Abstract
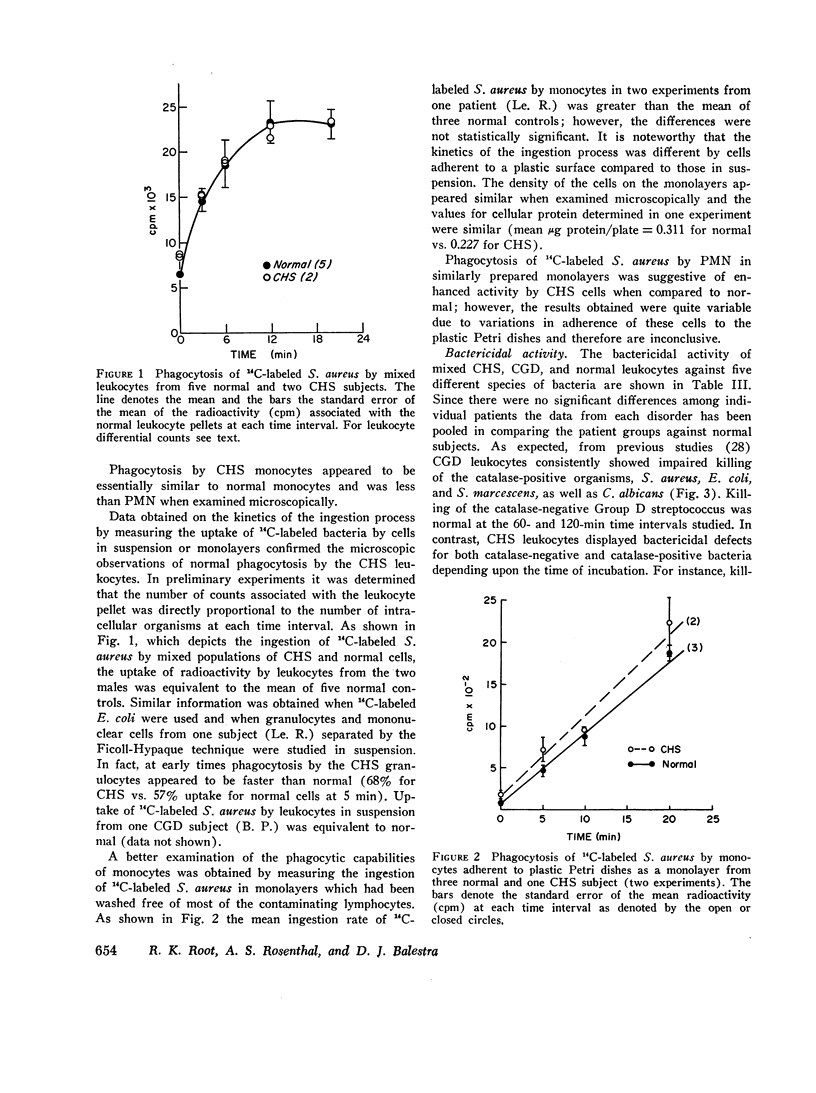
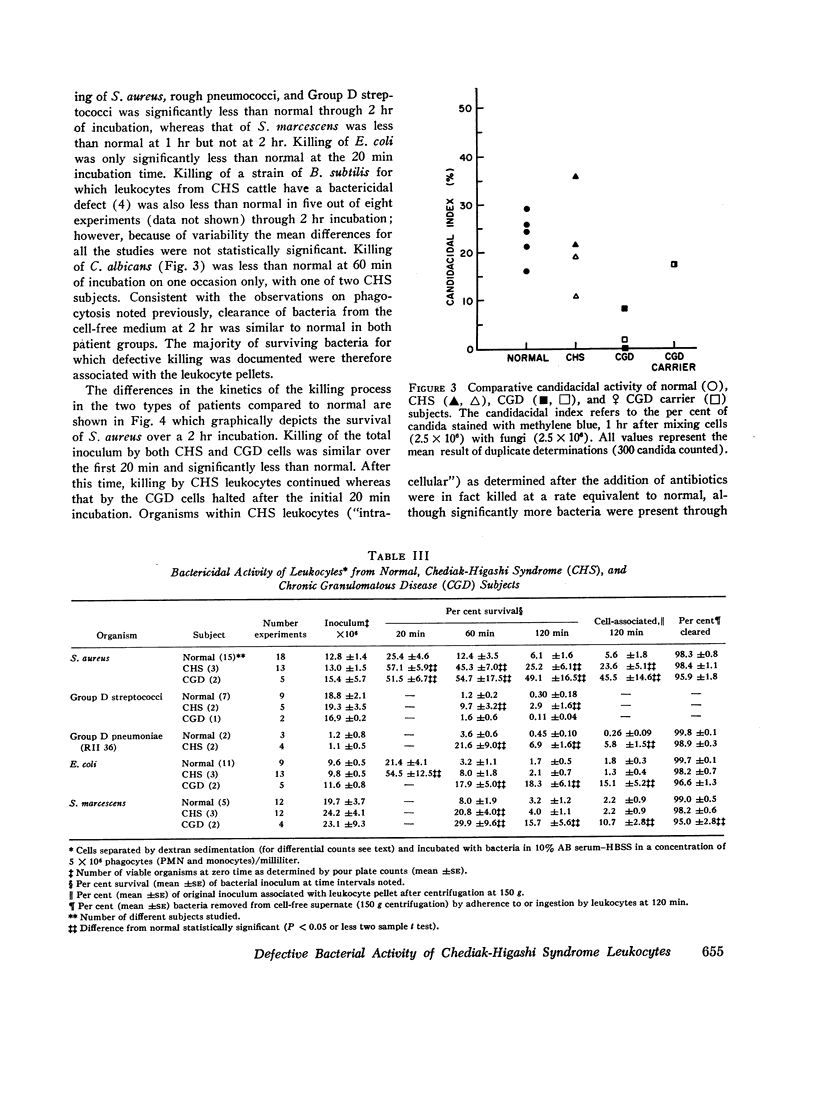
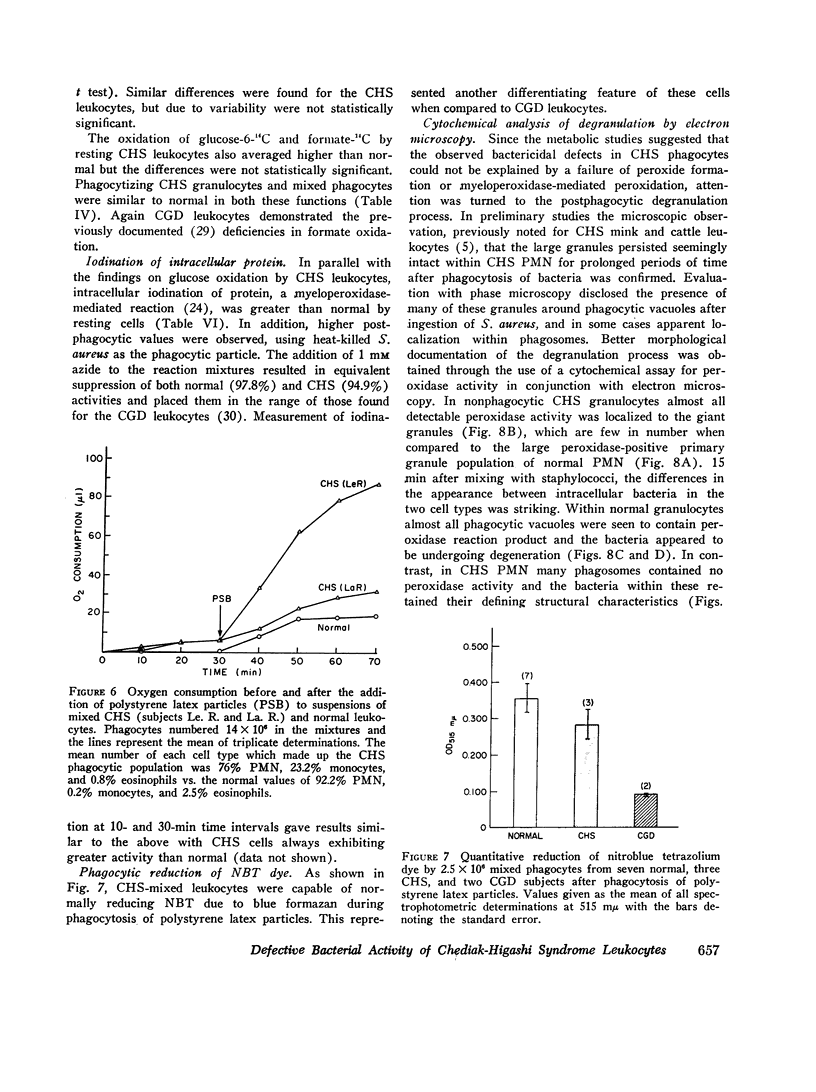
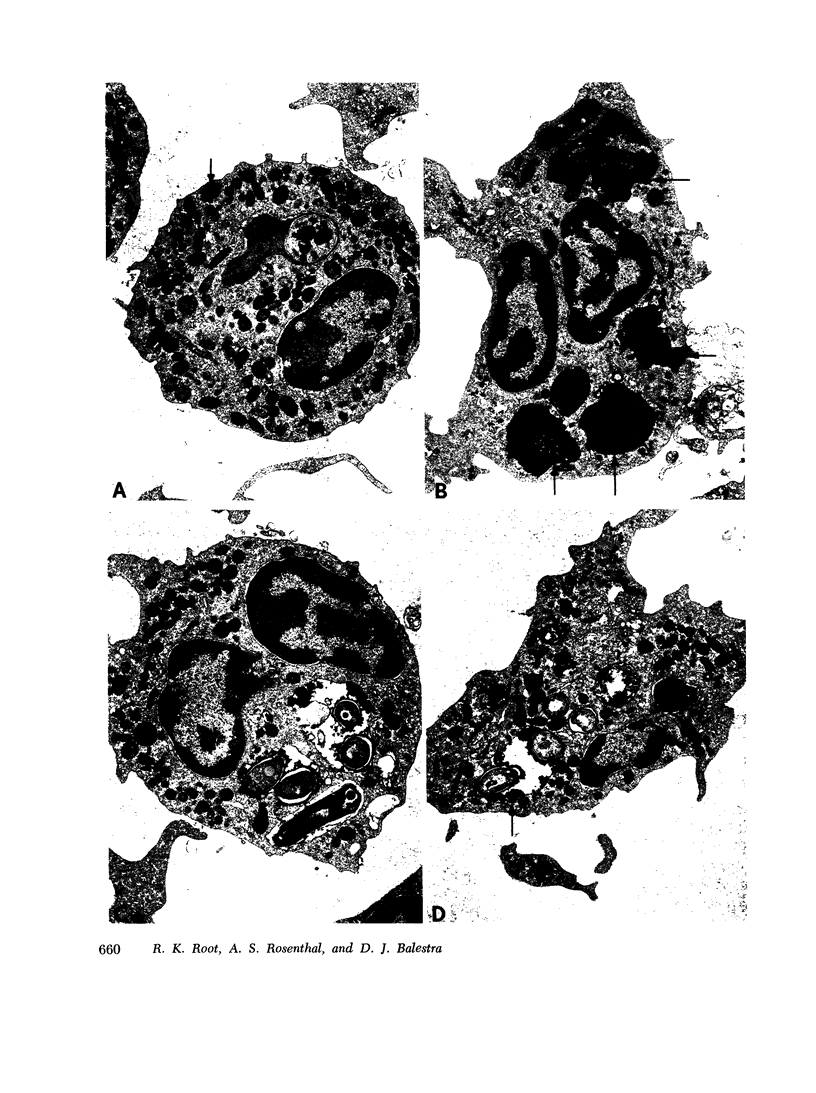
Phagocytic, antimicrobial, and metabolic functions were studied in leukocytes obtained from three patients with the Chediak-Higashi syndrome (CHS) and compared to normals, individuals, heterozygous for Chediak-Higashi syndrome, and two subjects with chronic granulomatous disease of childhood (CGD). Chediak-Higashi syndrome leukocytes showed normal ingestion of a variety of bacteria, Candida albicans, and polystyrene latex particles. Intracellular destruction was significantly impaired for Staphylococcus aureus, Group D streptococci, and a rough strain of Type II pneumococci over a 2 hr incubation. Killing of Serattia marcescens was consistently delayed at 1 hr whereas that of Escherichia coli and C. albicans appeared normal, unless the incubations were shortened to 20 min. Examination of the rates of killing indicated that the greatest defect occurred in the first 20 min of contact between Chediak-Higashi syndrome cells and bacteria. Separation of Chediak-Higashi syndrome granulocytes from monocytes revealed that the former were most defective in bactericidal activity. After phagocytosis, Chediak-Higashi syndrome granulocytes displayed a normal burst in oxygen consumption and oxidation of glucose-1-14C and glucose-6-14C and formate-14C. Oxidation of glucose-1-14C by non-phagocytizing Chediak-Higashi syndrome granulocytes and monocytes averaged 2-3 times normal, whereas glucose-6-14C and formate-14C oxidation were not significantly increased by resting cells. Iodination of intracellular protein by Chediak-Higashi syndrome leukocytes was significantly increased above normal in both the resting and phagocytizing state. Electron microscopic histochemistry revealed that almost all peroxidase activity was localized to the giant granules in Chediak-Higashi granulocytes, and after bacterial ingestion there was a failure of delivery of peroxidase to many phagosomes. Upon longer incubation more phagosomes acquired peroxidase activity, presumably through a fusion process, although many giant granules remained intact. The contrasting patterns and kinetics of the killing defects and the differing metabolic properties of Chediak-Higashi syndrome and chronic granulomatous disease leukocytes emphasize the pleiomorphic nature of inherited disorders of leukocyte function.
Full text
PDF











Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Axline S. G. Functional biochemistry of the macrophage. Semin Hematol. 1970 Apr;7(2):142–160. [PubMed] [Google Scholar]
- Baehner R. L., Nathan D. G. Quantitative nitroblue tetrazolium test in chronic granulomatous disease. N Engl J Med. 1968 May 2;278(18):971–976. doi: 10.1056/NEJM196805022781801. [DOI] [PubMed] [Google Scholar]
- Baggiolini M., Hirsch J. G., De Duve C. Resolution of granules from rabbit heterophil leukocytes into distinct populations by zonal sedimentation. J Cell Biol. 1969 Feb;40(2):529–541. doi: 10.1083/jcb.40.2.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellanti J. A., Cantz B. E., Schlegel R. J. Accelerated decay of glucose 6-phosphate dehydrogenase activity in chronic granulomatous disease. Pediatr Res. 1970 Sep;4(5):405–411. doi: 10.1203/00006450-197009000-00003. [DOI] [PubMed] [Google Scholar]
- Blume R. S., Bennett J. M., Yankee R. A., Wolff S. M. Defective granulocyte regulation in the Chediak-Higashi syndrome. N Engl J Med. 1968 Nov 7;279(19):1009–1015. doi: 10.1056/NEJM196811072791901. [DOI] [PubMed] [Google Scholar]
- Clark R. A., Kimball H. R. Defective granulocyte chemotaxis in the Chediak-Higashi syndrome. J Clin Invest. 1971 Dec;50(12):2645–2652. doi: 10.1172/JCI106765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cline M. J., Lehrer R. I. Phagocytosis by human monocytes. Blood. 1968 Sep;32(3):423–435. [PubMed] [Google Scholar]
- FALLON H. J., FREI E., 3rd, DAVIDSON J. D., TRIER J. S., BURK D. Leukocyte preparations from human blood: evaluation of their morphologic and metabolic state. J Lab Clin Med. 1962 May;59:779–791. [PubMed] [Google Scholar]
- HIRSCH J. G., STRAUSS B. STUDIES ON HEAT-LABILE OPSONIN IN RABBIT SERUM. J Immunol. 1964 Jan;92:145–154. [PubMed] [Google Scholar]
- Holmes B., Page A. R., Good R. A. Studies of the metabolic activity of leukocytes from patients with a genetic abnormality of phagocytic function. J Clin Invest. 1967 Sep;46(9):1422–1432. doi: 10.1172/JCI105634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes B., Quie P. G., Windhorst D. B., Good R. A. Fatal granulomatous disease of childhood. An inborn abnormality of phagocytic function. Lancet. 1966 Jun 4;1(7449):1225–1228. doi: 10.1016/s0140-6736(66)90238-8. [DOI] [PubMed] [Google Scholar]
- KARNOVSKY M. L. Metabolic basis of phagocytic activity. Physiol Rev. 1962 Jan;42:143–168. doi: 10.1152/physrev.1962.42.1.143. [DOI] [PubMed] [Google Scholar]
- KRITZLER R. A., TERNER J. Y., LINDENBAUM J., MAGIDSON J., WILLIAMS R., PRESIG R., PHILLIPS G. B. CHEDIAK-HIGASHI SYNDROME. CYTOLOGIC AND SERUM LIPID OBSERVATIONS IN A CASE AND FAMILY. Am J Med. 1964 Apr;36:583–594. doi: 10.1016/0002-9343(64)90106-8. [DOI] [PubMed] [Google Scholar]
- Kanfer J. N., Blume R. S., Yankee R. A., Wolff S. M. Alteration of sphingolipid metabolism in leukocytes from patients with the Chediak-Higashi syndrome. N Engl J Med. 1968 Aug 22;279(8):410–413. doi: 10.1056/NEJM196808222790806. [DOI] [PubMed] [Google Scholar]
- Klebanoff S. J. Iodination of bacteria: a bactericidal mechanism. J Exp Med. 1967 Dec 1;126(6):1063–1078. doi: 10.1084/jem.126.6.1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klebanoff S. J. Myeloperoxidase: contribution to the microbicidal activity of intact leukocytes. Science. 1970 Sep 11;169(3950):1095–1097. doi: 10.1126/science.169.3950.1095. [DOI] [PubMed] [Google Scholar]
- LOWRY O. H., ROSEBROUGH N. J., FARR A. L., RANDALL R. J. Protein measurement with the Folin phenol reagent. J Biol Chem. 1951 Nov;193(1):265–275. [PubMed] [Google Scholar]
- Lehrer R. I., Cline M. J. Interaction of Candida albicans with human leukocytes and serum. J Bacteriol. 1969 Jun;98(3):996–1004. doi: 10.1128/jb.98.3.996-1004.1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutzner M. A., Lowrie C. T., Jordan H. W. Giant granules in leukocytes of the beige mouse. J Hered. 1967 Nov-Dec;58(6):299–300. doi: 10.1093/oxfordjournals.jhered.a107620. [DOI] [PubMed] [Google Scholar]
- Mandell G. L., Hook E. W. Leukocyte bactericidal activity in chronic granulomatous disease: correlation of bacterial hydrogen peroxide production and susceptibility to intracellular killing. J Bacteriol. 1969 Oct;100(1):531–532. doi: 10.1128/jb.100.1.531-532.1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mickenberg I. D., Root R. K., Wolff S. M. Leukocytic function in hypogammaglobulinemia. J Clin Invest. 1970 Aug;49(8):1528–1538. doi: 10.1172/JCI106370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moran T. J., Estevez J. M. Chediak-Higashi disease. Morphologic studies of a patient and her family. Arch Pathol. 1969 Oct;88(4):329–339. [PubMed] [Google Scholar]
- PAGE A. R., BERENDES H., WARNER J., GOOD R. A. The Chediak-Higashi syndrome. Blood. 1962 Sep;20:330–343. [PubMed] [Google Scholar]
- Padgett G. A. Neutrophilic function in animals with the Chediak-Higashi syndrome. Blood. 1967 Jun;29(6):906–915. [PubMed] [Google Scholar]
- Pincus S. H., Klebanoff S. J. Quantitative leukocyte iodination. N Engl J Med. 1971 Apr 8;284(14):744–750. doi: 10.1056/NEJM197104082841402. [DOI] [PubMed] [Google Scholar]
- Reed P. W. Glutathione and the hexose monophosphate shunt in phagocytizing and hydrogen peroxide-treated rat leukocytes. J Biol Chem. 1969 May 10;244(9):2459–2464. [PubMed] [Google Scholar]
- SARAIVA L. G., AZEVEDO M., CORREA J. M., CARVALHO G., PROSPERO J. D. Anomalous panleukocytic granulation. Blood. 1959 Oct;14:1112–1127. [PubMed] [Google Scholar]
- Sadan N., Yaffe D., Rozenszajn L., Adar H., Soroker B., Efrati P. Cytochemical and genetic studies in four cases of Chediak-Higashi-Steinbrinck syndrome. Acta Haematol. 1965 Jul;34(1):20–29. doi: 10.1159/000209426. [DOI] [PubMed] [Google Scholar]
- Salazar Mallén M., Amezcua Chavarría M. E., Rivas Pástor E. S. Comportamiento antibacteriano de los leucocitos en sujetos normales, en la enfermedad de Chediak-Highashi y en la anomalia de Pelger-Huet. Rev Invest Salud Publica. 1970 Jan-Mar;30(1):5–16. [PubMed] [Google Scholar]
- Stossel T. P., Pollard T. D., Mason R. J., Vaughan M. Isolation and properties of phagocytic vesicles from polymorphonuclear leukocytes. J Clin Invest. 1971 Aug;50(8):1745–1747. doi: 10.1172/JCI106664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stossel T. P., Root R. K., Vaughan M. Phagocytosis in chronic granulomatous disease and the Chediak-Higashi syndrome. N Engl J Med. 1972 Jan 20;286(3):120–123. doi: 10.1056/NEJM197201202860302. [DOI] [PubMed] [Google Scholar]
- Ward P. A., Schlegel R. J. Impaired leucotactic responsiveness in a child with recurrent infections. Lancet. 1969 Aug 16;2(7616):344–347. doi: 10.1016/s0140-6736(69)92699-3. [DOI] [PubMed] [Google Scholar]
- Wolff S. M. The Chediak-Higashi syndrome: studies of host defenses. Ann Intern Med. 1972 Feb;76(2):293–306. doi: 10.7326/0003-4819-76-2-293. [DOI] [PubMed] [Google Scholar]






