Failed ERCP appears to decrease the success rate of a laparoscopic approach for common bile duct exploration.
Keywords: Choledocholithiasis, Laparoscopy, Endoscopic retrograde, Cholangiopancreatography
Abstract
Objectives:
To compare the effectiveness of laparoscopic common bile duct exploration in patients with failed endoscopic retrograde cholangiopancreatography (ERCP).
Methods:
This is a descriptive, comparative study. Patients with an indication of common bile duct exploration between February 2005 and October 2008 were included. We studied 2 groups: Group A: patients with failed ERCP who underwent LCBDE plus LC. Group B: patients with common bile duct stones managed with the 1-step approach (LCBDE + LC) with no prior ERCP.
Results:
Twenty-five patients were included. Group A: 9 patients, group B: 16 patients. Success rate, operative time, and hospital stay were as follows: group A 66% vs group B 87.5%; group A 187 minutes vs 106 minutes; group A 4.5 days vs 2.3 days; respectively.
Conclusion:
Patients with failed ERCP should be considered as high-complex cases in which the laparoscopic procedure success rate decreases, and the conversion rate increases considerably.
INTRODUCTION
Secondary bile duct stones are present in as many as 15% of patients with gallstones. They are associated with severe complications, such as pancreatitis and cholangitis.1,2
After the introduction of laparoscopic cholecystectomy, endoscopic retrograde cholangiopancreatography (ERCP) replaced open surgery as the gold standard for the treatment of common bile duct stones. The benefits of the preoperative endoscopic treatment (ERCP) followed by LC (2-step approach) are substantially better compared with open surgery, regarding postoperative pain, hospital stay, return to work, and cosmesis.3,4
However, ERCP has some issues, such as procedure-related complications and failed ERCP with a rate as high as 10% to 25%.5,6 The limitations of endoscopic treatment are related to the complexity of doing a correct cannulation of the ampulla of Vater and stone retrieval. Patients with failed ERCP are considered high-complex cases.5–7
The failure in retrieving bile duct stones by using ERCP is an absolute indication for performing CBDE. Once the laparoscopic surgeons have gained experience with laparoscopic cholecystectomy, minimally invasive surgery moved one step forward, to LCBDE. Since the first experiences reported in 1991,8–10 this procedure has been done together with new technologies, currently considered as effective as ERCP.11,12 Some reports support the 1-step approach over the 2-step approach in terms of costs and hospital stay.13–15
We reported our initial experience with LCBDE in 2005.16 Thereafter, we have been doing the procedure with the choledochoscope and the fluoroscopic-guided wire basket.17,18 Some of our patients are referred to us because of failed ERCP, in particular high-complex patients. The objective of this article is to report our experience with LCBDE in patients with failed ERCP and compare them with the outcomes of patients who underwent the 1-step approach (LCBE+LC) with no prior ERCP.
METHODS
This is a descriptive, comparative, longitudinal study that included 25 patients with the indication of common bile duct exploration between February 2005 and October 2008. All the patients were included in the LCBDE protocol. Then after 3 and a half years, we retrospectively analyzed the variables contained in our database.
Preoperative evaluation included liver function tests, abdominal ultrasound, and cardiovascular evaluation. All patients were informed regarding therapeutic options, and informed consents were signed.
Technique for Laparoscopic Common Bile Duct Exploration
Once Calot's triangle is dissected and the anatomic structures identified, an intraoperative cholangiography is performed (IOC). IOC is achieved by placing an LT 300 titanium clip in the proximal aspect of the cystic duct, and a partial cut distal to the clip is done with a laparoscopic scissors. A cholangiocatheter or Intracath N°14 is introduced into the abdominal cavity via the Intracath needle, using it as an additional trocar so that the surgeon's hands are free to perform the cystic cannulation. The catheter is advanced through the cystic duct and is secured by using an additional clip. After a test with physiologic solution, taking care of any leak due to a loose clip, the contrast is passed under direct vision using the fluoroscope.
The IOC allows the surgical team to identify or confirm the presence of bile duct stones (Figure 1). The IOC also depicts a map of the extrahepatic biliary anatomy, especially in patients with failed ERCP, due to the difficulty in cannulating the ampulla of Vater.
Figure 1.
Intraoperative cholangiography showing dilated common bile duct and multiple stones.
After a positive IOC, the next step is to perform a common bile duct exploration. The LCBDE should begin via the cystic duct given that, compared with a choledochotomy this pathway is associated with lower morbidity and costs.19,20 However, regarding patients with failed ERCP, due to the difficulty in bile duct stone retrieval, the transcystic approach appears to be unfeasible, and a choledochotomy is usually done.
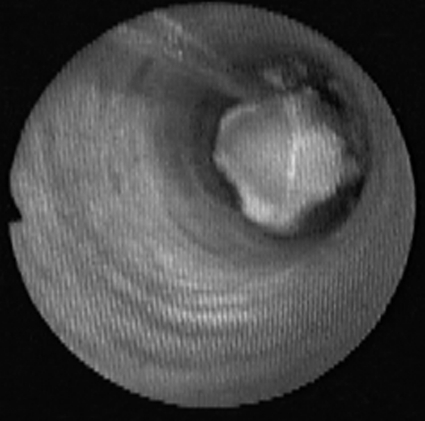
Before the supraduodenal choledochotomy is done, a 4-0 Vicryl suture is placed over the common bile duct to handle it and make the procedure more feasible. Once the choledochotomy is done, the exploration and bile duct stone retrieval begins under direct vision using a choledochoscope, which has been our standard procedure since 2005 (Figure 2). Sometimes, in these high-complex cases, a wider choledochotomy is needed matching the size of the bigger stone, preventing serious tears in the common bile duct (Figure 3). After retrieving the bile duct stones, a T tube is placed and secured, and a final IOC is done. A subhepatic drain is placed.
Figure 2.
Common bile duct stone under direct vision of choledochoscope.
Figure 3.
Choledochotomy must match the size of the larger stone.
Statistical Analysis
The variables and demographics were compared with the rate of success and the postoperative course. The means were calculated for continuous variables. The frequency and percentage were calculated for nominal variables. The Student t test was calculated to compare the success rate between the 2 groups.
RESULTS
Nine of the 25 patients (36%) included in this study were referred from the department of gastroenterology after a failed ERCP. A 1-step approach, LCBDE+LC, was performed in the other 16 patients.
The failed ERCPs were due to the difficulty in cannulating the ampulla of Vater (4 patients) and difficulty in stone retrieval (5 patients), due to the presence of intrahepatic bile duct stones or huge common bile duct stones (Table 1).
Table 1.
Causes of ERCP Failure in Patients Admitted With Unresolved Choledocholithiasis
| Causes | n = 9 |
|---|---|
| Impossbility in Cannulating the Ampulla of Vater | |
| Antrectomy | 1 |
| Duodenal diverticulum | 2 |
| Not specified | 1 |
| 2. Difficulty in Stone Retrieval | |
| Intrahepatic stones | 2 |
| Big and multiple stones | 3 |
These 9 patients were operated on with the intention of performing LCBDE; however, the conversion rate was 33.3%. Intrahepatic bile duct stones and embedded stones in the ampulla of Vater were the cause of conversion to an open procedure (Table 2). The hospital stay was 4.5 days (range, 2 to 8), which is related to the conversion rate shown, and also because these patients underwent a common bile duct exploration via choledochotomy. In a mean follow-up of 22 months, no residual lithiasis has been reported.
Table 2.
Laparoscopic Common Bile Duct Exploration in Patients With Complex Choledocholithiasis
| Results | Number of Patients |
|---|---|
| Successful | 6 (66,6%) |
| Conversion | 3 (33,3%) |
| Intrahepatic bile stones | 1 |
| Embedded stones | 2 |
Comparing high-complex cases (failed ERCP) with the 1-step approach cases (LCBDE+LC), the success rate between them is widely evident (66% vs 87.5%, respectively). The same happens when operative time and hospital stay between both groups are compared. However, because this series is small, no statistical significance in these parameters exists (Table 3).
Table 3.
Laparoscopic Common Bile Duct Exploration: Comparison Between Cases With Failed Endoscopic Retrograde Cholangiopancreatography (ERCP) and Cases With the 1-step Approach (LCBDE+LC)
| LCBDE in failed ERCP (Group A) | LCBDE + LC (1-step approach) (Group B) | P Value* | |
|---|---|---|---|
| Age (years) | 45 (28 to 78) | 39 (29 to 59) | NS |
| Conversion | 33.3% | 12.5% | P<0.05 |
| Complications | 11.1% | 6.25% | NS |
| Operative time (min) | 187′ | 106′ | |
| LCBDE Transcystic | —- | 99′ | NR |
| LCBDE Choledochotomy | 187′ | 119′ | NR |
| Hospital stay (days) | 4.5 (2 to 8) | 2.3 (2 to 5) | NR |
| Residual lithiasis | 0% | 0% | NR |
NS=not significant; NR=not rated.
DISCUSSION
After its introduction in the 1970s, ERCP along with the endoscopic sphincterotomy became the gold standard in the treatment of common bile duct stones. This procedure is done in patients with a high-suspicion of common bile duct stones or patients with demonstrated bile duct stones. ERCP effectiveness is between 75% and 90%.5–7
This endoscopic procedure (ERCP) has some failure-related factors, such as postsurgical gastrointestinal anatomic variations (Billroth II), duodenal diverticulum, embedded stones in the ampulla of Vater, intrahepatic bile duct stones, and common bile duct strictures.5
The presence of a duodenal diverticulum is frequent, particularly in the elderly. Ampullae of Vater located at the bottom of the diverticulum are the main cause of failure in cannulation and stone retrieval. Cannulation rate in juxtapapillary diverticulum is 78% and 38% when the ampulla is at the bottom.21,22
The presence of several stones or big stones is usually the cause of ERCP failure. The multiple attempts and maneuvers performed increase the complication rate, such as pancreatitis, bleeding, or perforation.23
Biliary strictures are another cause of ERCP failure. Fortunately, they are infrequent in our area. Billroth II gastrectomy is considered a big challenge for ERCP performers with success rate barely reaching 60%. The complexity is not only due to the difficulty in reaching the ampulla but also in achieving the exact location of the endoscope prior to cannulating it.24
Surgery must be performed in every patient with a failed ERCP. With the advance in minimally invasive surgery, LCBDE is now considered effective, safe, and feasible.12,25
The development of new surgical techniques and reaching the learning curve for LCBDE has led to considering the 1-step approach as an option for patients with gallstones and suspected choledocholithiasis. The United States National Institutes of Health consensus and the British Society of Gastroenterology recommendations report LCBDE as effective as ERCP in the treatment of choledocholithiasis.12,26
We strongly suggest the routine use of the choledochoscope assistance in all cases. It has been our standard procedure. In our experience, the success rate of the blind basket technique or under fluoroscopic guidance is as low as 30%. We have been performing LCBDE since 2005 with a global success rate of 80%, morbidity of 8%, and no mortalities.16,17–18 However, when analyzing the cases of failed ERCP only, we notice that the effectiveness decreases (66%). The main causes of conversion to an open procedure, as in specialized centers, are the presence of intrahepatic bile duct stones and embedded stones in the ampulla of Vater.27 There are no preoperative indicators for LCBDE failure.
CONCLUSION
Similar to the findings of Karaliotas et al in 2008,28 who reported a success rate of 64.5%, this study shows that patients with failed ERCP should definitely be considered complex cases. In these patients, the effectiveness of the laparoscopic procedure decreases, and the conversion rate increases considerably.
Footnotes
Financial support was provided by the Scientific and Humanistic Development Center (CDCH) of the Central University of Venezuela.
Contributor Information
Aléxis Sanchez, Surgery Professor, Medicine Faculty, Central University of Venezuela, Surgery Department III, Laparoscopic Surgery Program Co-Director, University Hospital of Caracas, Caracas, Venezuela..
Omaira Rodriguez, Surgery Professor, Medicine Faculty, Central University of Venezuela, Surgery Department III, University Hospital of Caracas, Caracas, Venezuela..
Omar Bellorín, Surgery Department III, University Hospital of Caracas, Caracas, Venezuela..
Renata Sánchez, Surgery Professor, Medicine Faculty, Central University of Venezuela, Surgery Department III, University Hospital of Caracas, Caracas, Venezuela..
Gustavo Benítez, Surgery Professor, Medicine Faculty, Central University of Venezuela, Surgery Department III, Chairman, University Hospital of Caracas, Caracas, Venezuela..
References:
- 1. Petelin JB. Surgical management of common bile duct stones. Gastrointest Endosc. 2002; 56(6 Suppl): S183–189 [DOI] [PubMed] [Google Scholar]
- 2. Sahai AV, Mauldin PD, Marsi V, Hawes RH, Hoffman BJ. Bile duct stones and laparoscopic cholecystectomy: a decision analysis to asses the roles of intraoperative cholangiography, EUS, and ERCP. Gastrointest Endosc. 1999; 49(3): 334–343 [DOI] [PubMed] [Google Scholar]
- 3. Perissat J, Huibregtse K, Keane F, Rusell R, Neoptolemos J. Management of bile duct stones in the era of laparoscopic cholecystectomy. Br J Surg. 1994; 81(6): 799–810 [DOI] [PubMed] [Google Scholar]
- 4. Cotton PB. Endoscopic retrograde cholangiopancreatography and laparoscopy cholecystectomy. Am J Surg. 1993; 165(4): 474–478 [DOI] [PubMed] [Google Scholar]
- 5. Tai C, Tang C, Ha J, Chau C, Siu W, Li M. Laparoscopic exploration of common bile duct in difficult choledocholithiasis. Surg Endosc. 2004; 18(6): 910–914 [DOI] [PubMed] [Google Scholar]
- 6. Rhodes M, Sussman L, Cohen L, Lewis MP. Randomised trial of laparoscopic exploration of common bile duct stones in a postoperative endoscopic retrograde cholangiography for common bile duct stones. Lancet. 1998; 351: 159–161 [DOI] [PubMed] [Google Scholar]
- 7. Tang C, Li M. Technical aspects in the laparoscopic management of complicated common bile duct stones. J Hepatobiliary Pancreat Surg. 2005; 12: 444–450 [DOI] [PubMed] [Google Scholar]
- 8. Jacobs M, Verdeja JC, Goldstein HS. Laparoscopic choledocholithotomy. J Laparoendosc Surg. 1991; 1(2): 79–82 [DOI] [PubMed] [Google Scholar]
- 9. Petelin J. Laparoscopic approach to common duct pathology. Surg Laparosc Endosc. 1991; 1(1): 33–41 [PubMed] [Google Scholar]
- 10. Shapiro SJ, Gordon LA, Daykhovsky L, Grundfest W. Laparoscopic exploration of the common bile duct: experience in 16 selected patients. J Laparoendosc Surg. 1991; 1(6): 333–341 [DOI] [PubMed] [Google Scholar]
- 11. Berthou J, Dron B, Charbonneau PH, Moussalier K, Pellisier L. Evaluation of laparoscopic treatment of common bile duct stones in a prospective series of 505 patients: Indications and results. Surg Endosc. 2007; 21: 1970– 1974 [DOI] [PubMed] [Google Scholar]
- 12. NIH state-of-the-science statement on endoscopic retrograde cholangiopancreatography (ERCP) for diagnosis and therapy. NIH Consens State Sci Statements. 2002; 19 (1): 1–23 [PubMed] [Google Scholar]
- 13. Cuschieri A, Lezoche E, Morino M, et al. E.A.E.S. multicenter prospective randomized trial comparing two-stage vs single-stage management of patients with gallstone disease and ductal calculi. Surg Endosc. 1999; 13: 952–957 [DOI] [PubMed] [Google Scholar]
- 14. Liberman M, Phillips E, Carroll B, Fallas M, Rosenthal R, Hiatt J. Cost-effective management of complicated choledocholithiasis: laparoscopic transcystic duct exploration or endoscopic sphincterotomy. J Am Coll Surg. 1996; 182(6): 488–489 [PubMed] [Google Scholar]
- 15. Urbach D, Khajanchee Y, Jobe B, Standage B, Hansen P, Swanstrom L. Cost-effective management of common bile duct stones. Surg Endosc. 2001; 15: 4–13 [DOI] [PubMed] [Google Scholar]
- 16. Sánchez A, Benítez G, Rodriguez O, et al. Exploración laparoscópica de la vía biliar. Primera experiencia en el Hospital Universitario de Caracas. Rev Venez Cir. 2005; 58(2): 68–77 [Google Scholar]
- 17. Rodriguez O, Sánchez Ismayel A, Benítez G, Pujadas Z, Valero R, Sánchez R. Instrumentación laparoscópica de la vía biliar bajo control fluoroscópico. Análisis luego de dos años de experiencia. Rev Venez Cir. 2007; 60(2): 57–64 [Google Scholar]
- 18. Sánchez A, Rodriguez O, Sánchez R, Benítez G, Bellorín O, Paredes J. Coledocoscopia en la exploración laparoscópica de la vía biliar para resolución de coledocolitiasis. Rev Venez Cir. 2007; 60(4): 177–182 [Google Scholar]
- 19. Millat B, Fingerhut A, Deleuze A, et al. Prospective evaluation in 121 unselected patients undergoing laparoscopic treatment of choledocholithiasis. Br J Surg. 1995; 82(9): 1266–1269 [DOI] [PubMed] [Google Scholar]
- 20. Petelin JB. Laparoscopic common bile duct exploration. Surg Endosc. 2003; 17(11): 1705–1715 [DOI] [PubMed] [Google Scholar]
- 21. Chang-Chien C. Do Juxtapapillary diverticula of the duodenum interfere with cannulation at endoscopic retrograde cholangiopancreatography? A prospective study Gastrointest Endosc. 1987; 33: 298–300 [DOI] [PubMed] [Google Scholar]
- 22. Lobo D, Balfour T, Iftikhar S. Periampullary diverticula: consequences of failed ERCP. Ann R Coll Surg Engl. 1998; 80: 326– 331 [PMC free article] [PubMed] [Google Scholar]
- 23. Andriulli A, Loperfido S, Napolitano G, et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007; 102(8): 1781–1788 [DOI] [PubMed] [Google Scholar]
- 24. Lin L, Siauw C, Ho K, Tung J. ERCP in post-Billroth II gastrectomy patients: emphasis on technique. Am J Gastroenterol. 1999; 94: 144–148 [DOI] [PubMed] [Google Scholar]
- 25. Poulose B, Arbogast P, Holzman M. National Analysis of in-hospital resource utilization in choledocholithiasis management using propensity scores. Surg Endosc. 2006; 20: 186–190 [DOI] [PubMed] [Google Scholar]
- 26. Williams E, Green J, Beckingham I, Parks R, Martin D, Lombard M. British Society of Gastroenterology. Guidelines on the management of common bile duct stones (CBDS). Gut. 2008; 57(7): 1004–1021 [DOI] [PubMed] [Google Scholar]
- 27. Stromberg C, Nilsson M, Leijonmarck C. Stone clearance and risk factors for failure in laparoscopic transcystic exploration of the common bile duct. Surg Endosc. 2008; 22: 1194–1199 [DOI] [PubMed] [Google Scholar]
- 28. Karaliotas C, Sgourakis G, Goumas C, Papaioannou N, Lilis C, Leandros E. Laparoscopic common bile duct exploration after failed endoscopic stone extraction. Surg Endosc. 2008; 22: 1826–1831 [DOI] [PubMed] [Google Scholar]