Abstract
Virtual blood bank is the computer-controlled, electronically linked information management system that allows online ordering and real-time, remote delivery of blood for transfusion. It connects the site of testing to the point of care at a remote site in a real-time fashion with networked computers thus maintaining the integrity of immunohematology test results. It has taken the advantages of information and communication technologies to ensure the accuracy of patient, specimen and blood component identification and to enhance personnel traceability and system security. The built-in logics and process constraints in the design of the virtual blood bank can guide the selection of appropriate blood and minimize transfusion risk. The quality of blood inventory is ascertained and monitored, and an audit trail for critical procedures in the transfusion process is provided by the paperless system. Thus, the virtual blood bank can help ensure that the right patient receives the right amount of the right blood component at the right time.
Keywords: Computer crossmatch, laboratory information system, virtual blood bank
INTRODUCTION
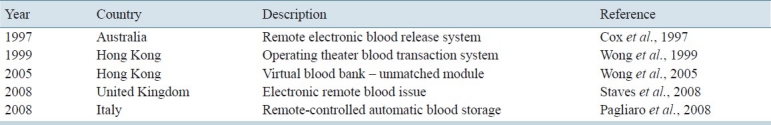
The term “virtual transfusion” first appeared in an editorial of Transfusion in 1997[1] in response to an article by Cox et al, on remote electronic blood release system.[2] Subsequently, several groups have published their experience on virtual blood bank[3–6] [Table 1], which is basically an extension of computer crossmatch with electronically controlled release of blood for transfusion at a remote site. The advent of technology and informatics has thus realized the possibility of real-time delivery and release of compatible and even unmatched blood for transfusion at remote sites and also end-to-end electronic control of the whole transfusion process.
Table 1.
Published experience on virtual blood banks
BACKGROUND
The antiglobulin phase of serologic crossmatch was traditionally considered the definitive test of compatibility. Subsequently, it was shown that the test could be omitted if no clinically significant antibody was detected by the antiglobulin phase in antibody screen.[7,8] Immediate spin was added as a safeguard against ABO incompatibility between the recipient serum and donor red cells. It was then shown that the immediate spin could be replaced by repeat ABO typing and computer checking of donor-recipient ABO compatibility before blood issue thus eliminating the need of testing the recipient serum against donor red cells.[9,10] This has led to the development of computer crossmatch, which is a combination of antibody screen, repeat ABO typing and electronic confirmation of ABO compatibility.
Although there is much variation in the system requirements for computer crossmatch in different countries, most blood banks require two separate ABO types, which are obtained from the patient's current specimen and historic record or from two specimens taken at two different occasions or from the current specimen with the ABO typing performed twice by different personnel or with different reagents. The computer logic should be able to check and validate the presence of (A) two concordant ABO typing results, (B) ABO compatibility between recipient and donor and (C) antibody screen negativity (with its validity set within a limited period of time).[11] Some systems require the software not to display the previous ABO typing result unless the current result has been entered.[12] . The software is tested (against the existing transfusion rules and different scenarios) and validated on-site before being put into operation. There should be appropriate measures to ascertain correct labeling of the donor units either at the blood collection service during blood component production or at the blood bank before its release for transfusion.
Computer crossmatch has paved the way for the development of virtual blood bank that allows the release of computer-crossmatched blood for transfusion at places away from the central blood bank and without on-site technical support.
NETWORKED INFORMATION MANAGEMENT SYSTEM FOR THE BLOOD BANK
The availability of a safe and secure networked information management system is yet another prerequisite for the development of virtual blood bank as it allows remote and real-time access to patient and blood bank information and provides paperless documentation and continuous monitoring of transfusion-related activities. It would suffice to say that the virtual blood bank is an extension of computer crossmatch on the platform of networked information management system and is supported by communication technology and laboratory automation.
Many functions of the traditional hospital transfusion service can extend beyond the walls of the blood bank and even the hospital with the use of networked and interfaced information management system. The blood bank laboratory information system (BBLIS) comprises the software that collects, stores, processes and distributes information related to and generated by the blood bank operations.[13] A basic requirement for transfusion safety is accurate identification of the patient and donor unit. This is facilitated by the use of portable identification devices such as the barcoded identification bracelet with one or more unique patient identifiers readable by a handheld barcode scanner. Barcode labeling will minimize the manual input of data thus eliminating the associated transcription errors. Barcode scanning can serve as an adjunct to manual checking and a prompt to take the operator through each step of patient identification. Major problems related to the use of barcoded identification bracelet are (A) the availability of equipment (barcode scanner and printer) at each point of care and (B) the need to remove the identification bracelet for patient treatment, such as during surgery. It is important to note that electronic control of the transfusion process can only help reduce, but not totally eliminate, human errors. It should never replace human thinking and should be treated only as an adjunct to manual checking and verification.
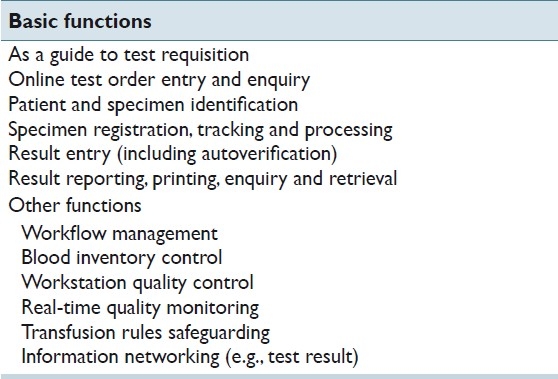
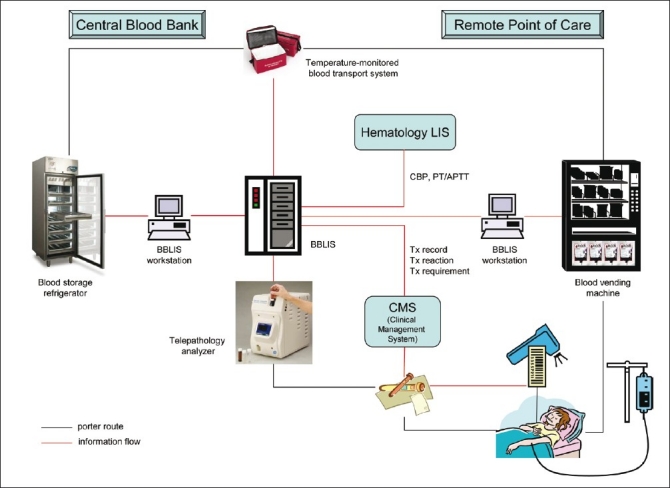
The BBLIS is interfaced bidirectionally with the hospital electronic patient record system, allowing the download of specimen data, patient and physician demographics, the upload of immunohematology test results and reports, and the transfer of test results from the site of testing to that of transfusion. The screen format should be made simple with minimal keyboard activity, and should include safety prompts for standard procedures to prevent the issue of incompatible or unsuitable blood components and to alert the user to special transfusion requirements. The BBLIS can be provided by a vendor or can be built in-house. It is, however, preferable to have in-house support (hematologists, clinical scientists and medical technologists) skilled at adapting the system to fit local needs and to connect more effectively to other information systems within the organization. The BBLIS helps reduce manual input or data transcription and, thus, paperwork and clerical errors. It can provide speedy results and keep accurate, up-to-date records. It also enables web-based connectivity between the central blood bank and the remote sites (satellite blood banks) thus opening up the possibility of virtual blood banking. The functions of the BBLIS are shown in Table 2.
Table 2.
Functions of the blood bank laboratory information system
The computer software and hardware integrity of the BBLIS should be ascertained and safeguarded. Information security and patient privacy should be ensured. The system design and logic should be validated and field tested before being put into operation, and revalidated particularly when there is newly added function, change in algorithms or rules, system upgrade or recovery from unscheduled downtime. It should be designed as a high-availability system with uninterrupted power supply and backup servers or even stand-alone database workstations. A documented manual backup system with the use of photocopy and facsimile and retrospective data entry of all transactions should be planned and drilled.[14] Adequate personnel training and carefully formulated standard operating procedures are essential to avoid misunderstanding and ensure smooth system operation. All these measures can ensure an uninterrupted service and maintain the information integrity, which are essential for a reliable and dependable virtual blood bank.
ELECTRONICALLY CONTROLLED REAL-TIME REMOTE BLOOD RELEASE SYSTEM
It has been shown that most blood banks take at least 30 min to deliver blood to the operating theater (OT), as measured from the time of request by OT personnel.[15] The delay in providing blood for transfusion at the point of care, particularly when it is needed urgently, is undesirable, and may result in overordering and overstocking of blood in order to safeguard against a long delay in blood availability. The concept of a centralized blood bank with crossmatch capacity and remote delivery and release of blood is not new and was in place even before the development of computer crossmatch. Triulzi et al, reported such a centralized transfusion service with a regional blood bank serving three other geographically separated hospitals for non-emergency transfusion.[16] Patient specimens collected from these satellite locations are sent to the central blood bank. A designated portion of the blood inventory at each satellite location would have segments removed and stored at the central blood bank. The segments are used as a source of donor red cells for serologic crossmatch, and the crossmatch result will be printed at the satellite location through interfaced BBLIS. The advantages of such a system are labor cost savings and quality improvement through standardization of best practices. Nevertheless, a stat-testing facility is still required on-site for handling urgent transfusion requests. Later, Cheng et al, implemented a self-service blood ordering system that required manual matching and checking of a computer-generated list of the serial numbers of all group-identical donor units available in the blood bank inventory.[17] Specific donor units are no longer assigned to surgical patients with a valid negative antibody screen. This is probably the first example of extension of computer crossmatch beyond the blood bank, with prompt blood release without the use of pneumatic tube system or on-demand and impromptu porter service. Other measures to bring the blood bank closer to the sites of transfusion include the use of portable blood storage refrigerator[18] and the use of a basket of group O Rh D-negative blood for intraoperative unmatched transfusion.[19]
With the advent of information technology, electronic control of the transfusion process has become possible. The virtual blood bank, which incorporates computer crossmatch and electronic control of blood issue/return at remote sites, has come into play. Characteristics and functions of the virtual blood bank are [Figure 1]:
Figure 1.
Virtual blood bank - toward closing the loop of safe blood transfusion. BBLIS = Blood bank laboratory information system; CBP = complete blood picture; PT = prothrombin time; APTT = activated partial thromboplastin time; Tx = transfusion
Blood Storage
Appropriate numbers of donor units of different ABO groups are stored separately in designated compartments of blood storage refrigerators at the remote site according to the service size and transfusion requirement.
Blood Issue
Non-laboratory staff (often, the nursing staff) will go through identity and security check with the system and scan the patient's identity when blood is required for transfusion. The system software will check with the BBLIS for the patient's eligibility (i.e., ABO/Rh D type, antibody screen negativity and its validity). For non-emergency transfusion, group-identical and electronically crossmatched donor units will be issued for patients with a negative antibody screen. The system will prevent the allocation of ABO non-identical blood and check the concordance of ABO typing results tested on different specimens and/or at different occasions. Some systems may allow the release of group-compatible donor units in the absence of group-identical blood, particularly at small remote sites where an adequate stock of donor units of all ABO groups may be a problem.[2] For patients with specific transfusion requirements such as those with irregular antibodies, only designated donor units will be issued (the designated donor units may have been delivered and stored in a remote refrigerator or they will have to be collected from the central blood bank). The expiry date of the donor unit is checked before its release, and some systems can allocate donor unit closest to the end of its shelf life.[6]
A compatibility label is printed and affixed to the donor unit at the time of blood release.[2,5,6] In some systems, however, no additional tagging or labeling of the donor unit is required; only a computer printout with the patient's demographics, the donor unit's information and compatibility status will be issued for the clinician's confirmation.[3] The barcode on the attached compatibility label and/or the barcode for the donation identification number on the label affixed by the blood collection service is scanned to further ascertain the compatibility.[2,3,5,6] The central blood bank will be alerted of the blood release.
Some systems provide real-time blood counts to the clinicians through wireless-linked handheld computers.[20] Algorithms incorporated in the prescription guidelines and based on the patient's most recent hematology test results are used to promote adherence to guidelines for appropriate blood usage.
Unmatched Blood Issue
Some systems can release group O blood for unmatched transfusion.[6] Our group has pioneered the provision of group-identical unmatched blood for intraoperative transfusion during dire emergency.[4] Group O blood will be issued if the blood group of the recipient is not yet known. If the blood group is known (with a historic record in the BBLIS) and has been confirmed from a current specimen, the non-laboratory staff at the remote site will be instructed to take group-identical blood for transfusion and group O blood will no longer be issued. Furthermore, a real-time indication of the expected time for completion of the antibody screen and possible availability of computer crossmatch-compatible blood (for those with a negative antibody screen) will be given once the blood bank has received and registered the specimen and the antibody screen has been processed [Figure 2]. This is estimated from the registration time of the specimen and the promised turnaround time of the antibody screen. Keeping the clinician informed of the progress of the antibody screen will facilitate decision making in emergency transfusion and reduce the need of unmatched blood.[21] The blood bank will be alerted immediately if unmatched blood has been issued.
Figure 2.
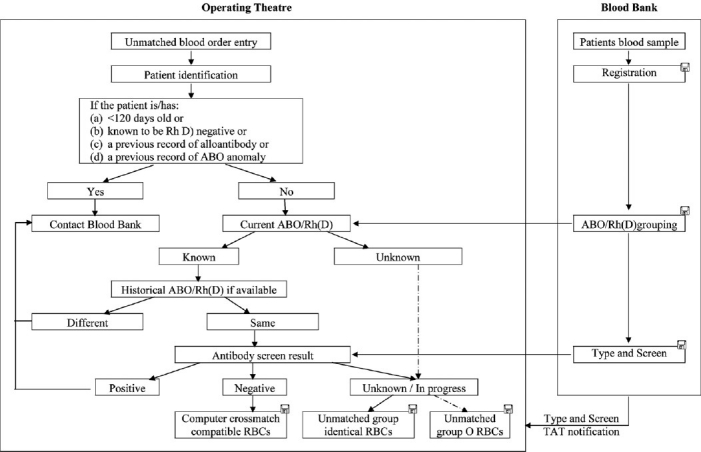
Workflow and audit of remote release of unmatched blood. Electronic records are kept for the activities marked by . RBCs = red cells; TAT = turnaround time
Blood Return and Re-issue
Unused donor units can be returned to the remote refrigerator through the BBLIS. The time when the donor unit leaves the refrigerator will be recorded, and it will be barred from re-issue if the donor unit is returned after 30 min. This will safeguard the integrity of the donor unit and prevent bacterial overgrowth and other problems associated with inappropriate storage. The virtual blood bank has been shown to be able to reduce the crossmatch-transfusion ratio while, at the same time, minimizing blood wastage.[2,3]
Blood Stock Maintenance
The existing stock of each ABO group will be checked automatically at regular intervals and the blood bank staff will be alerted if it falls below a pre-set limit, which is determined by the historic consumption rate and the distribution of ABO group in the population.[3] The stock will be replenished by the blood bank staff accordingly.
Audit Trail and Tracking
Incorrect removal of a donor unit will trigger off the on-site alarm and alert the central blood bank. All transactions and personnel involved will be recorded electronically. Such an electronic audit trail can replace the traditional paper-based documentation system.
Blood Vending Machine
A latest addition to the virtual blood bank is the blood vending machine. The latter consists of two components: (A) an intelligent temperature-controlled blood storage and dispensing refrigerator with computerized controlled electromagnetic door lock and (B) an attached kiosk that is a purpose-built computer terminal with identity card reader and barcode scanner for personnel login and patient identification, process control and compatibility label printing.[5,6] The refrigerator contains a rotating carousel with individually electronically controlled and lockable compartments for undesignated donor units of each ABO group and one compartment for reserved and serologically crossmatched donor units, which enable physical and electronic control of access, allocation and dispensing of group-identical electronically crossmatched or reserved serologically crossmatch-compatible donor units. The blood vending machine allows bidirectional informatics connectivity and ensures that (A) only authorized personnel can gain access, (B) expiry date of donor unit is checked, (C) validity of reserved unit is confirmed, (D) oldest available donor unit is dispensed and (E) inventory and temperature are monitored continuously by the central blood bank. The donor unit will be automatically assigned and dispensed by the refrigerator and labeled at the kiosk. It has further enhanced the safety, efficacy and security of the virtual blood bank as it limits access to only the correct donor units, reduces donor unit expiry and provides an audit trail for the personnel involved and procedures undertaken. The stock can be replenished at the convenience of the blood bank staff who will be alerted when the inventory falls below a pre-set limit. An obstacle to the wider use of such a blood vending machine is probably its cost, which is, at present, several times that of the usual blood storage refrigerator.
Blood Transport System
A pre-cooled refrigerated and continuous temperature-monitored transport system is currently available for providing a complete documented storage history during blood transportation.[22] Although this has yet to be incorporated into the virtual blood bank, it may further ensure a safe and waste-free transfusion.
Most ABO-incompatible transfusions occur because of errors of sampling or blood administration. In order to close the loop, it is important to have an end-to-end control of blood sampling, delivery and administration.[23,24] This involves the use of a handheld computer/barcode scanner and a portable barcode label printer (as described in the previous section), and relies on the application of password, identification bracelet, smartcard, barcode scanning, electronic checking, electronic process control/constraint, electronic lock and procedure audit.
ZERO-RISK, ZERO-TIME-LAG AND ZERO-WASTAGE TRANSFUSION: A MYTH OR A REALITY?
The benefits of a virtual blood bank are manifold: (A) increased safety - restricted access to only the correct donor units, (B) increased efficiency – expressed delivery of crossmatch-compatible and even unmatched blood, (C) increased cost-effectiveness – reduced overall blood inventory, usage and wastage and (D) increased security for remote blood storage with audit trail and tracking. In fact, all virtual blood banks currently in use have demonstrated remarkable success in terms of reducing the time for delivery of donor units to remote sites (from over 30 min to <1 min), reducing blood wastage (by 25-30%) and crossmatch-transfusion ratio.[2–5] They remove the need of phone enquiries thus eliminating the error-prone communication for blood ordering and delivery and reducing the stress of both clinical and laboratory staff, particularly at times of emergency or massive transfusion.
Contrary to common belief, it has been shown that increased autonomy of clinicians and enhanced accessibility of blood will not lead to increased usage but rather to more rational request because of increased confidence as an unlimited supply is practically instantly ensured.[3,5] It will thus improve patient care and ensure better utilization of the scarce blood stock. The virtual blood bank enables the provision of an on-demand and need-to-give transfusion service, removing the need of a maximum blood ordering schedule, and helps ensure the compliance with transfusion guidelines and regulatory requirements (from bedside to blood bank). It has been proven safe and no incident of ABO-incompatible transfusion has ever been reported.[2–6] The virtual blood bank (Operating Theatre Blood Transaction System, OTBTS) was first developed and implemented in Hong Kong at the Queen Elizabeth Hospital in 1997.[3] It was later expanded to include an unmatched blood module that allowed emergency order and issue of unmatched blood for intraoperative transfusion in patients who did not yet have a valid type and screen result.[4,21] During the period from May 1997 to November 2010, the OTBTS has issued 37,324 units of blood to 11,282 patients for intraoperative transfusion. Among them, 336 units of unmatched blood (group O:group-identical blood in a ratio of about 2.5:1) has been given for intraoperative transfusion in dire emergency. The average time required for issuing the first unit of blood is 23 s. No delay/error in transfusion or postponement of surgery has been reported. The system has now been installed in a specialist center for joint replacement surgery and two other major acute hospitals in the territory.
Virtual blood banks currently in use are not perfect. For instance, they cannot distribute mini-packs for pediatric patients or other blood components such as platelet concentrates. Furthermore, most systems do not allow the release of group-identical unmatched blood for emergency transfusion. Another concern is the patient identification as the bracelet commonly used by most centers is an inconvenient method, particularly for patients in the OT as it is not always readily accessible for checking and it may sometimes be removed because of the surgical site, and for patients attending the pre-admission clinic in advance of surgery as they will not be wearing the bracelet. The use of biometrics, such as fingerprint technology, or the use of radiofrequency identification will have to be explored. Lastly, it is often necessary to transport specimens from the remote site to the central blood bank for pre-transfusion testing. A telemedicine system is recently available that allows remote inspection and interpretation of pre-transfusion tests, such as those performed by gel technology.[25] This may remove the need of specimen delivery from the remote site.
CONCLUSION
Blood transfusion is a high-risk process because of the complexity of its many procedures (from blood sampling to laboratory testing and blood administration) and the involvement of multiple staff from different departments. The virtual blood bank has taken the full advantage of computer crossmatch, i.e. immediate availability of compatible blood without the need of prior allocation of donor units to designated patients, and has allowed the controlled use of group-identical blood, real-time inventory monitoring and early stock replenishment. The use of barcode or other identification devices can eliminate human errors in data transcription. Electronic process control can help ensure compliance with transfusion guidelines and regulatory requirements. The advent of information technology has enabled us to come closer to the goal of zero-risk, zero-time-lag and zero-wastage transfusion – a goal that was only a dream in the past but might be reachable in the not-so-distant future.[26]
Acknowledgments
The author would like to thank Mr. H. L. Hui for providing the image for Figure 1.
Footnotes
Available FREE in open access from: http://www.jpathinformatics.org/text.asp?2011/2/1/6/76155
REFERENCES
- 1.Shulman IA. The “virtual” transfusion service laboratory. Transfusion. 1997;37:883–5. doi: 10.1046/j.1537-2995.1997.37997454011.x. [DOI] [PubMed] [Google Scholar]
- 2.Cox C, Enno A, Deveridge S, Seldon M, Richards R, Martens V, et al. Remote electronic blood release system. Transfusion. 1997;37:960–4. doi: 10.1046/j.1537-2995.1997.37997454025.x. [DOI] [PubMed] [Google Scholar]
- 3.Wong KF, Lee AW, Hui HL, Chang FK, Mak CS, Kwan AM. Operating Theater Blood Transaction System - a –virtual— blood transfusion service that brings the blood bank to the operating table. Am J Clin Pathol. 1999;112:481–4. doi: 10.1093/ajcp/112.4.481. [DOI] [PubMed] [Google Scholar]
- 4.Wong KF, Kwan AM. Virtual blood banking - a 7-year experience. Am J Clin Pathol. 2005;124:124–8. doi: 10.1309/13CUJ61YRB50B1CT. [DOI] [PubMed] [Google Scholar]
- 5.Staves J, Davies A, Kay J, Pearson O, Johnson T, Murphy MF. Electronic remote blood issue: A combination of remote blood issue with a system for end-to-end electronic control of transfusion to provide a “total solution” for a safe and timely hospital blood transfusion service. Transfusion. 2008;48:415–24. doi: 10.1111/j.1537-2995.2007.01545.x. [DOI] [PubMed] [Google Scholar]
- 6.Pagliaro P, Turdo R. Transfusion management using a remote-controlled, automated blood storage. Blood Transfus. 2008;6:101–6. doi: 10.2450/2008.0029-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wallis JP. Is it time to give up the crossmatch? J Clin Pathol. 2000;53:673–5. doi: 10.1136/jcp.53.9.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Butch SH. Computerization in the transfusion service. Vox Sang. 2002;83:105–10. doi: 10.1111/j.1423-0410.2002.tb05279.x. [DOI] [PubMed] [Google Scholar]
- 9.Butch SH, Judd WJ, Steiner EA, Stoe M, Oberman HA. Electronic verification of donor-recipient compatibility: The computer crossmatch. Transfusion. 1994;34:105–9. doi: 10.1046/j.1537-2995.1994.34294143935.x. [DOI] [PubMed] [Google Scholar]
- 10.Säfwenberg J, Högman CF, Cassemar B. Computerized delivery control-a useful and safe complement to the type and screen compatibility testing. Vox Sang. 1997;72:162–8. doi: 10.1046/j.1423-0410.1997.7230162.x. [DOI] [PubMed] [Google Scholar]
- 11.Ashford P, Gozzard D, Jones J, Revill J, Wallis J, Bruce M. Guidelines for blood bank computing. Transfus Med. 2000;10:307–14. doi: 10.1046/j.1365-3148.2000.00273.x. [DOI] [PubMed] [Google Scholar]
- 12.Butch SH, Judd WJ. Requirements for the computer crossmatch. Transfusion. 1994;34:187. doi: 10.1046/j.1537-2995.1994.34294143958.x. [DOI] [PubMed] [Google Scholar]
- 13.Nightingale M, Prowse C. BCSH: The specification and use of Information Technology (IT) systems in Blood Transfusion Practice. Transfus Med. 2007;17:150. doi: 10.1111/j.1365-3148.2007.00750.x. [DOI] [PubMed] [Google Scholar]
- 14.Zeiler T, Slonka J, Bürgi HR, Kretschmer V. How to maintain blood supply during computer network breakdown: A manual backup system. Transfus Med. 2000;10:283–90. doi: 10.1046/j.1365-3148.2000.00265.x. [DOI] [PubMed] [Google Scholar]
- 15.Novis DA, Friedberg RC, Renner SW, Meier FA, Walsh MK. Operating room blood delivery turnaround time: A College of American Pathologists Q-Probe Study of 12647 units of blood components in 466 institutions. Arch Pathol Lab Med. 2002;126:909–14. doi: 10.5858/2002-126-0909-ORBDTT. [DOI] [PubMed] [Google Scholar]
- 16.Triulzi DJ, Portman WH, Mango PD, Lopez-Plaza I, Hahn LF. Centralized transfusion service: A novel approach to the delivery of transfusion services. Transfus Med Rev. 1995;9:123–30. doi: 10.1016/s0887-7963(05)80051-3. [DOI] [PubMed] [Google Scholar]
- 17.Cheng G, Chiu DS, Chung AS, Wong HF, Chan MW, Lui YK, et al. A novel system for providing compatible blood to patients during surgery: “self-service” electronic blood banking by nursing staff. Transfusion. 1996;36:347–50. doi: 10.1046/j.1537-2995.1996.36496226151.x. [DOI] [PubMed] [Google Scholar]
- 18.Haynes DH, Puckett DH, Monaghan WP. Blood storage and transport using a portable thermoelectric refrigerator: Field testing. Mil Med. 1988;153:86–9. [PubMed] [Google Scholar]
- 19.Weiskopf RB, Webb M, Stangle D, Klinbergs G, Toy P. A procedure for rapid issue of red cells for emergency use. Arch Pathol Lab Med. 2005;129:492–6. doi: 10.5858/2005-129-492-APFRIO. [DOI] [PubMed] [Google Scholar]
- 20.National Health Service Evidence - QIPP. Electronic blood transfusion systems. [Last cited on 2010 Oct 10]. Available from: http//www.evidence.nhs.uk/qualityandproductivity .
- 21.Wong KF, Kwan AM. A procedure for rapid issue of red cells for emergency use. Arch Pathol Lab Med. 2006;130:145. doi: 10.5858/2006-130-145a-APFRIO. [DOI] [PubMed] [Google Scholar]
- 22.Rawlinson PS, Brown G, Paterson G, Clark P. The integration of data logging and transport technology to provide waste-free emergency transfusion support to distant hospital facilities. Transfus Med. 2004;14:323–4. doi: 10.1111/j.0958-7578.2004.00522.x. [DOI] [PubMed] [Google Scholar]
- 23.Davies A, Staves J, Kay J, Casbard A, Murphy MF. End-to-end electronic control of the hospital transfusion process to increase the safety of blood transfusion: Strengths and weaknesses. Transfusion. 2006;46:352–64. doi: 10.1111/j.1537-2995.2006.00729.x. [DOI] [PubMed] [Google Scholar]
- 24.Miyata S, Kawai T, Yamamoto S, Takada M, Iwatani Y, Uchida O, et al. Network computer-assisted transfusion-management system for accurate blood component-recipient identification at the bedside. Transfusion. 2004;44:364–72. doi: 10.1111/j.1537-2995.2004.00652.x. [DOI] [PubMed] [Google Scholar]
- 25.Meza M, Breskvar M, Kosir A, Bricl I, Tasic J, Rozman P. Telemedicine in the blood transfusion laboratory: Remote interpretation of pre-transfusion tests. J Telemed Telecare. 2007;13:357–62. doi: 10.1258/135763307782215370. [DOI] [PubMed] [Google Scholar]
- 26.Wong KF. A total solution for zero-risk, zero-time lag and zero-wastage blood transfusion service? Transfusion. 2006;46:1848. doi: 10.1111/j.1537-2995.2006.00983.x. [DOI] [PubMed] [Google Scholar]


