Results of this study suggest that ultrasound can be used to quantitatively estimate the degree of adhesions between intestine and the abdominal wall.
Keywords: Ultrasound, Adhesion, Laparoscopy, Surgery
Abstract
Background and Objectives:
Laparoscopic treatment of incisional hernias reduces surgical traumas and postoperative pain. It requires intraperitoneal placement of a foreign body that might cause adhesions, leading to postoperative complications. The aim of this study was to improve reliability of ultrasound in quantitatively estimating adhesions to exploit the other advantages of ultrasound, such as availability and versatility.
Methods:
The ultrasound examination was performed by using a hand-held 3.5MHz curved linear probe. The image data were analyzed prior to scan conversion. Two square regions of interest were defined, one in the abdominal wall and one in the underlying bowels. A cross correlation-based algorithm tracked each region by using a time span of 3 frames. Subtracting the 2 displacement functions from each other yielded a relative displacement function, indicating the degree of bowel adhesions. This was compared with the intraoperative findings.
Results and Conclusions:
The method was proven to be a rapid and robust method for quantitatively estimating the degree of bowel adhesions. It is limited to evaluation of adhesions between bowel and abdominal wall. However, this ultrasound technique could assist in the safe placement of ports prior to redo laparoscopic surgery.
INTRODUCTION
Abdominal surgeries are reported to cause incisional hernias in 3% to 29% of patients.1,2 Incisional hernias are treated surgically by the implantation of wall reinforcement either in the extraperitoneal or intraperitoneal space. Intraperitoneal positioning is gaining in popularity, mainly due to the associated reduction of postoperative complications. However, it may cause problems by generating postoperative adhesions.
The incidence of intraperitoneal adhesions ranges from 67% to 93% after general surgical abdominal operations.3,4 Approximately one-third of the patients undergoing intraabdominal surgery are later readmitted to the hospital for problems possibly related to these adhesions.5,6 One of every 20 patients needs to be reoperated on for problems related to adhesions.7 Adhesion formation therefore presents a considerable burden to health care and society and is associated with high workloads for hospitals and high costs.
Adhesions are the main reason for the development of chronic abdominal or pelvic pain after surgery.8 In addition, adhesion formation may complicate re-entry of the abdominal cavity at subsequent intraabdominal surgeries and may be responsible for complications during these procedures, such as bowel perforation. Also, a laparoscopic approach may be impossible in certain cases due to severe adhesions, and conversion to open surgery might be necessary.
Laparoscopic surgery offers several benefits to the patients, such as a shorter recovery period and in-hospital stay, less postoperative pain, and improved cosmetics. There are also several ways in which a minimally invasive surgery (MIS) approach may reduce adhesion formation: (1) it reduces injury and ischemia to the peritoneum due to a more gentle manipulation of tissues, and (2) it reduces the exposure to foreign particles, such as powder from gloves and gauze particles. In addition, a laparoscopic approach prevents drying of the peritoneal surface, which has also been related to adhesion formation.9 Furthermore, bowel recovery is quicker after MIS. The normal activity and movement of the bowel after MIS can thus reduce adhesion formation by mechanically separating the fibrinous strands between the injured surfaces. This benefit, however, may be cancelled by the introduction of a foreign body, as is the case in laparoscopic hernia repair (Figure 1).
Figure 1.
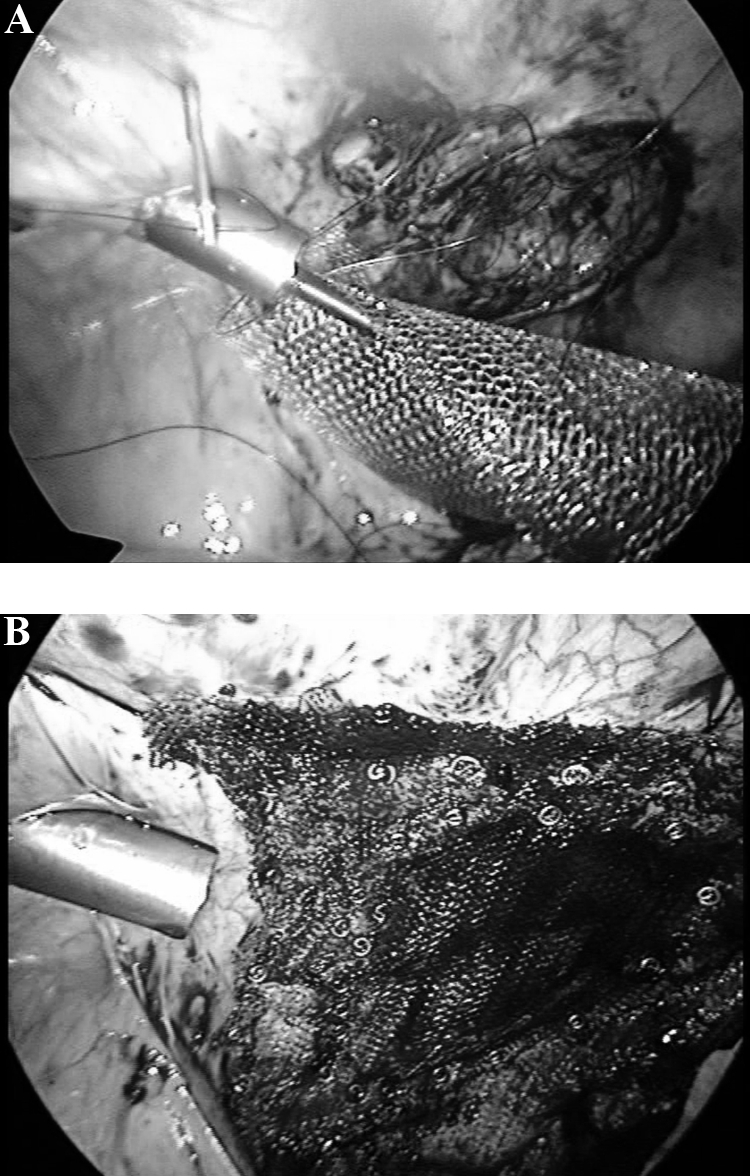
The sequence of endoscopic images (freeze frames of video) shows laparoscopic hernia repair, (a) lifting the mesh up to cover the hernia and (b) after attaching the mesh.
Estimating intraabdominal adhesion formation is of interest as a diagnostic tool, but also when evaluating the efficacy of intraabdominal prosthetic materials in the treatment of incisional hernias. Furthermore, detecting adhesions may decrease the risk of bowel injury during re-do laparoscopy.
Ultrasound imaging (USI) and magnetic resonance imaging (MRI) are the noninvasive methods hitherto described to detect adhesions.10–14 MRI seems to yield good results, but it is expensive and cumbersome to use. Furthermore, the methods reported in the literature rely only on a rough visual estimation of the degree of adhesion. These manual methods are often tedious and prone to interuser variability. A potential advantage of the MRI-based techniques is the fact that this method can be used to detect adhesions in the entire abdominal cavity. In practice however, this demands a full 3D abdominal scan and demands a lot of time for the operator to examine the whole data set. MRI can be used to detect not only adhesions to the abdominal wall but also those between the bowels. A quantitative method based on ultrasound15 reports localization of adhesions. However, it relies on visual tracking of the bowel displacements. The aim of this study was to improve reliability and accuracy of ultrasound in quantitatively estimating adhesions, to exploit the other advantages of USI, such as availability, versatility, and real-time imaging capabilities.
MATERIALS AND METHODS
Patients and Examination
The study included 7 patients scheduled for open abdominal surgery. All patients had previously undergone abdominal surgery. An ultrasound examination was performed less than one day before surgery. The surgical department of the University Hospital in Trondheim approved the project. Informed consent was obtained from the patients before ultrasound scanning. No data that could identify the patients were stored.
We used a hand-held curved linear array (CLA) probe on a GE Vivid 7 scanner (GE Vingmed Ultrasound, Norway). The abdomen was scanned systematically in 9 sectors as indicated in Figure 2. The degree of adhesion was classified according to a scale from 0–3, 0 being no adhesion, 1 being a few adhesions, 2 being some, and 3 signifying severe adhesion. The array was 1.5 dimensional (1.5D), thus allowing for dynamic elevation focusing. Several transmit focus points were used over the imaging depth, typically 3 foci distributed over 4-cm to 6-cm imaging depth and 90° wide sector. For further optimizing image quality, Harmonic imaging was used with a transmitting frequency 3.5MHz and receiving at 7MHz. The images were acquired in the sagittal plane during normal breathing, which was the driving force for the bowel displacements. The various areas of the abdomen that were scanned are shown in Figure 2. The width and depth of the sector were adjusted to include abdominal organs, such as the bowel. Using these settings, frame rates of 40 images to 50 images per second were obtained.
Figure 2.
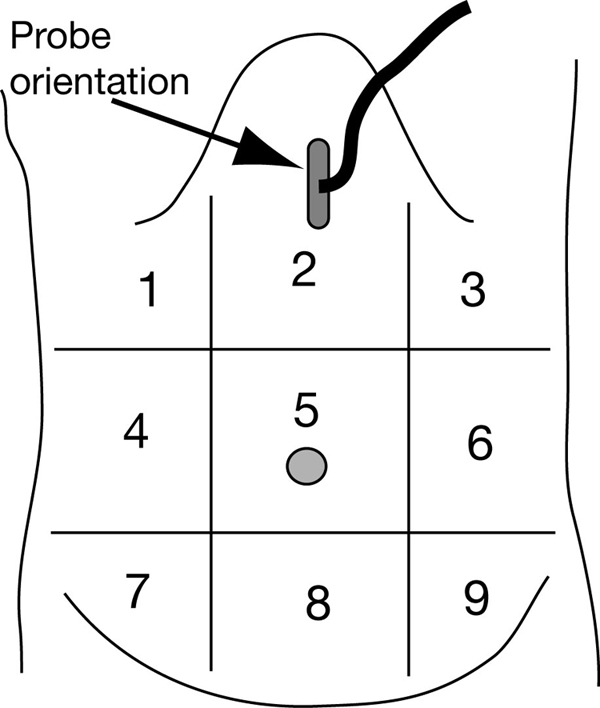
The illustration shows the zones of ultrasound scanning on the abdomen and the orientation of the ultrasound probe during scanning.
During surgery, the surgeon noted the degree of adhesion in the areas previously scanned by ultrasound by direct visual inspection (Figure 3). These findings were used when assessing the quality of the ultrasound method.
Figure 3.

(a) an area with no adhesion and (b) severe adhesions between the abdominal wall and the bowel.
The surgeon was unaware of the scores from ultrasound scanning during scoring in the OR the day after. Two 2 data sets were excluded, because the recordings could not be performed in a manner allowing further processing.
Ultrasound Processing
To ensure the homogeneity of the information density during the mathematical processing, the image data were analyzed before scan conversion. Two square regions of interest (ROI) were manually defined, one in the abdominal wall and one in the underlying bowels as shown in Figure 4, which also shows an illustration of the different layers of the abdomen visible in the ultrasound image. Some structures are naturally more apparent with a live scanning view, and, hence, not easily discernable on the still image shown here. The size of the ROI was set to 60x60 pixels in ultrasound beam space.
Figure 4.
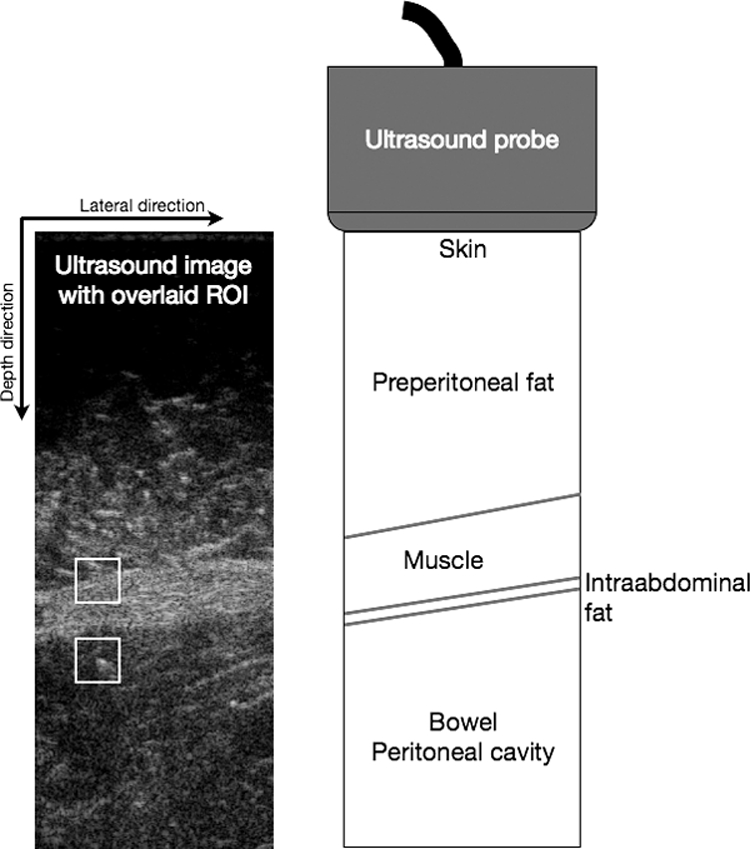
The ultrasound image contains overlays of the defined ROIs, the top one set in the abdominal wall and the lower ROI set in the underlying bowel. The drawing indicates the various structures covered by the image.
A cross correlation-based algorithm was implemented in MATLAB (MathWorks Inc.) and used for tracking each ROI over a breath cycle. The correlation coefficients were calculated as
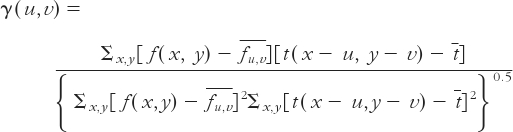 |
where f(x,y) is the search region,  is the mean of the search region under the template, t(x,y) is the template and
is the mean of the search region under the template, t(x,y) is the template and  its average. Each square ROI of side length 2a (template) was cross-correlated with a square of the same center and padded with a in every direction, called search region taken from frame number n-3. Given the discrete nature of the data, whenever the maximum of correlation occurred less than one pixel off center, the algorithm detected no displacement at all between the 2 frames. To overcome this, the template and the search region were 3 time frames apart, and the resulting displacement was weighted with one-third. This feature improved the continuity of the velocity function similar to a moving average.
its average. Each square ROI of side length 2a (template) was cross-correlated with a square of the same center and padded with a in every direction, called search region taken from frame number n-3. Given the discrete nature of the data, whenever the maximum of correlation occurred less than one pixel off center, the algorithm detected no displacement at all between the 2 frames. To overcome this, the template and the search region were 3 time frames apart, and the resulting displacement was weighted with one-third. This feature improved the continuity of the velocity function similar to a moving average.
The algorithm was implemented so that the ROI tracked at each point in time is fixed in the ultrasound field. This provides a Eulerian description of the velocity at a spatial position rather than for a material point. The velocity is however integrated for an imaginary material point, thus neglecting tissue strain over the distance between the location of the material point and the ROI. This assumption seems reasonable as the tissue is almost incompressible and the rigid body motion considerable.
The displacements thus calculated are given in pixels and can be converted into millimeters using the scan conversion parameters stored during the imaging of the patient. The relative displacement of the 2 ROIs will have components in 2 directions. However, only the lateral direction (Figure 4) carries information relevant to the estimation of adhesions. Therefore, the displacements calculated at the depth of each ROI are simply multiplied by a factor proportional to its distance to the virtual origin of the ultrasound sector. Subtracting the 2 displacement functions from each other yielded a relative displacement function, the span of which was the primary quantitative estimator of bowel adhesion.
The peak amplitude of the relative displacement can be used as a measurement of the freedom of movement between peritoneum and bowels. But because peak values are sensitive to noise and numeric errors, the final relative displacement is further smoothed with a Fourier low pass filter, preserving only the 8 lowest frequencies.
RESULTS
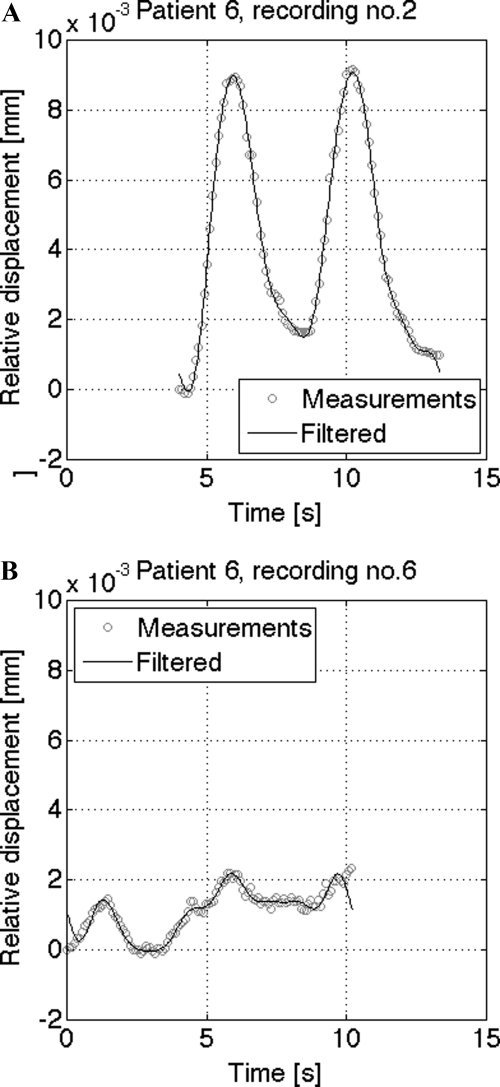
Images from areas with varying degrees of adhesion were acquired in all patients. Naturally, all patients had areas of no adhesion, while only 2 of the 7 pilot cases did not show the highest degree of adhesion according to surgical scoring during the intervention, which was set to 3 on a scale from 0 to 3, as described above. Zero signified free relative movement between the bowel and the abdomen (Figure 5A), while 3 implied no relative movement (Figure 5B).
Figure 5.
Patient with surgical score of 0 (no adhesions) and with a surgical score of 3 (severe adhesion).
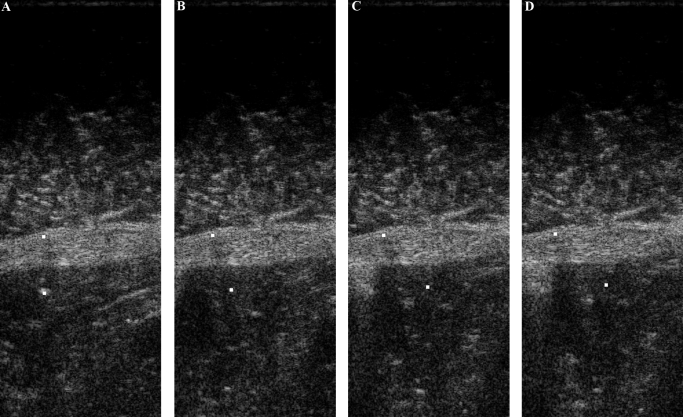
From the image sequence shown in Figure 6, it can be seen how the ROI follows the bowel movement. It should be emphasized that such a depiction is difficult to show without the live ultrasound view of the recorded ultrasound sequence, but structures in the upper half can be seen to be consistent throughout, while the lower ROI moves to the right, and the image in the lower half varies more.
Figure 6.
Tracking of the region of interest, marked by white dot moums to the right over a breathing cycle, in the bowel.
The computation time was approximately 80 seconds for 13 seconds of ultrasound recording (400 frames) using Matlab R2009a (The Mathworks) on a MacBook Pro 2.4 GHz Intel Core 2 Duo with 4GB memory.
DISCUSSION
These preliminary results indicate a good correlation between estimated degree of ultrasound-detected adhesions and intraoperative findings. This method is limited to adhesions affecting the abdominal wall. Adhesions between loops of the bowel and intraabdominal organs cannot be judged by this method. Keeping this in mind, there are clinical settings in which ultrasound estimated adhesions are of interest. Adhesions after an intraabdominally placed prosthesis are of particular interest. It is conceivable that these might be followed longitudinally, as these probably change over time, at least with regard to density.
A key advantage of the method presented here is that the evaluation of the degree of adhesion is less user-dependent. A few parameters still play a certain role as the placement of the ultrasound transducer at a right angle (roll and pitch) to the surface of the abdomen, and the recognition of the abdominal wall for the placement of the regions of interest. However, these parameters do not require advanced training in ultrasound scanning. Evaluation of adhesions could thus be performed by less-trained personnel, relieving the surgeon's workload.
Other groups that have published results from ultrasound-based detection of abdominal adhesions often perform this based on induced viscera slide, such as deep inspiration or manual compression.15 We were able to detect the adhesions, not only with a semi-automatic setup, but also with the patients breathing in a normal manner, acquiring data over several breath cycles.
The image analysis method detects a relative displacement between the abdominal wall and the underlying bowel. However, it does not take into account the driving force for the motion. Although the patients were instructed to breathe normally, the displacement created by the diaphragm may vary strongly from patient to patient. Shallow breathing may initiate small motions that are discarded by the image analysis. Additionally, the angle of the ultrasonic plane may reduce the amplitude of the calculated displacement. Further work is required to standardize those factors and statistically assess the clinical validity.
Compared with MRI techniques for detecting adhesions, ultrasound is an easily available, flexible, and real-time imaging modality that can be used by the surgeon before a procedure. Ultrasound may be used to plan the procedure, ie, the operator can safely plan the position of the first trocar and modify its position according to adhesions to avoid damage to the bowel, especially in case of severe adhesions periumbilically.16 Locating postoperative adhesions preoperatively might reduce the risk of injury to intraabdominal organs, both in open and laparoscopic approaches.
The gold standard was the scores provided by the surgeon in the operating room. We are aware that the same surgeon performed the ultrasound scans as well as the scores based on direct visual inspection during surgery. However, we believe that this is not of great significance, because this is a method of development and validation (pilot) mainly, the scores during ultrasound scanning were provided the day before surgery, and several zones were logged for adhesion values. In other words, during the surgical procedure, it was rather difficult for the surgeon to remember the scores assigned during ultrasound scanning the day before. In our clinical validation and follow-up studies, these procedures will be performed by 2 different persons, thus removing the possible inherent bias.
CONCLUSION
The method was proven to be a rapid and robust method for quantitatively estimating the degree of bowel adhesion after intraabdominal surgery. Based on visual inspection, we verified that each ROI correctly followed the bowel movement and the abdominal wall. The correspondence between the degrees of adhesion as stated by the surgeon performing the ultrasound scans, the values given by the surgeon performing the surgical procedure, and the numeric results of our algorithm were high. Hence, the use of preoperative transabdominal USI seems to be a useful technique to identify intraabdominal adhesions before surgery in patients with previous open abdominal surgical procedures. We believe that further development and a widespread application of this technique in patients with previous abdominal surgery may decrease trocar-related injuries during laparoscopic access and serve as a method for evaluating adhesion formation after intraabdominal positioned prosthetic materials in the treatment of incisional hernias.
Contributor Information
Sebastien Muller, SINTEF Health Research, 7465 Trondheim, Norway..
Thomas Langø, SINTEF Health Research, 7465 Trondheim, Norway..
Reidar Brekken, SINTEF Health Research, 7465 Trondheim, Norway..
Brynjulf Ystgaard, St. Olavs Hospital, Surgical Department, 7006 Trondheim, Norway..
References:
- 1. Cengiz Y, Israelsson LA. Incisional hernias in midline incisions: an eight-year follow up. Hernia. 1998;2:175–177 [Google Scholar]
- 2. Turner PL, Park AE. Laparoscopic repair of ventral incisional hernias: pros and cons. Surg Clin North Am. 2008;88(1):85–100 [DOI] [PubMed] [Google Scholar]
- 3. Liakakos T, Thomakos N, Fine PM, Dervenis C, Young RL. Peritoneal adhesions: etiology, pathophysiology, and clinical significance. Dig Surg. 2001;18(4):260–273 [DOI] [PubMed] [Google Scholar]
- 4. Adye B, Luna G. Incidence of abdominal wall hernia in aortic surgery. Am J Surg. 1998;9(175):400–402 [PubMed] [Google Scholar]
- 5. Ellis H, Moran BJ, Thompson JN, et al. Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet. 1995;3533(9163):1476–1480 [DOI] [PubMed] [Google Scholar]
- 6. Lower AM, Hawthorn RJ, Ellis H, O'Brien F, Buchan S, Crowe AM. The impact of adhesions on hospital readmissions over ten years after 8849 open gynaecological operations: an assessment from the Surgical and Clinical Adhesions Research Study. BJOG. 2000;107(7):855–862 [DOI] [PubMed] [Google Scholar]
- 7. Ellis H, Moran BJ, Thompson JN, et al. Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet. 1999;353(9163):1476–1480 [DOI] [PubMed] [Google Scholar]
- 8. Swank DJ, van Erp WFM, Repelaer van Driel OJ, Hop WCJ, Bonjer HJ, Jeekel H. A prospective analysis of predictive factors on the results of laparoscopic adhesiolysis in patients with chronic abdominal pain. Surg Laparosc Endosc Percutan Tech. 2003;13(2):88–94 [DOI] [PubMed] [Google Scholar]
- 9. Yesildaglar N, Koninckx PR. Adhesion formation in intubated rabbits increases with high insufflation pressure during endoscopic surgery. Hum Reprod. 2000;15(3):687–691 [DOI] [PubMed] [Google Scholar]
- 10. Aube C, Pessaux P, Tuech JJ, et al. Detection of peritoneal adhesions using ultrasound examination for the evaluation of an innovative intraperitoneal mesh. Surg Endosc. 2004;18(1):131–135 [DOI] [PubMed] [Google Scholar]
- 11. Fischer T, Ladurner R, Gangkofer A, Mussack T, Reiser M, Lienemann A. Functional cine MRI of the abdomen for the assessment of implanted synthetic mesh in patients after incisional hernia repair: initial results. Eur Radiol. 2007;17(12):3123–3129 [DOI] [PubMed] [Google Scholar]
- 12. Mussack T, Fischer T, Ladurner R, et al. Cine magnetic resonance imaging vs high-resolution ultrasonography for detection of adhesions after laparoscopic and open incisional hernia repair: a matched pair pilot analysis. Surg Endosc. 2005;19(12):1538–1543 [DOI] [PubMed] [Google Scholar]
- 13. Lang RA, Buhmann S, Hopman A, et al. Cine-MRI detection of intraabdominal adhesions: correlation with intraoperative findings in 89 consecutive cases. Surg Endosc. 2008;22(11):2455–2461 [DOI] [PubMed] [Google Scholar]
- 14. Bingener J, Kazantsev GB, Chopra S, Schwesinger WH. Adhesion formation after laparoscopic ventral incisional hernia repair with polypropylene mesh: a study using abdominal ultrasound. JSLS. 2004;8:127–131 [PMC free article] [PubMed] [Google Scholar]
- 15. Sigel B, Golub RM, Loiacono LA, et al. Technique of ultrasonic detection and mapping of abdominal wall adhesions. Surg Endosc. 1991;5(4):161–165 [DOI] [PubMed] [Google Scholar]
- 16. Steitz H-O, Lang RA, Meimarakis G, Schildberg FW. Validity of sonographic evaluation of adhesions. Chir Praxis. 2003;61:579–584 [Google Scholar]