Abstract
Castration experiments in rodents demonstrate that the stromal vasculature is critical to the androgen-mediated prostate growth regulation. However, the role of angiogenesis inhibitors, such as thrombospondin-1 (TSP-1), in this process is unclear. TSP-1 is a multi-functional glycoprotein that can function as a potent angiogenesis inhibitor and an in vivo activator of latent transforming growth factor-β (TGF-β) in some tissues. Based on these observations, we hypothesized that TSP-1 regulated androgen withdrawal-induced prostate regression and that this process was mediated not only through anti-angiogenic activity but also through TGF-β activation. To test this, we evaluated angiogenic activity in human prostate epithelial and stromal cells treated with androgens and hypoxia in vitro. TSP-1 knockout mice were characterized to investigate the in vivo functions of TSP-1. In vitro, we found that androgens and hypoxia differentially regulated TSP-1 and angiogenic activity. Androgens stimulated normal epithelial cell, but inhibited normal stromal cell, angiogenic activity. Conversely, hypoxia stimulated stromal while inhibiting epithelial activity. Thus, in vivo, net angiogenic activity must reflect cellular interactions. And, we found that media conditioned by epithelial cells grown under normoxic conditions stimulated stromal cell angiogenic activity, and if epithelial cells were grown under hypoxic conditions, stromal activity was further increased. TSP-1 levels, however, were unchanged. In vivo, TSP-1 loss in a mouse model led to prostate epithelial hyperplasia by three months of age with only a modest stromal effect. Androgens suppressed TSP-1 as expression increased following castration in both normal mouse prostate and in human prostate cancer tissues. In addition, TSP-1 expression corresponded to increased TGF-β activation in mouse tissues, specifically in the stromal compartment. These data demonstrate a critical role for TSP-1 in prostate epithelial and stromal growth regulation through angiogenic inhibition and activation of latent TGF-β. Therefore, loss of TSP-1 during tumorigenesis would eliminate two barriers to cancer progression.
Keywords: Angiogenesis, Cancer, Prostate, Thrombospondin-1, Transforming growth factor-β, Vascular endothelial growth factor
Androgens stimulate prostate growth during development, and maintain the gland in adulthood. This modulation of prostate growth by androgens is mediated in part through regulation of angiogenesis. In the normal adult prostate, blood vessels are maintained in a quiescent state in the stroma by a predominance of angiogenic inhibitors over inducers in the tissue milieu. Induction of angiogenesis is necessary for tumor progression, and supporting this, many studies have shown that increased microvascular density (MVD) has prognostic value in prostate cancer (PCa) patients.1-4 We have previously shown that, compared to normal prostate epithelial cells, the balance of angiogenic mediators is altered in PCa cells;5,6 however, the stromal contribution to angiogenesis has not been well studied.
In the normal rodent prostate, androgen withdrawal induces endothelial cell apoptosis and vascular regression prior to epithelial cell apoptosis.7-13 The initial vascular regression is likely due to a sharp decrease in levels of the angiogenesis inducer, vascular endothelial growth factor (VEGF).14 In the rat prostate, the microvascular endothelial cells do not express the androgen receptor.15,16 Thus, rather than a direct effect on the endothelial cells, the effects of androgen withdrawal are likely mediated through the androgen receptor-positive epithelial and stromal cells. Supporting this, androgen treatment does stimulate VEGF expression in normal prostate epithelial cells and in androgen-sensitive PCa cells.12,17 However, in the rat model, VEGF levels rebound to baseline by 3 days post-castration.18-20 This rebound is likely due to the tissue hypoxia resulting from the vascular regression.18-20 However, despite the hypoxia-induced increase in VEGF, vascular regression continues. These observations indicate that other angiogenic mediators must participate in suppressing the vasculature. We have previously shown increased expression of the angiogenesis inhibitor, pigment epithelium-derived factor (PEDF), following androgen withdrawal in both rodent and human PCa tissues,6 thus, identifying one inhibitor in the continued regression. We have also observed that another angiogenesis inhibitor, thrombospondin-1 (TSP-1), is strongly expressed in normal prostate tissues, and this expression is down-regulated in human PCa tissues.5 In vitro, the TSP-1 secreted by normal prostate epithelial cells functions as an angiogenesis inhibitor.5 Colombel et al. have observed increased TSP-1 expression following castration in a rat model,21 and in PCa patients receiving androgen deprivation therapy (ADT), tissue levels of TSP-1 increased while VEGF decreased compared to those patients who had no hormone therapy.4 These observations suggest that TSP-1 could be a second angiogenesis inhibitor functioning in the continued vascular regression. However, the direct effect of androgens and hypoxia on TSP-1 regulation and angiogenic activity in normal prostate epithelial and stromal cells have not been investigated.
TSP-1 is a multifunctional glycoprotein secreted by a variety of cell types including endothelial and epithelial cells, fibroblasts and smooth muscle cells,22 so its inhibitory effects on the prostate are unlikely to be through angiogenic regulation alone. TSP-1 activates latent transforming growth factor-β (TGF-β) in vivo in some tissues,23-25 and TGF-β inhibits proliferation and stimulates apoptosis of normal prostatic epithelial cells and functions in stromal differentiation. In the early stages of PCa, TGF-β inhibits tumor progression.26 Therefore, TSP-1 activation of TGF-β could be critical in regulating prostate growth. Like TSP-1, TGF-β levels increase in the human prostate following castration,27 suggesting that TGF-β may function in the regression process. Interestingly, in normal rat prostatic epithelial cells, either 1α,25-dihydroxy vitamin D3 or retinoic acid increased both TSP-1 and TGF-β expression, and the increase in TSP-1 could be inhibited by anti-TGF-β antibodies.28 These data suggest coordinated regulation between these molecules in the prostate.
Based on the above observations, we hypothesized that the angiogenesis inhibitor TSP-1 plays a major role in prostate growth and homeostasis and has a critical role in the androgen withdrawal response. Moreover, function of TSP-1 in both epithelial and stromal cells was mediated not only through its anti-angiogenic activity but also, in part, through its activation of latent TGF-β. To test this hypothesis, we evaluated the in vitro angiogenic activity of normal prostate epithelial cells and cancer epithelial cells as well as normal stromal cells to the two stimuli important in the castration response – androgen and hypoxia. To evaluate the function of TSP-1 in the prostate in vivo we used a surgical castration model and characterized the prostate phenotype of TSP-1 knockout (KO) mice.
MATERIALS AND METHODS
Cell Culture
Human normal prostate epithelial and stromal cell strains and dermal microvascular endothelial cells were purchased from Lonza (Walkersville, MD) and maintained per the manufacturer’s instructions. PCa cell lines DU145, LNCaP and PC-3 were obtained from the American Type Culture Collection and maintained in Dulbecco’s Modified Eagle Medium plus 10% fetal bovine serum and antibiotics. Short-term cultures of normal prostate stromal cells were established as described.5,6 Androgen treatments were performed using the testosterone derivative, dihydrotestosterone (DHT) at 0-10−7 M as previously described.6 For hypoxia experiments, normoxia was standard culture conditions (20% O2), and hypoxia was induced by growth at 0.5% O2 in a hypoxia chamber or by treatment with 100 μM cobalt chloride (CoCl), a chemical mimic of hypoxia.29 TGF-β neutralizing antibody (Genzyme) was used at 10 μg/ml. Serum-free conditioned media was collected as described.5,6 Results were analyzed from at least two independent experiments on each cell type with consistent results.
Angiogenesis Assay
Angiogenic activity in the conditioned media was evaluated using the microvascular endothelial cell migration assay as previously described.5 Serum-free medium, containing 0.1% bovine serum albumin (BSA), served as the control for background migration, and human VEGF (250-500 pg/ml) or basic fibroblast growth factor (bFGF, 15 ng/ml) (R&D Systems) served as the positive control (250-500 pg/ml). Neutralizing TSP-1 antibody (clone A4.1; Thermo Fisher, Fremont, CA) was used at 40 μg/ml as previously described.5 Controls for the neutralizing activity of this antibody were included in the assays (Supplemental Figure 1a), and we have previously demonstrated the specificity of this antibody to TSP-1.30,31 CoCl2 (0-100 μM) and DHT (0-10−7 M) were also tested alone as controls, and no change in activity from background levels was observed with either substance (Supplemental Figure 1b,c). All samples were tested in quadruplicate, and results were reported as mean percent of maximal migration toward the positive control ± standard error (SE).
Protein Analysis
TSP-1 and PEDF levels in serum-free conditioned media were analyzed by Western blot as previously described.5,6 Equal protein loading was verified by Coomassie staining of identically loaded gels. Purified protein was included on gels (20-30 ng/lane) as a positive control, and BIO-RAD prestained molecular weight markers (Hercules, California) were included as size standards. Relative band intensities were determined using densitometry and values normalized to Coomassie staining intensity. VEGF protein levels in conditioned media were quantified by enzyme-linked immuosorbent assay (ELISA; R&D Systems) per manufacturer’s instructions. Data are presented as the mean ± standard deviation (SD) of duplicate wells.
Animal Model
The construction of the TSP-1 KO mouse has been described.32 Prostate tissues from TSP-1 KO and wildtype C57Bl/6 control mice, the background strain of the TSP-1 KO model, were harvested from mice at 1 to 25 months of age at seven timepoints (1, 3, 6, 9, 12, 18 and 25 months). At least 5 mice per age group were used for comparison between genotypes. Castration was performed on wildtype and TSP-1 KO mice at 5-6 months of age, and prostate tissues were harvested at days 1–21 post-castration (Timepoints 1, 3, 5, 7, 14 and 21 days; n=5 per group). All animals used in these studies were housed in accordance with guidelines from the American Association for Laboratory Animal Care, and all research protocols were approved by the Institutional Animal Care and Use Committee.
Human Prostate Tissues
Human prostate biopsy specimens were taken before and 3-7 days after surgical castration from PCa patients (n=8) at Umea University (Umea, Sweden). Human tissue collection was approved by Internal Review Board committees and all guidelines for patient consent were followed.
Tissue Analysis
Tissues were formalin-fixed, paraffin-embedded and sectioned for staining. A hematoxylin and eosin (H&E) stain was performed for tissue characterization, and an Avidin-Biotin-Peroxidase protocol was used for immunostaining. Antibodies were used as followed: anti-TSP-1 (Thermo Fisher, Freemont, CA), anti-total and anti-active TGF-β (R&D Systems, Minneapolis, MN), proliferating cell nuclear antigen (PCNA) as a measure of cell proliferation, and anti-Factor VIII-related antigen to determine MVD as a measure of angiogenesis (DAKO, Carpenteria, CA). Slides with omission of the primary antibody served as the negative control. Cell types were identified by morphology. TGF-β staining intensity was graded by assigning a grade of 1, 2 or 3 to individual glands with staining positivity as <35%, 36-75% and >75% epithelial cells positive, respectively, and a score assigned by averaging gland intensity. A minimum of 25 glands per mouse were counted. PCNA and MVD were quantified as described.5,6 TSP-1 staining was quantified as previously described.5
Statistical Analysis
Statistical significance of the data was determined using Student t-tests with P values ≤ 0.05 considered significant.
RESULTS
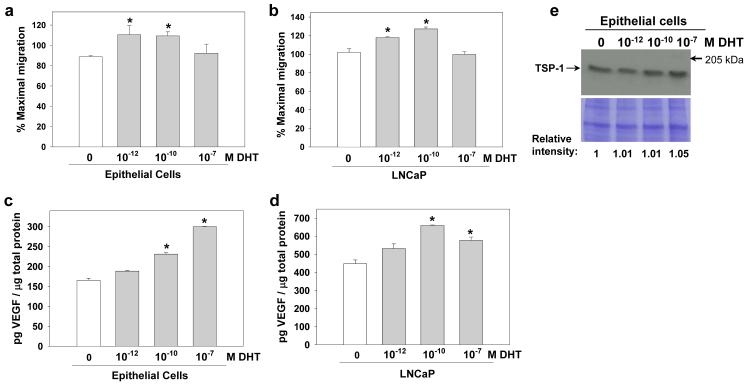
DHT increases angiogenic activity in both normal prostate epithelial and PCa cells
We have observed that TSP-1 localizes to both the stromal and epithelial cells in human prostate tissue and that this TSP-1 expression is decreased in human PCa patient tissues.5 We have also shown that normal prostate epithelial cells (PrEC) secrete TSP-1 in vitro while the androgen-sensitive LNCaP and androgen-insensitive PC-3 PCa cell lines do not.5 Following castration, the drop in androgens initiates vascular regression which in turn induces tissue hypoxia. Therefore, we investigated the effects of both androgen and hypoxia on angiogenic activity and TSP-1 expression. We treated cells with DHT, a potent testosterone derivative, or incubated them in hypoxic conditions and tested angiogenic activity in the serum-free conditioned media using a microvascular endothelial cell migration assay. VEGF and TSP-1 levels by ELISA and Western blot, respectively. In control experiments, DHT alone did not affect the migration of endothelial cells indicating that DHT does not directly elicit angiogenesis (Supplemental Figure 1b). However, DHT treatment did significantly increase angiogenic activity in PrEC at both the 10−12 and 10−10 M DHT doses, low and high proliferative doses, respectively, by more than 20% over untreated cells (Figure 1a; P<0.05). With the 10−7 M DHT treatment, a growth static dose, there was no change in angiogenic activity compared to untreated cells (Figure 1a). Similar results were obtained with androgen-sensitive LNCaP PCa cells. DHT treatment increased angiogenic activity by 16% and 25% at the 10−12 and 10−10 M doses, respectively, and again with no change at the 10−7 M treatment, compared to untreated cells (Figure 1b; P<0.05). Consistent with published studies,7,8,11-13,18 with the 10−10 and 10−7 M DHT treatments, VEGF levels were increased in both normal PrECs, by 40% and 82%, respectively, and in LNCaP cells, by 47% and 29%, respectively (Figure 1c,d; P<0.05). TSP-1 secretion was not significantly altered by DHT treatment in PrEC (Figure 1e). In our previous studies, the angiogenesis inhibitor PEDF was also not altered by DHT treatment.6 Thus, in normal prostate epithelial cells and androgen-sensitive PCa cells, androgens stimulate angiogenic activity, due to increased VEGF levels.
Figure 1.
Androgens induce angiogenic activity in prostate epithelial cells. Serum-free conditioned media were collected from normal prostate epithelial cells (PrEC) and from androgen sensitive LNCaP PCa cells treated with DHT (0-10−7 M). (a,b) Angiogenic activity was assessed in PrEC and LNCaP conditioned media (20 μg/ml) using a microvascular endothelial cell migration assay, and data are presented as the mean ± SE of the percent maximum migration toward the positive control. (c,d) VEGF levels were measured in conditioned media by ELISA. Data are presented as mean ± SD of two replicates. (e) TSP-1 expression was evaluated by Western blot. The lower panel is an identically loaded gel to show equal protein loading between lanes. Protein levels relative to untreated (0 DHT) were determined by densitometry. Protein size standard is indicated. *Significantly different compared to the untreated cells within each experiment, P<0.05.
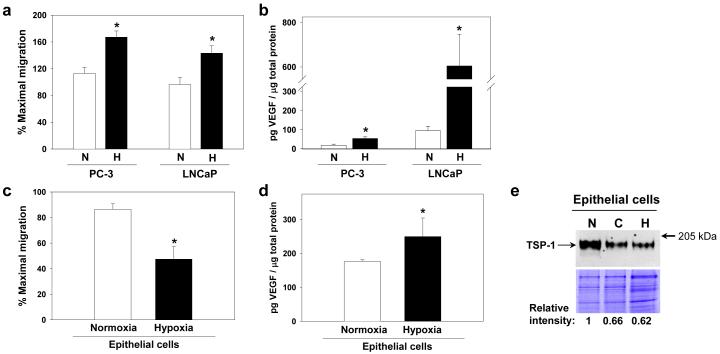
Unlike normal prostate epithelial cells, hypoxia increases angiogenic activity in PCa cells
In most cancer cells, hypoxia increases VEGF and angiogenic activity. In LNCaP cells, hypoxia stimulated angiogenic activity by almost 50% (Figure 2a; P<0.05), and this increase in activity corresponded to a six-fold increase in VEGF (Figure 2b; P<0.05). Since LNCaP cells do not secrete either TSP-1 or PEDF,5,6 the high level of VEGF may be responsible for the angiogenic induction. Similar results were obtained with the androgen-insensitive PC-3 PCa cell line whereby hypoxia increased angiogenic activity by almost 50% and was associated with a three-fold increase in VEGF (Figure 2a,b; P<0.05). While PC-3 cells do not secrete TSP-1,5 they do secrete PEDF, which we have previously reported to be down-regulated by hypoxia,6 thus net angiogenic activity can be augmented by only a modest increase in VEGF.
Figure 2.
Hypoxia inhibits angiogenesis and TSP-1 expression in normal prostate epithelial cells while angiogenesis is induced in PCa cells. Normal prostate epithelial cells (PrEC) and androgen sensitive LNCaP and androgen-insensitive PC-3 PCa cells grown under standard conditions (normoxia, N) or hypoxia-treated conditions [50 μM CoCl2 (C) or in a hypoxia chamber (H), 0.5% O2] and serum-free conditioned media were collected. (a) Angiogenic activity of PC-3 and LNCaP conditioned media (20 μg/ml) was assessed using a microvascular endothelial cell migration assay. Data are presented as mean ± SE of the percent maximum migration toward the positive control. (b) VEGF levels were assayed by ELISA, and data are presented as mean ± SD. (c) Angiogenic activity (d) and VEGF levels were evaluated in PrEC as above. (e) TSP-1 expression was evaluated by Western blot. The lower panel is an identically loaded gel to show equal protein loading between lanes. Protein levels relative to cells grown in normoxia were determined by densitometry. Protein size standard is indicated. *Significantly different compared to cells grown under normoxic conditions, P<0.05.
In striking contrast to the cancer cells, hypoxia suppressed angiogenic activity secreted by normal PrEC by 45% compared to untreated (Figure 2c; P<0.05). While VEGF levels were increased by 41% with hypoxia compared to untreated cells, TSP-1 was inhibited by hypoxia, or CoCl2, a chemical mimetic of hypoxia, by more than 30% (Figure 2d,e). Since we previously observed hypoxic induction of PEDF in these cells,6 it appears that the PEDF is key to maintaining the anti-angiogenic activity in normal epithelial cells under hypoxic stimuli.
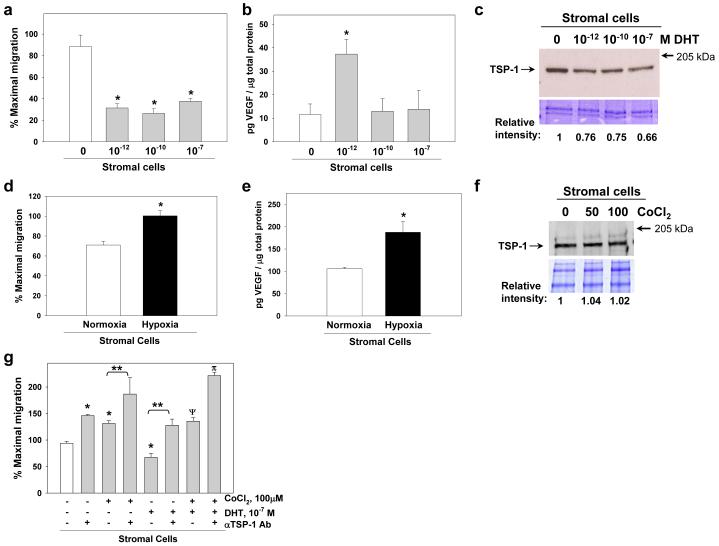
Stromal cell response to DHT and hypoxia opposes that of normal epithelial cells
As TSP-1 localizes to the prostate stroma in vivo and normal prostate stromal cells (PrSC) secrete TSP-1 in vitro,5 we tested the response of PrSC to DHT and hypoxia as above. Surprisingly, in contrast to normal epithelial cells, angiogenesis was significantly decreased in PrSC with DHT treatment by over 55% at all doses tested (10−12 - 10−7 M) compared to untreated cells (Figure 3a; P<0.05). However, VEGF was increased three-fold at 10−12 M DHT, though higher concentrations had no effect compared to untreated cells (Figure 3b; P<0.05). TSP-1 secretion was decreased in a dose-dependent manner by DHT treatment by 25-34% (Figure 3c). Our previous experiments showed that DHT treatment also decreases PEDF in a dose dependent manner.6 Thus, at the 10−12 M DHT concentration, the TSP-1 and PEDF levels are likely still sufficient to inhibit angiogenesis even with the increased VEGF. The inhibition at the higher doses with decreased TSP-1 and PEDF suggests that additional molecules are involved.
Figure 3.
Androgens inhibit while hypoxia induces angiogenic activity in normal prostate stromal cells. Normal prostate stromal cells (PrSC) were treated with DHT (0-10−7 M) or grown under standard conditions (normoxia) or hypoxia-treated conditions [50-100 μM CoCl2 or grown in a hypoxia chamber, 0.5% O2 (hypoxia)] and serum-free conditioned media collected. (a) Angiogenic activity was assessed in conditioned media (20 μg/ml) using a microvascular endothelial cell migration assay. Data are presented as the mean ± SE of the percent maximum migration toward the positive control. (b) VEGF levels were assayed by ELISA. Data are presented as mean ± SD of two replicates. (c) TSP-1 expression was evaluated by Western blot. The lower panel is an identically loaded Coomassie-stained gel to show equal protein loading between lanes. Relative intensity was determined by densitometry. Protein size standard is indicated. Angiogenic activity (d) and VEGF levels (e) were measured as above in hypoxia-treated cells. (f) TSP-1 expression was evaluated as above. (g) The functional activity of TSP-1 in media conditioned by PrSC treated with DHT (10−7 M) and/or CoCl2 (100 μM) was tested by the addition of neutralizing anti-TSP-1 antibody in a migration assay. Data are presented as the mean ± SE of the percent maximal migration toward the positive control. *Significantly different compared to untreated controls in each experiment, P<0.05. **Samples between bars are significantly different, P<0.05. ΨSignificantly increased compared to untreated or DHT-treated, P<0.002, but not significantly different than CoCl2 alone, P=0.64. πSignificantly increased over the combined hypoxia and DHT treatment sample, P<0.00001.
In contrast to DHT treatment, hypoxia significantly increased angiogenic activity by 41% in PrSC (Figure 3d; P<0.05). Consistent with published studies,33 hypoxia treatment increased PrSC VEGF secretion by 77% compared to untreated cells (Figure 3e; P<0.05). However, TSP-1 secretion levels were not altered (Figure 3f). Our previous experiments showed suppression of PEDF by hypoxia in these cells,6 so this taken with the increase in VEGF may explain the net increase in angiogenic activity.
TSP-1 contribution to angiogenic activity in stromal cells
To verify that the TSP-1 secreted by PrSC under DHT or hypoxia treatment had anti-angiogenic function, we tested activity in the presence of neutralizing TSP-1 antibody. Consistent with our previous results,5 neutralizing TSP-1 antibody significantly increased secreted angiogenic activity in untreated cells by 55% (Figure 3g; P<0.05). In this assay, we used CoCl2 (100 μM) to mimic hypoxia, and in control experiments, CoCl2 alone showed no affect on angiogenic activity (Supplemental Figure 1c). In normal stromal cells, CoCl2 treatment stimulated angio-inductive activity by 40% compared to untreated cells (Figure 3g; P<0.05). Addition of neutralizing TSP-1 antibody further increased this activity by 42% and 98% compared to CoCl2-treated and untreated cells, respectively (Figure 3g; P<0.05). Conversely, DHT treatment (10−7 M) inhibited activity by 28%, but addition of neutralizing TSP-1 antibody relieved this inhibition, increasing activity by 90% and 36% compared to DHT-treated and untreated cells, respectively (Figure 3g; P<0.05). When PrSC were subjected to both DHT and CoCl2 treatment, the net response was angio-inductive but was not significantly different from CoCl2 alone (Figure 3g). These data confirm that stromal-derived TSP-1 retains potent anti-angiogenic activity and show that in the setting of androgen withdrawal-induced hypoxia, isolated stromal and epithelial cells have opposing angiogenic activity.
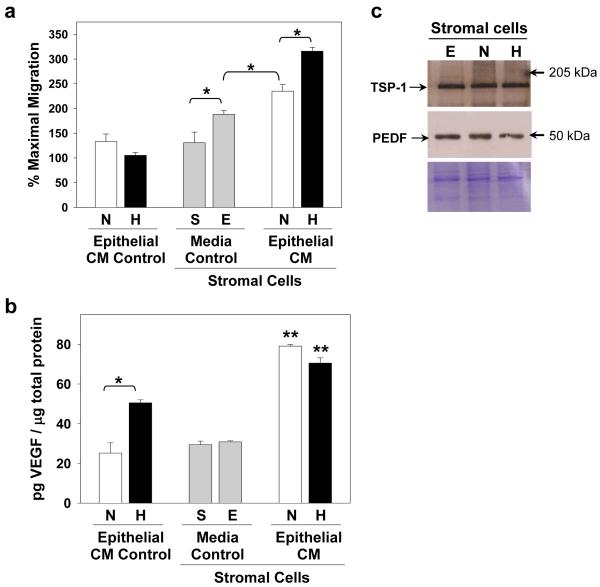
Epithelial secretions stimulate stromal angiogenic response
As the blood vessels reside within the prostate stroma, it is likely that epithelial cell secretions modify the stromal angiogenic response. To investigate this, we incubated PrSC in media conditioned by PrEC grown under normal or hypoxic conditions. Because PrSC are grown in a different culture media than PrEC, we tested the effects of the PrEC media alone on PrSC as a control, and we did observe an increase in angiogenic activity of PrSC (P<0.05; Figure 4a). However, incubation of PrSC in media conditioned by PrEC significantly increased activity by 25% over that of the epithelial media alone (P<0.03; Figure 4a). Moreover, incubation of PrSC in media conditioned by PrEC grown in hypoxic conditions further increased activity by an additional 35% (P<0.003; Figure 4a). Consistent with the results above, hypoxia increased VEGF levels in PrEC (Figure 4b). While incubation of PrSC in epithelial media alone did not alter VEGF levels, incubation in media conditioned by PrEC from both normoxic and hypoxic conditions significantly increased VEGF levels by two-fold compared to the media control (P<0.005; Figure 4b). However, VEGF levels were not different between PrSC treated with PrEC normoxia or hypoxia conditioned media (Figure 4b). The increase in angiogenic activity was independent of TSP-1 or PEDF since their expression levels were not changed (Figure 4c). These data illustrate that epithelial signals can stimulate stromal angiogenic activity primarily through changes in VEGF expression.
Figure 4.
Stromal-epithelial interaction regulates net angiogenic response. Normal stromal cells were treated with normal epithelial cell conditioned media collected under standard (normoxia, N) or hypoxic (H, 0.5% O2) conditions. As a control, stromal cells were grown in both epithelial media (E) and their standard stromal media (S). (a) Angiogenic activity was tested using a microvascular endothelial cell migration assay. Data are presented mean ± SE of the percent maximal migration toward the positive control. (b) VEGF levels were measured by ELISA, and data are presented as mean ± SD. (c) TSP-1 and PEDF expression were evaluated by Western blot. The lower panel is an identically loaded gel to show equal protein loading between lanes. Protein levels relative to cells grown in epithelial media (E) were determined by densitometry but showed no significant changes. Protein size standards are indicated. *Samples between bars are significantly different from each other, P<0.05. **Significantly increased over stromal cells grown in epithelial media, P<0.006.
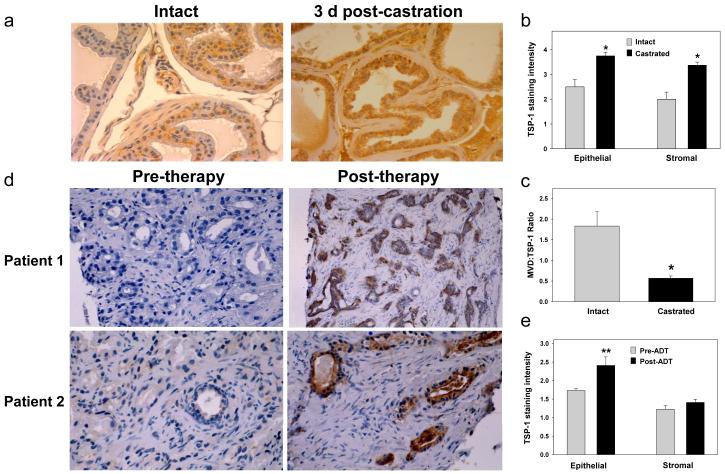
TSP-1 expression increases in response to androgen ablation in vivo
Because DHT and hypoxia modify PrEC and PrSC angiogenic activity and TSP-1 expression in vitro in opposing directions, we asked if androgens suppressed TSP-1 expression in vivo using a mouse castration model and human PCa tissues. We observed localization of TSP-1 in both the stromal and epithelial compartments of the ventral, lateral and dorsal lobes of the intact mouse prostate (Figure 5a). While epithelial expression was variable between glands, it was up-regulated in the dorsal prostate lobe by three days post-castration (Figure 5a). These observations are consistent with a study in rats showing an increase in TSP-1 expression in post-castration tissues.21 We graded the TSP-1 staining in the epithelium and stroma, demonstrating a significant increase in staining in both compartments post-castration (Figure 5b; n=5 per group; P<0.008). As expected, MVD was reduced in the castrated tissues (3.4 ± 0.43 vs. 1.92 ± 0.39; P<0.003). To determine if MVD correlated with TSP-1 staining, we calculated an MVD:TSP-1 staining ratio, and this ratio was significantly decreased in the castrated mice (Figure 5c; P<0.012). We have previously shown that in human PCa specimens there is a positive correlation between MVD:TSP-1 ratio and higher grade cancers,5 and other studies have shown that stromal MVD decreases following ADT in human cancer tissues.34,35 In addition, one study has reported that patients undergoing ADT have increased TSP-1 levels compared to patients who had not undergone ADT.4 However, a direct correlation between androgen-withdrawal and TSP-1 expression was not possible in this study. Therefore, we addressed this question by examining TSP-1 expression in patient-matched PCa biopsy specimens taken before and 3-7 days after androgen-ablation therapy. In pre-therapy specimens, TSP-1 was minimal to absent in both the stromal and epithelial cell compartments (Figure 5d). In two of eight cases, the post-therapy TSP-1 staining remained unchanged compared to the pre-therapy, with only focal epithelial staining present in these specimens. However, in the other six cases, there was a marked increase in TSP-1 staining in the epithelial cells with some focal stromal positivity noted post therapy (Figure 5d). When quantified, the TSP-1 staining was significantly increased in the epithelial compartment (P<0.013) while the stromal staining was not increased (Figure 5e). Taken together these observations suggest that TSP-1 functions in the vascular regression induced by androgen withdrawal. As we have similar results with PEDF expression (increase in seven of eight of patient tissues6), it seems that angiogenesis inhibitors play a critical role in mediating ADT-induced cancer regression.
Figure 5.
TSP-1 expression increases following androgen ablation in the mouse prostate and in patient-matched biopsy specimens in vivo. Prostate tissue sections were immunostained with anti-TSP antibody. (a) Prostate tissues were collected from intact or castrated (1-21 days post-castration; n=5 per group) wildtype (C57Bl/6) mice. Sections from intact and 3 days post-castration are shown. (b) TSP-1 staining intensity was graded on a 1-4 scale in the epithelium and stroma of the dorsal prostate. (c) The vessels were counted in the dorsal prostate stroma and the MVD:TSP-1 staining ratio calculated. (d) Patient-matched biopsies were taken from PCa patients before and 3-7 days after androgen ablation therapy. Six of eight patient tissues showed increased immunoreactivity following androgen ablation therapy. Pre- and post-therapy tissues are shown for two patients. (e) TSP-1 staining was graded on a 1-4 scale in the epithelial and stromal compartments. *Significantly increased in castrated compared to intact, P<0.012, and **significantly increased in human post-ADT tissues, P<00.013.
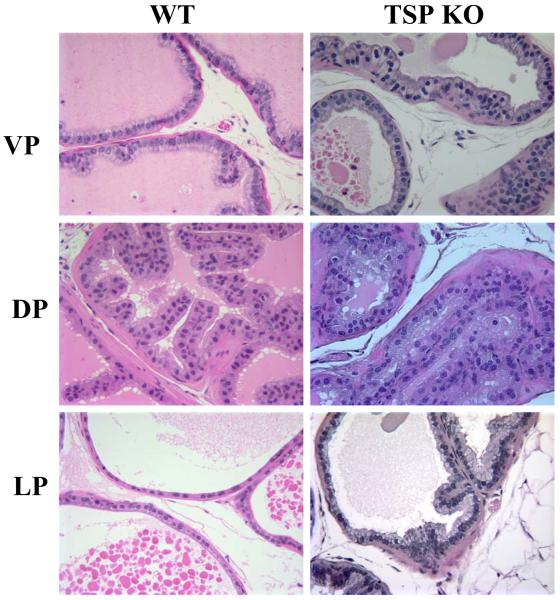
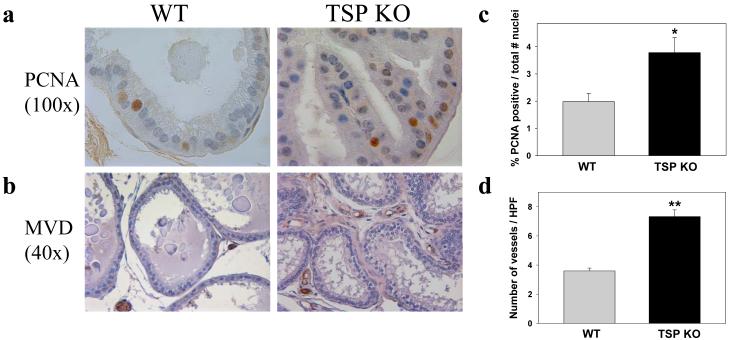
Loss of TSP-1 expression in the mouse results in prostate hyperplasia
We and others have previously reported that loss of TSP-1 disrupts the normal architecture of several tissues including the lungs, pancreas, liver and testes;23,32 however, the prostate phenotype has not been reported. The prostate in TSP-1 KO was compared to age-matched C57Bl/6 wildtype mice, the background strain of the TSP-1 KO with a minimum of 5 mice per group analyzed. In the TSP-1 KO, we observed dysregulated epithelial growth in the ventral, dorsal and lateral lobes of the prostate, as compared to controls (Figure 6). Hyperplasia was present in both the ventral and dorsal lobes and was evident by 3 months of age and progressive with age. The hyperplasia was characterized by increased tufting, stratification of cells in the epithelial cell layer with non-basally located, hyperchromatic and pleomorphic nuclei. In the lateral prostate, there was also a metaplasia phenotype evident by regions of cells with mucin accumulation, which does not normally occur in the lateral prostate. The epithelial hyperplasia was characterized by immunostaining prostate tissues with antibody against PCNA and factor VIII-related antigen for proliferation and MVD, respectively (Figure 7a,b; n=6 per group). TSP-1 KO mice showed a 2-fold increase in percent PCNA positive epithelial nuclei when compared to wildtype mice (P<0.007; Figure 7c), and stromal MVD was increased 2-fold in the TSP-1 KO prostate tissues as compared to wildtype controls (P<0.0003; Figure 7d). These data demonstrate that TSP-1 function is necessary for in vivo regulation of prostate growth, and the increase in stromal MVD supports angiogenic regulation as one mechanism of this growth regulation.
Figure 6.
The TSP-1 KO mouse has prostate hyperplasia. Compared to wildtype (WT), the TSP-1 KO (TSP KO) mouse prostate demonstrated epithelial and stromal cell hyperplasia by 3 months of age with nuclear atypia (hyperchromatic and pleomorphic nuclei) in the glandular cells. Evidence of hyperplasia was observed in the ventral prostate (VP), dorsal prostate (DP) and lateral prostate (LP). Representative H&E sections are shown at 5-6 months of age.
Figure 7.
Prostate tissue of TSP-1 KO has increased epithelial cell proliferation and MVD. Mouse prostate tissues were immunostained with anti-PCNA (a) and anti-factor VIII-related antigen (b) to assess proliferation and MVD, respectively. Representative tissue sections are shown. (c) The number of PCNA-positive and the total number of epithelial nuclei were counted at 100X to quantify proliferative activity. A minimum of 150 nuclei were counted for each mouse (n=6 per group). PCNA positivity is presented as a percent of the total number of nuclei counted; *P<0.007. (d) MVD quantified by counting vessels in 5 high power fields (HPF; 40X) for each mouse (n=6 per group; **P<0.00003).
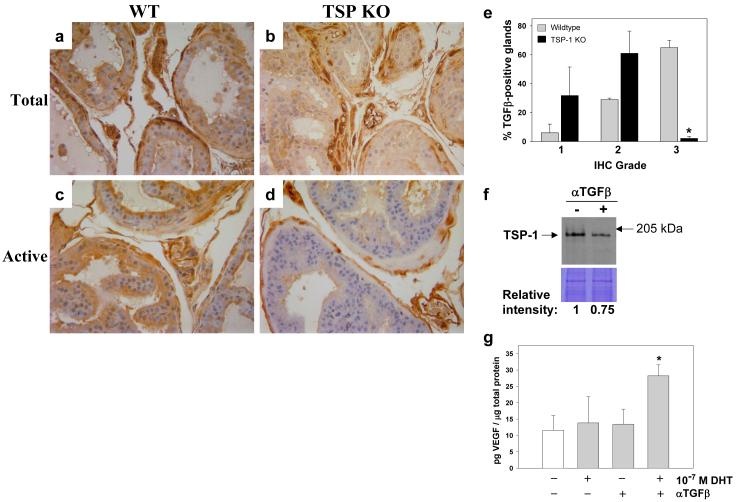
TSP-1 activates TGF-β in the mouse prostate
TSP-1 is a multi-functional protein, and in addition to its anti-angiogenic activity, TSP-1 can also activate latent TGF-β in vivo in other tissue types,23 but prostate activation has not been investigated. As TGF-β is a key regulator of prostate growth, we examined prostate tissues from wildtype and TSP-1 KO mice by immunostaining using antibodies against total and active TGF-β. With the antibody against total TGF-β, there was no difference in immunoreactivity between wildtype and TSP-1 KO tissues (Figure 8a,b; n=5 per group). With antibody against active TGF-β, staining was similar between wildtype and the TSP-1 KO in the lateral and ventral lobes of the prostate. However, in the TSP-1 KO dorsal prostate, there was significantly less active TGF-β compared to wildtype tissues (Figure 8c,d). When this staining was quantified by grading staining intensity within the glands on a 1-3 scale, there was significantly fewer high-staining glands (grade 3) in the TSP-1 KO prostate as compared to the wildtype tissues (P<0.001; Figure 8e). These data identify a novel function for TSP-1 in the prostate and suggest that TSP-1 activation of TGF-β is lobe specific. This difference may have significance as the dorsal lobe is considered to be the most analogous to the human prostate peripheral zone which is the zone where the majority of PCa arises.
Figure 8.
TSP-1 - TGF-β regulation in the prostate. Wildtype (C57Bl/6) and TSP-1 KO mouse prostate tissues (n=5 per group) were immunostained with antibody against total (a,b) and active TGF-β (c,d). (e) In the dorsal prostate, where staining differences were observed, active TGF-β-positive glands were graded on a 1-3 scale: 1 = light, 2 = medium and 3 = intense staining. The number of grade 3 glands was significantly decreased in the TSP-1 null mice as compared to wildtype (*P<0.0001). (f) Stromal cells were treated with neutralizing TGF-β antibody and TSP-1 levels assessed by Western blot analysis. The lower panel is an identically loaded Coomassie-stained gel to verify equal protein loading. Protein levels relative to the untreated cells was quantified by densitometry. (g) VEGF levels in normal stromal cells treated with DHT ± neutralizing TGF-β antibody VEGF were measured by ELISA. **Significantly decreased compared to untreated cells, P<0.05.
From studies in other tissue types, it also appears that active TGF-β can induce TSP-1 expression, showing a positive feedback regulation. To investigate this in prostate cells, we treated PrSC with neutralizing TGF-β antibodies. TSP-1 secretion in treated cells was suppressed 25% compared to untreated cells (Figure 8f). In addition, above we show that treatment with 10−7 M DHT did not induce VEGF expression (Figure 3b); however, when neutralizing TGF-β antibody was added, VEGF was significantly increased (Figure 8g). While TGF-β can act directly on endothelial cells, these data suggest that in the prostate it also contributes to angiogenic regulation through inducing TSP-1 expression and suppressing VEGF expression.
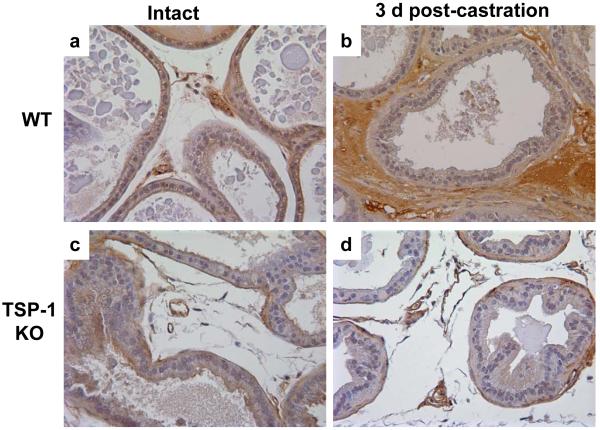
To determine if TSP-1 activates TGF-β in vivo following androgen withdrawal, we castrated wildtype and TSP-1 KO mice, collected prostate tissues at 1-21 days post-castration, and immunostained for total and active TGF-β. In the castrated tissues, with antibody against total TGF-β, no differences were observed between wildtype and TSP-1 KO mice. In the wildtype mice, there was a characteristic thickening of the stroma by 3 days post-castration compared to the intact animals, and active TGF-β strongly localized to this region (Figure 9a,b). While some of this staining is non-specific staining of the red blood cells leaking from the regressing vasculature, stromal positivity is also evident (Figure 9b). In contrast, TSP-1 KO mice did not demonstrate a thickening of the stroma and active TGF-β levels were unchanged in post-castration tissues (Figure 9c,d). These observations suggest that TSP-1 expression is necessary for the stromal response by increasing TGF-β activation in post-castration tissues.
Figure 9.
Stromal activation of TGF-β is decreased in the TSP-1 KO prostate post-castration. Wildtype (WT) and TSP-1 KO mice were castrated or sham-operated (intact), and prostate tissues were collected at 3-8 days post-castration and immunostained with antibody against active TGF-β. TSP-1 KO did not have the stromal thickening seen in WT mice and active TGF-β positivity was not increased in TSP-1 KO (n=3 per genotype per group per time point).
DISCUSSION
The importance of angiogenesis in tumor growth is well established, and a growing body of data supports its importance in regulating normal organ homeostasis as well. Prostate development and maintenance of the adult gland is dependent on androgens, and this appears to be mediated in part via regulation of angiogenesis. Androgen withdrawal induces regression of the glandular epithelium; however, endothelial apoptosis and vascular regression precedes the epithelial apoptosis.18-20 While the role of the angiogenesis inducer, VEGF, is well-studied in this process, the role of angiogenesis inhibitors has not been well established. Although the initial vascular regression can be explained by a sharp decrease in VEGF expression,14 the vascular regression leads to tissue hypoxia and VEGF returns to baseline levels.18-20 As the vascular regression continues, other angiogenic mediators must be involved. Here we show that TSP-1 expression increases following androgen withdrawal in normal mouse prostate tissues and in human PCa tissues. Thus, the anti-angiogenic activity of TSP-1 would contribute to the continued vascular regression. Similarly, we have observed up-regulation of PEDF in response to androgen withdrawal in normal mouse prostate and human PCa tissues.6 These observations suggest that angiogenesis inhibitors are critical to androgen-mediated regulation of the stromal vasculature. These data are of particular interest since ADT is a primary therapy for metastatic disease and is used in conjunction with other therapies in locally advanced PCa. Supporting this, ADT has been shown to decrease stromal MVD in human PCa tissues.34,35 The re-expression of TSP-1 shown above, and our previous study showing re-expression of PEDF,6 both most strongly in the epithelial cells, suggests a critical role for these angiogenesis inhibitors in mediating ADT-induced prostate cancer regression and that analysis of their expression following ADT could provide prognostic information.
As the prostate endothelial cells do not express the androgen receptor,15,16 it is likely that the epithelial and stromal cells mediate this response. To dissect this, we tested the androgen- and hypoxia-mediated angiogenic response in both cell types. Surprisingly, they revealed opposing responses in vitro. In epithelial cells, TSP-1 expression was suppressed by hypoxia, while in stromal cells hypoxia had no effect. With DHT treatment however, stromal TSP-1 was suppressed while epithelial cell TSP-1 was not affected. Though other molecules likely contribute, the net angiogenic activity in response to either stimulus could be explained when VEGF, TSP-1 and PEDF levels were considered. With these opposing responses, it seemed likely that the in vivo response may be modified by cell interactions. Toward this, we showed that stromal cell angiogenic activity is stimulated by epithelial cell secretions and that this modulation was sensitive to changes in epithelial growth in normoxia versus hypoxia. While these data demonstrate a complex regulation of angiogenic mediators by stromal-epithelial interactions, they also illustrate two caveats in angiogenic research. The first is that testing isolated epithelial cancer cells may not be representative of in vivo angiogenic activity, and the second is that measuring a single angiogenic mediator may not be an accurate indicator of angiogenic balance in the tissue.
Further supporting the critical role of angiogenesis and the inhibitor TSP-1 in regulating prostate growth, we also show that developmental loss of TSP-1 leads to prostate epithelial hyperplasia in mice, characterized by both increased epithelial cell proliferation and increased stromal angiogenesis. This phenotype was similar to the phenotype we observed in PEDF KO mice. Both molecules regulate prostate growth through vascular inhibition, and PEDF can also induce apoptosis of PCa cell.6 We have previously shown that TSP-1 and PEDF expression are decreased in PCa tissues compared to benign tissues.5,6 And, others have shown that circulating TSP-1 levels are decreased in PCa serum as compared to patients with benign prostatic hyperplasia and that these levels differentiated benign versus malignant disease.36 These observations suggest a broader function of angiogenic inhibitors as growth regulators in the prostate.
TSP-1 and TSP-1-derived peptides have also shown efficacy in directly inhibiting PCa cell proliferation in vitro37 and xenograft growth in vivo.38,39 However, one study has noted that, in a LNCaP xenograft model, the tumors eventually escaped the inhibitory effects of TSP-1,21 which could be linked to progression to hormone-independent cancer. In the current study, we show that TSP-1 activated latent TGF-β in the mouse prostate. TGF-β is a negative regulator of normal prostate epithelial cells. In human PCa, early stage cancers are sensitive to the growth inhibitory effects of TGF-β; however, advanced stage cancers are insensitive due to mutated or decreased expression of TGF-β receptors and altered intracellular signaling pathways. Thus, decreased sensitivity to the growth inhibitory effects of TGF-β, may be one mechanism by which tumors become insensitive to TSP-1 inhibition. Therefore, if TSP-1 expression is lost during tumorigenesis, multiple blockades to tumor growth are lost including inhibition of stromal angiogenesis and activation of latent TGF-β. Thus, for PCa patients, combining ADT with an anti-angiogenic therapy, such as a VEGF-neutralizing therapy or a TSP-1 therapy, and/or a therapy targeting the TGF-β pathway, could delay time to recurrence to androgen-independent disease.
Supplementary Material
Acknowledgements
This work was supported in parts by NIH Grant CA64329 (SEC) and DOD grant DAMD17-99-1-9521 (JAD), and P50-CA090386 (CL) and by a NorthShore University HealthSystem Research Career Development Award (JAD). The authors wish to thank Dr. Jack Lawler (Yale University, New Haven, CT) for providing the TSP-1 knockout mice and Dr. Beth Plunkett (NorthShore University HealthSystem, Evanston, IL) for her helpful discussions and critical analysis of this manuscript.
Sources of support: This work was supported in parts by NIH Grant CA095301 (SEC) and DOD grant DAMD17-99-1-9521 (JAD), and P50-CA090386 and by a NorthShore University HealthSystem Research Career Development Award (JAD)
List of abbreviations
- ADT
Androgen deprivation therapy
- BSA
bovine serum albumin
- DHT
Dihydrotestosterone
- ELISA
Enzyme-linked immunosorbent assay
- H&E
Hematoxylin and Eosin
- KO
Knockout
- MVD
Microvessel density
- PCa
Prostate Cancer
- PCNA
Proliferating cell nuclear antigen
- PEDF
Pigment epithelium-derived factor
- PrEC
Prostate epithelial cells
- PrSC
Prostate stromal cells
- SD
Standard deviation
- SE
Standard error
- TGF-β
Transforming growth factor-beta
- TSP-1
Thrombospondin-1
- VEGF
Vascular endothelial growth factor
Footnotes
Disclosure/Duality of Interest
The authors have no conflict of interest to disclose.
Supplementary information is available at Laboratory Investigation’s website.
References
- 1.Lissbrant IF, Stattin P, Damber JE, et al. Vascular density is a predictor of cancer-specific survival in prostatic carcinoma. Prostate. 1997;33:38–45. doi: 10.1002/(sici)1097-0045(19970915)33:1<38::aid-pros7>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 2.Silberman MA, Partin AW, Veltri RW, et al. Tumor angiogenesis correlates with progression after radical prostatectomy but not with pathologic stage in Gleason sum 5 to 7 adenocarcinoma of the prostate. Cancer. 1997;79:772–9. doi: 10.1002/(sici)1097-0142(19970215)79:4<772::aid-cncr14>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 3.Mehta R, Kyshtoobayeva A, Kurosaki T, et al. Independent association of angiogenesis index with outcome in prostate cancer. Clin Cancer Res. 2001;7:81–8. [PubMed] [Google Scholar]
- 4.Kwak C, Jin RJ, Lee C, et al. Thrombospondin-1, vascular endothelial growth factor expression and their relationship with p53 status in prostate cancer and benign prostatic hyperplasia. BJU Int. 2002;89:303–9. doi: 10.1046/j.1464-4096.2001.01417.x. [DOI] [PubMed] [Google Scholar]
- 5.Doll JA, Reiher FK, Crawford SE, et al. Thrombospondin-1, vascular endothelial growth factor and fibroblast growth factor-2 are key functional regulators of angiogenesis in the prostate. Prostate. 2001;49:293–305. doi: 10.1002/pros.10025. [DOI] [PubMed] [Google Scholar]
- 6.Doll JA, Stellmach VM, Bouck NP, et al. Pigment epithelium-derived factor regulates the vasculature and mass of the prostate and pancreas. Nat Med. 2003;9:774–80. doi: 10.1038/nm870. [DOI] [PubMed] [Google Scholar]
- 7.Franck-Lissbrant I, Haggstrom S, Damber JE, et al. Testosterone stimulates angiogenesis and vascular regrowth in the ventral prostate in castrated adult rats. Endocrinology. 1998;139:451–6. doi: 10.1210/endo.139.2.5683. [DOI] [PubMed] [Google Scholar]
- 8.Lekas E, Johansson M, Widmark A, et al. Decrement of blood flow precedes the involution of the ventral prostate in the rat after castration. Urol Res. 1997;25:309–14. doi: 10.1007/BF01294656. [DOI] [PubMed] [Google Scholar]
- 9.Lekas E, Engstrand C, Bergh A, et al. Transient ischemia induces apoptosis in the ventral prostate of the rat. Urol Res. 1999;27:174–9. doi: 10.1007/s002400050106. [DOI] [PubMed] [Google Scholar]
- 10.Shabsigh A, Chang DT, Heitjan DF, et al. Rapid reduction in blood flow to the rat ventral prostate gland after castration: preliminary evidence that androgens influence prostate size by regulating blood flow to the prostate gland and prostatic endothelial cell survival. Prostate. 1998;36:201–6. doi: 10.1002/(sici)1097-0045(19980801)36:3<201::aid-pros9>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 11.Jain RK, Safabakhsh N, Sckell A, et al. Endothelial cell death, angiogenesis, and microvascular function after castration in an androgen-dependent tumor: role of vascular endothelial growth factor. Proc Natl Acad Sci U S A. 1998;95:10820–5. doi: 10.1073/pnas.95.18.10820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Joseph IB, Nelson JB, Denmeade SR, et al. Androgens regulate vascular endothelial growth factor content in normal and malignant prostatic tissue. Clin Cancer Res. 1997;3:2507–11. [PubMed] [Google Scholar]
- 13.Sordello S, Bertrand N, Plouet J. Vascular endothelial growth factor is up-regulated in vitro and in vivo by androgens. Biochem Biophys Res Commun. 1998;251:287–90. doi: 10.1006/bbrc.1998.9328. [DOI] [PubMed] [Google Scholar]
- 14.Shibata Y, Kashiwagi B, Arai S, et al. Direct regulation of prostate blood flow by vascular endothelial growth factor and its participation in the androgenic regulation of prostate blood flow in vivo. Endocrinology. 2004;145:4507–12. doi: 10.1210/en.2004-0288. [DOI] [PubMed] [Google Scholar]
- 15.Prins GS, Birch L. Immunocytochemical analysis of androgen receptor along the ducts of the separate rat prostate lobes after androgen withdrawal and replacement. Endocrinology. 1993;132:169–78. doi: 10.1210/endo.132.1.8419121. [DOI] [PubMed] [Google Scholar]
- 16.Prins GS, Birch L, Greene GL. Androgen receptor localization in different cell types of the adult rat prostate. Endocrinology. 1991;129:3187–99. doi: 10.1210/endo-129-6-3187. [DOI] [PubMed] [Google Scholar]
- 17.Levine AC, Liu XH, Greenberg PD, et al. Androgens induce the expression of vascular endothelial growth factor in human fetal prostatic fibroblasts. Endocrinology. 1998;139:4672–8. doi: 10.1210/endo.139.11.6303. [DOI] [PubMed] [Google Scholar]
- 18.Shabsigh A, Ghafar MA, de la Taille A, et al. Biomarker analysis demonstrates a hypoxic environment in the castrated rat ventral prostate gland. J Cell Biochem. 2001;81:437–44. [PubMed] [Google Scholar]
- 19.Rudolfsson SH, Bergh A. Testosterone-stimulated growth of the rat prostate may be driven by tissue hypoxia and hypoxia-inducible factor-1alpha. J Endocrinol. 2008;196:11–9. doi: 10.1677/JOE-07-0272. [DOI] [PubMed] [Google Scholar]
- 20.Rudolfsson SH, Bergh A. Hypoxia drives prostate tumour progression and impairs the effectiveness of therapy, but can also promote cell death and serve as a therapeutic target. Expert Opin Ther Targets. 2009;13:219–25. doi: 10.1517/14728220802626249. [DOI] [PubMed] [Google Scholar]
- 21.Colombel M, Filleur S, Fournier P, et al. Androgens repress the expression of the angiogenesis inhibitor thrombospondin-1 in normal and neoplastic prostate. Cancer Res. 2005;65:300–8. [PubMed] [Google Scholar]
- 22.Kazerounian S, Yee KO, Lawler J. Thrombospondins in cancer. Cell Mol Life Sci. 2008;65:700–12. doi: 10.1007/s00018-007-7486-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Crawford SE, Stellmach V, Murphy-Ullrich JE, et al. Thrombospondin-1 is a major activator of TGF-beta1 in vivo. Cell. 1998;93:1159–70. doi: 10.1016/s0092-8674(00)81460-9. [DOI] [PubMed] [Google Scholar]
- 24.Schultz-Cherry S, Lawler J, Murphy-Ullrich JE. The type 1 repeats of thrombospondin 1 activate latent transforming growth factor-beta. J Biol Chem. 1994;269:26783–8. [PubMed] [Google Scholar]
- 25.Yehualaeshet T, O’Connor R, Green-Johnson J, et al. Activation of rat alveolar macrophage-derived latent transforming growth factor beta-1 by plasmin requires interaction with thrombospondin-1 and its cell surface receptor, CD36. Am J Pathol. 1999;155:841–51. doi: 10.1016/s0002-9440(10)65183-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jones E, Pu H, Kyprianou N. Targeting TGF-beta in prostate cancer: therapeutic possibilities during tumor progression. Expert Opin Ther Targets. 2009;13:227–34. doi: 10.1517/14728220802705696. [DOI] [PubMed] [Google Scholar]
- 27.Wikstrom P, Westin P, Stattin P, et al. Early castration-induced upregulation of transforming growth factor beta1 and its receptors is associated with tumor cell apoptosis and a major decline in serum prostate-specific antigen in prostate cancer patients. Prostate. 1999;38:268–77. doi: 10.1002/(sici)1097-0045(19990301)38:4<268::aid-pros2>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 28.Danielpour D. Induction of transforming growth factor-beta autocrine activity by all-trans-retinoic acid and 1 alpha,25-dihydroxyvitamin D3 in NRP-152 rat prostatic epithelial cells. J Cell Physiol. 1996;166:231–9. doi: 10.1002/(SICI)1097-4652(199601)166:1<231::AID-JCP24>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 29.Goldberg MA, Dunning SP, Bunn HF. Regulation of the erythropoietin gene: evidence that the oxygen sensor is a heme protein. Science. 1988;242:1412–5. doi: 10.1126/science.2849206. [DOI] [PubMed] [Google Scholar]
- 30.Good DJ, Polverini PJ, Rastinejad F, et al. A tumor suppressor-dependent inhibitor of angiogenesis is immunologically and functionally indistinguishable from a fragment of thrombospondin. Proc Natl Acad Sci U S A. 1990;87:6624–8. doi: 10.1073/pnas.87.17.6624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tolsma SS, Volpert OV, Good DJ, et al. Peptides derived from two separate domains of the matrix protein thrombospondin-1 have anti-angiogenic activity. J Cell Biol. 1993;122:497–511. doi: 10.1083/jcb.122.2.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lawler J, Sunday M, Thibert V, et al. Thrombospondin-1 is required for normal murine pulmonary homeostasis and its absence causes pneumonia. J Clin Invest. 1998;101:982–92. doi: 10.1172/JCI1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Berger AP, Kofler K, Bektic J, et al. Increased growth factor production in a human prostatic stromal cell culture model caused by hypoxia. Prostate. 2003;57:57–65. doi: 10.1002/pros.10279. [DOI] [PubMed] [Google Scholar]
- 34.Matsushima H, Goto T, Hosaka Y, et al. Correlation between proliferation, apoptosis, and angiogenesis in prostate carcinoma and their relation to androgen ablation. Cancer. 1999;85:1822–7. doi: 10.1002/(sici)1097-0142(19990415)85:8<1822::aid-cncr24>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 35.Montironi R, Diamanti L, Thompson D, et al. Analysis of the capillary architecture in the precursors of prostate cancer: recent findings and new concepts. Eur Urol. 1996;30:191–200. doi: 10.1159/000474169. [DOI] [PubMed] [Google Scholar]
- 36.Shafer MW, Mangold L, Partin AW, et al. Antibody array profiling reveals serum TSP-1 as a marker to distinguish benign from malignant prostatic disease. Prostate. 2007;67:255–67. doi: 10.1002/pros.20514. [DOI] [PubMed] [Google Scholar]
- 37.Bastian M, Steiner M, Schuff-Werner P. Expression of thrombospondin-1 in prostate-derived cell lines. Int J Mol Med. 2005;15:49–56. [PubMed] [Google Scholar]
- 38.Jin RJ, Kwak C, Lee SG, et al. The application of an anti-angiogenic gene (thrombospondin-1) in the treatment of human prostate cancer xenografts. Cancer Gene Ther. 2000;7:1537–42. doi: 10.1038/sj.cgt.7700266. [DOI] [PubMed] [Google Scholar]
- 39.Quesada AJ, Nelius T, Yap R, et al. In vivo upregulation of CD95 and CD95L causes synergistic inhibition of angiogenesis by TSP1 peptide and metronomic doxorubicin treatment. Cell Death Differ. 2005;12:649–58. doi: 10.1038/sj.cdd.4401615. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.