Abstract
We describe a patient with rhabdomyolysis and acute renal dysfunction due to hypothyroidism, attributed to Hashimoto's disease. Though rhabdomyolysis could be life-threatening, it is a rare complication of hypothyroidism, especially when other precipitating factors, such as exercise, alcohol, medications or renal failure, are absent. Nevertheless, hypothyroidism can be an authentic cause of rhabdomyolysis and should always be considered when elevated creatine kinase (CK) and other muscle enzymes concentrations cannot be attributed to any major factor.
Keywords: Hashimoto's disease, hypothyroidism, renal dysfunction, rhabdomyolysis
Hypothyroidism has a broad spectrum of clinical findings. The manifestations of myopathy, or even myositis, such as muscle weakness, myalgias, muscle stiffness or tenderness, are common among hypothyroid patients1. Sometimes muscle enzymes are moderately elevated. On the other hand, rhabdomyolysis due to hypothyroidism is rare, and is usually exacerbated by exercise, lipid-lowering drugs, alcohol and renal failure2. Only a few cases of overt rhabdomyolysis caused by hypothyroidism alone have been reported2–5. We report such a case of rhabdomyolysis, without the presence of any precipitating factors, in a patient subsequently diagnosed with thyroiditis Hashimoto and hypothyroidism.
Case presentation
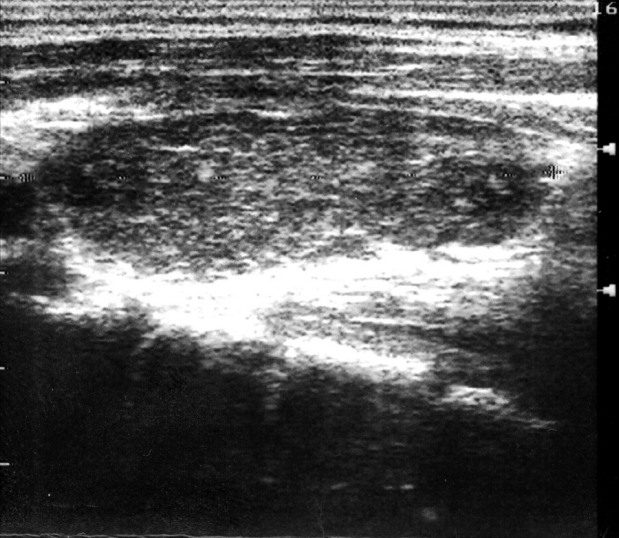
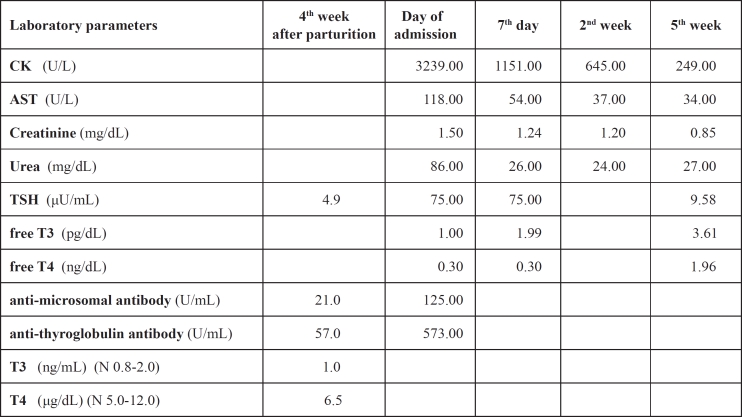
A 41 year-old woman presented to the hospital with a one-month history of proximal muscle weakness of the extremities and muscle cramps. She also referred a sixmonth history of generalized body swelling, sleepiness, hair loss, weight gain, constipation, and a three-month history of amenorrhea and a hoarse voice. She gave birth to her second child seven months ago. The patient was under no medications, had no recent event of muscle injury or surgical operation, and denied any familial or prior personal history of thyroid or autoimmune disease and muscle disorder. On admission, she had generalized oedema of the face and body, diffuse alopecia, a dry coarse skin, and diffuse goitre. Her heart rate, blood pressure and electocardiographic findings were normal. The laboratory findings were the following: creatine kinase (CK) 3239 U/L (normal 38-174), AST 118 U/L, ALT 89 U/L, LDH 704 U/L, myoglobin 150 µg/L (normal 14,3-65,8), aldolase 17,5 U/L (normal 1,3-8,2), serum creatinine 1,5 mg/dL, urea 86 mg/dL, total cholesterol 402 mg/dL. Thyroid-stimulating hormone (TSH) levels were markedly elevated (75,00 µU/mL, normal 0,40-4.00), plasma concentrations of free T3 and free T4 were decreased (1,00 pg/dL and 0,30 ng/dL respectively, normal 1,8-4,2 and 0,8-1,9), with elevated titers of the anti-microsomal antibody (TPOAb: 125 U/mL, normal <60) and of the anti-thyroglobulin antibody (TgAb: 573 U/mL, normal <60). Hormonic and immunologic control of the thyroid a month after labor, were normal. Urine analysis was positive for blood, with only 0-1 erythrocytes per optical field (myoglobinuria). All the above findings led to the diagnosis of rhabdomyolysis, as a result of hypothyroidism due to autoimmune thyroiditis. The final diagnosis of Hashimotos disease was based on the following points: a) The presence of a diffuse, firm goiter. b) Normal titers of anti-microsomal and antithyroglobulin antibodies a month after parturition. c) The ultrasonographic findings: enlarged thyroid gland, mixed echogenicity, interspersed small hypoechogenic lumps and moderately increased vascularity. d) Diffuse uptake in an enlarged gland on the radioisotopic scan. (Japan Thyroid Association - Guidelines for the Diagnosis of Chronic Thyroiditis). The patient was treated with intravenous fluids, alkalization of the urine and received thyroxine replacement. On discharge, two weeks after admission, she was clinically improved. Her CK, AST and ALT levels dropped to 645 U/L, 37 U/L and 30 U/L respectively, while her kidney function was normal. She was re-evaluated three weeks after discharge: muscle enzyme values and total cholesterol levels were normalized, free T3 and free T4 presented normal concentrations, while TSH was significantly decreased, but still remained high (9,58 µU/mL).
Discussion
Rhabdomyolysis, or muscular lysis, is a syndrome caused by any damage or injury that results in the desruption of the sarcolemma of skeletal muscles, and the leakage of quantities of intracellular myocyte components, such as myoglobin, CK, electrolytes and uric acid, into plasma. It is characterized by the triad: muscle weakness, myalgias and dark urine (due to myoglobin), although it isn't necessary for all three to be present. The causes of rhabdomyolysis can be divided into inherited (enzyme deficiencies) and acquired, such as muscle trauma and compression, ischemic injury, bacterial and viral infections, inflammatory myopathies, drugs and myotoxins, alcohol, exertional activity, heat-related syndromes, cold exposure, and metabolic disorders6,7. CK levels suggest rhabdomyolysis when they are five times higher than the reference level4. It should be mentioned that rhabdomyolysis can be life-threatening, as it could result in acute renal failure, compartment syndrome, disseminated intravascular coagulation, electrolyte abnormalities and cardiac arrest.
Early diagnosis and treatment is important. Acute renal failure is the most severe complication of rhabdomyolysis. Approximately one third of patients presenting with rhabdomyolysis will develop renal failure, if they are not carefully treated. The mechanisms that can lead to acute renal failure in patients with rhabdomyolysis include: a) renal vasoconstriction and subsequent ischemia, b) intraluminal obstruction by myoglobin and uric acid cylinders, which are formated under conditions of acid urine pH, and c) ferrihemate direct nephrotoxicity6,7.
Hypothyroidism has been associated with myopathy, myositis and muscle enzyme elevations1. CK levels are usually high, but lower than ten times up the reference level3,6. Hypothyroidism has been recognised as a genuine risk factor for rhabdomyolysis, when other aggravating factors, such as statins or intensive exercise, are also present. Hashimotos disease, as cause of rhabdomyolysis, has been described only in one other case3. The true cause of rhabdomyolysis in hypothyroidism still remains unclear. A reversible defect in glycogenolysis, as well as a probable mitochondrial metabolism impairment, due to low mitochondrial enzyme activity1,8 have been implicated.
Figure 1. Ultrasound of the thyroid gland of our patient: enlarged gland, mixed echogenicity, small hypoechogenic lumps, moderately increased vascularity.
Table 1. Main laboratory parameters of our patient: one month after parturition. the day of admission in the hospital. in the middle of hospitalization (7th day). on discharge (2nd week) and during follow-up (5th week). N=normal.
References
- 1.Madariaga MG, Gamarra N, Dempsey S, Barsano CP. Polymyositis-Like Syndrome in Hypothyroidism: Review of Cases Reported Over the Past Twenty-Five Years. Thyroid. 2002;12:331–336. doi: 10.1089/10507250252949478. [DOI] [PubMed] [Google Scholar]
- 2.Barahona MJ, Mauri A, Sucunza N, Paredes R, Wägner AM. Hypothyroidism as a Cause of Rhabdomyolysis. Endocrine Journal. 2002;49:621–623. doi: 10.1507/endocrj.49.621. [DOI] [PubMed] [Google Scholar]
- 3.Jobι J, Corman V, Fumal A, Maertens de Noordhout A, Legros JJ. Rhabdomyolysis and hypothyroidism. Rev Med Liege. 2007;62:484–486. [PubMed] [Google Scholar]
- 4.Altay M, Duranay M, Ceri M. Rhabdomyolysis due to hypothyroidism. Nephrol Dial Transplant. 2005;20:847–848. doi: 10.1093/ndt/gfh745. [DOI] [PubMed] [Google Scholar]
- 5.Rabhi M, Chaari J, Toloune F. Rhabdomyolysis disclosing Hypothyroidism. Europ J Intern Med. 2006;17:220. doi: 10.1016/j.ejim.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 6.Bosch X, Poch E, Grau JM. Rhabdomyolysis and acute kidney injury. N Engl J Med. 2009;361:62–72. doi: 10.1056/NEJMra0801327. [DOI] [PubMed] [Google Scholar]
- 7.Efstratiadis G, Voulgaridou A, Nikiforou D, Kyventidis A, Kourkouni E, Vergoulas G. Rhabdomyolysis updated. Hippokratia. 2007;11:129–137. [PMC free article] [PubMed] [Google Scholar]
- 8.Kaminsky P, Robin-Lherbier B, Brunotte F, Escanye JM, Walker P, Klein M, et al. Energetic metabolism in hypothyroid skeletal muscle, as studied by phosphorus magnetic resonance spectroscopy. J Clin Endocrinol Metab. 1992;74:124–129. doi: 10.1210/jcem.74.1.1727810. [DOI] [PubMed] [Google Scholar]