Abstract
Transcutaneous electrical nerve stimulation (TENS) refers to the delivery of electrical currents through the skin to activate peripheral nerves. The technique is widely used in developed countries to relieve a wide range of acute and chronic pain conditions, including pain resulting from cancer and its treatment. There are many systematic reviews on TENS although evidence is often inconclusive because of shortcomings in randomised control trials methodology. In this overview the basic science behind TENS will be discussed, the evidence of its effectiveness in specific clinical conditions analysed and a case for its use in pain management in developing countries will be made.
Keywords: Transcutaneous Electrical Nerve Stimulation (TENS), Pain, Analgesia, Pain relief, Pain management, Developing countries, Pain gate theory
Introduction
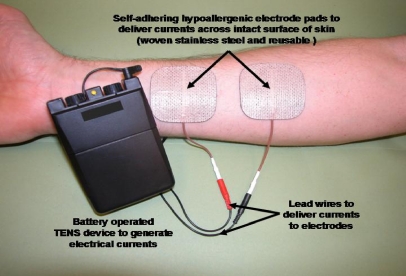
Transcutaneous electrical nerve stimulation (TENS) is widely used in western and developed countries to relieve a wide range of painful conditions, including non-malignant acute and chronic pain and pain resulting from cancer and its treatment [1–3]. TENS is inexpensive, non-invasive and safe with no major side effects. TENS can be self administered by patients following simple training and because there is no potential for toxicity, patients can titrate the dosage on an as-needed basis. During TENS pulsed electrical currents are generated by a small battery operated TENS device that can be kept in the pocket or attached to the user's belt. Currents from the TENS device are delivered through the skin by two self-adhering electrode pads (Figure 1).
Figure 1.
A standard TENS device.
The purpose of TENS is to selectively activate nerve fibers. Maximal pain relief is achieved when TENS generates a strong non-painful electrical sensation beneath the electrodes. Pain relief is usually rapid in onset and stops shortly after TENS is turned off. For this reason patients are encouraged to deliver TENS for as long as needed, which may be for hours at a time and throughout the day. The main contraindication is patients with implanted stimulators such as pacemakers. In the UK, TENS devices can be purchased without prescription, although this is not the case in some European countries. TENS devices, including electrode leads, pads and battery, retail for approximately £30GBP although bulk buying can markedly reduce cost. Interestingly, TENS does not appear to be widely available for patient use in developing countries.
In this review the basic science behind TENS will be discussed, the evidence of its effectiveness in specific clinical conditions will be provided and a case for its use in pain management in developing countries will be made.
Physiological principle of TENS induced pain relief
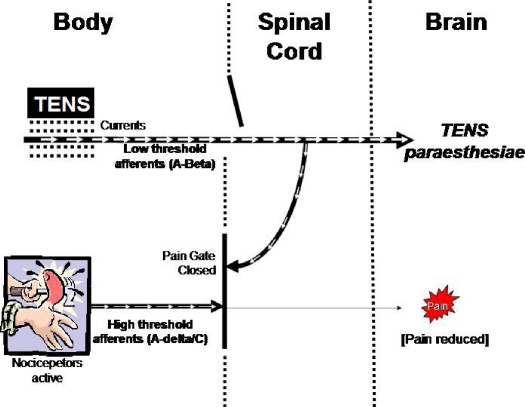
The ancient Egyptians are usually acknowledged as the first people who used electrogenic fish to apply electricity for pain relief. Yet, the first documented use of this kind of pain relief is of a Roman Physician in 46 AD [4]. In 1786, Luigi Galvani, an Italian doctor, demonstrated that the leg of a frog contained electricity. This observation and other advancements in generating electricity lead to a resurgence in the use of electricity to treat different illnesses and relieve pain. However, increased use of pharmacological agents to manage pain resulted in the decline of the electrotherapy at the end of the 19th century. In 1965, Ronald Melzack from McGill University in Montreal Canada and Patrick Wall from University College London UK, published their seminal paper which proposed a gating mechanism in the central nervous system to regulate the flow of nerve signals from peripheral nerves en-route to the brain [5]. According to this Gate-Control Theory of Pain, activity in large diameter low threshold mechanoreceptive (touch-related) nerve fibers could inhibit the transmission of action potentials from small diameter higher threshold nociceptive (pain-related) fibers through pre and post synaptic inhibition in the dorsal horn of spinal cord. Humans utilise this mechanism whenever they rub their skin to relieve pain. Because nociceptive fibers (A-delta and C-fibers) have a higher threshold of activation than mechanoreceptive fibers (A-beta fibers) Melzack and Wall proposed that it would be possible to selectively stimulate mechanoreceptive fibers by titrating the amplitude of electrical currents delivered across the surface of the skin (ie TENS). This would prevent signals from nociceptive fibers from reaching higher centres of the brain, thus reducing pain (Figure 2). In essence, TENS electrically rubs pain away.
Figure 2.
Diagrammatic representation of the principle of conventional TENS. By selectively activating A-beta fibers, TENS shuts the Pain Gate on A-delta and C fibers preventing pain-related signals reaching the brain.
In addition to interrupting nociceptive signals, at spinal cord dorsal horn, we now know that TENS analgesia also involves a descending inhibitory mechanism that could be partially prevented by spinalization [6]. Activity in nerve fibers descending from the brain can also block onward transmission of peripheral nerve signals within the spinal cord. Humans utilise this mechanism whenever they mentally distract themselves to not feel pain despite the presence of tissue damage (Figure 2)
Evidence gathered from animal studies suggested that low frequency TENS effects may be due to release of endogenous opioids [6]. This explains why analgesia may persist for hours after electrical stimulation has stopped because endorphins have long lasting effects in the central nervous system. The released opioids may generate their analgesic action at peripheral, spinal and supraspinal sites [7, 8]. However, other neurochemicals have been implicated in TENS analgesia including GABA [9], acetylcholine [10], 5-HT [11], noradrenaline [12] and adenosine [13].
TENS and TENS-like devices
In health care the term TENS refers to the delivery of currents using a ‘standard TENS device’ (Table 1) [3]. However, there are a variety of devices that deliver electrical currents through the skin but have technical output characteristics that differ from a standard TENS device. We have previously described these as “TENS-like devices” and include Trancutaneous Spinal Electroanalgesia, Interferential Therapy, Microcurrent Stimulation and Pain Gone pens (see [3, 14, 15] for a review of these devices). The remainder of this review will focus on standard TENS devices.
Table 1.
Technical output specifications of a standard TENS device
| Weight | 50–250g |
| Dimensions | 6 × 5 × 2 cm (small device) |
| 12 × 9 × 4 cm (large device) | |
| Cost | Approximately £30 |
| Pulse waveform (usually fixed) | Monophasic symmetrical biphasic asymmetrical biphasic |
| Pulse amplitude (usually adjustable) | 1–50mA into a 1 kΩ load |
| Pulse duration (sometimes fixed, sometimes adjustable) | 10–1000µs |
| Pulse frequency (usually adjustable) | 1–250pps |
| Pulse pattern | usually continuous and burst available (some devices have modulated amplitude, modulated frequency, modulated pulse duration, random frequency) |
| Channels | 1 or 2 |
| Batteries | PP3 (9V), rechargeable |
| Additional features | Timer, most devices deliver constant current output |
TENS Techniques
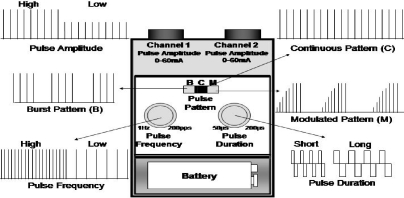
TENS is a technique to stimulate different categories of nerve fibers. The most commonly used TENS technique is termed conventional TENS. During conventional TENS, low-intensity pulsed currents are administered at high-frequencies (between 10–200 pulses per second, pps) at the site of pain. The user experiences a “strong, non-painful TENS sensation often described as ‘tingling’ or pleasant ‘electrical paraesthesiae’. Physiologically, conventional TENS activates large diameter non-noxious afferents which has been shown to close the pain gate at spinal segments related to the pain [6]. Another technique, which is used less often is acupuncture-like TENS (AL-TENS) using high-intensity and low-frequency (less than 10pps, usually 2pps) administered over muscles, acupuncture and trigger points [16]. The purpose of AL-TENS is to activate small diameter afferents which has been shown to close the pain gate using extra-segmental mechanisms [2]. TENS can also be used as a counter-irritant, termed intense TENS, using high-intensity and high-frequency currents (Table 2, Figure 3).
Table 2.
TENS techniques
| TENS parameters | Patient experience | Electrode location | Physiological Intention | Regimen | Analgesic profile | |
|---|---|---|---|---|---|---|
| Conventional TENS | Low intensity (amplitude), high frequency (10–200 pps) | Strong, non-painful TENS paraesthesia with minimal muscle activity | Dermatomes Site of pain | To stimulate large diameter non-noxious afferents (A-beta) to produce segmental analgesia | Use TENS whenever in pain | Usually rapid onset and offset |
| AL-TENS | High intensity (amplitude), low frequency (1–5 bursts of 100 pps) | Strong comfortable muscle twitching | Muscles Motor nerves Acupuncture points | To stimulate small diameter cutaneous and motor afferents (A-delta) to produce extrasegmental analgesia | Use TENS for 20–30 minutes at a time | May be delayed onset and offset |
| Intense TENS | High amplitude (uncomfortable/noxious), high frequency (50–200pps) | Uncomfortable (painful) electrical paraesthesia | Dermatomes Site of pain Nerves proximal to pain | To stimulate small diameter cutaneous afferents (A-delta) to produce counter irritation | Short periods only 5–15 minutes at a time | Rapid onset and delayed offset |
Figure 3.
Output characteristics (settings) of a standard TENS device. The user can control the amplitude (intensity), duration (width), frequency (rate) and pattern (mode) of the pulsed electrical currents.
Clinical effectiveness of TENS
In Western clinical practice TENS has been shown to have a role in pain management [2]. There are many systematic reviews on TENS although evidence is often inconclusive because of shortcomings in RCT methodology. Early systematic reviews suggested that TENS was of limited benefit as a stand alone pain therapy for acute pain. Carroll et al. judged there to be no benefit of TENS for postoperative pain because 15 of 17 RCTs found no differences in pain relief between active and placebo TENS [17]. However, Bjordal et al. re-assessed the evidence and concluded that TENS reduced post-operative analgesic consumption if TENS was applied using adequate TENS technique [18]. Systematic reviews have also concluded that there was no evidence for TENS producing beneficial analgesic effects during childbirth [19, 20] and insufficient evidence to determine the effectiveness of TENS in reducing pain associated with primary dysmenorrhoea [21]. RCTs suggest that TENS is effective for acute orofacial pain, painful dental procedures, fractured ribs and acute lower back pain (for review see [22].
Previously, systematic reviews suggested that TENS may be of benefit for chronic pain but definitive conclusions were hindered by shortcomings in RCT methodology [23, 24]. Reviews on rheumatoid arthritis of the hand [25], whiplash and mechanical neck disorders [26], chronic low back pain [27], poststroke shoulder pain [28] and chronic recurrent headache [29] were inconclusive. In contrast, systematic reviews have demonstrated TENS efficacy for knee osteoarthritis [30] and chronic musculoskeletal pain [31]. RCTs have also demonstrated effects for a range of other chronic pain conditions including localized muscle pain, post-herpetic neuralgia, trigeminal neuralgia, phantom limb and stump pain and diabetic neuropathies (for review see [3]. A recent Cochrane review by Robb et al. concluded that there is insufficient available evidence to determine the effectiveness of TENS in treating cancer-related pain [32, 33].
Pain Management in developing countries: Could TENS help?
The International Association for The Study of Pain (IASP) speculate that “the prevalence of most types of pain may be much higher in developing countries than in developed countries”, although epidemiological evidence is lacking [34]. It is known that there is a higher incidence of pain conditions associated with epidemics such as HIV/aids in the developing world. An IASP Developing Countries Task Force, which included Africa and the Middle East reported that pain management in the general population was inadequate, although there was considerable variations between regions [35]. Limited resources, ignorance by health care professionals and a lack of pain specialists were contributing factors. This has impacted significantly on pharmacological therapy with many drugs commonly used in the developed world being unavailable to the general public because of the weak economy and limited purchasing power of citizens [36]. In addition, drugs even when available may be fake, adulterated, passed their expiry date or perished due to inadequate storage.
TENS is advantageous in this regard. It is inexpensive when compared to drug therapy. The cost of a TENS device is £30GBP, although devices are available for less than £15GBP if bought in bulk. Once purchased a TENS device will not perish or deteriorate and devices in the developed world are used for many decades without the need for further servicing or repair. Often clinics purchase TENS devices in bulk and loan them to patients for short and long term use, on the proviso that the patient returns the device to the clinic when it is no longer needed. Running costs are minimal and include battery and reusable electrode pad replacement. Manufacturers recommend that individual pads have longevity of one month on daily use, although patients often use them for far greater lengths of time, especially if they take care to store them carefully. Electrode costs can be reduced by using carbon rubber electrodes which are smeared with electrode gel and attached to the skin with micropore tape, rather than using self adhering electrodes. In general, battery and electrode use depends on how often the patient uses TENS.
TENS has no known drug interactions and so can be used in combination with pharmacotherapy to reduce medication, medication-related side effects and medication costs. TENS has very few side effects with no incidents of serious or adverse events reported in the literature. TENS has a rapid onset of action, unlike medication, and there is no potential for toxicity or overdose.
Clearly, there is a case to use TENS for pain management in the developing world. However, research is needed to determine the feasibility of TENS use in developing countries. Perhaps health promotion authorities should alert the public and heath care practitioners to the role of TENS as an important aid in the fight against pain.
References
- 1.Barlas P., Lundeberg T. Transcutaneous electrical nerve stimulation and acupuncture, in Melzack and Wall's Textbook of Pain. In: McMahon S., Koltzenburg M., editors. Philadelphia: Elsevier Churchill Livingstone; 2006. pp. 583–90. [Google Scholar]
- 2.Walsh D. 1st ed. New York: Churchill Livingstone; 1997. TENS.Clinical applications and related theory. [Google Scholar]
- 3.Johnson M. Transcutaneous Electrical Nerve Stimulation, in Electrotherapy: Evidence based practice. In: Watson T., editor. Edinburgh: Churchill Livingstone; 2008. pp. 253–96. [Google Scholar]
- 4.Gildenberg P.L. History of electrical neuromodulation for chronic pain. Pain Med. 2006;7(1):S7–S13. [Google Scholar]
- 5.Melzack R., Wall P. Pain mechanisms: A new theory. Science. 1965;150:971–79. doi: 10.1126/science.150.3699.971. [DOI] [PubMed] [Google Scholar]
- 6.Sluka K.A., Walsh D. Transcutaneous electrical nerve stimulation: basic science mechanisms and clinical effectiveness. J Pain. 2003;4(3):109–21. doi: 10.1054/jpai.2003.434. [DOI] [PubMed] [Google Scholar]
- 7.Sluka K.A., et al. Spinal blockade of opioid receptors prevents the analgesia produced by TENS in arthritic rats. J Pharmacol Exp Ther. 1999;289(2):840–46. [PubMed] [Google Scholar]
- 8.Kalra A., Urban M.O., Sluka K.A. Blockade of opioid receptors in rostral ventral medulla prevents antihyperalgesia produced by transcutaneous electrical nerve stimulation (TENS) J Pharmacol Exp Ther. 2001;298(1):257–63. [PubMed] [Google Scholar]
- 9.Maeda Y., et al. Release of GABA and activation of GABA(A) in the spinal cord mediates the effects of TENS in rats. Brain Res. 2007;1136(1):43–50. doi: 10.1016/j.brainres.2006.11.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Radhakrishnan R., Sluka K.A. Spinal muscarinic receptors are activated during low or high frequency TENS-induced antihyperalgesia in rats. Neuropharmacology. 2003;45(8):1111–19. doi: 10.1016/s0028-3908(03)00280-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Radhakrishnan R., et al. Spinal 5-HT(2) and 5-HT(3) receptors mediate low, but not high, frequency TENS-induced antihyperalgesia in rats. Pain. 2003;105(1–2):205–13. doi: 10.1016/s0304-3959(03)00207-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.King E.W., et al. Transcutaneous electrical nerve stimulation activates peripherally located alpha-2A adrenergic receptors. Pain. 2005;115(3):364–73. doi: 10.1016/j.pain.2005.03.027. [DOI] [PubMed] [Google Scholar]
- 13.Sawynok J. Adenosine receptor activation and nociception. Eur J Pharmacol. 1998;347(1):1–11. doi: 10.1016/s0014-2999(97)01605-1. [DOI] [PubMed] [Google Scholar]
- 14.Johnson M. Transcutaneous Electrical Nerve Stimulation (TENS) and TENS-like devices. Do they provide pain relief? Pain Reviews. 2001;8:121–28. [Google Scholar]
- 15.Johnson M.I. A critical review of the analgesic effects of TENS-like devices. Physical Therapy Reviews. 2001;6:153–73. [Google Scholar]
- 16.Johnson M. The analgesic effects and clinical use of Acupuncture-like TENS (AL-TENS) Physical therapy Reviews. 1998;3:73–93. [Google Scholar]
- 17.Carroll D., et al. Randomization is important in studies with pain outcomes: systematic review of transcutaneous electrical nerve stimulation in acute postoperative pain. Br J Anaesth. 1996;77(6):798–803. doi: 10.1093/bja/77.6.798. [DOI] [PubMed] [Google Scholar]
- 18.Bjordal J.M., Johnson M.I., Ljunggreen A.E. Transcutaneous electrical nerve stimulation (TENS) can reduce postoperative analgesic consumption. A meta-analysis with assessment of optimal treatment parameters for postoperative pain. Eur J Pain. 2003;7(2):181–88. doi: 10.1016/S1090-3801(02)00098-8. [DOI] [PubMed] [Google Scholar]
- 19.Carroll D., et al. Transcutaneous electrical nerve stimulation does not relieve in labour pain: updated systematic review. Contemporary Reviews in Obstetrics and Gynecology, 1997. 1997 Sep;:195–205. [Google Scholar]
- 20.Carroll D., et al. Transcutaneous electrical nerve stimulation in labour pain: a systematic review. Br J Obstet Gynaecol. 1997;104(2):169–75. doi: 10.1111/j.1471-0528.1997.tb11039.x. [DOI] [PubMed] [Google Scholar]
- 21.Proctor M.L., et al. Transcutaneous electrical nerve stimulation and acupuncture for primary dysmenorrhoea. Cochrane Database Syst Rev. 2002;(1):CD002123. doi: 10.1002/14651858.CD002123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnson M., Oxberry S., Simpson K. Transcutaneous Electrical Nerve Stimulation (TENS) and acupuncture for acute pain, in Acute Pain. In: Macintyre P., Walker S., Rowbotham D., editors. Clinical Pain Management. Second Edition. London: Hodder Arnold; 2008. pp. 271–90. [Google Scholar]
- 23.Carroll D., et al. Transcutaneous electrical nerve stimulation (TENS) for chronic pain. Cochrane Database of Systematic Reviews (Online: Update Software) 2003;(3):CD003222. doi: 10.1002/14651858.CD003222. [DOI] [PubMed] [Google Scholar]
- 24.Nnoaham K.E., Kumbang J. Transcutaneous electrical nerve stimulation (TENS) for chronic pain. Cochrane Database Syst Rev. 2008;(3):CD003222. doi: 10.1002/14651858.CD003222.pub2. [DOI] [PubMed] [Google Scholar]
- 25.Brosseau L., et al. Transcutaneous electrical nerve stimulation (TENS) for the treatment of rheumatoid arthritis in the hand. Cochrane Database Syst Rev. 2003;(3):CD004287. doi: 10.1002/14651858.CD004377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kroeling P., Gross A.R., Goldsmith C.H. A Cochrane review of electrotherapy for mechanical neck disorders. Spine. 2005;30(21):E641–8. doi: 10.1097/01.brs.0000184302.34509.48. [DOI] [PubMed] [Google Scholar]
- 27.Khadilkar A., et al. Transcutaneous electrical nerve stimulation (TENS) versus placebo for chronic low-back pain. Cochrane Database Syst Rev. 2008;(4):CD003008. doi: 10.1002/14651858.CD003008.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Price C.I., Pandyan A.D. Electrical stimulation for preventing and treating post-stroke shoulder pain: a systematic Cochrane review. Clin Rehabil. 2001;15(1):5–19. doi: 10.1191/026921501670667822. [DOI] [PubMed] [Google Scholar]
- 29.Bronfort G., et al. Non-invasive physical treatments for chronic/recurrent headache. Cochrane Database Syst Rev. 2004;(3):CD001878. doi: 10.1002/14651858.CD001878.pub2. [DOI] [PubMed] [Google Scholar]
- 30.Bjordal J.M., et al. Short-term efficacy of physical interventions in osteoarthritic knee pain. A systematic review and meta-analysis of randomised placebo-controlled trials. BMC Musculoskelet Disord. 2007;8:51. doi: 10.1186/1471-2474-8-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Johnson M., Martinson M. Efficacy of electrical nerve stimulation for chronic musculoskeletal pain: a meta-analysis of randomized controlled trials. Pain. 2007;130(1–2):157–65. doi: 10.1016/j.pain.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 32.Robb K., et al. A Cochrane Systematic Review of Transcutaneous Electrical Nerve Stimulation for Cancer Pain. J Pain Symptom Manage. 2008 doi: 10.1016/j.jpainsymman.2008.03.022. [DOI] [PubMed] [Google Scholar]
- 33.Robb K.A., et al. Transcutaneous electric nerve stimulation (TENS) for cancer pain in adults. Cochrane Database Syst Rev. 2008;(3):CD006276. doi: 10.1002/14651858.CD006276.pub2. [DOI] [PubMed] [Google Scholar]
- 34.Woodruff R. Pain and palliative care in the developing world and marginalized populations: A global challenge. Indian J Palliat Care. 2004;10:80. [Google Scholar]
- 35.Bond M., et al. Education and Training for Pain management in Developing Countries. 2007. WWW.IASP-PAIN.ORG acessed on 3/10/2008.
- 36.Omoti A.E., Omoti C.E. Pharmacological strategies for the management of cancer pain in developing countries. Pharmacy Practice. 2007;5(3):99–104. doi: 10.4321/s1886-36552007000300001. [DOI] [PMC free article] [PubMed] [Google Scholar]