Abstract
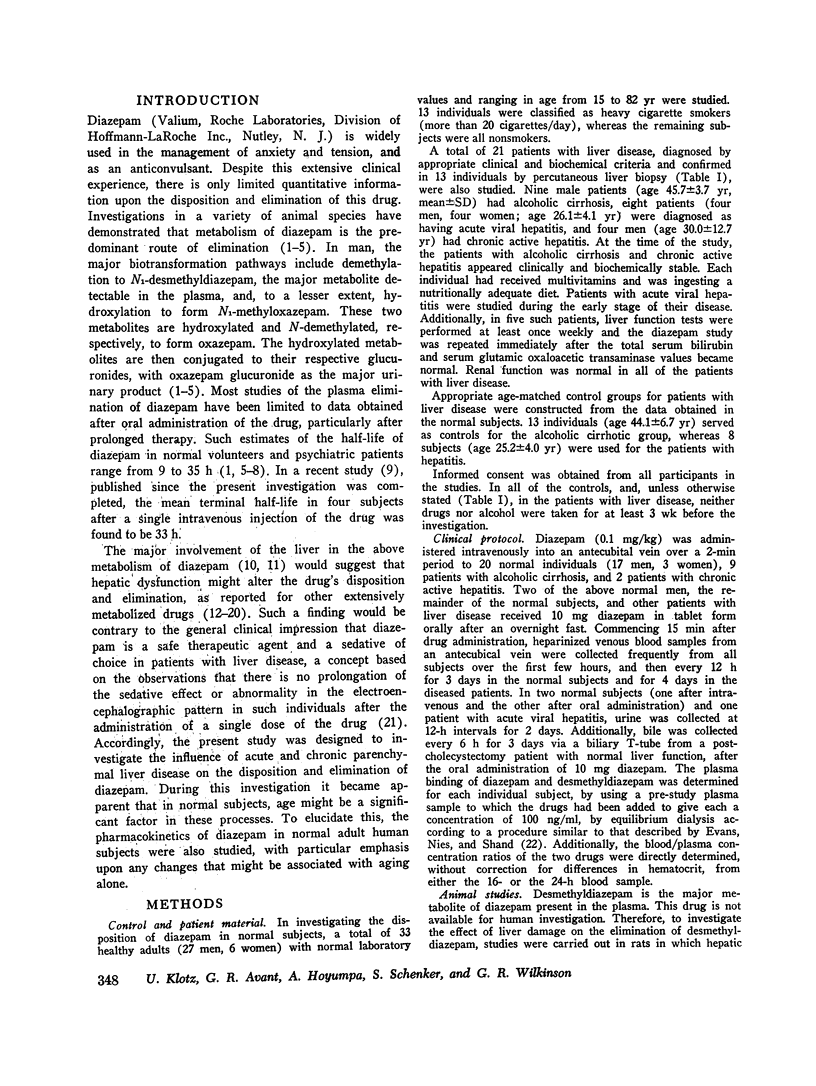
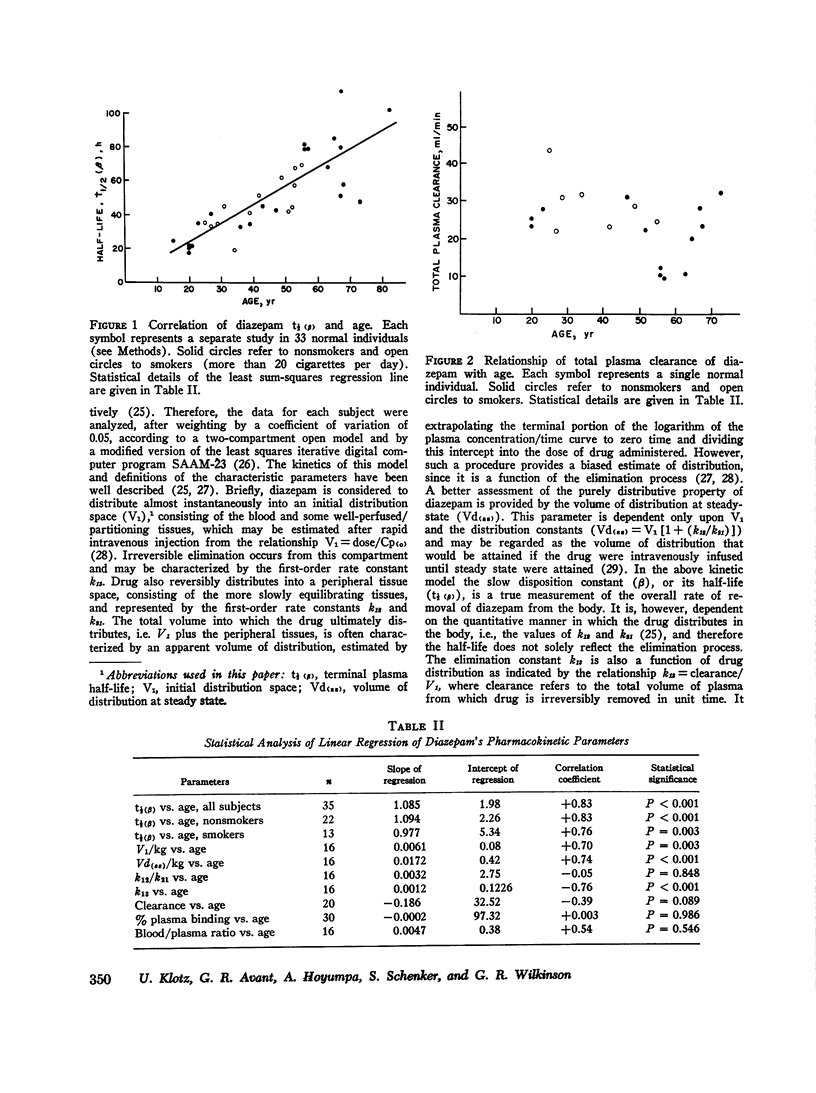
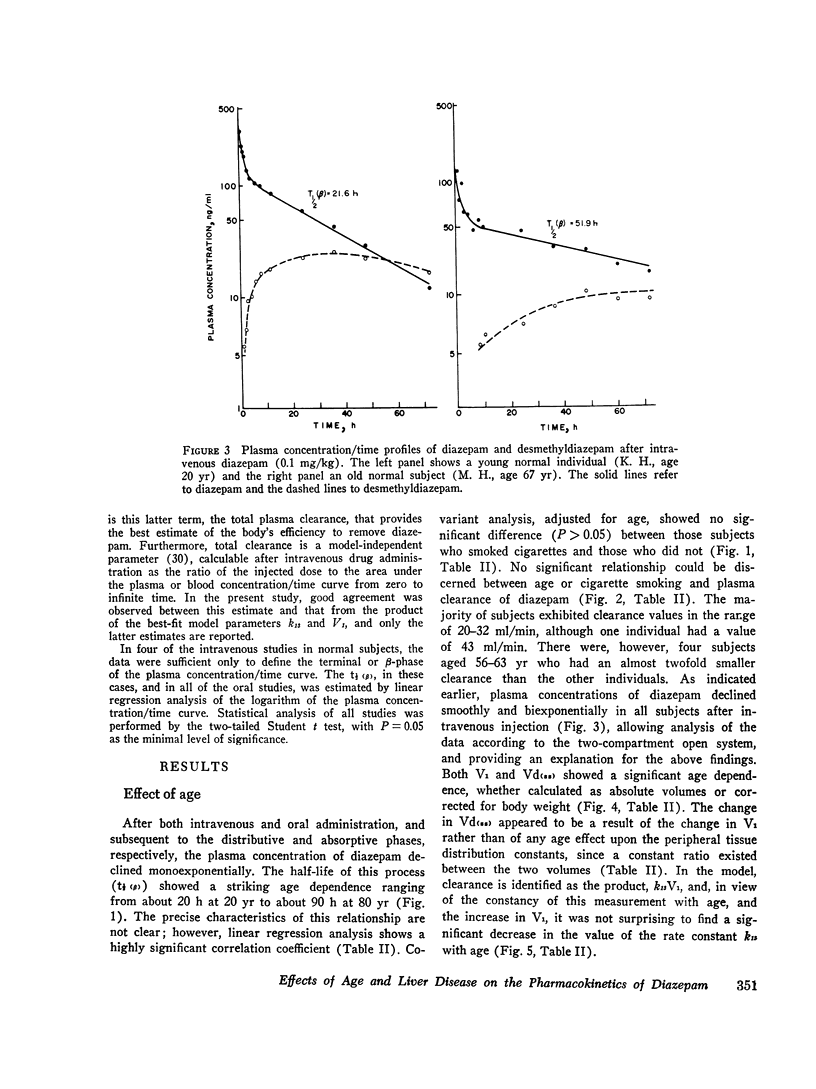
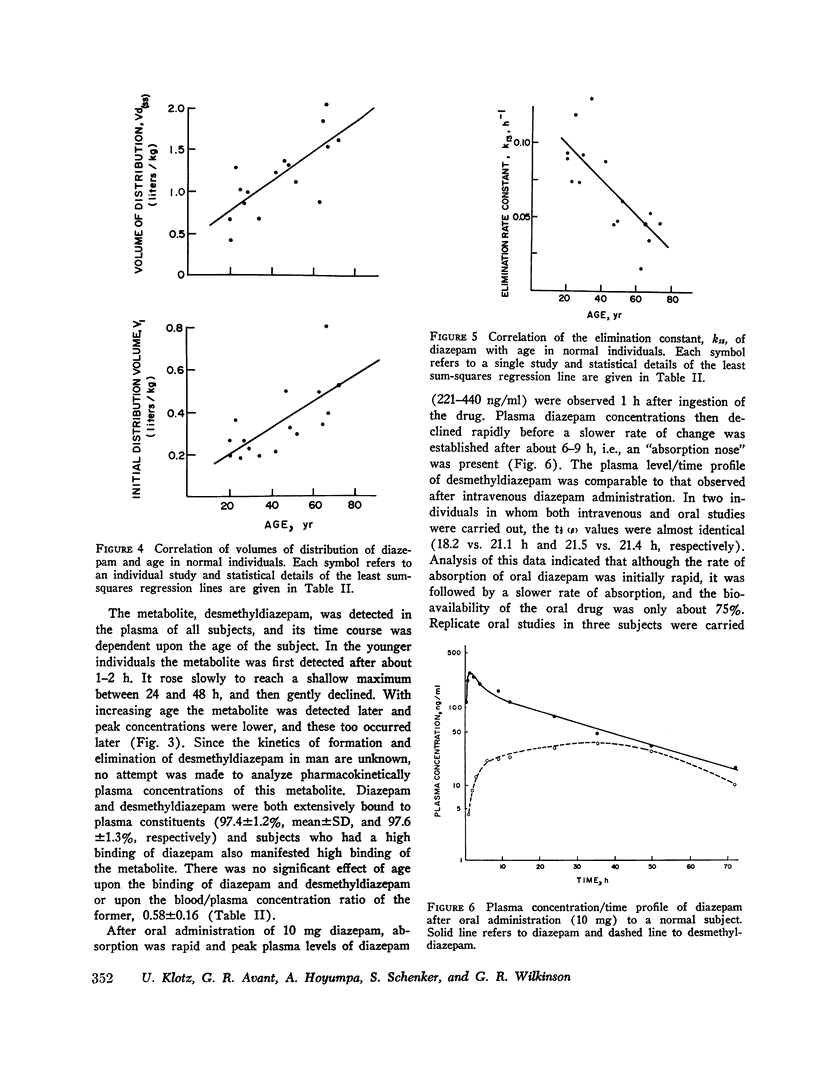
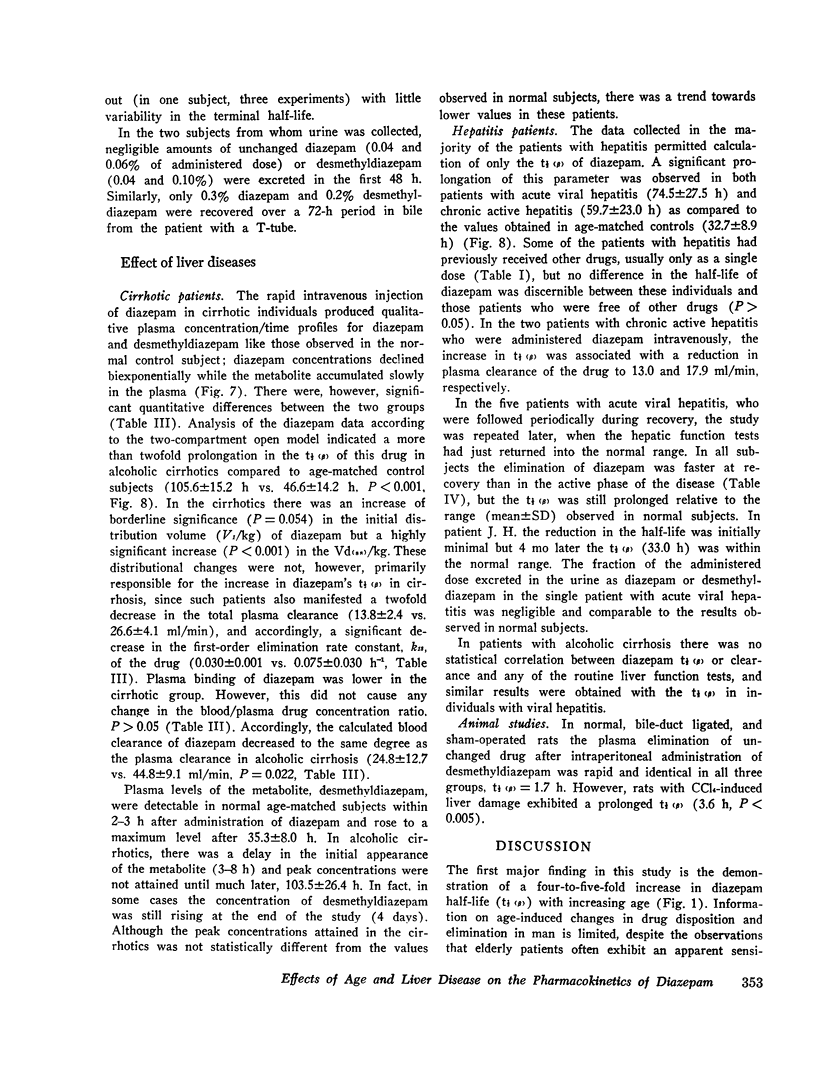
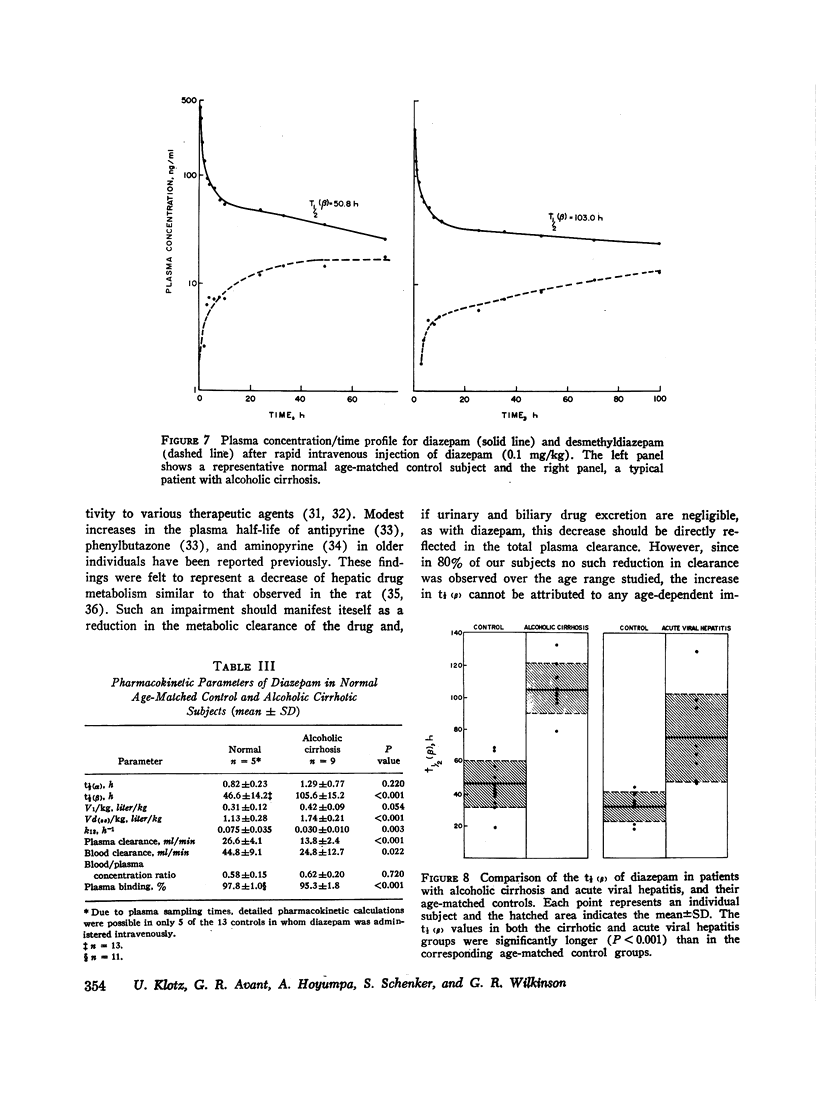
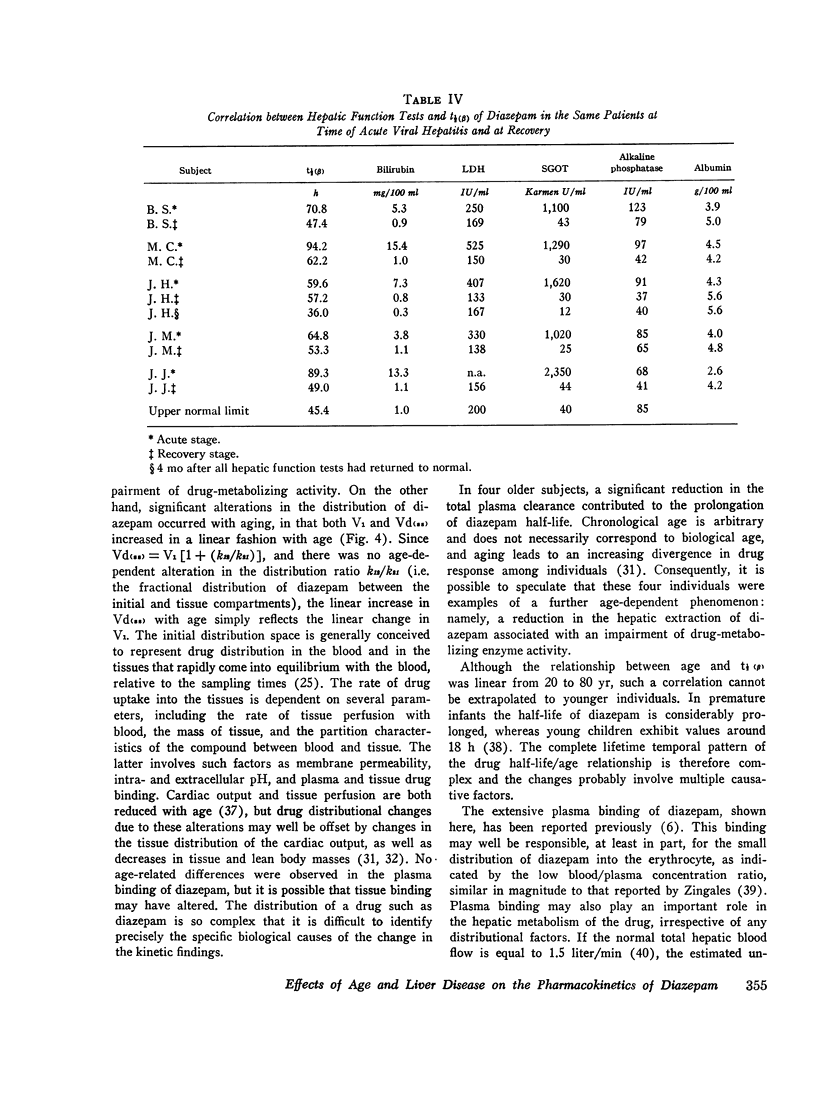
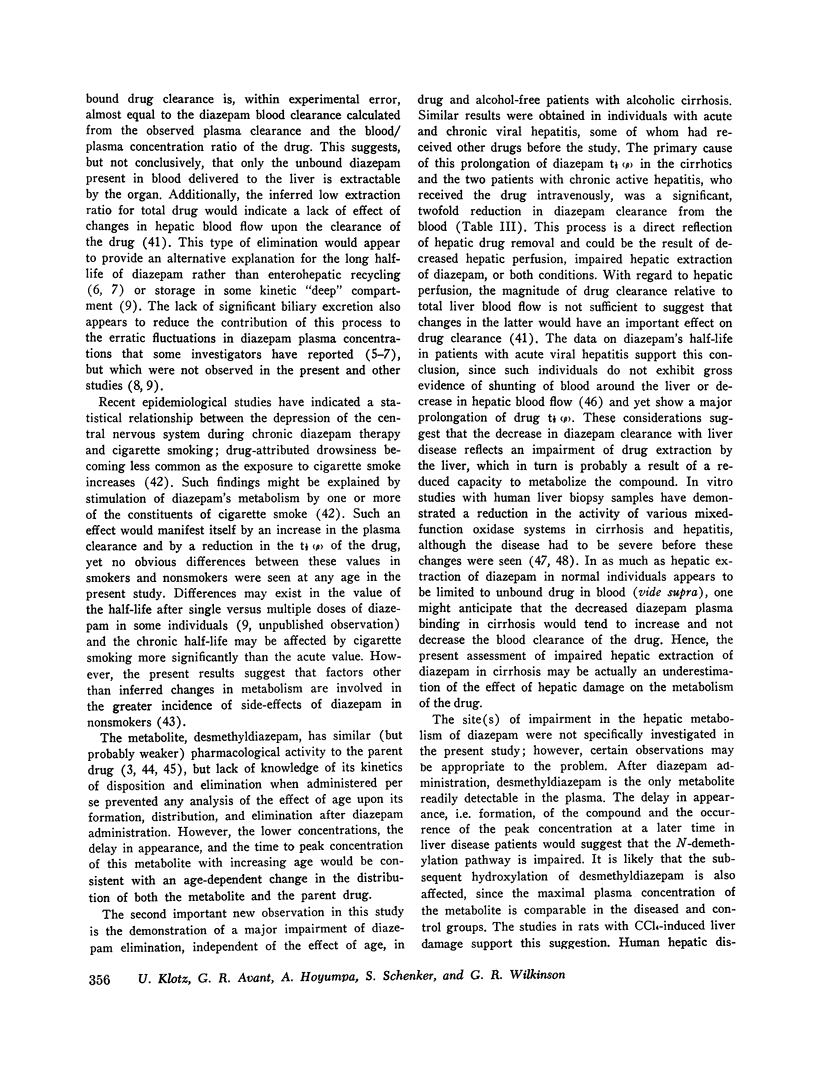
This study investigates the separate effects of age and hepatocellular liver disease on the disposition and elimination of diazepam (Valium) in man. The drug was given either by rapid intravenous injection (0.1 mg/kg) or orally (10 mg) to 33 normal volunteers rnaging in age from 15 to 82 yr as well as to 9 individuals with alcoholic cirrhosis, 8 with acute viral hepatitis, and 4 with chronic active hepatitis. In the normal individuals, the terminal plasma half-life of diazepam, (t 1/2 (B)) exhibited a striking age-dependence; at 20 yr the t 1/2 (beta) was about 20 h, but it increased linearly with age to about 90 h at 80 yr. The plasma clearance of diazepam in the majority of the normal subjects was between 20 and 32 ml/min and showed no significant age-dependence. Cigarette smoking did not affect the half-life or the clearance. Additionally, neither the plasma binding (97.4 plus or minus 1.2%, mean plus or minus SD) nor the blood/plasma concentration ratio (0.58 plus or minus 0.16) of diazepam showed any age-related changes (P greater than 0.05). By contrast, analysis of the intravenous data according to a two-compartment open model indicated that both the initial distribution space (V1) and the volume of distribution at steady state [Vd(ss)] of diazepam increased linearly with age (P less than 0.005). The increase in Vd(ss) was secondary to the change in V1. It appears then that the prolongation of t 1/2 (beta) of diazepam with age is primarily dependent on an increase in the initial distribution volume of the drug. The plasma concentration/time course of the metabolite, desmethyldiazepam, was also affected by age. In older individuals, the initial presence and the peak values of desmethyldiazepam were observed later and the metabolite was present in lower concentrations. Despite the profound prolongation of t 1/2 (theta) with age, the constancy of diazepam clearance indicates that drug plasma concentrations will not accumulate any more in the old than the young, and chronic dosage more in the old than the young, and chronic dosage modifications based on pharmacokinetic considerations are unnecessary. Data obtained in patients with liver disease were compared with those found in age-matched control groups. Patients with cirrhosis showed a more than twofold prolongation in the half-life of diazepam (105.6 plus or minus 15.2 vs. 46.6 plus or minus 14.2 h, P less than 0.001).
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Acocella G., Bonollo L., Garimoldi M., Mainardi M., Tenconi L. T., Nicolis F. B. Kinetics of rifampicin and isoniazid administered alone and in combination to normal subjects and patients with liver disease. Gut. 1972 Jan;13(1):47–53. doi: 10.1136/gut.13.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BENDER A. D. PHARMACOLOGIC ASPECTS OF AGING: A SURVEY OF THE EFFECT OF INCREASING AGE ON DRUG ACTIVITY IN ADULTS. J Am Geriatr Soc. 1964 Feb;12:114–134. doi: 10.1111/j.1532-5415.1964.tb00344.x. [DOI] [PubMed] [Google Scholar]
- BENDER A. D. THE EFFECT OF INCREASING AGE ON THE DISTRIBUTION OF PERIPHERAL BLOOD FLOW IN MAN. J Am Geriatr Soc. 1965 Mar;13:192–198. doi: 10.1111/j.1532-5415.1965.tb02665.x. [DOI] [PubMed] [Google Scholar]
- Bender A. D. Pharmacodynamic consequences of aging and their implications in the treatment of the elderly patient. Med Ann Dist Columbia. 1967 May;36(5):267–271. [PubMed] [Google Scholar]
- Berlin A., Siwers B., Agurell S., Hiort A., Sjöqvist F., Ström S. Determination of bioavailability of diazepam in various formulations from steady state plasma concentration data. Clin Pharmacol Ther. 1972 Sep-Oct;13(5):733–744. doi: 10.1002/cpt1972135part1733. [DOI] [PubMed] [Google Scholar]
- Bhattacharya I. C., Goldstein L., Pfeiffer C. C. Influence of acute and chronic nicotine administration on EEG reactivity to drugs in rabbits. 2. Psychoactive agents. Res Commun Chem Pathol Pharmacol. 1970 Jan;1(1):109–114. [PubMed] [Google Scholar]
- Branch R. A., Herbert C. M., Read A. E. Determinants of serum antipyrine half-lives in patients with liver disease. Gut. 1973 Jul;14(7):569–573. doi: 10.1136/gut.14.7.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branch R. A., Nies A. S., Shand D. G. The disposition of propranolol. 8. General implications of the effects of liver blood flow on elimination from the perfused rat liver. Drug Metab Dispos. 1973 Sep-Oct;1(5):687–690. [PubMed] [Google Scholar]
- Breen K. J., Shaw J., Alvin J., Henderson G. I., Hoyumpa A. M., Jr, Schenker S. Effect of experimental hepatic injury on the clearance of phenobarbital and paraldehyde. Gastroenterology. 1973 May;64(5):992–1004. [PubMed] [Google Scholar]
- Coutinho C. B., Cheripko J. A., Carbone J. J. Correlation between the duration of the anticonvulsant activity of diazepam and its physiological disposition in mice. Biochem Pharmacol. 1970 Feb;19(2):363–379. doi: 10.1016/0006-2952(70)90192-9. [DOI] [PubMed] [Google Scholar]
- De Silva J. A., Koechlin B. A., Bader G. Blood level distribution patterns of diazepam and its major metabolite in man. J Pharm Sci. 1966 Jul;55(7):692–702. doi: 10.1002/jps.2600550706. [DOI] [PubMed] [Google Scholar]
- De Silva J. A., Puglisi C. V. Determination of medazepam (nobrium), diazepam(valium) and their major biotransformation products in blod and urine by electron capture s-liquid chromatography. Anal Chem. 1970 Dec;42(14):1725–1736. doi: 10.1021/ac50160a040. [DOI] [PubMed] [Google Scholar]
- Doshi J., Luisada-Opper A., Leevy C. M. Microsomal pentobarbital hydroxylase activity in acute viral hepatitis. Proc Soc Exp Biol Med. 1972 Jun;140(2):492–495. doi: 10.3181/00379727-140-36487. [DOI] [PubMed] [Google Scholar]
- Evans G. H., Nies A. S., Shand D. G. The disposition of propranolol. 3. Decreased half-life and volume of distribution as a result of plasma binding in man, monkey, dog and rat. J Pharmacol Exp Ther. 1973 Jul;186(1):114–122. [PubMed] [Google Scholar]
- Fanelli R., Marcucci F., Mussini E., Garattini S. The metabolism of diazepam by liver microsomal enzymes of rats and mice. Eur J Pharmacol. 1969 Sep;7(3):307–313. doi: 10.1016/0014-2999(69)90097-1. [DOI] [PubMed] [Google Scholar]
- Hoffman T. A., Cestero R., Bullock W. E. Pharmacodynamics of carbenicillin in hepatic and renal failure. Ann Intern Med. 1970 Aug;73(2):173–178. doi: 10.7326/0003-4819-73-2-173. [DOI] [PubMed] [Google Scholar]
- Jori A., Di Salle E., Quadri A. Rate of aminopyrine disappearance from plasma in young and aged humans. Pharmacology. 1972;8(4):273–279. doi: 10.1159/000136343. [DOI] [PubMed] [Google Scholar]
- Jusko W. J., Gibaldi M. Effects of change in elimination on varous parameters of the two-compartment open model. J Pharm Sci. 1972 Aug;61(8):1270–1273. doi: 10.1002/jps.2600610820. [DOI] [PubMed] [Google Scholar]
- KATO R., VASSANELLI P., FRONTINO G., CHIESARA E. VARIATION IN THE ACTIVITY OF LIVER MICROSOMAL DRUG-METABOLIZING ENZYMES IN RATS IN RELATION TO THE AGE. Biochem Pharmacol. 1964 Jul;13:1037–1051. doi: 10.1016/0006-2952(64)90100-5. [DOI] [PubMed] [Google Scholar]
- KUNIN C. M., GLAZKO A. J., FINLAND M. Persistence of antibiotics in blood of patients with acute renal failure. II. Chloramphenicol and its metabolic products in the blood of patients with severe renal disease or hepatic cirrhosis. J Clin Invest. 1959 Sep;38:1498–1508. doi: 10.1172/JCI103928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan S. A., Jack M. L., Alexander K., Weinfeld R. E. Pharmacokinetic profile of diazepam in man following single intravenous and oral and chronic oral administrations. J Pharm Sci. 1973 Nov;62(11):1789–1796. doi: 10.1002/jps.2600621111. [DOI] [PubMed] [Google Scholar]
- Kato R., Takanaka A. Metabolism of drugs in old rats. II. Metabolism in vivo and effect of drugs in old rats. Jpn J Pharmacol. 1968 Dec;18(4):389–396. doi: 10.1254/jjp.18.389. [DOI] [PubMed] [Google Scholar]
- Klotz U., McHorse T. S., Wilkinson G. R., Schenker S. The effect of cirrhosis on the disposition and elimination of meperidine in man. Clin Pharmacol Ther. 1974 Oct;16(4):667–675. doi: 10.1002/cpt1974164667. [DOI] [PubMed] [Google Scholar]
- Kvetina J., Marcucci F., Fanelli R. Metabolism of diazepam in isolated perfused liver of rat and mouse. J Pharm Pharmacol. 1968 Oct;20(10):807–808. doi: 10.1111/j.2042-7158.1968.tb09648.x. [DOI] [PubMed] [Google Scholar]
- Levi A. J., Sherlock S., Walker D. Phenylbutazone and isoniazid metabolism in patients with liver disease in relation to previous drug therapy. Lancet. 1968 Jun 15;1(7555):1275–1279. doi: 10.1016/s0140-6736(68)92292-7. [DOI] [PubMed] [Google Scholar]
- Marcucci F., Fanelli R., Mussini E., Garattini S. Further studies on species difference in diazepam metabolism. Eur J Pharmacol. 1970 Feb;9(2):253–256. doi: 10.1016/0014-2999(70)90308-0. [DOI] [PubMed] [Google Scholar]
- Marcucci F., Guaitani A., Kvetina J., Mussini E., Garattini S. Species difference in diazepam metabolism and anticonvulsant effect. Eur J Pharmacol. 1968 Nov;4(4):467–470. doi: 10.1016/0014-2999(68)90036-8. [DOI] [PubMed] [Google Scholar]
- Mawer G. E., Miller N. E., Turnberg L. A. Metabolism of amylobarbitone in patients with chronic liver disease. Br J Pharmacol. 1972 Mar;44(3):549–560. doi: 10.1111/j.1476-5381.1972.tb07292.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morselli P. L., Principi N., Tognoni G., Reali E., Belvedere G., Standen S. M., Sereni F. Diazepam elimination in premature and full term infants, and children. J Perinat Med. 1973;1(2):133–141. doi: 10.1515/jpme.1973.1.2.133. [DOI] [PubMed] [Google Scholar]
- Murray-Lyon I. M., Young J., Parkes J. D., Knill-Jones R. P., Williams R. Clinical and electroencephalographic assessment of diazepam in liver disease. Br Med J. 1971 Oct 30;4(5782):265–266. doi: 10.1136/bmj.4.5782.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Malley K., Crooks J., Duke E., Stevenson I. H. Effect of age and sex on human drug metabolism. Br Med J. 1971 Sep 11;3(5775):607–609. doi: 10.1136/bmj.3.5775.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RANDALL L. O., HEISE G. A., SCHALLEK W., BAGDON R. E., BANZIGER R., BORIS A., MOE R. A., ABRAMS W. B. Pharmacological and clinical studies on Valium (T.M.) a new psychotherapeutic agent of the benzodiazepine class. Curr Ther Res Clin Exp. 1961 Sep;3:405–425. [PubMed] [Google Scholar]
- Riegelman S., Loo J. C., Rowland M. Shortcomings in pharmacokinetic analysis by conceiving the body to exhibit properties of a single compartment. J Pharm Sci. 1968 Jan;57(1):117–123. doi: 10.1002/jps.2600570123. [DOI] [PubMed] [Google Scholar]
- Riegelman S., Loo J., Rowland M. Concept of a volume of distribution and possible errors in evaluation of this parameter. J Pharm Sci. 1968 Jan;57(1):128–133. doi: 10.1002/jps.2600570125. [DOI] [PubMed] [Google Scholar]
- Rowland M., Benet L. Z., Graham G. G. Clearance concepts in pharmacokinetics. J Pharmacokinet Biopharm. 1973 Apr;1(2):123–136. doi: 10.1007/BF01059626. [DOI] [PubMed] [Google Scholar]
- Schoene B., Fleischmann R. A., Remmer H., von Oldershausen H. F. Determination of drug metabolizing enzymes in needle biopsies of human liver. Eur J Clin Pharmacol. 1972 Mar;4(2):65–73. doi: 10.1007/BF00562499. [DOI] [PubMed] [Google Scholar]
- Schwartz M. A., Koechlin B. A., Postma E., Palmer S., Krol G. Metabolism of diazepam in rat, dog, and man. J Pharmacol Exp Ther. 1965 Sep;149(3):423–435. [PubMed] [Google Scholar]
- Schwartz M. A., Postma E. Metabolism of diazepam in vitro. Biochem Pharmacol. 1968 Dec;17(12):2443–2449. doi: 10.1016/0006-2952(68)90134-2. [DOI] [PubMed] [Google Scholar]
- Thomson P. D., Melmon K. L., Richardson J. A., Cohn K., Steinbrunn W., Cudihee R., Rowland M. Lidocaine pharmacokinetics in advanced heart failure, liver disease, and renal failure in humans. Ann Intern Med. 1973 Apr;78(4):499–508. doi: 10.7326/0003-4819-78-4-499. [DOI] [PubMed] [Google Scholar]
- UEDA H., SAKURAI T., OTA M., NAKAJIMA A., KAMII K., MAEZAWA H. DISAPPEARANCE RATE OF TOLBUTAMIDE IN NORMAL SUBJECTS AND IN DIABETES MELLITUS, LIVER CIRRHOSIS, AND RENAL DISEASE. Diabetes. 1963 Sep-Oct;12:414–419. doi: 10.2337/diab.12.5.414. [DOI] [PubMed] [Google Scholar]
- Westlake W. J. Time integral of drug concentration in the central (plasma) compartment. J Pharm Sci. 1970 May;59(5):722–723. doi: 10.1002/jps.2600590537. [DOI] [PubMed] [Google Scholar]
- Zingales I. A. Diazepam metabolism during chronic medication unbound fraction in plasma, erythrocytes and urine. J Chromatogr. 1973 Jan 3;75(1):55–78. doi: 10.1016/s0021-9673(01)83413-0. [DOI] [PubMed] [Google Scholar]
- van der Kleijn E. Pharmacokinetics of distribution and metabolism of ataractic drugs and an evaluation of the site of antianxiety activity. Ann N Y Acad Sci. 1971 Jul 6;179:115–125. doi: 10.1111/j.1749-6632.1971.tb46894.x. [DOI] [PubMed] [Google Scholar]
- van der Klejin E., van Rossum J. M., Muskens E. T., Rijntjes N. V. Pharmacokinetics of diazepam in dogs, mice and humans. Acta Pharmacol Toxicol (Copenh) 1971;29 (Suppl 3):109–127. doi: 10.1111/j.1600-0773.1971.tb03291.x. [DOI] [PubMed] [Google Scholar]


