Abstract
Summary
Background and objectives
The increasing number of podocyte-expressed genes implicated in steroid-resistant nephrotic syndrome (SRNS), the phenotypic variability, and the uncharacterized relative frequency of mutations in these genes in pediatric and adult patients with SRNS complicate their routine genetic analysis. Our aim was to compile the clinical and genetic data of eight podocyte genes analyzed in 110 cases (125 patients) with SRNS (ranging from congenital to adult onset) to provide a genetic testing approach.
Design, setting, participants, & measurements
Mutation analysis was performed by sequencing the NPHS1, NPHS2, TRPC6, CD2AP, PLCE1, INF2, WT1 (exons 8 and 9), and ACTN4 (exons 1 to 10) genes.
Results
We identified causing mutations in 34% (37/110) of SRNS patients, representing 67% (16/24) familial and 25% (21/86) sporadic cases. Mutations were detected in 100% of congenital-onset, 57% of infantile-onset, 24 and 36% of early and late childhood-onset, 25% of adolescent-onset, and 14% of adult-onset patients. The most frequently mutated gene was NPHS1 in congenital onset and NPHS2 in the other groups. A partial remission was observed in 7 of 26 mutation carriers treated with immunosuppressive agents and/or angiotensin-converting enzyme inhibitors. Patients with NPHS1 mutations showed a faster progression to ESRD than patients with NPHS2 mutations. None of these mutation carriers relapsed after kidney transplantation.
Conclusions
We propose a genetic testing algorithm for SRNS based on the age at onset and the familial/sporadic status. Mutation analysis of specific podocyte-genes has a clinical value in all age groups, especially in children.
Introduction
Nephrotic syndrome (NS) is characterized by proteinuria, hypoalbuminemia, edema, and dyslipidemia. Approximately 10% of children and 40% of adults with idiopathic NS are steroid resistant (SRNS) and progress to ESRD (1–5). In these cases, renal histology typically shows focal segmental glomerulosclerosis (FSGS). The remaining patients are steroid responsive, with a favorable long-term prognosis (6). Mutations in several single genes expressed by glomerular podocytes have been identified in patients with SRNS (7).
The phenotypic spectrum caused by mutations in these genes is wider than initially expected. NPHS1, encoding for nephrin, was identified as the causative gene in the most common type of congenital NS (CNS), CNS of the Finnish-type (CNF) (8). Recently, NPHS1 mutations have also been reported in childhood- (9) and adult-onset SRNS (10). NPHS2, encoding for podocin, was identified as the causative gene in early-onset autosomal-recessive (AR) SRNS (11). Nevertheless, NPHS2 mutations have also been found in CNS (12–15) and in a few cases of adult-onset FSGS (16–18). Mutations of phospholipase C-ε (PLCE1) have been identified in 10 to 50% of patients with NS and diffuse mesangial sclerosis (DMS) and in 12% of familial AR FSGS (19–22).Mutations in exons 8 and 9 of the Wilms tumor suppressor gene (WT1) were discovered in patients with syndromic SRNS (23,24) but can also cause isolated SRNS (25,26). Mutations in LAMB2, encoding for lamini-β2 and implicated in Pierson syndrome (27), have been found in one family with CNS (28). Finally, mutations in TRPC6 (encoding for transient receptor potential channel 6) (29,30), ACTN4 (α-actinin-4) (31), CD2AP (CD2-associated protein) (32), and lately INF2 (33) were detected in several families with autosomal-dominant (AD) FSGS and adult-onset NS. However, some studies have reported mutations in these genes in a small number of patients with childhood-onset FSGS (34–40).
The genetic heterogeneity of SRNS, the significant phenotypic variability, and the lack of knowledge of the relative frequency of mutations in these genes in pediatric and adult patients with NS hinder the routine genetic analysis for SRNS. In fact, there are only a few studies searching for mutations in several of these genes and only in pediatric patients (14–43). The aim of this study was to compile the clinical and genetic data of eight podocyte genes analyzed in our Spanish cohort of patients with NS (ranging from congenital to adult onset) to propose an adequate genetic testing approach.
Materials and Methods
Patients
From a cohort of 204 Spanish patients with primary NS, we excluded patients who responded to steroid or immunosuppressive treatment and those developing steroid resistance at a later stage of the disease or with recurrence after kidney transplant, because we considered that an immune pathogenesis was the most likely cause of the disease in these cases. Thus, 125 patients belonging to 110 families with CNS or primary FSGS/DMS or/and SRNS were included. Diagnosis of NS and, when applicable, response to steroid treatment was determined following published criteria (1). A partial response was defined as the disappearance of edema, an increase in the serum albumin concentration, and the persistence of proteinuria below nephrotic range. Prematurely born patients presenting with a large placenta and severe proteinuria at birth or with proven renal biopsy were considered as CNF (n = 10). Twenty-eight patients belonging to 18 families were classified as AR SRNS, defined as families with either two or more affected children (n = 11) or one affected individual in consanguineous families (n = 7). Ten patients belonging to six families showed evidence of AD disease because multiple generations were affected. The remaining 86 patients were considered sporadic cases. The age at onset of NS, response to treatment, histology, and clinical course from first presentation to last clinical examination are listed in Table 1. We will refer to patients studied when assessing clinical data and to families studied when assessing genetic data, because siblings may follow a different clinical course but should bear the same mutations.
Table 1.
Clinical data according to mutation status for 125 patients from 110 families with NS
| Age at Onset of NS (Mean ± SD [years], Median, Range [years]) | Response to CR (No. of Patients with NR/NG/NA) | Response to IS with/without ACEI (No. of Patients with NR/PR/NG/NA) | Histology (No. of Patients with CNF/DMS/MCNS/FSGS/NP) | ESRD (No. of patients [%]) | Age at ESRD (Mean ± SD [years], Median, Range [years]) | Progression Time to ESRD (Mean ± SD [years], Median, Range [years]) | Kidney Transplant (No. of patients [%]) | |
|---|---|---|---|---|---|---|---|---|
| Total | 17.5 ± 16.5; n = 125 | 78/32/15 | 50/7/36/32 | 3/3/2/108/9 | 69 (55) | 27.3 ± 19.1; n = 69 | 5.3 ± 5.5; n = 69 | 53 (76) |
| 14.0 (0.0 to 56.0) | 24.0 (0.2 to 61.0) | 3.0 (0.0 to 26.0) | ||||||
| Congenital onset | 0.1 ± 0.1; n = 15 | 4/11/0 | 1/0/13/1 | 3/3/0/2/7 | 7 (47) | 1.4 ± 1.2; n = 7 | 1.4 ± 1.2; n = 7 | 5 (71) |
| (0 to 3 months) | 0.1 (0.0 to 0.2) | 1.0 (0.2 to 4.0) | 1.0 (0.2 to 3.9) | |||||
| Infantile onset | 0.8 ± 0.2; n = 8 | 7/0/1 | 4/2/0/2 | 0/0/0/7/1 | 5 (63) | 5.6 ± 0.9; n = 5 | 4.8 ± 0.9; n = 5 | 3 (60) |
| (4 to 12 months) | 0.8 (0.3 to 1.0) | 5.0 (5.0 to 7.0) | 4.3 (4.2 to 6.4) | |||||
| Early childhood onset | 3.4 ± 1.3; n = 24 | 22/1/1 | 15/1/1/7 | 0/0/1/22/1 | 9 (37) | 8.3 ± 5.2; n = 9 | 4.5 ± 5.0; n = 9 | 9 (100) |
| (13 months to 5 years) | 3.3 (1.2 to 5.7) | 6.5 (3.0 to 17.0) | 1.9 (1.0 to 13.0) | |||||
| Late childhood onset | 8.1 ± 1.9; n = 13 | 13/0/0 | 12/1/0/0 | 0/0/0/13/0 | 4 (31) | 10.0 ± 3.4; n = 4 | 2.3 ± 1.9; n = 4 | 2 (50) |
| (6 to 12 years) | 7.5 (6.0 to 12.0) | 8.5 (8.0 to 15.0) | 1.5 (1.0 to 5.0) | |||||
| Adolescent onset | 15.6 ± 1.3; n = 9 | 6/2/1 | 5/0/2/2 | 0/0/0/9/0 | 7 (78) | 22.7 ± 4.4; n = 7 | 7.1 ± 4.9; n = 7 | 6 (86) |
| (13 to 17 years) | 16.0 (13.0 to 17.0) | 24.0 (17.0 to 29.0) | 8.0 (2.0 to 13.0) | |||||
| Adult onset | 33.9 ± 10.6; n = 56 | 26/18/12 | 12/4/20/20 | 0/0/1/55/0 | 37 (66) | 41.1 ± 13.0; n = 37 | 6.4 ± 6.4; n = 37 | 26 (70) |
| (>18 years) | 33.0 (18.0 to 56.0) | 40.0 (21.0 to 61.0) | 3.5 (0.0 to 26.0) | |||||
| Patients with 2 NPHS1 mutations | 2.6 ± 6.8; n = 16 | 5/10/1 | 3/1/12/0 | 3/1/0/6/6 | 6 (35) | 1.5 ± 1.3; n = 6 | 1.5 ± 1.3; n = 6 | 4 (67) |
| 0.1 (0.0 to 27.0) | 1.0 (0.2 to 4.0) | 1.0 (0.2 to 3.9) | ||||||
| two severe mutations | 0.1 ± 0.1; n = 12 | 2/10/0 | 0/0/12/0 | 3/1/0/2/6 | 6 (50) | 1.5 ± 1.3; n = 6 | 1.5 ± 1.3; n = 6 | 4 (67) |
| 0.0 (0.0 to 0.1) | 1.0 (0.2 to 4.0) | 1.0 (0.2 to 3.9) | ||||||
| at least one mild mutation | 10.3 ± 11.5; n = 4 | 3/0/1 | 3/1/0/0 | 0/0/0/4/0 | 0 (0) | – | – | – |
| 6.5 (1.0 to 27.0) | ||||||||
| Patients with 2 NPHS2 mutations | 11.8 ± 11.6; n = 19 | 19/0/0 | 13/3/0/3 | 0/0/1/16/2 | 13 (68) | 19.9 ± 14.5, n = 13 | 6.5 ± 3.8, n = 13 | 10 (77) |
| 8.0 (0.02 to 39.0) | 15.0 (5.0 to 50.0) | 5.0 (1.0 to 13.0) | ||||||
| two pathogenic mutations | 2.8 ± 2.6; n = 10 | 10/0/0 | 6/2/0/2 | 0/0/1/7/2 | 6 (60) | 7.6 ± 2.5, n = 6 | 4.2 ± 2.7, n = 6 | 4 (67) |
| 2.3 (0.02 to 8.0) | 7.0 (5.0 to 12.0) | 3.7 (1.0 to 8.0) | ||||||
| one pathogenic mutation + p.R229Q | 21.8 ± 9.1; n = 9 | 9/0/0 | 7/1/0/1 | 0/0/0/9/0 | 7 (78) | 30.4 ± 11.8, n = 71 | 8.4 ± 3.7, n = 7 | 6 (86) |
| 19.0 (10 0.0– 39.0) | 26.0 (15.0 to 50.0) | 9.0 (4.0 to 13.0) | ||||||
| Patients with WT1 mutations | 1.3 ± 1.2; n = 5 | 3/2/0 | 3/2/0/0 | 0/2/0/3/0 | 2 (40) | 0.3 ± 0.2, n = 2 | 0.2 ± 0.2, n = 2 | 1 (50) |
| 1.0 (0.2 to 2.8) | 3.0 (1.0 to 5.0) | 2.4 (0.7 to 4.0) | ||||||
| Patients with TRPC6 mutations | 24.4 ± 16.9; n = 4 | 3/1/0 | 0/1/1/2 | 0/0/0/3/1 | 1 (25) | 39.0, n = 1 | 14.0, n = 1 | 1 (100) |
| 25.0 (7.2 to 41.0) | ||||||||
| Patients with INF2 mutations | 32.0 ± 16.6; n = 5 | 0/5/0 | 0/0/5/0 | 0/0/0/5/1 | 4 (80) | 36.5 ± 17.3, n = 4 | 4.5 ± 4.0, n = 4 | 4 (100) |
| 31.0 (16.0 to 50.0) | 33.5 (21.0 to 58.0) | 4.5 (1.0 to 8.0) |
CR, corticoids; IS, immunosuppressants; MCNS, minimal change nephrotic syndrome; NA, not available; NG, not given; NP, not performed; NR, no response; PR, partial response.
Mutation Analysis
Genomic DNA was isolated from peripheral blood cells using the salting-out method (44) after obtaining informed consent from affected individuals or their parents. The study was approved by the institutional review boards of each participating hospital. Mutation analysis was performed by direct sequencing of all 29 exons of NPHS1, all 8 exons of NPHS2, all 13 exons of TRPC6, all 34 exons of PLCE1, all 22 exons of INF2, exons 1 to 10 of ACTN4, and exons 8 and 9 of WT1. We only tested exons 8 and 9 of WT1 and exons 1 to 10 of ACTN4 because mutations in these genes have only been reported in these exons (26,37). Exons were amplified by PCR using intron-flanking primers, as described previously (11,19,25,29–31,33,45–47). Primer data are available on request. In addition, total RNA was extracted from peripheral blood cells with TRIzol (Invitrogen, Carlsbad, CA). Total RNA (1 μg) was reverse transcribed with the High-Capacity cDNA Archive Kit (Applied Biosystems, Foster City, CA) using random hexamers. The entire CD2AP cDNA was amplified in three overlapping fragments with primers designed with Primer Express software (Applied Biosystems). All RT-PCR products and exons were sequenced using the Big Dye DNA Sequencing kit v1.1 (Applied Biosystems) and an ABI PRISM 3100-Avant genetic analyzer (Applied Biosystems).
Sequencing of both strands was performed for all sequence variants detected. Segregation of these changes with disease was assessed from all available family members. Unpublished missense mutations were screened in ≥200 unrelated controls of matched ethnic origin either by direct sequencing or by restriction enzyme digestion.
We first analyzed the NPHS2 gene in the entire group of patients. Afterward, we examined WT1 in those cases without clear causative mutations. The NPHS1 gene was studied in those cases without WT1 mutations. Then, patients without pathogenic mutations in the previous genes were subsequent analyzed for the ACTN4, CD2AP, and TRPC6 genes. Finally, we analyzed PLCE1 only for the familial AR cases and INF2 for the AD ones. We did not evaluate the LAMB2 gene because all our patients with DMS were explained by causative mutations in other genes. Partial data of TRPC6, NPHS1, and NPHS2 mutation analysis have been previously published (10,34,48).
Classification of Amino Acid Substitutions
To evaluate the pathogenicity of amino acid substitutions, we developed an in silico scoring system (10,34,48), as described previously for other genes (49–51). We classified patients with two NPHS1 mutations as (1) patients with two severe mutations and (2) patients with at least one mild mutation, as suggested elsewhere (9,10). In addition, we classified patients with two NPHS2 mutations as (1) patients with two pathogenic mutations and (2) patients with one pathogenic mutation plus the p.R229Q variant, as previously reported (52,53). Additional information about the classification of amino acid substitutions is provided in Supplementary Table 1.
Statistical Analyses
Data are expressed as mean ± SD or median and range. Comparisons between continuous values were made using the Mann–Whitney U test (SPSS Software), and P < 0.05 was considered significant.
Results
Podocyte Gene Mutation Frequencies
Mutation analysis of NPHS1, NPHS2, WT1, TRPC6, CD2AP, ACTN4, PLCE1 (only for AR familial FSGS), and INF2 (only for AD familial FSGS) showed disease-causing mutations in 34% (37 of 110) of all SRNS cases (Table 2). Recessive pathogenic mutations in NPHS1 were found in 13.5% (15 of 110) of cases. Mutations in NPHS2 were detected in 12% (13 of 110) of patients. Dominant mutations in WT1 and TRPC6 were found in 4.5 and 3% of cases, respectively. No pathogenic mutations in ACTN4 and CD2AP genes were identified in our cohort of patients. Three cases were carriers of a single NPHS1 (n = 1) or NPHS2 (n = 2) pathogenic mutation, which cannot be considered causative by itself. In AR FSGS families, no PLCE1 mutation was found, whereas one INF2 mutation was identified in one AD family (one of six).
Table 2.
Frequency of pathogenic mutations in NPHS1, NPHS2, WT1, TRPC6, INF2, ACTN4, and CD2AP in 110 unrelated cases with SRNS
| Pathogenic Mutations | Total | Congenital Onset (0 to 3 months) | Infantile Onset (4 to 12 months) | Early Childhood Onset (13 months to 5 years) | Late Childhood Onset (6 to 12 years) | Adolescent Onset (13 to 18 years) | Adult Onset (>18 years) | Familial SRNS | Sporadic SRNS |
|---|---|---|---|---|---|---|---|---|---|
| No. of patients (cases) | 125 (110) | 15 (15) | 8 (7) | 24 (21) | 13 (11) | 9 (8) | 56 (48) | 35 (24) | 90 (86) |
| NPHS1, No. of cases (%) | 15 (13.5) | 12 (80) | 1 (14) | 0 (0) | 1 (9) | 0 (0) | 1 (2) | 6 (25) | 9 (11) |
| NPHS2, No. of cases (%) | 13 (12) | 1 (7) | 2 (29) | 3 (14) | 2 (18) | 1 (12.5) | 4 (8) | 8 (34) | 5 (6) |
| WT1, No. of cases (%) | 5 (4.5) | 2 (13) | 1 (14) | 2 (10) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 5 (6) |
| TRPC6, No. of cases (%) | 3 (3) | 0 (0) | 0 (0) | 0 (0) | 1 (9) | 0 (0) | 2 (4) | 1 (4) | 2 (2) |
| ACTN4, No. of cases (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| CD2AP, No. of cases (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| PLCE1 No. of cases (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | ND | ND | ND | 0 (0) | ND |
| INF2 No. of cases (%) | 1 (1) | ND | ND | ND | ND | 1 (12.5) | 0 (0) | 1 (4) | ND |
| No. of cases with mutations (%) | 37 (34) | 15 (100) | 4 (57) | 5 (24) | 4 (36) | 2 (25) | 7 (14) | 16 (67) | 21 (25) |
| No. of cases without mutations (%) | 73 (66) | 0 (0) | 3 (43) | 16 (76) | 7 (64) | 6 (75) | 41 (86) | 8 (33) | 65 (75) |
When two members of a single family presented an age of onset for the disease that fell between two different categories, we included both in the category of the patient presenting the earlier age of onset for NS. To calculate the percentage of mutations, we used the number of cases. ND, not determined.
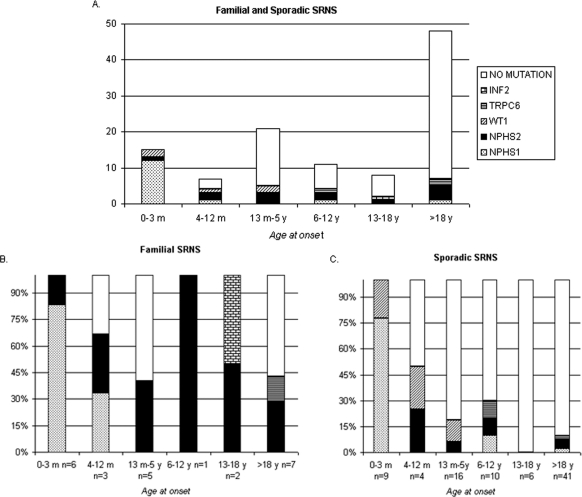
The frequencies and distribution of mutations in podocyte genes differed depending on the age at onset (Table 2; Figure 1A). In congenital onset (onset from 0 to 3 months), mutations were detected in 100% of cases: NPHS1, 80% (12 of 15); NPHS2, 7% (1 of 15); WT1, 13% (2 of 15). In infantile onset (from 4 to 12 months), mutations were found in 57% of patients: NPHS1, 14% (1 of 7); NPHS2, 29% (2 of 7); WT1, 14% (1 of 7). However, we only explained 24% of the early childhood-onset cases (from 13 months to 5 years) caused by mutations in the NPHS2 (14%, 3 of 21) and WT1 (10%, 2 of 21) genes and 36% of the late childhood-onset patients (from 4 to 12 years) caused by mutations in the NPHS1 (9%, 1 of 11), NPHS2 (18%, 2 of 11), and TRPC6 (9%, 1 of 11) genes. Finally, we identified pathogenic mutations for 25% (1 NPHS2; 1 INF2) of adolescent patients (from 13 to 17 years) and for 14% (7 of 48) of adult patients (>18 years): NPHS1, 2%; NPHS2, 8%; TRPC6, 4%.
Figure 1.
Age at diagnosis of NS in correlation to detected pathogenic mutations in NPHS1, NPHS2, WT1, TRPC6, and INF2 in 110 families (we did not include the ACTN4 and CD2AP genes because no pathogenic mutations were identified in our cohort). (A) Familial and sporadic cases. (B) Percentage of mutations in familial cases. (C) Percentage of mutations in sporadic cases.
The mutation detection rate for familial cases was 67% (16 of 24), but only 25% (21 of 86) for sporadic ones (Table 2). In familial cases, the most common mutated gene was NPHS2 (34%), whereas NPHS1 (11%) was the most common for nonfamilial cases. If we divide familial cases between AR and AD SRNS, we identified pathogenic mutations in 78% (14 of 18) and 33% (2 of 6) of cases, respectively. The frequencies of mutations according to the age at onset were also different between familial and sporadic cases (Figure 1, B and C). In familial cases, we explained 100% of congenital-onset (NPHS1 83%, 5 of 6; NPHS2 17%, 1 of 6), 66% of infantile-onset (NPHS1 33%, 1 of 3; NPHS2 33%, 1 of 3), 40% of early childhood-onset (NPHS2, 2 of 5), 100% of late childhood-onset (NPHS2, 1 of 1), 100% of adolescent-onset (NPHS2, 1 of 2, INF2 1 of 2), and 43% of adult-onset cases (NPHS2 29%, 2 of 7; TRPC6 14%, 1 of 7). In sporadic cases, we also detected pathogenic mutations in 100% of congenital cases (NPHS1 78%, 7 of 9; WT1 22%, 2 of 9) and in 50% of infantile-onset cases (NPHS2 25%, 1 of 4; WT1 25%, 1 of 4), but only in 19% of early childhood-onset (NPHS2 6%, 1 of 16; WT1 13%, 2 of 16), 30% of late childhood-onset (NPHS1 10%, 1 of 10; NPHS2 10%, 1 of 10; TRPC6 10%, 1 of 10), 0% of adolescent-onset (0 of 6), and 10% of adult-onset cases (NPHS1 2.5%, 1 of 41; NPHS2 5%, 2 of 41; TRPC6 2.5%, 1 of 41).
A description of all of the mutations detected is given in Supplementary Table 2.
Genotype–Phenotype Correlations
Genotype and age at NS onset.
Earlier presentation was found in patients with two severe NPHS1 mutations, followed by patients with WT1 mutations and two pathogenic NPHS2 mutations. Later NS onset was found in patients with TRPC6 and INF2 mutations or one pathogenic NPHS2 mutation in compound heterozygosity with the p.R229Q variant. Patients with NPHS1 mutations showed significantly earlier onset of NS than patients with two NPHS2 mutations (median, 0.1 [range, 0.0 to 27.0] versus 8.0 years [range, 0.02 to 39.0]; P < 0.001; Table 1). This correlation was also present among patients with two severe NPHS1 mutations compared with patients with two pathogenic NPHS2 mutations (median 0.0 [range, 0.0 to 0.1] versus 2.3 years [range 0.02 to 8.0]; P < 0.001). In addition, patients with at least one mild NPHS1 mutation also manifested the disease earlier than patients with one NPHS2 pathogenic mutation plus the p.R229Q variant (median 6.5 [range, 1 to 27.0] versus 19.0 years [range 10.0 to 39.0]; P = 0.05). In contrast, age at onset of NS was later in patients with WT1 mutations than in patients with two severe NPHS1 mutations (P = 0.004), but there was no significant difference compared with patients with two pathogenic NPHS2 mutations. Finally, no difference was observed in the age at onset of NS between patients with TRPC6 mutations (median, 25.0 years; range, 7.2 to 41.0 years) and patients with at least one mild NPHS1 mutation or one NPHS2 pathogenic mutation plus the p.R229Q variant.
Genotype and renal histology.
Renal biopsy was performed in 10 of 16 patients (62.5%) belonging to 15 families with NPHS1 mutations, and the most common histology pattern was FSGS (55%, 6 of 11; Table 1; Supplementary Table 1). For patients without FSGS, the histology findings were as follows: CNF, 3 of 11 (27%); DMS, 1 of 11 (9%). Renal biopsy was performed in 17 of 19 patients (90%) belonging to 13 families carrying NPHS2 mutations, and the histology findings were as follows: FSGS, 16 of 17 (94%); minimal change NS, 1 of 17 (6%). For patients with WT1 mutations, the histology findings were as follows: FSGS, 3 of 5 (60%); DMS, 2 of 5 (40%). The three patients with TRPC6 mutations and renal biopsy performed showed FSGS. Five patients of the same family carried one pathogenic INF2 mutation, and two of them showed FSGS, whereas the remaining three had only four glomeruli in the biopsy with complete sclerosis in one or two of them and small foci of tubular atrophy and interstitial fibrosis.
Genotype and response to treatment.
One of four patients with NPHS1 mutations treated with immunosuppressive treatment exhibited partial response to tacrolimus and angiotensin-converting enzyme inhibitors (ACEIs) (10). Data on response to immunosuppressive and ACEI treatment were available for 16 patients with NPHS2 mutations, among them being three patients with decreased nephrotic proteinuria (Table 1; Supplementary Table 1). Three patients with WT1 mutations received immunosuppressive therapy, and none of them experienced a sustained reduction of proteinuria. The remaining two patients with WT1 mutations were only treated with ACEIs and they partially responded. Only one patient with a TRPC6 mutation was treated with immunosuppressive treatment, and she experienced a sustained reduction of proteinuria to subnephrotic levels (34). Patients with INF2 mutations did not received steroid or immunosuppressive treatment.
Genotype and age at ESRD onset.
Age at ESRD was earlier in patients with NPHS1 mutations than in patients with NPHS2 mutations (P < 0.001; Table 1). Six children with NPHS1 severe mutations progressed to ESRD within a median time of 1.0 year after the onset of the disease, whereas the group of six children with two pathogenic NPHS2 mutations developed ESRD after a median time of 3.7 years (P = 0.002). Two patients with WT1 mutations developed ESRD at a median age of 3 years, which was significantly different from the group of two pathogenic NPHS2 mutations. Only one patient with a TRPC6 mutation reached ESRD in a time interval of 14 years. Patients with INF2 mutations reached ESRD in a time interval of 4.5 years.
Discussion
The increasing knowledge of the molecular basis of NS represents a milestone in nephrology but also adds greater complexity to clinical nephrologists' decisions about when and which genetic tests should be indicated. The aim of this study was to provide a practical guideline for genetic testing in SRNS. Our study represents the largest cohort of patients with SRNS undergoing a multistep molecular evaluation of eight podocyte genes and the first to include adult-onset patients with FSGS. Our data confirm not only that mutations in different genes manifest with NS at different ages but also that different mutations in the same gene result in distinct ages of onset for NS. We show here that 34% (37/110) of SRNS patients could be explained by mutations in one of these genes, of whom 67% (16/24) were familial cases and 25% (21/86) were sporadic. We found disease-causing mutations in 100% of congenital-onset cases and in 57% of infantile-onset cases, which is higher than previously described (14,15,42,45). Interestingly, in our Spanish cohort of CNS patients, we identified more pathogenic mutations in NPHS1 than in NPHS2, whereas an equal mutation rate for these two genes was reported in central European patients (15), probably because of the high frequency of the p.R138Q mutation in this region (53). The percentage of patients with mutations decreases as the age at onset increases and the distribution of mutations changes between children with congenital onset (most of them with mutations in NPHS1) and other ages of presentation (most of them with mutations in NPHS2). In childhood onset, we found a lower rate of mutations than previously published [reviewed by Benoit et al. (7)], but in adolescent and adult-onset patients, a higher than expected rate was observed (18,54,55).
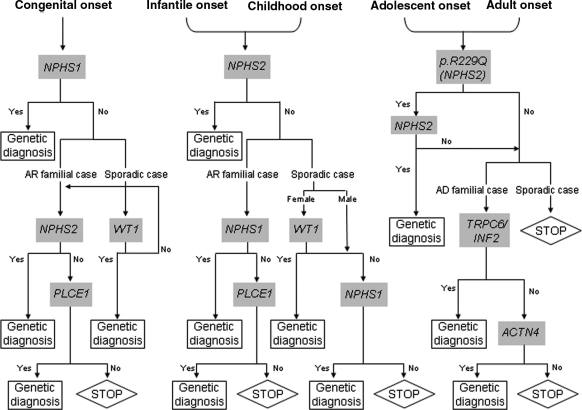
The frequency of mutations among these genes in our Spanish cohort and the revision of the literature allowed us to propose a genetic testing approach for diagnostic purposes (Figure 2). In congenital-onset cases, it is important to analyze several podocyte genes in a multistep strategy because of the high chances of finding mutations in these cases. The first step should be to screen for NPHS1 and, if no mutations are found, screening for NPHS2 in familial cases and for WT1 in the sporadic ones. If negative, in sporadic congenital-onset cases, the next step should be to analyze the NPHS2 gene. The last step for both sporadic and familial CNS would be PLCE1 analysis (42). In infantile onset and in childhood onset, we propose starting with the NPHS2 gene and, if no mutations are found, screening for NPHS1 in familial and sporadic cases and WT1 only in females with sporadic SRNS. Although we have not found pathogenic mutations in PLCE1 in early-onset SRNS, PLCE1 analysis would be indicated in those cases with familial DMS/FSGS (20,22). Finally, in adolescent- and adult-onset cases, we suggest screening for p.R229Q in the NPHS2 gene and, if positive, to analyze the whole gene. We recommend further TRPC6 and INF2 testing only for AD late-onset familial FSGS and, if negative, to analyze ACTN4 (37). Mutations in the TRPC6 gene have been found in 1 of 41 cases of sporadic adult-onset SRNS, being a rare cause of adult-onset FSGS. It is worth noting the incomplete penetrance of TRPC6 mutations, limiting its diagnostic value (30,34,56). Because CD2AP pathogenicity has been clearly shown only in one patient (38) and we have not found any mutation in our Spanish cohort with SRNS, we do not suggest screening for this gene. Benoit et al. (7) have recently proposed a similar genetic testing approach for SRNS, taking into account the renal biopsy. In our cohort of pediatric patients with SRNS, renal histology was not a key tool to indicate the most appropriate gene to analyze because most cases presented with FSGS, but when available, cases with FSGS must be tested for NPHS1 and NPHS2 and cases with DMS must first be tested for WT1 followed by PLCE1 (7). However, our study is limited by the small sample size, especially for each age group under 18 years, and for the homogeneous geographic origin/ethnicity of the studied cohort; therefore, larger studies would help to improve the proposed genetic testing algorithm for SRNS.
Figure 2.
Genetic approach in children and adults with SRNS.
A partial response was observed in 7 of 26 patients carrying podocyte gene mutations who received either immunosuppressive and ACEI treatment or only ACEI treatment. Calcineurin inhibitors induced a partial remission of proteinuria in several other children with genetic forms of NS (57). Recently, it has been shown that most patients with genetic CNS/SRNS presented lower response to cyclosporine A compared with nongenetic patients and showed rapid progression to ESRD (43). On the other hand, three patients with familial FSGS treated with early angiotensin inhibition resulted in a partial to complete remission of proteinuria (58), suggesting that some patients could benefit from ACEI treatment. Further studies would be necessary to adequately determine which treatment can be beneficial for genetic SRNS patients. Patients with NPHS1 mutations showed a shorter progression time to ESRD than patients with two NPHS2 mutations. In addition, none of the patients with pathogenic mutations relapsed after kidney transplantation.
In conclusion, our data indicate that two main criteria determine the appropriate genes to test: (1) age at onset and (2) familial/sporadic status. Because in our cohort of congenital-, infantile-, and childhood-onset patients with mutations, renal histology was not a determinant criterion because most presented with FSGS, we recommend starting with genetic testing before renal biopsy because it is a noninvasive technique. In adults, renal biopsy is the first step because it allows ruling out other causes of NS such as membranous nephropathy. Although the analysis of multiple genes is time-consuming and expensive, the identification of pathogenic mutations can help (1) to avoid adverse effects of steroid/immunosuppressive treatment, (2) to encourage living donor kidney transplantation, (3) to perform a prognosis depending on which gene is mutated and which kind of mutations are detected, and (4) to offer the possibility of presymptomatic, prenatal, and preimplantation genetic diagnosis.
Disclosures
None.
Acknowledgments
We thank the patients and their families for taking part in this study. This work was funded by grants from the Spanish Health Ministry (FIS-05/0761 and FIS-09/01506) and the REDinREN (Red renal de investigación española 16/06, RETICS, Instituto de Investigación Carlos III). We thank the physicians who provided samples and clinical information for this study (Supplemental Appendix 1).
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1. Short versus standard prednisone therapy for initial treatment of idiopathic nephrotic syndrome in children. Arbeitsgemeinschaft fur Padiatrische Nephrologie. Lancet 1: 380–383, 1988 [PubMed] [Google Scholar]
- 2. Tune BM, Mendoza SA: Treatment of the idiopathic nephrotic syndrome: Regimens and outcomes in children and adults. J Am Soc Nephrol 8: 824–832, 1997 [DOI] [PubMed] [Google Scholar]
- 3. Braden GL, Mulhern JG, O'Shea MH, Nash SV, Ucci AA, Jr, Germain MJ: Changing incidence of glomerular diseases in adults. Am J Kidney Dis 35: 878–883, 2000 [DOI] [PubMed] [Google Scholar]
- 4. Troyanov S, Wall CA, Miller JA, Scholey JW, Cattran DC: Focal and segmental glomerulosclerosis: Definition and relevance of a partial remission. J Am Soc Nephrol 16: 1061–1068, 2005 [DOI] [PubMed] [Google Scholar]
- 5. Antignac C: Genetic models: Clues for understanding the pathogenesis of idiopathic nephrotic syndrome. J Clin Invest 109: 447–449, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Savin VJ, Sharma R, Sharma M, McCarthy ET, Swan SK, Ellis E, Lovell H, Warady B, Gunwar S, Chonko AM, Artero M, Vincenti F: Circulating factor associated with increased glomerular permeability to albumin in recurrent focal segmental glomerulosclerosis. N Engl J Med 334: 878–883, 1996 [DOI] [PubMed] [Google Scholar]
- 7. Benoit G, Machuca E, Antignac C: Hereditary nephrotic syndrome: A systematic approach for genetic testing and a review of associated podocyte gene mutations. Pediatr Nephrol 25: 1621–1632, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kestila M, Lenkkeri U, Mannikko M, Lamerdin J, McCready P, Putaala H, Ruotsalainen V, Morita T, Nissinen M, Herva R, Kashtan CE, Peltonen L, Holmberg C, Olsen A, Tryggvason K: Positionally cloned gene for a novel glomerular protein–nephrin–is mutated in congenital nephrotic syndrome. Mol Cell 1: 575–582, 1998 [DOI] [PubMed] [Google Scholar]
- 9. Philippe A, Nevo F, Esquivel EL, Reklaityte D, Gribouval O, Tete MJ, Loirat C, Dantal J, Fischbach M, Pouteil-Noble C, Decramer S, Hoehne M, Benzing T, Charbit M, Niaudet P, Antignac C: Nephrin mutations can cause childhood-onset steroid-resistant nephrotic syndrome. J Am Soc Nephrol 19: 1871–1878, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Santin S, Garcia-Maset R, Ruiz P, Gimenez I, Zamora I, Pena A, Madrid A, Camacho JA, Fraga G, Sanchez-Moreno A, Cobo MA, Bernis C, Ortiz A, de Pablos AL, Pintos G, Justa ML, Hidalgo-Barquero E, Fernandez-Llama P, Ballarin J, Ars E, Torra R: Nephrin mutations cause childhood- and adult-onset focal segmental glomerulosclerosis. Kidney Int 76: 1268–1276, 2009 [DOI] [PubMed] [Google Scholar]
- 11. Boute N, Gribouval O, Roselli S, Benessy F, Lee H, Fuchshuber A, Dahan K, Gubler MC, Niaudet P, Antignac C: NPHS2, encoding the glomerular protein podocin, is mutated in autosomal recessive steroid-resistant nephrotic syndrome. Nat Genet 24: 349–354, 2000 [DOI] [PubMed] [Google Scholar]
- 12. Koziell A, Grech V, Hussain S, Lee G, Lenkkeri U, Tryggvason K, Scambler P: Genotype/phenotype correlations of NPHS1 and NPHS2 mutations in nephrotic syndrome advocate a functional inter-relationship in glomerular filtration. Hum Mol Genet 11: 379–388, 2002 [DOI] [PubMed] [Google Scholar]
- 13. Schultheiss M, Ruf RG, Mucha BE, Wiggins R, Fuchshuber A, Lichtenberger A, Hildebrandt F: No evidence for genotype/phenotype correlation in NPHS1 and NPHS2 mutations. Pediatr Nephrol 19: 1340–1348, 2004 [DOI] [PubMed] [Google Scholar]
- 14. Sako M, Nakanishi K, Obana M, Yata N, Hoshii S, Takahashi S, Wada N, Takahashi Y, Kaku Y, Satomura K, Ikeda M, Honda M, Iijima K, Yoshikawa N: Analysis of NPHS1, NPHS2, ACTN4, and WT1 in Japanese patients with congenital nephrotic syndrome. Kidney Int 67: 1248–1255, 2005 [DOI] [PubMed] [Google Scholar]
- 15. Hinkes BG, Mucha B, Vlangos CN, Gbadegesin R, Liu J, Hasselbacher K, Hangan D, Ozaltin F, Zenker M, Hildebrandt F: Nephrotic syndrome in the first year of life: Two thirds of cases are caused by mutations in 4 genes (NPHS1, NPHS2, WT1, and LAMB2). Pediatrics 119: e907–e919, 2007 [DOI] [PubMed] [Google Scholar]
- 16. Tsukaguchi H, Sudhakar A, Le TC, Nguyen T, Yao J, Schwimmer JA, Schachter AD, Poch E, Abreu PF, Appel GB, Pereira AB, Kalluri R, Pollak MR: NPHS2 mutations in late-onset focal segmental glomerulosclerosis: R229Q is a common disease-associated allele. J Clin Invest 110: 1659–1666, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tonna SJ, Needham A, Polu K, Uscinski A, Appel GB, Falk RJ, Katz A, Al-Waheeb S, Kaplan BS, Jerums G, Savige J, Harmon J, Zhang K, Curhan GC, Pollak MR: NPHS2 variation in focal and segmental glomerulosclerosis. BMC Nephrol 9: 13, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Machuca E, Hummel A, Nevo F, Dantal J, Martinez F, Al-Sabban E, Baudouin V, Abel L, Grunfeld JP, Antignac C: Clinical and epidemiological assessment of steroid-resistant nephrotic syndrome associated with the NPHS2 R229Q variant. Kidney Int 75: 727–735, 2009 [DOI] [PubMed] [Google Scholar]
- 19. Hinkes B, Wiggins RC, Gbadegesin R, Vlangos CN, Seelow D, Nurnberg G, Garg P, Verma R, Chaib H, Hoskins BE, Ashraf S, Becker C, Hennies HC, Goyal M, Wharram BL, Schachter AD, Mudumana S, Drummond I, Kerjaschki D, Waldherr R, Dietrich A, Ozaltin F, Bakkaloglu A, Cleper R, Basel-Vanagaite L, Pohl M, Griebel M, Tsygin AN, Soylu A, Muller D, Sorli CS, Bunney TD, Katan M, Liu J, Attanasio M, O'Toole JF, Hasselbacher K, Mucha B, Otto EA, Airik R, Kispert A, Kelley GG, Smrcka AV, Gudermann T, Holzman LB, Nurnberg P, Hildebrandt F: Positional cloning uncovers mutations in PLCE1 responsible for a nephrotic syndrome variant that may be reversible. Nat Genet 38: 1397–1405, 2006 [DOI] [PubMed] [Google Scholar]
- 20. Gbadegesin R, Hinkes BG, Hoskins BE, Vlangos CN, Heeringa SF, Liu J, Loirat C, Ozaltin F, Hashmi S, Ulmer F, Cleper R, Ettenger R, Antignac C, Wiggins RC, Zenker M, Hildebrandt F: Mutations in PLCE1 are a major cause of isolated diffuse mesangial sclerosis (IDMS). Nephrol Dial Transplant 23: 1291–1297, 2008 [DOI] [PubMed] [Google Scholar]
- 21. Gbadegesin R, Bartkowiak B, Lavin PJ, Mukerji N, Wu G, Bowling B, Eckel J, Damodaran T, Winn MP: Exclusion of homozygous PLCE1 (NPHS3) mutations in 69 families with idiopathic and hereditary FSGS. Pediatr Nephrol 24: 281–285, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Boyer O, Benoit G, Gribouval O, Nevo F, Pawtowski A, Bilge I, Bircan Z, Deschenes G, Guay-Woodford LM, Hall M, Macher MA, Soulami K, Stefanidis CJ, Weiss R, Loirat C, Gubler MC, Antignac C: Mutational analysis of the PLCE1 gene in steroid resistant nephrotic syndrome. J Med Genet 47: 445–452, 2010 [DOI] [PubMed] [Google Scholar]
- 23. Pelletier J, Bruening W, Li FP, Haber DA, Glaser T, Housman DE: WT1 mutations contribute to abnormal genital system development and hereditary Wilms' tumour. Nature 353: 431–434, 1991 [DOI] [PubMed] [Google Scholar]
- 24. Barbaux S, Niaudet P, Gubler MC, Grunfeld JP, Jaubert F, Kuttenn F, Fekete CN, Souleyreau-Therville N, Thibaud E, Fellous M, McElreavey K: Donor splice-site mutations in WT1 are responsible for Frasier syndrome. Nat Genet 17: 467–470, 1997 [DOI] [PubMed] [Google Scholar]
- 25. Jeanpierre C, Denamur E, Henry I, Cabanis MO, Luce S, Cecille A, Elion J, Peuchmaur M, Loirat C, Niaudet P, Gubler MC, Junien C: Identification of constitutional WT1 mutations, in patients with isolated diffuse mesangial sclerosis, and analysis of genotype/phenotype correlations by use of a computerized mutation database. Am J Hum Genet 62: 824–833, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mucha B, Ozaltin F, Hinkes BG, Hasselbacher K, Ruf RG, Schultheiss M, Hangan D, Hoskins BE, Everding AS, Bogdanovic R, Seeman T, Hoppe B, Hildebrandt F: Mutations in the Wilms' tumor 1 gene cause isolated steroid resistant nephrotic syndrome and occur in exons 8 and 9. Pediatr Res 59: 325–331, 2006 [DOI] [PubMed] [Google Scholar]
- 27. Zenker M, Aigner T, Wendler O, Tralau T, Muntefering H, Fenski R, Pitz S, Schumacher V, Royer-Pokora B, Wuhl E, Cochat P, Bouvier R, Kraus C, Mark K, Madlon H, Dotsch J, Rascher W, Maruniak-Chudek I, Lennert T, Neumann LM, Reis A: Human laminin beta2 deficiency causes congenital nephrosis with mesangial sclerosis and distinct eye abnormalities. Hum Mol Genet 13: 2625–2632, 2004 [DOI] [PubMed] [Google Scholar]
- 28. Hasselbacher K, Wiggins RC, Matejas V, Hinkes BG, Mucha B, Hoskins BE, Ozaltin F, Nurnberg G, Becker C, Hangan D, Pohl M, Kuwertz-Broking E, Griebel M, Schumacher V, Royer-Pokora B, Bakkaloglu A, Nurnberg P, Zenker M, Hildebrandt F: Recessive missense mutations in LAMB2 expand the clinical spectrum of LAMB2-associated disorders. Kidney Int 70: 1008–1012, 2006 [DOI] [PubMed] [Google Scholar]
- 29. Winn MP, Conlon PJ, Lynn KL, Farrington MK, Creazzo T, Hawkins AF, Daskalakis N, Kwan SY, Ebersviller S, Burchette JL, Pericak-Vance MA, Howell DN, Vance JM, Rosenberg PB: A mutation in the TRPC6 cation channel causes familial focal segmental glomerulosclerosis. Science 308: 1801–1804, 2005 [DOI] [PubMed] [Google Scholar]
- 30. Reiser J, Polu KR, Moller CC, Kenlan P, Altintas MM, Wei C, Faul C, Herbert S, Villegas I, Vila-Casado C, McGee M, Sugimoto H, Brown D, Kalluri R, Mundel P, Smith PL, Clapham DE, Pollak MR: TRPC6 is a glomerular slit diaphragm-associated channel required for normal renal function. Nat Genet 37: 739–744, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kaplan JM, Kim SH, North KN, Rennke H, Correia LA, Tong HQ, Mathis BJ, Rodriguez-Perez JC, Allen PG, Beggs AH, Pollak MR: Mutations in ACTN4, encoding alpha-actinin-4, cause familial focal segmental glomerulosclerosis. Nat Genet 24: 251–256, 2000 [DOI] [PubMed] [Google Scholar]
- 32. Kim JM, Wu H, Green G, Winkler CA, Kopp JB, Miner JH, Unanue ER, Shaw AS: CD2-associated protein haploinsufficiency is linked to glomerular disease susceptibility. Science 300: 1298–1300, 2003 [DOI] [PubMed] [Google Scholar]
- 33. Brown EJ, Schlondorff JS, Becker DJ, Tsukaguchi H, Tonna SJ, Uscinski AL, Higgs HN, Henderson JM, Pollak MR: Mutations in the formin gene INF2 cause focal segmental glomerulosclerosis. Nat Genet 42: 72–76, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Santin S, Ars E, Rossetti S, Salido E, Silva I, Garcia-Maset R, Gimenez I, Ruiz P, Mendizabal S, Luciano NJ, Pena A, Camacho JA, Fraga G, Cobo MA, Bernis C, Ortiz A, de Pablos AL, Sanchez-Moreno A, Pintos G, Mirapeix E, Fernandez-Llama P, Ballarin J, Torra R, Zamora I, Lopez-Hellin J, Madrid A, Ventura C, Vilalta R, Espinosa L, Garcia C, Melgosa M, Navarro M, Gimenez A, Cots JV, Alexandra S, Caramelo C, Egido J, San J, de la CF, Sala P, Raspall F, Vila A, Daza AM, Vazquez M, Ecija JL, Espinosa M, Justa ML, Poveda R, Aparicio C, Rosell J, Muley R, Montenegro J, Gonzalez D, Hidalgo E, de Frutos DB, Trillo E, Gracia S, de los Rios FJ: TRPC6 mutational analysis in a large cohort of patients with focal segmental glomerulosclerosis. Nephrol Dial Transplant 24: 3089–3096, 2009 [DOI] [PubMed] [Google Scholar]
- 35. Heeringa SF, Moller CC, Du J, Yue L, Hinkes B, Chernin G, Vlangos CN, Hoyer PF, Reiser J, Hildebrandt F: A novel TRPC6 mutation that causes childhood FSGS. PLoS One 4: e7771, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Choi HJ, Lee BH, Cho HY, Moon KC, Ha IS, Nagata M, Choi Y, Cheong HI: Familial focal segmental glomerulosclerosis associated with an ACTN4 mutation and paternal germline mosaicism. Am J Kidney Dis 51: 834–838, 2008 [DOI] [PubMed] [Google Scholar]
- 37. Weins A, Kenlan P, Herbert S, Le TC, Villegas I, Kaplan BS, Appel GB, Pollak MR: Mutational and biological analysis of alpha-actinin-4 in focal segmental glomerulosclerosis. J Am Soc Nephrol 16: 3694–3701, 2005 [DOI] [PubMed] [Google Scholar]
- 38. Lowik MM, Groenen PJ, Pronk I, Lilien MR, Goldschmeding R, Dijkman HB, Levtchenko EN, Monnens LA, van den Heuvel LP: Focal segmental glomerulosclerosis in a patient homozygous for a CD2AP mutation. Kidney Int 72: 1198–1203, 2007 [DOI] [PubMed] [Google Scholar]
- 39. Gigante M, Pontrelli P, Montemurno E, Roca L, Aucella F, Penza R, Caridi G, Ranieri E, Ghiggeri GM, Gesualdo L: CD2AP mutations are associated with sporadic nephrotic syndrome and focal segmental glomerulosclerosis (FSGS). Nephrol Dial Transplant 24: 1858–1864, 2009 [DOI] [PubMed] [Google Scholar]
- 40. Benoit G, Machuca E, Nevo F, Gribouval O, Lepage D, Antignac C: Analysis of recessive CD2AP and ACTN4 mutations in steroid-resistant nephrotic syndrome. Pediatr Nephrol 25: 445–451, 2010 [DOI] [PubMed] [Google Scholar]
- 41. Lowik M, Levtchenko E, Westra D, Groenen P, Steenbergen E, Weening J, Lilien M, Monnens L, van den HL: Bigenic heterozygosity and the development of steroid-resistant focal segmental glomerulosclerosis. Nephrol Dial Transplant 23: 3146–3151, 2008 [DOI] [PubMed] [Google Scholar]
- 42. Machuca E, Benoit G, Nevo F, Tete MJ, Gribouval O, Pawtowski A, Brandstrom P, Loirat C, Niaudet P, Gubler MC, Antignac C: Genotype-phenotype correlations in non-Finnish congenital nephrotic syndrome. J Am Soc Nephrol 21: 1209–1217, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Buscher AK, Kranz B, Buscher R, Hildebrandt F, Dworniczak B, Pennekamp P, Kuwertz-Broking E, Wingen AM, John U, Kemper M, Monnens L, Hoyer PF, Weber S, Konrad M: Immunosuppression and renal outcome in congenital and pediatric steroid-resistant nephrotic syndrome. Clin J Am Soc Nephrol 5: 2075–2084, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Miller SA, Dykes DD, Polesky HF: A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res 16: 1215, 1988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lenkkeri U, Mannikko M, McCready P, Lamerdin J, Gribouval O, Niaudet PM, Antignac CK, Kashtan CE, Homberg C, Olsen A, Kestila M, Tryggvason K: Structure of the gene for congenital nephrotic syndrome of the finnish type (NPHS1) and characterization of mutations. Am J Hum Genet 64: 51–61, 1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Shibata R, Hashiguchi A, Sakamoto J, Yamada T, Umezawa A, Hata J: Correlation between a specific Wilms tumour suppressor gene (WT1) mutation and the histological findings in Wilms tumour (WT). J Med Genet 39: e83, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kohler B, Pienkowski C, Audran F, Delsol M, Tauber M, Paris F, Sultan C, Lumbroso S: An N-terminal WT1 mutation (P181S) in an XY patient with ambiguous genitalia, normal testosterone production, absence of kidney disease and associated heart defect: Enlarging the phenotypic spectrum of WT1 defects. Eur J Endocrinol 150: 825–830, 2004 [DOI] [PubMed] [Google Scholar]
- 48. Santin S, Tazon-Vega B, Silva I, Cobo MA, Gimenez I, Ruiz P, Garcia-Maset R, Ballarin J, Torra R, Ars E: Clinical value of NPHS2 analysis in early- and adult-onset steroid-resistant nephrotic syndrome. Clin J Am Soc Nephrol 2: 344–354, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Tavtigian SV, Deffenbaugh AM, Yin L, Judkins T, Scholl T, Samollow PB, de SD, Zharkikh A, Thomas A: Comprehensive statistical study of 452 BRCA1 missense substitutions with classification of eight recurrent substitutions as neutral. J Med Genet 43: 295–305, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Rossetti S, Consugar MB, Chapman AB, Torres VE, Guay-Woodford LM, Grantham JJ, Bennett WM, Meyers CM, Walker DL, Bae K, Zhang QJ, Thompson PA, Miller JP, Harris PC: Comprehensive molecular diagnostics in autosomal dominant polycystic kidney disease. J Am Soc Nephrol 18: 2143–2160, 2007 [DOI] [PubMed] [Google Scholar]
- 51. Barnetson RA, Cartwright N, van VA, Haq N, Drew K, Farrington S, Williams N, Warner J, Campbell H, Porteous ME, Dunlop MG: Classification of ambiguous mutations in DNA mismatch repair genes identified in a population-based study of colorectal cancer. Hum Mutat 29: 367–374, 2008 [DOI] [PubMed] [Google Scholar]
- 52. Weber S, Gribouval O, Esquivel EL, Moriniere V, Tete MJ, Legendre C, Niaudet P, Antignac C: NPHS2 mutation analysis shows genetic heterogeneity of steroid-resistant nephrotic syndrome and low post-transplant recurrence. Kidney Int 66: 571–579, 2004 [DOI] [PubMed] [Google Scholar]
- 53. Hinkes B, Vlangos C, Heeringa S, Mucha B, Gbadegesin R, Liu J, Hasselbacher K, Ozaltin F, Hildebrandt F: Specific podocin mutations correlate with age of onset in steroid-resistant nephrotic syndrome. J Am Soc Nephrol 19: 365–371, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Aucella F, De BP, Gatta G, Muscarella LA, Vigilante M, di GG, D'Errico M, Zelante L, Stallone C, Bisceglia L: Molecular analysis of NPHS2 and ACTN4 genes in a series of 33 Italian patients affected by adult-onset nonfamilial focal segmental glomerulosclerosis. Nephron Clin Pract 99: c31–c36, 2005 [DOI] [PubMed] [Google Scholar]
- 55. McKenzie LM, Hendrickson SL, Briggs WA, Dart RA, Korbet SM, Mokrzycki MH, Kimmel PL, Ahuja TS, Berns JS, Simon EE, Smith MC, Trachtman H, Michel DM, Schelling JR, Cho M, Zhou YC, Binns-Roemer E, Kirk GD, Kopp JB, Winkler CA: NPHS2 variation in sporadic focal segmental glomerulosclerosis. J Am Soc Nephrol 18: 2987–2995, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Zhu B, Chen N, Wang ZH, Pan XX, Ren H, Zhang W, Wang WM: Identification and functional analysis of a novel TRPC6 mutation associated with late onset familial focal segmental glomerulosclerosis in Chinese patients. Mutat Res 664: 84–90, 2009 [DOI] [PubMed] [Google Scholar]
- 57. Bensman A, Niaudet P: Non-immunologic mechanisms of calcineurin inhibitors explain its antiproteinuric effects in genetic glomerulopathies. Pediatr Nephrol 25: 1197–1199, 2010 [DOI] [PubMed] [Google Scholar]
- 58. Copelovitch L, Guttenberg M, Pollak MR, Kaplan BS: Renin-angiotensin axis blockade reduces proteinuria in presymptomatic patients with familial FSGS. Pediatr Nephrol 22: 1779–1784, 2007 [DOI] [PubMed] [Google Scholar]