Abstract
Background:
Management of empyema in children has progressed from open thoracotomy to video-assisted thoracoscopic surgery (VATS). The purpose of the present study was to evaluate the efficacy and safety of VATS in children with multiloculated empyemas.
Methods:
Nine children (mean age, 4 years; range, 21 months to 13 years) with empyema, in whom multiple loculations were found on computed tomography, were treated with VATS from January, 1994, to November, 1996. All patients underwent VATS under general anesthesia, with drainage of the empyemas, decortication, and placement of chest tubes under direct vision.
Results:
In all nine patients, VATS was successful. Average operating time was 120 minutes. Blood loss was insignificant, except in one patient who needed an intraoperative blood transfusion. This child required extensive decortication, with blood oozing from raw areas. All patients recovered well, with no recurrences to date. An algorithm for the use of VATS in the treatment plan for children with empyema was established.
Conclusion:
VATS provides safe and effective treatment in the management of pediatric empyema. Moreover, it avoids lengthy hospitalization, prolonged intravenous antibiotic therapy, and unnecessary pain and stress secondary to placement of chest tubes without anesthesia.
Keywords: Adolescence, Child, Empyema, Pleural, Thoracoscopy, Video recording
INTRODUCTION
Use of thoracoscopy to manage empyema has been gradually increasing in the adult population.1–3 Technological advances allow for sophisticated fiberoptic examination of the thorax by video-assisted thoracoscopy. The safety of thoracoscopy for the diagnosis of intrathoracic lesions in children has been previously established.4 Recent reports demonstrate the efficacy and safety of video-assisted thoracoscopic surgery (VATS) in the evacuation and debridement of empyema in children.5–8 The purpose of the present study was to evaluate retrospectively our use of VATS for treating empyema in children, and also its outcomes when used aggressively before chest tube management 9,10 in terms of length of recovery and hospitalization.
PATIENTS AND METHODS
Nine children with empyema were treated with VATS from January, 1994, to November, 1996. Mean age was 4 years (range, 21 months to 13 years). There were three males and six females. Three patients had tube thoracostomy prior to VATS because of respiratory compromise. Tube thoracostomy provided some temporary relief, but it failed to resolve the empyema. The remaining six patients were treated by VATS as a primary drainage procedure within 72 hours of admission.
Computerized tomography (CT) in all patients demonstrated significant loculation of the empyema. In three cases the empyemas were on the left side, and in six cases on the right side. All patients had fever and other symptoms related to empyema. Six patients had significant respiratory distress at presentation, five of whom required oxygen therapy by mask, and one who required endotracheal intubation and ventilation. All patients received oral or intravenous antibiotic therapy before admission. Intravenous broad spectrum antibiotics were continued until discharge, and given orally at home for a total of two weeks. Urokinase was used, as previously described,11 in two patients postoperatively to unblock the chest tube.
SURGICAL TECHNIQUE
The VATS technique we used has been previously described by the senior author (GS).6 The procedure is performed using general endotracheal anesthesia, with the patient placed in a supine position with the affected side of the chest elevated at 45 degrees. This position provides adequate exposure and prevents the overflowing of secretions from the affected lung to the opposite healthy side. (In the present series, the first three patients underwent the procedure in a posterolateral thoracotomy position, and the last six underwent it in the supine position described here.) A single lumen endotracheal tube is used. Appropriate monitoring is essential, especially oxygen saturation and endtidal carbon dioxide measurement.
The first trocar is placed in the 5th or 6th intercostal space, midaxillary line, using an open technique. After space is created in this area, one or two other ports are placed. These ports can be 5 or 10 mm, depending on the size of the child. Continuous flow of carbon dioxide is used for lung deflation.6 Carbon dioxide pressure over 8 mm Hg is usually not necessary. Careful attention must be paid to possible displacement of the mediastinum with subsequent impairment in oxygenation, decreased blood return to the heart and carbon dioxide retention. Attentiveness to displacement is especially important in small children, in whom the mediastinum can be more easily displaced than in older children or adults.
Removal of thick fibrin clots and decortication is done by using ring forceps or biliary stone clamps, like the ones used for common bile duct exploration. These clamps, which are available in a variety of sizes and shapes, can be introduced in the pleural cavity directly, without the use of the trocars. Temporary pressure can be applied with the tip of the finger to avoid losing carbon dioxide pressure. Copious antibiotic warm irrigation is used to clean the pleural cavity. Finally, one or two chest tubes are placed under direct visualization.
RESULTS
VATS proved to be safe and effective in all cases. After surgery, patients were admitted to the pediatric intensive care unit for an overnight stay, and were discharged to a regular pediatric floor the next day. Fever subsided within 24 hours in five patients, and within 48 hours in two others. Two patients continued to have low-grade fever for 72 hours, and the fever resolved after the chest tubes were successfully unblocked with the urokinase protocol.11 The average operating time was 120 minutes. Blood loss was insignificant, except in one patient who needed an intraoperative blood transfusion. This child required extensive decortication, with blood oozing from raw areas. Cultures were taken from the pleural cavity in all patients. Only two patients had positive cultures: one had Streptococcus viridans, and the other had Group A streptococcus. Chest tubes were removed postoperatively in three days in two patients, four days in three patients, five days in three patients and ten days in one patient. This latter child initially presented with a pyopneumothorax and had a persistent bronchopleural fistula that closed spontaneously about eight days post-VATS.
Patients were discharged home the day after the chest tubes were removed. All patients had significant improvement demonstrated by chest films prior to discharge. Follow-up after discharge demonstrated complete resolution of the empyema with lung re-expansion in all patients, and with no recurrences to date.
DISCUSSION
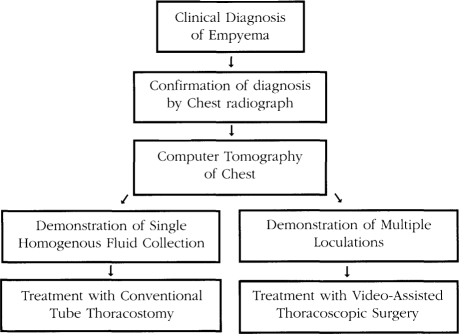
Thoracoscopy has made great advances since its inception. With the advent of fiberoptics and better instrumentation, more thoracoscopic procedures are now possible.12,13 The safety of thoracoscopy has been well established.1,3,14 The successful use of VATS for drainage of empyema and pulmonary decortication in adults and children has been previously reported.1–8 Because of our previously successful experience with the use of VATS for drainage of empyemas and pulmonary decortication in children,6 we designed an algorithm in which VATS is used to treat empyema early in the course of the disease (Figure 1).
Figure 1.
Management protocol for empyema in children.
After the empyema has been diagnosed clinically and confirmed by chest radiography, we proceed with CT of the chest. If a single homogenous fluid collection is found, then we treat the patient with tube thoracostomy, using either general anesthesia or conscious sedation. If loculations are found, then we treat the patient with VATS drainage and decortication as described above.
We believe that by following this management protocol, we have achieved a faster recovery in our group of patients, as compared with that achieved by other treatment options such as repeated chest tube insertion to drain multiple loculations and long-term antibiotic therapy.9–10 Although use of open drainage and decortication is effective, and it has been used extensively by us in the past, VATS is superior because it provides complete visualization of the pleural cavity, removal of pus, fibrin clots and fibrin peel under direct vision, with better cosmetic results and tolerable postoperative pain.
In conclusion, VATS is a safe and effective treatment modality in the management of empyema in children. It should be used early, especially when multiple loculations are present and when simple tube thoracostomy has failed. Moreover, aggressive use of VATS can avoid lengthy hospitalization, prolonged intravenous antibiotic therapy, and unnecessary pain and stress secondary to placement of chest tubes without anesthesia.
References:
- 1. Ridley PD, Braimbridge MV. Thoracoscopic debridement and pleural irrigation in the management of empyema thoracis. Ann Thorac Surg. 1991; 51: 46l–464 [DOI] [PubMed] [Google Scholar]
- 2. Hutter JA, Harari D, Braimbridge MV. The management of empyema thoracis by thoracoscopy and irrigation. Ann Thorac Surg. 1985;39:517–520 [DOI] [PubMed] [Google Scholar]
- 3. Ferguson MK. Thoracoscopy for empyema, bronchopleural fistula, and chylothorax. Ann Thorac Surg. 1993;56:644–645 [DOI] [PubMed] [Google Scholar]
- 4. Rodgers BM, Talbert JL. Thoracoscopy for diagnosis of intrathoracic lesions in children. J Pediatr Surg. 1976;11:703–708 [DOI] [PubMed] [Google Scholar]
- 5. Kern JA, Rodgers BM. Thoracoscopy in the management of empyema in children. J Pediatr Surg. 1993;28:1128–1132 [DOI] [PubMed] [Google Scholar]
- 6. Stringel G, Hartman AR, Marandi P. Video-assisted thoracoscopy for pulmonary decortication in children. Pediatr Surg Int. 1995;10:205–206 [Google Scholar]
- 7. Stovroff M, Teague G, Heiss KF, Parker P, Ricketts RR. Thoracoscopy in the management of pediatric empyema. J Pediatr Surg. 1995;30:1211–1215 [DOI] [PubMed] [Google Scholar]
- 8. Silen ML, Weber TR. Thoracoscopic debridement of loculated empyema thoracis in children. Ann Thorac Surg. 1995;59:1166–1168 [DOI] [PubMed] [Google Scholar]
- 9. Gocmen A, Kiper N, Toppare M, Ozcelik U, Cengizlier R, Cetinkaya F. Conservative treatment of empyema in children. Respiration. 1993;60:182–185 [DOI] [PubMed] [Google Scholar]
- 10. Hoff SJ, Neblett WW, Edwards KM, et al. Parapneumonic empyema in children: decortication hastens recovery in patients with severe pleural infections. Pediatr Infect Dis J. 1991;10:194–199 [PubMed] [Google Scholar]
- 11. Stringel G, Hartman AR. Intrapleural instillation of urokinase in the treatment of loculated pleural effusions in children. J Pediatr Surg. 1994;29:1539–1540 [DOI] [PubMed] [Google Scholar]
- 12. Yim AP, Hui-Ping L. Complications and failures of videoassisted thoracic surgery: experience from two centers in Asia. Ann Thorac Surg. 1996;61:538–541 [DOI] [PubMed] [Google Scholar]
- 13. Rodgers BM. Pediatric thoracoscopy: where have we come and what have we learned? Ann Thorac Surg. 1993;56:704–707 [DOI] [PubMed] [Google Scholar]
- 14. Colt HG. Thoracoscopy: a prospective study of safety and outcome. Chest. 1995;108:324–329 [DOI] [PubMed] [Google Scholar]