Abstract
Background:
The goal of our study was to compare the incidence of motor vehicle accidents (MVA), attempted or completed suicides, and injuries inflicted by others between individuals with and without epilepsy.
Methods:
Individuals with and without epilepsy were identified using linked administrative databases between 1996 and 2003 in a Canadian health region with a 1.4 million population. We used a validated epilepsy case definition: anyone who had 2 physician claims, one hospitalization, or one emergency room visit coded with an International Classification of Diseases (ICD)-9-CM or ICD-10 epilepsy code any time during a 2-year period. Four subjects without epilepsy were matched to one patient with epilepsy by age (within 1 year) and sex. The incidence of MVAs, attempted or completed suicides, and inflicted injuries was assessed in 2003–2004. Outcomes were adjusted using the Elixhauser comorbidity index.
Results:
A total of 10,240 individuals with epilepsy and 40,960 individuals without epilepsy were identified. Mean age was 39.0 ± 21.3 years (range 0.12–99.4) and 48.5% were female. One-year odds ratios before and after adjustment for comorbidity were 1.83 (95% confidence interval [CI] 1.33–2.54) and 1.38 (95% CI 0.97–1.96) for MVAs, 4.32 (95% CI 2.79–6.69) and 1.32 (95% CI 0.81–2.15) for attempted or completed suicides, and 3.54 (95% CI 2.66–4.72) and 1.46 (95% CI 1.04–2.03) for injuries inflicted by others.
Conclusion:
In this cohort-controlled population-based study, once important medical and psychiatric comorbidities were adjusted for, people with epilepsy were not more likely to attempt suicide or experience MVAs, but were still more likely to be assaulted compared to those without epilepsy.
Epilepsy accounts for 1% of the total burden of diseases in the world and affects people regardless of age, gender, race, or socioeconomic status. Epilepsy can be associated with serious psychosocial consequences including but not limited to unemployment, poor social relationships, lack of independence, and lower educational achievement.1 Those with epilepsy are also often faced with questions such as whether or not they will be able to drive and whether they may be more at risk for injuries inflicted by others or suicides than those without epilepsy.
Motor vehicle accidents (MVAs) are a concern for those with epilepsy, hence driving restrictions are enforced to varying degrees in these patients. Evidence pointing to a greater risk of MVAs in those with epilepsy is inconsistent among studies.2–4
Suicide accounts for around 1.5% of total deaths worldwide,5 with 10% of deaths in epilepsy being attributed to suicide.6 Suicide was a major cause of death in epilepsy in large population-based cohort studies from the United Kingdom and Sweden.7,8 Studies have shown an increased risk of suicide in those with epilepsy compared to the general population.9–11
To our knowledge, there has only been one study examining the association between homicides and epilepsy.12 This study found that those with epilepsy were more likely to die from a homicide in their home compared to those without epilepsy.
Our group was interested in studying MVAs, suicides, and assaults in those with and without epilepsy as they are all conditions associated with trauma or injuries and are all causes of mortality. The specific objective of our cohort-controlled population-based study was to determine the 1-year incidence of MVAs, attempted or completed suicides, and inflicted injuries in those with and without epilepsy, adjusting for important confounders such as psychiatric comorbidities.
METHODS
Data sources.
The Alberta Health Services Calgary Zone comprises 4 hospitals (3 adult, 1 pediatric), serving a 1.4 million population. The following administrative databases were linked from fiscal years 1996–2003 (i.e., April 1, 1996, until March 31, 2004): Alberta Health Care Insurance Plan Registry, a hospital discharge abstract database, an emergency room visits database, a physician claims database, and the vital statistics database. Due to the availability of universal health care in Alberta, the Alberta insurance registry is nearly complete, and is used as a proxy for the population of Alberta. Individuals who are included in the Alberta Health Care Insurance Registry (>99% of the population) are assigned a Personal Health Number which can be used to link the various databases. The hospital discharge abstract database captures all hospitalized patients' information including but not limited to their demographics, procedures, principal diagnoses, and comorbidities. The emergency rooms visit database captures all visits to the emergency room and also contains diagnoses and procedures. The physician claims database captures all inpatient and outpatient encounters with a physician and includes up to 3 diagnoses. Vital statistics was used to look at suicide-related deaths.
Study population.
Two study populations were identified: persons with epilepsy as cases and persons without epilepsy as controls taking the following steps.
Step 1.
Epilepsy cases were identified using the following International Classification of Diseases (ICD) codes: ICD-9-CM epilepsy code 345 (up to March 31, 2002) or ICD-10 epilepsy codes G40–41 (from April 1, 2002). Convulsion code 780.3 was excluded in this study as we were trying to capture an epilepsy-specific cohort in the 3 databases (physician claims, hospitalization discharge abstracts, and emergency room visits).
Step 2.
To enhance validity of epilepsy cases identification, we only selected patients with either of the above ICD-9-CM or ICD-10 epilepsy codes in 2 physician claims or one hospital discharge abstract record or one emergency room visit record in 2 years (between April 1, 1996, and March 31, 2003). ICD-9-CM and ICD-10 coding for epilepsy has been validated in our hospital and emergency room administrative databases using this methodology with sensitivity and positive predictive values >98%.13
Step 3.
Patients without epilepsy were captured by excluding patients with epilepsy from all recipients of the Alberta Health Care Insurance Plan. Four people without epilepsy were matched to each epilepsy case by age (±1 year) and sex. We excluded all those who had died prior to March 31, 2003. Thus we included all accumulated alive persons with epilepsy and those matched individuals without epilepsy prior to March 31, 2003, and followed them up for 1 year (April 1, 2003–March 31, 2004) for the outcomes of interest (see below: MVA, attempted or completed suicides, and inflicted injuries).
Defining motor vehicle accidents, attempted or completed suicides, and inflicted injuries.
MVAs (traffic accidents only), attempted or completed suicides, and inflicted injuries were defined as any of the mentioned mechanisms that occurred within 1 year after March 31, 2003. ICD-9-CM and ICD-10 codes for motor vehicle accidents, attempted or completed suicides, and inflicted injury codes were used to define each of the mechanisms (table e-1 on the Neurology® Web site at www.neurology.org). The injuries were those in which medical attention was sought in any location, such as an outpatient clinic setting, an emergency department, or during hospitalization. MVA was investigated as 1) passenger, pedestrian, and driver; 2) driver alone. Each of the outcomes was only counted once per patient during the 1-year period (fiscal year 2003). If an individual attempted suicide twice, this person would only be included once in the attempted or completed suicide category. Thus an individual could contribute to one or more of the outcomes categories (i.e., could have been involved in a MVA, attempted suicide, and was the victim of an inflicted injury) but would only be counted once in each category.
Comorbidities were identified for each cohort subject in order to adjust for these in the final statistical model (see statistical analysis below). We used 7 years of data (April 1, 1996–March 31, 2003) including all databases to identify the comorbidities. Comorbidities were defined using ICD-9-CM and ICD-10 coding algorithms based on the modified Elixhauser comorbidity index,14 which includes congestive heart failure, cardiac arrhythmia, valvular disease, pulmonary circulation disorders, peripheral vascular disease, hypertension (uncomplicated and complicated), paralysis, chronic pulmonary disease, diabetes (uncomplicated and complicated), fluid and electrolyte disorders, blood loss anemia, deficiency anemia, alcohol abuse, drug abuse, psychoses, depression, and other neurologic disorders. Presence of these comorbidities was determined by matching diagnostic codes in physician claims, hospital discharge, and emergency room visit databases with the coding algorithms developed by our group.14
Statistical analysis.
Descriptive statistics were used to assess baseline demographics and the distribution of each of the outcomes of interest (MVAs, attempted or completed suicide, and inflicted injuries) in the study population. Adjusted odds ratios (ORs) with their respective 95% confidence intervals (CIs) were calculated for MVAs, attempted or completed suicides, and inflicted injuries. The difference in incidence of each outcome between subjects with and without epilepsy was first tested using the χ2 method and then using logistic regression analysis after adjustment for comorbidities. Binary coded indicator variables (1 = outcome present; 0 = outcome not present) for the 3 outcomes of interest were used for the logistic regression analysis. For the univariate analysis, p values were adjusted for multiple comparisons using the Bonferroni method (p ≤ 0.002). Significance for the multivariate logistic regression adjusting for comorbidities (Elixhauser comorbidities) was set at p ≤ 0.05.
Standard protocol approvals, registrations, and patient consents.
Ethical approval was obtained for the study from our Medical Bioethics Board (study #E20747).
RESULTS
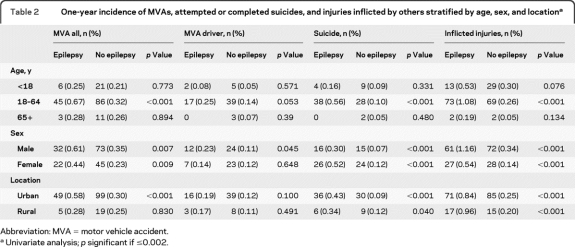
A total of 10,240 subjects with epilepsy were identified using our case definition and 40,960 controls matched for age and sex. The mean age was 39.0 ± 21.3 (SD) years with a range of 0.12–99.4 years. Men represented 51.5% of subjects. All comorbidities were significantly higher in those with epilepsy compared to those without epilepsy (p < 0.001) (table 1).
Table 1.
Characteristics of patients with and without epilepsya
Univariate analysis; p significant if ≤0.002.
All Elixhauser comorbidities are significantly different between cases and controls at the p < 0.001 level.
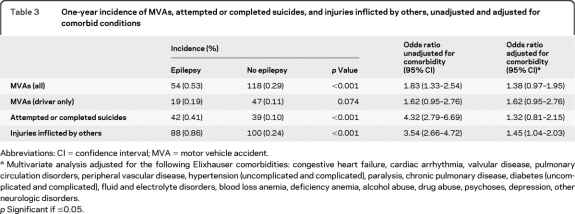
Table 2 shows the 1-year incidence of MVAs, attempted or completed suicides, and inflicted injuries stratified by age, gender, and geographic area in urban (living in Calgary) vs rural (outside of Calgary) dwelling. Univariate subgroup analyses corrected for multiple comparisons showed that overall MVAs (with subjects as a passenger, pedestrian, or driver) were not significantly higher in males and females with epilepsy compared to males and females without epilepsy (male: 0.61% vs 0.35%, p = 0.007; female: 0.44% vs 0.23%, p = 0.009). However, overall MVAs were significantly higher in those aged 18–64 with epilepsy compared to those aged 18–64 without epilepsy (0.67% vs 0.32%, p < 0.001). Overall MVAs were significantly higher in urban Calgary for those with epilepsy compared to those in urban Calgary without epilepsy (0.58% vs 0.30%, p < 0.001).
Table 2.
One-year incidence of MVAs, attempted or completed suicides, and injuries inflicted by others stratified by age, sex, and locationa
Abbreviation: MVA = motor vehicle accident.
Univariate analysis; p significant if ≤0.002.
Overall attempted or completed suicides were also significantly higher in both males and females with epilepsy compared to those without epilepsy (male: 0.30% vs 0.07% p < 0.001, female: 0.52% vs 0.12%, p < 0.001). The incidence of attempted or completed suicides was significantly higher in those aged 18–64 with epilepsy compared to those in the same age group without epilepsy (0.56% vs 0.10%, p < 0.001), but not in the other age groups (table 2). The incidence of attempted or completed suicides was also significantly higher in those who lived in urban Calgary with epilepsy compared to those in the same geographic area without epilepsy (0.43% vs 0.09%, p < 0.001).
Inflicted injuries were more likely in both males and females with epilepsy compared to males and females without epilepsy (male: 1.16% vs 0.34%, p < 0.001; female: 0.54% vs 0.14%, p < 0.001). Those between the ages of 18 and 64 with epilepsy were more likely to experience an inflicted injury compared to those without epilepsy (1.08% vs 0.26%; p < 0.001). Inflicted injuries were also more likely in those with epilepsy in both urban and rural Calgary compared to those without epilepsy (urban: 0.84% vs 0.25%, p < 0.001; rural: 0.96% vs 0.20%, p < 0.001).
Sex and age interactions were sought for all the outcomes but none were significant (results not shown).
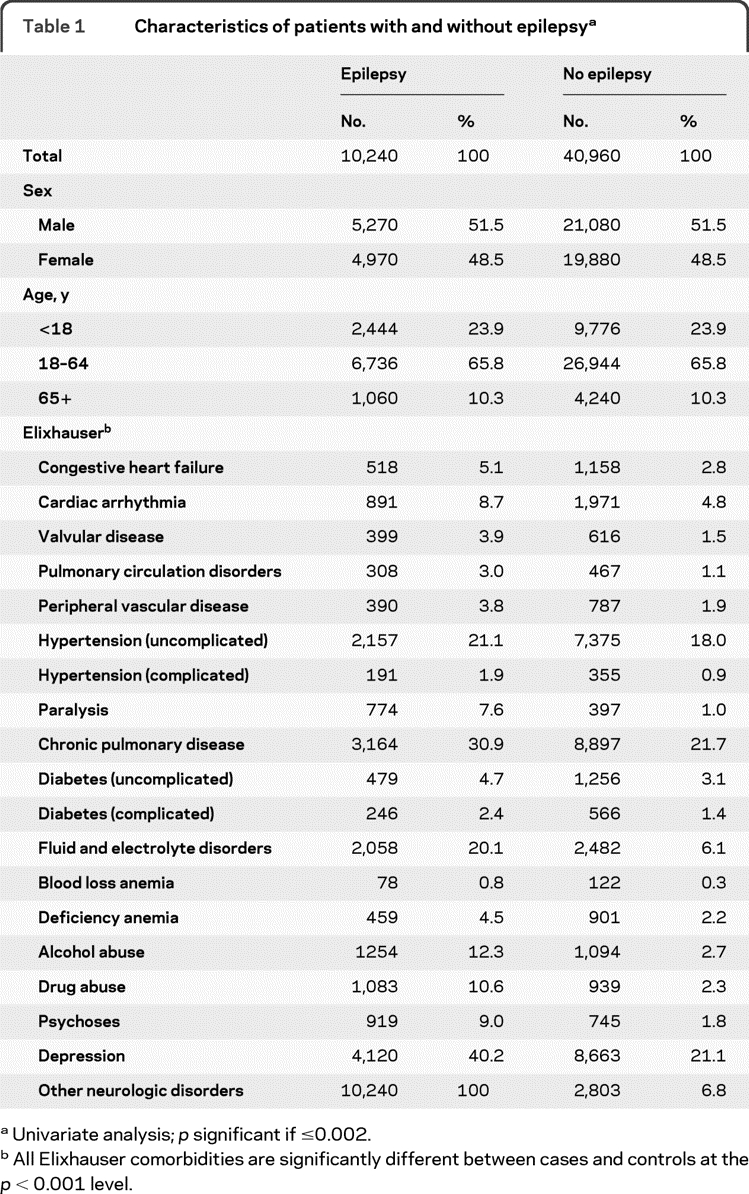
The results of the univariate analysis are shown in table 3 for each of the outcomes of interest: incidence of MVAs with the subjects as passenger, pedestrian, and driver was 0.53% among those with epilepsy and 0.29% among those without epilepsy (p < 0.001); incidence of MVAs among subjects as drivers was 0.19% among those with epilepsy and 0.11% in those without epilepsy (p = 0.074); incidence of attempted or completed suicides was 0.41% among those with epilepsy and 0.10% among those without epilepsy (p < 0.001). There was one completed suicide among those with epilepsy but 5 (0.01%) completed suicides among those without epilepsy. The incidence of inflicted injuries was 0.86% among those with epilepsy and 0.24% in those without epilepsy (p < 0.001). For a list of inflicted injuries and manners of completed or attempted suicide (n, %) in each group, see table e-2.
Table 3.
One-year incidence of MVAs, attempted or completed suicides, and injuries inflicted by others, unadjusted and adjusted for comorbid conditions
Abbreviations: CI = confidence interval; MVA = motor vehicle accident.
Multivariate analysis adjusted for the following Elixhauser comorbidities: congestive heart failure, cardiac arrhythmia, valvular disease, pulmonary circulation disorders, peripheral vascular disease, hypertension (uncomplicated and complicated), paralysis, chronic pulmonary disease, diabetes (uncomplicated and complicated), fluid and electrolyte disorders, blood loss anemia, deficiency anemia, alcohol abuse, drug abuse, psychoses, depression, other neurologic disorders.
p Significant if ≤0.05.
Unadjusted ORs and adjusted ORs (for comorbidity using the Elixhauser index) are shown in table 3. Unadjusted ORs were higher for all outcomes of interest in people with epilepsy except for MVAs with subjects as drivers (table 3). However, after adjusting for comorbid conditions using the Elixhauser index, which includes psychiatric comorbidities, ORs (95% CI) were not significantly different between persons with and without epilepsy for MVAs (with subject as passengers, pedestrians, and drivers) 1.38 (0.97–1.96), MVAs (drivers) 1.62 (0.95–2.76), and attempted or completed suicides 1.32 (0.81–2.15). Only inflicted injuries remained significantly higher in those with epilepsy OR 1.46 (1.04–2.03).
DISCUSSION
In our population-based study looking at the association between epilepsy and MVAs, attempted or completed suicides, and inflicted injuries we found that 1) those with epilepsy were not more likely to be involved in a MVA compared to the general population; 2) people with epilepsy were not more likely to attempt or complete suicide overall compared to those without epilepsy after adjusting for comorbidities including psychiatric comorbidities; 3) people with epilepsy are 1.5 times more likely to be assaulted compared to those without epilepsy.
Previous studies examining the association between MVAs and epilepsy have reported inconsistent results. Some studies have reported no increase in the risk of MVAs in those with epilepsy.1,15 Using 1995–1997 data from the Centers for Disease Control and Prevention, an average of 44,027 US drivers were reported to have died annually from motor vehicle crashes.15 Only 86 of these were seizure-related, accounting for only 0.2% of fatal crashes. Other medical causes such as diabetes had an average of 0.3% fatal crashes, cardiovascular and hypertensive disorders accounted for 4.1%, and 30.5% were alcohol-related.15 On the contrary, some studies report an association between MVAs and epilepsy.3,4 Furthermore, one retrospective cohort study including epilepsy cases (n = 159) and controls (n = 559) matched for age, gender, place of residence, and exposure period found that those with epilepsy were 7 times more likely to be treated at a casualty department following a MVA compared to the control cohort (the Danish Central Person Register).4 We did not find a statistically significant increase in the likelihood of MVAs in those with epilepsy compared to our age- and sex-matched controls after adjusting for comorbidities using the Elixhauser index (includes psychiatric comorbidities in addition to medical comorbidities). This suggests that comorbidities such as alcohol and drug abuse may be important contributing factors in those with epilepsy who sustain a MVA. Other confounders such as long seizure-free intervals, reliable auras, and having had recent antiepileptic drug modifications have all been found to decrease the odds of MVAs in those with epilepsy.16 We could not adjust for the latter variables in our study.
Our second outcome of interest was attempted and completed suicides. Although epilepsy was associated with suicide in our unadjusted model, this association was no longer significant after adjusting for comorbidities (including medical and psychiatric comorbidities) using the Elixhauser index (OR 1.32, 95% CI 0.81–2.15). This highlights the importance of adjusting for mental health conditions in any studies looking at suicide as an outcome. The importance of such risk adjustment is exemplified in a recent study where the incidence of suicide-related events in those on antiepileptic drug was assessed.17 Suicide-related events were higher in those with epilepsy (whether on or off antiepileptic drug treatment) compared to those without epilepsy initially, but not after adjusting for mental health disorders.17 A meta-analysis of 74 articles looking at suicide and epilepsy found that the incidence of suicide is increased in those with epilepsy with an overall standardized mortality ratio (SMR) of 3.3 (95% CI 2.8–3.7).11 However, most studies included did not adjust for a psychiatric history in their analysis. The SMR was significantly increased in people in epilepsy institutions (SMR 4.64, 95% CI 2.87–7.10), people with temporal lobe epilepsy (SMR 6.57, 95% CI 1.79–16.8), people post temporal lobe resection (SMR 13.9, 95% CI 8.93–20.74), and in those with other types of epilepsy surgery (SMR 6.37, 95% CI 3.06–11.72).11 One large population-based study also reported an association between epilepsy and suicide (risk ratio 3.17, p < 0.001), but the risk of suicide was especially high, not surprisingly, in those with epilepsy who also had a concurrent history of psychiatric comorbidities (rate ratio 29.2, p < 0.0001).9 Similar findings were reported in a Swedish case-control study where a 9-fold increase in the risk of suicide was reported in those with epilepsy who also had a mental health condition.18 Our group previously (2007) reported a 25% lifetime prevalence of suicidal ideation in people with epilepsy compared to 13.3% in those without epilepsy, using population-based national health survey data.19 This may explain the higher incidence of attempted suicide in people with epilepsy in some studies, although adjustment for psychiatric comorbidities is crucial in any studies looking at the association between suicide and any chronic conditions such as epilepsy.
To date, there has only been one study that explored the association between homicides and epilepsy compared to those without epilepsy.12 In that study, patients with epilepsy were more likely to die from a homicide in their own home as compared to those without epilepsy (relative risk ratio of 2.29, p < 0.001).12 Our study also found that those with epilepsy are more likely (OR = 1.5) to sustain inflicted injuries compared to those without epilepsy. Although attitudes toward epilepsy have improved over time, epilepsy misconceptions, stigma, and discrimination are still evident against those with epilepsy, and may explain why those with epilepsy are more likely to be assaulted.20 In one study, 63% of school children believed that those with epilepsy were more likely to be bullied compared to those without epilepsy.21 Psychosocial difficulties leading to social isolation, depression, anxiety, and other neuropsychiatric comorbidities may also render these individuals more vulnerable in general.22 It may also be that those with epilepsy become exposed and helpless due to a seizure in public and as a result can be assaulted or taken advantage of during periods of ictal or postictal agitation and confusion.
There are strengths and limitations to our study. Miscoding of epilepsy in administrative databases could be an issue; however, we have validated ICD-9-CM and ICD-10 epilepsy coding in our region.13 Another limitation of our study is that we only studied the incidence of inflicted injuries, attempted or complete suicides, and MVAs over a 1-year period. Longer follow-up would be of greater benefit. We did not have the ability to do subgroup analysis by epilepsy severity, thus we cannot tell if patients with only sporadic seizures are underrepresented, compared to those with refractory epilepsy. In addition, our study only captures outcomes in which medical attention was sought, thus likely capturing more severe outcomes. Finally, the results may not be generalizable to other regions or countries where driving laws, social structure, and epilepsy care may differ. Despite these limitations, our study is truly population-based, and captured >99% of the population in the region, eliminating selection bias. All diagnoses in our study are physician-based and the results are likely to represent a more accurate picture than those derived from health surveys or self-report.
Supplementary Material
Editorial, page 770
Supplemental data at www.neurology.org
- CI
- confidence interval
- ICD
- International Classification of Diseases
- MVA
- motor vehicle accident
- OR
- odds ratio
AUTHOR CONTRIBUTIONS
Statistical analysis was conducted by Dr. Mingfu Liu.
DISCLOSURE
Dr. Kwon and Dr. Liu report no disclosures. Dr. Quan serves as Associate Editor of BMC Health Services Research and has received salary support from an Alberta Innovation Health Solutions Health Scholar Award. Dr. Thoo reports no disclosures. Dr. Wiebe serves on the editorial boards of Neurology®, Epileptic Disorders, Epilepsy & Behavior, and Canadian Journal of Neurological Sciences and receives research support from the Alberta Heritage Foundation for Medical Research, Canadian Institutes of Health Research, and University of Calgary (Hopewell Professorship of Clinical Neurosciences Research). Dr. Jetté serves on the editorial board of Epilepsia and receives salary/research support from present Alberta Innovates Health Solutions, Canadian Institutes for Health Research, and the University of Calgary.
REFERENCES
- 1. Hinnell C, Williams J, Metcalfe A, et al. Health status and health-related behaviors in epilepsy compared to other chronic conditions: a national population-based study. Epilepsia 2010;51:853–861 [DOI] [PubMed] [Google Scholar]
- 2. Taylor J, Chadwick D, Johnson T. Risk of accidents in drivers with epilepsy. J Neurol Neurosurg Psychiatry 1996;60:621–627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hansotia P, Broste SK. The effect of epilepsy or diabetes mellitus on the risk of automobile accidents. N Engl J Med 1991;324:22–26 [DOI] [PubMed] [Google Scholar]
- 4. Lings S. Increased driving accident frequency in Danish patients with epilepsy. Neurology 2001;57:435–439 [DOI] [PubMed] [Google Scholar]
- 5. Murray C, Lopez AD, Mathers CD, Stein C. The global burden of disease 2000 project: aims, methods and data sources. 2000. [updated 2000; cited]. Available at: http://www.who.int/healthinfo/paper36.pdf Accessed May 25, 2010
- 6. Robertson M. Suicide, Parasuicide, and Epilepsy. Philadelphia: Lippincott-Raven; 1997 [Google Scholar]
- 7. White SJ, McLean AE, Howland C. Anticonvulsant drugs and cancer: a cohort study in patients with severe epilepsy. Lancet 1979;2:458–461 [DOI] [PubMed] [Google Scholar]
- 8. Nilsson L, Tomson T, Farahmand BY, Diwan V, Persson PG. Cause-specific mortality in epilepsy: a cohort study of more than 9,000 patients once hospitalized for epilepsy. Epilepsia 1997;38:1062–1068 [DOI] [PubMed] [Google Scholar]
- 9. Christensen J, Vestergaard M, Mortensen PB, Sidenius P, Agerbo E. Epilepsy and risk of suicide: a population-based case-control study. Lancet Neurol 2007;6:693–698 [DOI] [PubMed] [Google Scholar]
- 10. Mainio A, Alamaki K, Karvonen K, Hakko H, Sarkioja T, Rasanen P. Depression and suicide in epileptic victims: a population-based study of victims during the years 1988–2002 in northern Finland. Epilepsy Behav 2007;11:389–393 [DOI] [PubMed] [Google Scholar]
- 11. Bell GS, Gaitatzis A, Bell CL, Johnson AL, Sander JW. Suicide in people with epilepsy: how great is the risk? Epilepsia 2009;50:1933–1942 [DOI] [PubMed] [Google Scholar]
- 12. Bowman SM, Aitken ME, Sharp GB. Disparities in injury death location for people with epilepsy/seizures. Epilepsy Behav 2010;17:369–372 [DOI] [PubMed] [Google Scholar]
- 13. Jetté N, Reid AY, Quan H, Hill MD, Wiebe S. How accurate is ICD coding for epilepsy? Epilepsia 2010;51:62–69 [DOI] [PubMed] [Google Scholar]
- 14. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005;43:1130–1139 [DOI] [PubMed] [Google Scholar]
- 15. Sheth SG, Krauss G, Krumholz A, Li G. Mortality in epilepsy: driving fatalities vs other causes of death in patients with epilepsy. Neurology 2004;63:1002–1007 [DOI] [PubMed] [Google Scholar]
- 16. Krauss GL, Krumholz A, Carter RC, Li G, Kaplan P. Risk factors for seizure-related motor vehicle crashes in patients with epilepsy. Neurology 1999;52:1324–1329 [DOI] [PubMed] [Google Scholar]
- 17. Arana A, Wentworth CE, Ayuso-Mateos JL, Arellano FM. Suicide-related events in patients treated with antiepileptic drugs. N Engl J Med 2010;363:542–551 [DOI] [PubMed] [Google Scholar]
- 18. Nilsson L, Ahlbom A, Farahmand BY, Asberg M, Tomson T. Risk factors for suicide in epilepsy: a case control study. Epilepsia 2002;43:644–651 [DOI] [PubMed] [Google Scholar]
- 19. Tellez-Zenteno JF, Patten SB, Jetté N, Williams J, Wiebe S. Psychiatric comorbidity in epilepsy: a population-based analysis. Epilepsia 2007;48:2336–2344 [DOI] [PubMed] [Google Scholar]
- 20. Jacoby A. Stigma, epilepsy, and quality of life. Epilepsy Behav 2002;3:10–20 [DOI] [PubMed] [Google Scholar]
- 21. Austin JK, Shafer PO, Deering JB. Epilepsy familiarity, knowledge and perceptions of stigma: report from a survey of adolescents in the general population. Epilepsy Behav 2002;3:368–375 [DOI] [PubMed] [Google Scholar]
- 22. Moore PM, Baker GA. The neuropsychological and emotional consequences of living with intractable temporal lobe epilepsy: implications for clinical management. Seizure 2002;11:224–230 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.