Abstract
Since the first description of the concept of natural orifice translumenal endoscopic surgery (NOTES), a substantial number of clinical NOTES reports have appeared in the literature. This editorial reviews the available human data addressing research questions originally proposed by the white paper, including determining the optimal method of access for NOTES, developing safe methods of lumenal closure, suturing and anastomotic devices, advanced multitasking platforms, addressing the risk of infection, managing complications, addressing challenges with visualization, and training for NOTES procedures. An analysis of the literature reveals that so far transvaginal access and closure appear to be the most feasible techniques for NOTES, with a limited, but growing transgastric, transrectal, and transesophageal NOTES experience in humans. The theoretically increased risk of infection as a result of NOTES procedures has not been substantiated in transvaginal and transgastric procedures so far. Development of suturing and anastomotic devices and advanced platforms for NOTES has progressed slowly, with limited clinical data on their use so far. Data on the optimal management and incidence of intraoperative complications remain sparse, although possible factors contributing to complications are discussed. Finally, this editorial discusses the likely direction of future NOTES development and its possible role in clinical practice.
Keywords: Natural orifice translumenal endoscopic surgery, Outcomes, Complications, Endoscopic, Surgery
INTRODUCTION
The concept of natural orifice translumenal endoscopic surgery (NOTES®) has generated intense interest in the surgical and gastroenterology communities. Accessing the peritoneal or thoracic spaces through internal, transvisceral incisions instead of transabdominal incisions has the potential benefits of decreasing postoperative pain, wound complications, improving cosmesis, decreasing the physiologic and immune response to surgery, decreasing anesthesia requirements, accelerating patient recovery and return to normal function, and improving access to organs that are currently difficult to reach with conventional open or laparoscopic approaches (e.g. esophagus, rectum). Given the intense interest in NOTES and its potential to revolutionize current surgical therapy, several working groups throughout the world have been formed to help guide NOTES research and clinical development. These groups include EURO-NOTES, EATS (European Association for Transluminal Surgery™), D-NOTES, ASIA-NOTES, NOSLA (Natural Orifice Surgery Latin America), Japan-NOTES, India NOTES, NOTES Research Group Brazil, and NOSCAR, which published a white paper in 2006 outlining the perceived barriers to the clinical adoption of NOTES[1]. These barriers included determining the optimal orifice to access the peritoneal cavity, developing a reliable means to close a viscotomy, minimizing the risk of infection as a result of access through a non-sterile orifice, developing an endoscopic suturing device, addressing difficulties with spatial orientation inherent to a NOTES technique, developing multi-tasking platforms to perform NOTES procedures, managing intraoperative complications, and developing NOTES training to allow safe, widespread adoption of the techniques. Although there have been numerous studies addressing some of these questions in animal and cadaver models, reports of clinical NOTES procedures in humans, and human data addressing these questions have only started to appear since 2007. This editorial will discuss the progress made on these questions by reviewing the currently available human outcomes data and clinical NOTES publications in the literature.
ACCESS TO THE PERITONEAL CAVITY
A comprehensive review of the human NOTES literature was conducted using PubMed to search the MEDLINE database with the search terms of “human natural orifice surgery, human transvaginal, human transrectal, human transgastric, or human NOTES surgery,” for articles published between January 1, 2 004 and September 1, 2 010. Manuscripts describing clinical human NOTES procedures include the use of transgastric, transvaginal, transrectal, and transesophageal approaches. Currently, the most frequently used orifice for NOTES is the vagina, with cholecystectomy accounting for the highest number of cases in the published literature[2]. Transvaginal access has the longest history of use for intraperitoneal procedures, prior to the recent description of NOTES. In 1949, Bueno described a series of transvaginal appendectomies performed with open instruments (without an endoscope) at the time of hysterectomy[3]. Since then, transvaginal access for intraperitoneal procedures in the form of culdoscopy has developed as an accepted, safe procedure in the gynecology community[4-7]. Transvaginal access can be established using a posterior colpotomy created under direct vision with open instruments, or with the use of direct trocar insertion under laparoscopic guidance. Establishment of transvaginal access does not require the use of a flexible endoscope or transanal endoscopic microsurgery (TEM) platform, unlike transgastric, transrectal, and transesophageal approaches that have been described to date. Likewise, closure of transvaginal access sites is performed with direct suturing using open instruments.
While transvaginal access is the most frequently used NOTES approach to date and can be safely performed, the potential for complications should not be overlooked. The close proximity of the rectum posteriorly, the ureters laterally, and the tendency for the small intestine to occupy the pelvis should be kept in mind while performing transvaginal NOTES. Reported complications of NOTES transvaginal access include rectal and colonic injuries, small bowel injuries, ureterovaginal fistula formation, vulvar lacerations, and bladder injuries[8-14]. Given the possibility of these complications, assistance from a gynecologist experienced in transvaginal access should be considered, at least initially, in the performance of transvaginal NOTES. In addition, simultaneous visualization of colpotomy creation with a transumbilical laparoscope, along with the use of a uterine manipulator to anteriorly retract the uterus may minimize the likelihood of rectal, bladder, or bowel injuries during the creation of transvaginal access. Most cases reported so far have utilized a “hybrid” NOTES approach, with at least one laparoscopic port used for initial visualization, retraction, and assistance with the dissection. Until instruments for NOTES improve, a “hybrid” NOTES approach may be preferable to a “pure” NOTES approach (without any percutaneous or laparoscopic assistance) in order to increase the safety of the procedures.
Transgastric access is the second-most frequently reported access route after transvaginal access in the literature. Experience with transgastric NOTES includes at least 70 transgastric peritoneoscopy procedures reported by Nau et al[15,16] and Nikfarjam et al[17], as well as several series which have reported at least 42 cholecystectomies, 15 appendectomies, PEG rescue, and 6 cases of transgastric, stapled cystogastrostomy[11,15,16,18-24]. Transgastric access in all of these cases was obtained in the anterior stomach (antrum or body) using needle knife cautery and balloon dilation through a flexible endoscope, except in cases of PEG-rescue and cystogastrostomy. Most cases were performed with placement of a laparoscopic port prior to gastrotomy creation to allow laparoscopic guidance and insufflation, while some were performed without any previous laparoscopic ports or insufflation. It is interesting to note that although no bowel injuries were recorded in transgastric peritoneoscopy cases performed without prior laparoscopic port placement, the authors noted there were instances of cautery burns to the anterior peritoneum or the under surface of the liver that were discovered after subsequent abdominal inspection with a laparoscope[15]. As such, it is not surprising that the majority of transgastric cases have been performed in a hybrid fashion, with laparoscopic visualization of the access point in order to prevent injuries to surrounding organs or the gastroepiploic vessels, which may be difficult or impossible to see from inside the stomach[2].
Transesophageal access has been used to perform esophageal myotomies in a series of 17 patients with achalasia, reported by Inoue et al[25]. This procedure, termed Per-Oral Esophageal Myotomy (POEM), incises the inner circular muscle layer of the distal esophagus and lower esophageal sphincter, while completely avoiding the hiatal dissection and disruption of the phrenoesophageal ligament that occurs during laparoscopic Heller myotomy. Transesophageal access begins at the anterior, mid-esophagus with the creation of a submucosal bleb using a sclerotherapy needle. The submucosal bleb is then incised using electrocautery and the endoscope is advanced through the incision to create a submucosal tunnel distally past the gastro-esophageal (GE) junction onto the cardia of the stomach. The inner circular muscle distal to the mucosal incision is then incised. Currently transesophageal access has been used to perform only procedures on the esophageal wall. In one case, full separation of the outer longitudinal esophageal muscle layer occurred, exposing the mediastinum. Per the authors, however, this patient did not have any adverse consequences as a result; this suggests that as long as closure of the proximal mucosal incision is ensured, transesophageal mediastinal or thoracic access through a submucosal tunnel may be clinically feasible in the future. However, no clinical studies have been performed to date investigating the safety of transesophageal mediastinal or thoracic access.
In contrast to other forms of NOTES access, transrectal access has been the least reported in the literature. The only two published cases are of a proctosigmoidectomy for cancer[26], and a transanal pull-through for Hirschsprung’s disease[27]. The proctosigmoidectomy was performed using a TEM platform, with a circumferential rectal dissection proceeding cephalad from the distal rectum, assisted by laparoscopy. The transanal pull-through was performed in an infant, without the use of the TEM; instead the authors reported using trocars inserted directly through the rectal wall to allow passage of a rigid laparoscope and rigid instruments. Although no complications were reported to have occurred in either case, further data is needed in order to accurately determine the risks of this approach.
Although so far various access points for a variety of NOTES procedures have been attempted, the specific indications that are best suited for each orifice will need to be defined. For example, the ideal indications for transoral access may end up being limited to therapeutic esophageal or gastric procedures, or diagnostic procedures in the intraperitoneal cavity. Transoral access may be poorly suited to advanced therapeutic intraperitoneal procedures given the requirement for complex, flexible instrumentation, as well as the small native diameter of the esophagus which makes extraction of large, bulky specimens potentially hazardous. Similarly, transrectal access may be best suited to colorectal applications, and transvaginal access may end up being ideally suited for gynecologic indications. However, if these two approaches prove to be the most forgiving in terms of ease of access, ability to reach the upper abdomen, complications, and the ability to introduce both flexible and rigid instruments through the orifice, it is possible that these approaches may become “workhorse” approaches for intraperitoneal NOTES procedures or specimen removal in female and male patients, respectively.
VISCERAL CLOSURE
Transvaginal closure is currently the most feasible closure method for NOTES, as the incision is closed by direct suturing. Aside from potential injuries to surrounding structures as previously mentioned, there have been no reports of vaginal dehiscence or herniation through the vaginal incision. Also, the consequences of a vaginal wound dehiscence would likely not be as potentially dangerous as a gastric leak or a rectal leak, which would introduce highly caustic or infectious luminal contents into the abdomen.
In contrast to transvaginal closure, transgastric closure currently requires the use of flexible endoscopic clips or tissue anchors, with or without laparoscopic sutures to buttress the closure. Although several groups have reported successful performance of transgastric closures without leaks, data on the true safety of current transgastric closure techniques are sparse at best. In 2010, Zorron et al[14] reported results from a prospective, multi-center NOTES registry, including data from 43 transgastric operations (29 cholecystectomies and 14 appendectomies), in which the stomach was closed using laparoscopic suturing. No gastric leaks were reported in this study. Similarly, reports of transgastric closure by other groups using endoscopic clips or anchors, with or without laparoscopic sutures, accounting for a total of approximately 30 patients, did not include any postoperative gastric leaks[18-21,23,24]. However, there has been at least one reported complication of gastric closure: a pneumothorax which occurred due to the aberrant placement of a tissue anchor through the diaphragm[24]. Innovative solutions for transgastric closure that have been reported in humans include the creation of a gastric valve mechanism made with tissue anchors, through which a gastrotomy is created[21]. The gastrotomy is then closed with additional tissue anchors once the procedure is finished. Although this technique has been successfully used in 5 patients so far, the majority of transgastric cases reported in the literature continue to rely on laparoscopic suturing alone or in combination with endoscopic instruments. Completely endoscopic means for closing gastrostomies will need to be developed and evaluated in human studies for transgastric NOTES to become feasible without laparoscopic assistance. Numerous prototype closure devices and techniques have been developed and tested in pre-clinical models. However, a detailed discussion of these devices and their results in animals are beyond the scope of this editorial.
Transesophageal NOTES closure has so far been reported using endoscopic clips to close the longitudinal mucosal incision at the entrance to the submucosal tunnel during POEM. No esophageal leaks or mediastinitis were reported in a series of 17 patients[25]. These clips slough off into the GI tract, with healing of the mucosal incision demonstrated on follow-up endoscopy.
Closure of transrectal NOTES access has so far been accomplished by incorporating the rectotomy into a hand-sewn coloanal anastomosis. This technique increases the safety of transrectal NOTES since it uses currently accepted anastomotic techniques, but it is limited to resections of the left colon and rectum. The safety of transrectal closures left in situ (not incorporated into the anastomosis) remains to be determined, although there is evidence from the TEM literature suggesting that intraperitoneal rectal closures can be performed as safely as those without peritoneal entry during full-thickness rectal tumor excision[28]. Research to test closure techniques for transrectal surgery will ultimately need to be performed on human tissue rather than porcine models for it to be useful. However, initial closure tests should be attempted on tissues that are already targeted for removal, such as in portions of the colon that will be removed following colectomy, to ensure patient safety.
RISK OF INFECTION
Concerns about potentially higher rates of infection have repeatedly been raised in regards to NOTES. The notion of introducing surgical instruments through non-sterile orifices into the normally sterile peritoneal cavity runs counter to years of established surgical dogma. Many groups performing clinical NOTES have adopted the routine use of preoperative intravenous (IV) antibiotics combined with local application of antibiotic or antiseptic solutions such as povidone-iodine at the site of visceral entry as a precaution. Although the data are currently limited, concerns about increased infectious risk with a transvaginal approach compared to conventional laparoscopy have not been substantiated. The best data so far are from a large, prospective NOTES registry including 488 patients that underwent transvaginal cholecystectomy[13]. Complications reported in this registry included urinary tract infection, abscess in the pouch of Douglas, wound infection, vaginal mycosis, and bacterial vaginitis, with a combined incidence of 1%, which is comparable to the rate of infectious complications seen with conventional laparoscopic cholecystectomy[29].
Bacterial contamination has been quantified during performance of laparoscopic roux-en-y gastric bypass (LRYGB) as a surrogate for NOTES, and during actual transgastric NOTES peritoneoscopy by investigators at Ohio State University[30,31]. These authors measured contamination in 50 patients undergoing LRYGB given preoperative IV Cefazolin alone without additional luminal decontamination, and showed that native levels of bacteria in the stomach were higher (mean 22 303 CFU/mL) compared to that of the peritoneum after the operation (1102 CFU/mL), with significant correlation between these levels. These results indicate that some cross-contamination occurs during transgastric peritoneoscopy, but that the degree of contamination is not dependent on the pre-existing level of bacteria in the stomach. In addition, despite the documented levels of contamination, no clinically obvious infections were found with a minimum of 30 d of follow-up for all patients. A follow-up study in patients undergoing transgastric NOTES peritoneoscopy prior to a planned pancreaticoduodenectomy also showed minimal cross-contamination with insignificant levels of intra-operative peritoneal contamination (160 CFU/mL), and no infectious complications in a group of 10 patients with 30 d follow-up. An observation requiring further investigation, though, was that patients on proton-pump inhibitors (PPIs) had significantly higher levels of bacteria in the stomach (median 33 000 CFU/mL) compared to those not on PPIs (median 0 CFU/mL). Differences in post-operative peritoneal contamination between patients with or without PPI use preoperatively approached, but did not reach, statistical significance due to a limited number of patients in the study. Thus, while the risk of clinically significant infection as a result of transgastric NOTES appears to be low, the optimal perioperative management of patients on PPIs undergoing NOTES requires further study.
In contrast to transvaginal and transgastric NOTES access, transesophageal and transrectal access have a theoretically higher risk of infectious complications due to their proximity to the oropharyngeal and colonic flora, respectively. Unfortunately, to date no human studies have directly quantified the levels of bacterial contamination from either of these NOTES approaches, or the true incidence of clinically significant infections. Nevertheless, in the reported series of 17 POEM patients who received preoperative IV antibiotics and irrigation of the submucosal tunnel with dilute antibiotic solution prior to closure, no infectious complications were noted with a mean follow-up period of 5 mo (minimum 1 mo)[25]. In addition, the two transrectal NOTES procedures reported in the literature to date did not report any infectious complications. The rectosigmoid resection patient underwent preoperative mechanical bowel preparation with oral sodium phospho soda, received preoperative IV Cefoxitin, and had a dilute Betadine irrigation of the rectum[26]. The 5-d-old patient who underwent a NOTES transanal pull-through received perioperative systemic antibiotics for 24 h following the case with no reported complications. In short, more data are needed to accurately estimate the risk of infectious complications with transrectal and transesophageal NOTES approaches.
The fear of increased infectious risk from NOTES procedures has so far not been substantiated by examining available clinical outcomes and bacteriologic studies. It is likely that IV antibiotics alone for transgastric procedures, along with some form of luminal disinfection for transvaginal, transrectal or transesophageal procedures will be the ultimate strategy adopted clinically.
DEVELOPMENT OF ENDOSCOPIC SUTURING OR ANASTOMOTIC DEVICES
The development of endoscopic suturing and anastomotic devices was deemed by the white paper to be necessary in order for NOTES to ultimately be applied to the wide spectrum of current surgical therapy[1]. However, the development of these devices and their use in clinical trials has proceeded slowly since 2005. Currently, two types of endoscopic suturing devices have been approved: OverStitch™ (Apollo Endosurgery, Inc., Austin, TX, USA) and the Tissue Apposition System (TAS, Ethicon Endo-surgery, Cincinnati, OH, USA). However, only use of the TAS has so far been reported clinically to approximate partial colonic wall defects at the time of laparoscopic-assisted polypectomy[32]. The TAS system works by sequentially deploying a threaded T-tag through the bowel wall on each side of a defect using an endoscopic hollow bore needle; once two threaded T-tags have been placed on either side of a defect, the two threads are cinched together and trimmed by a one-way locking mechanism in order to approximate both sides of the luminal defect. A similar endoscopic T-tag closure technique using instruments from Cook Medical (Bloomington, IN, USA) was employed by Park et al. to close gastrotomy defects during transgastric NOTES[24]. One of the difficulties with existing endoscopic T-tag systems, however, is the inability to directly visualize deployment of the T-tag from the extraluminal side of the defect without a laparoscope. This impaired visualization may contribute to the risk of inadvertent injury to surrounding organs, or deployment through a vessel. As mentioned previously, inadvertent deployment of a T-tag through the diaphragm during a gastric closure was reported to have resulted in a pneumothorax discovered post-operatively[24]. The OverStitch™, in contrast to T-tag based systems, employs a lateral needle-passing mechanism more similar to conventional suturing techniques. However, the OverStitch™ still requires assistance from an endoscopic grasper, and may be limited by the visual and mechanical constraints of conventional flexible endoscopes. Human use data will be needed to adequately evaluate the potential of the OverStitch™ for use in luminal closures.
The development of endoscopic anastomotic devices for NOTES has proceeded even more slowly than the development of suturing devices. The only reports of NOTES procedures with anastomoses have utilized hand-sewn coloanal anastomoses during colorectal resections, or a flexible, powered surgical stapler (SurgAssist™ SLC 55, Power Medical Interventions, Langhorn, PA, USA) during cystogastrostomy[33]. In the cystogastrostomy cases, the stapler was passed down the esophagus through an overtube, alongside a flexible gastroscope. Although this stapler was used successfully to create a cystogastrostomy, the authors reported significant difficulty in passing the rigid part of the stapler through the esophagus, even through a previously placed overtube. In addition, the authors reported significant difficulty directing the stapler into the appropriate angle once inside the stomach. Unfortunately, since the publication of the study, the stapler has been removed from the market due to the acquisition of Power Medical, Inc. by Covidien (Mansfield, MA) and is not currently available for use. Development of flexible, articulating, low-profile staplers is needed to make creation of anastomoses or luminal closures during NOTES more feasible. Additional features which may make application of stapling technology to NOTES more feasible include the addition of visualization and steering capabilities. These features might allow staplers to be more precisely directed into difficult to reach areas and fired with more confidence.
SPATIAL ORIENTATION
The difficulty with correct spatial orientation during NOTES and its consequences in hindering the performance of advanced procedures was foreseen in the white paper. These difficulties are inherent to the use of current flexible endoscopes to perform NOTES, and have the potential to create not only a difficult operation, but may also increase the risk of complications during NOTES. Perretta et al[34] reported a case of misinterpretation of biliary anatomy during transgastric NOTES which was fortunately recognized, preventing the occurrence of a common bile duct injury. The authors in this case converted to a laparoscopic view temporarily to clarify the unclear biliary anatomy. As emphasized by the authors, current NOTES techniques may alter the usual surgical anatomy that is seen due to the difficulty in achieving adequate retraction without laparoscopic instruments, and the spatial confusion created by retroflexion when using a flexible endoscope. A solution to the problem of difficult spatial orientation during NOTES may be the use of rigid endoscopes whenever possible. However, the use of rigid endoscopes is potentially feasible only through transvaginal or transrectal approaches, or through the umbilicus in the case of transgastric surgery. Short of using a rigid endoscope routinely, surgeons performing NOTES with flexible endoscopes should have a low threshold to convert to a laparoscopic view, even temporarily, to resolve any confusion in regards to the surgical anatomy. Although image-guided systems have been described as having potential applications for NOTES, none of these systems have been applied in a clinical setting so far[35]. Future solutions to the problem of spatial orientation may also involve the use of small, wireless cameras that are able to provide a wider, overhead view of the surgical field, and can be moved to the appropriate location as needed. Use of this type of camera has been described for human single-incision laparoscopy (SIL) cases[36]. However, it should be noted that these cameras are not currently FDA-approved.
DEVELOPMENT OF A MULTITASKING PLATFORM
The creation of a multitasking platform to allow the performance of multiple NOTES procedures with the same platform continues to be an issue of the highest priority in the development of NOTES as a viable technique. Although several types of advanced operations (nephrectomy[12,37], partial gastrectomy[38,39], sigmoidectomy[40,41], and splenectomy[42]) have been reported using a NOTES technique, many of these procedures have relied heavily on laparoscopic instruments for visualization and dissection. In order for “pure” NOTES (without laparoscopic or percutaneous assistance) to become feasible, a multi-tasking platform that balances flexibility and maneuverability with the ability to provide powerful retraction and instrument mobility, as well as an intuitive interface for the surgeon will need to be developed. Examples of the novel application of multi-lumen operating platforms for NOTES include use of a TEM platform (Figure 1) to perform proctosigmoidectomy, and the use of the TransPort™ (USGI Medical, San Clemente, CA, USA) multi-channel access port for transgastric NOTES (Figure 2). Use of a TEM platform for transrectal surgery allows the simultaneous use of rigid instruments with a flexible or rigid endoscope to perform intra-abdominal surgery. This combination of operating instruments permits strong retraction, while allowing flexible visualization and dissection capabilities through the flexible endoscope. Current limitations of such a system, however, include the difficulty of reaching beyond the sacral promontory with rigid instruments, and the limitations of dissection performed with current flexible endoscopes. The TransPort™ device is a flexible, multi-channel device which allows passage of a flexible endoscope through one channel as well as additional flexible instruments through the other channels. This device is flexible enough to be passed transgastrically and has the ability to retroflex and assume a rigid configuration independent of the endoscope. While it has been used for transgastric cholecystectomy and appendectomy[19,21,23], use of the flexible instruments through its channels is similar to the use of accessories through a conventional flexible endoscope in that the instruments have limited degrees of freedom and lack the ability to make lateral or vertical movements independent of the endoscope in an intuitive fashion. The limitations of both of these platforms make them less than ideal multi-tasking platforms for NOTES. However, the development of a system combining aspects of both platforms, along with robotic control may greatly facilitate the performance of NOTES procedures and may be the crucial enabling technology that would allow NOTES development to proceed exponentially, similar to the way the development of the charge-coupled device (CCD) camera revolutionized laparoscopy. Examples of experimental platforms with some of these capabilities that may be seen in future clinical reports include Anubis (Karl-Storz, Tuttlingen, Germany, Figure 3), EndoSamurai (Olympus, Tokyo, Japan, Figure 4), and the Direct-Drive Endoscopic System (Boston Scientific, Natick, MA, USA, Figure 5). Economic concerns continue to be an issue with regard to the development of these platforms, however. The emergence of single-incision laparosopy (SIL) has caused a tremendous amount of resources to be redirected away from NOTES, towards the development of SIL technology. Although some of this technology may end up being adapted for NOTES, the development of SIL will likely delay the development of NOTES-specific technology such as advanced multitasking platforms. Both industry and innovators in minimally-invasive surgery need to not lose site of the potential promise of NOTES, while SIL occupies the spotlight.
Figure 1.

The Transanal Endoscopic Operations device from Karl-Storz allows the insertion of rigid or flexible instruments through the anus and is currently used for performing transanal endoscopic microsurgery excisions of rectal tumors. It also has the potential to serve as a stable transrectal natural orifice translumenal endoscopic surgery (NOTES®) platform. Image used with permission (©Karl Storz).
Figure 2.

The TransPort™ multi-channel access device from USGI has been used as a transgastric natural orifice translumenal endoscopic surgery platform. It has a steering mechanism similar to a flexible endoscope, along with multiple, large-diameter channels to accommodate a small-diameter flexible endoscope and other large caliber flexible endoscopic instruments (g-Prox® tissue anchor device is shown). Image used with permission (©USGI Medical).
Figure 3.

The Anubis® platform from Karl-Storz is an advanced flexible natural orifice translumenal endoscopic surgery platform (in development), with a tip that opens to expose working instruments capable of multiple degrees of freedom controlled by the surgeon. Image used with permission (©Karl Storz).
Figure 4.
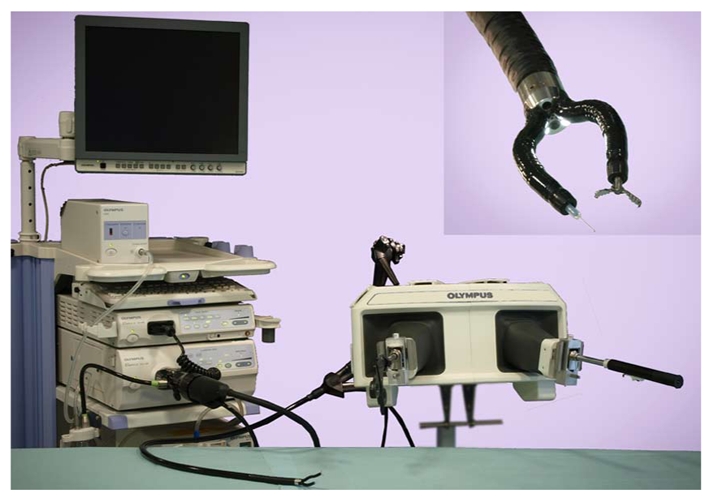
EndoSamurai is a prototype, advanced platform in development by Olympus. To operate the system, a surgeon uses an intuitive, bi-manual interface to control instruments with multiple degrees of freedom (inset shows close-up of endoscope tip with working instruments). Image used with permission (©Olympus Medical Systems Corp.).
Figure 5.

Direct-Drive Endoscopic System from Boston Scientific is a prototype, advanced multi-channel platform currently in development, featuring instruments with multiple degrees of freedom controlled through a bi-manual user interface. Inset figure shows close-up of device tip with a small diameter flexible endoscope in place. Image used with permission (©Boston Scientific).
TRAINING
There are currently not enough data from human studies to make quantitative recommendations in regards to the ideal amount of previous endoscopic or laparoscopic clinical or laboratory NOTES training prior to the performance of clinical NOTES procedures. Nevertheless, a conservative approach described in the white paper recommends that NOTES procedures be performed by multi-disciplinary teams after a period of laboratory training in a properly equipped facility in order to maximize patient safety and ensure continuing regulatory acceptance of early NOTES development.
Future NOTES practitioners will likely need some form of fundamental surgical training, along with platform-specific and procedure-specific training once the field has undergone significant development. The current paradigm of performing NOTES primarily with flexible endoscopes is reaching the limits of practicality and safety, and will arguably become quickly obsolete with the availability of advanced multitasking platforms. Thus, recommendations made in regards to training surgeons for NOTES using currently available instruments and techniques may quickly become obsolete.
COMPLICATIONS OF NOTES
Complications are an inevitable part of surgical practice, especially during the application of new techniques such as NOTES. Intraoperative complications inherent to all procedures, such as bleeding, will need to be managed appropriately to ensure patient safety. Along with the development of better endoscopic instruments to manage hemorrhage, surgical decision-making will need to evolve based on laboratory and clinical data. Although the method of hemorrhage control will always depend on the situation and surgeon judgment, it will be useful to determine what is realistically manageable using a pure versus hybrid NOTES technique, and when it would be most beneficial to convert to a full laparoscopic procedure. Unfortunately, data from human studies to answer this question are currently limited. The reported incidence of bleeding in a prospective NOTES registry of 488 transvaginal cholecystectomy patients was 0% for intraoperative bleeding, and 0.6% for postoperative bleeding, comparable with the incidence of bleeding during laparoscopic cholecystectomy[13]. However, it should be kept in mind that the dominant technique in these cases did not include the use of any flexible endoscopes or accessories, and relied heavily on dissection through a transumbilical laparoscopic port. These results may thus only apply to NOTES performed exclusively with rigid instruments, as opposed to NOTES performed using a combination of flexible and rigid instruments. A more accurate picture of NOTES outcomes from operations performed primarily with flexible endoscopes (with or without laparoscopic assistance) may be derived from the registry by Zorron et al[14], which reported the incidence of intraoperative bleeding to be approximately 2% for transvaginal cholecystectomy (all from the cystic artery), 8% for transvaginal appendectomy (all from the appendiceal artery), and a combined incidence of 4.7% for all transgastric procedures (7% for the appendiceal artery and 3.4% from the gastroepiploic artery)[14]. Although these rates of bleeding may seem high, it should be kept in mind that all of these bleeding complications occurred intraoperatively and were managed laparoscopically or endoscopically with the exception of 1 instance of gastroepiploic bleeding during transgastric access which required conversion to an open procedure. In addition, no cases of delayed postoperative bleeding were reported. Future research on the optimal method to control hemorrhage during NOTES will likely need to be performed in animal models (for ethical reasons), and should involve both the development of new instruments and algorithms to help guide intraoperative decision-making.
In addition to bleeding, the authors of the white paper foresaw the possibility that physiologic complications and compression syndromes might be more frequently seen during NOTES procedures, compared to existing laparoscopic procedures. So far the incidence of these complications in the literature has been low (0.8% of 362 NOTES procedures), however, as reported by Zorron et al[14] in a large, multi-institutional registry. These complications consisted of two episodes of intraoperative abdominal hypertension which resolved with desufflation of gas and fluid therapy, as well as one episode of facial and cervical subcutaneous emphysema following transvaginal, retroperitoneal cyst excision from the kidney[14,43]. This complication was reported to have been managed with oxygen therapy and observation in the intensive care unit, without requiring re-intubation. Although it was reported that most groups in the registry used laparoscopic insufflators through a transabdominal port or Veress needle, the case with subcutaneous emphysema used a laparoscopic carbon dioxide (CO2) insufflator connected to one of the flexible endoscopic channels with pressure maintained between 12 to 16 mmHg. Although the overall incidence of physiologic and compression syndrome complications was low in this registry report, surgeons performing NOTES should be aware that these complications may still occur and the risk of their occurrence may depend on the insufflation gas or insufflators used, and the anatomic compartment where dissection is performed.
Although the use of pressure-controlled CO2 insufflation is likely to continue being a key component of NOTES procedures, lower insufflation pressures compared to conventional laparoscopy may be feasible, further reducing the risk of compression syndromes and subcutaneous emphysema.
More serious complications during NOTES cases have been reported that would otherwise be rare in the corresponding laparoscopic operations. These are worth noting to caution those who might be tempted to prematurely or over-enthusiastically adopt this still nascent approach to intra-abdominal surgery, and also to prioritize areas for potential improvement through better patient selection or technical modifications to NOTES procedures. Reported complications of this kind during transvaginal cholecystectomy include 4 bladder injuries (0.8%), 2 rectal injuries (0.4%), and 1 small bowel injury (0.2%). All bladder injuries were reported to have occurred in older, obese women. However, it was not clear from the report whether these injuries occurred during the establishment of transvaginal access using a transvaginal trocar inserted under laparoscopic guidance or whether they occurred during the latter parts of the procedures. The occurrence of these complications emphasizes the extreme care that should be taken when establishing transvaginal access, closing the defect, and with the use of rigid transvaginal laparoscopic instruments. Similarly, the registry report by Zorron et al noted 2 esophageal hematomas, 1 esophageal laceration, and 1 esophageal perforation during 29 transgastric cholecystectomies, accounting for a combined rate of 13.7% esophageal complications. This is an unacceptably high rate of complications compared to conventional laparoscopic cholecystectomy, which is normally performed with minimal morbidity and mortality. Investigators from the International Multicenter Trial on Clinical Natural Orifice Surgery (IMTN) investigators addressed this high rate of esophageal complications and recommended the use of esophageal overtubes to protect the esophagus during the procedures, especially during specimen extraction. In agreement with this recommendation, a study conducted by our group found that preoperative ultrasound measurements of gallbladder stones can be used to help predict which gallbladders are able to be extracted through an esophageal overtube[44]. Gallbladders found to be full of multiple small stones, in which the size of the largest stone cannot be determined, as well as those in which the largest gallstone is greater than or equal to 10 mm, are unlikely to pass through an overtube. Patients with these ultrasound findings may be better managed with conventional laparoscopic cholecystectomy. Criteria such as these may help improve patient selection for transgastric cholecystectomy, for example.
Ultimately, once more human data on the risks and benefits of NOTES procedures become available surgeons will have to decide whether the benefits of NOTES are worth the risks. It should be kept in mind that just because a procedure has an inherently higher rate of a specific complication doesn’t mean it is not worthwhile. Laparoscopic cholecystectomy, for example, has been shown have increased rates of common bile duct injury compared to open cholecystectomy[45,46]. However, this risk is acceptable given that the other benefits of laparoscopic cholecystectomy (decreased postoperative pain, decreased wound complications, improved cosmesis, and a faster rate of recovery for patients) outweigh its potential for harm. The same type of analysis weighing the risks and benefits of NOTES will need to be applied to determine its ultimate role in surgical practice.
NOTES MOVING FORWARD
In the five years since the publication of the NOTES white paper, there has been a substantial proliferation of clinical NOTES publications. Progress has been made addressing the questions originally foreseen as the likely barriers to the introduction of NOTES into clinical practice. However, NOTES development in the next 10-15 years is likely to change surgical practice through a series of small incremental gains, rather than through an overnight revolution as in the case of laparoscopic surgery. This evolution may involve first a change in the practice of specimen extraction, with the use of natural orifices instead of the abdominal wall. Finally, once advanced platforms reach the clinical arena surgeons may shift to using the natural orifice not only for specimen extraction, but also for dissection. The evolution may also occur more quickly for some indications than others. For example, esophageal and colorectal NOTES applications may evolve more quickly compared to hernia, solid-organ, biliary, and general intra-abdominal applications given the already excellent outcomes and ease of laparoscopic techniques in performing these later procedures. NOTES may be able to more easily establish a niche in the thoracic esophagus, distal colon and rectum, or other anatomic locations where laparoscopic approaches are currently challenging or where there is still significant morbidity with traditional approaches. For example, limited resections performed through a natural orifice may replace the current practice of removing a large segment of colon or rectum for endoscopically unresectable polyps, assuming that oncologic outcomes can be maintained or equaled using alternative methods to assess or treat the possibility of disease in regional lymph nodes.
Given this likely evolutionary pattern for NOTES, the original goals of NOTES should be re-thought and re-prioritized. Transgastric NOTES in the near-term is unlikely to be useful to perform advanced therapeutic procedures or operations requiring removal of bulky specimens, even with the appearance of suturing devices for conventional flexible endoscopes. Rather transgastric NOTES may be better suited for diagnostic peritoneoscopy, using lower profile endoscopes that are able to traverse the gastric wall without the need for complicated closures of large, potentially dangerous gastrostomies. In addition to a decreased primary emphasis on transgastric NOTES as the access route of choice, the NOTES community should re-think its primary emphasis on flexible endoscopy as the preferred platform for NOTES, and instead be open to the use of rigid, pre-bent, or articulating instrumentation either in concert or instead of flexible instruments, until more advanced platforms become available.
CONCLUSION
In summary, since the first description of the concept of NOTES, many clinical NOTES cases have been reported in the literature, adding to the body of human data with which to begin to answering questions raised by the white paper. So far, transvaginal access has been the most feasible access route for NOTES procedures, although there is growing experience with transgastric, transesophageal, and transrectal approaches. Luminal closure appears to be most feasible with a transvaginal approach, with smaller but nevertheless good outcomes also reported for transgastric and transesophageal closures. Data on the feasibility of true, intraperitoneal transrectal closures remain limited by the fact that the only closures performed to date have been hand-sewn coloanal anastomoses. Infection appears to be a non-issue with regard to transvaginal and transgastric surgery with the use of preoperative IV antibiotics (and local disinfection in the case of transvaginal procedures), with additional data required to more accurately estimate the risk with transesophageal and transrectal procedures. Development of suturing and anastomotic devices for NOTES has progressed slowly, with limited clinical data on their use so far. Likewise, the development of true multitasking platforms for NOTES has been slow and has not yet reached the clinical arena. The optimal management of intraoperative complications has still not been determined, but the data suggest that intraoperative hemorrhage may not automatically require conversion to laparoscopy. The incidence of compression syndromes appears low, as long as procedures are performed primarily with controlled, laparoscopic insufflation using CO2. Additional major complications specific to NOTES procedures that would normally not occur during the corresponding laparoscopic operations have been noted in the literature. These types of complications absolutely need to be reported in order to constructively analyze the current status of NOTES and optimize patient selection and techniques to minimize their occurrence. As far as recommendations for NOTES training, there are no data to provide more specific recommendations outside of previous recommendations in the white paper and those from large NOTES registries. Finally, it may be useful to re-prioritize the development of NOTES to focus on high-yield colorectal and esophageal applications that are more likely to succeed in the near-term, instead of seeking the holy-grail of being able to perform entire, complicated procedures through transgastric access alone.
Footnotes
Peer reviewers: Mitsuhiro Asakuma, MD, PhD, Assistant Professor, Department of General and Gastroenterological Surgery, Osaka Medical College, 2-7 Daigaku-machi, Takatsuki, Osaka 569-8686, Japan; Mohammad Al-Haddad, MD, Assistant Professor of Clinical Medicine, Director, Endoscopic Ultrasound Fellowship Program, Indiana University School of Medicine, 550 N. University Blvd, Suite 4100, Indianapolis, IN 46 202, United States; Jeffrey Michael Marks, MD, Associate Professor, Department of Surgery, Director of Surgical Endoscopy, University Hospitals, 11 100 Euclid Avenue, Cleveland, OH 44106, United States
S- Editor Sun H L- Editor O’Neill M E- Editor Ma WH
References
- 1.Rattner D, Kalloo A. ASGE/SAGES Working Group on Natural Orifice Translumenal Endoscopic Surgery. October 2005. Surg Endosc. 2006;20:329–333. doi: 10.1007/s00464-005-3006-0. [DOI] [PubMed] [Google Scholar]
- 2.Auyang ED, Santos BF, Enter DA, Hungness ES, Soper NJ. Natural Orifice Translumenal Endoscopic Surgery (NOTES®): A Technical Review. Surg Endosc. 2011:In press. doi: 10.1007/s00464-011-1718-x. [DOI] [PubMed] [Google Scholar]
- 3.Bueno B. [Primer Caso de Apendicectomia Por Via Vaginal] Tokoginecol Pract. 1949;8:152–158. [PubMed] [Google Scholar]
- 4.Gordts S, Watrelot A, Campo R, Brosens I. Risk and outcome of bowel injury during transvaginal pelvic endoscopy. Fertil Steril. 2001;76:1238–1241. doi: 10.1016/s0015-0282(01)02887-4. [DOI] [PubMed] [Google Scholar]
- 5.Moore ML, Cohen M, Liu GY. Experience with 109 cases of transvaginal hydrolaparoscopy. J Am Assoc Gynecol Laparosc. 2003;10:282–285. doi: 10.1016/s1074-3804(05)60313-1. [DOI] [PubMed] [Google Scholar]
- 6.Shibahara H, Shimada K, Kikuchi K, Hirano Y, Suzuki T, Takamizawa S, Fujiwara H, Suzuki M. Major complications and outcome of diagnostic and operative transvaginal hydrolaparoscopy. J Obstet Gynaecol Res. 2007;33:705–709. doi: 10.1111/j.1447-0756.2007.00636.x. [DOI] [PubMed] [Google Scholar]
- 7.Tsin DA, Bumaschny E, Helman M, Colombero LT. Culdolaparoscopic oophorectomy with vaginal hysterectomy: an optional minimal-access surgical technique. J Laparoendosc Adv Surg Tech A. 2002;12:269–271. doi: 10.1089/109264202760268050. [DOI] [PubMed] [Google Scholar]
- 8.Michalik M, Orlowski M, Bobowicz M, Frask A, Trybull A. The First Report on Hybrid NOTES Adjustable Gastric Banding in Human. Obes Surg. 2010:Epub ahead of print. doi: 10.1007/s11695-010-0130-2. [DOI] [PubMed] [Google Scholar]
- 9.Decarli LA, Zorron R, Branco A, Lima FC, Tang M, Pioneer SR, Sanseverino JI, Menguer R, Bigolin AV, Gagner M. New hybrid approach for NOTES transvaginal cholecystectomy: preliminary clinical experience. Surg Innov. 2009;16:181–186. doi: 10.1177/1553350609339375. [DOI] [PubMed] [Google Scholar]
- 10.Federlein M, Borchert D, Müller V, Atas Y, Fritze F, Burghardt J, Elling D, Gellert K. Transvaginal video-assisted cholecystectomy in clinical practice. Surg Endosc. 2010;24:2444–2452. doi: 10.1007/s00464-010-0983-4. [DOI] [PubMed] [Google Scholar]
- 11.Salinas G, Saavedra L, Agurto H, Quispe R, Ramírez E, Grande J, Tamayo J, Sánchez V, Málaga D, Marks JM. Early experience in human hybrid transgastric and transvaginal endoscopic cholecystectomy. Surg Endosc. 2010;24:1092–1098. doi: 10.1007/s00464-009-0733-7. [DOI] [PubMed] [Google Scholar]
- 12.Sotelo R, de Andrade R, Fernández G, Ramirez D, Di Grazia E Carmona O, Moreira O, Berger A, Aron M, Desai MM, Gill IS. NOTES hybrid transvaginal radical nephrectomy for tumor: stepwise progression toward a first successful clinical case. Eur Urol. 2010;57:138–144. doi: 10.1016/j.eururo.2009.04.031. [DOI] [PubMed] [Google Scholar]
- 13.Lehmann KS, Ritz JP, Wibmer A, Gellert K, Zornig C, Burghardt J, Büsing M, Runkel N, Kohlhaw K, Albrecht R, et al. The German registry for natural orifice translumenal endoscopic surgery: report of the first 551 patients. Ann Surg. 2010;252:263–270. doi: 10.1097/SLA.0b013e3181e6240f. [DOI] [PubMed] [Google Scholar]
- 14.Zorron R, Palanivelu C, Galvão Neto MP, Ramos A, Salinas G, Burghardt J, DeCarli L, Henrique Sousa L, Forgione A, Pugliese R, et al. International multicenter trial on clinical natural orifice surgery--NOTES IMTN study: preliminary results of 362 patients. Surg Innov. 2010;17:142–158. doi: 10.1177/1553350610370968. [DOI] [PubMed] [Google Scholar]
- 15.Nau P, Anderson J, Happel L, Yuh B, Narula VK, Needleman B, Ellison EC, Melvin WS, Hazey JW. Safe alternative transgastric peritoneal access in humans: NOTES. Surgery. 2011;149:147–152. doi: 10.1016/j.surg.2009.10.060. [DOI] [PubMed] [Google Scholar]
- 16.Nau P, Anderson J, Yuh B, Muscarella P Jr, Christopher Ellison E, Happel L, Narula VK, Melvin WS, Hazey JW. Diagnostic transgastric endoscopic peritoneoscopy: extension of the initial human trial for staging of pancreatic head masses. Surg Endosc. 2010;24:1440–1446. doi: 10.1007/s00464-009-0797-4. [DOI] [PubMed] [Google Scholar]
- 17.Nikfarjam M, McGee MF, Trunzo JA, Onders RP, Pearl JP, Poulose BK, Chak A, Ponsky JL, Marks JM. Transgastric natural-orifice transluminal endoscopic surgery peritoneoscopy in humans: a pilot study in efficacy and gastrotomy site selection by using a hybrid technique. Gastrointest Endosc. 2010;72:279–283. doi: 10.1016/j.gie.2010.03.1070. [DOI] [PubMed] [Google Scholar]
- 18.Asakuma M, Perretta S, Allemann P, Cahill R, Con SA, Solano C, Pasupathy S, Mutter D, Dallemagne B, Marescaux J. Challenges and lessons learned from NOTES cholecystectomy initial experience: a stepwise approach from the laboratory to clinical application. J Hepatobiliary Pancreat Surg. 2009;16:249–254. doi: 10.1007/s00534-009-0089-3. [DOI] [PubMed] [Google Scholar]
- 19.Auyang ED, Hungness ES, Vaziri K, Martin JA, Soper NJ. Human NOTES cholecystectomy: transgastric hybrid technique. J Gastrointest Surg. 2009;13:1149–1150. doi: 10.1007/s11605-009-0813-y. [DOI] [PubMed] [Google Scholar]
- 20.Rao GV, Reddy DN, Banerjee R. NOTES: human experience. Gastrointest Endosc Clin N Am. 2008;18:361–370; x. doi: 10.1016/j.giec.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 21.Ujiki MB, Martinec DV, Diwan TS, Denk PM, Dunst CM, Swanström LL. Video: natural orifice translumenal endoscopic surgery (NOTES): creation of a gastric valve for safe and effective transgastric surgery in humans. Surg Endosc. 2010;24:220. doi: 10.1007/s00464-009-0547-7. [DOI] [PubMed] [Google Scholar]
- 22.Marks JM, Ponsky JL, Pearl JP, McGee MF. PEG “Rescue”: a practical NOTES technique. Surg Endosc. 2007;21:816–819. doi: 10.1007/s00464-007-9361-2. [DOI] [PubMed] [Google Scholar]
- 23.Horgan S, Cullen JP, Talamini MA, Mintz Y, Ferreres A, Jacobsen GR, Sandler B, Bosia J, Savides T, Easter DW, et al. Natural orifice surgery: initial clinical experience. Surg Endosc. 2009;23:1512–1518. doi: 10.1007/s00464-009-0428-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Park PO, Bergström M. Transgastric peritoneoscopy and appendectomy: thoughts on our first experience in humans. Endoscopy. 2010;42:81–84. doi: 10.1055/s-0029-1243795. [DOI] [PubMed] [Google Scholar]
- 25.Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265–271. doi: 10.1055/s-0029-1244080. [DOI] [PubMed] [Google Scholar]
- 26.Sylla P, Rattner DW, Delgado S, Lacy AM. NOTES transanal rectal cancer resection using transanal endoscopic microsurgery and laparoscopic assistance. Surg Endosc. 2010;24:1205–1210. doi: 10.1007/s00464-010-0965-6. [DOI] [PubMed] [Google Scholar]
- 27.Velhote MC, Velhote CE. A NOTES modification of the transanal pull-through. J Laparoendosc Adv Surg Tech A. 2009;19:255–257. doi: 10.1089/lap.2008.0211. [DOI] [PubMed] [Google Scholar]
- 28.Gavagan JA, Whiteford MH, Swanstrom LL. Full-thickness intraperitoneal excision by transanal endoscopic microsurgery does not increase short-term complications. Am J Surg. 2004;187:630–634. doi: 10.1016/j.amjsurg.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 29.A prospective analysis of 1518 laparoscopic cholecystectomies. The Southern Surgeons Club. N Engl J Med. 1991;324:1073–1078. doi: 10.1056/NEJM199104183241601. [DOI] [PubMed] [Google Scholar]
- 30.Narula VK, Happel LC, Volt K, Bergman S, Roland JC, Dettorre R, Renton DB, Reavis KM, Needleman BJ, Mikami DJ, et al. Transgastric endoscopic peritoneoscopy does not require decontamination of the stomach in humans. Surg Endosc. 2009;23:1331–1336. doi: 10.1007/s00464-008-0161-0. [DOI] [PubMed] [Google Scholar]
- 31.Narula VK, Hazey JW, Renton DB, Reavis KM, Paul CM, Hinshaw KE, Needleman BJ, Mikami DJ, Ellison EC, Melvin WS. Transgastric instrumentation and bacterial contamination of the peritoneal cavity. Surg Endosc. 2008;22:605–611. doi: 10.1007/s00464-007-9661-6. [DOI] [PubMed] [Google Scholar]
- 32.Delaney CP, Champagne BJ, Marks JM, Sanuk L, Ermlich B, Chak A. Tissue apposition system: new technology to minimize surgery for endoscopically unresectable colonic polyps. Surg Endosc. 2010;24:3113–3118. doi: 10.1007/s00464-010-1098-7. [DOI] [PubMed] [Google Scholar]
- 33.Pallapothu R, Earle DB, Desilets DJ, Romanelli JR. NOTES(®) stapled cystgastrostomy: a novel approach for surgical management of pancreatic pseudocysts. Surg Endosc. 2011;25:883–839. doi: 10.1007/s00464-010-1289-2. [DOI] [PubMed] [Google Scholar]
- 34.Perretta S, Dallemagne B, Donatelli G, Mutter D, Marescaux J. Multimedia article. The fear of transgastric cholecystectomy: misinterpretation of the biliary anatomy. Surg Endosc. 2011;25:648. doi: 10.1007/s00464-010-1234-4. [DOI] [PubMed] [Google Scholar]
- 35.Coughlin G, Samavedi S, Palmer KJ, Patel VR. Role of image-guidance systems during NOTES. J Endourol. 2009;23:803–812. doi: 10.1089/end.2008.0121. [DOI] [PubMed] [Google Scholar]
- 36.Cadeddu J, Fernandez R, Desai M, Bergs R, Tracy C, Tang SJ, Rao P, Desai M, Scott D. Novel magnetically guided intra-abdominal camera to facilitate laparoendoscopic single-site surgery: initial human experience. Surg Endosc. 2009;23:1894–1899. doi: 10.1007/s00464-009-0459-6. [DOI] [PubMed] [Google Scholar]
- 37.Kaouk JH, Haber GP, Goel RK, Crouzet S, Brethauer S, Firoozi F, Goldman HB, White WM. Pure natural orifice translumenal endoscopic surgery (NOTES) transvaginal nephrectomy. Eur Urol. 2010;57:723–726. doi: 10.1016/j.eururo.2009.10.027. [DOI] [PubMed] [Google Scholar]
- 38.Fischer LJ, Jacobsen G, Wong B, Thompson K, Bosia J, Talamini M, Horgan S. NOTES laparoscopic-assisted transvaginal sleeve gastrectomy in humans-description of preliminary experience in the United States. Surg Obes Relat Dis. 2009;5:633–636. doi: 10.1016/j.soard.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 39.Nakajima K, Nishida T, Takahashi T, Souma Y, Hara J, Yamada T, Yoshio T, Tsutsui T, Yokoi T, Mori M, et al. Partial gastrectomy using natural orifice translumenal endoscopic surgery (NOTES) for gastric submucosal tumors: early experience in humans. Surg Endosc. 2009:Epub ahead of print. doi: 10.1007/s00464-009-0474-7. [DOI] [PubMed] [Google Scholar]
- 40.Lacy AM, Delgado S, Rojas OA, Almenara R, Blasi A, Llach J. MA-NOS radical sigmoidectomy: report of a transvaginal resection in the human. Surg Endosc. 2008;22:1717–1723. doi: 10.1007/s00464-008-9956-2. [DOI] [PubMed] [Google Scholar]
- 41.Sanchez JE, Rasheid SH, Krieger BR, Frattini JC, Marcet JE. Laparoscopic-assisted transvaginal approach for sigmoidectomy and rectocolpopexy. JSLS. 2009;13:217–220. [PMC free article] [PubMed] [Google Scholar]
- 42.Targarona EM, Gomez C, Rovira R, Pernas JC, Balague C, Guarner-Argente C, Sainz S, Trias M. NOTES-assisted transvaginal splenectomy: the next step in the minimally invasive approach to the spleen. Surg Innov. 2009;16:218–222. doi: 10.1177/1553350609345488. [DOI] [PubMed] [Google Scholar]
- 43.Zorron R, Goncalves L, Leal D, Kanaan E, Cabral I, Saraiva P. Transvaginal hybrid natural orifice transluminal endoscopic surgery retroperitoneoscopy--the first human case report. J Endourol. 2010;24:233–237. doi: 10.1089/end.2009.0230. [DOI] [PubMed] [Google Scholar]
- 44.Santos BF, Auyang ED, Hungness ES, Desai KR, Chan ES, van Beek DB, Wang EC, Soper NJ. Preoperative ultrasound measurements predict the feasibility of gallbladder extraction during transgastric natural orifice translumenal endoscopic surgery cholecystectomy. Surg Endosc. 2010:Epub ahead of print. doi: 10.1007/s00464-010-1334-1. [DOI] [PubMed] [Google Scholar]
- 45.Russell JC, Walsh SJ, Mattie AS, Lynch JT. Bile duct injuries, 1989-1993. A statewide experience. Connecticut Laparoscopic Cholecystectomy Registry. Arch Surg. 1996;131:382–388. doi: 10.1001/archsurg.1996.01430160040007. [DOI] [PubMed] [Google Scholar]
- 46.Targarona EM, Marco C, Balagué C, Rodriguez J, Cugat E, Hoyuela C, Veloso E, Trias M. How, when, and why bile duct injury occurs. A comparison between open and laparoscopic cholecystectomy. Surg Endosc. 1998;12:322–326. doi: 10.1007/s004649900662. [DOI] [PubMed] [Google Scholar]


