials are required to establish the benefit of laparoscopic management of PDD in the wider surgical community.
References:
- 1.Hinchey EJ, Schaal PG, Richards GK. Treatment of perforated diverticular disease of the colon. Adv Surg. 1978;12:85–109 [PubMed] [Google Scholar]
- 2.Formento E, Guglielminotti P, Reggio D, Saracco M, Patelli E. Diverticular disease and its treatment [in Italian]. Minerva Chir. 1997;52 3:261–270 [PubMed] [Google Scholar]
- 3.Hansen O, Graupe F, Stock W. Prognostic factors in perforating diverticulitis of the large intestine [in German]. Chirurg. 1998;69 4:443–449 [DOI] [PubMed] [Google Scholar]
- 4.Taylor CJ, Layani L, Ghusn MA, White SI. Perforated diverticulitis managed by laparoscopic lavage.[see comment]. Aust N Z J Surg. 2006;76 11:962–965 [DOI] [PubMed] [Google Scholar]
- 5.Faranda C, Barrat C, Catheline JM, Champault GG. Two-stage laparoscopic management of generalized peritonitis due to perforated sigmoid diverticula: eighteen cases. Surg Laparosc Endosc Percutan Tech. 2000;139;103:135–8; discussion 139–141 [DOI] [PubMed] [Google Scholar]
- 6.Franklin ME, Anwar R, Trevino JM, Ggonzalez JJ, Jaramillo E, Glass JL. Laparoscopic Drainage of Perforated Diverticulitis with Peritonitis. San Antonio, Texas: Texas Endosurgery Institute; 2006:S1–S32 [Google Scholar]
- 7.Myers E, Hurley M, O'Sullivan GC, Kavanagh D, Wilson I, Winter DC. Laparoscopic peritoneal lavage for generalized peritonitis due to perforated diverticulitis. Br J Surg. 2008;95 1:97–101 [DOI] [PubMed] [Google Scholar]
- 8.Hamy A, Paineau J, Société de chirurgie viscérale del'ouest (SCV) Percutaneous drainage of perisigmoid abscesses of diverticular origin [in French]. Ann Chir. 2001;126 2:133–137 [DOI] [PubMed] [Google Scholar]
- 9.Kaiser AM, Jiang JK, Lake JP, et al. The management of complicated diverticulitis and the role of computed tomography. Am J Gastroenterol. 2005;100 4:910–917 [DOI] [PubMed] [Google Scholar]
- 10.Mutter D, Bouras G, Forgione A, Vix M, Leroy J, Marescaux J. Two-stage totally minimally invasive approach for acute complicated diverticulitis. Colorectal Dis. 2006;8 6:501–505 [DOI] [PubMed] [Google Scholar]
- 11.Lovisetto F, Zonta S, Rota E, et al. Left pneumothorax secondary to colonoscopic perforation of the sigmoid colon: a case report. Surg Laparosc Endosc Percutan Tech. 2007;17 1:62–64 [DOI] [PubMed] [Google Scholar]
- 12.Mehdi A, Closset J, Gay F, Deviere J, Houben J, Lambilliotte J. Laparoscopic treatment of a sigmoid perforation after colonoscopy. Case report and review of literature. [Review]. Surg Endosc. 1996;10 6:666–667 [DOI] [PubMed] [Google Scholar]
- 13.Schlinkert RT, Rasmussen TE. Laparoscopic repair of colonoscopic perforations of the colon. J Laparoendosc Surg. 1994;4 1:51–54 [DOI] [PubMed] [Google Scholar]
- 14.Velez MA, Riff DS, Mule JM. Laparoscopic repair of a colonoscopic perforation. Surg Endosc. 1997;11 4:387–389 [DOI] [PubMed] [Google Scholar]
- 15.Hansen AJ, Tessier DJ, Anderson ML, Schlinkert RT. Laparoscopic repair of colonoscopic perforations: indications and guidelines. J Gastrointest Surg. 2007;11 5:655–659 [DOI] [PubMed] [Google Scholar]
- 16.Fonso-Ballester R, Lo Pez-Mozos F, Mart-Obiol R, Garcia-Botello SA, Lledo-Matoses S. Laparoscopic treatment of endoscopic sigmoid colon perforation: a case report and literature review. Surg Laparosc Endosc Percutan Tech. 2006;16 1:44–46 [DOI] [PubMed] [Google Scholar]
- 17.King SK, Sutcliffe JR, Hutson JM. Laparoscopic sero-muscular colonic biopsies: a surgeon's experience. J Pediatr Surg. 2005;40 2:381–384 [DOI] [PubMed] [Google Scholar]
- 18.Nezhat C, Seidman D, Nezhat F, Nezhat C. The role of intraoperative proctosigmoidoscopy in laparoscopic pelvic surgery. J Am Assoc Gynecol Laparosc.2004;11 1:47–49 [DOI] [PubMed] [Google Scholar]
- 19.Hayashi K, Urata K, Munakata Y, Kawasaki S, Makuuchi M. Laparoscopic closure for perforation of the sigmoid colon by endoscopic linear stapler. [Review] Surg Lapaosc Endosc. 1996;6 5:411–413 [PubMed] [Google Scholar]
- 20.Yamamoto A, Ibusuki K, Koga K, Taniguchi S, Kawano M, Tanaka H. Laparoscopic repair of colonic perforation associated with colonoscopy: use of passing sutures and endoscopic linear stapler. Surg Laparosc Endosc Percutan Tech. 2001;11 1:19–21 [PubMed] [Google Scholar]
- 21.Sher ME, Agachan F, Bortul M, Nogueras JJ, Weiss EG, Wexner SD. Laparoscopic surgery for diverticulitis. Surg Endosc. 1997;11 3:264–267 [DOI] [PubMed] [Google Scholar]
- 22.Bottger TC, Muller M, Terzic A, Hermeneit S, Rode-horst A. Laparoscopic resection with primary anastomosis in Hinchey stages I and II without previous abscess drainage [in German]. Chirurg. 2007;78 5:454, 456–4, 460 [DOI] [PubMed] [Google Scholar]
- 23.Pugliese R, Di LS, Sansonna F, et al. Laparoscopic treatment of sigmoid diverticulitis: a retrospective review of 103 cases. Surg Endosc. 2004;18 9:1344–1348 [DOI] [PubMed] [Google Scholar]
- 24.Kockerling F, Schneider C, Reymond MA, et al. Laparoscopic resection of sigmoid diverticulitis. Results of a multicenter study. Laparoscopic Colorectal Surgery Study Group. Surg Endosc. 1999;13 6:567–571 [DOI] [PubMed] [Google Scholar]
- 25.Scheidbach H, Schneider C, Rose J, et al. Laparoscopic approach to treatment of sigmoid diverticulitis: changes in the spectrum of indications and results of a prospective, multicenter study on 1,545 patients. Dis Colon Rectum. 2004;47 11:1883–1888 [DOI] [PubMed] [Google Scholar]
- 26.Medina VA, Papanicolaou GK, Tadros RR, Fielding LP. Acute perforated diverticulitis: primary resection and anastomosis? Conn Med. 1991;55 5:258–261 [PubMed] [Google Scholar]
- 27.Richter S, Lindemann W, Kollmar O, Pistorius GA, Maurer CA, Schilling MK. One-stage sigmoid colon resection for perforated sigmoid diverticulitis (Hinchey Stages III and IV). World J Surg. 2006;30 6:1027–1032 [DOI] [PubMed] [Google Scholar]
- 28.Kohler L, Sauerland S, Neugebauer E. Diagnosis and treatment of diverticular disease: results of a consensus development conference. The Scientific Committee of the European Association for Endoscopic Surgery. Surg Endosc. 1999;13 4:430–436 [DOI] [PubMed] [Google Scholar]
- 29.Chapman JR, Dozois EJ, Wolff BG, Gullerud RE, Larson DR. Diverticulitis: a progressive disease? Do multiple recurrences predict less favorable outcomes? Ann Surg. 2006;243 6:876–830 [DOI] [PMC free article] [PubMed] [Google Scholar]