Abstract
BACKGROUND
A large body of literature suggests that socioeconomic status (SES) is positively associated with mental and physical health. However, little research has examined the impact of SES on psychological adjustment after a major stressor. The current study examined whether SES (education and financial status) was associated with distress (anxiety and depression) in women diagnosed with ductal carcinoma in situ (DCIS). This study also explored whether social support explained the association between SES and distress and whether social support buffered the impact of low SES on distress.
METHODS
A total of 487 women with newly diagnosed DCIS were enrolled in the study. Participants completed questions about sociodemographic, psychosocial, and clinical characteristics at the time of enrollment and 9 months after their diagnosis.
RESULTS
Financial status was inversely associated with anxiety and depression at the 9-month follow-up. Financial status also predicted change in anxiety and depression. Women with high financial status reported a decline in anxiety and depression during the study period, whereas women with medium or low financial status reported an increase in anxiety and depression. In addition, the probability of exceeding the screening threshold suggestive of clinical depression increased with decreasing financial status. Education was not associated with anxiety or depression. The presence of social support did not explain the association between financial status and change in distress. Social support did not buffer the effect of low SES on anxiety and depression.
CONCLUSIONS
Women with medium or low SES were vulnerable to escalating anxiety and depression after a DCIS diagnosis.
Keywords: ductal carcinoma in situ, intraductal, noninfiltrating, social class, anxiety, depression, social support
Ductal carcinoma in situ (DCIS) is a noninvasive breast cancer that constitutes between 12% and 15% of breast cancers.1 Although the biological characteristics and treatment options of DCIS have been the subject of growing research over the past several decades, only a small number of studies have examined the psychosocial sequelae of a DCIS diagnosis.2–6 In addition, no research has been conducted to identify socioeconomic subgroups of women who might be vulnerable to psychological morbidity after a DCIS diagnosis.
Research on the psychosocial sequelae of a DCIS diagnosis is warranted for several reasons. First of all, DCIS is generally not life-threatening. When treated with standard therapy, the majority of cases will not result in local or systemic recurrence.1,7 Yet, similar to invasive breast cancer, the primary treatment for DCIS is surgery, with 30% of women undergoing mastectomy and 60% undergoing a breast-conserving procedure.1 Consequently, women with DCIS may experience many of the same psychosocial issues as women who are treated for invasive breast cancer, such as anxiety,8–10 depression, sexual problems, and negative body image.9 In fact, the limited research that has directly compared women with DCIS to women with invasive breast cancer has found no difference in their levels of psychological symptoms (ie, difficulty sleeping, anxiety, and depression),2 quality of life, and overall well-being.3 However, women with DCIS may experience fewer physical symptoms, better general health, and a less negative impact on their sex life and interpersonal relationships than women with invasive breast cancer.3
The word carcinoma and the surgical treatments for DCIS suggest a level of disease severity, and the distinction between invasive and noninvasive cancer can be confusing for many patients.4,5 In addition, women report being frustrated by the lack of available information about their DCIS.4,5 A shortage of information may leave women with DCIS unaware of their true breast cancer risk. For example, research suggests that women with DCIS do not differ from women with invasive breast cancer in their perceived risk of local or distant recurrence or distant metastases2 or of dying from their disease.3 Furthermore, between 54% and 61% of women perceived at least a moderate risk for disease recurrence,6,11 and 39% perceived at least a moderate risk for invasive cancer in the next 5 years.6 These risk perceptions are inaccurate, as true risk for local recurrence in the form of DCIS or invasive breast cancer after modern therapy ranges approximately 1% to 7%.12–14 Prior work from our group suggests that distress may contribute to inaccurate risk perceptions. For example, women with elevated DCIS-related intrusive or avoidant thoughts were more likely to overestimate their risk of metastasis, whereas women with elevated anxiety were more likely to overestimate their risk of a DCIS or invasive breast cancer recurrence and of developing invasive breast cancer in their lifetime.6
To effectively address the psychosocial needs of women with DCIS, it is important to consider that the incidence and prevalence of distress after DCIS may not be equal across all women, but instead may vary by socioeconomic status (SES). SES is inversely associated with psychological morbidity after an invasive cancer diagnosis.15–22 In addition, SES dictates access to important resources such as money, knowledge, and social connections/support that could be used to minimize the impact of a major health crisis such as a cancer diagnosis.23–29 Women with low SES may not have the same financial and psychosocial resources to cope with their DCIS; thus, this population may be vulnerable to anxiety and depression after their diagnosis. The extent to which SES affects distress after a DCIS diagnosis has not been previously addressed.
The authors conducted a prospective longitudinal observational study to examine the psychosocial impact of a DCIS diagnosis.6 The current paper analyzes a subset of these data to examine whether SES was associated with anxiety and depression in these women. Because social support is inversely associated with distress across populations,30,31 and social support is positively associated with SES,24–28 this paper also explores whether the association between SES and distress was explained by differences in social support (mediation) and whether social support buffered against distress among women with low SES (moderation). We hypothesized that 1) women’s distress (anxiety and depression) would be inversely associated with their SES (education and financial status) at baseline and at the 9-month follow-up; 2) SES would predict a change in distress from baseline to the 9-month follow-up; and 3) social support would mediate and moderate the association between SES and anxiety and depression.
MATERIALS AND METHODS
Participants
All women newly diagnosed with DCIS were identified by review of pathology records from participating academic centers and community-based hospitals using the Dana-Farber/Harvard Cancer Center Rapid Case Registry. Women were eligible if they had a diagnosis of DCIS without evidence of invasion, a final surgical procedure no more than 3 months before enrollment in the study, and were able to understand written and spoken English or written Spanish. Women were excluded if they had a previous diagnosis of invasive breast cancer and if their physician did not provide study staff permission to contact them. Eligible women were sent a letter of introduction and an informational pamphlet about the study. Enclosed with these materials was a preaddressed stamped decline card that women could return if they did not wish to be contacted about the study. If project staff did not receive the decline card within 10 to 14 days of when the letter was sent, women were mailed a consent form and the baseline questionnaire.
To maximize data quality and improve compliance with the study, the questionnaires were administered by trained interviewers via telephone. After the consent form was received, a telephone interviewer called participants to confirm their willingness to participate and schedule a 45-minute interview to collect the questionnaire data. Participants were reassessed using these data-collection procedures 9 months after their diagnosis.
Measures
Study participants completed measures of their sociodemographic, psychosocial, and clinical characteristics.
SES
Two indicators of SES were assessed. Education was measured as the highest grade of schooling that women completed. Education was chosen because it is a stable marker of resources and social standing. Financial status was measured with the question, “how would you describe your household’s financial situation right now.” Response options referred to the level of difficulty that women experienced with paying their bills. Financial status was chosen because it captures women’s present resources for meeting life’s challenges. Education and financial status were measured at baseline.
Sociodemographic Variables
The following sociodemographic characteristics were assessed: age, ethnicity, employment status, medical insurance (yes/no), and marital status. These variables were measured at baseline.
Depression
Symptoms of depression were measured using the Center for Epidemiologic Studies Depression scale (CES-D), a 20-item scale that measures the frequency of respondents’ depressive symptomatology over the previous week.32 The CES-D was scored on a 4-point Likert scale, with response options ranging from rarely or none of the time to most or all of the time. Possible scores range from 0 to 60, with higher scores indicating more symptoms. A score of ≥16 is traditionally interpreted as suggestive of clinical depression and a need for further screening. Cronbach alpha ranged from .84 to .90. Test-retest reliability ranged from .41 to .54 in 3- to 12-month intervals. The CES-D demonstrates good concurrent and convergent validity. Depression was measured at baseline and at the 9-month follow-up.
DCIS-related Anxiety
DCIS-related anxiety was measured with the 15-item Impact of Events Scale (IES) modified to refer to DCIS as the stressor. The IES comprises 2 subscales. The intrusive thoughts subscale measures the frequency with which thoughts, images, and dreams intrude into consciousness.33 The avoidance subscale measures the frequency with which thoughts and feelings associated with an event are avoided.33 A composite of the intrusive thoughts and avoidance subscales was used for all analyses. The IES is scored on a 4-point Likert scale with the response options ranging from not at all to often. The numerical scores associated with these 4 response options are 0, 1, 3, and 5. Possible scores on the IES range from 0 to 75. A score of 26 to 43 is suggestive of moderate symptoms; a score ≥44 is suggestive of severe symptoms. Cronbach alpha was .78 for the intrusion subscale and .82 for the avoidance subscale. Test-retest reliability for the combined scale was .87. This scale also demonstrates good concurrent and convergent validity. DCIS-related anxiety was measured at baseline and at the 9-month assessment.
Social Support
Social support was measured using the Medical Outcomes Study Social Support Survey, a 20-item scale that assesses how often someone receives 4 different aspects of social support: emotional/informational, tangible, positive social interaction, and expressions of affection.34 A composite social support variable was used in all analyses. This scale is scored on a 5-point Likert scale, with response options ranging from none of the time to all of the time. Mean scores for each subscale were computed and then transformed so that the lowest score was 0 and the highest score was 100. Cronbach alpha ranged from .97 to .97 across the subscales. The Medical Outcomes Study Social Support Survey also demonstrates good convergent and discriminant validity. Social support was measured at baseline.
Clinical Variables
Women were asked about the following clinical characteristics: menopausal status, major comorbid conditions, type of surgical procedure, receipt of radiotherapy, and the use of tamoxifen. DCIS grade and the presence of comedonecrosis were abstracted from women’s medical records.
Statistical Analysis
Multivariate linear regression was used to test whether education or financial status was associated with participants’ anxiety and depression at baseline and at the 9-month follow-up, and whether education or financial status predicted change in participants’ anxiety or depression after controlling for baseline levels. A chi-square test was used to assess whether the probability of scoring ≥16 on the CES-D and ≥26 on the IES at baseline and at the 9-month follow-up differed by education and financial status. The procedure recommended by Baron and Kenny35 was used to test whether level of social support explained (ie, mediated) the relationship between SES and change in the dependent variables (anxiety and depression) after controlling for baseline levels. First, the hypothesized mediator, social support, was regressed on the independent variable, SES, to assess whether a relation existed between them. Second, the dependent variables were regressed separately on SES to test whether they were related. Third, the dependent variables were regressed on social support. Fourth, the dependent variables were regressed on social support and SES simultaneously. Mediation was supported if the first 3 models were statistically significant and the effect of group on change in the dependent variables was lessened or eliminated in the presence of social support.35 To test whether social support buffered (ie, moderated) the association between SES and change in anxiety and depression, a SES by social support interaction term was entered into a multivariate linear regression model to predict change in anxiety and depression. All multivariate models controlled for sociodemographic (age, marital status, employment status, and race/ethnicity) and clinical (menopausal status, receipt of tamoxifen, number of comorbidities, receipt of mastectomy, grade, and presence of comedonecrosis) factors that were hypothesized a priori as being potential confounders of the association between SES and anxiety and depression or that were associated with both SES and distress in univariate analyses. All statistical tests were 2-sided, and all analyses were conducted using the SAS system for Windows (Release 9.1; SAS Institute, Cary, NC).
RESULTS
Participant Characteristics
Eight hundred fifteen women with newly diagnosed DCIS were identified from the Rapid Case Registry. Of these, 45 women were deemed ineligible, 205 declined to participate when contacted, and 72 women did not respond despite repeated attempts to contact them. Four hundred eighty-seven women (64% of eligible patients) consented to participate and completed the baseline questionnaires. These women were younger than the women who did not enroll in the study (P < .001); however, no other differences were found between the women who were identified and the women who enrolled. Four hundred twenty-six women completed the 9-month assessment (87%). These women had higher financial status (P < .001), underwent more procedures to treat their DCIS (P < .001), and were more likely to have had a mastectomy (P < .001) than women who did not complete the 9-month assessment. Participant characteristics at baseline are summarized in Table 1.
Table 1.
Sample Characteristics (N = 487)
| Characteristic | No. | % |
|---|---|---|
| Race | ||
| White | 459 | 94 |
| Nonwhite | 27 | 6 |
| Missing | 1 | |
| Marital status | ||
| Married/living as married | 333 | 68 |
| Divorced/separated | 66 | 14 |
| Single | 47 | 10 |
| Widowed | 40 | 8 |
| Missing | 1 | |
| Education | ||
| High school graduate or less | 75 | 16 |
| Technical/vocational school graduate | 11 | 2 |
| Some college | 104 | 21 |
| College graduate | 150 | 31 |
| Postcollege graduate | 147 | 30 |
| Financial status | ||
| High (money for special things that you want) | 339 | 70 |
| Medium (little spare money to buy extra or special things) | 86 | 18 |
| Low (able to pay bills, but need to cut back on special things and difficulty paying the bills no matter what) | 57 | 12 |
| Comorbid conditions | ||
| 0 | 253 | 53 |
| 1 | 113 | 24 |
| 2+ | 114 | 23 |
| Missing | 13 | |
| Menopause within previous 12 months | 27 | 55 |
| Tamoxifen | 184 | 43 |
| Mastectomy | ||
| Yes | 145 | 30 |
| No | 280 | 57 |
| Missing | 62 | 13 |
| Radiation | 211 | 50 |
| Grade of DCIS | ||
| 1 | 97 | 23 |
| 2 | 171 | 40 |
| 3 | 163 | 38 |
| Missing/unknown | 25 | |
| Comedonecrosis | ||
| Yes | 118 | 26 |
| No | 344 | 74 |
| Missing | 25 | |
| Sample Mean σ | ||
| Age y | 54.04 | 11.02 |
| Depression (baseline) | 9.84 | 9.22 |
| Anxiety (baseline) | 15.86 | 14.05 |
DCIS indicates ductal carcinoma in situ.
SES, Anxiety, and Depression
Financial status was not associated with distress at baseline. However, financial status was positively associated with depression and anxiety at the 9-month follow-up (Table 2). In addition, financial status predicted change in anxiety (F2,345 = 7.78, P = .0005) and depression (F2,348 = 7.54, P = .0006) from baseline to follow-up. Figure 1 suggests that women with high financial status experienced a decline in anxiety and depression over time, whereas women with medium or low financial status experienced an increase in anxiety and depression over the study period. Contrary to our hypothesis, education was not associated with either anxiety or depression in cross-sectional or longitudinal analyses. The percentage of women who scored ≥16 on our measure of depression—suggesting clinical depression and a need for further screening—increased with decreasing financial status at baseline (chi-square [2, n = 480] = 12.39, P = .002) and follow-up (chi-square [2, n = 414] = 18.06, P = .0001). We saw a similar pattern of results with respect to women who exceeded the threshold for moderate symptoms of anxiety; however, these findings were not statistically significant. The probability of scoring ≥16 on our measure of depression and exceeding the threshold for moderate anxiety did not differ by educational attainment.
Table 2.
The Cross-Sectional Association Between Socioeconomic Status and Psychological Morbidity at Baseline and Follow-Upa
| Dependent Variable | Independent Variable | F | df | P |
|---|---|---|---|---|
| BL depression | Education | 0.00 | 2364 | .99 |
| BL depression | Financial status | 2.94 | 2360 | .05b |
| BL anxiety | Education | 0.48 | 2363 | .62 |
| BL anxiety | Financial status | 1.26 | 2359 | .29 |
| FU depression | Education | 0.15 | 2353 | .86 |
| FU depression | Financial status | 9.84 | 2349 | .0001 |
| FU anxiety | Education | 2.02 | 2350 | .13 |
| FU anxiety | Financial status | 10.17 | 2346 | .0001 |
BL indicates baseline; FU, follow-up.
All models controlled for age, marital status, employment status, menopausal status, number of comorbidities, receipt of tamoxifen, receipt of mastectomy, grade, and comedonecrosis.
The sample size for Table 2 ranged from 377 to 388 due to missing data.
P = .054.
Figure 1.
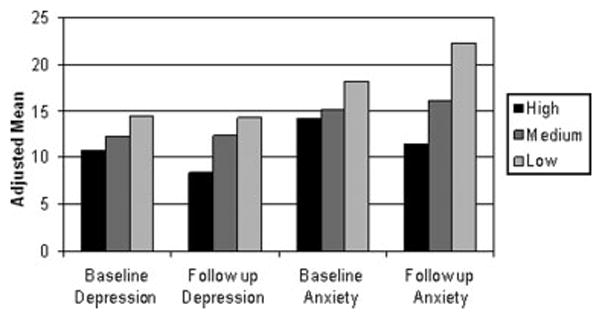
Mean anxiety and depression are shown by financial status.
Mediation
Education was not associated with anxiety or depression; thus, it was not included in our tests for mediation. The mediation analyses for financial status suggested the following: 1) social support was associated with financial status (Table 3); 2) financial status predicted change in anxiety and depression; and 3) social support was associated with change in anxiety and depression (Table 3). However, when we added social support to a model that also contained financial status, financial status was still significantly associated with change in anxiety and depression (Table 3). Thus, social support did not mediate the relationship between financial status and change in anxiety and depression. From these analyses we conclude that the relationship between financial status and change in anxiety and depression is not explained by differences in social support.
Table 3.
Mediation Analysesa
| Mediation Step | Independent Variable | Dependent Variable | Mediator | F | df | P |
|---|---|---|---|---|---|---|
| I | Financial status | Total support | 3.45 | 2361 | .03 | |
| III | Total support | Δ Anxiety | 7.26 | 1350 | .01 | |
| Total support | Δ Depression | 17.75 | 1353 | .00 | ||
| IV | Financial status | Δ Anxiety | Total support | 6.89 | 2344 | .00 |
| Financial status | Δ Depression | Total support | 6.38 | 2347 | .00 |
Δ indicates change.
All models controlled for age, marital status, employment status, menopausal status, number of comorbidities, receipt of tamoxifen, receipt of mastectomy, grade, and comedonecrosis.
The sample size for Table 2 ranged from 373 to 388 due to missing data.
Moderation
Social support did not consistently moderate the association between SES (education and financial status) and distress (anxiety and depression). Thus, we conclude that social support did not buffer the impact of low financial status or education on anxiety and depression.
DISCUSSION
Contrary to our hypothesis, financial status was not associated with distress at baseline. However, as hypothesized, financial status was inversely associated with anxiety and depression at the 9-month follow-up. In addition, the association between financial status and distress appears to be graded: women with high financial status reported a decline in depression and anxiety; women with medium financial status reported a small increase in depression and anxiety; and women with low financial status reported a relatively large increase in depression and anxiety during the study. Furthermore, the percentage of women who scored ≥16 on our measure of depression—suggesting clinical depression and a need for further screening—increased with decreasing financial status, thereby suggesting that our findings were not only statistically significant but also clinically significant.
Collectively, these results suggest that after a stressful life event such as a DCIS diagnosis, women with medium or low financial status may not have the same resources to cope with their health problems as women with high financial status. In addition, women with medium and low SES are forced to manage competing stressors: the stress of financial hardship and the stress of a major health event. Women who are unable to work after their DCIS, a situation more common for people with lower SES,36–40 have another stressor that must be dealt with. The combination of fewer coping resources and greater concomitant stressors leave women with medium or low SES vulnerable to escalating distress after their DCIS diagnosis. Our findings for financial status are consistent with other studies published in invasive cancer populations suggesting that SES was inversely associated with psychological morbidity such as symptom distress, mood disturbance,17,19 and post-traumatic stress disorder-like symptoms,20 and positively associated with aspects of mental health15–22 such as post-traumatic growth16 and psychosocial adjustment.17,18
Education was not associated with anxiety or depression in cross-sectional or longitudinal analyses, which is contrary to other studies that found a positive association between education and health outcomes.41–44 Educational attainment is important for health because it shapes employment opportunities and earning potential,41,42 and it is positively associated with psychosocial resources that can be protective after a stressful life experience.41 Although important for health when examined at the population level, education is actually 1 mechanism through which one obtains material and psychosocial resources. It is possible that actual material and psychosocial resources are more important for health, especially when we examine health outcomes at an individual level.
A second aim of this study was to examine whether social support explained the association between SES and distress. On the basis of our mediation analyses, social support was strongly associated with financial status and distress; however, social support did not mediate the association between these 2 variables. Thus, the association between financial status and distress was not explained by differences in social support.
The final aim of the study was to assess whether social support buffered the impact of low SES on distress. Contrary to our hypothesis, social support did not consistently moderate the association between SES (financial status and education) and change in distress (anxiety and depression).
Limitations
The biggest limitation of this research was the response rate. Only 64% of eligible patients consented to participate and completed the baseline questionnaires. The women who enrolled appeared to be representative all eligible women (with the exception of being younger); however, the response rate that we achieved limits the generalizability of our findings. Second, social support and financial status were only measured at baseline; thus, we have no data on whether these factors changed over time. Third, we were unable to distinguish whether concerns about DCIS, financial burdens, or some other factor explained the association between financial status and distress. Fourth, we did not collect data on the provider who managed women’s care (eg, medical oncologist or surgeon); in addition, we do not know whether women saw a social worker or psychologist during their treatment. Thus, we do not know to what extent women’s psychosocial needs were assessed and addressed during treatment and how this could have affected the results of our study.
Strengths
This study also has some important strengths. First of all, it is the largest longitudinal study conducted to date to address psychosocial functioning in women with DCIS, and the results provide valuable information about which women are likely to experience poor psychological adjustment. In addition, we collected 2 measures of SES, which allowed us to examine the relative importance of each for anxiety and depression. Finally, our results indicated that a measure of financial resources may be a stronger predictor of adjustment than other indicators of SES when adjustment is measured at the individual level.
Conclusions
Women with medium or low SES were vulnerable to escalating anxiety and depression during the study. Although we could not determine the pathways through which financial status increased distress, our results suggested that women with low financial status may benefit from a psychosocial intervention that is designed to accommodate their unique needs. Although not specifically addressed by the current study, patient navigators may be a mechanism to address the psychosocial needs of low SES women with DCIS as well as other underserved cancer populations.45–47 The utility of patient navigation for this population should be explored in future research.
Footnotes
CONFLICT OF INTEREST DISCLOSURES
This research was supported by Dana-Farber/Harvard Cancer Center Specialized Program of Research Excellence in Breast Cancer (5 P50 CA89393-03), the Harvard Education Program in Cancer Prevention Control (5R25CA057711-15), and Dissemination Research to Reduce Cancer Disparities (5K05CA124415-02).
References
- 1.Winchester DP, Jeske JM, Goldschmidt RA. The diagnosis and management of ductal carcinoma in-situ of the breast. CA Cancer J Clin. 2000;50:184–200. doi: 10.3322/canjclin.50.3.184. [DOI] [PubMed] [Google Scholar]
- 2.Rakovitch E, Franssen E, Kim J, et al. A comparison of risk perception and psychological morbidity in women with ductal carcinoma in situ and early invasive breast cancer. Breast Cancer Res Treat. 2003;77:285–293. doi: 10.1023/a:1021853302033. [DOI] [PubMed] [Google Scholar]
- 3.van Gestel YRBM, Voogd AC, Vingerhoets AJJM, et al. A comparison of quality of life, disease impact and risk perception in women with invasive breast cancer and ductal carcinoma in situ. Eur J Cancer. 2007;43:549–556. doi: 10.1016/j.ejca.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 4.De Morgan S, Redman S, White KJ, Cakir B, Boyages J. Well, have I got cancer or haven’t I?” The psychosocial issues for women diagnosed with ductal carcinoma in situ. Health Expect. 2002;5:310–318. doi: 10.1046/j.1369-6513.2002.00199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Webb C, Koch T. Women’s experiences of non-invasive breast cancer: literature review and study report. J Adv Nurs. 1997;25:514–525. doi: 10.1046/j.1365-2648.1997.t01-1-1997025514.x. [DOI] [PubMed] [Google Scholar]
- 6.Partridge A, Adloff K, Blood E, et al. Risk perceptions and psychosocial outcomes of women with ductal carcinoma in situ: longitudinal results from a cohort study. J Natl Cancer Inst. 2008;100:243–251. doi: 10.1093/jnci/djn010. [DOI] [PubMed] [Google Scholar]
- 7.Sanders ME, Schuyler PA, Dupont WD, Page DL. The natural history of low-grade ductal carcinoma in situ of the breast in women treated by biopsy only revealed over 30 years of long-term follow-up. Cancer. 2005;103:2481–2484. doi: 10.1002/cncr.21069. [DOI] [PubMed] [Google Scholar]
- 8.Gottschalk LA, Hoigaard-Martin J. The emotional impact of mastectomy. Psychiatry Res. 1986;17:153–167. doi: 10.1016/0165-1781(86)90070-3. [DOI] [PubMed] [Google Scholar]
- 9.Goldberg JA, Scott RN, Davidson PM, et al. Psychological morbidity in the first year after breast surgery. Eur J Surg Oncol. 1992;18:327–331. [PubMed] [Google Scholar]
- 10.Burgess C, Cornelius V, Love S, Graham J, Richards M, Ramirez A. Depression and anxiety in women with early breast cancer: 5 year observational cohort study. BMJ. 2005;330:702. doi: 10.1136/bmj.38343.670868.D3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bluman LG, Borstelmann NA, Rimer BK, Iglehart JD, Winer EP. Knowledge, satisfaction, and perceived cancer risk among women diagnosed with ductal carcinoma in situ. J Womens Health Gend Based Med. 2001;10:589–598. doi: 10.1089/15246090152543175. [DOI] [PubMed] [Google Scholar]
- 12.Fisher B, Dignam J, Wolmark N, et al. Lumpectomy and radiation therapy for the treatment of intraductal breast cancer: findings from National Surgical Adjuvant Breast and Bowel Project B-17. J Clin Oncol. 1998;16:441–452. doi: 10.1200/JCO.1998.16.2.441. [DOI] [PubMed] [Google Scholar]
- 13.Fisher B, Dignam J, Wolmark N, et al. Tamoxifen in treatment of intraductal breast cancer: National Surgical Adjuvant Breast and Bowel Project B-24 randomized controlled trial. Lancet. 1999;353:1993–2000. doi: 10.1016/S0140-6736(99)05036-9. [DOI] [PubMed] [Google Scholar]
- 14.Lee L, Silverstein M, Chung C, et al. Breast cancer-specific mortality after invasive local recurrence in patients with ductal carcinoma-in-situ of the breast. Am J Surg. 2006;192:416–419. doi: 10.1016/j.amjsurg.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 15.Parker PA, Baile WF, de Moor C, Cohen L. Psychosocial and demographic predictors of quality of life in a large sample of cancer patients. Psychooncology. 2003;12:183–193. doi: 10.1002/pon.635. [DOI] [PubMed] [Google Scholar]
- 16.Cordova MJ, Cunningham LLC, Carlson CR, Andrykowski MA. Posttraumatic growth following breast cancer: a controlled comparison study. Health Psychol. 2001;20:176–185. [PubMed] [Google Scholar]
- 17.Kornblith AB, Anderson J, Cella DF, et al. Comparison of psychosocial adaptation and sexual function of survivors of advanced Hodgkin disease treated by MOPP, ABVD, or MOPP alternating with ABVD. Cancer. 1992;70:2508–2516. doi: 10.1002/1097-0142(19921115)70:10<2508::aid-cncr2820701020>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 18.Schnoll RA, Harlow LL. Using disease-related and demographic variables to form cancer-distress risk groups. J Behav Med. 2001;24:57–74. doi: 10.1023/a:1005686404723. [DOI] [PubMed] [Google Scholar]
- 19.Kornblith AB, Anderson J, Cella DF, et al. Hodgkin disease survivors at increased risk for problems in psychosocial adaptation. The Cancer and Leukemia Group B. Cancer. 1992;70:2214–2224. doi: 10.1002/1097-0142(19921015)70:8<2214::aid-cncr2820700833>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 20.Cordova MJ, Andrykowski MA, Kenady DE, McGrath PC, Sloan DA, Redd WH. Frequency and correlates of posttraumatic-stress-disorder-like symptoms after treatment for breast cancer. J Consult Clin Psychol. 1995;63:981–986. doi: 10.1037//0022-006x.63.6.981. [DOI] [PubMed] [Google Scholar]
- 21.Marmot MG, Fuhrer R, Ettner SL, Marks NF, Bumpass LL, Ryfff CD. Contribution of psychosocial factors to socioeconomic differences in health. Milbank Q. 1998;76:403–448. doi: 10.1111/1468-0009.00097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adler NE, Conner Snibbe A. The role of psychosocial processes in explaining the gradient between socioeconomic status and health. Curr Dir Psychol Sci. 2003;12:119–123. [Google Scholar]
- 23.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;(Spec No):80–94. [PubMed] [Google Scholar]
- 24.Cohen S, Kaplan GA, Salonen JT. The role of psychological characteristics in the relation between socioeconomic status and perceived health. J Appl Soc Psychol. 1999;29:445–468. [Google Scholar]
- 25.Mickelson KD, Kubzansky LD. Social distribution of social support: the mediating role of life events. Am J Commun Psychol. 2003;32:265–281. doi: 10.1023/b:ajcp.0000004747.99099.7e. [DOI] [PubMed] [Google Scholar]
- 26.Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: do negative emotions play a role? Psychol Bull. 2003;129:10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- 27.Taylor SE, Seeman TE. Psychosocial resources and the SES-health relationship. Ann N Y Acad Sci. 1999;896:210–225. doi: 10.1111/j.1749-6632.1999.tb08117.x. [DOI] [PubMed] [Google Scholar]
- 28.Turner RJ, Noh S. Class and psychological vulnerability among women: the significance of social support and personal control. J Health Soc Behav. 1983;24:2–15. [PubMed] [Google Scholar]
- 29.Lachman ME, Weaver SL. The sense of control as a moderator of social class differences in health and well-being. J Pers Soc Psychol. 1998;74:763–773. doi: 10.1037//0022-3514.74.3.763. [DOI] [PubMed] [Google Scholar]
- 30.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98:310–357. [PubMed] [Google Scholar]
- 31.Cohen S. Psychosocial models of the role of social support in the etiology of physical disease. Health Psychol. 1988;7:269–297. doi: 10.1037//0278-6133.7.3.269. [DOI] [PubMed] [Google Scholar]
- 32.Radloff LS. The CES-D scale: a new self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 33.Horowitz M, Wilner N, Alvarez W. Impact of Events Scale: measure of subjective stress. Psychosom Med. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Sherbourne CD, Stewart AL. The MOS Social Support Survey. Soc Sci Med. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 35.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 36.Short PF, Vasey JJ, Tunceli K. Employment pathways in a large cohort of adult cancer survivors. Cancer. 2005;103:1292–1301. doi: 10.1002/cncr.20912. [DOI] [PubMed] [Google Scholar]
- 37.Bradley CJ, Neumark D, Luo Z, Bednarek H, Schenk M. Employment outcomes of men treated for prostate cancer. J Natl Cancer Inst. 2005;97:958–965. doi: 10.1093/jnci/dji171. [DOI] [PubMed] [Google Scholar]
- 38.Bouknight RR, Bradley CJ, Luo Z. Correlates of return to work for breast cancer survivors. J Clin Oncol. 2006;24:345–353. doi: 10.1200/JCO.2004.00.4929. [DOI] [PubMed] [Google Scholar]
- 39.Taskila-Abrandt T, Martikainen R, Virtanen SV, Pukkala E, Hietanen P, Lindbohm M. The impact of education and occupation on the employment status of cancer survivors. Eur J Cancer. 2004;40:2488–2493. doi: 10.1016/j.ejca.2004.06.031. [DOI] [PubMed] [Google Scholar]
- 40.Drolet M, Maunsell E, Brisson J, Brisson C, Masse B. Not working 3 years after breast cancer: predictors in a population-based study. J Clin Oncol. 2005;23:1–8. doi: 10.1200/JCO.2005.09.500. [DOI] [PubMed] [Google Scholar]
- 41.Ross CE, Wu C. The links between education and health. Am Sociol Rev. 1995;60:719–745. [Google Scholar]
- 42.Ross CE, Van Willigen M. Education and subjective quality of life. J Health Soc Behav. 1997;37:275–297. [PubMed] [Google Scholar]
- 43.Reynolds JR, Ross CE. Social stratification and health: education’s benefit beyond economic status and social origins. Soc Probl. 1998;45:221–247. [Google Scholar]
- 44.Murrell SA, Salsman NL, Meeks S. Educational attainment, positive psychological mediators, and resources for health and vitality in older adults. J Aging Health. 2003;15:591–615. doi: 10.1177/0898264303256198. [DOI] [PubMed] [Google Scholar]
- 45.Wells KJ, Battaglia TA, Dudley DJ, et al. Patient navigation: state of the art or is it science? Cancer. 2008;113:1999–2010. doi: 10.1002/cncr.23815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dohan D, Schrag D. Using navigators to improve care of underserved patients. Cancer. 2005;104:848–855. doi: 10.1002/cncr.21214. [DOI] [PubMed] [Google Scholar]
- 47.Calhoun EA, Whitley EM, Esparza A, et al. A national patient navigator training program. Health Promot Pract. 2008 doi: 10.1177/1524839908323521. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]


