The authors conclude that single port access cholecystectomy is a viable alternative to multi-port cholecystectomy.
Keywords: Laparoscopy, Cholecystectomy, Single port access surgery, Minimal access surgery, SPA surgery
Abstract
Introduction:
Laparoscopy is a constantly evolving field of surgery. New technology, applications, and benefits prompt continual improvement. We have developed a Single Port Access (SPA) surgical technique that allows for the entire cholecystectomy to be performed through a single incision within the umbilicus while maintaining safe standard dissection and retraction techniques of currently performed multi-port laparoscopic cholecystectomy.
Methods:
Fifteen consecutive patients underwent SPA cholecystectomy. Indications were cholelithiasis, cholecystitis, CBD stones, and biliary akinesia. The entire procedure was performed through a single umbilical incision measuring <1.8 cm within the umbilicus. Three trocars and a rigid grasper were inserted through separate fascial sites within the same skin incision. The cholecystectomy procedures are then performed in the standard fashion described in multi-port cholecystectomy.
Results:
Fifteen patients successfully underwent Single Port Access cholecystectomy. One patient required a second 5-mm port site secondary to difficulty with retraction of a large liver. Operative times averaged 107 minutes. Blood loss, patient recovery, and outcomes have been comparable to those of standard multi-port procedures. No umbilical hernias have been seen at 2 years of follow-up.
Conclusion:
We present the SPA cholecystectomy as an alternative to multi-port cholecystectomy. In the first 2 years, SPA surgery has evolved into a technique easily taught and performed without the restrictions of new equipment or added cost.
INTRODUCTION
The natural progression of any surgical technique is gradual change and improvement. Open surgery was the mainstay of general surgery, but over the years procedures evolved, becoming less invasive with smaller incisions. In the late 1980s, laparoscopic surgery saw the beginnings of enormous growth in application. Although this technique was met with great skepticism, it is now the standard of care for many general surgery procedures. Historically, this technology had been used in the past, introduced by Kellig with celioscopy.1 A consistent number of cases was first seen with tubal ligations performed in gynecology. With the development of the video laparoscope and improved instrumentation, laparoscopic surgery was applied to larger cases in general surgery, such as the cholecystectomy. Criticism was vast because this technique used a completely novel means of operating, with new equipment and visualization. The eventual acceptance was due to the persistence of surgeons, such as McKernan and Saye and Reddick and Olsen, with dedication to teaching and proving patient benefits. After laparoscopic cholecystectomy proved beneficial in patient recovery, the procedure became the gold standard. The basic principles of this evolving technique were then applied to general surgical procedures across the board.
Since its conception, laparoscopic cholecystectomy has remained virtually unchanged. Throughout the years, many surgeons have suggested modifications in the technique but have failed to prove added benefits. In 1996 Navarra2 reported on a single-incision laparoscopic cholecystectomy using transabdominal sutures. This technique was subsequently applied and reported by others as well.3 Although innovative, added benefits were not apparent. In a communication, Navarra listed the lack of benefits and reasons he felt the procedure would not develop.4 The possibility of injuring adjacent abdominal structures by introducing the sharp needle added unnecessary risk. More recently, the idea of reduced port surgeries, such as the 3-port cholecystectomy, has been reported.5 Although benefits may be minimal, if the same procedure is done safely, there is no reason to insert the extra unneeded port.
Completely new techniques of gallbladder removal have also been introduced recently. NOTES procedures have been performed in the porcine model, removing the gallbladder transvaginally or transgastricly.6 Potential benefits of this technique include decreased anesthesia requirements, faster recovery, and enhanced cosmesis. These proposed benefits have yet to be proven, and this procedure, especially transgastric removal, is associated with unacceptable risks of leak and infection. Scarless surgery, however, is immediately attractive to both physicians and patients.
Possibly influenced by all these ideas, in the last year we have seen the emergence of a new approach using fewer incisions, with multiple instruments entering through a single port device or entry site and/or strategically placed sutures for static retraction.7,8 Many different techniques have been developed concurrently, suggesting the need and desire for change and improvement. Improved technology and development of new surgical instrumentation has also appeared in response to these new ideas. Central to all these techniques is the idea of incision reduction.
We performed the first case of single port access (SPA) surgery in April 2007.9 We have developed this unique access technique utilizing the basic principles of current laparoscopic surgery and standard instrumentation and access devices. In May and June 2007, we applied this technique to laparoscopic cholecystectomy and gynecologic procedures, respectively. Our initial experience with these procedures was presented at the Society of Laparoendoscopic Surgeons, Asian American Summit III in February 2008.
The single port access technique (SPA Surgery) has become our standard of care for laparoscopic cholecystectomy as well as a large number of other procedures. All patients presenting with gallbladder pathology requiring removal are offered this operation without bias. We present our initial 15 patients who underwent SPA cholecystectomy. Over the first 2 years of performing SPA surgery, we can now report not only our results with the technique, but the changes and improvements we have developed. Furthermore, we can address the concern about hernia formation with a new entry technique using a single portal of entry to insert multiple instruments.
METHODS
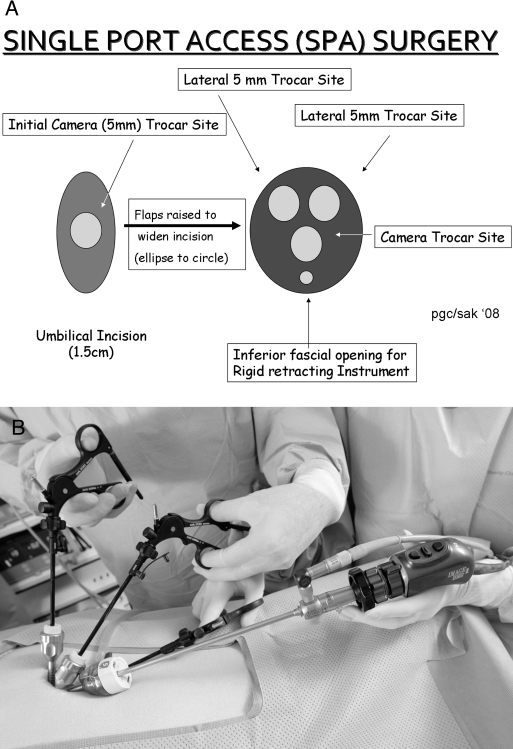
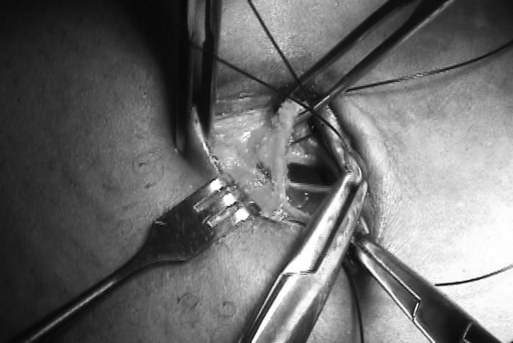
Fifteen consecutive patients were offered SPA cholecystectomy. Indications varied: cholecystitis, biliary akinesia, cholelithiasis, gallbladder polyp, choledocholithiasis (Table 1). Mean age was 50 years, and mean weight was 158lb. Initial preparation and access were the same for all patients. The patient was positioned supine, the abdomen prepped wide to allow for conversion to multiple ports or open surgery. An incision approximately 15mm in length was made in the median fold of the umbilicus (Figure 1). The skin and subcutaneous adipose tissue were elevated from the fascia, creating lateral skin and soft tissue flaps on either side of the incision (Figure 2). This SPA “Circle of Entry” measured approximately 5cm across under the skin (Figure 3a, b). A clear, bladeless 5-mm trocar (Xcel, Ethicon) was inserted under direct visualization in the center of the incision. The abdomen was insufflated and inspected. The 2 lateral “very low profile” trocars (disposable Hunt cannula, Apple Medical, or Karl Storz reusable 5-mm trocar) were then inserted 1.5cm to 2cm from the central trocar in a triangulated fashion through separate fascial openings. The clear bladeless inner trocar was exchanged for the sharp blade of the very low profile trocars. This enabled visualization for a safer insertion (Figure 4). This created a triangulated arrangement of trocars each with individual fascial access points. Finally, in the last 6 patients, a rigid grasper was inserted directly through the fascia in the caudal midline just below the central trocar, but through the same skin incision. This grasper provided retraction of the gallbladder fundus atop the liver (Figure 5).
Table 1.
Results of Cholecytectomy With 2 and 3 Instrument Technique
| Patient | Indication | Concomitant Procedures | Age | Weight (lbs) | Operative Time | Length of Stay (hrs) | Additional Ports |
|---|---|---|---|---|---|---|---|
| 2 Instrument Technique | |||||||
| 1 | Cholecystitis | 17 | 110 | 120 | 48 | ||
| 2 | Akinesia | 31 | 154 | 94 | 24 | Subxyphoid | |
| 3 | Cholelithiasis | 62 | 156 | 57 | 48 | ||
| 4 | Cholelithiasis | Ventral hernia repair | 57 | 244 | 104 | 24 | |
| 5 | Akinesia | 28 | 135 | 113 | 24 | ||
| 6 | Cholelithiasis | 48 | 180 | 120 | 48 | ||
| 7 | Cholecystitis | 45 | 306 | 168 | 24 | ||
| 8 | Polyp | 46 | 136 | 95 | 24 | ||
| 9 | Cholelithiasis | Ureteral dilitation | 56 | 102 | 111 | 24 | |
| 10 | Cholelithiasis | Hysterectomy | 71 | 162 | 82 | 48 | |
| Mean | 46 | 169 | 106 | ||||
| 3 Instrument Technique | |||||||
| 11 | Choledocolithiasis | CBD stone s/p ERCP | 85 | 140 | 61 | 6 days | |
| 12 | Cholelithiasis | 28 | 180 | 102 | 24 | ||
| 13 | Akinesia | 50 | 149 | 110 | 24 | ||
| 14 | Cholelithiasis | 44 | 110 | 88 | 24 | ||
| 15 | Cholelithiasis | Adhesiolysis | 63 | 160 | 175 | 24 | |
| Mean | 54 | 148 | 107 | ||||
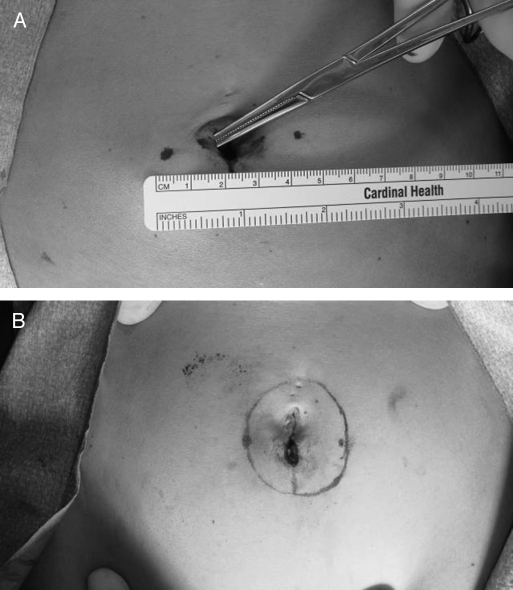
Figure 1.
Initial skin incision.
Figure 2.
Creation of skin flaps.
Figure 3.
(A) SPA Circle of Entry; (B) SPA Circle of Entry.
Figure 4.
Visualization on entry.
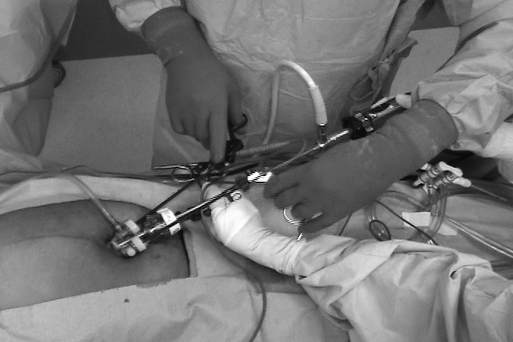
Figure 5.
Fundal retracting instrument.
The SPA trocar entry technique is demonstrated in Figure 6a, b.
Figure 6.
(A) SPA schematic setup; (B) Final SPA setup.
Initial cases were performed with standard-length rigid scopes through the central 5-mm trocar. In subsequent cases, we used an extended-length rigid bronchoscope to move the camera head out of the field of the instrument handles (Figure 7). The lateral very low profile trocars were used for exchanging operative instruments of choice throughout the procedure. In the initial 5 procedures, articulating instrumentation was used to compensate for lack of separate fundal retraction. In the last 10 cases, rigid instrumentation was used. The third instrument, a rigid grasper, was introduced after the tenth case to reliably ensure visualization of the “critical view” of the cystic duct-common bile duct relationship. The third instrument remained in place throughout the operation for dynamic retraction of the fundus of the gallbladder and liver (Figure 8).
Figure 7.
Long scope.
Figure 8.
Fundal retraction.
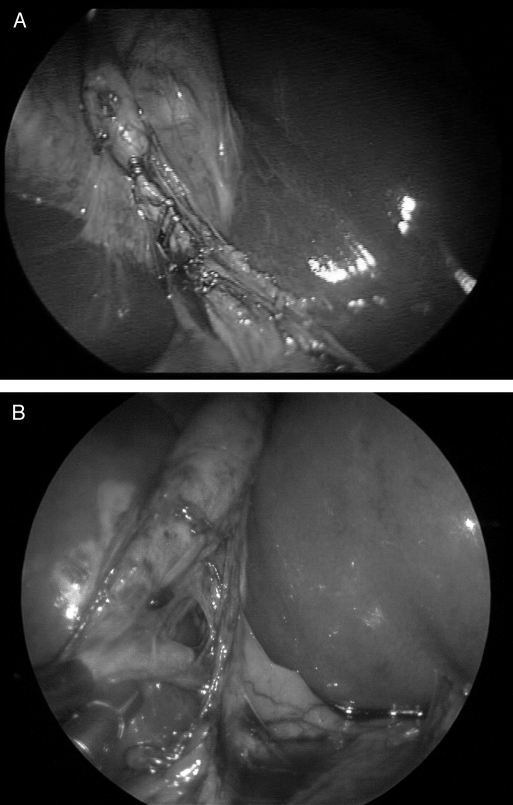
Thirteen of the 15 procedures were completed with standard retrograde dissection of the gallbladder following dissection, securing, and transection of the cystic duct. The gallbladder was then cauterized off of the liver bed in a retrograde fashion. Two procedures were performed using the “dome down” technique given inflammation in the area of the cystic duct. PDS Endoloops were secured around the cystic duct and artery, and these structures were transected.
In all patients, the gallbladder was extracted through the umbilicus. In those patients with small akinetic gallbladders, the specimen could be removed through the 5-mm central incision. In those patients with large stones or more diseased gallbladders, the fascial openings were connected to facilitate delivery. In 2 patients, the 5-mm central trocar was replaced with a 10-mm retrieval bag device to retrieve the specimen. After final inspection of the abdomen and liver bed, all fascial openings were closed with 0 Vicryl suture. The subcutaneous tissue and skin were then approximated using 3- 0 and 4 - 0 suture, respectively (Figure 9).
Figure 9.
Closure.
Patients had office follow-up at 2 weeks, 3 months, 6 months, 1 year, and 2 years.
RESULTS
All 15 procedures were performed without conversion to open cholecystectomy. In one early SPA cholecystectomy performed using the 2-instrument technique, an additional epigastric trocar was inserted for retraction.
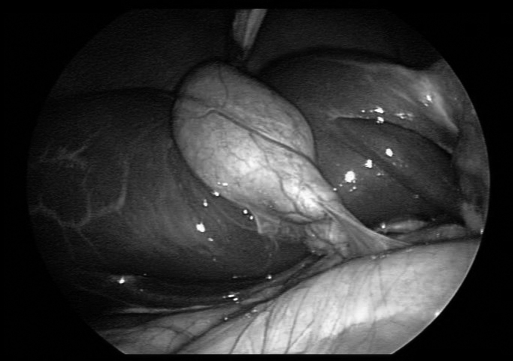
Three trocars were inserted, all through an umbilical incision, for the first 10 patients. Two articulating instruments were used for retraction and dissection. A rigid grasper was inserted directly through the fascia in the last 5 patients (Table 1). Attention to the “critical view ” was observed in each case. This was easily obtained in the 3-instrument technique. In the 2-instrument technique and those procedures utilizing articulation, the critical view was oftentimes difficult to obtain and not clearly demonstrated in a number of patients (Figure 10a). The 3-instrument technique always demonstrated the critical view (Figure 10b).
Figure 10.
(A) Lack of critical view; (B) Critical view.
Mean operative time for all 15 procedures was 107 minutes (Table 1). The mean operative time for the first 10 cases using 2 articulating instruments was 106 minutes. The last 5 cases performed with 3 rigid instruments had a mean operative time of 107 minutes. The longest operative time of 175 minutes was in a patient who also underwent extensive adhesiolysis. Length of stay was typically a 24-hour observation. One patient underwent TAH/BSO and remained in the hospital for 2 days on the gynecology service. One patient was admitted for a CHF exacerbation and developed acute cholecystitis. He was discharged 3 days postoperatively. Final skin incisions all measured <2cm (Figure 11).
Figure 11.
Final skin incision.
All patients were discharged with Percocet for pain management. By postoperative day 3, no one was using narcotics for relief.
Follow-up at 2 weeks revealed 3 umbilical seromas with minimal clear drainage. There was no accompanying erythema or irritation. No wound infections were observed. No umbilical hernias were observed at 1- and 2-year follow-up for all patients.
Return to daily activities varied, because with no patient selection the patients had variable states of health preoperatively. Our first patient, a 26-year-old female, returned to light house work on postoperative day 3, and work on postoperative day 5. Our 85-year-old patient with CHF was discharged home independently without the need for admission to a skilled nursing or rehabilitation facility.
DISCUSSION
We developed Single Port Access surgery as an alternative approach to standard multi-port laparoscopy. Proposed advantages benefit both surgeons and patients, offering increased surgeon comfort, improved cosmesis, and possibly quicker recovery and decreased pain. With our initial results, recovery is comparable to that of standard multiple incision laparoscopic cholecystectomy with slightly longer operative times attributed to learning curves. Cosmesis is improved with a single incision hidden within the folds of the umbilicus. Thus far, we have not observed umbilical hernia formation. Closure must be done carefully, and extended follow-up is necessary to address concerns about umbilical hernia development.
Initially, we performed reduced trocar laparoscopic procedures with articulating instruments.10 Gradually, as skill and comfort with the articulating instruments improved, we began to move the trocars to the umbilicus. In the first 10 cases presented here, we used 2 articulating instruments. Although this technique was similar to standard multi-port procedures, exposure by retraction and dissection were altered with loss of the third instrument for dedicated fundal retraction. Although it initially appeared that articulating instruments would compensate for the loss of independent manipulation of the fundus and infundibulum, the angles of dissection were skewed. Clear exposure of the critical view was suboptimal. Retraction was inadequate with only 2 instruments. To improve the ease and safety of this technique, we added a rigid grasper to provide fundal retraction of the gallbladder atop the liver. By adding this grasper, the exact exposure of standard multi-port laparoscopic cholecystectomy was mimicked. With the addition of the third instrument directly through the fascia, we were able to obtain dynamic retraction and independent manipulation of the gallbladder fundus and infundibulum.
Some authors who have attempted incision reduction in the past used transabdominal sutures. This provides retraction but in a static fashion. By adding the third instrument, we were able to retract the gallbladder cephalad and inferero-laterally to expose the classic described critical view.11
Initially we were using articulating instrumentation to create a triangulated surgical field within the abdomen. Using these instruments decreased availability and increased the cost of the procedure. Additionally, there was a learning curve with articulation. The addition of the third retracting instrument allowed for the use of all rigid instrumentation. Fundal retraction, infundibular manipulation, and dissection are all carried out with separate instruments just as in standard cholecystectomy. In addition, by placing the instruments in a 5-cm SPA Circle of Entry, we have moved the triangulation to the abdominal wall and have eliminated the need to create the triangulation in the abdomen.
Recently, a focus on the ergonomics of surgery has appeared in the literature.12,13 In our experience, this technique is more ergonomic for the surgeon and assistant. Initially, we were using a standard operative scope. Exchanging this for an extended length camera positions the assistant closer to the patient's feet, affording the surgeon a larger operative space. The set up of multiple trocars in a single incision results in the surgeons hands in closer proximity, mimicking open procedures. The surgeon is no longer reaching across the table and patient.
Using 3 trocars allows for each instrument to have independence of movement. Movement of one instrument does not affect movement of others. The pliable fascia allows this unique property we have not seen in multi-port trocars. Independence of movement at the level of the trocars then allows the other instruments to safely dissect within the triangle of Calot and provides uninhibited retraction. Further scientific analysis will be needed to prove this observed ergonomic benefit.
Initial exposure to NOTES procedures certainly is intriguing but is often associated with an extensive learning curve and limited applicability. We believe this stems from the thought of “leaping” from 4 laparoscopic incisions to one transoral, transrectal, or transvaginal entry site. In this respect, we see Single Port Access surgery as not only a potential benefit to patients, but also as a stepping stone to the road to NOTES-based surgery. It is certainly easier to visualize NOTES once we begin by reducing the current number of incisions. The next step will simply be moving them to another site (ie, mouth, anus, or vagina).
Our technique maintains the standard procedure and instrumentation, but improves access. In addition, the access technique maintains the “independence of movement” necessary to safely and adequately perform dissection within the abdominal cavity using standard, familiar rigid instrumentation. The standard rigid instruments are used in the same number and manner as standard laparoscopic cholecystectomy.
An important component of the follow-up and reporting of any new technique is its safety, applicability, and attention to potential added costs. In addition, follow-up of potential development of umbilical hernia is an important consideration in this novel approach to laparoscopy. For this reason, initial reports need to be reviewed with a critical eye to ensure adherence to safe, accepted standards, addressing potential concerns and providing adequate follow-up. In addition, the applicability of a new technique across surgical procedures needs to be considered, with a cost conscious view.
CONCLUSION
We illustrate the evolution of our own technique over the year. Most important is maintaining safety. We must strive to always be critical of new techniques, because there is always room for further improvement. We recommend attending courses that focus on various forms of reducedor single-incision laparoscopic surgery.9 We recommend beginning by reducing port sites slowly and working to develop the skills to operate via a single port.
We present this series of 15 cholecystectomies to suggest an alternative approach to cholecystectomy. Our initial results prove that no weight, age, or comorbidity biases exist. Long-term follow-up of large series will be necessary to prove potential benefits of recovery, pain relief, and umbilical hernia formation. SPA cholecystectomy is now offered consecutively to all of our patients.
Contributor Information
Erica R. Podolsky, Drexel University, College of Medicine, Department of Surgery, Philadelphia, Pennsylvania..
Steven J. Rottman, Drexel University, College of Medicine, Department of Surgery, Philadelphia, Pennsylvania..
Paul G. Curcillo, II, Drexel University, College of Medicine, Department of Surgery, Philadelphia, Pennsylvania..
References:
- 1. Schollmeyer T, Soyinka AS, Schollmeyer M, et al. Georg Kelling (1866-1945): the root of modern day minimal invasive surgery. A forgotten legend? Arch Gynecol Obstet. 2007;276:505–509 [DOI] [PubMed] [Google Scholar]
- 2. Navarra G, Pozza E, Occhionorelli S, et al. One-wound laparoscopic cholecystectomy. Br J Surg. 1997;84:695. [PubMed] [Google Scholar]
- 3. Piskun G, Rajpal S. Transumbilical laparoscopic cholecystectomy utilizes no incisions outside the umbilicus. J Laparoendosc Adv Surg Tech. 1999;9:361–364 [DOI] [PubMed] [Google Scholar]
- 4. Navarra G, La Malfa G, Bartoletta G, Curro G. The invisible cholecystectomy: a different way. Surg Endosc. 2003;22:2103. [DOI] [PubMed] [Google Scholar]
- 5. Kumar M, Agrawal CS, Gupta RK. Three-port versus standard four-port laparoscopic cholecystectomy: a randomized controlled clinical trial in a community-based teaching hospital in eastern Nepal. JSLS. 2007;11(3): 358–362 [PMC free article] [PubMed] [Google Scholar]
- 6. de la Fuente SG, Demaria EJ, Reynolds JD, et al. New developments in surgery: Natural Orifice Transluminal Endoscopic Surgery (NOTES). Arch Surg. 2007;142:295–297 [DOI] [PubMed] [Google Scholar]
- 7. Afthinos JN, Forrester GJ, Binenbaum SJ, Harvey EJ, Kim GJ, Teixeira JA. Single-incision laparoscopic cholecystectomy using flexible endoscopy: saline infiltration gallbladder fossa dissection technique. Surg Endosc. Epub ahead of print 2009 Mar 19 [DOI] [PubMed] [Google Scholar]
- 8. Teixeira J, McGill K, Binenbaum S, Forrester G. Laparoscopic single-site surgery for placement of an adjustable gastric band: initial experience. Surg Endosc. 2009;23(6): 1409–1414 Epub 2009 Mar 14 [DOI] [PubMed] [Google Scholar]
- 9. Podolsky ER, Rottman SJ, King SA, Curcillo PG. Single Port Access Surgery (SPA) Gastrostomy Tube in Patients Unable to receive Percutaneous Endoscopic Gastrostomy Placement. Surg Endosc. 2009;23(5): 1142–1145 Epub 2009 Mar 5 [DOI] [PubMed] [Google Scholar]
- 10. Podolsky ER, Rottman SJ, Poblete H, King SA, Curcillo PG., II Single Port Access (SPA SurgeryTM) Cholecystectomy: a completely transumbilical approach. J Laparoendosc Adv Surg Tech. 2009;19(2): 219–222 [DOI] [PubMed] [Google Scholar]
- 11. Strasberg SM, Hertl M, Soper NJ. Analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180:101–105 [PubMed] [Google Scholar]
- 12. Lee G, Lee T, Dexter D, Godinez C, Meenaghan N, Catania R, Park A. Ergonomic risk associated with assisting in minimally invasive surgery. Surg Endosc. 2009;23(1): 182–188 [DOI] [PubMed] [Google Scholar]
- 13. Manasnayakorn S, Cuschieri A, Hanna GB. Ergonomic assessment of optimum operating table height for hand-assisted laparoscopic surgery. Surg Endosc. 2008;22(8): 1838–1844 [DOI] [PubMed] [Google Scholar]