Abstract
This presentation reviews the literature regarding the current surgical treatment of perforated ulcers, describes the surgical techniques for laparoscopic repair, and reviews the clinical algorithm used by laparoscopic surgeons at Duke University Medical Center.
Keywords: Laparoscopy, Perforated duodenal ulcer
INTRODUCTION
The presentation of a patient with a perforated duodenal ulcer requires that a surgeon make a series of clinical decisions. In 1992, Feliciano1 described 5 decisions facing the surgeon in this situation. Those decisions are as follows: (1) Is the performance of an operation indicated? (2) Is an omental plication sufficient or is a definitive ulcer operation indicated? (3) Is the patient stable enough to undergo a definitive ulcer operation? (4) Which definitive ulcer operation is indicated? (5) Should the availability of newer medical options influence the choice of operation? The successful development of advanced laparoscopic skills and procedures during the past decade begs a sixth question: (6) Should the procedure be performed laparoscopically or by laparotomy?
Sixty-two years ago, Roscoe Graham in a landmark treatise “A Surgeon's Problem in Duodenal Ulcer” declared duodenal ulcer to be not a local disease but a local manifestation of a constitutional disturbance. He highlighted 3 factors that would affect the treatment outcome of perforated duodenal ulcers: correction of the biochemical disturbance caused by the perforation and peritonitis, subsequent surgery to close the acute perforation, and a well-regulated medical regimen.2 Over the years, with improved understanding of the pathogenesis of duodenal ulcers and with phenomenal advances in surgical expertise, intensive care and pharmacological management, the basic principles remain unchanged. If the goal of surgery is simple closure of the perforated duodenal ulcer and if this can be achieved safely with minimally invasive techniques, it is no doubt the desired approach. Since the first description of laparoscopic management of perforated duodenal ulcer in 1990,3 several studies have sought to determine the feasibility and safety of this approach.4–8 This presentation reviews the current literature, the various laparoscopic techniques, and the recommendations for successful management of a perforated duodenal ulcer.
INCIDENCE OF PEPTIC ULCER DISEASE AND ITS COMPLICATIONS
The incidence of peptic ulcer disease has declined over the past few years following a more streamlined pharmacological intervention. This can be attributed to the efficiency of histamine2 (H2) blockers and proton pump inhibitors. Additionally, the diagnosis and eradication of Helicobacter pylori (H. pylori) infection, now known to be a major factor in the pathogenesis of peptic ulcer disease, has almost eliminated the role of surgery in the elective management of peptic ulcer disease. However, the incidence of perforated duodenal ulcers has either remained the same9 or has been increasing with the resultant increase in the incidence of emergency surgery.10 Although the use of potent H2 blockers and proton pump inhibitors has caused a marked decline in the incidence of peptic ulcer perforation, no such decline has been seen in the eradication of H. pylori infection.11 Patients with perforated duodenal ulcers include those with acute ulcers, such as patients on nonsteroidal anti-inflammatory drugs (NSAIDs) and those with chronic ulcer disease who are refractory to or noncompliant with medical treatment. Another contributing factor to the increased incidence of complications of duodenal ulcer is the decrease in elective anti-ulcer surgery.12 Patients presenting with an acute abdomen suggestive of a perforated duodenal ulcer are generally between 40 and 60 years of age although the number of patients over the age of 60 has been gradually increasing.13 Approximately 50% to 60% of these patients have a history of peptic ulcer disease,14,15 while a smaller number have a history of use of NSAIDs.16 The odds ratio for NSAID use is substantially increased for perforations,17 and simultaneous use of multiple NSAIDs as well as use of a single individual NSAID at high doses has been implicated. H. pylori infection and NSAID use are 2 independent risk factors associated with perforated duodenal ulcers, and the lack of duodenitis in NSAID users as compared with those with H. pylori infection suggests a differing pathogenesis.18 The use of crack cocaine has also led to an increase in perforated ulcer disease,19 and giant duodenal ulcers have a strong association with stimulant abuse.20
OPERATIVE MANAGEMENT OF PERFORATED DUODENAL ULCER
Surgery is the mainstay of management of a perforated duodenal ulcer. In the past, the high mortality rate following surgery for a perforated duodenal ulcer21 led to the emergence of nonoperative management.22 Berne et al23 have studied the nonoperative management of patients with perforated duodenal ulcers, with sealing of perforation documented by upper gastrointestinal radiographs with water-soluble contrast. With improved peri-operative care, the morbidity and mortality of surgery for perforated peptic ulcer disease has decreased, and a comparative randomized study24 has shown no difference in the morbidity or mortality in the surgical and nonsurgical groups. However, the length of hospital stay was significantly increased in the nonsurgical group. Failure of nonsurgical treatment was higher in patients over the age of 70 (67%), compared with only 16% in younger patients. Today, nonoperative management is usually reserved for the terminally septic patient.
INVESTIGATIONS
The evaluation of patients suspected of having a perforated duodenal ulcer routinely involves obtaining a history and a thorough physical examination, white blood cell count, and abdominal films. Some centers perform abdominal ultrasonography, or computerized tomography (CT) scans,8 in lieu of upper gastrointestinal studies. With current radiological techniques, 80% to 90% of cases are correctly diagnosed in most institutions. Approximately 5% to 10% of patients experience shock, with a mean arterial pressure of less than 80 mm Hg. This group of patients must be resuscitated,15 and the final decision regarding the mode of intervention made after assessing the response to the resuscitation efforts.
LAPAROSCOPIC INTERVENTION
Mouret et al3 first described laparoscopic intervention for perforated duodenal ulcers in 1990. Subsequently, this approach has found wide acceptance and has been successfully incorporated into the surgical armamentarium at many hospitals. Laparoscopic management has obvious benefits in reducing the size of the incision resulting in better cosmesis, reducing the incidence of postoperative wound infection, and the occurrence of incisional hernias. Formation of intraperitoneal adhesions is potentially reduced, although randomized studies to address this question have not been conducted. When faced with a patient with suspected or documented perforated ulcer disease, the surgeon should now consider whether the procedure should be performed laparoscopically. The major factor in this decision-making is the laparoscopic expertise of the surgeon. This has been the determining factor for patients being managed laparoscopically in a majority of studies.7, 15, 25 Advanced laparoscopic methods, increasingly available to young surgeons and residents, are available at most hospitals. Several studies have shown laparoscopic management of a perforated duodenal ulcer to be a feasible and safe alternative to open surgery.8, 7, 26 An overview of several studies comparing the open and laparoscopic approaches in the management of a perforated duodenal ulcer is summarized in Table 1.
Table 1.
Open and Laparoscopic Approaches in the Management of a Perforated Duodenal Ulcer
| Study | Type* | No.of Patients | Open | Laparoscopic | Converted to Open | Laparoscopic Procedure | Mortality† | Conclusion† |
|---|---|---|---|---|---|---|---|---|
| Urbano, et al 19945 | RN | 6 | - | 6 | - | 5 Peritoneal lavage/drain 1 Omentopexy | 0% | Peritoneal lavage/drainage of prime importance. |
| Thompson, et al 199536 | PN | 10 | 5 | 2 | 3 | Graham plication | 0% | Safe, effective. |
| Lau 199525 | P | 100 | - | 93 | 7 | 35 Raphy 44 Raphy/omentopexy 21 Fibrin glue | 3% | Safe, feasible. Analgesic needed less in laparoscopic group. Laparoscopic glue repair decreases operating time. |
| Lau, et al 199635 | PR | 103 | 51 | 41 | 11 | Raphy/sutureless repair | O = 2% L = 4% | Safe. Less operating time with suture repair. |
| So, et al 19967 | RN | 53 | 38 | 14 | 1 | Omentopexy alone | O = 10% L = 0% | Safe. Analgesic needed less in laparoscopic group. Operating time for L > O. |
| Miserez 199614 | RN | 34 | 13 | 18 | 3 | Raphy | O+C = 12% L = 5% | Technically feasible. Analgesic needed less in laparoscopic group. Operating time for L > O. |
| Druart, et al 19978 | PN | 100 | - | 92 | 8 | 14 Raphy alone 67 Raphy/omentopexy 7 Fibrin glue | 5% | Morbidity and mortality comparable. High risk: shock, delayed presentation, age >70. |
| Naesgaard 199926 | RN | 74 | 49 | 20 | 5 | Raphy/Omentopexy | O = 12.5% L+C = 20% | Safe. Increased mortality associated with delayed presentation. Operating time for L > O. |
| Katkhouda 200015 | P | 46 | 16 | 25 | 5 | Omentopexy alone | O = 6% L = 3.3% | Not beneficial in shock. Increased conversion rate in shock and delayed presentation. |
| Robertson 200031 | NC | 36 | 16 | 18 | 2 | Omentopexy | O = 12.5% L = 10% | Laparoscopy does not increase peri-op risk in peritonitis. Operating time for L = O. |
RN = Retrospective nonrandomized; PN = Prospective nonrandomized; PR = Prospective randomized; NC = Nonrandomized, concurrent cohort
O = Open; L = Laparoscopic; C = Laparoscopic converted to open.
LAPAROSCOPIC TECHNIQUES
The patient is positioned in a 15- to 20-degree reverse Trendelenburg position. The surgeon stands on the patient's right or between the patient's legs with an assistant on each side. Carbon dioxide pneumoperitoneum (12 to 15 mm Hg) is established through an umbilical incision with either a Veress needle or a Hassan cannula and a 30-degree angled laparoscope introduced through a 10-mm port. A port is introduced in the epigastrium for liver retraction or retraction of the gallbladder, and 2 working ports are introduced in the right mid and lower abdomen. Peritoneal lavage is one of the key interventions in the management of a perforated duodenal ulcer, and meticulous lavage consumes the bulk of the operative time. Lavage is performed with 6 to 10 liters of warm saline. The supra- and subhepatic spaces, the lateral gutters, the left subdiaphragmatic space, and the pelvic cavity are irrigated thoroughly in the dependent position. As a diagnostic tool, laparoscopy is extremely valuable, and a careful evaluation of the peritoneal cavity is routinely performed. Studies show that it is not difficult to identify the perforated duodenal ulcer in the majority of cases;27 however, one of the more common causes of conversion to open surgery is the inability to adequately localize the ulcer.8, 26 Perforations on the lateral wall of the second part of the duodenum may occasionally require mobilization of the duodenum to clearly visualize the extent of the perforation. Inflammatory adhesions can be divided with electrocautery, blunt or sharp dissection, or ultrasonic dissection.15
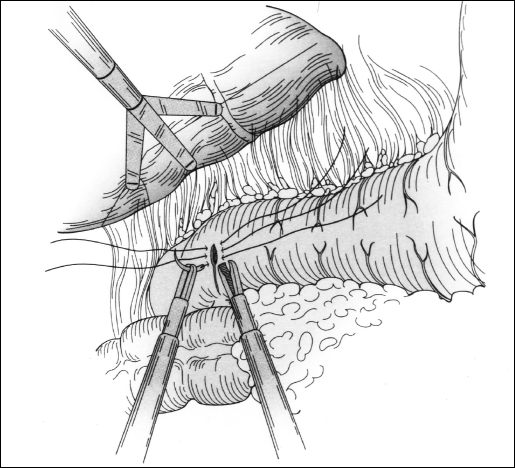
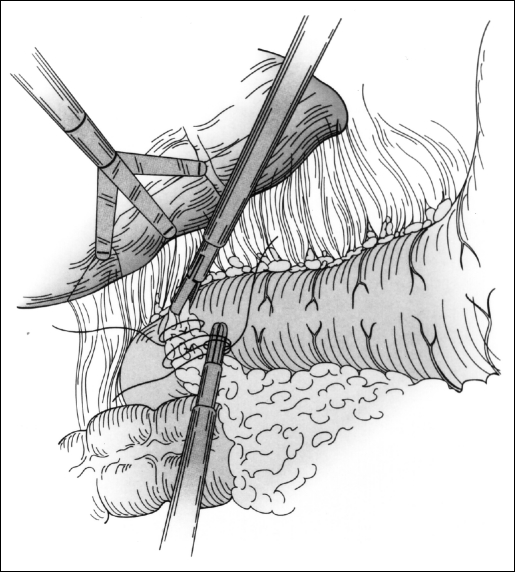
Walsh et al28 used laparoscopy to confirm their diagnosis of perforated duodenum. If perforation was confirmed and the presence of a naturally occurring omental plug was demonstrated, the plug was left undisturbed and peritoneal lavage was completed. Omentopexy was reserved for ulcers without a plug. Urbano et al5 successfully treated 5 of 6 cases of perforated duodenal ulcer with peritoneal lavage and placement of drains in the peritoneal cavity. In spite of a delayed presentation of greater than 12 hours following the perforation in 3 of 5 patients, these patients improved with surgery and were discharged in 7 days. A number of studies7, 15, 26,29–31 use omentopexy alone in the laparoscopic management of perforated duodenal ulcers. Three sutures are taken through viable duodenum on either side of the perforation and tied to close the perforation (Figure 1), and omentum is secured across the perforation (Figure 2). Some authors have sutured the falciform ligament over the perforated ulcer.32 Sutureless techniques of laparoscopic repair of perforated duodenal ulcers eliminate the need for laparoscopic suturing and have been shown to decrease operative time.25 These include the use of a piece of gelatin sponge shaped into a cone and placed into the ulcer with prewarmed fibrin sealant injected around the plug,33 the use of fibrin glue alone to seal the hole with omentum,3,34 or the use of a plug of ligamentum teres. Although several studies report routinely draining the site near the perforation or the subhepatic spaces,8,14 others do not.15 Operating time was slightly longer in the laparoscopic group,14,35 but familiarity with laparoscopic skills and widespread availability of good irrigation and suction apparatus should result in decreased operating times.
Figure 1.
Three sutures are placed through viable duodenum on either side of the perforation and tied to close the perforation. Reproduced with permission from Shah AS, Pappas TN. Atlas of Laparoscopic Surgery. In: Pappas TN, Chekan EG, Eubanks S, eds. Laparoscopic Repair of Perforated Ulcer and Vagotomy. Philadelphia, Pa: Current Medicine; 1999.
Figure 2.
Laparoscopic suturing of a pedicle of omentum placed across the perforation completes the Graham patch. Reproduced with permission from Shah AS, Pappas TN. Atlas of Laparoscopic Surgery. In: Pappas TN, Chekan EG, Eubanks S, eds. Laparoscopic Repair of Perforated Ulcer and Vagotomy. Philadelphia, Pa: Current Medicine; 1999.
INDICATIONS FOR CONVERSION OF A LAPAROSCOPIC PROCEDURE TO AN OPEN PROCEDURE
Cardiovascular instability has been a previously published indication for conversion to an open procedure. Relative indications for conversion include an ulcer greater than 6 mm in diameter or an ulcer with extremely friable edges,15 posterior location of the ulcer, inadequate localization, and rarely inadequate instrumentation.8 Presence of a perforated gastric ulcer36 or a prepyloric ulcer has occasionally necessitated conversion to an open procedure. While a gastric ulcer may need an open procedure for definitive surgery in cases of suspected malignancy, a prepyloric ulcer may be managed laparoscopically with omentopexy alone. Prognostic factors resulting in conversion are shock at the time of presentation (50% conversion rate in patients in shock as opposed to an 8% conversion rate in patients without shock) and the time lapse between perforation and presentation (33% conversion rate in patients presenting more than 24 hours after perforation, compared with no conversion in patients presenting earlier than 24 hours after perforation).15
POSTOPERATIVE MANAGEMENT
All patients had nasogastric suction postoperatively for approximately 24 hours, and oral intake was resumed after ileus resolved. Antibiotics were administered for 5 days,5 or until fever subsided. H2 blockers were started in the immediate postoperative period.7, 14 While the Visick scores between open and laparoscopic groups were comparable, a significant decrease occurred in the need for analgesics in the laparoscopic groups.7, 14 Naesgaard et al26 did not see this decrease in need for analgesia in the first 10 postoperative days. It was felt that the pain from peritonitis regulated the need for anal-gesics more than the pain from incisions. No statistically significant differences were noted between the 2 groups with regard to length of hospital stay or of return to work,7,26 but postoperative comfort was subjectively increased and noticed by most laparoscopic surgeons.8 Postoperative complications in most studies increase with an increase in mean age at presentation, shock at the time of presentation, presentation delayed for more than 24 hours, and confounding medical conditions. However, prospective randomized controlled studies will be needed to determine whether in this group of patients open versus laparoscopic management shows a significant difference in outcome.
TREATMENT OF H. PYLORI INFECTION
In 1995, Sebastian et al37 reported a high prevalence of H. pylori infection in patients with perforated duodenal ulcers, and persistent infection was found to be associated with persistent ulceration. H. pylori seropositivity rates are similar in patients with peptic ulcer disease, with or without complications, indicating that H. pylori infection is not necessarily associated with increased severity of the disease.38 Eradication of H. pylori infection in the postoperative period is critical because the recurrence rate following complete eradication of H. pylori is dramatically decreased,39,40 thus negating the need for definitive anti-ulcer surgery. Although some studies7 identify H. pylori status and treat it only in cases of persistent or recurrent disease, others give all patients with perforated duodenal ulcers a full course of anti-H. pylori treatment.31
PERITONITIS AND INSUFFLATION
CO2 insufflation of the peritoneal cavity in the presence of peritonitis has been shown in rat models to cause an increase in bacterial translocation41, 42 from the peritoneal cavity to the bloodstream. Although laparoscopic intervention would have been thought to be unsafe, such is not the case, and several studies have documented that laparoscopic surgery is to be safe even in the presence of peritonitis.14, 31 However, the incidence of postoperative pneumonia was significantly higher in patients undergoing laparoscopic repair of a perforated duodenal ulcer as compared with the open procedure.26 This pulmonary complication could not be attributed to time from perfo-ration, because the time interval was the same in both groups. Controlled trials to study the effects of pneumoperitoneum on infectious complications will be necessary to more clearly define the true risks and benefits of laparoscopic repairs. Differences if any between patients undergoing open surgery and patients initially explored laparoscopically and subsequently converted to open43 may also shed more light on this problem.
DEFINITIVE SURGERY
Today, surgery for peptic ulcer disease is aimed at treating the complications of the disease rather than curing the disease itself.44 Earlier studies45 had shown an 85% recurrence rate in patients with perforated duodenal ulcer (mean age of 44 years) treated with simple closure alone and concluded that ulcers expected to run a chronic course should be treated with definitive surgery and that acute ulcers should be treated by simple closure. Perforated duodenal ulcers secondary to the use of crack cocaine are caused by ischemia of the gastric mucosa and treatment of these ulcers does not require an acid-reducing operation.19 Definitive surgery is now indicated for patients unable to afford long-term medical management,46 those known to be noncompliant, or patients with hemorrhage accompanying the perforation.47 Occasionally, pyloroplasty is required when the pylorus is narrowed, especially following simple closure. Several groups have rigorously undertaken endoscopic follow-up at regular intervals. Definitive acid reducing anti-ulcer surgery at the time of perforation is felt to be unnecessary due to the effectiveness of H2 blockers and proton pump inhibitors and because eradication of H. pylori infection is possible. Evaluation for H. pylori should be conducted postoperatively and infected patients treated with combined medical therapy. Definitive surgery will be needed in only a minority of those patients who relapse after appropriate medical therapy. Further studies of perforated duodenal ulcers secondary to NSAID use are also needed to help define which patients require definitive surgery for ulcer disease.
A follow-up study of elderly patients (age > 70) treated with simple closure of a perforated duodenal ulcer showed a recurrence rate of 14% among survivors.48 With a 27% mortality at 30 days and an in-hospital mortality of 30%, the conclusion was that simple closure of the perforated ulcer was adequate treatment in the elderly. Even in a younger age group, definitive surgery may not be indicated at the time of repair of the perforation. When needed, vagotomy and other modalities of definitive surgery, such as posterior truncal vagotomy and anterior linear gastrectomy, can be safely undertaken laparoscopically.49–52
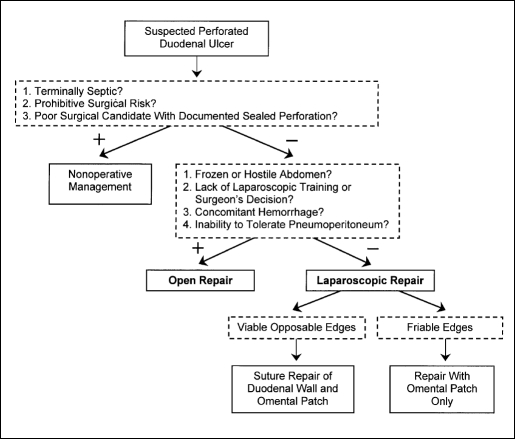
DUKE UNIVERSITY MEDICAL CENTER (DUMC) APPROACH TO MANAGEMENT OF THE PERFORATED DUODENAL ULCER
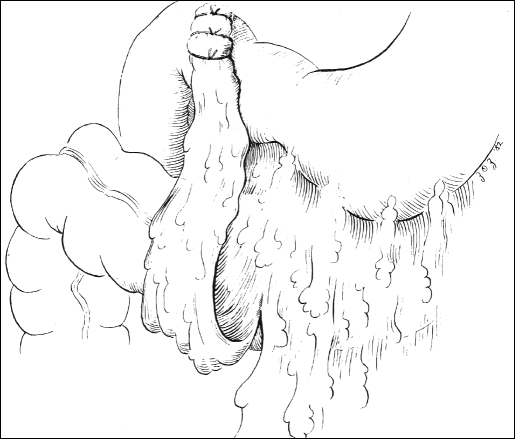
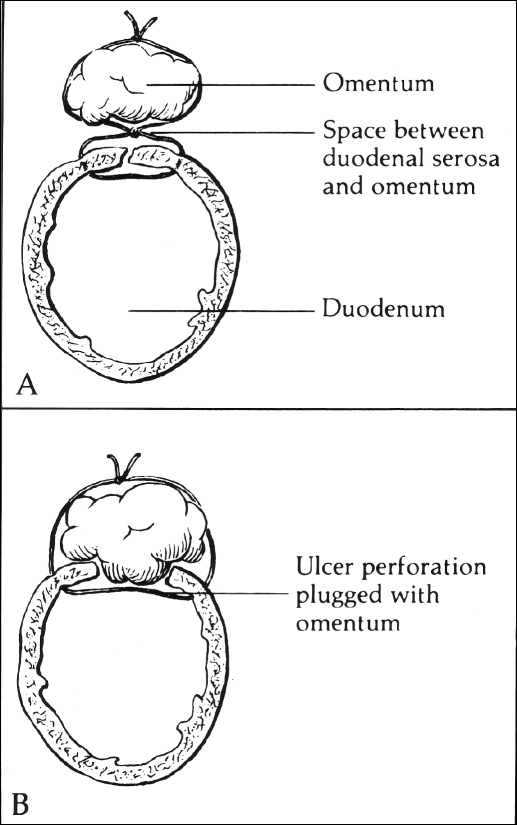
At the Duke University Medical Center, nonoperative management is limited to terminally septic patients, those with prohibitive surgical risk, or poor surgical candidates with documented contrast studies showing that the perforation has completely sealed. An open surgical approach is chosen for patients with a hostile or frozen abdomen that would prevent safe access, combined perforation and bleeding in the unstable patient, or the presence of comorbid cardiovascular or respiratory factors that compromise a patient's ability to tolerate a pneumoperitoneum. Another consideration is the lack of a surgeon's experience with advanced laparoscopy or a surgeon's decision based on the availability of trained operating room personnel and equipment. At laparoscopy, if the ulcer edges will not hold sutures adequately, repair is accomplished with a sutured omental patch only (Figure 3). Suture repair of viable opposable edges of the duodenal perforation is carried out as shown in Figure 4A, and reinforcement with an omen-tal patch is undertaken. Figure 4B shows a cross-sectional view of omentum used alone to seal the perforation. The DUMC approach to management of perforated duodenal ulcers is outlined in the algorithm in Figure 5.
Figure 3.
Repair of duodenal perforation with omentopexy alone. Reproduced with permission from Baker RJ. Mastery of Surgery. In: Nyhus LM, Baker RJ, Fischer JE, eds. Operation for Acute Perforated Duodenal Ulcer. London: Little, Brown and Company; 1997.
Figure 4.
A. Suture repair of viable opposable edges of the duodenal perforation and reinforcement with an omental patch.
B. Omentum plugs the hole of the perforation. Reproduced with permission from Baker RJ. Mastery of Surgery. In: Nyhus LM, Baker RJ, Fischer JE, eds. Operation for Acute Perforated Duodenal Ulcer. London: Little, Brown and Company; 1997.
Figure 5.
The Duke Medical Center algorithm for management of a suspected perforated duodenal ulcer.
CONCLUSIONS
The need for surgical management of peptic ulcer disease in the elective setting has markedly decreased. In patients who need elective surgery, most definitive surgery can be performed safely with laparoscopic techniques. Surgery continues to play a key role in the management of perforated duodenal ulcers in all but the most terminally septic patients. Successful management involves recognition and attention to 3 key factors: the patient's clinical status, the characteristics of the perforation, and the pathogenesis of the ulcer disease. Meticulous attention to resuscitation and treatment of confounding medical conditions, surgery for peritoneal lavage and repair of the perforation, and a strict postoperative medical regimen to treat the ulcer diathesis contribute towards the outcome. Often, the laparoscopic approach to repair the perforated duodenal ulcer is appropriate. Several studies have shown that laparoscopic intervention is safe, feasible, and cosmetically appealing. Laparoscopic repair of a perforated duodenal ulcer has resulted in less opiate analgesia use, but the open and laparoscopic groups currently have similar reported outcomes.31, 53 A randomized study54 comparing the acute phase response in patients with perforated ulcer undergoing laparoscopic or open repair concluded that the laparoscopic approach does not lead to the reduction in acute stress seen in elective surgery. As with most laparoscopic surgery, a decreased incidence is seen in postoperative wound infection and subsequent hernia formation. The subjective comfort following laparoscopic surgery has been noticed by patients and surgeons alike. Information regarding time of presentation in relation to the perforation is critical when considering the mode of surgical intervention, and these data can be reliably obtained from a majority of patients. Patients presenting in shock or presenting more than 24 hours following the perforation have increased morbidity and mortality. Here, laparoscopic intervention should be used with caution because the risk of hemodynamic instability is higher, with an increased tendency towards bacterial translocation following insufflation of the peritoneal cavity and an increase in the conversion rate. Prospective randomized trials will be needed to determine whether these factors are unique to the laparoscopic mode of intervention. Today, the patient with a perforated duodenal ulcer presenting for surgery tends to be older, sicker, or using NSAIDs as opposed to his counterpart 15 years ago. This patient population can benefit from the appropriately applied laparoscopic approach of surgical intervention. Further trials are needed to evaluate parameters that determine optimal safety of surgical approaches in this patient group.
References:
- 1. Feliciano DV. Do perforated duodenal ulcers need an acid-decreasing surgical procedure now that omeprazole is available? Surg Clin North Am. 1992;72(2):369–380 [DOI] [PubMed] [Google Scholar]
- 2. Graham RR. The surgeon's problem in duodenal ulcer. Am J Surg. 1938;40:102–117 [Google Scholar]
- 3. Mouret P, Francois Y, Vignal J, et al. Laparoscopic treatment of perforated peptic ulcer. Br J Surg. 1990;77(9):1006. [DOI] [PubMed] [Google Scholar]
- 4. Darzi A, Carey PD, Menzies-Gow N, Monson JR. Preliminary results of laparoscopic repair of perforated duodenal ulcers. Surg Laparosc Endosc. 1993;3(3):161–163 [PubMed] [Google Scholar]
- 5. Urbano D, Rossi M, De Simone P, et al. Alternative laparoscopic management of perforated peptic ulcers. Surg Endosc. 1994;8(10):1208–1211 [DOI] [PubMed] [Google Scholar]
- 6. Matsuda M, Nishiyama M, Hanai T, et al. Laparoscopic omental patch repair for perforated peptic ulcer. Ann Surg. 1995;221(3):236–240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. So JB, Kum CK, Fernandes ML, Goh P. Comparison between laparoscopic and conventional omental patch repair for perforated duodenal ulcer. Surg Endosc. 1996; 10(11):1060–1063 [DOI] [PubMed] [Google Scholar]
- 8. Druart ML, Van Hee R, Etienne J, et al. Laparoscopic repair of perforated duodenal ulcer. A prospective multicenter clinical trial. Surg Endosc. 1997;11(10):1017–1020 [DOI] [PubMed] [Google Scholar]
- 9. Svanes C, Lie RT, Kvale G, et al. Incidence of perforated ulcer in western Norway, 1935-1990: cohort- or period-dependent time trends? Am J Epidemiol. 1995;141(9):836–844 [DOI] [PubMed] [Google Scholar]
- 10. Liu TJ, Wu CC. Peptic ulcer surgery: Experience in Taiwan from 1982 to 1993. Asian Journal of Surgery. 1997;20(4):305–314 [Google Scholar]
- 11. Hermansson M, von Holstein CS, Zilling T. Peptic ulcer perforation before and after the introduction of H2-receptor blockers and proton pump inhibitors [published erratum appears in Scand J Gastroenterol. 1997;32(10):1072]. Scand J Gastroenterol. 1997;32(6):523–529 [DOI] [PubMed] [Google Scholar]
- 12. Jamieson GG. Current status of indications for surgery in peptic ulcer disease. World J Surg. 2000;24(3):256–258 [DOI] [PubMed] [Google Scholar]
- 13. Svanes C, Salvesen H, Stangeland L, et al. Perforated peptic ulcer over 56 years. Time trends in patients and disease characteristics. Gut. 1993;34(12):1666–1671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Miserez M, Eypasch E, Spangenberger W, et al. Laparoscopic and conventional closure of perforated peptic ulcer. A comparison. Surg Endosc. 1996;10(8):831–836 [DOI] [PubMed] [Google Scholar]
- 15. Katkhouda N, Mavor E, Mason RJ, et al. Laparoscopic repair of perforated duodenal ulcers: outcome and efficacy in 30 consecutive patients. Arch Surg. 1999;134(8):845–850 [DOI] [PubMed] [Google Scholar]
- 16. Bliss DW, Stabile BE. The impact of ulcerogenic drugs on surgery for the treatment of peptic ulcer disease. Arch Surg. 1991;126(5):609–612 [DOI] [PubMed] [Google Scholar]
- 17. Gutthann SP, Garcia Rodriguez LA, Raiford DS. Individual non-steroidal antiinflammatory drugs and other risk factors for upper gastrointestinal bleeding and perforation. Epidemiology. 1997;8(1):18–24 [DOI] [PubMed] [Google Scholar]
- 18. Taha AS, Dahill S, Nakshabendi I, et al. Duodenal histology, ulceration, and Helicobacter pylori in the presence or absence of non-steroidal anti-inflammatory drugs. Gut. 1993;34(9):1162–1166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Arrillaga A, Sosa JL, Najjar R. Laparoscopic patching of crack cocaine-induced perforated ulcers. Am Surg. 1996;62(12):1007–1009 [PubMed] [Google Scholar]
- 20. Pecha RE, Prindiville T, Pecha BS, et al. Association of cocaine and methamphetamine use with giant gastroduodenal ulcers. Am J Gastroenterol. 1996;91(12):2523–2527 [PubMed] [Google Scholar]
- 21. Boey J, Choi SK, Poon A, Alagaratnam TT. Risk stratification in perforated duodenal ulcers. A prospective validation of predictive factors. Ann Surg. 1987;205(1):22–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Donovan AJ, Vinson TL, Maulsby GO, Gewin JR. Selective treatment of duodenal ulcer with perforation. Ann Surg. 1979;189(5):627–636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Berne TV, Donovan AJ. Nonoperative treatment of perforated duodenal ulcer. Ann Surg. 1989;124(7):830–832 [DOI] [PubMed] [Google Scholar]
- 24. Crofts TJ, Park KG, Steele RJ, et al. A randomized trial of nonoperative treatment for perforated peptic ulcer. N Engl J Med. 1989;320(15):970–973 [DOI] [PubMed] [Google Scholar]
- 25. Lau WY, Leung KL, Zhu XL, et al. Laparoscopic repair of perforated peptic ulcer. Br J Surg. 1995;82(6):814–816 [DOI] [PubMed] [Google Scholar]
- 26. Naesgaard JM, Edwin B, Reiertsen O, et al. Laparoscopic and open operation in patients with perforated peptic ulcer. Eur J Surg. 1999;165(3):209–214 [DOI] [PubMed] [Google Scholar]
- 27. Isaac J, Tekant Y, Kiong KC, et al. Laparoscopic repair of perforated duodenal ulcer. Gastrointest Endosc. 1994;40(1):68–69 [DOI] [PubMed] [Google Scholar]
- 28. Walsh CJ, Khoo DE, Motson RW. Laparoscopic repair of perforated peptic ulcer. Br J Surg. 1993;80(1):127. [PubMed] [Google Scholar]
- 29. Siu WT, Leong HT, Li MK. Single stitch laparoscopic omen-tal patch repair of perforated peptic ulcer. J R Coll Surg Edinb. 1997;42(2):92–94 [PubMed] [Google Scholar]
- 30. Takeuchi H, Kawano T, Toda T, et al. Laparoscopic repair for perforation of duodenal ulcer with omental patch: report of initial six cases. Surg Laparosc Endosc. 1998;8(2):153–156 [PubMed] [Google Scholar]
- 31. Robertson GS, Wemyss-Holden SA, Maddern GJ. Laparoscopic repair of perforated peptic ulcers. The role of laparoscopy in generalised peritonitis. Ann R Coll Surg Engl. 2000;82(1):6–10 [PMC free article] [PubMed] [Google Scholar]
- 32. Munro WS, Bajwa F, Menzies D. Laparoscopic repair of perforated duodenal ulcers with a falciform ligament patch. Ann R Coll Surg Engl. 1996;78(4):390–391 [PMC free article] [PubMed] [Google Scholar]
- 33. Tate JJ, Dawson JW, Lau WY, Li AK. Sutureless laparoscopic treatment of perforated duodenal ulcer. Br J Surg. 1993;80(2):235. [DOI] [PubMed] [Google Scholar]
- 34. Benoit J, Champault GG, Lebhar E, Sezeur A. Sutureless laparoscopic treatment of perforated duodenal ulcer. Br J Surg. 1993;80(9):1212. [DOI] [PubMed] [Google Scholar]
- 35. Lau WY, Leung KL, Kwong KH, et al. A randomized study comparing laparoscopic versus open repair of perforated peptic ulcer using suture or sutureless technique. Ann Surg. 1996;224(2):131–138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Thompson AR, Hall TJ, Anglin BA, Scott-Conner CE. Laparoscopic plication of perforated ulcer: results of a selective approach. South Med J. 1995;88(2):185–189 [DOI] [PubMed] [Google Scholar]
- 37. Sebastian M, Chandran VP, Elashaal YI, Sim AJ. Helicobacter pylori infection in perforated peptic ulcer disease. Br J Surg. 1995;82(3):360–362 [DOI] [PubMed] [Google Scholar]
- 38. Lee WJ, Wu MS, Chen CN, et al. Seroprevalence of Helicobacter pylori in patients with surgical peptic ulcer. Arch Surg. 1997;132(4):430–434 [DOI] [PubMed] [Google Scholar]
- 39. Forbes GM, Glaser ME, Cullen DJ, et al. Duodenal ulcer treated with Helicobacter pylori eradication: seven-year follow-up. Lancet. 1994;343(8892):258–260 [DOI] [PubMed] [Google Scholar]
- 40. Hopkins RJ, Girardi LS, Turney EA. Relationship between Helicobacter pylori eradication and reduced duodenal and gastric ulcer recurrence: a review. Gastroenterology. 1996;110(4): 1244–1252 [DOI] [PubMed] [Google Scholar]
- 41. Bloechle C, Emmermann A, Treu H, et al. Effect of a pneumoperitoneum on the extent and severity of peritonitis induced by gastric ulcer perforation in the rat. Surg Endosc. 1995;9(8):898–901 [DOI] [PubMed] [Google Scholar]
- 42. Gurtner GC, Robertson CS, Chung SC, et al. Effect of carbon dioxide pneumoperitoneum on bacteraemia and endotoxaemia in an animal model of peritonitis. Br J Surg. 1995;82(6):844–848 [DOI] [PubMed] [Google Scholar]
- 43. Bloechle C, Emmermann A, Zornig C. Laparoscopic and conventional closure of perforated peptic ulcer. Surg Endosc. 1997;11(12):1226–1227 [DOI] [PubMed] [Google Scholar]
- 44. Ohmann C, Imhof M, Roher HD. Trends in peptic ulcer bleeding and surgical treatment. World J Surg. 2000;24(3):284–293 [DOI] [PubMed] [Google Scholar]
- 45. Tanphiphat C, Tanprayoon T, Na Thalang A. Surgical treatment of perforated duodenal ulcer: a prospective trial between simple closure and definitive surgery. Br J Surg. 1985;72(5):370–372 [DOI] [PubMed] [Google Scholar]
- 46. Casas AT, Gadacz TR. Laparoscopic management of peptic ulcer disease. Surg Clin North Am. 1996;76(3):515–522 [DOI] [PubMed] [Google Scholar]
- 47. Baker RJ. Operation for acute perforated duodenal ulcer. In: Nyhus LM, Baker RJ, Fischer JE. eds. Mastery of Surgery. Vol 1. Boston, Mass: Little, Brown and Co; 1997:916–920 [Google Scholar]
- 48. Blomgren LG. Perforated peptic ulcer: long-term results after simple closure in the elderly. World J Surg. 1997;21(4):412–415 [DOI] [PubMed] [Google Scholar]
- 49. Gomez-Ferrer F, Ballyque JG, Azagra S, et al. Laparoscopic surgery for duodenal ulcer: first results of a multicenter study applying a personal procedure. Hepatogastroenterology. 1999;46(27):1517–1521 [PubMed] [Google Scholar]
- 50. Mouiel J, Kathouda N. Posterior vagotomy and anterior seromyotomy as elective surgery for duodenal ulcer disease. Hepatogastroenterology. 1999;46(27):1507–1516 [PubMed] [Google Scholar]
- 51. Cadiere GB, Bruyns J, Himpens J, et al. Laparoscopic highly selective vagotomy. Hepatogastroenterology. 1999;46(27):1500–1506 [PubMed] [Google Scholar]
- 52. Dubois F. New surgical strategy for gastroduodenal ulcer: laparoscopic approach. World J Surg. 2000;24(3):270–276 [DOI] [PubMed] [Google Scholar]
- 53. Bergamaschi R, Marvik R, Johnsen G, et al. Open vs laparoscopic repair of perforated peptic ulcer. Surg Endosc. 1999;13(7):679–682 [DOI] [PubMed] [Google Scholar]
- 54. Lau JY, Lo SY, Ng EK, et al. A randomized comparison of acute phase response and endotoxemia in patients with perfo-rated peptic ulcers receiving laparoscopic or open patch repair. Am J Surg. 1998;175(4):325–327 [DOI] [PubMed] [Google Scholar]