Abstract
In actinic cheilitis, the current view is that the keratinocytes have undergone transformation forming a field of epithelium with the potential for neoplastic transformation. Clinical features include diffuse and poorly demarcated atrophic, erosive or keratotic plaques that may affect some parts of, or the entire vermilion border. Fair-complexioned people, those with albinism and people with eversion of the lip are all subject to actinic cheilitis. Prophylactic measures against all forms of sunlight-induced lesions must include limitation of exposure to the sun during peak sunlight hours, the use of appropriate protective clothing, and the use of a sunscreen cream. In this article, a case of albinism is used to illustrate the nature of actinic cheilitis, its clinical features and its treatment.
Keywords: Actinic cheilitis, UVB, Squamous cell carcinoma
INTRODUCTION
Actinic cheilitis is a pathological condition that most frequently affects the vermilion border of the lower lip.1–3 In persons with everted lower lips, as a racial characteristic or as an inherited trait, the mucosal surface of the lower lip, which is partly exposed to sunlight, is also affected. When both the upper and lower lips are prominent, as in bimaxillary protrusion, the upper lip may also be more vulnerable to sunlight exposure. In the past, actinic cheilitis was regarded as being potentially malignant, with not infrequent transformation into invasive, metastasizing squamous cell carcinoma.
An alternative view states that the keratinocytes in actinic cheilitis have already undergone ultraviolet light-induced molecular and genetic transformation into neoplastic keratinocytes, that actinic cheilitis is in fact the result of clonal expansion of the transformed keratinocytes,3–7 and that it should be considered from its initiation to be an in-situ squamous cell carcinoma.8
The affected person complains of an inelastic or tight sensation in the lip. On examination one finds mottling of the lip with atrophic areas or shallow erosions and rough, scaly, flaky keratotic patches on some parts, or on the entire exposed portion of the lip and sometimes with small wrinkles in the vermilion border.2,3 When the surface of the lesion is palpated, there is a fine sandpaper-like feeling.2 The keratotic patches progress to palpable thickening and induration, and eventually one or more of them may become clearly demarcated or may ulcerate. Such changes are suggestive of invasive squamous cell carcinoma.2,3,7,9
Histopathological changes in actinic cheilitis range from atrophy to hyperplasia of the squamous cell epithelium of the vermilion border, with varying degrees of keratinisation, disordered maturation, increased mitotic activity and cytological atypia. Drop-shaped epithelial pegs are often present, but the basement membrane is intact. The underlying connective tissue shows basophilic degeneration (solar elastosis).7,10 Based on the above-mentioned microscopic changes, actinic cheilitis should be regarded as an intra-epithelial, or in-situ neoplasm.3,8
Anyone who has suffered excessive exposure to the sun can develop actinic cheilitis, but fair-complexioned people, especially people affected with albinism, are particularly at risk.8
CASE REPORT
A 35-year-old black female with type 1 oculocutaneous albinism and multiple basal cell carcinomas of the face (Figure 1) was referred for diagnosis and treatment of lesions of the vermilion borders of the lips (Figure 2), which were of six months duration. The patient reported that her basal cell carcinomas had been diagnosed two years previously and had been treated with topical 5-fluorouracil, but with only partial success. She was still attending at the dermatology clinic. Apart from the oculocutaneous albinism and the facial basal cell carcinomas, the patient claimed to be healthy. There were multiple irregular, rough, scaly macules on the vermilion borders of both the upper and lower lips, extending beyond the vermilion-cutaneous margins in places, and both lips were swollen and painful (Figure 2). Microscopic examination of two incisional biopsy specimens showed epithelial changes of hyperkeratosis, acanthosis, dyskeratosis and moderate dysplasia, with a dense chronic inflammatory infiltrate and basophilic degeneration of the lamina propria. The diagnosis was actinic cheilitis.
Figure 1.
Multiple basal cell carcinomas of the face (arrows).
Figure 2.
Actinic cheilitis of the upper and lower lips. Incisional biopsies were taken from the areas marked as X and Y. The arrows show the extension of the lesions beyond the vermilion-cutaneous margins.
In view of the extent of the lip lesions, it was decided to treat both upper and lower lips surgically. Microscopic examination of the tissue removed by vermilionectomy showed areas of severe dysplasia and severe basophilic degeneration. There was no evidence of in-situ squamous cell carcinoma or invasive squamous cell carcinoma. The patient was given advice about sunlight protection. The healing was uneventful (Figure 3). The patient had slight chronic periodontitis, which was treated.
Figure 3.
The lips 4 weeks after treatment.
DISCUSSION
The wavelength of ultraviolet (UV) light lies within the range of 100–400 nm (1 nm = 10−9 m) of the electromagnetic spectrum. UV light is classified as UV-A, -B and -C. UVC is in the range of 100–290 nm; UVB, 290–320 nm; and UVA, about 320–400 nm. Sunlight UVC is almost completely filtered out by the atmosphere. Both UVA and UVB can contribute to ageing of the skin by damaging collagen, breaking down vitamin A,11 by causing local immunosuppression12 and by ionisation, which releases hydroxyl and oxygen radicals and thus contributes indirectly to DNA damage. UVB from the sun, which is only partly filtered out by the atmosphere, can cause mutagenic changes; a common event of this kind is the formation of aberrant covalent bonds between adjacent cytosine bases in epithelial DNA. Cells with these dimers of cytosine in their DNA then propagate, giving rise to clones of mutated cells.
Actinic keratosis of the skin is thus a primarily UVB-induced intra-epithelial neoplasm: the analogous lesion of the vermilion border of the lip is called actinic cheilitis.13 In the initiation stage of actinic-induced carcinogenesis following significant exposure to the sun, UVB causes mutations in the epithelial p53 tumour-suppressor gene that result in the dysregulation of its functions.6
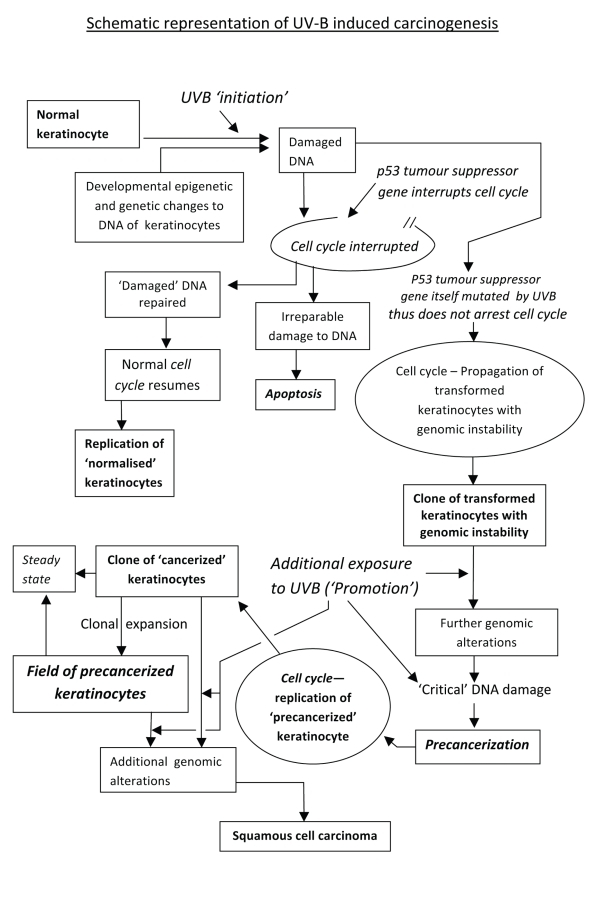
If there is only limited exposure to UVB, p53 can retain sufficient functionality to arrest the cell cycle, permitting activation of repair processes of cellular DNA before the cell enters the phase of DNA synthesis. A cell with repaired DNA can then proceed through the rest of the cell cycle to cell division. Very severe UVB exposure, in contrast, can damage the DNA sufficiently to render it beyond repair, and p53 then activates cellular pathways leading to programmed cell death (apoptosis) (Figure 4).14
Figure 4.
Schematic representation of UV-B induced carcinogenesis.
UVB-induced dysregulation of the function of the tumour-suppressor gene p53 results in genomic instability, making the cells susceptible to further critical UVB-induced genetic alterations with ultimate malignant transformation of the affected cells (Figure 4).6,15 It is evident that UVB is a complete carcinogen since it not only initiates the genetic alteration of epithelial cells but also subsequently promotes the expansion of clones of transformed cells, which then display all the characteristics of malignancy.6,16 Actinic keratosis and actinic cheilitis occur more frequently in pale people, particularly in those with fair complexions, persons with albinism, males, the elderly, those who live at high altitudes or close to the equator, and of course, those who by reason of their occupations or their leisure activities have excessive exposure to the sun.6,8
The vermilion border of the lower lip may also be more vulnerable to sunlight-induced lesions because its epithelium is thin, has a thin keratin layer and has a lower melanin content.2 Smoking and infection of the lip by the human papillomavirus may cause additional cytogenetic alterations and further increase the risk of actinic cheilitis becoming carcinomatous.13
Oculocutaneous albinism (OCA) encompasses a heterogeneous group of four genetically inherited autosomal recessive conditions characterised by hypopigmentation of the skin, hair and eyes brought about by a complete or partial reduction in melanin biosynthesis. At least four defective genes are associated with OCA, and they cause OCA types 1, 2, 3, and 4.17 OCA type 1, the most common type of albinism worldwide, results from a genetic absence of tyrosinase, which is an essential enzyme necessary for melanin production.18 In OCA type 2, the most common type of albinism in black people in Africa, there is some degree of tyrosinase activity and melanin production.17 Black persons with OCA type 2 have pale skin, sandy-coloured hair and light-brown or blue irises.19
As melanin protects the basal (progenitor) layer of keratinocytes from solar energy, persons with relatively few granules of melanin in their keratinocytes, especially those with OCA, are more likely to develop non-malignant and malignant actinic skin lesions, including sunburns, blisters, solar elastosis and lentigenes, and squamous and basal cell carcinomas.19
It has been reported that in Africa, black persons with albinism are often exposed to social discrimination as a result of superstitious beliefs.19,20 As a result of the stigma attached to albinism, black persons with albinism may be shunned by their communities and may delay seeking medical treatment until late in the course of any actinic lesion, most importantly carcinoma.19 Our patient with albinism was in fact well integrated in her community, was an office worker, and was not occupationally exposed to the sun. As is typical for persons with albinism, our patient had actinic cheilitis and multiple basal cell carcinomas. Because albinism itself is not a premalignant condition, her actinic skin lesions must have resulted from the fact that in the part of South Africa where she lives, there has been on average in the past 2½ years, 8.55 hours of sunlight per day and the altitude is 1306 meters above sea level, so substantial exposure to the sun is inescapable.21
Actinic cheilitis may show epithelial changes of simple keratosis, different grades of epithelial dysplasia, in-situ carcinoma or even invasive squamous cell carcinoma, all of which at some stage may have similar clinical appearances.2,3 It cannot be predicted whether or when actinic cheilitis will progress to squamous cell carcinoma. Consequently, a clinical diagnosis of actinic cheilitis must always be supported by histopathological evidence, but a single biopsy result may not be conclusive, and the prudent clinician would be well advised to take a biopsy from more than one site.3,22
Indeed, in some cases, surgical excision of the entire vermilion border (vermilionectomy) with histological examination of serial sections is the preferred treatment.3 Other possible treatment modalities include electrodessication, cryosurgery, laser treatment, photodynamic therapy, or topical treatment with the antineoplastic agent 5-fluorouracil or the immunomodulator imiquimod; however, with these modalities, the tissue is not available for histological examination.1,2,8,9,23,24
It has recently been reported that photodynamic therapy using the methyl-ester of aminolevulinic acid as a photosensitising agent is a very effective treatment modality for actinic cheilitis. It is well tolerated by patients and provides excellent cosmetic outcomes.23
Regardless of the treatment modality used for actinic cheilitis, regular clinical follow-up is essential.5 Protection against the potentially damaging effects of sunlight exposure depends upon taking a few straightforward precautions that must be introduced in childhood and continued throughout life. The basic precautions are: avoidance of outdoor activities during peak sunlight hours; wearing of protective clothing that covers as much of the skin as the outdoor activity will allow and of a wide-brimmed hat for the face and lips; and the liberal and frequent use of an effective sunscreen preparation.1,16,24
CONCLUSIONS
Actinic cheilitis is the result of clonal expansion of UVB-induced transformed keratinocytes characterised by molecular and genomic alterations causing genomic instability. Additional UVB-induced genetic changes are necessary for full malignant transformation with the potential for invasiveness and metastasis.
Prevention of actinic cheilitis can be achieved by reducing cumulative exposure to UVB radiation. The use of protective clothing, reduced outdoor activities, and the use of sunscreens should be introduced early in childhood and continued throughout life.
REFERENCES
- 1.Schwartz RA, Bridges TM, Butani AK, Ehrlich A. Actinic keratoses: an occupational and environmental disorder. Eur Acad Dermatol Venerol. 2008;22:606–615. doi: 10.1111/j.1468-3083.2008.02579.x. [DOI] [PubMed] [Google Scholar]
- 2.Markopoulos A, Albanidou-Farmaki E, Kayavis I. Actinic chelitis: clinical and pathologic characteristics in 65 cases. Oral Dis. 2004;10:212–216. doi: 10.1111/j.1601-0825.2004.01004.x. [DOI] [PubMed] [Google Scholar]
- 3.Nico MMS, Rivitti EA, Laurenco SV. Actinic chelitis: histologic study of the entire vermilion and comparison with previous biopsy. J Cutan Pathol. 2007;34:309–314. doi: 10.1111/j.1600-0560.2006.00606.x. [DOI] [PubMed] [Google Scholar]
- 4.Röewert-Huber J, Stockfleth E, Kerl H. Pathology and pathobiology of actinic (solar) keratosis – an update. Br J Dermatol. 2007;157(suppl 2):18–20. doi: 10.1111/j.1365-2133.2007.08267.x. [DOI] [PubMed] [Google Scholar]
- 5.Ackerman AB, Mones JM. Solar (actinic) keratosis in squamous cell carcinoma. Br J Dermatol. 2006;155:9–22. doi: 10.1111/j.1365-2133.2005.07121.x. [DOI] [PubMed] [Google Scholar]
- 6.Bickers DR. Photosensitivity and other reactants to light. In: Kasper DL, et al., editors. Harrison’s Principles of Internal Medicine. 16th ed. New York: McGraw-Hill; 2005. pp. 324–329. [Google Scholar]
- 7.Cockerell CJ. Pathology and pathobiology of the actinic (solar) keratosis. Br J Dermatol. 2003;149(suppl 66):34–36. doi: 10.1046/j.0366-077x.2003.05625.x. [DOI] [PubMed] [Google Scholar]
- 8.Rossi R, Mor M, Lott T. Actinic keratosis. Int J Dermatol. 2007;46:895–904. doi: 10.1111/j.1365-4632.2007.03166.x. [DOI] [PubMed] [Google Scholar]
- 9.Holmes C, Foley P, Freeman M, Chong AH. Solar keratosis: Epidemiology, pathogenesis, presentation and treatment. Australas J Dermatol. 2007;48:67–76. doi: 10.1111/j.1440-0960.2007.00339.x. [DOI] [PubMed] [Google Scholar]
- 10.Neto Pimentel DR, Michalany N, Alchorne M, Abreu M, Borra RC, Weckx L. Actinic cheilitis: histopathology and p53. J Cutan Pathol. 2006;33:539–544. doi: 10.1111/j.1600-0560.2006.00440.x. [DOI] [PubMed] [Google Scholar]
- 11.Torma H, Berne B, Vahlquist A. UV irradiation and topical vitamin A modulate retinol esterification in hairless mouse epidermis. Acta Derm Venereol. 1988;68:291–299. [PubMed] [Google Scholar]
- 12.Matsumura Y, Ananthaswamy HN. Toxic effects of ultraviolet radiation on the skin. Toxicology and Applied Pharmacology. 2004;195:298–308. doi: 10.1016/j.taap.2003.08.019. [DOI] [PubMed] [Google Scholar]
- 13.Chiller KG, Washington C, Sober AJ, Koh HK. Cancer of the skin. In: Kasper DL, et al., editors. Harrisons Principles of Internal Medicine. 16th ed. New York: McGraw-Hill; 2005. pp. 497–503. [Google Scholar]
- 14.Nghiem P, Kupper TS. Basal- and squamous-cell carcinomas. In: Jameson JL, Collins FS, editors. Principles of Molecular Medicine Molecular Genetics. Humana Press Inc; New Jersey: 1998. pp. 785–788. [Google Scholar]
- 15.Horta MCR, de Assis LAP, de Souza AF, de Araujo VC, Gomez RS, Aguiar MCF. p53 and p21 WAF1/CIP1 overexpression at the invasive front of lower lip squamous cell carcinoma. J Oral Pathol Med. 2007;36:88–92. doi: 10.1111/j.1600-0714.2007.00495.x. [DOI] [PubMed] [Google Scholar]
- 16.Leffell DL. The scientific basis of skin cancer. J Am Acad Dermatol. 2000;42:518–522. doi: 10.1067/mjd.2000.103340. [DOI] [PubMed] [Google Scholar]
- 17.Gronskov K, Ek J, Brondum-Nielsen K. Oculocutaneous albinism. Orphanet J Rare Dis. 2007;2:43–53. doi: 10.1186/1750-1172-2-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bolognia JL, Braverman IM. Skin manifestation of internal disease. In: Kasper DL, et al., editors. Harrison’s Principles of Internal Medicine. 16th ed. New York: McGraw-Hill; 2005. pp. 296–311. [Google Scholar]
- 19.Hong ES, Zeeb H, Repacholi MH. Albinism in Africa as a public health issue. BMC Public Health. 2006;6:212–222. doi: 10.1186/1471-2458-6-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McBride SR, Leppard BJ. Attitudes and beliefs of an albino population toward sun avoidance. Arch Dermatol. 2002;138:629–632. doi: 10.1001/archderm.138.5.629. [DOI] [PubMed] [Google Scholar]
- 21.The South African Weather Service. Personal Communication. 2009 Sep 11; [Google Scholar]
- 22.Ulrich M, Maltusch A, Röewert-Huber J, González S, Sterry W, Stockfleth E, et al. Actinic keratoses: non-invasive diagnosis for field cancerisation. Br J Dermatol. 156(suppl 3):13–17. doi: 10.1111/j.1365-2133.2007.07865.x. 207. [DOI] [PubMed] [Google Scholar]
- 23.Rossi R, Assad GB, Buggiani G, Lotti T. Photodynamic therapy: treatment of choice for actinic cheilitis? Dermatol Ther. 2008;21:412–415. doi: 10.1111/j.1529-8019.2008.00224.x. [DOI] [PubMed] [Google Scholar]
- 24.Brawley OW, Kramer BS. Prevention and early detection of cancer. In: Kasper DL, et al., editors. Harrisons Principles of Internal Medicine. 16th ed. New York: McGraw-Hill; 2005. pp. 441–447. [Google Scholar]