Abstract
This review focuses on the evidence accumulated in humans and animal models to the effect that mitochondria are key players in the progression of heart failure (HF). Mitochondria are the primary source of energy in the form of adenosine triphosphate that fuels the contractile apparatus, and are thus essential for the pumping activity of the heart. We evaluate changes in mitochondrial morphology and alterations in the main components of mitochondrial energetics, such as substrate utilization and oxidative phosphorylation coupled with the level of respirasomes, in the context of their contribution to the chronic energy deficit and mechanical dysfunction in HF.
Keywords: Heart failure, Mitochondria, Respirasomes, Oxidative phsophorylation, Reversible phosphorylation
1. Introduction
Heart failure (HF) is an enormous medical and societal burden. More than 2% of the US population is affected, with an annual mortality rate for mild-to-moderate failure of 10%1,2 and for severe failure over 50%, and a cost in the USA of $28 billion annually for treatment.3 HF is a complex multifactorial syndrome characterized by mechanical dysfunction of the myocardium and the inability of the heart to supply adequate amounts of blood to meet the perfusion and metabolic needs of the body. Defects in bioenergetics, increased preload and afterload, altered signal transduction pathways, abnormalities of calcium homeostasis, as well as neurohormonal dysregulation are major pathogenic factors for myocardial dysfunction in HF. Despite significant advances in therapy, particularly inhibition of the renin–angiotensin and sympathetic nervous systems, HF remains a progressive syndrome.
In order to support both electrical and mechanical activities (contractility and diastolic relaxation), the heart needs a continuous energy supply. This requirement is met by the daily synthesis of approximately 30 kg of the high-energy molecule adenosine triphosphate (ATP),4 produced mainly by mitochondrial oxidative phosphorylation. Cardiac energy deficits have been reported in HF5–7 due to alterations in all components of cardiac energetics.2,8 Therefore, the improvement of myocardial energetics becomes a promising approach to the treatment of HF.
Mitochondrial oxidative phosphorylation relies not only on the activities of individual complexes, but also on the coordinated action of supramolecular assemblies (respirasomes) of the electron transport chain (ETC) complexes in both normal9 and failing heart.10 In human mtDNA mutant cybrids with impaired mitochondrial respiration, the recovery of mitochondrial function correlates with the formation of respirasomes11 suggesting that respirasomes represent regulatory units of mitochondrial oxidative phosphorylation12 by facilitating the electron transfer between the catalytic sites of the ETC. We recently reported a decrease in mitochondrial respirasomes in HF10 that fits in the category of a new mitochondrial cytopathy.
This review provides an overview of the regulation of the cardiac mitochondrial function in health and disease, and the current state of knowledge concerning the contribution of mitochondrial energy deficit to the progression of HF.
2. Cardiac mitochondrial populations in heart and disease
2.1. Morphology
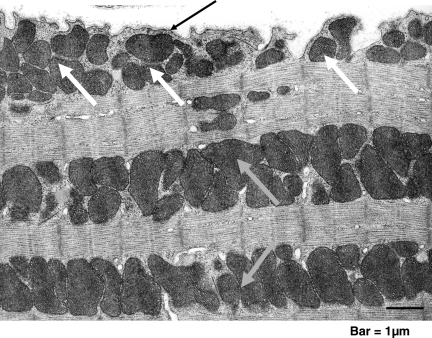
Conventional transmission electron microscopy of mammalian cardiac tissue reveals mitochondria to be elliptical individual organelles situated either in clusters beneath the sarcolemma (subsarcolemmal mitochondria, SSM) or in parallel, longitudinal rows ensconced within the contractile apparatus (interfibrillar mitochondria, IFM) (Figure 1). The two mitochondrial populations differ in their cristae morphology,13 with a lamelliform orientation in SSM, whereas the cristae orientation in IFM is tubular.14
Figure 1.
Cardiac mitochondria. Transmission electron micrograph of mouse myocardium. Clusters of subsarcolemmal mitochondria (SSM, white arrows) are situated immediately beneath the sarcolemma (black arrow); longitudinal rows of mitochondria that are located within the contractile apparatus (myofibrils) are interfibrilar mitochondria (IFM, grey arrows).
The morphology of mitochondria is responsive to changes in cardiomyocytes. For example, following endurance exercise in mice, cardiac hypertrophy is accompanied by giant mitochondria with disorganized cristae.15 Cardiac hypertrophy secondary to aortic constriction in rats16 is associated with increased mitochondrial size, as well as increased replication of mitochondrial DNA. Alterations of other non-mitochondrial cardiomyocyte compartments may be associated with changes in mitochondria. For example, transgenic mice harbouring a missense allele of cardiac troponin T to mimic the human familial hypertrophic cardiomyopathy experience cardiac myofibrillar degeneration associated with an increased number of small mitochondria with a loss of membranes and cristae.17
By examining endocardial biopsies from humans with hypertrophic and dilated cardiomyopathy, Baandrup et al.18 found giant mitochondria with decreased matrix density in some cardiomyocytes, associated with increased mitochondrial number. Also, in a canine model of chronic HF of moderate severity, an increased number of smaller mitochondria with the loss of matrix density and intramitochondrial myelin figures19 was reported. These alterations in mitochondrial morphology are associated with changes in mitochondrial bioenergetics, such as decreased oxidative phosphorylation measured in both permeabilized cardiac fibres19 and isolated mitochondria.10
2.2. Mitochondrial biogenesis
Modifications in mitochondrial morphology are usually associated with changes in mitochondrial number. The dividing of pre-existent organelles is dependent on mitochondrial fission, requires neosynthesis of phospholipids and proteins, and is controlled at the level of transcription of both mitochondrial and nuclear DNA. Mitochondrial transcription is promoted by the binding of the mitochondrial transcription factor A (mtTFA) on an upstream enhancer of the two mitochondrial DNA strands. The peroxisome proliferator-activated receptor (PPAR) gamma co-activator (PGC-1α) is considered the master synchronizer of the two genomes, by increasing the transcriptional activity of the nuclear respiratory factors (NFRs) on mtTFA promoter and of the PPARα. NFRs increase the expression of mtTFA and the vast majority of nuclear-encoded subunits of the tricarboxylic acid cycle and ETC complexes. The transcription factor PPARα increases the expression of genes encoding for the mitochondrial fatty acid (FA) transport and oxidation enzymes. The PGC-1α controls the optimal mitochondrial content that is critical for cardiomyocyte function.20,21
2.2.1. Mitochondrial biogenesis in physiological hypertrophy
Mitochondrial content needs to parallel cardiomyocyte growth in order to meet cellular energy requirement. However, whether cardiomyocyte enlargement induced by physiological stimuli (i.e. sustained exercise training) is accompanied by an increase in mitochondrial biogenesis is not clear, and was reported either increased22 or unchanged.23,24 Also, it is still debated if physiological stimuli drive an increase in mitochondrial content independent of cardiomyocyte hypertrophy. Notable, FA oxidation was reported unchanged25 suggesting the absence of a metabolic remodelling in physiological hypertrophy.
2.2.2. Mitochondrial biogenesis in pathological hypertrophy
The activities of the mitochondrial marker enzyme citrate synthase and of cytochrome c oxidase, as well as the expression of oxidative phosphorylation genes26,27 were reported unchanged when measured in the homogenates of cardiac tissue originating from hypertrophied hearts. These data suggest that mitochondrial biogenesis matches the energy demand of the hypertrophic cardiomyocyte during compensated cardiac hypertrophy.
2.2.3. Mitochondrial biogenesis in HF
A downregulation of the entire pathway of mitochondrial biogenesis was reported in HF. First, a decrease in cardiac expression of the transcription factor PGC-1α was found in different experimental models of HF.28–30 Second, downregulation of NFRs and mtTFA was also reported,28 as well as of tricarboxylic acid cycle and ETC enzymes.28,31,32
In contrast, primary mitochondrial defects in both humans and animal models are associated with increased mitochondrial proliferation and cardiomyopathy. For example, Sebastiani et al.32 found an increase in mtDNA and mitochondrial proliferation with myofibril displacement, associated with increased expression of genes involved in mitochondrial biogenesis in humans with cardiomyopathies induced by mitochondrial defects. Increased mitochondrial proliferation was also found in murine models of cardiomyopathies associated with ablation of the adenine nucleotide translocase 1,33 frataxin,34 Mn-SOD,35 and mtTFA.36 The increased mitochondrial mass in the myocardium of mtTFA knockout mice is accompanied by a decrease in mtDNA and transcripts for cytochrome c oxidase subunit I (encoded by mtDNA), as well as reduced expression of PPARα transcripts, PPARα-dependent genes, and impaired ETC. The severe ATP depletion indicates that the mitochondrial defect cannot be compensated by the increase in mitochondrial number. Of notice, this model of cardiomyopathy is characterized by a discrepancy between increased mitochondrial proliferation and decreased mitochondrial maturation (decreased mtDNA and mtDNA transcripts, with defects in all ETC complexes containing mtDNA-encoded subunits). Single polymorphisms in the PGC-1α gene have been identified which correlate with an increased risk of hypertrophic cardiomyopathy.37 Taken together, these observations suggest that primary alterations in mitochondrial biogenesis may contribute to cardiac pathologies.
2.3. Biochemical properties
Cardiac SSM and IFM differ in both their inherited properties and response to disease. Rat,38 rabbit,39 hamster,40 and human41 heart IFM oxidize substrates at higher rates compared with heart SSM, with no differences in their coupling abilities and cytochrome content. The greater permeability of SSM to exogenous NADH42 suggests a decrease in their inner membrane intactness. SSM also are more susceptible to calcium overload-mediated cytochrome c release and mitochondrial damage compared with IFM.43
An increased susceptibility of cardiac SSM to ischaemic damage has been observed in rat44 and rabbit.45 During ischaemia of the isolated perfused rabbit heart, cardiac SSM sustain a loss of the phospholipid cardiolipin (CL), with decrease in oxidative phosphorylation through cytochrome oxidase and loss of cytochrome c.45 SSM also produce reactive oxygen species (ROS) following ischaemic damage.46 In contrast, cardiac IFM experience an age-related increased susceptibility towards mitochondrial permeability transmission pore opening47 associated with decreased yield and oxidative phosphorylation39 due to a defect in the cytochrome c binding site in complex III. Ageing-related mitochondrial defects predispose to a greater susceptibility to ischaemia compared with adult hearts due to a defect in the iron–sulfur protein in complex III.48 Despite an increase in the antioxidant defense mechanisms, a significant increase in oxidative stress markers was described in cardiac IFM compared with SSM with age.49
Cardiac IFM are also more sensitive to diabetic damage. Experimental-induced diabetes in rats causes a decrease in CL content, oxidative phosphorylation, and complex III activity, associated with an increase in superoxide production and oxidative-induced modifications of proteins and lipids in cardiac IFM.50 Also, increased apoptotic susceptibility of cardiac IFM was reported in experimental diabetes, with lower mitochondrial membrane potential and antiapoptotic proteins, and increased permeability transition pore opening.51
These data emphasize the importance of studying both mitochondrial populations when attempting to elucidate the contribution of mitochondrial dysfunction to cardiac failure. In contrast, other studies report that both cardiac mitochondrial populations are equally affected in HF. For example, a decrease in the content of CL and activity of complex III occur acutely after myocardial infarction in both cardiac SSM and IFM, which lead to decreased mitochondrial respiration and increased ROS production.52 A loss of CL also was reported in dilated cardiomyopathy in humans and spontaneously hypertensive HF in rats, and correlated with reduced complex IV activity in both populations of cardiac mitochondria.53 In a model of microembolims-induced HF of moderate severity in dogs, we found that both populations of heart mitochondria experience a decrease in oxidative phosphorylation and amount of supercomplexes,10 without changes in CL content and molecular species.
3. Myocardial substrate metabolism in the normal and failing heart
3.1. Substrate utilization in the normal heart
ATP utilized by the heart is synthesized mainly by means of oxidative phosphorylation in the inner mitochondrial membrane, a process that involves the coupling of electron transfer and oxygen consumption with phosphorylation of ADP to ATP. The catabolism of exogenous substrates (FAs, glucose, pyruvate, lactate, and ketone bodies) provides the reduced intermediates, NADH (nicotinamide adenine dinucleotide, reduced) and FADH2 (flavin adenine dinucleotide, reduced), as donors for mitochondrial electron transport.
The myocardium has the remarkable ability to switch between carbohydrate and fat as fuel sources (metabolic flexibility) so that ATP production is maintained at a constant rate in the face of diverse physiological and dietary conditions. The catabolism of FA provide up to 90% of the ATP in the healthy heart.4 The contribution of glucose to the acetyl CoA pool in the heart is increased by insulin during the postprandial period and during exercise. Substrate switching also is achieved by acute regulation of transcription of metabolic enzymes in response to changes in substrate level,54 oxygen availability,55 and the intrinsic circadian clock within cardiomyocytes.56,57
3.2. ‘Metabolic remodelling’58 in the failing heart
Most clinical59–61 and experimental62–64 studies find that both hypertrophied and failing heart have an intrinsic metabolic inflexibility characterized by a shift toward glucose oxidation at the expense of FA oxidation. However, most studies report that the decrease in FA oxidation is not compensated for by an increase in glucose oxidation.63,65 As a consequence, the failing heart is an energy-compromised organ.
Does mitochondrial remodelling underlie this metabolic remodelling?
Defects at specific sites of the mitochondrial ETC, decrease in oxidative phosphorylation, as well as decrease in mitochondrial density may impair the capacity of myocardium to oxidize FAs as energetic substrates, whereas glycolysis is unaffected. Impairment of FA oxidation also may be secondary to changes in the activity and kinetic properties of carnitine palmitoyltransferase I (CPT I), the controlling step in the entry of long-chain FAs to the mitochondria. CPT I is inhibited by malonyl-CoA. The results reported by various studies differ regarding the changes in the content of malonyl-CoA in the failing myocardium.66–68 In moderately severe HF in dogs, our group did not observe any difference in the activity of CPT I and its sensitivity toward inhibition by malonyl-CoA. However, malonyl-CoA content was decreased by 22% with HF, suggesting less in vivo inhibition of CPT I activity.
Alternatively, the decline in FA oxidation in the failing heart is due to the reduction in the expression of genes involved in mitochondrial transport and oxidation of FAs as a consequence of the decline in the activity of the nuclear receptor PPARα. However, changes reported in patients with HF lack consistency.69,70 Moreover, discrepancies between the expression of PPARα, mRNA, and protein content of FA oxidation enzymes, and FA oxidation rates were reported in HF,71 suggesting that postranslational modifications may play a role in the regulation of FA oxidation enzymes and FA oxidation rates.
Since sustained activation of the β-adrenergic receptor-stimulatory GTP-binding protein-adenylyl cyclase (AC) signalling pathway in HF has deleterious effects on the heart, treatment with β-blockers is beneficial.72 However, it was reported that the β-blocker, metoprolol, inhibits mitochondrial FA β-oxidation via a direct effect on the catalytic activity and malonyl-CoA sensitivity of CPT I.73 CPT I stably interacts and is directly controlled by phosphorylation induced by cAMP-protein kinase A (PKA) pathway as an effector of the β1-adrenergic receptor signalling.74 PKA enhances the binding between the anchoring protein, AKAP149, and both liver and heart CPT I isoforms on heart mitochondria, increases the phosphorylated state, and decreases malonyl-CoA sensitivity without affecting the catalytic activity of CPT I.
4. New aspects of mitochondrial function and dysfunction in HF
4.1. Oxidative phosphorylation and respirasomes
Mitochondrial oxidative phosphorylation forms the basis for ATP production. In mammalian mitochondria, the oxidative phosphorylation system is composed of four oxidoreductase complexes (complexes I, II, III, and IV) and the ATP synthase (complex V). Three of the four oxidoreductase complexes couple electron transport with translocation of protons from the mitochondrial matrix to the intermembrane space, thus generating an inner membrane proton gradient75 that drives the synthesis of ATP from ADP and Pi by complex V.
According to the structural model of the mitochondrial inner membrane, initially proposed more than 50 years ago by Chance and Williams76 and expanded and amplified by Schagger's group,9 the structural support for oxidative phosphorylation is provided by assemblies of the ETC complexes into supercomplexes. The supercomplex consisting of complex I, dimeric complex III, and one copy of complex IV (I1III2IV1) found in rodent,77 dog,10 and bovine9 heart mitochondria, also contains coenzyme Q and cytochrome c, and functions as a cohesive respiratory unit (respirasome) because it transports electrons from NADH to reduce oxygen.78 According to the three-dimensional map of the bovine heart I1III2IV1 supercomplex,79 the individual complexes physically interact in this assembly, and the electron carriers have short diffusion distances between complexes, supporting the concept of channelled electron transfer that decreases electron leakage and superoxide production.80
The ETC complexes, whether unincorporated in respirasomes or organized in supercomplexes, are embedded in the phospholipid bilayer of the mitochondrial inner membrane. CL is an anionic phospholipid present almost exclusively in the mitochondrial inner membrane of eukaryotic cells. Tetra-linoleoyl-CL [(C18:2)4-CL] is the predominant form of all CL species and provides structural and functional support to components of both the mitochondrial ETC and phosphorylation apparatus.81–85 Recent studies suggest that CL plays a central role in the higher order organization of mitochondrial ETC in supercomplexes. It was reported that CL is essential for either formation86 or stabilization of respiratory supercomplexes in both yeast87,88 and humans.89
4.2. Regulation of mitochondrial function
As the main ATP provider for cardiomyocytes, mitochondrial function is regulated according to cellular energetic needs via signal transduction pathways that involve second messengers, such as cAMP, calcium, or ROS.
4.2.1. Reversible phosphorylation
Reversible phosphorylation of proteins is a main cellular regulatory mechanism. The largely impermeable inner mitochondrial membrane keeps mitochondrial proteins out of reach of signalling cascades initiated by cytosolic kinases. However, a computational analysis predicted that 5% of protein kinases are targeted to mitochondria in yeast.90 A recent review estimated that 18 out of 63 mitochondrial phosphoproteins participate in oxidative phosphorylation.91 However, the list of mitochondrial phosphoproteins has markedly increased since then.
There is accumulating evidence that reversible phosphorylation at serine and threonine amino acid residues induced by cAMP-activated PKA changes the function of mitochondrial proteins. The cAMP/PKA signalling pathway is enhanced by sympathetic stimulation. Cardiomyocytes β1 receptors couple to the stimulatory G protein, activate the AC, and increase cytosolic cAMP. Binding of cAMP to the regulatory subunits of PKA induces the dissociation of the holoenzyme and phosphorylation by the catalytic subunits of sarcolemmal L-type Ca channels and sarcoplasmic phospholamban, with increase in the cytosolic calcium responsible for the positive chronotropic and inotropic effects. There is a pronounced activation of the sympathetic system in animals and patients with HF that is inversely correlated with survival. The use of β1-selective receptor blockers is clinically beneficial,72 leading to a reduction by a third or more in the risk of death, a benefit considered greater than that yielded by any other drug used in HF. These data suggest that the regulation of the cAMP/PKA pathway may be responsible for the protective effect of β1-receptor antagonists in HF.
Besides the transmembrane AC, soluble AC regulated by pH, bicarbonate, and calcium, and localized mainly to mitochondria and nucleus92 has been identified. The two distinct ACs suggest subcellular pools of cAMP that can be regulated differently in response to either extra- or intracellular signals. Fluorescent resonance energy transfer analysis revealed a rapid increase in cAMP within mitochondria of cells stimulated with a β agonist,93 despite the restricted diffusion of cAMP in the cytosol (<1 µm). These data suggest either a preferential accumulation of cAMP within the mitochondria or an increase in the activity of mitochondrial soluble AC induced by β-adrenergic stimulation. Recently, it was shown that the cAMP that activates mitochondrial PKA and increases oxidative phosphorylation via phosphorylation of complex IV subunits is generated within the mitochondria by mitochondrial AC activated by the tricarboxylic acid cycle-generated CO2.94 Thus, cAMP represents a regulator of oxidative phosphorylation, ensuring that electron transport responds to both extracellular and mitochondrial stimuli.
Additional evidence shows that mitochondria have a complete cAMP-PKA signalling pathway: (i) using both immuno-gold electron microscopy and ELISA95 in tissues and isolated mitochondria, respectively, PKA holoenzyme has been identified at the inner membrane and matrix of heart, skeletal muscle, brain, and kidney mitochondria; (ii) there is functional evidence for the presence of PKA in the mitochondrial inner membrane;96–100 (iii) PKA is recruited to the outer mitochondrial membrane by A-kinase anchoring proteins (AKAPs);101–103 (iv) signal-terminating mechanisms, such as phosphodiesterases94 and phosphatases104,105 also, are present within the mitochondria.
cAMP/PKA-induced phosphorylation events that change the function of the proteins occur on components of all mitochondrial ETC complexes and phosphorylation apparatus (Table 1). However, the mere identification of a phophorylation event in relation to a mitochondrial protein is insufficient to conclude that the post-translational modification regulates mitochondrial function. At least two other criteria must be met. First, the existence of these phopshorylation events must be confirmed in vivo. For example, the phosphorylation of the ESSS subunit in complex I was not identified in vivo,106 and the site of phosphorylation not conserved in mammals.107 Therefore, the significance of this post-translational modification in the regulation of complex I assembly at present is not established in mammalian mitochondria. Second, solid evidence of the regulatory effect of these phosphorylation events on the function of the protein is mandatory.
Table 1.
Mitochondrial phosphoproteins and their potential role in regulation of mitochondrial function
| Protein | Location | Role | Source | Phosphorylation (P*) sites | Effect of P* on function |
|---|---|---|---|---|---|
| C I | |||||
| ESSS | Matrix arm of complex I | C I assembly145 | Bovine heart107 | Serine 20107 | Increases C I activity90 |
| Mouse fibroblasts90 | |||||
| 10 kDa subunit | Intermembrane site in C I | C I assembly146 | Bovine heart107 | Serine 55107,147 | Increases C I activity and decreases ROS production147 |
| Rat heart147 | |||||
| 42 kDa subunit | MIM148 | NADH-binding149 | Bovine heart106 | Threonine?106 | Unknown |
| Serine 59150 | |||||
| C II | |||||
| Flavo protein subunit | Matrix side of C II | FAD binding and succinate-ubiquinone reduction | Tumour cells151 | Unknown | Decreases succinate-ubiquinone reductase and increases fumarate reductase activities151 |
| C III | |||||
| Core I | MIM | Bovine heart150 | Unknown | Unknown | |
| Human sperma152 | |||||
| Core II | MIM | Bovine heart150 | Unknown | Unknown | |
| Yeast153 | Serine 141 | Unknown | |||
| Cyt c | Mitochondrial intermembrane space | Transfer of electrons from C III to C IV | Bovine heart154 | Tyrosine 97154 | Reduces oxidation of P*-cytochrome c by C IV154,155 |
| Bovine liver155 | Tyrosine 48155 | ||||
| C IV | |||||
| Subunit I | MIM | Cyt c oxidation, oxygen reduction, proton translocation | Bovine heart and liver113,114 | Tyrosine 304113,114 | Inhibits complex IV activity113,114 |
| Bovine heart156 | Suggested serine 441110; threonine?156 | Turns on the allosteric inhibition of complex IV by high ATP156 | |||
| Subunit II | MIM | Cyt c oxidation, oxygen reduction, proton translocation | Human osteoclasts | Tyrosine?157 | Increases C IV activity157 |
| Murine fibroblasts | Tyrosine?158 | Decreases COX activity and ATP level158 | |||
| Subunit IV | MIM | Regulation of C IV by the ATP/ADP ratio | Bovine liver159 | Unknown159 | Unknown |
| Bovine heart156 | Serine 34156 | Unknown | |||
| Yeast153 | Threonine 55153 | Unknown | |||
| Subunit Va | Matrix side of C IV | Regulation of complex IV by thyroid hormons | Bovine heart156 | Serine 4156 | Unknown |
| Threonine 35156 | |||||
| Subunit VIb | Intermembrane side of C IV | Cooperativity between the two cyt c binding sites within the C IV dimer | Yeast153 | Serine 82153 | Unknown |
| C V | |||||
| Subunit α | Matrix part of C V (F1) | ATP synthesis from ADP and Pi | Bovine heart Potato160 | Unknown; | Unknown |
| Yeast153 | Serine 178 | Unknown | |||
| Subunit β | Matrix part of C V (F1) | ATP synthesis from ADP and Pi | Human skeletal muscle161 | Threonine? | Unknown |
| Yeast153 | Serine 373; Threonine 237153 | Unknown | |||
| Subunit δ | Matrix part of C V (F1) | ATP synthesis from ADP and Pi | Potato | Unknown | Unknown |
| Subunit γ | Matrix part of C V (F1) | ATP synthesis from ADP and Pi | Yeast | Serine 62153 | Decreases the dimerization of C V153 |
| Adenine nucleotide translocase | MIM | ADP, ATP transport | Yeast153 | Serine 42, 155, 157; Threonine 39, 156153 | Unknown |
| Tyrosine 190, 194162 | Facilitates nucleotide transport and increases cellular respiration | ||||
| Phosphate carrier | MIM | Phosphate transport | Bovine heart106 | Unknown;106 | Unknown |
| Yeast153 | Serine 4, 145; Threonine 297153 | Unknown | |||
C I, Complex I; C II, Complex II; C III, Complex III; C IV, Complex V; MIM, mitochondrial inner membrane; Cyt c, cytochrome c; ?, sequence not given.
Recent studies suggest that cytochrome c oxidase is a main target for the regulation of oxidative phosphorylation by cAMP-dependent phosphorylation.108,109 Phophorylation of serine 441 in subunit I of isolated kidney and bovine heart cytochrome c oxidase switches on the allosteric inhibition of the enzyme at high intramitochondrial ATP,108,110 whereas calcium-activated dephosphorylation turns it off. These data led to the proposal of the second regulatory mechanism of oxidative phosphorylation by high intramitochondrial ATP/ADP ratios.110,111 In contrast to the first mechanism of respiratory control, mediated through the proton gradient across the mitochondrial inner membrane, the second mechanism is independent of proton motive force, but based on the exchange of bound ADP by ATP in subunit IV at high intramitochondrial ATP ratios. The dependency of ATP synthase on membrane potential (Δψm) leads to high intramitochondrial ATP at a Δψm of 100–120 mV followed by phosphorylation and inhibition of cytochrome c oxidase, which prevents further increase in membrane potential. Because at Δψm values above 140 mV, mitochondrial ROS formation increases exponentially with increasing Δψm,112 it is proposed that the second mechanism of respiratory control maintains low Δψm values and prevents ROS production.
The allosteric regulation of complex IV by ADP/ATP ratio is overruled by a cAMP-dependent tyrosine phosphorylation of subunit I at tyrosine 304 induced by an as-yet unknown tyrosine kinase. This modification causes alterations in the kinetic properties of cytochrome c oxidase, with decrease in Vmax and increase in Km and full inhibition at physiological concentration of the substrate cytochrome c.113 This tyrosine residue is conserved in all eukaryotes examined and in some bacteria. Moreover, glucagon and TNFα have similar inhibitory effects on cytochrome c oxidase,114 suggesting that this regulation has significance in vivo. It is suggested that the phosphorylation of tyrosine 304 in subunit I located at the interface between the two complex IV monomers may regulate their interaction.113
Phosphorylation of complex IV subunits emerges as either detrimental or beneficial for complex IV activity in both normal cardiac mitochondria (Table 1), as well as in mitochondria isolated from pathologic myocardium. Experimental hypoxia and cardiac ischaemia cause increased PKA-dependent phosphorylation of subunits I, IVi1, and Vb of complex IV115 associated with lower activity of complex IV and increased ROS production.116 In contrast to these studies, upregulation of mitochondrial soluble AC improves COX activity and mitochondrial respiration,94 as well as mitochondrial biogenesis in a ROS-dependent manner, in cultured cells and in animals with COX deficiency.117
4.2.2. Calcium
Mitochondria are targets of calcium signalling in cardiomyocytes. Close apposition with the endoplasmic reticulum (ER) allow mitochondria to rapidly accumulate calcium upon its release from the ER via ryanodine receptors through the opening of the inositol 1,4,5-triphosphate-gated channels.118 It was shown that the increase in mitochondrial calcium concentration leads to increased NADH production119–122 and upregulation of ATP production.123
Calcium directly activates key mitochondrial metabolic enzymes (pyruvate, α-ketoglutarate, and isocitrate dehydrogenases). Recent work has shown that there are additional calcium-dependent signalling pathways operative in mitochondria which may affect oxidative phosphorylation, such as calcium-dependent protein kinases and calcineurin.
The calcium- and phospholipid-dependent signalling pathway is represented by the classical members of the protein kinase C (PKC) family. Activation of PKC-α leads to a sustained decrease in oxidative phosphorylation and membrane depolarization preceded by an inhibition of ATP synthase activity.124 In a different study, Liu et al.125 showed that the α, β, and ε subunits of ATP synthase have PKC consensus motifs, and the PKC-α-induced phosphorylation of β subunit of ATP synthase on a serine residue inhibits the activity of complex V. PKC-dependent phosphorylation of subunit IV of complex IV increases complex IV activity in neonatal cardiac myocytes.126
The effect of mitochondrial calcium-activated serine/threonine phosphatase calcineurin signalling pathway on mitochondria was uncovered by studies of transgenic mice with cardiac-specific expression of an active calcineurin cDNA which exhibit cardiac hypertrophy that progresses to HF.127 Cardiac SSM from such mice have decreased ADP-dependent oxidative phosphorylation rates with complex II and IV substrates, protein contents of ND3 subunit of complex I and subunit I of complex IV (encoded by mitochondrial DNA), as well as subunit IV of complex IV (encoded by nuclear DNA) and increased superoxide production. These calcium-dependent changes in mitochondrial function might contribute to the development of HF.
4.3. Defects in individual components of the ETC and phosphorylation apparatus in HF
A variety of mitochondrial defects has been described in the ETC complexes and components of the phosphorylation apparatus in both humans and experimental models of HF, and was evaluated by us in a recent review.128 Most of these mitochondrial defects have not been confirmed by other groups. Moreover, a direct causal relationship between the purported mitochondrial defects and HF either has not been studied or has proven elusive.129 In addition, the link between the reported specific defects and the decrease in mitochondrial oxidative phosphorylation has not been studied. Why is this link important? Mitochondria achieve the maximal oxidative capacity when the limitation by the phosphorylation system is released experimentally by the addition of an uncoupler.10,130 These data suggest that there is an apparent excess in the activity of ETC complexes relative to the phosphorylation apparatus and the oxidative phosphorylation requirement.131,132 The sites of control of respiration in normal heart-isolated mitochondria are located at complex I in the ETC133 and at adenine nucleotide translocase and complex V in the phosphorylation apparatus.134 In contrast, in a large variety of intact cells, the site of control of oxidative phosphorylation is located in complex IV135 due to the ATP-allosteric inhibition of the complex.136 Therefore, flux control analysis is necessary in both heart mitochondria and cardiac fibres isolated from failing hearts to establish a link between the ETC defects and the decreased oxidative phosphorylation.
4.4. Abnormalities in integrated mitochondrial function
The analysis of oxidative phosphorylation assesses the integrated function of the ETC coupled to ATP synthesis, membrane transport, dehydrogenase activities, and the structural integrity of the mitochondria. Decreased ADP-dependent respiratory rates were reported when oxygen consumption28 was measured in saponin-permeabilized cardiac fibres isolated from rat,28,137 dog,19 and human138 hearts with dilated cardiomyopathy as well as pressure overload and ischaemic HF.138,139 In contrast, oxygen consumption by swine myocardium with pressure overload congestive HF was unchanged.140 The reduced respiratory rates in cardiac fibres may be due to either a drop in mitochondrial function or a decrease in mitochondrial density. Citrate synthase activity and mitochondrial DNA copy number have been considered markers of mitochondrial density. However, discrepancies between these parameters were reported in HF, suggesting that these parameters may not be reliable to indicate changes in mitochondrial biogenesis in the failing cardiomyocytes.28 Also, respiratory studies on cardiac fibres do not differentiate between the two distinct mitochondrial populations, SSM and IFM mitochondria.38,42 Some of the reported disparate findings regarding defects in mitochondrial respiration in HF141–143 were reconciled when the two distinct populations of cardiac mitochondria were separated and investigated.40,144 These data were evaluated by us in a previous review.128 We conclude here that studies on oxidative phosphorylation in freshly isolated cardiac SSM and IFM give a more accurate picture of the topology of bioenergetic defect in cardiac pathology.
4.5. Decrease in oxidative phosphorylation and respirasomes in HF
In a follow-up to the work of Sharov et al.19 on oxidative phosphorylation in saponin-permeabilized cardiac fibres, we performed a comprehensive study of respiratory properties of the two populations of heart mitochondria10 in a canine model of intracoronary microembolization-induced HF of moderate severity. Both populations of heart mitochondria were equally affected in this model of HF. We found a dramatic decrease in state 3 respiratory rates with substrates donating electrons at different sites in the ETC that was not relieved by an uncoupler, indicating that the defect in oxidative phosphorylation is localized in the terminal part of the ETC at the level of complex IV. However, neither complex IV activity nor the amount of the substrate cytochrome c was altered in HF. We concluded that the decrease in oxidative phosphorylation of heart mitochondria can be explained by the decrease in the amount of functional respirasomes.
We further asked whether this defect in the supramolecular assembly is due to changes in the phospholipids of the mitochondrial inner membrane or modifications of the subunits of the ETC complexes. The content of the main phospholipid species, including CL, as well as the molecular species of CL, was unchanged in cardiac mitochondria in HF. In heart mitochondria isolated from HF, complex IV not incorporated into the respirasomes contained an increased content of threonine phosphorylation. This suggested that cAMP-dependent phosphorylation may have a role in decreasing the level of supercomplexes. In saponin-permeabilized heart muscle fibres, cAMP caused a decrease in oxidative phosphorylation, at least at the level of complex IV (unpublished observations). We suggest that phosphorylation of specific complex IV subunits either limits the incorporation of complex IV in supercomplexes or decreases supercomplex stability.
According to our findings,10 we propose a mechanistic pathway by which the decrease in mitochondrial functional respirasomes drives the progression of HF. The decrease in respirasomes in HF is the primary event causing the decrease in mitochondrial oxidative phosphorylation, and is coupled with an increase in electron leakage and superoxide generation in complexes I and III that are not incorporated within respirasomes. Complex I-generated superoxide is responsible for the oxidative alterations of mtNDA and the adjacent mitochondrial inner membrane lipids and proteins including subunits of the ETC complexes. These modifications cause the decreased activity of ETC complexes reported by others in severe HF, potentially decrease oxidative phosphorylation, and finally lead to the degradation of the damaged complexes. Complex III-generated superoxide is responsible for the oxidative alterations of the cytosolic myofibrillar proteins. This sequence of events signals the transition to irreversible heart damage.
5. Conclusions, future direction
HF is a multifactorial syndrome characterized by mechanical dysfunction of the myocardium. Recent studies identify mitochondria as both the target and the origin of major pathogenic pathways which lead to the progression of myocardial dysfunction. As the main process that drives the cardiac pump, mitochondrial oxidative phosphorylation is regulated by reversible phosphorylation induced by cAMP, which is either synthesized within the mitochondria or generated by the stimulatory G protein-coupled AC as an effector of the β-receptor activation. Therefore, excessive sympathetic stimulation may dysregulate mitochondrial function by affecting either individual complexes or their supramolecular assemblies (respirasomes). Mitochondrial defects lead to metabolic remodelling, deficit in cardiac energetics, and increased oxidative stress. Therefore, the elucidation of mitochondrial cytopathy in HF is crucial and forms the basis of a therapeutic strategy to maintain mitochondrial integrity, optimize substrate metabolism, alleviate oxidative stress, and improve the contractile function of myocardium.
Funding
This work was supported by the National Heart, Lung and Blood Institute Program Project Grant PO1 (PO1 HL074237).
Acknowledgements
We thank Bernard Tandler for editorial assistance, and Hisashi Fujioka for providing the electron micrograph of the mouse heart.
Conflict of interest: none declared.
References
- 1.McMurray JJ, Pfeffer MA. Heart failure. Lancet. 2005;365:1877–1889. doi: 10.1016/S0140-6736(05)66621-4. doi:10.1016/S0140-6736(05)66621-4. [DOI] [PubMed] [Google Scholar]
- 2.Neubauer S. The failing heart—an engine out of fuel. NEJM. 2007;356:1140–1151. doi: 10.1056/NEJMra063052. doi:10.1056/NEJMra063052. [DOI] [PubMed] [Google Scholar]
- 3.Dayer M, Cowie MR. Heart failure: diagnosis and healthcare burden. Clin Med. 2004;4:13–18. doi: 10.7861/clinmedicine.4-1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ashrafian H, Frenneaux MP. Metabolic modulation in heart failure: the coming of age. Cardiovasc Drug Ther. 2007;21:5–7. doi: 10.1007/s10557-007-6000-z. doi:10.1007/s10557-007-6000-z. [DOI] [PubMed] [Google Scholar]
- 5.Sanbe A, Tanonaka K, Kobayasi R, Takeo S. Effects of long-term therapy with ACE inhibitors, captopril, enalapril and trandolapril, on myocardial energy metabolism in rats with heart failure following myocardial infarction. J Mol Cell Cardiol. 1995;27:2209–2222. doi: 10.1016/s0022-2828(95)91551-6. doi:10.1016/S0022-2828(95)91551-6. [DOI] [PubMed] [Google Scholar]
- 6.Neubauer S, Horn M, Cramer M, Harre K, Newell JB, Peters W, et al. Myocardial phosphocreatine-to-ATP ratio is a predictor of mortality in patients with dilated cardiomyopathy. Circulation. 1997;96:2190–2196. doi: 10.1161/01.cir.96.7.2190. [DOI] [PubMed] [Google Scholar]
- 7.Beer M, Seyfarth T, Sandstede J, Landschutz W, Lipke C, Kostler H, et al. Absolute concentrations of high-energy phosphate metabolites in normal, hypertrophied, and failing human myocardium measured noninvasively with (31)P-SLOOP magnetic resonance spectroscopy. J Am Coll Cardiol. 2002;40:1267–1274. doi: 10.1016/s0735-1097(02)02160-5. doi:10.1016/S0735-1097(02)02160-5. [DOI] [PubMed] [Google Scholar]
- 8.Stanley WC, Recchia FA, Lopaschuk GD. Myocardial substrate metabolism in the normal and failing heart. Physiol Rev. 2005;85:1093–1129. doi: 10.1152/physrev.00006.2004. doi:10.1152/physrev.00006.2004. [DOI] [PubMed] [Google Scholar]
- 9.Schagger H, Pfeiffer K. Supercomplexes in the respiratory chains of yeast and mammalian mitochondria. EMBO J. 2000;19:1777–1783. doi: 10.1093/emboj/19.8.1777. doi:10.1093/emboj/19.8.1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosca MG, Vazquez EJ, Kerner J, Parland W, Chandler MP, Stanley W, et al. Cardiac mitochondria in heart failure: decrease in respirasomes and oxidative phosphorylation. Cardiovasc Res. 2008;80:30–39. doi: 10.1093/cvr/cvn184. doi:10.1093/cvr/cvn184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.D'Aurelio M, Gajewski CD, Lenaz G, Manfredi G. Respiratory chain supercomplexes set the threshold for respiration defects in human mtDNA mutant cybrids. Hum Mol Genet. 2006;15:2157–2169. doi: 10.1093/hmg/ddl141. doi:10.1093/hmg/ddl141. [DOI] [PubMed] [Google Scholar]
- 12.Boekema EJ, Braun HP. Supramolecular structure of the mitochondrial oxidative phosphorylation system. J Biol Chem. 2007;282:1–4. doi: 10.1074/jbc.R600031200. doi:10.1074/jbc.R600031200. [DOI] [PubMed] [Google Scholar]
- 13.Hoppel CL, Tandler B, Fujioka H, Riva A. Dynamic organization of mitochondria in human heart and in myocardial disease. Int J Biochem Cell Biol. 2009;41:1949–1956. doi: 10.1016/j.biocel.2009.05.004. doi:10.1016/j.biocel.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Riva A, Tandler B, Loffredo F, Vazquez E, Hoppel C. Structural differences in two biochemically defined populations of cardiac mitochondria. Am J Physiol. 2005;289:H868–H872. doi: 10.1152/ajpheart.00866.2004. doi:10.1152/ajpcell.00115.2005. [DOI] [PubMed] [Google Scholar]
- 15.Coleman R, Silbermann M, Gershon D, Reznick AZ. Giant mitochondria in the myocardium of aging and endurance-trained mice. Gerontol. 1987;33:34–39. doi: 10.1159/000212851. doi:10.1159/000212851. [DOI] [PubMed] [Google Scholar]
- 16.Zak R, Rabinowitz M, Rajamanickam C, Merten S, Kwiatkowska-Patzer B. Mitochondrial proliferation in cardiac hypertrophy. Basic Res Cardiol. 1980;75:171–178. doi: 10.1007/BF02001410. doi:10.1007/BF02001410. [DOI] [PubMed] [Google Scholar]
- 17.Tardiff JC, Hewett TE, Palmer BM, Olsson C, Factor SM, Moore RL, et al. Cardiac troponin T mutations result in allele-specific phenotypes in a mouse model for hypertrophic cardiomyopathy. J Clin Invest. 1999;104:469–481. doi: 10.1172/JCI6067. doi:10.1172/JCI6067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baandrup U, Florio RA, Roters F, Olsen EG. Electron microscopic investigation of endomyocardial biopsy samples in hypertrophy and cardiomyopathy. A semiquantitative study in 48 patients. Circulation. 1981;63:1289–1298. doi: 10.1161/01.cir.63.6.1289. [DOI] [PubMed] [Google Scholar]
- 19.Sharov VG, Goussev A, Lesch M, Goldstein S, Sabbah HN. Abnormal mitochondrial function in myocardium of dogs with chronic heart failure. J Mol Cell Cardiol. 1998;30:1757–1762. doi: 10.1006/jmcc.1998.0739. doi:10.1006/jmcc.1998.0739. [DOI] [PubMed] [Google Scholar]
- 20.Lai L, Leone TC, Zechner C, Schaeffer PJ, Kelly SM, Flanagan DP, et al. Transcriptional coactivators PGC-1alpha and PGC-lbeta control overlapping programs required for perinatal maturation of the heart. Genes Dev. 2008;22:1948–1961. doi: 10.1101/gad.1661708. doi:10.1101/gad.1661708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lehman JJ, Barger PM, Kovacs A, Saffitz JE, Medeiros DM, Kelly DP. Peroxisome proliferator-activated receptor gamma coactivator-1 promotes cardiac mitochondrial biogenesis. J Clin Invest. 2000;106:847–856. doi: 10.1172/JCI10268. doi:10.1172/JCI10268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stuewe SR, Gwirtz PA, Agarwal N, Mallet RT. Exercise training enhances glycolytic and oxidative enzymes in canine ventricular myocardium. J Mol Cell Cardiol. 2000;32:903–913. doi: 10.1006/jmcc.2000.1131. doi:10.1006/jmcc.2000.1131. [DOI] [PubMed] [Google Scholar]
- 23.Kayar SR, Conley KE, Claassen H, Hoppeler H. Capillarity and mitochondrial distribution in rat myocardium following exercise training. J Exp Biol. 1986;120:189–199. doi: 10.1242/jeb.120.1.189. [DOI] [PubMed] [Google Scholar]
- 24.Kemi OJ, Hoydal MA, Haram PM, Garnier A, Fortin D, Ventura-Clapier R, et al. Exercise training restores aerobic capacity and energy transfer systems in heart failure treated with losartan. Cardiovasc Res. 2007;76:91–99. doi: 10.1016/j.cardiores.2007.06.008. doi:10.1016/j.cardiores.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 25.Iemitsu M, Miyauchi T, Maeda S, Sakai S, Fujii N, Miyazaki H, et al. Cardiac hypertrophy by hypertension and exercise training exhibits different gene expression of enzymes in energy metabolism. Hypertens Res. 2003;26:829–837. doi: 10.1291/hypres.26.829. doi:10.1291/hypres.26.829. [DOI] [PubMed] [Google Scholar]
- 26.Nishio ML, Ornatsky OI, Craig EE, Hood DA. Mitochondrial biogenesis during pressure overload induced cardiac hypertrophy in adult rats. Can J Physiol Pharmacol. 1995;73:630–637. doi: 10.1139/y95-080. [DOI] [PubMed] [Google Scholar]
- 27.Wiesner RJ, Aschenbrenner V, Ruegg JC, Zak R. Coordination of nuclear and mitochondrial gene expression during the development of cardiac hypertrophy in rats. Am J Physiol. 1994;267:C229–C235. doi: 10.1152/ajpcell.1994.267.1.C229. [DOI] [PubMed] [Google Scholar]
- 28.Garnier A, Fortin D, Delomenie C, Momken I, Veksler V, Ventura-Clapier R. Depressed mitochondrial transcription factors and oxidative capacity in rat failing cardiac and skeletal muscles. J Physiol. 2003;551:491–501. doi: 10.1113/jphysiol.2003.045104. doi:10.1113/jphysiol.2003.045104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sun CK, Chang LT, Sheu JJ, Wang CY, Youssef AA, Wu CJ, et al. Losartan preserves integrity of cardiac gap junctions and PGC-1 alpha gene expression and prevents cellular apoptosis in remote area of left ventricular myocardium following acute myocardial infarction. Int Heart J. 2007;48:533–546. doi: 10.1536/ihj.48.533. doi:10.1536/ihj.48.533. [DOI] [PubMed] [Google Scholar]
- 30.Watson PA, Reusch JE, McCune SA, Leinwand LA, Luckey SW, Konhilas JP, et al. Restoration of CREB function is linked to completion and stabilization of adaptive cardiac hypertrophy in response to exercise. Am J Physiol. 2007;293:H246–H259. doi: 10.1152/ajpheart.00734.2006. doi:10.1152/ajpcell.00464.2006. [DOI] [PubMed] [Google Scholar]
- 31.Jullig M, Hickey AJ, Chai CC, Skea GL, Middleditch MJ, Costa S, et al. Is the failing heart out of fuel or a worn engine running rich? A study of mitochondria in old spontaneously hypertensive rats. Proteomics. 2008;8:2556–2572. doi: 10.1002/pmic.200700977. doi:10.1002/pmic.200700977. [DOI] [PubMed] [Google Scholar]
- 32.Sebastiani M, Giordano C, Nediani C, Travaglini C, Borchi E, Zani M, et al. Induction of mitochondrial biogenesis is a maladaptive mechanism in mitochondrial cardiomyopathies. J Am Coll Cardiol. 2007;50:1362–1369. doi: 10.1016/j.jacc.2007.06.035. doi:10.1016/j.jacc.2007.06.035. [DOI] [PubMed] [Google Scholar]
- 33.Graham BH, Waymire KG, Cottrell B, Trounce IA, MacGregor GR, Wallace DC. A mouse model for mitochondrial myopathy and cardiomyopathy resulting from a deficiency in the heart/muscle isoform of the adenine nucleotide translocator. Nat Genet. 1997;16:226–234. doi: 10.1038/ng0797-226. doi:10.1038/ng0797-226. [DOI] [PubMed] [Google Scholar]
- 34.Puccio H, Simon D, Cossee M, Criqui-Filipe P, Tiziano F, Melki J, et al. Mouse models for Friedreich ataxia exhibit cardiomyopathy, sensory nerve defect and Fe-S enzyme deficiency followed by intramitochondrial iron deposits. Nat Genet. 2001;27:181–186. doi: 10.1038/84818. doi:10.1038/84818. [DOI] [PubMed] [Google Scholar]
- 35.Li Y, Huang TT, Carlson EJ, Melov S, Ursell PC, Olson JL, et al. Dilated cardiomyopathy and neonatal lethality in mutant mice lacking manganese superoxide dismutase. Nat Genet. 1995;11:376–381. doi: 10.1038/ng1295-376. doi:10.1038/ng1295-376. [DOI] [PubMed] [Google Scholar]
- 36.Hansson A, Hance N, Dufour E, Rantanen A, Hultenby K, Clayton DA, et al. A switch in metabolism precedes increased mitochondrial biogenesis in respiratory chain-deficient mouse hearts. Proc Natl Acad Sci USA. 2004;101:3136–3141. doi: 10.1073/pnas.0308710100. doi:10.1073/pnas.0308710100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang S, Fu C, Wang H, Shi Y, Xu X, Chen J, et al. Polymorphisms of the peroxisome proliferator-activated receptor-gamma coactivator-1alpha gene are associated with hypertrophic cardiomyopathy and not with hypertension hypertrophy. Clin Chem Lab Med. 2007;45:962–967. doi: 10.1515/CCLM.2007.189. doi:10.1515/CCLM.2007.189. [DOI] [PubMed] [Google Scholar]
- 38.Palmer JW, Tandler B, Hoppel CL. Biochemical properties of subsarcolemmal and interfibrillar mitochondria isolated from rat cardiac muscle. J Biol Chem. 1977;252:8731–8739. [PubMed] [Google Scholar]
- 39.Fannin SW, Lesnefsky EJ, Slabe TJ, Hassan MO, Hoppel CL. Aging selectively decreases oxidative capacity in rat heart interfibrillar mitochondria. Arch Biochem Biophys. 1999;372:399–407. doi: 10.1006/abbi.1999.1508. doi:10.1006/abbi.1999.1508. [DOI] [PubMed] [Google Scholar]
- 40.Hoppel CL, Tandler B, Parland W, Turkaly JS, Albers LD. Hamster cardiomyopathy. A defect in oxidative phosphorylation in the cardiac interfibrillar mitochondria. J Biol Chem. 1982;257:1540–1548. [PubMed] [Google Scholar]
- 41.Weinstein ES, Benson DW, Fry DE. Subpopulations of human heart mitochondria. J Surg Res. 1986;40:495–498. doi: 10.1016/0022-4804(86)90221-0. doi:10.1016/0022-4804(86)90221-0. [DOI] [PubMed] [Google Scholar]
- 42.Palmer JW, Tandler B, Hoppel CL. Biochemical differences between subsarcolemmal and interfibrillar mitochondria from rat cardiac muscle: effects of procedural manipulations. Arch Biochem Biophys. 1985;236:691–702. doi: 10.1016/0003-9861(85)90675-7. doi:10.1016/0003-9861(85)90675-7. [DOI] [PubMed] [Google Scholar]
- 43.Palmer JW, Tandler B, Hoppel CL. Heterogeneous response of subsarcolemmal heart mitochondria to calcium. Am J Physiol. 1986;250:H741–H748. doi: 10.1152/ajpheart.1986.250.5.H741. [DOI] [PubMed] [Google Scholar]
- 44.Duan J, Karmazyn M. Relationship between oxidative phosphorylation and adenine nucleotide translocase activity of two populations of cardiac mitochondria and mechanical recovery of ischemic hearts following reperfusion. Can J Physiol Pharmacol. 1989;67:704–709. doi: 10.1139/y89-114. [DOI] [PubMed] [Google Scholar]
- 45.Lesnefsky EJ, Tandler B, Ye J, Slabe TJ, Turkaly J, Hoppel CL. Myocardial ischemia decreases oxidative phosphorylation through cytochrome oxidase in subsarcolemmal mitochondria. Am J Physiol. 1997;273:H1544–H1554. doi: 10.1152/ajpheart.1997.273.3.H1544. [DOI] [PubMed] [Google Scholar]
- 46.Lesnefsky EJ, Chen Q, Moghaddas S, Hassan MO, Tandler B, Hoppel CL. Blockade of electron transport during ischemia protects cardiac mitochondria. J Biol Chem. 2004;279:47961–47967. doi: 10.1074/jbc.M409720200. doi:10.1074/jbc.M409720200. [DOI] [PubMed] [Google Scholar]
- 47.Hofer T, Servais S, Seo AY, Marzetti E, Hiona A, Upadhyay SJ, et al. Bioenergetics and permeability transition pore opening in heart subsarcolemmal and interfibrillar mitochondria: effects of aging and lifelong calorie restriction. Mech Ageing Dev. 2009;130:297–307. doi: 10.1016/j.mad.2009.01.004. doi:10.1016/j.mad.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lesnefsky EJ, Gudz TI, Migita CT, Ikeda-Saito M, Hassan MO, Turkaly PJ, et al. Ischemic injury to mitochondrial electron transport in the aging heart: damage to the iron-sulfur protein subunit of electron transport complex III. Arch Biochem Biophys. 2001;385:117–128. doi: 10.1006/abbi.2000.2066. doi:10.1006/abbi.2000.2066. [DOI] [PubMed] [Google Scholar]
- 49.Judge S, Jang YM, Smith A, Hagen T, Leeuwenburgh C. Age-associated increases in oxidative stress and antioxidant enzyme activities in cardiac interfibrillar mitochondria: implications for the mitochondrial theory of aging. FASEB J. 2005;19:419–421. doi: 10.1096/fj.04-2622fje. [DOI] [PubMed] [Google Scholar]
- 50.Dabkowski ER, Williamson CL, Bukowski VC, Chapman RS, Leonard SS, Peer CJ, et al. Diabetic cardiomyopathy-associated dysfunction in spatially distinct mitochondrial subpopulations. Am J Physiol. 2009;296:H359–H369. doi: 10.1152/ajpheart.00467.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Williamson CL, Dabkowski ER, Baseler WA, Croston TL, Alway SE, Hollander JM. Enhanced apoptotic propensity in diabetic cardiac mitochondria: influence of subcellular spatial location. Am J Physiol. 2009;298:H633–H642. doi: 10.1152/ajpheart.00668.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Heather LC, Carr CA, Stuckey DJ, Pope S, Morten KJ, Carter EE, et al. Critical role of complex III in the early metabolic changes following myocardial infarction. Cardiovasc Res. 2010;85:127–136. doi: 10.1093/cvr/cvp276. doi:10.1093/cvr/cvp276. [DOI] [PubMed] [Google Scholar]
- 53.Sparagna GC, Chicco AJ, Murphy RC, Bristow MR, Johnson CA, Rees ML, et al. Loss of cardiac tetralinoleoyl cardiolipin in human and experimental heart failure. J Lipid Res. 2007;48:1559–1570. doi: 10.1194/jlr.M600551-JLR200. doi:10.1194/jlr.M600551-JLR200. [DOI] [PubMed] [Google Scholar]
- 54.Huss JM, Kelly DP. Nuclear receptor signaling and cardiac energetics. Circ Res. 2004;95:568–578. doi: 10.1161/01.RES.0000141774.29937.e3. doi:10.1161/01.RES.0000141774.29937.e3. [DOI] [PubMed] [Google Scholar]
- 55.Giordano FJ. Oxygen, oxidative stress, hypoxia, and heart failure. J Clin Invest. 2005;115:500–508. doi: 10.1172/JCI200524408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Young ME. The circadian clock within the heart: potential influence on myocardial gene expression, metabolism, and function. Am J Physiol. 2006;290:H1–H16. doi: 10.1152/ajpheart.00582.2005. [DOI] [PubMed] [Google Scholar]
- 57.Durgan DJ, Trexler NA, Egbejimi O, McElfresh TA, Suk HY, Petterson LE, et al. The circadian clock within the cardiomyocyte is essential for responsiveness of the heart to fatty acids. J Biol Chem. 2006;281:24254–24269. doi: 10.1074/jbc.M601704200. doi:10.1074/jbc.M601704200. [DOI] [PubMed] [Google Scholar]
- 58.van Bilsen M, Smeets PJ, Gilde AJ, van der Vusse GJ. Metabolic remodelling of the failing heart: the cardiac burn-out syndrome? Cardiovasc Res. 2004;61:218–226. doi: 10.1016/j.cardiores.2003.11.014. doi:10.1016/j.cardiores.2003.11.014. [DOI] [PubMed] [Google Scholar]
- 59.Sochor H, Schelbert HR, Schwaiger M, Henze E, Phelps ME. Studies of fatty acid metabolism with positron emission tomography in patients with cardiomyopathy. Eur J Nucl Med. 1986;12:S66–S69. doi: 10.1007/BF00258110. [DOI] [PubMed] [Google Scholar]
- 60.Davila-Roman VG, Vedala G, Herrero P, de las Fuentes L, Rogers JG, Kelly DP, et al. Altered myocardial fatty acid and glucose metabolism in idiopathic dilated cardiomyopathy. J Am Coll Cardiol. 2002;40:271–277. doi: 10.1016/s0735-1097(02)01967-8. [DOI] [PubMed] [Google Scholar]
- 61.de las Fuentes L, Herrero P, Peterson LR, Kelly DP, Gropler RJ, Davila-Roman VG. Myocardial fatty acid metabolism: independent predictor of left ventricular mass in hypertensive heart disease. Hypertension. 2003;41:83–87. doi: 10.1161/01.hyp.0000047668.48494.39. [DOI] [PubMed] [Google Scholar]
- 62.Allard MF, Schonekess BO, Henning SL, English DR, Lopaschuk GD. Contribution of oxidative metabolism and glycolysis to ATP production in hypertrophied hearts. Am J Physiol. 1994;267:H742–H750. doi: 10.1152/ajpheart.1994.267.2.H742. [DOI] [PubMed] [Google Scholar]
- 63.Recchia FA, McConnell PI, Bernstein RD, Vogel TR, Xu X, Hintze TH. Reduced nitric oxide production and altered myocardial metabolism during the decompensation of pacing-induced heart failure in the conscious dog. Circ Res. 1998;83:969–979. doi: 10.1161/01.res.83.10.969. [DOI] [PubMed] [Google Scholar]
- 64.Christe ME, Rodgers RL. Altered glucose and fatty acid oxidation in hearts of the spontaneously hypertensive rat. J Mol Cell Cardiol. 1994;26:1371–1375. doi: 10.1006/jmcc.1994.1155. [DOI] [PubMed] [Google Scholar]
- 65.Neglia D, De Caterina A, Marraccini P, Natali A, Ciardetti M, Vecoli C, et al. Impaired myocardial metabolic reserve and substrate selection flexibility during stress in patients with idiopathic dilated cardiomyopathy. Am J Physiol. 2007;293:H3270–H3278. doi: 10.1152/ajpheart.00887.2007. [DOI] [PubMed] [Google Scholar]
- 66.Osorio JC, Stanley WC, Linke A, Castellari M, Diep QN, Panchal AR, et al. Impaired myocardial fatty acid oxidation and reduced protein expression of retinoid X receptor-alpha in pacing-induced heart failure. Circulation. 2002;106:606–612. doi: 10.1161/01.cir.0000023531.22727.c1. [DOI] [PubMed] [Google Scholar]
- 67.Kantor PF, Robertson MA, Coe JY, Lopaschuk GD. Volume overload hypertrophy of the newborn heart slows the maturation of enzymes involved in the regulation of fatty acid metabolism. J Am Coll Cardiol. 1999;33:1724–1734. doi: 10.1016/s0735-1097(99)00063-7. [DOI] [PubMed] [Google Scholar]
- 68.Chandler MP, Kerner J, Huang H, Vazquez E, Reszko A, Martini WZ, et al. Moderate severity heart failure does not involve a downregulation of myocardial fatty acid oxidation. Am J Physiol. 2004;287:H1538–H1543. doi: 10.1152/ajpheart.00281.2004. [DOI] [PubMed] [Google Scholar]
- 69.Razeghi P, Young ME, Ying J, Depre C, Uray IP, Kolesar J, et al. Downregulation of metabolic gene expression in failing human heart before and after mechanical unloading. Cardiology. 2002;97:203–209. doi: 10.1159/000063122. [DOI] [PubMed] [Google Scholar]
- 70.Schupp M, Kintscher U, Fielitz J, Thomas J, Pregla R, Hetzer R, et al. Cardiac PPARalpha expression in patients with dilated cardiomyopathy. Eur J Heart Fail. 2006;8:290–294. doi: 10.1016/j.ejheart.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 71.Morgan EE, Chandler MP, Young ME, McElfresh TA, Kung TA, Rennison JH, et al. Dissociation between gene and protein expression of metabolic enzymes in a rodent model of heart failure. Eur J Heart Fail. 2006;8:687–693. doi: 10.1016/j.ejheart.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 72.Bristow MR. beta-adrenergic receptor blockade in chronic heart failure. Circulation. 2000;101:558–569. doi: 10.1161/01.cir.101.5.558. [DOI] [PubMed] [Google Scholar]
- 73.Sharma V, Dhillon P, Wambolt R, Parsons H, Brownsey R, Allard MF, et al. Metoprolol improves cardiac function and modulates cardiac metabolism in the streptozotocin-diabetic rat. Am J Physiol. 2008;294:H1609–H1620. doi: 10.1152/ajpheart.00949.2007. [DOI] [PubMed] [Google Scholar]
- 74.Sharma V, Abraham T, So A, Allard MF, McNeill JH. Functional effects of protein kinases and peroxynitrite on cardiac carnitine palmitoyltransferase-1 in isolated mitochondria. Mol Cell Biochem. 2010;337:223–237. doi: 10.1007/s11010-009-0303-2. [DOI] [PubMed] [Google Scholar]
- 75.Mitchell P. Possible molecular mechanisms of the protonmotive function of cytochrome systems. J Theor Biol. 1976;62:327–367. doi: 10.1016/0022-5193(76)90124-7. [DOI] [PubMed] [Google Scholar]
- 76.Chance B, Williams GR. A method for the localization of sites for oxidative phosphorylation. Nature. 1955;176:250–254. doi: 10.1038/176250a0. [DOI] [PubMed] [Google Scholar]
- 77.Wittig I, Carrozzo R, Santorelli FM, Schagger H. Supercomplexes and subcomplexes of mitochondrial oxidative phosphorylation. Biochim Biophys Acta. 2006;1757:1066–1072. doi: 10.1016/j.bbabio.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 78.Acin-Perez R, Fernandez-Silva P, Peleato ML, Perez-Martos A, Enriquez JA. Respiratory active mitochondrial supercomplexes. Mol Cell. 2008;32:529–539. doi: 10.1016/j.molcel.2008.10.021. [DOI] [PubMed] [Google Scholar]
- 79.Schafer E, Dencher NA, Vonck J, Parcej DN. Three-dimensional structure of the respiratory chain supercomplex I1III2IV1 from bovine heart mitochondria. Biochemistry. 2007;46:12579–12585. doi: 10.1021/bi700983h. [DOI] [PubMed] [Google Scholar]
- 80.Vonck J, Schafer E. Supramolecular organization of protein complexes in the mitochondrial inner membrane. Biochim Biophys Acta. 2009;1793:117–124. doi: 10.1016/j.bbamcr.2008.05.019. [DOI] [PubMed] [Google Scholar]
- 81.Fry M, Green DE. Cardiolipin requirement by cytochrome oxidase and the catalytic role of phospholipid. Biochem Biophys Res Commun. 1980;93:1238–1246. doi: 10.1016/0006-291x(80)90622-1. [DOI] [PubMed] [Google Scholar]
- 82.Hoch FL. Cardiolipins and biomembrane function. Biochim Biophys Acta. 1992;1113:71–133. doi: 10.1016/0304-4157(92)90035-9. [DOI] [PubMed] [Google Scholar]
- 83.Hoch FL. Cardiolipins and mitochondrial proton-selective leakage. J Bioenerg Biomembr. 1998;30:511–532. doi: 10.1023/a:1020576315771. [DOI] [PubMed] [Google Scholar]
- 84.Nalecz KA, Bolli R, Wojtczak L, Azzi A. The monocarboxylate carrier from bovine heart mitochondria: partial purification and its substrate-transporting properties in a reconstituted system. Biochim Biophys Acta. 1986;851:29–37. doi: 10.1016/0005-2728(86)90245-8. [DOI] [PubMed] [Google Scholar]
- 85.Paradies G, Petrosillo G, Ruggiero FM. Cardiolipin-dependent decrease of cytochrome c oxidase activity in heart mitochondria from hypothyroid rats. Biochim Biophys Acta. 1997;1319:5–8. doi: 10.1016/s0005-2728(97)00012-1. [DOI] [PubMed] [Google Scholar]
- 86.Zhang M, Mileykovskaya E, Dowhan W. Gluing the respiratory chain together. Cardiolipin is required for supercomplex formation in the inner mitochondrial membrane. J Biol Chem. 2002;277:43553–43556. doi: 10.1074/jbc.C200551200. [DOI] [PubMed] [Google Scholar]
- 87.Brandner K, Mick DU, Frazier AE, Taylor RD, Meisinger C, Rehling P. Taz1, an outer mitochondrial membrane protein, affects stability and assembly of inner membrane protein complexes: implications for Barth Syndrome. Mol Biol Cell. 2005;16:5202–5214. doi: 10.1091/mbc.E05-03-0256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Pfeiffer K, Gohil V, Stuart RA, Hunte C, Brandt U, Greenberg ML, et al. Cardiolipin stabilizes respiratory chain supercomplexes. J Biol Chem. 2003;278:52873–52880. doi: 10.1074/jbc.M308366200. [DOI] [PubMed] [Google Scholar]
- 89.McKenzie M, Lazarou M, Thorburn DR, Ryan MT. Mitochondrial respiratory chain supercomplexes are destabilized in Barth Syndrome patients. J Mol Biol. 2006;361:462–469. doi: 10.1016/j.jmb.2006.06.057. [DOI] [PubMed] [Google Scholar]
- 90.Scacco S, Vergari R, Scarpulla RC, Technikova-Dobrova Z, Sardanelli A, Lambo R, et al. cAMP-dependent phosphorylation of the nuclear encoded 18-kDa (IP) subunit of respiratory complex I and activation of the complex in serum-starved mouse fibroblast cultures. J Biol Chem. 2000;275:17578–17582. doi: 10.1074/jbc.M001174200. [DOI] [PubMed] [Google Scholar]
- 91.Pagliarini DJ, Dixon JE. Mitochondrial modulation: reversible phosphorylation takes center stage? Trends Biochem Sci. 2006;31:26–34. doi: 10.1016/j.tibs.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 92.Zippin JH, Chen Y, Nahirney P, Kamenetsky M, Wuttke MS, Fischman DA, et al. Compartmentalization of bicarbonate-sensitive adenylyl cyclase in distinct signaling microdomains. FASEB J. 2003;17:82–84. doi: 10.1096/fj.02-0598fje. [DOI] [PubMed] [Google Scholar]
- 93.DiPilato LM, Cheng X, Zhang J. Fluorescent indicators of cAMP and Epac activation reveal differential dynamics of cAMP signaling within discrete subcellular compartments. Proc Natl Acad Sci USA. 2004;101:16513–16518. doi: 10.1073/pnas.0405973101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Acin-Perez R, Salazar E, Kamenetsky M, Buck J, Levin LR, Manfredi G. Cyclic AMP produced inside mitochondria regulates oxidative phosphorylation. Cell Metab. 2009;9:265–276. doi: 10.1016/j.cmet.2009.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Schwoch G, Trinczek B, Bode C. Localization of catalytic and regulatory subunits of cyclic AMP-dependent protein kinases in mitochondria from various rat tissues. Biochem J. 1990;270:181–188. doi: 10.1042/bj2700181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Technikova-Dobrova Z, Sardanelli AM, Papa S. Phosphorylation of mitochondrial proteins in bovine heart. Characterization of kinases and substrates. FEBS Lett. 1993;322:51–55. doi: 10.1016/0014-5793(93)81109-d. [DOI] [PubMed] [Google Scholar]
- 97.Technikova-Dobrova Z, Sardanelli AM, Stanca MR, Papa S. cAMP-dependent protein phosphorylation in mitochondria of bovine heart. FEBS Lett. 1994;350:187–191. doi: 10.1016/0014-5793(94)00760-8. [DOI] [PubMed] [Google Scholar]
- 98.Sardanelli AM, Technikova-Dobrova Z, Scacco SC, Speranza F, Papa S. Characterization of proteins phosphorylated by the cAMP-dependent protein kinase of bovine heart mitochondria. FEBS Lett. 1995;377:470–474. doi: 10.1016/0014-5793(95)01407-1. doi:10.1016/0014-5793(95)01407-1. [DOI] [PubMed] [Google Scholar]
- 99.Papa S, Sardanelli AM, Cocco T, Speranza F, Scacco SC, Technikova-Dobrova Z. The nuclear-encoded 18 kDa (IP) AQDQ subunit of bovine heart complex I is phosphorylated by the mitochondrial cAMP-dependent protein kinase. FEBS Lett. 1996;379:299–301. doi: 10.1016/0014-5793(95)01532-9. [DOI] [PubMed] [Google Scholar]
- 100.Sardanelli AM, Technikova-Dobrova Z, Speranza F, Mazzocca A, Scacco S, Papa S. Topology of the mitochondrial cAMP-dependent protein kinase and its substrates. FEBS Lett. 1996;396:276–278. doi: 10.1016/0014-5793(96)01112-x. [DOI] [PubMed] [Google Scholar]
- 101.Chen Q, Lin RY, Rubin CS. Organelle-specific targeting of protein kinase AII (PKAII). Molecular and in situ characterization of murine A kinase anchor proteins that recruit regulatory subunits of PKAII to the cytoplasmic surface of mitochondria. J Biol Chem. 1997;272:15247–15257. doi: 10.1074/jbc.272.24.15247. [DOI] [PubMed] [Google Scholar]
- 102.Affaitati A, Cardone L, de Cristofaro T, Carlucci A, Ginsberg MD, Varrone S, et al. Essential role of A-kinase anchor protein 121 for cAMP signaling to mitochondria. J Biol Chem. 2003;278:4286–4294. doi: 10.1074/jbc.M209941200. [DOI] [PubMed] [Google Scholar]
- 103.Cardone L, de Cristofaro T, Affaitati A, Garbi C, Ginsberg MD, Saviano M, et al. A-kinase anchor protein 84/121 are targeted to mitochondria and mitotic spindles by overlapping amino-terminal motifs. J Mol Biol. 2002;320:663–675. doi: 10.1016/s0022-2836(02)00479-5. [DOI] [PubMed] [Google Scholar]
- 104.Signorile A, Sardanelli AM, Nuzzi R, Papa S. Serine (threonine) phosphatase(s) acting on cAMP-dependent phosphoproteins in mammalian mitochondria. FEBS Lett. 2002;512:91–94. doi: 10.1016/s0014-5793(02)02226-3. [DOI] [PubMed] [Google Scholar]
- 105.Pagliarini DJ, Wiley SE, Kimple ME, Dixon JR, Kelly P, Worby CA, et al. Involvement of a mitochondrial phosphatase in the regulation of ATP production and insulin secretion in pancreatic beta cells. Mol Cell. 2005;19:197–207. doi: 10.1016/j.molcel.2005.06.008. [DOI] [PubMed] [Google Scholar]
- 106.Schulenberg B, Aggeler R, Beechem JM, Capaldi RA, Patton WF. Analysis of steady-state protein phosphorylation in mitochondria using a novel fluorescent phosphosensor dye. J Biol Chem. 2003;278:27251–27255. doi: 10.1074/jbc.C300189200. [DOI] [PubMed] [Google Scholar]
- 107.Chen R, Fearnley IM, Peak-Chew SY, Walker JE. The phosphorylation of subunits of complex I from bovine heart mitochondria. J Biol Chem. 2004;279:26036–26045. doi: 10.1074/jbc.M402710200. [DOI] [PubMed] [Google Scholar]
- 108.Bender E, Kadenbach B. The allosteric ATP-inhibition of cytochrome c oxidase activity is reversibly switched on by cAMP-dependent phosphorylation. FEBS Lett. 2000;466:130–134. doi: 10.1016/s0014-5793(99)01773-1. [DOI] [PubMed] [Google Scholar]
- 109.Lee I, Bender E, Arnold S, Kadenbach B. New control of mitochondrial membrane potential and ROS formation—a hypothesis. Biol Chem. 2001;382:1629–1636. doi: 10.1515/BC.2001.198. [DOI] [PubMed] [Google Scholar]
- 110.Lee I, Bender E, Kadenbach B. Control of mitochondrial membrane potential and ROS formation by reversible phosphorylation of cytochrome c oxidase. Mol Cell Biochem. 2002;234–235:63–70. [PubMed] [Google Scholar]
- 111.Ludwig B, Bender E, Arnold S, Huttemann M, Lee I, Kadenbach B. Cytochrome C oxidase and the regulation of oxidative phosphorylation. Chembiochem. 2001;2:392–403. doi: 10.1002/1439-7633(20010601)2:6<392::AID-CBIC392>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 112.Korshunov SS, Skulachev VP, Starkov AA. High protonic potential actuates a mechanism of production of reactive oxygen species in mitochondria. FEBS Lett. 1997;416:15–18. doi: 10.1016/s0014-5793(97)01159-9. [DOI] [PubMed] [Google Scholar]
- 113.Lee I, Salomon AR, Ficarro S, Mathes I, Lottspeich F, Grossman LI, et al. cAMP-dependent tyrosine phosphorylation of subunit I inhibits cytochrome c oxidase activity. J Biol Chem. 2005;280:6094–6100. doi: 10.1074/jbc.M411335200. [DOI] [PubMed] [Google Scholar]
- 114.Samavati L, Lee I, Mathes I, Lottspeich F, Huttemann M. Tumor necrosis factor alpha inhibits oxidative phosphorylation through tyrosine phosphorylation at subunit I of cytochrome c oxidase. J Biol Chem. 2008;283:21134–21144. doi: 10.1074/jbc.M801954200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Fang JK, Prabu SK, Sepuri NB, Raza H, Anandatheerthavarada HK, Galati D, et al. Site specific phosphorylation of cytochrome c oxidase subunits I, IVi1 and Vb in rabbit hearts subjected to ischemia/reperfusion. FEBS Lett. 2007;581:1302–1310. doi: 10.1016/j.febslet.2007.02.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Prabu SK, Anandatheerthavarada HK, Raza H, Srinivasan S, Spear JF, Avadhani NG. Protein kinase A-mediated phosphorylation modulates cytochrome c oxidase function and augments hypoxia and myocardial ischemia-related injury. J Biol Chem. 2006;281:2061–2070. doi: 10.1074/jbc.M507741200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Acin-Perez R, Salazar E, Brosel S, Yang H, Schon EA, Manfredi G. Modulation of mitochondrial protein phosphorylation by soluble adenylyl cyclase ameliorates cytochrome oxidase defects. EMBO Mol Med. 2009;1:392–406. doi: 10.1002/emmm.200900046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Rizzuto R, Pinton P, Carrington W, Fay FS, Fogarty KE, Lifshitz LM, et al. Close contacts with the endoplasmic reticulum as determinants of mitochondrial Ca2 + responses. Science. 1998;280:1763–1766. doi: 10.1126/science.280.5370.1763. [DOI] [PubMed] [Google Scholar]
- 119.Rizzuto R, Bastianutto C, Brini M, Murgia M, Pozzan T. Mitochondrial Ca2 + homeostasis in intact cells. J Cell Biol. 1994;126:1183–1194. doi: 10.1083/jcb.126.5.1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Hajnoczky G, Robb-Gaspers LD, Seitz MB, Thomas AP. Decoding of cytosolic calcium oscillations in the mitochondria. Cell. 1995;82:415–424. doi: 10.1016/0092-8674(95)90430-1. [DOI] [PubMed] [Google Scholar]
- 121.Rohacs T, Nagy G, Spat A. Cytoplasmic Ca2 + signalling and reduction of mitochondrial pyridine nucleotides in adrenal glomerulosa cells in response to K + , angiotensin II and vasopressin. Biochem J. 1997;322:785–792. doi: 10.1042/bj3220785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Maechler P, Kennedy ED, Pozzan T, Wollheim CB. Mitochondrial activation directly triggers the exocytosis of insulin in permeabilized pancreatic beta-cells. EMBO J. 1997;16:3833–3841. doi: 10.1093/emboj/16.13.3833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Jouaville LS, Pinton P, Bastianutto C, Rutter GA, Rizzuto R. Regulation of mitochondrial ATP synthesis by calcium: evidence for a long-term metabolic priming. Proc Natl Acad Sci USA. 1999;96:13807–13812. doi: 10.1073/pnas.96.24.13807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Nowak G. Protein kinase C-alpha and ERK1/2 mediate mitochondrial dysfunction, decreases in active Na + transport, and cisplatin-induced apoptosis in renal cells. J Biol Chem. 2002;277:43377–43388. doi: 10.1074/jbc.M206373200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Liu X, Godwin ML, Nowak G. Protein kinase C-alpha inhibits the repair of oxidative phosphorylation after S-(1,2-dichlorovinyl)-L-cysteine injury in renal cells. Am J Physiol Renal Physiol. 2004;287:F64–F73. doi: 10.1152/ajprenal.00216.2003. [DOI] [PubMed] [Google Scholar]
- 126.Ogbi M, Chew CS, Pohl J, Stuchlik O, Ogbi S, Johnson JA. Cytochrome c oxidase subunit IV as a marker of protein kinase Cepsilon function in neonatal cardiac myocytes: implications for cytochrome c oxidase activity. Biochem J. 2004;382:923–932. doi: 10.1042/BJ20040468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Sayen MR, Gustafsson AB, Sussman MA, Molkentin JD, Gottlieb RA. Calcineurin transgenic mice have mitochondrial dysfunction and elevated superoxide production. Am J Physiol Cell Physiol. 2003;284:C562–C570. doi: 10.1152/ajpcell.00336.2002. [DOI] [PubMed] [Google Scholar]
- 128.Rosca MG, Hoppel CL. New aspects of impaired mitochondrial function in heart failure. J Bioenerg Biomembr. 2009;41:107–112. doi: 10.1007/s10863-009-9215-9. [DOI] [PubMed] [Google Scholar]
- 129.Jarreta D, Orus J, Barrientos A, Miro O, Roig E, Heras M, et al. Mitochondrial function in heart muscle from patients with idiopathic dilated cardiomyopathy. Cardiovasc Res. 2000;45:860–865. doi: 10.1016/s0008-6363(99)00388-0. [DOI] [PubMed] [Google Scholar]
- 130.Puchowicz MA, Varnes ME, Cohen BH, Friedman NR, Kerr DS, Hoppel CL. Oxidative phosphorylation analysis: assessing the integrated functional activity of human skeletal muscle mitochondria—case studies. Mitochondrion. 2004;4:377–385. doi: 10.1016/j.mito.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 131.Faustin B, Rossignol R, Rocher C, Benard G, Malgat M, Letellier T. Mobilization of adenine nucleotide translocators as molecular bases of the biochemical threshold effect observed in mitochondrial diseases. J Biol Chem. 2004;279:20411–20421. doi: 10.1074/jbc.M314259200. [DOI] [PubMed] [Google Scholar]
- 132.Rossignol R, Malgat M, Mazat JP, Letellier T. Threshold effect and tissue specificity. Implication for mitochondrial cytopathies. J Biol Chem. 1999;274:33426–33432. doi: 10.1074/jbc.274.47.33426. [DOI] [PubMed] [Google Scholar]
- 133.Groen AK, Wanders RJ, Westerhoff HV, van der Meer R, Tager JM. Quantification of the contribution of various steps to the control of mitochondrial respiration. J Biol Chem. 1982;257:2754–2757. [PubMed] [Google Scholar]
- 134.Gellerich FN, Bohnensack R, Kunz W. Control of mitochondrial respiration. The contribution of the adenine nucleotide translocator depends on the ATP- and ADP-consuming enzymes. Biochim Biophys Acta. 1983;722:381–391. doi: 10.1016/0005-2728(83)90086-5. [DOI] [PubMed] [Google Scholar]
- 135.Villani G, Attardi G. In vivo control of respiration by cytochrome c oxidase in human cells. Free Radic Biol Med. 2000;29:202–210. doi: 10.1016/s0891-5849(00)00303-8. [DOI] [PubMed] [Google Scholar]
- 136.Kadenbach B, Huttemann M, Arnold S, Lee I, Bender E. Mitochondrial energy metabolism is regulated via nuclear-coded subunits of cytochrome c oxidase. Free Radic Biol Med. 2000;29:211–221. doi: 10.1016/s0891-5849(00)00305-1. [DOI] [PubMed] [Google Scholar]
- 137.Sanbe A, Tanonaka K, Niwano Y, Takeo S. Improvement of cardiac function and myocardial energy metabolism of rats with chronic heart failure by long-term coenzyme Q10 treatment. J Pharmacol Exp Ther. 1994;269:51–56. [PubMed] [Google Scholar]
- 138.Sharov VG, Todor AV, Silverman N, Goldstein S, Sabbah HN. Abnormal mitochondrial respiration in failed human myocardium. J Mol Cell Cardiol. 2000;32:2361–2367. doi: 10.1006/jmcc.2000.1266. [DOI] [PubMed] [Google Scholar]
- 139.Sanbe A, Tanonaka K, Hanaoka Y, Katoh T, Takeo S. Regional energy metabolism of failing hearts following myocardial infarction. J Mol Cell Cardiol. 1993;25:995–1013. doi: 10.1006/jmcc.1993.1113. [DOI] [PubMed] [Google Scholar]
- 140.Gong G, Liu J, Liang P, Guo T, Hu Q, Ochiai K, et al. Oxidative capacity in failing hearts. Am J Physiol. 2003;285:H541–H548. doi: 10.1152/ajpheart.01142.2002. [DOI] [PubMed] [Google Scholar]
- 141.Sordahl LA, McCollum WB, Wood WG, Schwartz A. Mitochondria and sarcoplasmic reticulum function in cardiac hypertrophy and failure. Am J Physiol. 1973;224:497–502. doi: 10.1152/ajplegacy.1973.224.3.497. [DOI] [PubMed] [Google Scholar]
- 142.Lindenmayer GE, Harigaya S, Bajusz E, Schwartz A. Oxidative phosphorylation and calcium transport of mitochondria isolated from cardiomyopathic hamster hearts. J Mol Cell Cardiol. 1970;1:249–259. doi: 10.1016/0022-2828(70)90005-2. [DOI] [PubMed] [Google Scholar]
- 143.Wrogemann K, Blanchaer MC, Jacobson BE. Oxidative phosphorylation in cardiomyopathic hamsters. Am J Physiol. 1972;222:1453–1457. doi: 10.1152/ajplegacy.1972.222.6.1453. [DOI] [PubMed] [Google Scholar]
- 144.Lindenmayer GE, Sordahl LA, Schwartz A. Reevaluation of oxidative phosphorylation in cardiac mitochondria from normal animals and animals in heart failure. Circ Res. 1968;23:439–450. doi: 10.1161/01.res.23.3.439. [DOI] [PubMed] [Google Scholar]
- 145.Potluri P, Yadava N, Scheffler IE. The role of the ESSS protein in the assembly of a functional and stable mammalian mitochondrial complex I (NADH-ubiquinone oxidoreductase) Eur J Biochem. 2004;271:3265–3273. doi: 10.1111/j.1432-1033.2004.04260.x. [DOI] [PubMed] [Google Scholar]
- 146.Au HC, Seo BB, Matsuno-Yagi A, Yagi T, Scheffler IE. The NDUFA1 gene product (MWFE protein) is essential for activity of complex I in mammalian mitochondria. Proc Natl Acad Sci USA. 1999;96:4354–4359. doi: 10.1073/pnas.96.8.4354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Raha S, Myint AT, Johnstone L, Robinson BH. Control of oxygen free radical formation from mitochondrial complex I: roles for protein kinase A and pyruvate dehydrogenase kinase. Free Radic Biol Med. 2002;32:421–430. doi: 10.1016/s0891-5849(01)00816-4. [DOI] [PubMed] [Google Scholar]
- 148.Sazanov LA, Peak-Chew SY, Fearnley IM, Walker JE. Resolution of the membrane domain of bovine complex I into subcomplexes: implications for the structural organization of the enzyme. Biochemistry. 2000;39:7229–7235. doi: 10.1021/bi000335t. [DOI] [PubMed] [Google Scholar]
- 149.Yamaguchi M, Belogrudov GI, Matsuno-Yagi A, Hatefi Y. The multiple nicotinamide nucleotide-binding subunits of bovine heart mitochondrial NADH:ubiquinone oxidoreductase (complex I) Eur J Biochem. 2000;267:329–336. doi: 10.1046/j.1432-1327.2000.00999.x. [DOI] [PubMed] [Google Scholar]
- 150.Schilling B, Aggeler R, Schulenberg B, Murray J, Row RH, Capaldi RA, et al. Mass spectrometric identification of a novel phosphorylation site in subunit NDUFA10 of bovine mitochondrial complex I. FEBS Lett. 2005;579:2485–2490. doi: 10.1016/j.febslet.2005.03.061. [DOI] [PubMed] [Google Scholar]
- 151.Tomitsuka E, Kita K, Esumi H. Regulation of succinate-ubiquinone reductase and fumarate reductase activities in human complex II by phosphorylation of its flavoprotein subunit. Proc Jpn Acad. 2009;85:258–265. doi: 10.2183/pjab.85.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Ficarro S, Chertihin O, Westbrook VA, White F, Jayes F, Kalab P, et al. Phosphoproteome analysis of capacitated human sperm. Evidence of tyrosine phosphorylation of a kinase-anchoring protein 3 and valosin-containing protein/p97 during capacitation. J Biol Chem. 2003;278:11579–11589. doi: 10.1074/jbc.M202325200. [DOI] [PubMed] [Google Scholar]
- 153.Reinders J, Wagner K, Zahedi RP, Stojanovski D, Eyrich B, van der Laan M, et al. Profiling phosphoproteins of yeast mitochondria reveals a role of phosphorylation in assembly of the ATP synthase. Mol Cell Proteomics. 2007;6:1896–1906. doi: 10.1074/mcp.M700098-MCP200. [DOI] [PubMed] [Google Scholar]
- 154.Lee I, Salomon AR, Yu K, Doan JW, Grossman LI, Huttemann M. New prospects for an old enzyme: mammalian cytochrome c is tyrosine-phosphorylated in vivo. Biochemistry. 2006;45:9121–9128. doi: 10.1021/bi060585v. [DOI] [PubMed] [Google Scholar]
- 155.Yu H, Lee I, Salomon AR, Yu K, Huttemann M. Mammalian liver cytochrome c is tyrosine-48 phosphorylated in vivo, inhibiting mitochondrial respiration. Biochim Biophys Acta. 2008;1777:1066–1071. doi: 10.1016/j.bbabio.2008.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Helling S, Vogt S, Rhiel A, Ramzan R, Wen L, Marcus K, et al. Phosphorylation and kinetics of mammalian cytochrome c oxidase. Mol Cell Proteomics. 2008;7:1714–1724. doi: 10.1074/mcp.M800137-MCP200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Miyazaki T, Neff L, Tanaka S, Horne WC, Baron R. Regulation of cytochrome c oxidase activity by c-Src in osteoclasts. J Cell Biol. 2003;160:709–718. doi: 10.1083/jcb.200209098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Demory ML, Boerner JL, Davidson R, Faust W, Miyake T, Lee I, et al. Epidermal growth factor receptor translocation to the mitochondria: regulation and effect. J Biol Chem. 2009;284:36592–36604. doi: 10.1074/jbc.M109.000760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Steenaart NA, Shore GC. Mitochondrial cytochrome c oxidase subunit IV is phosphorylated by an endogenous kinase. FEBS Lett. 1997;415:294–298. doi: 10.1016/s0014-5793(97)01145-9. [DOI] [PubMed] [Google Scholar]
- 160.Bykova NV, Egsgaard H, Moller IM. Identification of 14 new phosphoproteins involved in important plant mitochondrial processes. FEBS Lett. 2003;540:141–146. doi: 10.1016/s0014-5793(03)00250-3. [DOI] [PubMed] [Google Scholar]
- 161.Hojlund K, Wrzesinski K, Larsen PM, Fey SJ, Roepstorff P, Handberg A, et al. Proteome analysis reveals phosphorylation of ATP synthase beta -subunit in human skeletal muscle and proteins with potential roles in type 2 diabetes. J Biol Chem. 2003;278:10436–10442. doi: 10.1074/jbc.M212881200. [DOI] [PubMed] [Google Scholar]
- 162.Feng J, Lucchinetti E, Enkavi G, Wang Y, Gehrig P, Roschitzki B, et al. Tyrosine phosphorylation by Src within the cavity of the adenine nucleotide translocase 1 regulates ADP/ATP exchange in mitochondria. Am J Physiol Cell Physiol. 2010;298:C740–C748. doi: 10.1152/ajpcell.00310.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]