Abstract
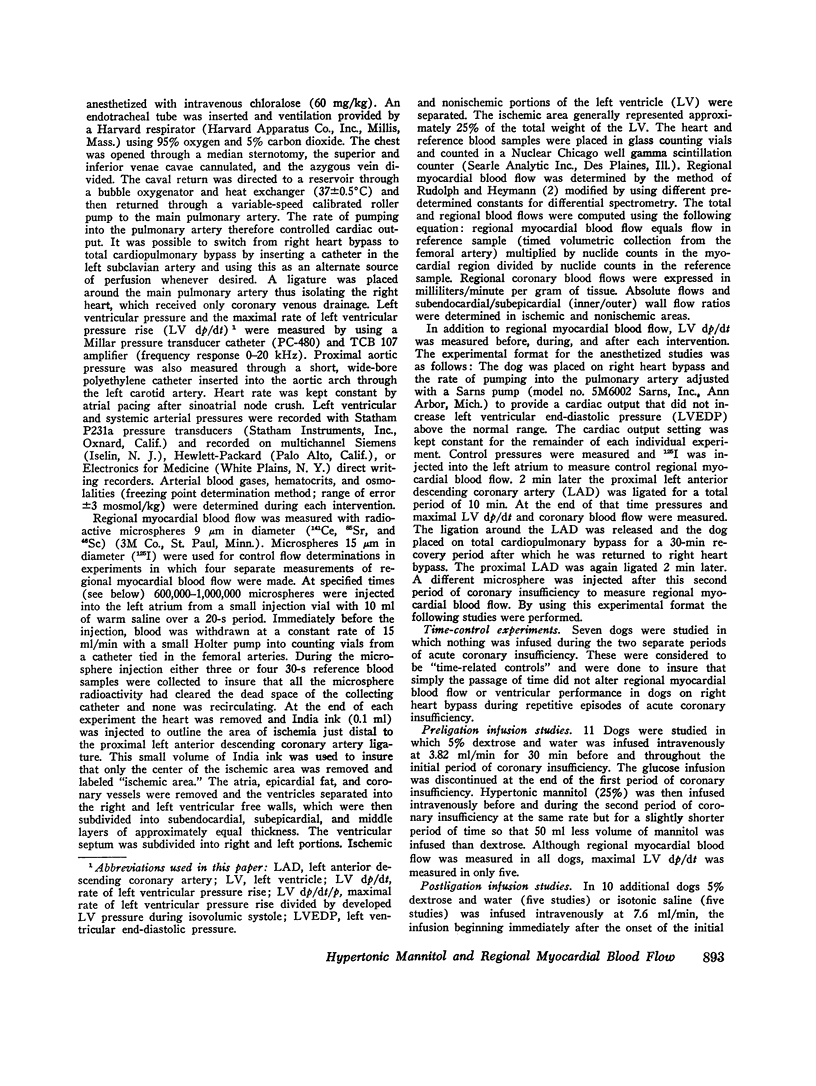
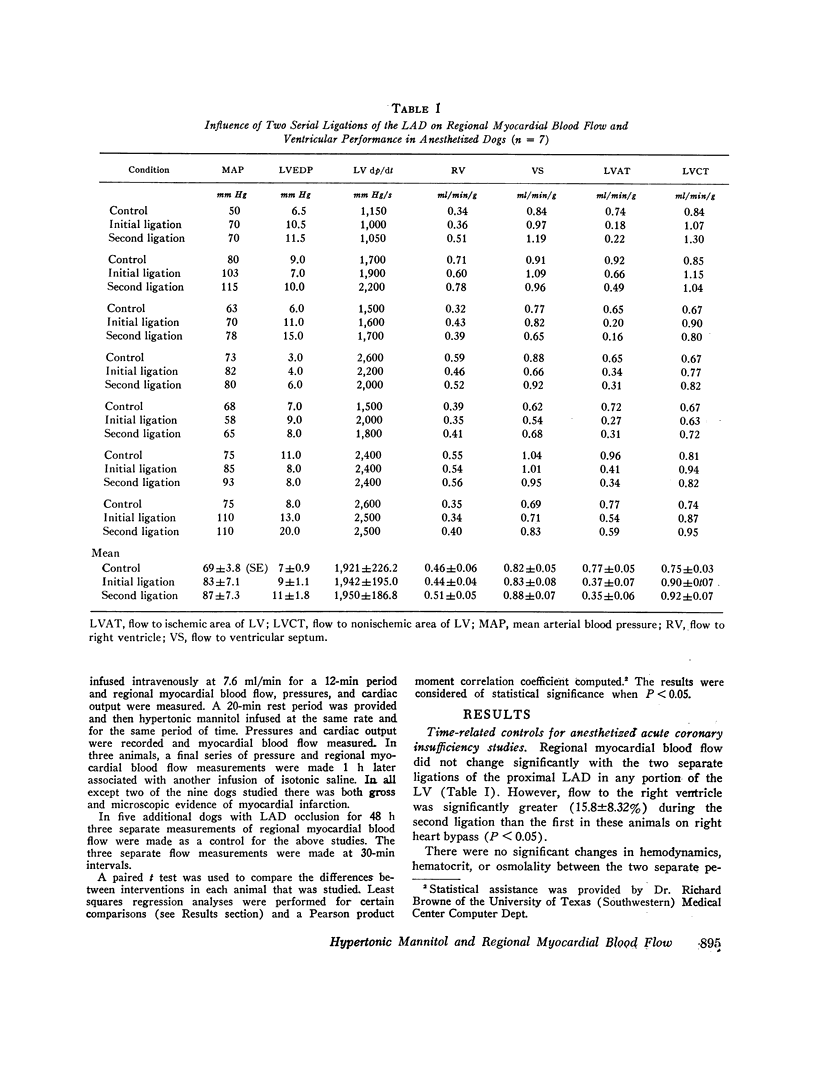
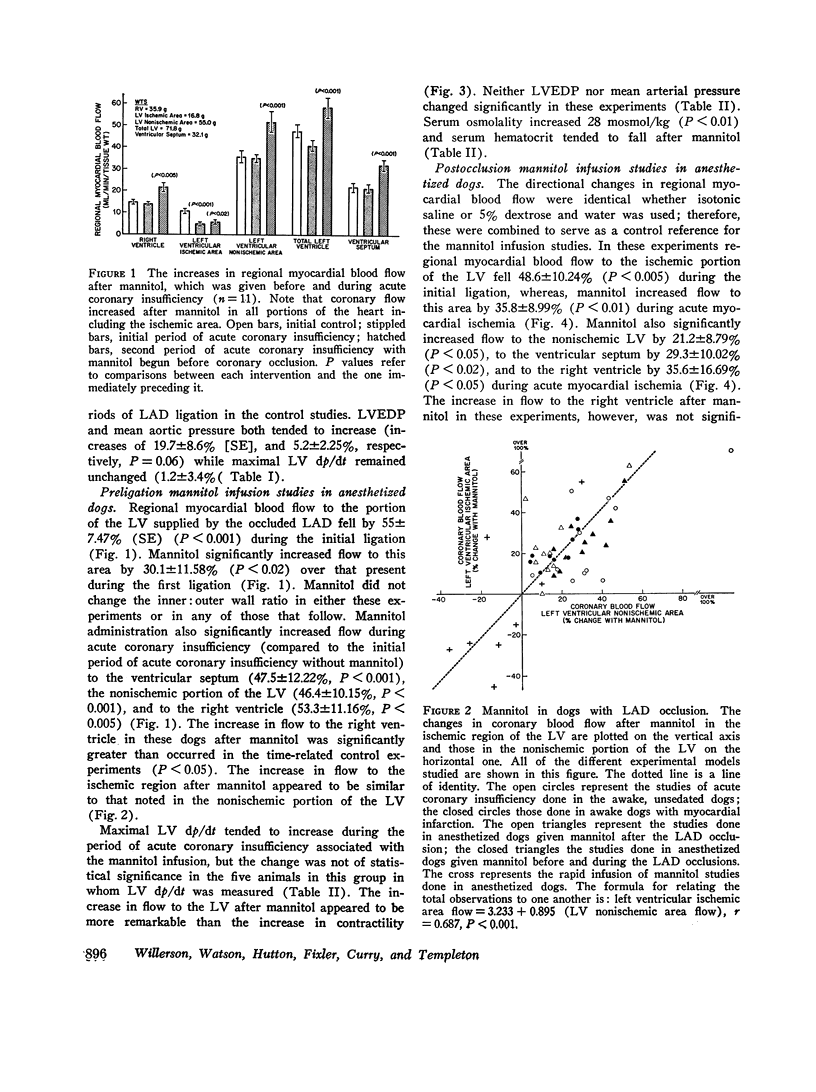
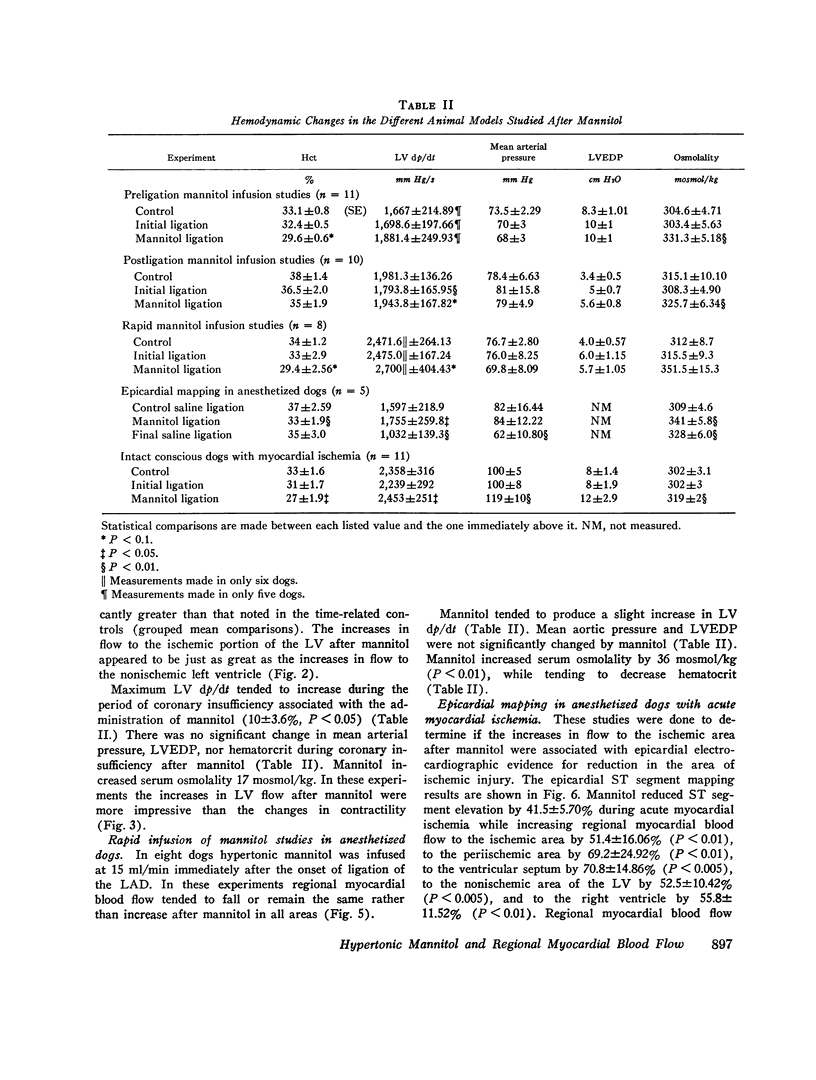
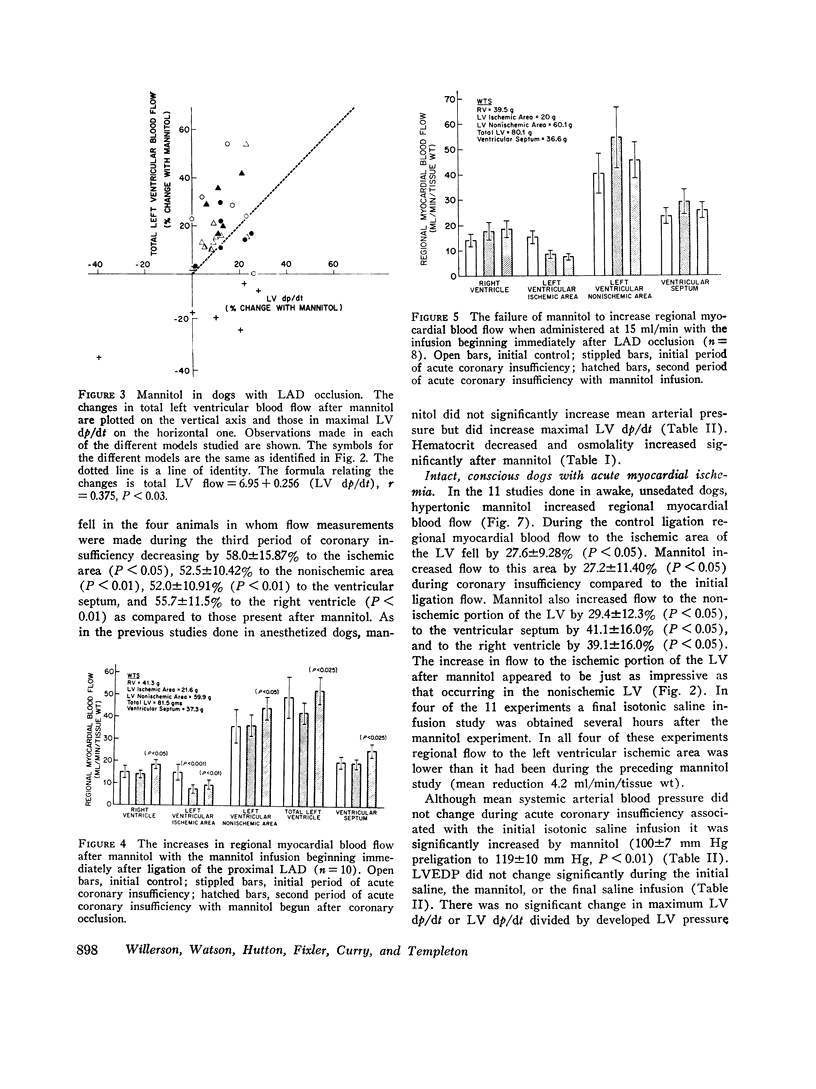
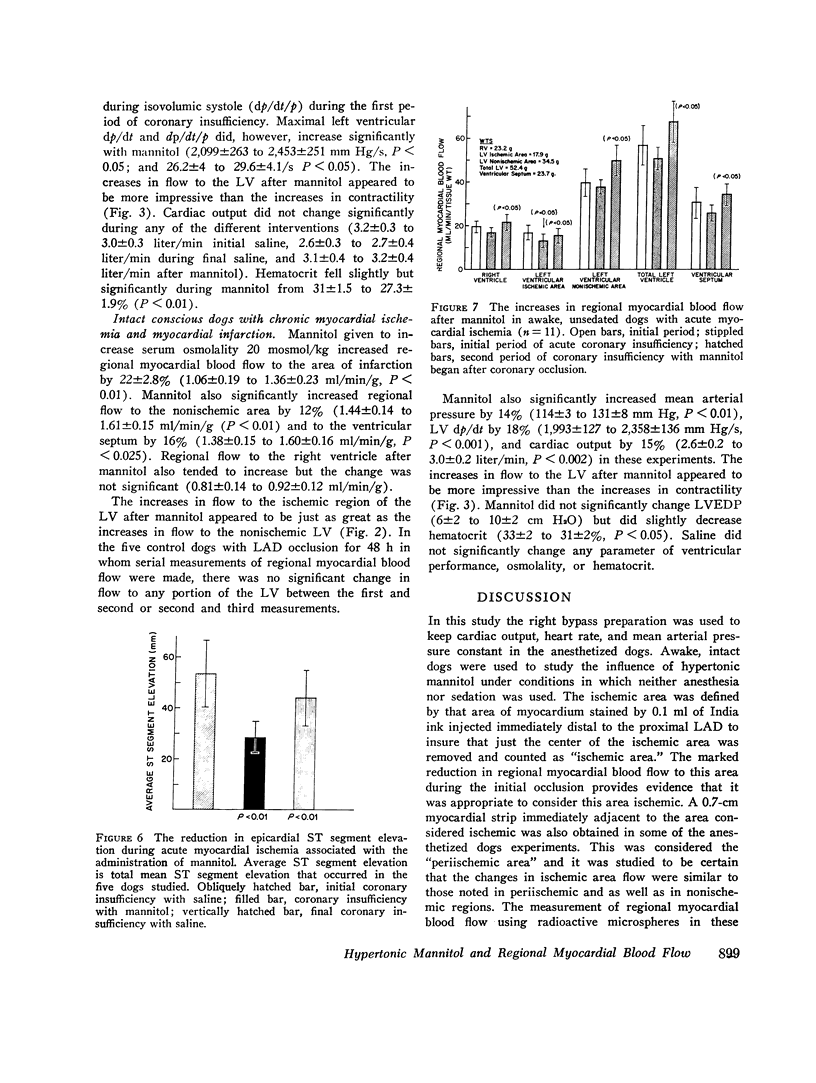
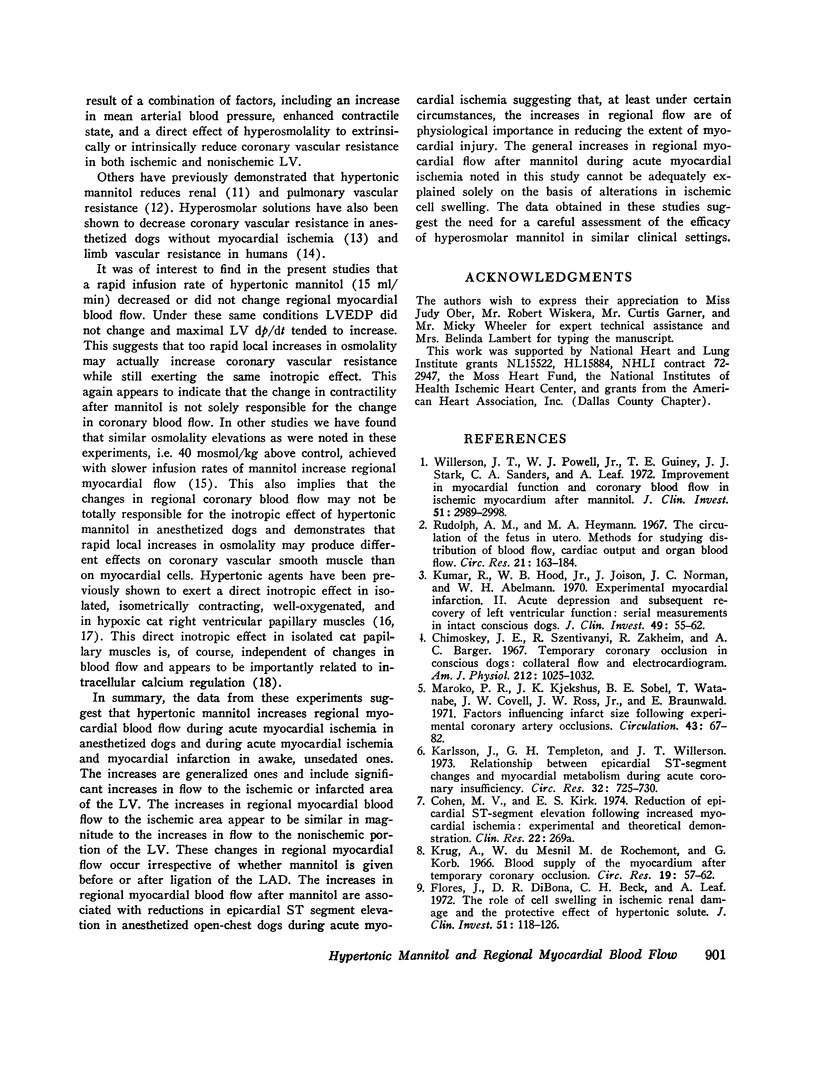
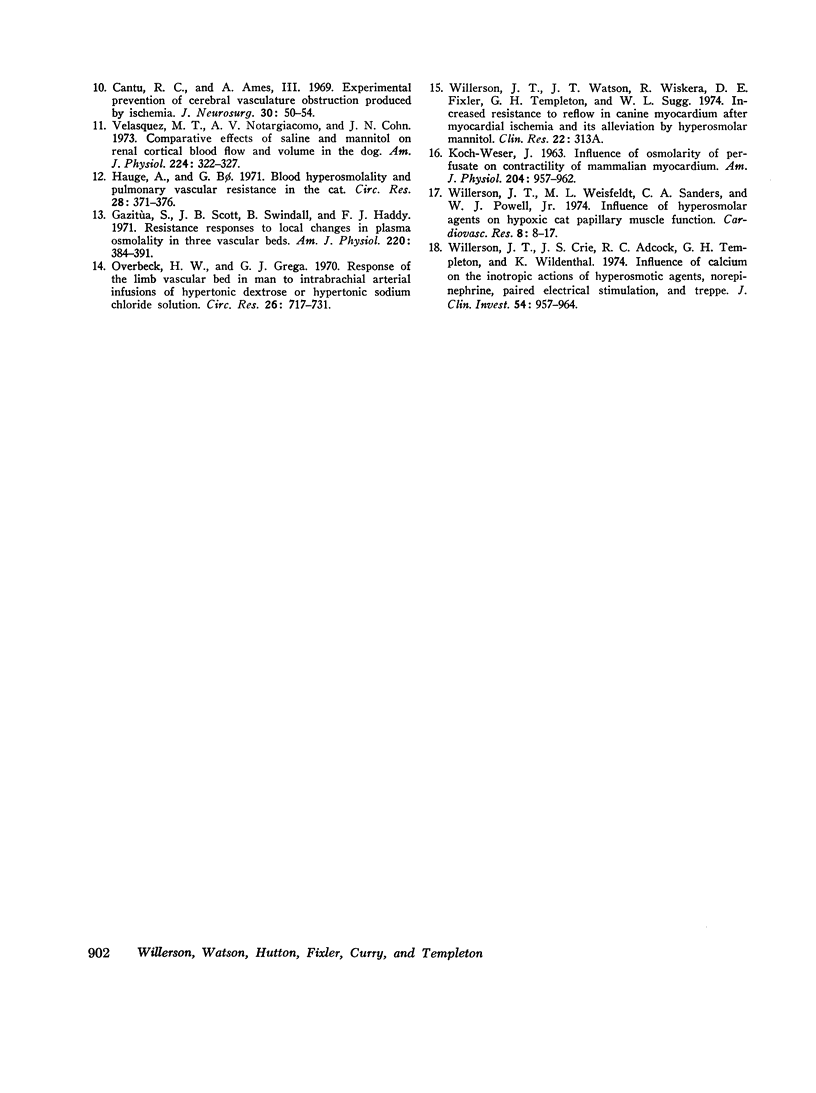
The influence of hypertonic mannitol on regional myocardial blood flow and ventricular performance was studied during acute myocardial ischemia in awake, unsedated and in anesthesized dogs and after myocardial infarction in awake unsedated dogs. Regional myocardial blood flow was measured with radioactive microspheres. Generalized increases in regional myocardial blood flow occurred after mannitol in all of the different animal models studied. The increases in coronary blood flow after mannitol were just as impressive in the nonischemic regions as in the ischemic portion of the left ventricle in all of the different models that were examined in this study. Improvement in regional myocardial blood flow to the ischemic area of the left ventricle after mannitol was associated with a reduction in ST segment elevation during acute myocardial ischemia in anesthetized dogs. The increases in regional myocardial flow after mannitol were also associated with increases in contractility, but the increases in flow appeared to be more impressive than the changes in contractility. The data obtained demonstrate that mannitol increases regional coronary blood flow to both ischemic and nonischemic myocardium in both anesthetized and awake, unsedated, intact dogs with acute and chronic myocardial ischemia and that mannitol reduces ST segment elevation during acute myocardial ischemia in anesthetized dogs. Thus the results suggest that under these circumstances the increases in regional myocardial blood flow after mannitol are of physiological importance in reducing the extent of myocardial injury. Since coronary blood flow increased to nonischemic regions the increases in regional myocardial flow demonstrated in this study after mannitol cannot be entirely explained by the mechanism of reduction in ischemic cell swelling.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cantu R. C., Ames A., 3rd Experimental prevention of cerebral vasculature obstruction produced by ischemia. J Neurosurg. 1969 Jan;30(1):50–54. doi: 10.3171/jns.1969.30.1.0050. [DOI] [PubMed] [Google Scholar]
- Chimoskey J. E., Szentivanyi M., Zakheim R., Barger A. C. Temporary coronary occlusion in conscious dogs: collateral flow and electrocardiogram. Am J Physiol. 1967 May;212(5):1025–1032. doi: 10.1152/ajplegacy.1967.212.5.1025. [DOI] [PubMed] [Google Scholar]
- Flores J., DiBona D. R., Beck C. H., Leaf A. The role of cell swelling in ischemic renal damage and the protective effect of hypertonic solute. J Clin Invest. 1972 Jan;51(1):118–126. doi: 10.1172/JCI106781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gazitùa S., Scott J. B., Swindall B., Haddy F. J. Resistance responses to local changes in plasma osmolality in three vascular beds. Am J Physiol. 1971 Feb;220(2):384–391. doi: 10.1152/ajplegacy.1971.220.2.384. [DOI] [PubMed] [Google Scholar]
- Hauge A., Bo G. Blood hyperosmolality and pulmonary vascular resistance in the cat. Circ Res. 1971 Mar;28(3):371–376. doi: 10.1161/01.res.28.3.371. [DOI] [PubMed] [Google Scholar]
- KOCH-WESER J. Influence of osmolarity of perfusate on contractility of mammalian myocardium. Am J Physiol. 1963 Jun;204:957–962. doi: 10.1152/ajplegacy.1963.204.6.957. [DOI] [PubMed] [Google Scholar]
- Karlsson J., Templeton G. H., Willerson J. T. Relationship between epicardial S-T segment changes and myocardial metabolism during acute coronary insufficiency. Circ Res. 1973 Jun;32(6):725–730. doi: 10.1161/01.res.32.6.725. [DOI] [PubMed] [Google Scholar]
- Krug A., Du Mesnil de Rochemont, Korb G. Blood supply of the myocardium after temporary coronary occlusion. Circ Res. 1966 Jul;19(1):57–62. doi: 10.1161/01.res.19.1.57. [DOI] [PubMed] [Google Scholar]
- Kumar R., Hood W. B., Jr, Joison J., Norman J. C., Abelmann W. H. Experimental myocardial infarction. II. Acute depression and subsequent recovery of left ventricular function: serial measurements in intact conscious dogs. J Clin Invest. 1970 Jan;49(1):55–62. doi: 10.1172/JCI106223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maroko P. R., Kjekshus J. K., Sobel B. E., Watanabe T., Covell J. W., Ross J., Jr, Braunwald E. Factors influencing infarct size following experimental coronary artery occlusions. Circulation. 1971 Jan;43(1):67–82. doi: 10.1161/01.cir.43.1.67. [DOI] [PubMed] [Google Scholar]
- Overbeck H. W., Grega G. J. Response of the limb vascular bed in man to intrabrachial arterial infusions of hypertonic dextrose or hypertonic sodium chloride solutions. Circ Res. 1970 Jun;26(6):717–731. doi: 10.1161/01.res.26.6.717. [DOI] [PubMed] [Google Scholar]
- Rudolph A. M., Heymann M. A. The circulation of the fetus in utero. Methods for studying distribution of blood flow, cardiac output and organ blood flow. Circ Res. 1967 Aug;21(2):163–184. doi: 10.1161/01.res.21.2.163. [DOI] [PubMed] [Google Scholar]
- Velasquez M. T., Notargiacomo A. V., Cohn J. N. Comparative effects of saline and mannitol on renal cortical blood flow and volume in the dog. Am J Physiol. 1973 Feb;224(2):322–327. doi: 10.1152/ajplegacy.1973.224.2.322. [DOI] [PubMed] [Google Scholar]
- Willerson J. T., Crie J. S., Adcock R. C., Templeton G. H., Wildenthal K. Influence of calcium on the inotropic actions of hyperosmotic agents, norepinephrine, paired electrical stimulation, and treppe. J Clin Invest. 1974 Oct;54(4):957–964. doi: 10.1172/JCI107836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willerson J. T., Powell W. J., Jr, Guiney T. E., Stark J. J., Sanders C. A., Leaf A. Improvement in myocardial function and coronary blood flow in ischemic myocardium after mannitol. J Clin Invest. 1972 Dec;51(12):2989–2998. doi: 10.1172/JCI107126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willerson J. T., Weisfeldt M. L., Sanders C. A., Powell W. J., Jr Influence of hyperosmolar agents on hypoxic cat papillary muscle function. Cardiovasc Res. 1974 Jan;8(1):8–17. doi: 10.1093/cvr/8.1.8. [DOI] [PubMed] [Google Scholar]


