Abstract
Objective:
Sports-related concussion has received increasing attention as a cause of short- and long-term neurologic symptoms among athletes. The King-Devick (K-D) test is based on measurement of the speed of rapid number naming (reading aloud single-digit numbers from 3 test cards), and captures impairment of eye movements, attention, language, and other correlates of suboptimal brain function. We investigated the K-D test as a potential rapid sideline screening for concussion in a cohort of boxers and mixed martial arts fighters.
Methods:
The K-D test was administered prefight and postfight. The Military Acute Concussion Evaluation (MACE) was administered as a more comprehensive but longer test for concussion. Differences in postfight K-D scores and changes in scores from prefight to postfight were compared for athletes with head trauma during the fight vs those without.
Results:
Postfight K-D scores (n = 39 participants) were significantly higher (worse) for those with head trauma during the match (59.1 ± 7.4 vs 41.0 ± 6.7 seconds, p < 0.0001, Wilcoxon rank sum test). Those with loss of consciousness showed the greatest worsening from prefight to postfight. Worse postfight K-D scores (rs = −0.79, p = 0.0001) and greater worsening of scores (rs = 0.90, p < 0.0001) correlated well with postfight MACE scores. Worsening of K-D scores by ≥5 seconds was a distinguishing characteristic noted only among participants with head trauma. High levels of test-retest reliability were observed (intraclass correlation coefficient 0.97 [95% confidence interval 0.90–1.0]).
Conclusions:
The K-D test is an accurate and reliable method for identifying athletes with head trauma, and is a strong candidate rapid sideline screening test for concussion.
Sports-related concussion has received increasing attention in the lay press, but has been a topic of interest in the medical literature for nearly a decade.1–20 The importance of mild closed head injury is underscored by the frequent occurrence of postconcussion syndrome and the potential for devastating long-term symptoms, disability, and pathologic changes resembling those of Alzheimer disease.21–23 Repeated concussion is associated with neuropsychological deficits, electrophysiologic changes, and metabolic abnormalities by brain magnetic resonance spectroscopy (MRS).8,11–35
Since detecting early signs of concussion can improve outcomes,8–20 there is a need for a rapid screening test to assess athletes who may have had a concussion. The King-Devick (K-D) test is based on measurement of the speed of rapid number naming.36 Requiring less than 2 minutes to administer, the K-D test is practical for sideline use and is quicker than the other standard tests of cognition such as Immediate Post-Concussion and Cognitive Testing (ImPACT)37 and the Military Acute Concussion Evaluation (MACE).38 The Standardized Assessment of Concussion (SAC) is a component of the MACE test and is used as a sideline measure of cognitive function, but does not assess eye movements or brainstem function.39 The K-D test captures impairment of eye movements, attention, language, and other areas that correlate with suboptimal brain function.40
We investigated the K-D test as a potential rapid sideline screening for concussion in a cohort of boxers and mixed martial arts (MMA) fighters. We determined if athletes with head trauma and loss of consciousness during matches differed in terms of their postfight K-D time scores or with regard to changes in scores from prefight to postfight. Test-retest reliability was examined, as were correlations between postfight K-D scores and the MACE test.
METHODS
Study participants.
For this cross-sectional study, boxers and MMA fighters were recruited and enrolled prior to sparring sessions and matches conducted in the Boston, MA, area. Boxers were amateurs recruited by their gym manager and invited to participate in 3-round sparring sessions. Standard and routine headgear and sparring-grade boxing gloves were worn. MMA fighters participated during a sanctioned MMA event. Written informed consent was obtained from all participants and principles outlined in the Declaration of Helsinki were followed.
The King-Devick test.
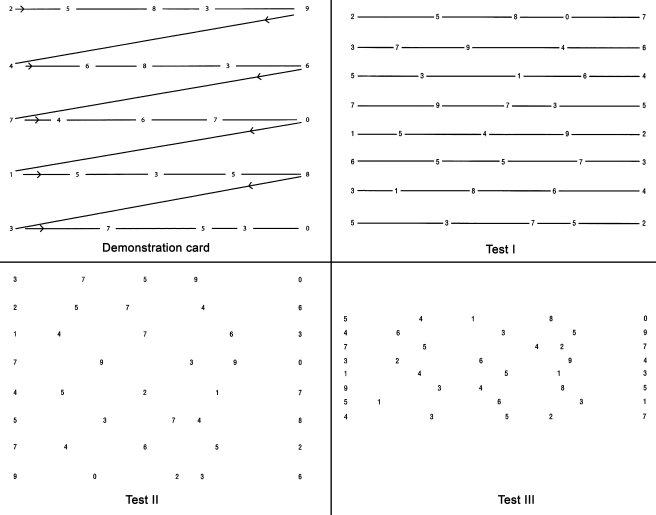
The K-D test is based on measurement of the speed of rapid number naming.36 The test involves reading aloud a series of single-digit numbers from left to right on 3 test cards. Standardized instructions are used, and the test requires less than 2 minutes to administer. The K-D test includes one practice (demonstration) card and 3 test cards, as shown in figure 1. To perform the K-D test, participants were asked to read the numbers on each card from left to right as quickly as possible but without making any errors. The sum of the 3 test card time scores constituted the summary score for the entire test, the K-D time score. Numbers of errors made in reading the test cards were recorded.
Figure 1. Demonstration and test cards for the King-Devick (K-D) Test, a candidate rapid sideline screening for concussion based on measurement of speed of rapid number naming.
To perform the K-D test, participants are asked to read the numbers on each card from left to right as quickly as possible but without making any errors. Following completion of the demonstration card (upper left), subjects are then asked to read each of the 3 test cards in the same manner. The times required to complete each card are recorded in seconds using a stopwatch. The sum of the 3 test card time scores constitutes the summary score for the entire test, the K-D time score. Numbers of errors made in reading the test cards are also recorded; misspeaks on numbers are recorded as errors only if the subject does not immediately correct the mistake before going on to the next number.
Military Acute Concussion Evaluation.
The MACE was used as a more comprehensive test for concussion among the MMA fighters. This test consists of 3 components, including a cognitive history, memory and orientation testing, and a neurologic screening.38 Based on the first 2 components, a total score is given (total possible 30). This test requires 15–20 minutes. A total MACE score less than 25 is considered to represent clinically relevant neurocognitive impairment and require further evaluation for brain injury.38
Testing procedures for boxers.
All boxers were tested at ringside immediately before a 3-round sparring session. Corrections were made for near vision as needed. Boxers were given standardized instructions for the K-D test. For purposes of determining test-retest reliability of precompetition K-D scores, all boxers were tested twice within a 15-minute period before their sparring session by the same examiners.
After the individual 9-minute sparring sessions, each boxer was retested once using the K-D test. Boxers who sustained head trauma during their fight were given the MACE test immediately after the sparring session followed by the K-D test. Among boxers, the MACE test was given only to those with head trauma. Head trauma was defined as overt blows to the head with or without loss of consciousness (LOC); judgments with regard to the occurrence of head trauma or LOC (falling down without movement, or being “out on their feet”) were made by an independent physician with prior ringside experience and expertise in boxing and MMA. This ringside physician was separate from the individuals who performed the K-D testing; the K-D testers were masked to the greatest extent possible to the head trauma/concussion status of each athlete.
Testing procedures for MMA fighters.
Fighters were tested on the day before the MMA event at the time of their weigh-ins. Protocols for K-D testing were the same as those used for the boxers (described above). Postfight testing was delayed by 30 to 60 minutes for 3 fighters due to nonhead injuries. MACE testing in this group was performed for all fighters in the cohort.
Statistical analysis.
Statistical analyses were performed using Stata 11.0 software. Given the common endpoints of head trauma and LOC, and their uniform definitions for both the boxers and MMA fighters, data were analyzed based on the combined study cohort. Differences in postfight K-D time scores and changes in scores from prefight to postfight were compared for participants with head trauma during the fight vs those without using the Wilcoxon rank sum test with exact variances. Among participants with head trauma, those with vs without LOC were compared similarly. Test-retest reliability was estimated for 2 prefight K-D test measurements by the intraclass correlation coefficient (ICC); ICCs were also used to examine agreement between prefight and postfight scores among participants without head trauma. The relation of postfight K-D scores and changes in scores to the MACE were determined using Spearman rank correlations.
RESULTS
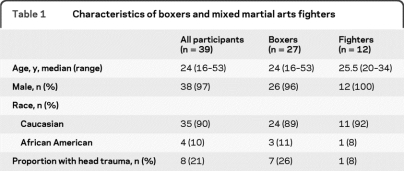
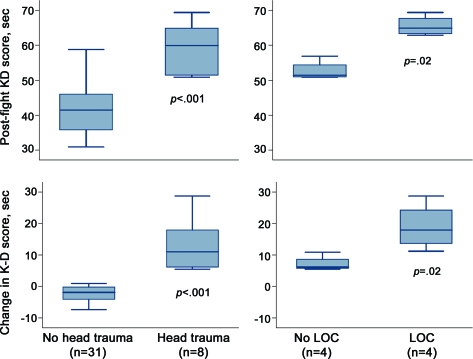
Characteristics and K-D testing data for the study cohort (n = 39) are shown in table 1. With the exception of one participant, all fighters and boxers were men. Prefight K-D scores were similar across groups, with slightly lower mean time scores noted for the second prefight testing session (table 2). ICCs of K-D scores between the 2 prefight testing sessions indicated a high degree of test-retest reliability (ICC 0.97 [95% confidence interval [CI] 0.90–1.0]).
Table 1.
Characteristics of boxers and mixed martial arts fighters
Table 2.
King-Devick (K-D) test and Military Acute Concussion Evaluation (MACE) scores
Abbreviations: CI = confidence interval; ICC = intraclass correlation coefficient.
Comparison of head trauma vs no head trauma groups, Wilcoxon rank sum test.
Comparison of loss of consciousness (LOC) vs no LOC groups, Wilcoxon rank sum test.
p Value from signed-rank test comparing best prefight K-D score to postfight K-D score within study participants.
Minimal but significant learning effects (postfight K-D score lower [better] than prefight score) were noted for participants with no head trauma.
Comparison of head trauma vs no head trauma groups for MACE scores, Wilcoxon rank sum test.
Higher (worse) postfight K-D time scores (rs = 0.79) and greater worsening of scores (rs = 0.90) were associated with lower postfight MACE scores.
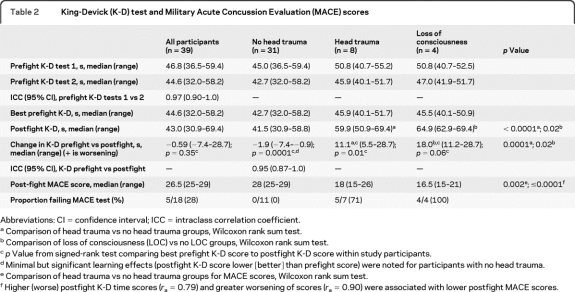
Postfight K-D time scores were significantly higher (worse) for participants who had head trauma during the match (59.1 ± 7.4 vs 41.0 ± 6.7 seconds, p < 0.0001, Wilcoxon rank sum test, table 2). Among those with head trauma, participants with LOC had even higher postfight K-D scores compared to those with no LOC (65.5 ± 2.9 vs 52.7 ± 2.9 seconds, p < 0.0001).
The median change in scores from prefight to postfight for participants who did not have head trauma was a 1.9-second improvement, while the median change for those with head trauma was an 11.1-second worsening (p < 0.001). Participants with LOC also had the greatest worsening of scores from prefight to postfight, with a median increase of 18.0 seconds (p = 0.02 vs no LOC). The numbers of errors were very few, with one participant making 2 errors and another one error on postfight testing. However, both of the participants who made errors were boxers who had head trauma.
Minimal improvement of scores from prefight to postfight was noted for participants with no head trauma (p = 0.0001, signed-rank test comparing prefight vs postfight scores, table 2). This observation likely reflects learning effects for the K-D test. Participants who did not have head trauma during their match (n = 31) also showed high degrees of test-retest reliability between the best prefight and postfight K-D scores, with ICC values of 0.95 (95% CI 0.87–1.0, table 2).
Among participants who were given the MACE test postfight, 5 of 7 (71%) with overt head trauma failed, while none of those without head trauma failed the MACE. Worse postfight K-D scores (rs = −0.79, p = 0.0001) and greater worsening of scores (rs = 0.90, p < 0.0001) correlated well with postfight MACE scores.
The postfight K-D score distributions showed some overlap between the groups with and without head trauma (figure 2). However, there was no overlap in the distribution of changes in scores from prefight to postfight, with a substantial gap between the worst change in the no head trauma group and the best change in the head trauma group. As demonstrated in table 1, the lower limit of the range of worsening of K-D time scores for participants with head trauma was 5.5 seconds. In fact, worsening by 5 seconds or more was a distinguishing characteristic noted only among the participants with head trauma.
Figure 2. Box plots show the distributions of postfight King-Devick (K-D) time scores and changes in scores from prefight to postfight in participants with vs without head trauma or loss of consciousness (LOC).
The lines in the box represent the medians, and boxes delineate the interquartile range (25th–75th percentiles). Whiskers represent the range of observations minus outliers (no outlier values in this sample). p Values are based on Wilcoxon rank sum test with exact variances comparing groups with head trauma vs no head trauma and LOC vs no LOC.
DISCUSSION
Results of this study demonstrate that the K-D test is an accurate and reliable method for identifying athletes with head trauma, and is a strong candidate as a rapid sideline screening test for concussion. High degrees of test-retest reliability were noted for the K-D test in this study. Postfight time scores in this cohort of boxers and MMA fighters were greater (worse) postfight for participants who had head trauma during their match. Changes in scores from prefight to postfight also reflected this pattern and showed more separation between those with and without head trauma than the postfight scores alone. Worsening by 5 seconds or more was a distinguishing characteristic noted only among the participants with head trauma, suggesting that this threshold may be a useful cutoff for exploration in future studies as a criterion for having an athlete stop play pending medical evaluation for concussion.
Closed head injury, even in mild form, is a leading cause of both short-term and long-term cognitive impairment among athletes, particularly for those in contact sports such as football, boxing, soccer, rugby, and hockey.7–30 The annual incidence of sports-related concussion in the United States is 1.6 to 3.8 million, and the likelihood of an athlete in a contact sport experiencing a concussion is as high as 20% per season.21 While the majority of athletes who experience a concussion are expected to recover, the danger is greatly increased by a second concussion.31–33 Having a second concussion before recovering from an initial one can be associated with metabolic brain abnormalities as documented by MRS, electrophysiologic changes, and neuropsychological deficits.21,31–35
In cases of repetitive concussion among boxers, at least 17% develop chronic traumatic encephalopathy (CTE), a condition characterized by long-term cognitive and neurobehavioral difficulties.21,24,26 Symptoms of CTE include chronic headaches, fatigue, sleep difficulties, personality changes, sensitivities to light and noise, dizziness, and short-term memory deficits.7–20 This constellation of symptoms can be disabling for an athlete and can have lifelong implications.9,10,31
The recognition and management of concussion in athletes can be difficult for a number of reasons.21,18–20 1) Athletes who have experienced a concussion present with a wide variety of symptoms.15,17–20 Although the classic symptoms of loss of consciousness, confusion, and memory loss may be present in some athletes with mild concussion, there may or may not be obvious signs that a concussion has occurred. Symptoms of mild concussion are typically quite subtle and may go unnoticed or overlooked by the athlete, team medical staff, or coaches.13,18–20 2) Current management guidelines are not evidence-based and little to no scientific data support the multiple arbitrary systems that are in place to manage concussion.18–20 3) Traditional neurologic and radiologic procedures, such as CT scans, MRI scans, and EEG, although helpful in identifying more serious consequences of head trauma (e.g., skull fracture, hematoma, contusion, seizure), are not useful in identifying many of the effects of concussion.25 Such tests are typically nonspecific or normal, even in athletes sustaining a severe concussion. Thus, while structural neuroimaging techniques are insensitive to the effects of concussion, more advanced fMRI techniques have been able to document damage and to examine the window of metabolic brain vulnerability during which a second concussion could be even more dangerous.7,31–33 4) Most importantly, athletes may not understand the potential consequences of concussion and often minimize or deny symptoms so that they can return to play.13–20 Such underreporting of symptoms is a common practice at all levels of sport participation.
The K-D test is based on measurement of the speed of rapid number naming.36 As such, the K-D test can capture impairment of eye movements, attention, language, and other areas that correlate with suboptimal brain function.21,40 Saccadic and other types of eye movements are frequently abnormal following concussion, and early eye movement function may serve as a predictor of postconcussion syndrome.40 In a recent investigation of 36 patients with postconcussion syndrome vs 36 controls with good recovery following mild closed head injury of similar severity (140–163 days posttrauma),40 patients with postconcussion syndrome had significantly higher numbers of directional errors on antisaccade tasks (p = 0.006) and memory-guided sequences (p = 0.002). To the extent that the K-D test captures saccadic eye movements among other important elements of rapid number naming, these data suggest that this quick screening test will be helpful in identifying athletes with signs of concussion. Impaired eye movement function, particularly for those reflecting subcortical pathways, correlated well with severity of postconcussive symptoms and with limitation of activities of daily living. In another study, early eye movement function at 1 week was shown to predict development of postconcussion syndrome.40 Collectively, data on eye movement testing demonstrate a high degree of sensitivity and predictive value as an outcome measure for concussion.40
While the manifestations of postconcussion syndrome are best captured by extensive testing batteries such as ImPACT,37 and may be influenced by intellectual ability or depression, tests of rapid number naming such as K-D represent an objective measure. Because the K-D test captures many aspects of function, including subcortical (subconscious) pathways that extend beyond eye movements, this test may help coaches and trainers with game decisions regarding removal of a player who may have been concussed.
Since our study cohort consisted of boxers and MMA fighters, head trauma that occurred was observable and overt. In other sports such as football, closed head injury and concussion could occur in the context of plays involving many individuals, and head trauma may not be as readily detected. Worsening of K-D scores in this setting might be helpful for determining if a meaningful head blow has taken place.
Another important aspect of evaluating a potential screening test is the correlation of scores with an established battery of tests that measure the construct under study. Ongoing large-scale longitudinal studies of collegiate athletes are examining the relation of K-D test scores and changes in scores over the course of a season with ImPACT and other formal cognitive testing.37,38 In the present study, failing the MACE test (score <25 out of maximum 30 points)38 was associated with worse postfight K-D scores and with greater worsening of K-D scores from prefight to postfight, accounting for age and best prefight K-D scores. While the MACE in our cohort was administered only to participants with head trauma among the boxers, all MMA fighters took the MACE test and none of those without head trauma during their match failed the MACE. Correlations between postfight MACE scores as a continuous variable and K-D scores were also strong, thus providing preliminary evidence that K-D test scores reflect more global aspects of cognitive function in the setting of acute mild closed head injury and concussion.
In order for the K-D test to be used effectively over time and to be administered by different testers, such as athletic trainers, the interrater and test-retest reliability of this measure must be assessed. Results of our study show that K-D test time scores have a high degree of test-retest reliability, with ICCs of 0.97 (95% CI 0.90–1.0) for the 2 prefight measurements. These values indicate that a very high proportion of the variability in the dataset (97%) is due to between-participant differences rather than differences between testing sessions for the same participant. Reliability for K-D measurements prefight vs postfight was also excellent among participants who did not have head trauma during their match (ICC 0.95 [95% CI 0.87–1.0]). This finding suggests that K-D measurements are stable over the short term in the absence of intervening concussion.
The relatively uncommon occurrence of head trauma in our boxing cohort must be viewed in context of the fact that sparring sessions, rather than actual boxing matches, were assessed in this study. Boxers are at high risk for concussion and for more long-term manifestations of CTE, formerly termed dementia pugilistica.21,24–26 Nonetheless, our data indicate that head trauma events can be effectively identified by K-D test time scores, and that analyses of this new measure in future studies can establish its role as a rapid sideline screening test for concussion.
The K-D test, based on measurement of the speed of rapid number naming, can capture impairment of eye movements, attention, language, and other areas that correlate with suboptimal brain function. Data from this investigation demonstrate that the K-D test is an accurate and reliable method for identifying athletes with head trauma. The K-D test represents a strong candidate rapid sideline screening test for concussion, and has particular relevance to contact sports including football, soccer, hockey, MMA, and boxing. Prospective studies of collegiate athletes that are ongoing at the University of Pennsylvania will establish large-scale K-D test norms and expected ranges of precompetition scores for this age group, and will further investigate the capacity for K-D scores to capture closed head injury and concussion.
Editorial, page 1450
- CI
- confidence interval
- CTE
- chronic traumatic encephalopathy
- ICC
- intraclass correlation coefficient
- K-D
- King-Devick
- ImPACT
- Immediate Post-Concussion and Cognitive Testing
- LOC
- loss of consciousness
- MACE
- Military Acute Concussion Evaluation
- MMA
- mixed martial arts
- MRS
- magnetic resonance spectroscopy
- SAC
- Standardized Assessment of Concussion.
AUTHOR CONTRIBUTIONS
Statistical analysis was conducted by Dr. Balcer and Dr. Maguire.
DISCLOSURE
K.M. Galetta, J. Barrett, Dr. Allen, Dr. Madda, Dr. Delicato, Dr. Tennant, and Dr. Branas report no disclosures. Dr. Maguire serves on the editorial boards of Ophthalmology, Cornea, and Current Opinion in Ophthalmology; and receives research support from Inspire Pharmaceuticals, Pfizer Inc., and the NIH/NEI. Dr. Messner reports no disclosures. Dr. Devick is an employee of and holds stock in King-Devick Test, LLC; and has a patent pending re: The King-Devick Test. Dr. Galetta serves on the editorial boards of Neurology® and the Journal of Neuro-ophthalmology; has received speaker honoraria from Biogen Idec and Teva Pharmaceutical Industries Ltd.; has served as a consultant for Biogen Idec, Medtronic, Inc., and Teva Pharmaceutical Industries Ltd.: and serves on the speakers' bureau for Biogen Idec. Dr. Balcer serves on a scientific advisory board for Biogen Idec; has received speaker honoraria from Biogen Idec and Bayer Schering Pharma; and receives research support from the NIH/NEI and the National MS Society.
REFERENCES
- 1. Gregory S, Bissinger B. The most dangerous game: how to fix football; the crisis in schools. Time 2010;175:36–4520191758 [Google Scholar]
- 2. Hine C. Going to the max protect: IHSA has new concussion rule, but some critics demand more. Chicago Tribune 2010. August 26
- 3. Ortiz J. Injury that is coming to a head. USA Today 2010. August 27 [Google Scholar]
- 4. Dooren JC. Researchers see rise in children's sports-related concussions. Wall Street Journal 2010. August 30 [Google Scholar]
- 5. Miller G. A late hit for pro football players. Science 2009;325:670–672 [DOI] [PubMed] [Google Scholar]
- 6. Samson K. School sport concussions draw national attention as more states draft return-to-play laws. Neurology Today 2010;10:1–12 [Google Scholar]
- 7. Vastag B. Football brain injuries draw increased scrutiny. JAMA 2002;287:437–442 [DOI] [PubMed] [Google Scholar]
- 8. McCrea M, Guskiewicz KM, Marshall SW, et al. Acute effects and recovery time following concussion in collegiate football players. JAMA 2003;290:2556–2563 [DOI] [PubMed] [Google Scholar]
- 9. Guskiewicz KM, Marchall SW, Bailes J, et al. Association between recurrent concussion and late-life cognitive impairment in retired professional football players. Neurosurgery 2005;57:719–726 [DOI] [PubMed] [Google Scholar]
- 10. Cantu RC. Chronic traumatic encephalopathy in the National Football League. Neurosurgery 2007;61:223–225 [DOI] [PubMed] [Google Scholar]
- 11. Cantu RC. Athletic concussion: current understanding as of 2007. Neurosurgery 2007;60:963–964 [DOI] [PubMed] [Google Scholar]
- 12. Cantu RC, Herring SA, Putukian M. Concussion. N Engl J Med 2007;356:1787–1789 Letter. [DOI] [PubMed] [Google Scholar]
- 13. Mayers L. Return-to-play criteria after athletic concussion: a need for revision. Arch Neurol 2008;65:1158–1161 [DOI] [PubMed] [Google Scholar]
- 14. Casson IR, Pellman EJ, Viano DC. National Football League experiences with return to play after concussion. Arch Neurol 2009;66:419–420 [DOI] [PubMed] [Google Scholar]
- 15. Lovell M. The management of sports-related concussion: current status and future trends. Clin Sports Med 2009;28:95–111 [DOI] [PubMed] [Google Scholar]
- 16. Casson IR, Pellman EJ, Viano DC. Concussion in the National Football League: an overview for neurologists. Phys Med Rehabil Clin N Am 2009;20:195–214 [DOI] [PubMed] [Google Scholar]
- 17. Hunt T, Asplund C. Concussion assessment and management. Clin Sports Med 2010;29:5–17 [DOI] [PubMed] [Google Scholar]
- 18. McCrory P, Meeuwisee W, Johnston K, et al. Consensus statement on concussion in sport: the 3rd International Conference on Concussion in Sport held in Zurich, November 2008. Br J Sports Med 2009;43(suppl 1):i76–i84 [DOI] [PubMed] [Google Scholar]
- 19. Cantu RC. When to disqualify an athlete after a concussion. Curr Sports Med Rep 2009;8:6–7 [DOI] [PubMed] [Google Scholar]
- 20. Reddy CC, Collins MW. Sports concussion: management and predictors of outcome. Curr Sports Med Rep 2009;8:10–15 [DOI] [PubMed] [Google Scholar]
- 21. McKee AC, Cantu RC, Nowinski CJ, et al. Chronic traumatic encephalopathy in athletes: progressive tauopathy after repetitive head injury. J Neuropathol Exp Neurol 2009;68:709–735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Omalu BI, Hamilton RL, Kamboh I, DeKosky ST, Bailes J. Chronic traumatic encephalopathy (CTE) in a National Football League player: case report and emerging medicolegal practice questions. J Forensic Nurs 2009;6:40–46 [DOI] [PubMed] [Google Scholar]
- 23. Gavett B, Stern R, Cantu R, Nowinski C, McKee A. Mild traumatic brain injury: a risk factor for neurodegeneration. Alzheimers Res Ther 2010;2:18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zazryn R, McCrory PR, Cameron PA. Injury rates and risk factors in competitive professional boxing. Clin J Sports Med 2009;19:20–25 [DOI] [PubMed] [Google Scholar]
- 25. Orrison WW, Hanson EH, Alamo T, et al. Traumatic brain injury: a review and high-field MRI findings in 100 unarmed combatants using a literature-based checklist approach. J Neurotrauma 2009;26:689–701 [DOI] [PubMed] [Google Scholar]
- 26. Roberts GW, Allsop D, Bruton C. The occult aftermath of boxing. J Neurol Neurosurg Psychiatry 1990;53:373–378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Matser JT, Kessels AG, Jordan BD, Lezak MD, Troost J. Chronic traumatic brain injury in professional soccer players. Neurology 1998;51:791–796 [DOI] [PubMed] [Google Scholar]
- 28. Matser EJT, Kessels AG, Lezak MD, Jordan BD, Troost J. Neuropsychological impairment in amateur soccer players. JAMA 1999;282:971–973 [DOI] [PubMed] [Google Scholar]
- 29. Wennberg RA, Tator CH. Concussion incidence and time lost from play in the NHL during the past ten years. Can J Neurol Sci 2008;35:647–651 [DOI] [PubMed] [Google Scholar]
- 30. Emery CA, King J, Shrier I, et al. Risk of injury associated with body checking among youth ice hockey players. JAMA 2010;303:2265–2272 [DOI] [PubMed] [Google Scholar]
- 31. Covassin T, Elbin R, Kontos A, Larson E. Investigating baseline neurocognitive performance between male and female athletes with a history of multiple concussion. J Neurol Neurosurg Psychiatry 2010;81:597–601 [DOI] [PubMed] [Google Scholar]
- 32. Theriault M, De Beaumont L, Gosselin N, Filipinni M, Lassonde M. Electrophysiological abnormalities in well functioning multiple concussed patients. Brain Inj 2009;23:899–906 [DOI] [PubMed] [Google Scholar]
- 33. Vagnozzi R, Signoretti S, Cristofori L, et al. Assessment of metabolic brain damage and recovery following mild traumatic brain injury: a multicentre, proton magnetic resonance spectroscopic study in concussed patients. Brain Epub 2010 Aug 23 [DOI] [PubMed] [Google Scholar]
- 34. Vagnozzi R, Signoretti S, Tavazzi B, et al. Temporal window of metabolic brain vulnerability to concussion: a pilot 1H-magnetic resonance spectroscopic study in concussed patients: part III. Neurosurgery 2008;62:1286–1296 [DOI] [PubMed] [Google Scholar]
- 35. Henry LC, Tremblay S, Boulanger Y, Ellemberg D, Lassonde M. Neurometabolic changes in the acute phase after sports concussions correlate with symptom severity. J Neurotrauma 2010;27:65–76 [DOI] [PubMed] [Google Scholar]
- 36. Oride MK, Marutani JK, Rouse MW, DeLand PN. Reliability study of the Pierce and King-Devick saccade tests. Am J Optom Physiol Optics 1986;63:419–424 [DOI] [PubMed] [Google Scholar]
- 37. Schatz P. Long term test-retest reliability of baseline cognitive assessments using ImPACT. Am J Sports Med 2010;38:47–53 [DOI] [PubMed] [Google Scholar]
- 38. Coldren RL, Kelly MP, Parrish RV, Dretsch M, Russell ML. Evaluation of the Military Acute Concussion Evaluation for use in combat operations more than 12 hours after injury. Mil Med 2010;175:477–481 [DOI] [PubMed] [Google Scholar]
- 39. Barr WB, McCrea M. Sensitivity and specificity of standardized neurocognitive testing immediately following sports concussion. J Int Neuropsychol Soc 2001;7:693–702 [DOI] [PubMed] [Google Scholar]
- 40. Heitger MH, Jones RD, Macleod AD, Snell DL, Frampton CM, Anderson TJ. Impaired eye movements in post-concussion syndrome indicate suboptimal brain function beyond the influence of depression, malingering or intellectual ability. Brain 2009;132:2850–2870 [DOI] [PubMed] [Google Scholar]