The incidence of splenic injury may be higher than suggested in the literature. The authors caution against excessive force during colonoscopy and loop formation as splenic injury can occur in a normal spleen without intraperitoneal adhesions.
Keywords: Splenic injury, Colonoscopy, Splenectomy
Abstract
Splenic injury is a rare but serious complication of colonoscopy. Since the mid-1970s, 68 splenic injuries during colonoscopy including our 2 cases have been described. With the increasing use of colonoscopy, endoscopists, surgeons, and radiologists are more likely to encounter this unusual complication. Any cause of increased splenocolic adhesions, splenomegaly, or underlying splenic disease might be a predisposing factor for splenic injury during colonoscopy. However, it can occur in patients without significant adhesions or underlying splenic pathology. The diagnosis is often described in the literature as delayed, because many physicians are not aware of this complication of colonoscopy. Although computerized tomography is highly sensitive, knowledge of this complication is the best tool to aid in early diagnosis. Patients with abdominal pain, hypotension, and a drop in hematocrit without rectal bleeding after colonoscopy should be suspected of having splenic injury. Early recognition and interdisciplinary management are required to assure successful management of this potentially life-threatening injury. Patients with hemodynamic instability most often undergo surgery. We present 2 cases of splenic injury secondary to colonoscopy that required splenectomy.
INTRODUCTION
Colonoscopy has become a routine investigation in the diagnosis and treatment of many colonic diseases. Complications are few and consist mainly of hemorrhage (1% to 2%) and colonic perforation (0.1% to 0.2%). Other rare complications include bacteremia, vasovagal problems, ileus, EKG abnormalities, mesenteric tears, pneumothorax, pneumoperitoneum, pneumoscrotum, and colonic volvulus.1,2,3
Splenic injury after colonoscopy is rare, serious, and may become a lethal complication of the procedure. The most likely mechanism is tension on the splenocolic ligament or on pre-existing adhesions due to manipulations of the colon, or as a result of a direct injury to the spleen during passage through the splenic flexure. Intraperitoneal adhesions or any underlying splenic pathology may increase the risk.
With the increasing use of colonoscopy, physicians should be aware of the rare life-threatening complication of this procedure. We present 2 cases of splenic injury after colonoscopy in which splenectomy was mandatory. We reviewed the world literature by using Pubmed and Medline to identify the mechanism, risk factors, presenting signs and symptoms, preventive measures, and diagnostic and management options.
CASE REPORT 1
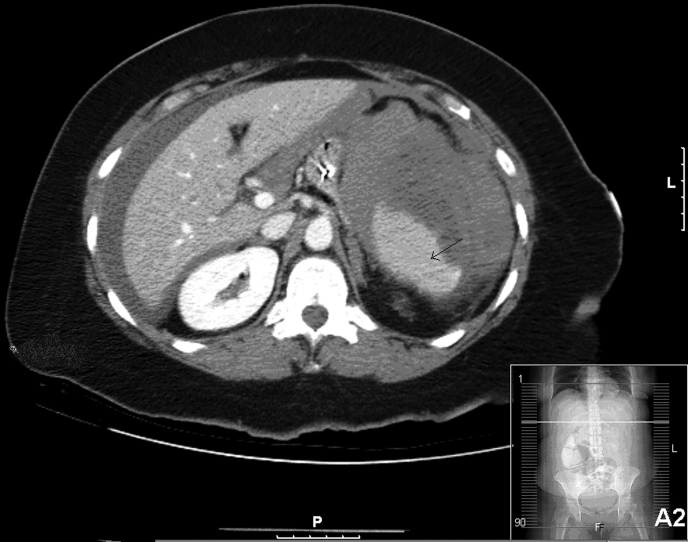
A 56-year-old woman with a past medical history of asthma, cholecystectomy, and hysterectomy, underwent routine screening colonoscopy. Seven polyps were removed in the ascending, transverse, and sigmoid colon without difficulties. Eight hours later, the patient developed severe diffuse abdominal pain that progressively worsened. She returned to the emergency department, where her blood pressure was 70/40 mm Hg, and her heart rate was 120/minute. On physical examination, she had diffuse abdominal tenderness, rebound, and guarding. Her hematocrit dropped to 30 mg/dL from a precolonoscopy value of 41 mg/dL. She was resuscitated with IV crystalloids. CT scan of the abdomen and pelvis revealed splenic injury with a large amount of blood in the left upper quadrant, perihepatic region, and pelvic areas (Figure 1).
Figure 1.
CT abdomen with intravenous and oral contrast. Free perihepatic and perisplenic fluids can be seen, hounsfield density consistent with blood. Arrow point to the medially displaced spleen by the surrounding hematoma.
The patient underwent exploratory laparotomy that revealed 2000 mL of blood and clots in the peritoneal cavity and nonperforated colon. Multiple adhesions were noted between the omentum and the liver, colon, spleen, and stomach. Lysis of adhesions was done, the splenocolic ligament was divided, and the splenic flexure was mobilized. Active bleeding from the splenic hilum was seen, and a splenectomy was performed. Surgical pathology examination showed a ruptured spleen with no underlying splenic pathology. The postoperative course was smooth. The patient remained stable over the course of her hospitalization. She tolerated an oral diet on the second postoperative day and was discharged home after receiving postsplenectomy vaccinations on the fourth postoperative day with an uneventful postoperative recovery.
CASE REPORT 2
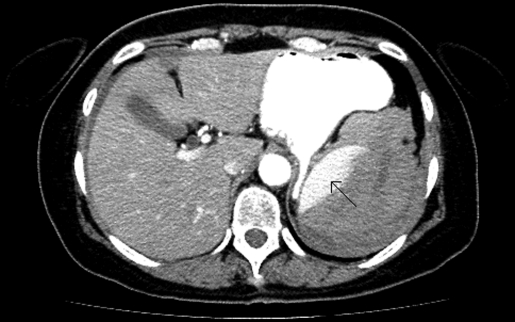
A 55-year-old woman with no significant past medical history underwent a routine screening colonoscopy. Two small flat polyps were removed from the hepatic flexure, and one sessile polyp was removed from the cecum. Twelve hours later, she presented to the emergency department with severe abdominal pain, nausea, and vomiting. Her heart rate was 73/minute and blood pressure was 100/50 mm Hg. Her abdomen was soft, distended, and tender in both left lower and left upper quadrants. Her hematocrit on presentation was 39 mg/dL, while it was 44 mg/dL before colonoscopy. CT scan of the abdomen and pelvis showed free intraperitoneal blood with hematoma around the spleen displacing the spleen medially (Figure 2).
Figure 2.
CT abdomen with intravenous and oral contrast. Arrow point to the medially and anteriorly displaced injured spleen with the surrounding hematoma.
Exploratory laparotomy revealed 1500 mL of fresh blood in the peritoneal cavity and 500 mL of clots around the spleen. The splenocolic and renocolic ligaments were divided, and the splenic flexure mobilized. Bleeding was active around the splenic hilum. Splenectomy was performed. The colon and the remaining intraperitoneal organs appeared normal, and no adhesions were seen. Surgical pathology showed a ruptured spleen with no underlying splenic pathology. The patient tolerated the procedure well. She was started on an oral diet on the first postoperative day. She received postsplenectomy vaccinations and was discharged home on the third day after surgery with an uneventful, stable postoperative course.
DISCUSSION
A review of the literature indicates that the first case of splenic injury associated with colonoscopy was reported in 1974,5 and fewer than 70 cases have been reported in the world literature since then.9 The most likely mechanism for this complication is tension on the splenocolic ligament, or on pre-existing adhesions, or on both, due to manipulations of the sigmoid, descending colon, or transverse colon, or due to a more direct effect, occurring during the passage of the endoscope through the splenic flexure resulting in parenchymal tears or avulsion of the spleen.1 Splenic rupture can occur in a normal spleen after a technically demanding colonoscopy. Patients with a history of previous abdominal surgery or trauma are at increased risk for splenic injury due to the presence of splenocolic adhesions. Hematological, infectious, and infiltrative diseases that lead to splenomegaly, inflammatory bowel disease, and pancreatitis increase the risk for splenic rupture after colonoscopy.2 In a review of 8 patients with splenic injury, Petersen et al9 found that loops causing difficulties occurred during the colonoscopy in 4 patients. However, many splenic injuries have occurred in reportedly easy colonoscopies in patients without significant adhesions.6 Other contributing factors to splenic injury include certain techniques used to navigate the splenic flexure, such as the blind advancement of the endoscope past the splenic flexure and hooking the splenic flexure to straighten the left colon.6 Splenic injury has also been reported in association with colonic perforation after colonoscopy and following endoscopic retrograde cholangiopancreatography in 2 case reports.4,7
The most common signs and symptoms are abdominal pain without radiographic evidence of perforation, left shoulder pain, peritoneal irritation, and orthostatic changes. Due to a low index of suspicion, many of the previously reported cases were diagnosed relatively late— up to 10 days after the procedure.8 Viamonte et al4 in a review of 14 patients with splenic injury after colonoscopy observed abdominal pain in 64% of the patients soon after the procedure, and that hemodynamic instability was nearly universally seen. In a review of 8 cases, Petersen et al9 found that all patients were symptom-free after colonoscopy, for 4 hours to 7 days. The diagnosis can be problematic, partly because of the characteristic symptom-free interval and partly because referring physicians or even endoscopists might not be aware of this unusual complication of the procedure.
CT scan is highly accurate for detecting splenic injury and the extent of hemoperitoneum. This examination is considered the diagnostic modality of choice in a stable patient.6 Espinal et al6 in a review of 17 cases found 8 patients were diagnosed by CT scan, 6 by laparotomy, and 1 each by angiography, ultrasound, and autopsy. Although splenectomy is required in the majority of cases, observation or splenorrhaphy may be options in select cases.6 The nonoperative approach is usually taken in patients with no intraperitoneal blood, a closed subcapsular hematoma, and a stable hemodynamic status.3
Preventive measures include good colonoscopy technique to avoid loop formation and to avoid the use of excessive force.9 The left lateral position of the patient may reduce the risk of splenic injury after colonoscopy compared with the supine position. It is reasoned that the supine position exerts opposing forces on the spleen from gravity and traction. This leads to an increase in the splenic capsule tear, especially if other predisposing factors are present, such as previous abdominal surgery. It has been suggested that the effect of these forces might decrease in the left lateral position.10
In both of our cases, the colonoscopy was uneventful; presentation was within 12 hours after the procedure, and the CT scan demonstrated splenic injury. Conservative management was not an option in either case due to the presence of active bleeding and a large amount of free intraperitoneal blood. Of note is that neither of the 2 patients had primary splenic pathological disease that might account for rupture. One of the patients had dense adhesions from a previous surgery.
CONCLUSION
The incidence of splenic rupture after colonoscopy may be higher than suggested in the literature, as many authors are not eager to publicize their morbidity. The endoscopist should suspect splenic injury after colonoscopy in a patient who develops abdominal pain and tenderness without any evidence of bowel perforation or rectal bleeding with or without hemodynamic instability. Excessive force and loop formation should be avoided during colonoscopy. Although patients with intraperitoneal adhesions and those with underlying splenic pathology have a greater chance of experiencing this complication, splenic injury can occur in a normal spleen and without intraperitoneal adhesions. Exploratory laparotomy should be considered for unstable patients and those with active bleeding in the peritoneal cavity. In our 2 cases, the spleen could not be preserved, and splenectomy was mandatory because the injury could not be managed using conservative techniques. In a stable patient, abdominal CT scan is advisable to help in the diagnosis and to select those patients who may be managed conservatively.
Contributor Information
Mohammad Sarhan, Department of Surgery, Harlem Hospital Center, New York, New York, USA..
Alexius Ramcharan, Department of Surgery, Harlem Hospital Center, New York, New York, USA.; Columbia University, New York, New York, USA.
Sarma Ponnapalli, Woodhull Medical Center, New York, New York, USA..
References:
- 1. Levine E, Wetzel LH. Splenic trauma during colonoscopy. AJR Am J Roentgenol. 1987;149(5): 939–940 [DOI] [PubMed] [Google Scholar]
- 2. Tuso P, McElligott J, Marignani P. Splenic rupture at colonoscopy. J Clin Gastroenterol. 1987;9(5): 559–562 [DOI] [PubMed] [Google Scholar]
- 3. Prowda JC, Trevisan SG, Lev-Toaff AS. Splenic injury after colonoscopy: conservative management using CT. AJR Am J Roentgenol. 2005;185(3): 708–710 [DOI] [PubMed] [Google Scholar]
- 4. Viamonte M, Wulkan M, Irani H. Splenic trauma as a complication of colonoscopy. Surg Laparosc Endosc. 1992;2(2): 154–157 [PubMed] [Google Scholar]
- 5. Wherry DC, Zehner H., Jr Colonoscopic fiberoptic colonoscopic approach to the colon and polypectomy. Med Ann DC. 1974;43:189–192 [PubMed] [Google Scholar]
- 6. Espinal EA, Hoak T, Porter JA, Slezak FA. Splenic rupture from colonoscopy. A report of two cases and review of the literature. Surg Endosc. 1997;11(1): 71–73 [DOI] [PubMed] [Google Scholar]
- 7. Lo AY, Washington M, Fischer MG. Splenic trauma following endoscopic retrograde cholangiopancreatography. Surg Endosc. 1994;8:692–693 [DOI] [PubMed] [Google Scholar]
- 8. Reissman P, Durst AL. Splenic hematoma, a rare complication of colonoscopy. Surg Endosc. 1998;12(2): 154–155 [DOI] [PubMed] [Google Scholar]
- 9. Petersen CR, Adamsen S, Gocht-Jensen P, Arnesen RB, Hart-Hansen O. Splenic injury after colonoscopy. Endoscopy. 2008;40(1): 76–79 [DOI] [PubMed] [Google Scholar]
- 10. Tse CC, Chung KM, Hwang JS. Splenic injury following colonoscopy. HONG KONG Med J. 1999;5(2): 202–203 [PubMed] [Google Scholar]