Abstract
Mouse mammary tumor virus (MMTV), which was discovered as a milk-transmitted, infectious cancer-inducing agent in the 1930s, has been used since that time as an animal model for the study of human breast cancer. Like other complex retroviruses, MMTV encodes a number of accessory proteins that both facilitate infection and affect host immune response. In vivo, the virus predominantly infects lymphocytes and mammary epithelial cells. High level infection of mammary epithelial cells ensures efficient passage of virus to the next generation. It also results in mammary tumor induction, since the MMTV provirus integrates into the mammary epithelial cell genome during viral replication and activates cellular oncogene expression. Thus, mammary tumor induction is a by-product of the infection cycle. A number of important oncogenes have been discovered by carrying out MMTV integration site analysis, some of which may play a role in human breast cancer.
Keywords: milk-borne virus, superantigen, intrinsic immunity, CIS, breast cancer
1. Introduction
Non-acute transforming retroviruses, which cause dysregulated expression of cellular oncogenes upon integration of the provirus into the host genome, have long been used to study both tumor development and progression in animal models [1]. Indeed, many oncogenes were originally identified because of their association with tumors caused by this type of retrovirus. Although the majority of non-acute transforming retroviruses induce cancer in cells of hematopoietic origin, one exception is the murine betaretrovirus MMTV, which causes mammary epithelial cell tumors. MMTV was first characterized in the 1930s as a milk-transmitted agent associated with mammary tumors in mice [2] and thus has long been used as an in vivo model for the study of human breast cancer [3]. Here, I briefly review MMTV molecular biology, its in vivo infection pathway, and what has been learned about how this virus causes mammary tumors.
2. MMTV genome and proteins
MMTV was originally classified as a simple retrovirus. The genomes of simple retroviruses encode the virion capsid/nucleocapsid (Gag) proteins, the enzymes needed for genome replication (reverse transcriptase and integrase; Pol/In) and the envelope proteins (Env) that bind the cell surface molecule(s) used for virus entry [1]. In contrast, the genomes of complex retroviruses, such as lentiviruses and deltaviruses, encode non-structural proteins that facilitate virus replication or that counteract intrinsic, innate or adaptive immune responses during in vivo infection. Because the MMTV genome encodes at least three known accessory proteins that carry out these functions, it is now considered a complex retrovirus.
The MMTV is 9 kb in length and like all retroviruses, is flanked by 5′ and 3′ long terminal repeats (LTRs), which in the case of MMTV are exceptionally long (approximately 1.3 kb). This is because the MMTV 3′ LTR encodes one of the viral accessory proteins, termed the superantigen (Sag) (Figure 1). In addition to the Sag coding region, there are a number of transcription factor binding sites in the LTR that determine tissue-specific, as well as glucocorticoid/progesterone-regulated virus expression [4–6]. Because they direct high level, hormone regulated expression in mammary epithelial cells, the MMTV LTRs have been extensively used to drive oncogene expression in transgenic mice as a means of creating mouse models of breast cancer [3]. Similarly, mammary gland-specific deletion of tumor suppressor genes using MMTV LTR-cre recombinase transgenic mice has resulted in additional breast cancer models [7].
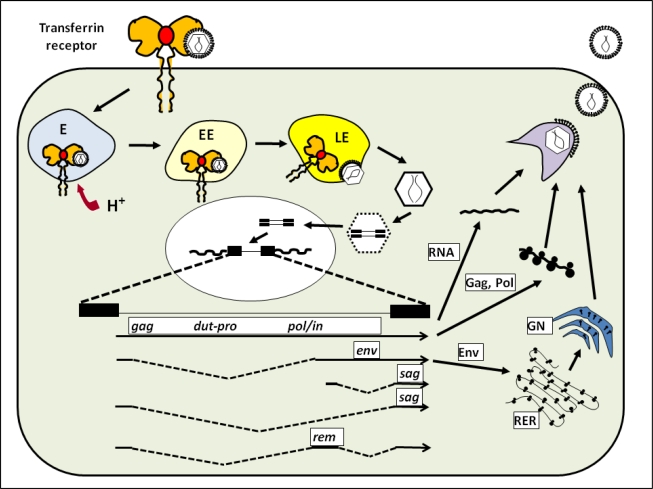
Figure 1.
MMTV infection. MMTV binds to TfR1 on the cell surface and is internalized into a low pH compartment. After uncoating, the viral genome is reverse-transcribed, is transported to the nucleus, and the provirus integrates into the genome. At least five different RNAs are transcribed from the integrated provirus (see text). The Env membrane proteins are synthesis in the rough endoplasmic reticulum (RER) and traffic through the Golgi network (GN). Little is known about MMTV virion assembly, although it occurs in an intra-cellular compartment. Abbreviations: E, endosome; EE, early endosome; LE, late endosome.
MMTV also infects lymphocytes in vivo (see next section) and the MMTV LTRs contain regulatory elements that control expression in B and T cells [8,9]. Thus, MMTV-oncogene transgenic mice frequently develop lymphoid as well as mammary cell tumors (for example, see [10]). Although MMTV infects and is expressed in lymphocytes, the virus usually only causes mammary tumors. However, there are MMTV variants with deletions/insertions in the LTRs that are causally associated with T cell lymphomas; the sequence alterations in the LTR are believed to result in the generation of transcriptional enhancers that activate linked cellular oncogene expression in these cells [11,12].
At least five transcripts are generated from the MMTV genome. A full-length, unspliced RNA that initiates in the 5′ LTR and terminates in the 3′ LTR serves as the viral genome and is packaged into virions [1]. This transcript also functions as the mRNA for the Gag and Pol proteins, as well as a dUTPase (Dut) and other proteins of unknown function (Figure 1). The role of the dUTPase in MMTV infection is not known, but the Dut of the lentivirus equine infectious anemia virus (EIAV) is thought to facilitate replication of EIAV in non-dividing cells by maintaining adequate nucleotide pools [13].
The Env protein, which mediates retroviral entry into cells by binding specific cell surface molecules, is encoded by a singly spliced mRNA (Figure 1). As with other retroviruses, the MMTV Env consists of two chains, generated by cellular furin processing of a 73 kD polyprotein precursor to a 52 kD cell surface (SU) protein, which binds the entry receptor, and a 36 kD transmembrane (TM) domain that is responsible for membrane fusion. MMTV uses transferrin receptor 1 (TfR1) for entry [14]. TfR1, the major means by which cells take up iron [15], traffics to the acidic endosome upon ligand (iron-bound transferrin) binding. MMTV entry requires low pH (<5.2) and thus, most likely co-traffics with TfR1 to a late endosomal compartment after binding at the cell surface [14,16] (Figure 1). TfR1 is highly expressed on activated lymphocytes and dividing mammary epithelial cells in vivo, which probably limits MMTV infection to these cell types [17–19]. Additionally, as described above, the transcriptional regulatory elements in the MMTV LTR function predominantly in mammary epithelia and lymphoid cells, thus further restricting infection and spread to other tissues in vivo.
At least two additional accessory genes, Sag and Rem, are encoded by other alternatively spliced mRNAs (Figure 1). The Sag protein is translated from two different transcripts (Figure 1). The first transcript initiates in the 5′ LTR and uses the same splice donor as the env mRNA. The second transcript uses a promoter and splice donor in env. Both transcripts use a splice acceptor just upstream of the open reading frame in the 3′ LTR [20–22]. The regulator of export of MMTV (Rem) protein is encoded by a double spliced mRNA [23,24]. Like the human immunodeficiency virus (HIV) Rev protein, Rem is required for efficient transport of unspliced viral RNA from the nucleus through interaction with a Rem-responsive element present in the MMTV RNA [25,26].
As is the case for other betaretroviruses, MMTV virion assembly occurs in an intracellular compartment and virions are then exported to the plasma membrane for egress from the cell [27]. However, little is known about either the viral or cellular requirements for MMTV assembly. In vivo, virus is shed from the apical surface of polarized mammary epithelial cells into the lumen of the end buds, along with the milk proteins and thus is transmitted to offspring [28].
3. MMTV in vivo infection
MMTV is transmitted from infected mothers to pups through nursing, most likely as cell-free virus which is present at very high levels in milk [29]. Susceptible strains that acquire exogenous MMTV through milk can be freed of the virus by foster-nursing on uninfected mothers. Viruses isolated from mice that shed milk-borne MMTV infect and cause tumors in different strains of mice to varying degrees [30]. This differential susceptibility to MMTV infection is due in large part to intrinsic, innate and adaptive immune responses to the virus that vary between mouse strains (see below). In addition to the exogenous form of MMTV, all commonly used inbred mice as well as many wild mice inherit endogenous copies of MMTV which are thought to have entered the mouse genome between 10–20 million years ago [31]. The vast majority of endogenous MMTVs do not produce infectious virus due to deletions or mutations in the proviral genome. At least 10 different exogenous and greater than 30 endogenous MMTVs have been identified (for example, see [32–35]).
With the exception of the virions found in milk, exogenous MMTV in infected mice is cell-associated [36] and infection of lymphocytes is critical for virus spread from the gut to the mammary tissue (reviewed in [37]). In brief, MMTV acquired through milk first infects dendritic cells (DCs) then spreads to T and B cells in the Peyer’s patches of the gut and ultimately to other lymph nodes and lymphoid organs. This spread is largely due to the viral Sag protein, which is presented to the T cell (TCR) on CD4+ T cells by major histocompatibility (MHC) class II proteins expressed on the surface of infected antigen presenting cells, such as DCs and B cells. The Sag-activated T cells proliferate, provide B cell help and produce cytokines that stimulate and recruit additional DCs, B and T cells, resulting in the establishment of a reservoir of infection-competent and infected lymphocytes. The mammary gland is considered mucosal-associated lymphoid tissue (MALT) and represents a site of normal lymphocyte trafficking. MMTV-infected lymphocytes are therefore not only an important reservoir for amplification of the virus in vivo, but also carry virus to the mammary gland [38,39].
MMTV infects mammary epithelial cells at a time when they are driven to divide, that is, during the cell division that accompanies both puberty and pregnancy. Mice that go through multiple rounds of pregnancy have much higher levels of MMTV infection in mammary tissue [36]. It is believed this is due to the increased susceptibility of dividing mammary epithelial cells to infection by lymphocyte-produced virus and not to horizontal spread of the virus between mammary cells [38]. Transcription of viral RNA and production of virus is highest during late lactation and pregnancy, thereby maximizing virion production in milk.
Different exogenous and endogenous MMTVs encode Sag proteins with different TCR specificity. Sags encoded by endogenous MMTVs cause the deletion of cognate T cells during shaping of the immune repertoire, while those encoded by exogenous virus produce a slower but none-the-less almost complete deletion of such lymphocytes [40]. This results in mice that are immune to infection by exogenous MMTVs with the same Sags because they lack responding T cells [41]. MMTV Sag-induced T cell deletion may also make some mouse strains more resistant to the pathogenic effects of Leishmania major because of loss of T cell responses [42]. Interestingly, while most of the endogenous MMTVs sustain mutations in the coding regions for the virion proteins, almost all retain intact Sag coding regions, suggesting that the anti-viral and -parasite protection might confer a selective advantage to mice that retain endogenous MMTVs.
There are other host genes that confer resistance or susceptibility to MMTV. These include MHC Class II genes required for efficient Sag presentation, the innate immune pathogen sensor toll-like receptor 4 (Tlr4), and several as-of-yet unidentified genes that affect the production of anti-MMTV antibodies or T cell responses to MMTV (reviewed in [43]). MMTV infection is also restricted by the intrinsic immune factor, apolipoprotein B editing complex 3 (APOBEC3) [44]. Different inbred mouse strains have polymorphisms in Apobec3 [45], which affect the ability of this factor to inhibit MMTV infection [46]. All of the host genes that affect MMTV lymphocyte infection also alter the incidence and kinetics of mammary tumor induction. Interestingly, host genes that affect mammary tumorigenesis do so by limiting virus infection; none have been shown to have a direct effect on the ability of the virus to transform mammary epithelial cells.
4. MMTV and Mammary Tumorigenesis
MMTV-induced mammary tumorigenesis is mediated by proviral integration, usually by enhancer -mediated activation of nearby cellular oncogenes, although a few examples of coding region insertions that alter the gene product have also been described [47]. Additionally, the MMTV Env protein has been implicated in mammary tumorigenesis. The MMTV Env has an immuno-tyrosine based activation motif (ITAM) commonly found in receptors expressed in hematopoietic cells; expression of the Env protein in normal mouse or human mammary epithelial cells induces morphological transformation in culture [48]. Moreover, when the ITAM motif was mutated in the virus, mammary tumor-induction was attenuated in infected mice [49].
In vivo infection levels usually affect mammary tumor incidence and kinetics because of an increased number of proviral integrations. A number of different common integration sites (CIS) have been implicated in MMTV-induced mammary tumors (Table 1), particularly the Wnt and Fgf genes [47]. MMTV-induced tumors appear to develop from infection of a single stem cell [50]. Mammary stem cells have the potential to form two epithelial lineages in the mammary gland, myoepithelial cells found on the outside of ducts, and ductal and alveolar luminal cells. MMTV-induced tumors proceed through at least two stages, the pregnancy-dependent hyperplastic alveolar nodule (HAN), followed by the hormone-independent mammary tumor [51]. Although the histopathological features of MMTV-induced tumors do not usually resemble the most frequent forms of human breast tumors such as invasive ductal carcinomas, many, if not all, of the human mammary lesions are thought to originate in the terminal ductal lobular unit and atypical lobular type A lesions (ALA) are morphologically similar to the mouse mammary HAN lesions [51].
Table 1.
MMTV common integration sites.
Most MMTV-induced mammary tumors contain 10 or more proviral integrations [51]. Whether MMTV-induced mammary tumors are the result of a single initiating integration or are a composite of multiple integrations is currently unclear, although it appears that progression of tumors from a pregnancy-dependent to a pregnancy-independent state depends on additional integration events and that the former frequently arise as polyclonal populations while the latter are generally monoclonal [34,52]. That mammary tumorigenesis requires the activation of multiple oncogenes is supported by several observations. First, a large percentage of mammary tumors derived from MMTV-infected wild type mice have “hits” at both Wnt1 and Fgf3; it is likely that additional genes are activated in these tumors. Second, the creation of double transgenic mice, such as MMTV-Wnt1/MMTV-Fgf3 accelerates the induction of mammary tumors [53–55]. Similarly, tumorigenesis is accelerated by MMTV infection of transgenic mice with genetic predisposition to mammary tumorigenesis, such as those that express the Wnt1, c-neu or TGFβ transgenes in mammary tissue [54,56].
The oncogenes listed in Table 1 were identified by infection of both wild type and transgenic mice expressing oncogenes in mammary tissue. Although most of the CIS listed in Table I were identified through low throughput analyses, more recently, high throughput analysis of MMTV insertion sites has been performed and uncovered gene families not previously associated with cancer [66]. MMTV target site analysis has great potential for uncovering pathways relevant to the human disease, particularly in transgenic strains with tumor morphology similar to that seen in humans. Even though MMTV-induced mammary tumors do not morphologically resemble most human breast cancers, there are molecular similarities between the mouse and human disease. For example, although Wnt1 itself has not been implicated in human breast cancer, other members of this family as well as targets of the Wnt signaling pathway, such as β-catenin, E-cadherin, cyclin D1, etc., are known to be mutated or deregulated in a number of human cancers [67,68] and several Fgf family members have been implicated in human breast cancer [59,69]. Moreover, a number of the novel CIS uncovered in the high throughput screens were found to be dysregulated in human breast cancer and correlated with one or more clinical parameters in the human tumors, such as angioinvasion, tumor grade or lymphatic infiltration, as well as metastasis [66].
Since the discovery of MMTV, numerous investigators have searched for a similar virus in human breast cancers (see [70] and [37] for a more extensive review). Early studies using immunological assays detected antibodies against MMTV proteins in sera from human breast cancer patients, but were later shown to be most likely due to non-specific cross-reactive proteins [71]. Molecular analyses for DNA sequences related to MMTV in human DNA resulted in the discovery of the first human endogenous retroviruses (HERVs) because of their homology to MMTV, particularly in the pol gene, but no MMTV-like sequences were identified [72]. More recently, several groups have used polymerase chain reaction (PCR)-based techniques to amplify MMTV-like sequences from human breast cancer biopsies [73,74]; however, others have been unable to replicate these studies [75–78]. Moreover, it has been reported that MMTV can infect cultured human mammary epithelial cells, but MMTV cannot use human transferrin receptor 1 as an entry receptor and thus would have to infect cells via a different entry mechanism [14,16,79]. Thus, the existence of a human MTV remains to be confirmed.
5. Conclusions and perspectives
Much has been learned about in vivo virus infection using MMTV and mice. This is in a large part due to our ability to study the natural route of milk-borne transmission and to the use of both inbred and genetically altered transgenic and knockout mice in the analysis of infection and oncogenesis. Because MMTV has existed as an infectious virus in mice for millions of years, it has evolved to take advantage of its host’s biology, using host genes from transcription factors to immune regulatory molecules, to establish infection. Although it causes mammary tumors, this does not occur until relatively late in life and thus the virus has persisted, since infected mothers are able to transmit virus to offspring. The lack of acute MMTV-induced pathogenesis is most likely due to different host means of limiting virus infection, including factors that operate at the cellular level like intrinsic restriction factors and immune response genes. As additional host-anti-viral genes are discovered, MMTV will continue to serve as an important model for testing the ability of these factors to function in vivo.
In addition to serving as an important means for studying virus infection, MMTV has provided a number of critical models for understanding human breast cancer. First, the analysis of MMTV CIS has led to the identification of oncogenes/pathways such as members of the Wnt family that are known to play roles in different human cancers. Second, ITAM-mediated signaling in mammary epithelial cells may represent a novel mechanism of transformation; indeed, a novel oncogene associated with invasive breast cancer in humans has been recently shown to transform cells through ITAM-mediated signaling [80]. Finally, the use of the MMTV LTR to direct oncogene expression to murine epithelial cells has resulted in the creation of numerous transgenic mouse strains that serve as critical models for understanding human breast cancer. It is likely that such transgenic mice will continue to be a critical tool as additional human breast cancer genes are identified through large-scale human genetic studies.
Acknowledgments
I thank the members of my laboratory for many useful discussions. Supported by PHS grants R01-AI-085015 and R01-CA-73746.
References and Notes
- 1.Coffin JM, Hughes SH, Varmus HE. Retroviruses. CSHL Press; Cold Spring Harbor, NY, USA: 1997. [PubMed] [Google Scholar]
- 2.Bittner JJ. Some possible effects of nursing on the mammary gland tumor incidence in mice. Science. 1936;84:162. doi: 10.1126/science.84.2172.162. [DOI] [PubMed] [Google Scholar]
- 3.Callahan R, Smith GH. The mouse as a model for mammary tumorigenesis: history and current aspects. J Mammary Gland Biol Neopl. 2008;13:269. doi: 10.1007/s10911-008-9094-4. [DOI] [PubMed] [Google Scholar]
- 4.Zhu Q, Maitra U, Johnston D, Lozano M, Dudley JP. The homeodomain protein CDP regulates mammary-specific gene transcription and tumorigenesis. Mol Cell Biol. 2004;24:4810–4823. doi: 10.1128/MCB.24.11.4810-4823.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ross SR. MMTV and the immune system. Adv Pharm. 1997;39:21–46. doi: 10.1016/s1054-3589(08)60068-x. [DOI] [PubMed] [Google Scholar]
- 6.Mink S, Hartig E, Jennewein P, Doppler W, Cato ACB. A mammary cell-specific enhancer in mouse mammary tumor virus DNA is composed of multiple regulatory elements including binding sites for CTF/NF-1 and novel transcription-factor, mammary cell-activating factor. Mol Cell Biol. 1992;11:4906–4918. doi: 10.1128/mcb.12.11.4906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wagner KU, McAllister K, Ward T, Davis B, Wiseman R, Hennighausen L. Spatial and temporal expression of the Cre gene under the control of the MMTV-LTR in different lines of transgenic mice. Transgenic Res. 2001;10:545–553. doi: 10.1023/a:1013063514007. [DOI] [PubMed] [Google Scholar]
- 8.Choi YC, Henrard DH, Lee I, Ross SR. The mouse mammary tumor virus long terminal repeat directs expression in epithelial and lymphoid cells of different tissues in transgenic mice. J Virol. 1987;61:3013–3019. doi: 10.1128/jvi.61.10.3013-3019.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reuss FU, Coffin JM. The mouse mammary tumor virus transcription enhancers for hematopoietic progenitor and mammary gland cells share functional elements. J Virol. 2000;74:8183–8187. doi: 10.1128/jvi.74.17.8183-8187.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leder A, Pattengale PK, Kuo A, Stewart TA, Leder P. Consequences of widespread deregulation of the c-myc gene in transgenicmice: multiple neoplasms and normal development. Cell. 1986;45:485–495. doi: 10.1016/0092-8674(86)90280-1. [DOI] [PubMed] [Google Scholar]
- 11.Ball JK, Diggelmann H, Dekaban GA, Grossi GF, Semmler R, Waight PA, Fletcher RF. Alterations in the U3 region of the long terminal repeat of an infectious thymotropic type B retrovirus. J Virol. 1988;62:2985–2993. doi: 10.1128/jvi.62.8.2985-2993.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mertz JA, Mustafa F, Meyers S, Dudley JP. Type B leukemogenic virus has a T-cell-specific enhancer that binds AML-1. J Virol. 2001;75:2174–2184. doi: 10.1128/JVI.75.5.2174-2184.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Payne SL, Elder JH. The role of retroviral dUTPases in replication and virulence. Curr Protein Pept Sci. 2001;2:381–388. doi: 10.2174/1389203013381008. [DOI] [PubMed] [Google Scholar]
- 14.Ross SR, Schofield JJ, Farr CJ, Bucan M. Mouse transferrin receptor 1 is the cell entry receptor for mouse mammary tumor virus. Proc Natl Acad Sci U S A. 2002;99:12386–12390. doi: 10.1073/pnas.192360099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ponka P, Lok CN. The transferrin receptor: role in health and disease. Int J BiochemCell Biol. 1999;31:1111–1137. doi: 10.1016/s1357-2725(99)00070-9. [DOI] [PubMed] [Google Scholar]
- 16.Wang E, Obeng-Adjei N, Ying Q, Meertens L, Dragic T, Davey RA, Ross SR. Mouse mammary tumor virus uses mouse but not human transferrin receptor 1 to reach a low pH compartment and infect cells. Virol. 2008;381:230–240. doi: 10.1016/j.virol.2008.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schulman HM, Ponka P, Wilczynska A, Gauthier Y, Shyamala G. Transferrin receptor and ferritin levels during murine mammary gland development. Biochim Biophys Acta. 1989;1010:1–6. doi: 10.1016/0167-4889(89)90176-6. [DOI] [PubMed] [Google Scholar]
- 18.Futran J, Kemp JD, Field EH, Vora A, Ashman RF. Transferrin receptor synthesis is an early event in B cell activation. J Immunol. 1989;143:787–792. [PubMed] [Google Scholar]
- 19.Brekelmans P, van Soest P, Voerman J, Platenburg PP, Leenen PJ, van Ewijk W. Transferrin receptor expression as a marker of immature cycling thymocytes in the mouse. Cell Immunol. 1994;159:331–339. doi: 10.1006/cimm.1994.1319. [DOI] [PubMed] [Google Scholar]
- 20.Xu L, Wrona TJ, Dudley JP. Strain-specific expression of spliced MMTV RNAs containing the superantigen gene. Virol. 1997;236:54–65. doi: 10.1006/viro.1997.8717. [DOI] [PubMed] [Google Scholar]
- 21.Reuss FU, Coffin JM. Stimulation of mouse mammary tumor virus superantigen expression by an intragenic enhancer. Proc Natl Acad Sci U S A. 1995;92:9293–9297. doi: 10.1073/pnas.92.20.9293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arroyo J, Winchester E, McLellan BS, Huber BT. Shared promoter elements between a viral superantigen and the major histocompatibility complex class II-associated invariant chain. J Virol. 1997;71:1237–1245. doi: 10.1128/jvi.71.2.1237-1245.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Indik S, Gunzburg WH, Salmons B, Rouault F. A novel, mouse mammary tumor virus encoded protein with Rev-like properties. Virol. 2005;337:1–6. doi: 10.1016/j.virol.2005.03.040. [DOI] [PubMed] [Google Scholar]
- 24.Mertz JA, Simper MS, Lozano MM, Payne SM, Dudley JP. Mouse mammary tumor virus encodes a self-regulatory RNA export protein and is a complex retrovirus. J Virol. 2005;79:14737–14747. doi: 10.1128/JVI.79.23.14737-14747.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mertz JA, Lozano MM, Dudley JP. Rev and Rex proteins of human complex retroviruses function with the MMTV Rem-responsive element. Retrovirol. 2009;6:10. doi: 10.1186/1742-4690-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mullner M, Salmons B, Gunzburg WH, Indik S. Identification of the Rem-responsive element of mouse mammary tumor virus. Nucleic Acids Res. 2008;36:6284–6294. doi: 10.1093/nar/gkn608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Swanstrom R, Wills JW. Synthesis, assembly, and processing of viral proteins. In: Coffin JM, Hughes SM, Varmus HE, editors. Retroviruses. Cold Spring Harbor Laboratory Press; Cold Spring Harbor, N.Y., USA: 1997. pp. 263–334. [PubMed] [Google Scholar]
- 28.St George JA, Cardiff RD, Young LJ, Faulkin LJ. Immunocytochemical distribution of mouse mammary tumor virus antigens in BALB/cfC3H mammary epithelium. J Natl Canc Inst. 1979;63:813–820. doi: 10.1093/jnci/63.3.813. [DOI] [PubMed] [Google Scholar]
- 29.Golovkina TV, Chervonsky A, Dudley JP, Ross SR. Transgenic mouse mammary tumor virus superantigen expression prevents viral infection. Cell. 1992;69:637–645. doi: 10.1016/0092-8674(92)90227-4. [DOI] [PubMed] [Google Scholar]
- 30.Bentvelzen P, Hilgers J. Murine mammary tumor virus. In: Klein G, editor. Viral Oncology. Raven Press; N.Y., USA: 1980. pp. 311–355. [Google Scholar]
- 31.Baillie GJ, van de Lagemaat LN, Baust C, Mager DL. Multiple groups of endogenous betaretroviruses in mice, rats and other mammals. J Virol. 2004;78:5784–5798. doi: 10.1128/JVI.78.11.5784-5798.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kozak C, et al. A standardized nomenclature for endogenous mouse mammary tumor viruses. J Virol. 1987;61:1651–1654. doi: 10.1128/jvi.61.5.1651-1654.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Imai S, Okumoto M, Iwai M, Haga S, Mori N, Miyashita N, Moriwaki K, Hilgers J, Sarkar NH. Distribution of mouse mammary tumor virus in Asian wild mice. J Virol. 1994;68:3437–3442. doi: 10.1128/jvi.68.5.3437-3442.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Callahan R, Smith GH. MMTV-induced mammary tumorigenesis: gene discovery, progression to malignancy and cellular pathways. Oncogene. 2000;19:992–1001. doi: 10.1038/sj.onc.1203276. [DOI] [PubMed] [Google Scholar]
- 35.Golovkina TV, Piazzon I, Nepomnaschy I, Buggiano V, de Olano Vela M, Ross SR. Generation of a tumorigenic milk-borne mouse mammary tumor virus by recombination between endogenous and exogenous viruses. J Virol. 1997;71:3895–3903. doi: 10.1128/jvi.71.5.3895-3903.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nandi S, McGrath CM. Mammary neoplasia in mice. Adv Canc Res. 1973;17:353–414. [Google Scholar]
- 37.Ross SR. MMTV infectious cycle and the contribution of virus-encoded proteins to transformation of mammary tissue. J Mammary Gland Biol Neopl. 2008;13:299–307. doi: 10.1007/s10911-008-9090-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Golovkina TV, Dudley JP, Ross SR. Superantigen activity is need for mouse mammary tumor virus spread within the mammary gland. J Immunol. 1998;161:2375–2382. [PubMed] [Google Scholar]
- 39.Finke D, Acha-Orbea H. Differential migration of in vivo primed B and T lymphocytes to lymphoid and non-lymphoid organs. Eur J Immunol. 2001;31:2603–2611. doi: 10.1002/1521-4141(200109)31:9<2603::aid-immu2603>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 40.Ignatowicz L, Kappler J, Marrack P. The effects of chronic infection with a superantigen-producing virus. J Exp Med. 1992;175:917–923. doi: 10.1084/jem.175.4.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Golovkina TV, Prescott JA, Ross SR. Mouse mammary tumor virus-induced tumorigenesis in sag transgenic mice: a laboratory model of natural selection. J Virol. 1993;67:7690–7694. doi: 10.1128/jvi.67.12.7690-7694.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Launois P, Maillard I, Pingel S, Swihart KG, Xenarios I, Acha-Orbea H, Diggelmann H, Locksley RM, MacDonald HR, Louis JA. IL-4 rapidly produced by V beta 4 V alpha 8 CD4+ T cells instructs Th2 development and susceptibility to Leishmania major in BALB/c mice. Immunity. 1997;6:541–549. doi: 10.1016/s1074-7613(00)80342-8. [DOI] [PubMed] [Google Scholar]
- 43.Okeoma CM, Ross SR. Genetics of host resistance to retroviruses and cancer. In: Dudley JP, editor. Retroviruses and Insights into Cancer. Springer Science and Business Media; N.Y., USA: 2010. in press. [Google Scholar]
- 44.Okeoma CM, Lovsin N, Peterlin BM, Ross SR. APOBEC3 inhibits mouse mammary tumor virus replication in vivo. Nature. 2007;445:927–930. doi: 10.1038/nature05540. [DOI] [PubMed] [Google Scholar]
- 45.Takeda E, Tsuji-Kawahara S, Sakamoto M, Langlois MA, Neuberger MS, Rada C, Miyazawa M. Mouse APOBEC3 restricts Friend leukemia virus infection and pathogenesis in vivo. J Virol. 2008;82:10998–11008. doi: 10.1128/JVI.01311-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Okeoma CM, Petersen J, Ross SR. Expression of murine APOBEC3 alleles in different mouse strains and their effect on mouse mammary tumor virus infection. J Virol. 2009;83:3029–3038. doi: 10.1128/JVI.02536-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Callahan R, Smith GH. Common integration sites for MMTV in viral induced mouse mammary tumors. J Mammary Gland Biol Neopl. 2008;13:309–321. doi: 10.1007/s10911-008-9092-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Katz E, Lareef MH, Rassa JC, Grande SM, King LB, Russo J, Ross SR, Monroe JG. MMTV Env encodes an ITAM responsible for transformation of mammary epithelial cells in three-dimensional culture. J Exp Med. 2005;201:431–439. doi: 10.1084/jem.20041471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ross SR, Schmidt JW, Katz E, Cappelli L, Hultine S, Gimmotty P, Monroe JG. An immunoreceptor tyrosine activation motif in the Mouse Mammary Tumor Virus envelope protein plays a role in virus-induced mammary tumors. J Virol. 2006;80:9000–9008. doi: 10.1128/JVI.00788-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kordon EC, Smith GH. An entire functional mammary gland may comprise the progeny from a single cell. Development. 1998;125:1921–1930. doi: 10.1242/dev.125.10.1921. [DOI] [PubMed] [Google Scholar]
- 51.Cardiff RD, Anver MR, Gusterson BA, Hennighausen L, Jensen RA, Merino MJ, Rehm S, Russo J, Tavassoli FA, Wakefield LM, Ward JM, Green JE. The mammary pathology of genetically engineered mice: the consensus report and recommendations from the Annapolis meeting. Oncogene. 2000;19:968–988. doi: 10.1038/sj.onc.1203277. [DOI] [PubMed] [Google Scholar]
- 52.Buggiano V, Levy CS, Gattelli A, Cirio MC, Marfil M, Nepomnaschy I, Piazzon I, Helguero L, Vanzulli S, Kordon EC. Origin and progression of pregnancy-dependent mammary tumors induced by new mouse mammary tumor virus variants. Breast Canc Res Treat. 2002;75:191–202. doi: 10.1023/a:1019932516887. [DOI] [PubMed] [Google Scholar]
- 53.Kwan H, Pecenka V, Tsukamoto A, Parslow TG, Guzman R, Lin TP, Muller WJ, Lee FS, Leder P, Varmus HE. Transgenes expressing the Wnt1 and int2 protooncogenes cooperate during mammary carcinogenesis in doubly transgenic mice. Mol Cell Biol. 1992;12:147–154. doi: 10.1128/mcb.12.1.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Shackleford GM, MacArthur CA, Kwan HC, Varmus HE. Mouse mammary tumor virus infection accelerates mammary carcinogenesis in Wnt1 transgenic mice by insertional activation of int2/Fgf3 and hst/Fgf4. Proc Natl Acad Sci U S A. 1993;90:740–744. doi: 10.1073/pnas.90.2.740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.MacArthur CA, Shankar DB, Shackleford GM. Fgf-8, activated by proviral insertion, cooperates with the Wnt-1 transgene in murine mammary tumorigenesis. J Virol. 1995;69:2501–2507. doi: 10.1128/jvi.69.4.2501-2507.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dievart A, Beaulieu N, Jolicoeur P. Involvement of Notch1 in the development of mouse mammary tumors. Oncogene. 1999;18:5973–59781. doi: 10.1038/sj.onc.1202991. [DOI] [PubMed] [Google Scholar]
- 57.Nusse R, Van Ooyen A, Cox D, Fung YKT, Varmus HE. Mode of proviral activation of a putative mammary oncogene (int 1) on mouse chromosome 15. Nature. 1984;307:131–136. doi: 10.1038/307131a0. [DOI] [PubMed] [Google Scholar]
- 58.Dickson C, Smith R, Brookes S, Peters G. Tumorigenesis by mouse mammary tumor virus: proviral activation of a cellular gene in the common integration region int-2. Cell. 1984;37:529–536. doi: 10.1016/0092-8674(84)90383-0. [DOI] [PubMed] [Google Scholar]
- 59.Theodorou V, Boer M, Weigelt B, Jonkers J, van der Valk M, Hilkens J. Fgf10 is an oncogene activated by MMTV insertional mutagenesis in mouse mammary tumors and overexpressed in a subset of human breast carcinomas. Oncogene. 2004;23:6047–6055. doi: 10.1038/sj.onc.1207816. [DOI] [PubMed] [Google Scholar]
- 60.Gallahan D, Callahan R. The mouse mammary tumor associated gene INT3 is a unique member of the NOTCH gene family (NOTCH4) Oncogene. 1997;14:1883–1890. doi: 10.1038/sj.onc.1201035. [DOI] [PubMed] [Google Scholar]
- 61.Durgam VR, Tekmal RR. The nature and expression of int-5, a novel MMTV integration locus gene in carcinogen-induced mammary tumors. Canc Lett. 1994;87:179–1786. doi: 10.1016/0304-3835(94)90220-8. [DOI] [PubMed] [Google Scholar]
- 62.Schroeder JA, Troyer KL, Lee DC. Cooperative induction of mammary tumorigenesis by TGFalpha and Wnts. Oncogene. 2000;19:3193–3199. doi: 10.1038/sj.onc.1203652. [DOI] [PubMed] [Google Scholar]
- 63.Marchetti A, Buttitta F, Miyazaki S, Gallahan D, Smith GH, Callahan R. Int-6, a highly conserved, widely expressed gene, is mutated by mouse mammary tumor virus in mammary preneoplasia. J Virol. 1995;69:1932–1938. doi: 10.1128/jvi.69.3.1932-1938.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lowther W, Wiley K, Smith GH, Callahan R. A new common integration site, Int7, for the mouse mammary tumor virus in mouse mammary tumors identifies a gene whose product has furin-like and thrombospondin-like sequences. J Virol. 2005;79:10093–10096. doi: 10.1128/JVI.79.15.10093-10096.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gattelli A, Zimberlin MN, Meiss RP, Castilla LH, Kordon EC. Selection of early-occurring mutations dictates hormone-independent progression in mouse mammary tumor lines. J Virol. 2006;80:11409–11415. doi: 10.1128/JVI.00234-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Theodorou V, Kimm MA, Boer M, Wessels L, Theelen W, Jonkers J, Hilkens J. MMTV insertional mutagenesis identifies genes, gene families and pathways involved in mammary cancer. Nat Genet. 2007;39:759–769. doi: 10.1038/ng2034. [DOI] [PubMed] [Google Scholar]
- 67.Li Y, Hively WP, Varmus HE. Use of MMTV-Wnt-1 transgenic mice for studying the genetic basis of breast cancer. Oncogene. 2000;19:1002–1009. doi: 10.1038/sj.onc.1203273. 19. [DOI] [PubMed] [Google Scholar]
- 68.Li Y, Welm B, Podsypanina K, Huang S, Chamorro M, Zhang X, Rowlands T, Egeblad M, Cowin P, Werb Z, Tan LK, Rosen JM, Varmus HE. Evidence that transgenes encoding components of the Wnt signaling pathway preferentially induce mammary cancers from progenitor cells. Proc Natl Acad Sci U S A. 2003;100:15853–15858. doi: 10.1073/pnas.2136825100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Meyers SL, Dudley JP. Sequence analysis of the int-2/fgf-3 gene in aggressive human breast carcinomas. Mol Carc. 1992;6:243–251. doi: 10.1002/mc.2940060405. [DOI] [PubMed] [Google Scholar]
- 70.Voisset C, Weiss RA, Griffiths DJ. Human RNA “rumor” viruses: the search for novel human retroviruses in chronic disease. Microbiol Mol Biol Rev. 2008;72:157–196. doi: 10.1128/MMBR.00033-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Goedert JJ, Rabkin CS, Ross SR. Prevalence of serologic reactivity against four strains of mouse mammary tumor virus among U.S. women with breast cancer. Br J Canc. 2006;94:548–551. doi: 10.1038/sj.bjc.6602977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ono M, Yasunaga T, Miyata T, Ushikubo H. Nucleotide sequence of human endogenous retrovirus genome related to the mouse mammary tumor virus genome. J Virol. 1986;60:589–598. doi: 10.1128/jvi.60.2.589-598.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wang Y, Holland JF, Bleiweiss IJ, Melana S, Liu X, Pelisson I, Cantarella A, Stellrecht K, Mani S, Pogo BG. Detection of mammary tumor virus ENV gene-like sequences in human breast cancer. CancRes. 1995;35:5173–5179. [PubMed] [Google Scholar]
- 74.Ford CE, Tran D, Deng Y, Ta VT, Rawlinson WD, Lawson JS. Mouse mammary tumor virus-like gene sequences in breast tumors of Australian and Vietnamese women. Clin Canc Res. 2003;9:1118–1120. [PubMed] [Google Scholar]
- 75.Mant C, Gillett C, D’Arrigo C, Cason J. Human murine mammary tumour virus-like agents are genetically distinct from endogenous retroviruses and are not detectable in breast cancer cell lines or biopsies. Virol. 2004;318:393–404. doi: 10.1016/j.virol.2003.09.027. [DOI] [PubMed] [Google Scholar]
- 76.Bindra A, Muradrasoli S, Kisekka R, Nordgren H, Warnberg F, Blomberg J. Search for DNA of exogenous mouse mammary tumor virus-related virus in human breast cancer samples. J Gen Virol. 2007;88:1806–1809. doi: 10.1099/vir.0.82767-0. [DOI] [PubMed] [Google Scholar]
- 77.Frank O, Verbeke C, Schwarz N, Mayer J, Fabarius A, Hehlmann R, Leib-Mosch C, Seifarth W. Variable transcriptional activity of endogenous retroviruses in human breast cancer. J Virol. 2008;82:1808–1818. doi: 10.1128/JVI.02115-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Park DJ, Southey MC, Giles GG, Hopper JL. No evidence of MMTV-like env sequences in specimens from the Australian Breast Cancer Family Study. Breast Canc Res Treat. 2010 doi: 10.1007/s10549-010-0946-4.. [DOI] [PubMed] [Google Scholar]
- 79.Indik S, Gunzburg WH, Salmons B, Rouault F. Mouse mammary tumor virus infects human cells. Canc Res. 2005;65:6651–6659. doi: 10.1158/0008-5472.CAN-04-2609. [DOI] [PubMed] [Google Scholar]
- 80.Katz E, Dubois-Marshall S, Sims AH, Faratian D, Li J, Smith ES, Quinn JA, Edward M, Meehan RR, Evans EE, Langdon SP, Harrison DJ. A gene on the HER2 amplicon, C35, is an oncogene in breast cancer whose actions are prevented by inhibition of Syk. Br J Canc. 2010;103:401–410. doi: 10.1038/sj.bjc.6605763. [DOI] [PMC free article] [PubMed] [Google Scholar]