Abstract
Aims
To determine the comparative levels of and associations between policing interference and characteristics of US syringe exchange programs (SEPs).
Design
Cross-sectional.
Setting
A national survey of US SEPs.
Participants
A total of 111 program managers (representing 59% of all US SEPs).
Measurements
Program manager self-report.
Findings
With overall interference profiles ranging from systematic to totally interference-free, 43% of respondents reported at least monthly client harassment, 31% at least monthly unauthorized confiscation of clients’ syringes, 12% at least monthly client arrest en route to or from SEP and 26% uninvited police appearances at program sites at least every 6 months. In multivariate modeling, legal status of SEP, jurisdiction’s syringe regulation environment and affiliation with health department were not associated with frequency of police interference. Programs serving pre-dominantly injection drug users (IDUs) of color were 3.56 times more likely to report frequent client arrest en route to or from SEP and 3.92 times more likely to report unauthorized syringe confiscation. Those serving more than three sites were 3.96 times more likely to report client harassment, while stationary operation was protective against uninvited police appearances. The majority (56%) reported not documenting adverse police events; those who did were 2.92 times more likely to report unauthorized syringe confiscation from clients.
Conclusions
Findings highlight limitations of the impact of legal reforms on aligning police activities with SEP operations. Systematic adverse event surveillance and evidence-based structural interventions are needed to maximize the benefits of public health prevention targeting IDUs and other criminalized populations. SEPs that report no adverse events may represent programs already working in harmony with law enforcement agencies, a priority highlighted in US Centers for Disease Control’s new SEP guidelines. The significance of mechanisms translating criminal justice disparities into health disparities is discussed.
Keywords: Criminal justice system, HIV, injection drug use, policy interventions, racial disparities, structural barriers, structural interventions, syringe access, syringe exchange programs
INTRODUCTION
The spread of blood-borne disease through injection drug use is a long-standing problem, with a significant proportion of all HIV, hepatitis B and hepatitis C cases in the United States attributable to injection-related behaviors [1-3]. The substance abuse-infectious disease syndemic disproportionately affects minority and marginalized populations due to links with social capital, social and drug-using networks and other structural factors [2,4-7]. Interventions demonstrated to reduce injection-related transmission of infectious disease include counseling, opioid maintenance therapy and syringe exchange programs (SEPs) [8-14].
By shaping the physical, psychological and economic environment, police practices influence public health efforts targeting injection drug users (IDUs) and other criminalized populations. Syringe confiscation, uninvited appearances at SEPs, use of SEP membership as a marker of criminality and client arrest can interfere with program operations and deter participation [15-25]. Direct experience with and perceptions of police practices can decrease IDU willingness and ability to engage in risk reduction practices [25-27]. The differential way in which racial groups experience and perceive the law and police activities may influence uptake of services, contributing in turn to observed racial disparities in HIV incidence [19,28-32]. There is evidence, however, that when it is aligned with public health efforts, police activity may promote drug user health, such as when police refer IDUs to SEPs [33-35].
Laws governing controlled substances and drug paraphernalia regulate syringe availability and direct police practice. Many US jurisdictions have looked to laws liberalizing syringe access and authorizing SEPs to curb injection-related HIV [36,37]. Gaps in the ‘policy transformation process’ [38], however, leave room for continued police interference with these initiatives post-reform [39]. This includes confiscation and destruction of injection equipment possessed legally by SEP clients [39-42]. Officers’ deviation from formal policy may result from poor legal knowledge, lax management, antagonism towards ‘enabling’ illegal behavior, occupational safety concerns and other factors [39]. By making SEPs more visible and boosting their scale, syringe access reforms may increase the risk of police interference [41,43].
Despite the influence of law and law enforcement on SEP operations, few systematic data exist on the prevalence or predictors of police interference with program functioning and police action targeting clients. Existing studies suggest that such practices are associated with client race and the SEP’s legal environment [21,41]. In a recent national survey, 29% of US SEPs listed police–client relations and 8% staff–police relations among operational problems [44]. No previous study, however, has examined program or client risk factors associated with police interference, whether SEPs document such incidents, or the measurable effect of law on police interference. At a time when the number of these programs is likely to expand, and when the US Centers for Disease Control (CDC) is encouraging programs to clear their activities with local law enforcement following the recent lifting of the ban on Federal funding, understanding SEP–police relations is especially crucial [45].
In this analysis, we investigate the prevalence of and factors associated with police practices targeting SEPs and their clients (collectively termed ‘police interference’). Based on existing literature, we hypothesized that: (i) formal laws related to syringe possession and authorization do not protect SEPs and clients from police interference; (ii) programs that are more ‘visible’ (in terms of annual volume of syringe distribution, number of sites per week, distribution methods) are more likely to experience police interference than their less visible counter-parts; (iii) SEPs serving primarily minority clients experience more police interference than those serving whites; and (iv) programs that document police interference systematically report more such events than SEPs without surveillance schemes.
METHODS
Study design
Between November 2008 and June 2009, a convenience sample of US SEP managers was assembled. During stage 1, Center for Interdisciplinary Research on AIDS (CIRA) staff recruited respondents attending a conference to complete a paper-and-pencil survey. Program name and location was noted on a separate list, used to exclude subsequent respondents representing SEPs already surveyed. During stage 2, SEP managers in locales unrepresented in stage 1 were invited via e-mail and telephone to complete an online Surveymonkey® version. All stage 2 contacts received reminders to encourage completion. Program names were not collected. Data were checked to eliminate multiple responses per SEP. The Human Investigation Committee at the Yale School of Medicine approved this study.
Study instrument
The 42-item survey assessed: (i) SEP program characteristics (e.g. region, types of area served, racial make-up of client base); (ii) legal environment (SEP authorization and legality of syringe possession); (iii) perceived life-time frequency of police interference events; (iv) characterization of program’s external relations; (v) types of training for and outreach to a variety of interactors; and (vi) perceived needs for improving relations between the SEPs and law enforcement. This study focuses on the associations between SEP characteristics, legal environment and the frequency of police interference.
Analytical methods
This analysis examines a set of four outcome variables that assessed the perceived life-time frequency of: (i) police harassment of clients; (ii) police confiscation of clients’ legal injection equipment; (iii) police arrest of clients en route to or from the SEP; and (iv) uninvited appearances by police at SEPs. To preserve power, a seven-point Likert response format for these items was trichotomized into ‘never/rarely’ versus ‘about once or twice per year’ versus ‘monthly/weekly/daily’. Because few SEPs reported uninvited police appearances, for this outcome data were dichotomized by ‘never/rarely’ versus ‘at least once a year’.
Our exposure variables included (i) legal environment (legality of syringe possession by SEP clients without a prescription by state or local law, legality of syringe possession by anyone without a prescription by state or local law and SEP authorization by state or local law); (ii) entity running SEP (health department/other); (iii) years in operation (mean + 1 standard deviation <16 years/≥16 years to improve distribution and power); (iv) annual syringe distribution volume (median split ≤90 000/>90 000); (v) program visibility: areas served (exclusively urban/non-exclusively urban), number of sites/week (median split ≤3/>3) and mobile distribution (yes/no); (vi) location in Northeast (yes/no), South (yes/no), West (yes/no) or Midwest (yes/no); (vii) modal client race/ethnicity (white/non-white); and (viii) systematically documenting police interference (yes/no).
Data were analyzed using STATA version 10 [46]. Standard descriptive statistics were used to characterize the sample. Bivariate analyses were conducted between all exposure variables and the four outcomes using generalized ordered logistic regression (OLR). This is the standard technique used with outcomes derived from Likert, where a dependent variable has a natural rank order but the relative magnitudes of those outcome values are unknown. We used gologit2 with the option autofit to fit partial proportional-odds models [47]. This approach tests the proportional-odds assumption for each coefficient, and for coefficients in which the assumption is not met, reports separate coefficients. Given the relatively small sample size and to address the problem of multiple comparisons on overall Type 1 error, only exposure variables significant at P < 0.10 level in bivariate analyses were entered into multinomial generalized ordered logistic regression models. Backward elimination of non-significant covariates produced models in which all coefficients were significant at the P < 0.05 level or for which removal did not change other coefficients by >10%.
RESULTS
Sample characteristics
Of the estimated 187 US SEPs [44], 111 (59%) programs from 34 states and territories completed this survey. The majority of programs serve mainly white clients, with only 27% reporting African American or Hispanic as the modal client race (Table 1). The median duration of operation was 10.5 years, with five volunteers and 2.5 paid staff members.
Table 1.
Sample characteristics in the Center for Interdisciplinary Research on AIDS (CIRA) syringe exchange program (SEP) survey (with data from the 2007 Beth Israel national SEP survey provided for sample comparison) (n = 111).
|
CIRA survey, n (%) |
Beth Israel survey, n (%)[44] |
|
|---|---|---|
| SEPs participating | 111 (60) | 131 (70) |
| Volume of exchange (units/year) | ||
| Small (<10 000) | 10 (11) | 23 (18) |
| Medium (10 000–55 000) | 29 (31) | 37 (28) |
| Large (55 001–499 999) | 42 (45) | 57 (44) |
| Very large (>500 000) | 13 (14) | 13 (10) |
| SEP services offered | ||
| Naloxone distribution | 45 (41) | 52 (40) |
| Condom distribution | 111 (100) | 130 (99) |
| Drug treatment referrals | 105 (96) | 120 (92) |
| HIV testing | 31 (28) | 115 (88)1 |
| HBV testing | 24 (22) | 30 (23)2 |
| Region | ||
| Northeast | 30 (29) | 31 (23) |
| South | 11 (11) | 13 (10) |
| West | 42 (40) | 61 (47) |
| Midwest | 22 (20) | 26 (20) |
| Modal race/ethnicity of clientele3 | ||
| White | 69 (72) | – |
| African American | 18 (19) | – |
| Hispanic | 8 (18) | – |
| Distribution modalities | ||
| Stationary | 81 (73) | – |
| Mobile | 62 (57) | – |
| Delivery | 39 (36) | 59 (45) |
| All three | 23 (21) | – |
| Program setting | ||
| Urban only | 44 (40) | – |
| Suburban only | 20 (18) | – |
| Rural only | 8 (7) | – |
| Urban and suburban | 10 (9) | – |
| Urban and rural | 11 (10) | – |
| Suburban and rural | 9 (8) | – |
| All three | 2 (2) | – |
| Legal environment | ||
| SEP operating illegally | 29 (26) | – |
| Any syringe possession w/o prescription legal | 50 (47) | – |
| Syringe possession w/o prescription legal only for SEP clients | 72 (65) | – |
| Operated by department of health | 21 (26) | 34 (26)4 |
| Receiving state funding | 61 (63) | 67 (52) |
Includes any HIV counseling or testing.
Includes any hepatitis B virus (HBV) counseling or testing.
No respondent indicated Asian, Native American, Pacific Islander or Other as the modal category.
Operated by city, county or state government.
In its demographic profile, our sample resembles closely that reported in the 2007 Beth Israel national SEP survey of US 131 programs [44] (Table 1). Close parity to this longitudinal study suggests that, although our data were collected from a convenience sample, we were able to cover a substantial and diverse cross-section of SEPs.
Only one-third (33%) of programs reported operating solely from a stationary location. Many (57%) also reported mobile sites and 36% provided delivery services; 21% reported all three distribution modes (Table 1). About one in four (24%) programs were single-site; half (51%) reported serving more than three sites/week. Although the majority of programs served urban areas (57%), a third reported operating in rural (33%) and 23% in suburban locales (Table 1).
All responding programs reported distributing condoms and safer sex supplies, 96% reported providing referrals to drug treatment, more than 65% reported conducting additional health promotion activities with their clients and more than 40% reported distributing naloxone, an opioid overdose antidote (Table 1). Nearly two-thirds (63%) received some state funding. At the time of this survey, US SEPs could not receive Federal funds [48].
The legal environment in which SEPs operated was varied (Table 1). Just fewer than half (49%) of programs reported being authorized by state law, 25% by local law and 26% operated illegally (Table 1). Syringe possession for SEP clients was reportedly sanctioned by state or local law for 65% of responding SEPs (Table 1); for a further 13% of programs, client possession was reportedly authorized through informal agreement with local authorities. About one in five programs (21%) reported that client syringe possession was illegal in their jurisdiction; 47% reported operating in locales where syringe possession had been completely deregulated (Table 1).
Frequency of police interference
Client harassment by police was the most frequently cited adverse encounter: almost half (43%) indicated that clients report these experiences at least monthly (Fig. 1), 23% at least weekly and 12 programs (11%) at least daily. The second most frequently reported event—unauthorized confiscation of clients’ injection equipment—was estimated to occur on at least a monthly basis by 31% of respondents (Fig. 1); 13% estimated these to occur on at least weekly and 6% on a daily basis.
Figure 1.
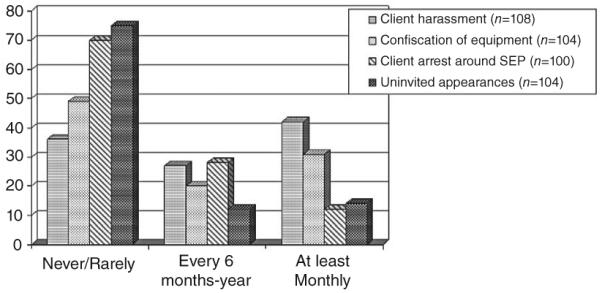
Percentage of syringe exchange programs (SEPs) reporting life-time frequency of events involving police
More than a quarter (28%) of the respondents reported client arrest en route to or from the exchange at least once or twice a year (Fig. 1), 12% estimated that this occurred at least monthly; only one program estimated client arrest to be a daily occurrence. Uninvited police appearances were the least frequent, with 12% estimating its occurrence once or twice a year, but 14 programs (14%) reported experiencing them at least monthly (Fig. 1). Just as a small core of programs claimed daily adverse events, a modest minority reported being completely free of police interference: The ‘never’ response was chosen by 11% of the programs on client harassment, 21% on unauthorized confiscation, 32% on client arrest and 55% on uninvited appearance items. The majority (56%) of respondent programs did not report having a system to document staff or client incidents involving police.
Bivariate regression analysis
Table 2 lists unadjusted odds ratios for the associations between program characteristics and interference meeting the cut-off (P < 0.10) for inclusion in further modeling. In these analyses, serving only urban areas, systematically documenting police interference and having more than three sites/week was associated significantly (P < 0.05) with increased frequency of client harassment. Exclusively targeting urban areas, operating more than three sites/week, serving primarily populations of color, systematically documented police interference and conducting mobile distribution was associated significantly with increased frequency of unauthorized syringe confiscation. Working only in urban areas, operating more sites per week, serving primarily minority clients and conducting mobile distribution were associated with reporting more frequent client arrests.
Table 2.
Unadjusted odds ratios representing the association between syringe exchange program (SEP) characteristics and adverse police encounters reported by US SEPs (n = 111).
|
Dependent variables |
||||
|---|---|---|---|---|
| Independent variables |
Client report of police harassment OR (95% CI); n |
Unauthorized confiscation of client syringes OR (95% CI); n |
Client arrests en route to or from SEP OR (95% CI); n |
Police appearances at SEP sites OR (95% CI); n |
| Modal race of SEP clients is African American or Hispanic |
2.29 (0.96–5.47); 92 | 3.40 (1.37–8.40); 88 | 3.56 (1.29–9.87); 86 | 4.32 (1.53–12.20); 90 |
| Only serving urban areas | 2.76(1.31–5.81); 107 | 2.34 (1.09–5.02); 101 | 3.24 (1.34–7.83); 99 | 3.14 (1.25–7.88); 103 |
| Providing mobile distribution | 2.03 (0.99–4.17); 106 | 2.32 (1.09–4.95); 100 | 2.20 (0.91–5.33); 98 | 6.11 (1.92–19.43); 102 |
| Providing stationary distribution |
0.43 (0.16–1.12); 92 | |||
| Located in Midwest | 0.43 (0.17–1.12); 97 | |||
| Not receiving state funds | 0.43 (0.20–0.94); 98 | |||
| Distributed more than 90 000/year syringes |
3.77 (1.24–11.53); 90 | |||
| Serving more than three sites | 3.96 (1.77–8.83); 92 | 2.62 (1.13–6.05); 86 | 5.26 (1.68–18.14); 90 | |
| Documenting problems with police |
2.16 (1.04–4.50); 109 | 2.67 (1.23–5.79); 109 | ||
| Number of years in operation | 5.25 (1.58–17.40); 102 | |||
CI: confidence interval; OR: odds ratio.
Similarly, serving only urban areas, more than three sites/week, non-white modal client race/ethnicity, higher number of syringes distributed, conducting distribution through a mobile exchange and longer history of operations was associated significantly with uninvited police appearances.
Remarkably, none of the three legal variables was associated with any of the interference outcomes. Similarly, the frequency of police action targeting clients and SEP operations did not vary significantly based on whether the SEP is operated by the Department of Health.
Multivariate logistic regression
In multivariate modeling, operation of more than three sites/week was associated independently with reporting more frequent client harassment [adjusted odds ratio (aOR) 3.96, 95% confidence interval (CI) 1.77–8.83)] (Table 3). Serving primarily non-white clients was associated independently with unauthorized confiscation (aOR 3.92, 95% CI 1.53–10.03) and client arrest en route to or from the SEP (aOR 3.56, 95% CI 1.29–9.87). Documenting police problems remained a significant correlate of unauthorized syringe confiscation (aOR 2.92, 95% CI 1.23–6.97). A greater number of years in operation was associated with a risk of uninvited police appearances at the SEP (aOR 4.74, 95% CI 1.36–16.56). Conversely, reporting stationary distribution was associated with a decreased risk of uninvited appearances by police (aOR 0.27, 95% CI 0.08–0.87).
Table 3.
Adjusted odds ratios representing the association between syringe exchange program (SEP) characteristics and adversepolice encounters reported by US SEPs (n = 111).
|
Dependent variables |
||||
|---|---|---|---|---|
| Independent variables |
Client report of police harassment aOR (95% CI) n |
Unauthorized confiscation of client syringes aOR (95% CI) n |
Client arrests en route to or from SEP aOR (95% CI) n |
Police appearances at SEP sites aOR (95% CI) n |
| Modal race of SEP clients is African American or Hispanic |
3.92 (1.53–10.03); 88 | 3.56 (1.29–9.87); 86 | ||
| Serving more than three sites | 3.96 (1.77–8.83); 92 | |||
| Documenting problems with police |
2.92 (1.23–6.97); 109 | |||
| Stationary distribution | 0.27 (0.08–0.87); 92 | |||
| Number of years in operation | 4.74 (1.36–16.56); 102 | |||
CI: confidence interval; aOR: adjusted odds ratio.
DISCUSSION
This is the first systematic survey addressing specifically the prevalence of and program characteristics associated with police practices targeting SEPs and their clients. The analysis supports our hypothesis that SEP authorization and laws governing syringe possession do not influence substantially the frequency of police interference. Gaps in street-level implementation of laws designed to improve syringe access [39] help to explain this finding and suggest that, without targeted efforts to change police policies and practices on the local level, formal legal reform alone may be insufficient to maximize the impact of SEPs and other interventions targeting IDUs.
Our findings also support the hypothesis that SEPs operated by health departments experience frequencies of police interference similar to other SEPs. This suggests that lateral communication between government agencies is not realized fully. Further, the results support the hypothesis that more visible programs—those serving more sites/week—are more likely to experience police interference. This may result from the larger geographic footprint of the programs, their visibility and their general ‘exposure’ to police activity.
That stationary exchanges experienced less frequent uninvited police appearances suggests that officers may be less likely to make unannounced visits if they know when and where SEPs are in operation. Consequently, programs may benefit from educating police about SEP locations and scheduling. Overall, communication and coordination between police and SEPs may reduce police interference, yielding improvements in overall effectiveness and cost-effectiveness [34]. This finding adds urgency to efforts to improve harmonization of effort between police and public health professionals. Closer analysis of SEPs at the extremes of the distribution continuum—those reporting very frequent or no problems with police (see Fig. 1)—can help to identify additional factors that shape such alignment. The latter group is especially notable, as it may represent SEPs already working in harmony with law enforcement agencies.
The greater risk of client arrest and unauthorized confiscation of injection equipment reported by SEPs serving primarily people of color underscores a pernicious disparity. This finding hints at a mechanism by which racial disparities in police interactions—such as stop-and-frisk searches, questioning and arrests—can deter participation in SEPs, and ultimately translate into elevated incidence of HIV infection in minority communities [49]. Further research is needed to examine how IDUs’ experience of these interactions and attitudes about police and criminal justice system influence the psychological, social, economic and other costs of participating in HIV prevention programs. In addition to the public health imperative to reduce HIV incidence, social justice concerns dictate increased emphasis upon and funding for empirical inquiry in this domain of health and human rights research. In view of mounting evidence that criminal justice involvement and adverse police events can influence HIV risk behavior [25-27], we advocate for the inclusion of items addressing this domain in behavioral surveillance surveys such as the US National HIV Behavioral Surveillance System, as well as in analogous international instruments.
Our finding that having a system for monitoring police events was associated with perceptions of more frequent interference may have a number of explanatory mechanisms. Some programs may institute a formal documentation policy as an institutional response to past adverse events and continue to experience higher levels of such events. Alternatively, these surveillance systems may be instituted on recommendations from oversight agencies or through horizontal knowledge exchange between SEPs. With data collection policies and systems in place, clients may be more likely to be prompted to report adverse events. In turn, these reports may be more likely to be captured, aggregated and discussed regularly than in settings without documentation systems. Collecting and tabulating adverse event data systematically may equip SEPs to engage in advocacy, litigation or other responsive activities that can help curb incidence, but the cross-sectional nature of this survey does not afford an opportunity to evaluate this effect. Future research should examine if, when and how programs use these data and whether having documentation systems influences adverse event incidence over time. Understanding what distinguishes programs that already collect this information and how these data are gathered and utilized can inform technical assistance efforts and funding priorities.
This research also dictates building a knowledge base about SEPs’ other responses to police interference and their ability to effectively prevent or address it. Measuring the influence of police-related experiential and attitudinal factors on SEP utilization necessitates triangulation. Such inquiry should include research with SEP clients, non-client IDUs and program staff, as well as police. Better understanding of these factors is antecedent to efforts to harmonize public health and criminal justice efforts [50].
This study has a number of limitations. Although our sample covers roughly two-thirds of all US SEPs, it is possible that some unaddressed factors distinguish responding programs, introducing sample bias and limiting generalizability. Despite the broad coverage, our sample size is relatively small; a larger sample, or a research design that directly captured individual clients’ experiences, could add statistical power to our multinomial regression analysis.
Our conclusions about the lack of association between the SEP’s legal environment and the perceived frequency of adverse police events should be interpreted in the context of a caveat: we utilized respondents’ report of the law, which may deviate from the jurisdictions’ actual laws. We identified minor discrepancies between states’ legal stance on syringe possession and responses given. It is beyond our capacity to determine such discrepancies on the local level. Policies regarding syringe possession are often conflicting and confusing, but these data suggest that SEP managers are not always optimally informed about the regulatory environment in which they operate.
Other limitations include definitional shortcomings within our instrument. For example, the term ‘police harassment’ may capture a broad range of subjective experience. Similarly, we assumed that uninvited police appearances at SEPs represent adverse events, but it is conceivable that such appearances may also represent neutral or positive interactions. Despite satisfactory piloting, the wording of some items may have been interpreted differentially by respondents. Another limitation is that three of the four outcomes reflect the SEP managers’ perceptions of client experience, which may underestimate the true levels for several reasons: (i) most programs report not collecting such data systematically; (ii) SEP managers do not always have direct, regular client contact; and (iii) client and staff attrition may mask the true incidence of adverse events, especially because only the experiences of those clients who continue to visit the SEP are captured. Although SEP managers are likely to be the ones to assess aggregate levels of police interference most accurately, assessing respondents’ years of service and connection to daily operations might have informed determination of potential biases. In the absence of a systematic nation-wide IDU survey on this topic, however, program managers’ reports serve as an important source of preliminary data.
CONCLUSION
Within a large national sample of US SEP operators, a substantial proportion reported a consistent burden of police interference, but the majority did not report having a system for documenting adverse events. Programs’ legal status, syringe possession laws and affiliation with the health department did not shape police interference significantly. Systematic surveillance of adverse events, along with client race, longer operation and program visibility were predictive of heavier burdens of interference, while having only stationary distribution had a protective effect. Findings underscore the importance of more systematic surveillance of key criminal justice-related events impacting population health, emphasis on evidence-based interventions to address these events and a better understanding of mechanisms that link racial disparities in criminal justice and public health domains. Priority should be placed on harmonizing HIV prevention and policing at a time when the number and scope of SEPs is likely to increase and Federal guidelines place expectations on programs to coordinate their efforts with local law enforcement [45]. The existence of programs that report no adverse events may represent a group of SEP already working in harmony with law enforcement agencies; such synergy carries a real potential to produce safer, healthier communities, while also realizing societal costsavings [51-54].
Acknowledgements
This work was supported, in part, by grants T32MH020031 and 2P30MH062294 from the National Institute of Mental Health and R01DA023408 from the National Institute on Drug Abuse. The content is solely the responsibility of the authors and does not necessarily represent the views of the National Institute of Mental Health or the National Institutes on Drug Abuse. The authors thank the Tides Foundation/DPA Rapid Response Grant program for supporting early survey development and Corey Davis, Esquire and Melissa Santos, who conducted preliminary survey efforts. We are indebted to Dr Des Jarlais and his colleagues at Beth Israel Medical Center, New York City for sharing unpublished data, as well as the team at the Harm Reduction Coalition, NASEN and SafetyWorks for recruitment assistance. Members of the CIRA postdoctoral fellowship program (T32MH020031) ably reviewed and commented on the manuscript.
Footnotes
Declarations of interest
The authors report no conflict of interest to any product or service mentioned in the paper.
References
- 1.Centers for Disease Control and Prevention [accessed 29 January 2009];Drug-Associated HIV Transmission Continues in United States: Fact Sheet. Available at: http://www.cdc.gov/hiv/resources/Factsheets/idu.htm. archived by WebCite® at http://www.webcitation.org/5tHzgQm1Z on 6 October 2010.
- 2.United Nations Joint Programme on HIV/AIDS (UNAIDS) AIDS Epidemic Update: 2007. UNAIDS; Geneva: 2007. [Google Scholar]
- 3.Needle RH, Kroeger K, Belani H, Hegle J. Substance abuse and HIV in Sub-Saharan Africa: introduction to the special issue. Afr J Drug Alcohol Stud. 2006;5:83–94. [Google Scholar]
- 4.Centers for Disease Control and Prevention Update to racial/ethnic disparities in diagnoses of HIV/AIDS—33 states, 2001–2005. Morb Mortal Wkly Rep. 2007;56:189–93. [PubMed] [Google Scholar]
- 5.United Nations Joint Programme on HIV/AIDS (UNAIDS) Criminalization of HIV Transmission. UNAIDS; Geneva: 2008. [Google Scholar]
- 6.Krieger N. Discrimination and Health. In: Berkman L, Kawachi I, editors. Social Epidemiology. Oxford University Press; New York: 2000. pp. 36–75. [Google Scholar]
- 7.Friedman SR, Furst RT, Jose B, Curtis R, Neaigus A, Des Jarlais DC, et al. Drug scene roles and HIV risk. Addiction. 1998;93:1403–16. doi: 10.1046/j.1360-0443.1998.939140311.x. [DOI] [PubMed] [Google Scholar]
- 8.Academy for Educational Development . A Comprehensive Approach: Preventing Blood-Borne Infections Among Injection Drug Users. Academy for Educational Development; Washington, DC: 2000. [Google Scholar]
- 9.Coyle SL, Needle RH, Normand J. Outreach-based HIV prevention for injecting drug users: a review of published outcome data. Public Health Rep. 1998;113:19–30. [PMC free article] [PubMed] [Google Scholar]
- 10.Ksobiech KA. Meta-analysis of needle sharing, lending, and borrowing behaviors of needle exchange program attenders. AIDS Edu Prev. 2003;15:257–68. doi: 10.1521/aeap.15.4.257.23828. [DOI] [PubMed] [Google Scholar]
- 11.Des Jarlais DC. Structural interventions to reduce HIV transmission among injecting drug users. AIDS. 2000;14:S41–6. doi: 10.1097/00002030-200006001-00006. [DOI] [PubMed] [Google Scholar]
- 12.Csete J. [accessed 14 February 2009];Do Not Cross: Policing and HIV Risk Faced by People Who Use Drugs. Available at: http://www.aidslaw.ca/publications/interfaces/downloadFile.php?ref=1080. archived by WebCite® at http://www.webcitation.org/5tHzq5Qgf on 6 October 2010.
- 13.Lazzarini Z, Bray S, Burris S. Evaluating the impact of criminal laws on HIV risk behavior. J Law Med Ethics. 2002;30:239–53. doi: 10.1111/j.1748-720x.2002.tb00390.x. [DOI] [PubMed] [Google Scholar]
- 14.Bluthenthal RN, Kral AH, Erringer EA, Edlin BR. Drug paraphernalia laws and injection-related infectious disease risk among drug injectors. J Drug Issues. 1999;29:1–16. [Google Scholar]
- 15.Koester S. The prevalence of additional injection-related HIV risk behaviors among injection drug users. J Acquir Immune Defic Syndr. 1996;12:202–7. doi: 10.1097/00042560-199606010-00015. [DOI] [PubMed] [Google Scholar]
- 16.Doe v. Bridgeport Police Department, 198 F.R.D. 325 (US Dist 2001).
- 17.Roe v. City of New York, 240 (S.D. N.Y. 2002).
- 18.Friedman SR, Cooper HL, Tempalski B, Keem M, Friedman R, Flom PL, et al. Relationships of deterrence and law enforcement to drug-related harms among drug injectors in US metropolitan areas. AIDS. 2006;20:93–9. doi: 10.1097/01.aids.0000196176.65551.a3. [DOI] [PubMed] [Google Scholar]
- 19.Cooper H, Moore L, Gruskin S, Krieger N. Characterizing perceived police violence: implications for public health. Am J Public Health. 2004;94:1109–18. doi: 10.2105/ajph.94.7.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cooper H, Moore L, Gruskin S, Krieger N. The impact of a police drug crackdown on drug injectors’ ability to practice harm reduction: a qualitative study. Soc Sci Med. 2005;61:673–84. doi: 10.1016/j.socscimed.2004.12.030. [DOI] [PubMed] [Google Scholar]
- 21.Davis C, Burris S, Metzger D, Becher J, Lynch K. Effects of an intensive street-level police intervention on syringe exchange program utilization: Philadelphia, Pennsylvania. Am J Public Health. 2005;95:233–36. doi: 10.2105/AJPH.2003.033563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aitken C, Moore D, Higgs P, Kelsall J, Kerger M. The impact of a police crackdown on a street drug scene: evidence from the street. Int J Drug Policy. 2002;13:189–98. [Google Scholar]
- 23.Blankenship K, Koester S. Criminal law, policing policy, and HIV risk in female street sex workers and injection drug users. J Law Med Ethics. 2002;30:548–59. doi: 10.1111/j.1748-720x.2002.tb00425.x. [DOI] [PubMed] [Google Scholar]
- 24.Blankenship K, Smoyer A, editors. Public Health, Research and Law Enforcement: The Case of HIV/AIDS Prevention. Yale University: Centre for Interdisciplinary Research on AIDS; 2004. [Google Scholar]
- 25.Kerr T, Small W, Wood E. The public health and social impacts of drug market enforcement: a review of the evidence. Int J Drug Policy. 2005;16:210–20. [Google Scholar]
- 26.Rhodes T, Mikhailova L, Sarang A, Lowndes CM, Rylkov A, Khutorskoy M, et al. Situational factors influencing drug injecting, risk reduction and syringe exchange in Togliatti City, Russian Federation: a qualitative study of micro risk environment. Soc Sci Med. 2002;57:39–54. doi: 10.1016/s0277-9536(02)00521-x. [DOI] [PubMed] [Google Scholar]
- 27.Grund J-PC, Heckathorn DD, Broadhead RS. In A. D. Eastern connecticut, IDUs purchase syringes from pharmacies but don’t carry syringes (Letter) J Acquir Immune Defic Syndr. 1995:104–05. doi: 10.1097/00042560-199509000-00016. [DOI] [PubMed] [Google Scholar]
- 28.Blankenship KM, Mattocks K, Stolar M. Drug policy, incarceration and black–white disparities in HIV/AIDS; Paper presented at 131st Annual Meeting of the American Public Health Association; San Francisco, CA. 2003. [Google Scholar]
- 29.Iguchi MY, Bell J, Ramchand RN, Fain T. How criminal system racial disparities may translate into health disparities. J Health Care Poor Underserv. 2005;16.4:48–56. doi: 10.1353/hpu.2005.0114. [DOI] [PubMed] [Google Scholar]
- 30.Shannon K, Kerr T, Allinott S, Chettiar J, Shoveller J, Tyndall MW. Social and structural violence and power relations in mitigating HIV risk of drug-using women in survival sex work. Soc Sci Med. 2008;66:911–21. doi: 10.1016/j.socscimed.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 31.Hammett T, Bartlett N, Chen Y, Ngud D, Cuonge DD, Phuonge NM, et al. Law enforcement influences on HIV prevention for injection drug users: observations from a cross-border project in China and Vietnam. Int J Drug Policy. 2005;16:235–45. [Google Scholar]
- 32.Small W, Kerr T, Charette J, Schechter MT, Spittal PM. Impacts of intensified police activity on injection drug users: evidence from an ethnographic investigation. Int J Drug Policy. 2006;17:85. [Google Scholar]
- 33.Cooper HLF, Wypij D, Krieger N. Police drug crackdowns and hospitalisation rates for illicit-injection-related infections in New York City. Int J Drug Policy. 2005;16:150. [Google Scholar]
- 34.DeBeck K, Wood E, Zhang R, Tyndall M, Montaner J, Kerr T. Police and public health partnerships: evidence from the evaluation of Vancouver’s supervised injection facility. Subst Abuse Treat Prev Policy. 2008;3:11. doi: 10.1186/1747-597X-3-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O’Keefe E. Altering public policy on needle exchange: the Connecticut experience. AIDS Public Policy J. 1991;6:159–64. [Google Scholar]
- 36.Burris S, Lurie P, Ng M. Harm reduction in the health care system: the legality of prescribing and dispensing syringes to drug users. Health Matrix. 2001;11:5–64. [PubMed] [Google Scholar]
- 37.Bray S, Lawson J, Heimer R. Doffing the cap: increasing syringe availability by law but not in practice. Int J Drug Policy. 2001;12:221–35. [Google Scholar]
- 38.Burris S, Blankenship KM, Donoghoe M, Blankenship K, Sherman S, Vernick JS, et al. Addressing the ‘risk environment’ for injection drug users: the mysterious case of the missing cop. Milbank Q. 2004;82:125–56. doi: 10.1111/j.0887-378X.2004.00304.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Beletsky L, Macalino G, Burris S. Attitudes of police officers towards syringe access, occupational needle-sticks, and drug use: a qualitative study of one city police department in the United States. Int J Drug Policy. 2005;16:267–74. [Google Scholar]
- 40.Maher L, Dixon D. Policing and public health: law enforcement and harm minimization in a street-level drug market. Br J Criminol. 1999;39:488–512. [Google Scholar]
- 41.Martinez AN, Bluthenthal RN, Lorvick J, Anderson R, Flynn N, Kral AH. The impact of legalizing syringe exchange programs on arrests among injection drug users in California. J Urban Health. 2007;84:423–35. doi: 10.1007/s11524-006-9139-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Heimer R, Bluthenthal RN, Singer M, Khoshnood K. Structural impediments to operational syringe-exchange programs. AIDS Public Policy J. 1996;11:169–84. [PubMed] [Google Scholar]
- 43.Bluthenthal RN, Heinzerling KG, Anderson R, Flynn NM, Kral AH. Approval of syringe exchange programs in California: results from a local approach to HIV prevention. Am J Public Health. 2007:278–83. doi: 10.2105/AJPH.2005.080770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Des Jarlais D, McKnight C, Goldblatt C, Purchase D. Doing harm reduction better: syringe exchange in the United States. Addiction. 2009;104:1447–8. doi: 10.1111/j.1360-0443.2008.02465.x. [DOI] [PubMed] [Google Scholar]
- 45.Centers for Disease Control and Prevention [accessed 16 July 2010];Interim Syringe Exchange/Acces Guidelines. 2010 Available at: http://www.cdc.gov/hiv/resources/guidelines/PDF/SSPguidanceacc.pdf. archived by WebCite® at http://www.webcitation.org/5tHzz7IRG on 6 October 2010.
- 46.StataCorp. STATA Statistical Software: Release 10. Stata Corporation; College Station, TX: 2007. [Google Scholar]
- 47.Williams R. Generalized ordered logit/partial proportional odds models for ordinal dependent variables. Stata J. 2006;6:58–82. [Google Scholar]
- 48.Sharon S. Ban lifted on federal funding for needle exchange. National Public Radio; Dec 18, 2009. Available at http://www.npr.org/templates/story/story.php?storyId=121511681 (Archived by WebCite® at http://www.webcitation.org/5tI2bfvd7 on 6 October 2010) [Google Scholar]
- 49.Beckett K, Nyrop K, Pfingst L. Race, drugs, and policing: understanding disparities in drug delivery arrests. Criminology. 2006;44:230–42. [Google Scholar]
- 50.Davis C, Beletsky L. Bundling occupational safety with harm reduction information as a feasible method for improving police receptiveness to syringe access programs: evidence from three U.S. cities. Harm Reduct J. 2009;6:1–18. doi: 10.1186/1477-7517-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lasker RD, Weiss ES, Miller R. Partnership synergy: a practical framework for studying and strengthening the collaborative advantage. Milbank Q. 2001;79:179–205. doi: 10.1111/1468-0009.00203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hammett TM, Harmon MP, Rhodes W. The burden of infectious disease among inmates of and releasees from US correctional facilities, 1997. Am J Public Health. 2002;92:1789–94. doi: 10.2105/ajph.92.11.1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Burris S. From security to health. In: Woods J, Dupont B, editors. Democracy and the Governance of Security. Cambridge University Press; Cambridge: 2006. pp. 196–216. [Google Scholar]
- 54.Burris S, Strathdee S. To serve and protect? Toward a better relationship between drug control policy and public health. AIDS. 2006;20:117–18. doi: 10.1097/01.aids.0000194806.81917.19. [DOI] [PubMed] [Google Scholar]


