Abstract
Mongrel or beagle dogs were submitted to bile duct ligation, or to extraenteric biliary diversion by means of choledochoureterostomy. The kinetics of intravenously administered FK506 was not changed from control status two weeks after bile duct ligation, but the bioavailability of orally administered FK506 was nearly quadrupled. Following oral administration, the absorption of FK508 was highly variable. The results indicate that in dogs FK506 is absorbed from the intestine just as efficiently in the absence of enteric bile and in presence of exogenous bile salt supplement when compared with its absorption in presence of normal bile drainage. These findings with FK506 are different from those with cyclosporine after biliary obstruction or diversion and will have important practical as well as experimental ramifications.
The immunosuppressive agent, FK506, (1) is a macrocyclic lactone that is highly lipid soluble. This drug is an effective immunosuppressant in rats, dogs, monkeys, baboons, and humans after liver, kidney or heart transplantation (2). FK506 is largely metabolized by the liver prior to elimination from the body (3) and the status of the liver is expected to influence its elimination. Since liver dysfunction or bile duct ligation decreases the availability of bile salts for solubilization of lipid soluble drugs, normal biliary drainage was predicted to be an important condition for the optimal absorption of FK506, as is the case with absorption of oral cyclosporine (4). In the present study, this expectation could not be supported in dogs submitted to bile duct ligation or extraenteric biliary diversion.
MATERIALS AND METHODS
Bile duct ligation
Five female mongrel dogs weighing between 18 and 22 kg and six female beagle dogs weighing between 8 and 10 kg were maintained in a 12-hr light-dark cycle from 7 A.M. to 7 P.M. On the day of the study the dogs were fasted overnight and for 4 hr after drug administration. Water was allowed ad libitum. Intravenous FK506 was diluted in normal saline and administered as a bolus (0.2 mg/kg) over 15 secs. Blood samples were obtained immediately before and 5, 10, 15, 30, 45 min after the bolus. Later, samples were obtained at 1, 2, 3, 4, 6, 8, 12, 18, 24, and 30 hr. Three days after the i.v. study, oral FK506 (1 mg/kg) was administered in a hard gelatin capsule. Blood samples were drawn before treatment, 15, 30, and 45 min afterward, and later at 1, 2, 3, 4, 6, 8, 12, 16, 24, and 30 hr.
Five days later, the common bile and cystic ducts were doubly ligated and divided under general anesthesia with pentobarbital-halothane anesthesia. The animals were given 1 g/day intramuscular cefamandole for three days postoperatively. Then 14 days later, the FK506 kinetic studies were performed in the same way as described preoperatively.
Biliary diversion with choledochoureterostomy
Female beagle dogs (n=6) weighing approximately 10 kg and with the conditions described above were given an oral dose of 1 mg/kg FK506 and blood samples were obtained at 0, 0.25, 0.5, 0.75, 1, 2, 3, 4, 6, 8, 12, 16, and 24 hr. Three days later, the dogs received 1 mg/kg of FK506 orally, 15 min after 1 g of lecithin and 250 mg of chenodeoxycholic acid, and FK506 kinetics was studied as described earlier. Nine days later, choledochoureterostomy was performed after right nephrectomy, using a previously described technique (5). Intramuscular cefamandole was used as in the previous section. Two weeks after biliary diversion, the oral FK506 absorption study was repeated, first with out any exogenous bile supplement and three days later, after administration of 250 mg chenodeoxycholic acid and 1 g lecithin.
Blood samples were centrifuged at room temperature and the plasma was frozen at −70°C until analyzed for FK506. The FK506 concentration was measured in plasma by Tamura's enzyme immunoassay method (6). This assay has a coefficient of variation of 22% at 0.5 ng/ml and 10% at 2.1 ng/ml. Liver function tests were carried out at the outset, and at the time of the subsequent studies.
The plasma concentration time curve was analyzed by standard techniques (7). Statistical Analysis was carried out using a nonparametric test (Mann Whitney's U test), t test, or ANOVA as appropriate, with P<0.05 being statistically significant.
RESULTS
Bile duct ligation
Serum GOT, GPT, alkaline phosphatase, and total bilirubin were in the normal range before bile duct ligation and were elevated in all of the doge after bile duct ligation (Table 1). While serum creatinine was lower after surgery, the BUN was normal throughout. Table 2 describes the biochemical parameters in dogs before and after biliary diversion. While the serum GOT and GPT were normal after biliary diversion, alkaline phosphatase and total bilirubin were slightly elevated after surgery, indicating minimal changes in the hepatic function.
Table 1.
Biochemical parameters in dogs before and after bile duct ligation (n = 11)
| Preoperative | Postoperative | P value | |
|---|---|---|---|
| SGOT (IU/L) | 33±11a | 357±251 | <0.05 |
| SGPT (IU/L) | 33±7 | 2707±1556 | <0.05 |
| Alkaline phosphatase (IU/L) | 61±36 | 6549±3061 | <0.05 |
| Total bilirubin (mg%) | 0.2±0.1 | 5.7±2.6 | <0.05 |
| Serum creatinine (mg%) | 1.1±0.3 | 0.8±0.2 | <0.05 |
| BUN | 13±3 | 11±4 | NSb |
| Total proteins (g%) | 5.5±0.6 | 6.2±0.5 | <0.05 |
| Albumin (g%) | 3.7±0.4 | 3.6±0.4 | NS |
Mean ± SD.
(NS) not significant.
Table 2.
Biochemical parameters in dogs before and after biliary diversion (n = 6)
| Preoperative | 14-day Postoperative | P value | |
|---|---|---|---|
| SGOT (IU/L) | 36±10a | 44±27 | NSb |
| SGPT (IU/L) | 36±18 | 144±174 | NS |
| Alkaline phosphate (IU/L) | 36±3 | 415±155 | <0.05 |
| Total bilirubin (mg%) | 0.1±0.1 | 0.3±0.2 | <0.05 |
| Serum Creatinine (mg%) | 1.1±0.1 | 1.2±0.2 | NS |
| BUN | 13±4 | 23±6 | <0.05 |
| Total proteins (g%) | 6.2±0.3 | 5.9±0.7 | NS |
| Albumin (g%) | 4.0±0.3 | 3.4±0.4 | <0.05 |
Mean ± SD.
(NS) not significant.
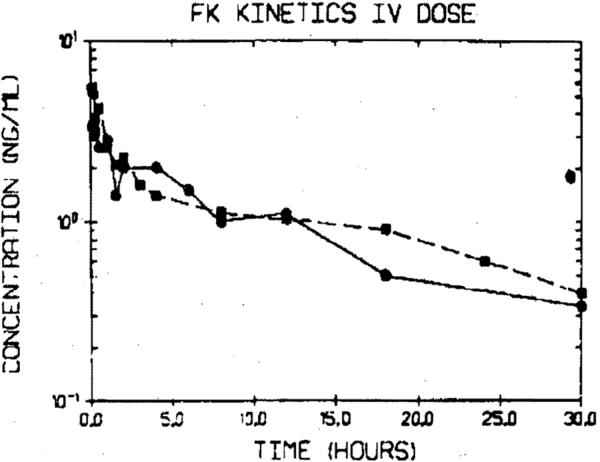
The plasma concentration–versus–time curve following intravenous administration of FK506 to a mongrel dog (No. 6) before and after bile duct ligation is shown in Figure 1. The kinetics of FK506 in dogs can be adequately described by a two-compartment model, with a rapid initial distribution phase followed by a slower disposition phase. The pharmacokinetic parameters calculated after i.v. FK506 are shown in Tables 3 and 4 for mongrel and beagle dogs, before and after bile duct ligation. Bile duct ligation did not significantly alter the disposition rate constant, half life, or the plasma clearance of FK506 in this group of dogs. However, the volume of distribution of FK506 was significantly increased in the mongrel dogs after bile duct ligation (P<0.05).
Figure 1.
Plasma concentration-versus-time curve following an intravenous dosing (0.2 mg/kg) in mongrel dog No. 6 before (●) and after (∎) bile duct ligation.
Table 3.
FK506 pharmacokinetics (i.v.) in mongrel dogs before and after bile duct ligation
| Dog No. | Disposition rate constant (hr−1) |
Half-life (hr) |
Clearance (ml/min) |
Volume of distribution at steady state |
||||
|---|---|---|---|---|---|---|---|---|
| Pre. | Post. | Pre. | Post. | Pre. | Post. | Pre. | Post. | |
| 1 | 0.0757 | 0.0677 | 9.2 | 10.2 | 2239 | 2699 | 1385 | 2240 |
| 3 | 0.0527 | 0.0475 | 13.2 | 14.6 | 1943 | 1665 | 1972 | 1928 |
| 4 | NDa | 0.0943 | ND | 7.4 | ND | ND | ND | 2384 |
| 5 | 0.0769 | 0.1112 | 9.0 | 6.2 | 3125 | 4072 | 1446 | 2040 |
| 6 | 0.0720 | 0.0688 | 9.6 | 10.1 | 1992 | 3750 | 1801 | 2040 |
| Mean | 0.0693 | 0.0779 | 10.3 | 9.7 | 2325 | 3047 | 1651 | 2324 |
| SD | ±0.0098 | ±0.0223 | ±1.7 | ±2.9 | ±475 | ±945 | ±282 | ±386b |
(ND) not determined.
Significantly different from the control values (p<0.05).
Table 4.
FK506 kinetics (i.v.) in beagle dogs before and after bile duct ligation
| Dog No. | Disposition rate constant (hr−1) |
Half-life (hr) |
Clearance (ml/min) |
|||
|---|---|---|---|---|---|---|
| Pre. | Post. | Pre. | Post. | Pre. | Post. | |
| 1 | 0.1115 | 0.0550 | 6.2 | 13.5 | 315 | 251 |
| 2 | 0.1166 | 0.0530 | 6.0 | 13.1 | 366 | 313 |
| 3 | 0.1312 | 0.0860 | 5.3 | 8.1 | 296 | 347 |
| 4 | 0.0400 | 0.0644 | 17.3 | 10.8 | 253 | 400 |
| 6 | 0.0858 | 0.0586 | 8.1 | 11.8 | 368 | 249 |
| Mean | 0.10 | 0.06 | 8.6 | 11.5 | 320 | 312 |
| SD | ±0.04 | ±0.01 | ±5.0 | ±2.2 | ±49 | ±65 |
| P | NS | NS | NS | |||
The plasma concentration–versus–time curve following oral administration of FK506 to dog No. 3 before and after bile duct ligation is shown in Figure 2. The pharmacokinetic parameters calculated in five mongrel and six beagle dogs after oral administration are listed in Tables 5 and 6. These results indicate a rapid absorption of FK506, with a mean peak plasma concentration of 2.8 (+ 1.1) and 7.8 (+2.0) ng/ml being reached in 1.2–1.3 hr. After bile duct ligation, the disposition rate constant, half-life, and the time to reach peak plasma concentrations were significantly altered while peak plasma concentrations were not different. More importantly, there was a significant increase in the area under the plasma concentration–versus–time curve (AVC). Consequently, the oral bioavailability of FK506 in bile duct ligated animals was significantly higher (3–4-fold) than that observed in normal animals.
Figure 2.
Plasma concentration versus-time-curve following oral administration (1 mg/kg) in mongrel dog No. 6 before (●) and after (∎) bile duct ligation.
Table 5.
Oral FK506 kinetics in mongrel dogs before and after bile duct ligation
| Dog No. | Disposition rate constant (hr−1) |
Half-life (hr) |
Maximum plasma concentration (ng/ml) |
Time to reach maximum plasma concentration (hr) |
Bioavail-ability (%) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre. | Post. | Pre. | Post. | Pre. | Post. | Pre. | Post. | Pre. | Post | |
| 1 | 0.096 | 0.042 | 7.2 | 16.5 | 1.9 | 4.0 | 2 | 4 | 9 | 56 |
| 3 | 0.120 | 0.096 | 5.8 | 7.2 | 2.3 | 11.3 | 1 | 2 | 9 | 42 |
| 4 | 0.123 | 0.066 | 5.6 | 10.4 | 2.8 | 3.2 | 1 | 4 | — | 21 |
| 5 | 0.088 | 0.087 | 7.9 | 8.0 | 4.9 | 1.8 | 1 | 3 | 12 | 23 |
| 6 | 0.114 | 0.084 | 6.1 | 8.2 | 2.5 | 3.1 | 2 | 6 | 5 | 60 |
| Mean | 0.114 | 0.075a | 6.5 | 10.1a | 2.9 | 4.7 | 1.4 | 3.8a | 9 | 40a |
| SD | ±0.002 | ±0.021 | 0.9 | 3.8 | ±1.2 | ±3.8 | ±0.55 | ±1.55 | ±3 | ±16 |
Significantly different from Pre. values (P<0.05).
Table 6.
Oral FK506 kinetics in beagle dogs before and after bile duct ligation
| Dog No. | Disposition rate constant (hr−1) |
Half-life (hr) |
Maximum plasma concentration (ng/ml) |
Time to reach maximum plasma concentration (hr) |
Bioavail-ability (%) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre. | Post. | Pre. | Post. | Pre. | Post. | Pre. | Post. | Pre. | Post. | |
| 1 | 0.0778 | 0.0962 | 8.9 | 7.2 | 10.2 | 29.2 | 2 | 2 | 8.8 | 33.3 |
| 2 | 0.1135 | 0.104 | 6.1 | 6.7 | 4.0 | 8.8 | 0.75 | 2 | 3.6 | 17.8 |
| 3 | 0.0498 | 0.118 | 13.9 | 5.9 | 4.2 | 8.7 | 2 | 3 | 4.7 | 19.1 |
| 4 | 0.0794 | 0.1166 | 8.7 | 5.9 | 9.2 | 8.3 | 0.75 | 1 | 6.1 | 13.3 |
| 5 | 0.0562 | 0.1210 | 12.3 | 5.8 | 8.6 | 8.8 | 1.0 | 4 | — | 20.5 |
| 6 | 0.0691 | 0.0983 | 10.0 | 7.1 | 10.6 | 14.6 | 0.5 | 2 | 9.2 | 26.1 |
| Mean | 0.07 | 0.11a | 10.0 | 6.4a | 7.8 | 13.1 | 1.2 | 2.3a | 6.5 | 21.7a |
| SD | ±0.02 | ±0.01 | 2.8 | 0.6 | ±2.0 | ±8.3 | ±0.07 | ±1.0 | ±2.5 | ±7.0 |
Significantly different from Pre. values (P<0.05).
Clwledoclwureterostomy
Two weeks after this operation, all 6 of the dogs had near-normal liver function tests. They were all eating and healthy. Biliary diversion or addition of exogenous bile salts did not result in any significant changes in the peak plasma concentrations, half-life, or the AVC after oral FK506 administration. The time to reach peak plasma concentration was, however, increased significantly after biliary diversion (Table 7).
Table 7.
Effect of biliary diversion and bile salt supplementation on FK506 oral absorption
| Peak concentration (ng/ml) | Time to peak (hr) | (AUC) (mg/ml/hr) | Half-life (hr) | |
|---|---|---|---|---|
| Control | 10.9±7.5 | 1.1±0.9 | 44.4±38.1 | 8.9±1.7 |
| Control and bile salt | 11.9±10.9 | 0.9±0.2 | 36.4±25.9 | 8.7±2.1 |
| Biliary diversion | 5.4±3.1 | 2.3±1.0a | 33.3±20.0 | 9.8±1.8 |
| Biliary diversion and bile salt | 7.2±3.5 | 2.2±1.0a | 38.6±26.2 | 9.7±1.5 |
Significantly different from the control animals (P<0.05).
DISCUSSION
The pharmacokinetics of intravenous FK506 were altered very little by bile duct ligation. This is different from the effect of bile duct ligation on cyclosporine, which has a reduced elimination under these circumstances (8). The difference between the 2 drugs given intravenously requires explanation since both agents are very lipid-soluble and are eliminated primarily by hepatic metabolism (3, 4). However, cyclosporine is cleared slowly from the body and thus is classified as a “low-clearance” drug, whereas FK506 has a plasma clearance that is actually higher than the hepatic blood flow.
The 2-week period of bile duct ligation probably caused minimal impairment of the hepatic blood flow in these dogs in spite of the significant but moderate hepatic injury that was measurable by standard liver function tests. Since FK506 appears to be a high-clearance drug and its elimination after i.v. administration depends on hepatic blood flow, severe liver dysfunction leading to reduced hepatic blood flow would be expected eventually to be a factor that would decrease the elimination of intravenously administered FK506. Apparently, this had not yet occuned within 14 days of duct ligation in both mongrel and beagle dogs.
In contrast to the minimum changes in intravenous pharmacokinetics, the oral pharmacokinetics of FK506 were drastically altered by bile duct ligation. The time to reach peak plasma FK506 concentrations and the bioavailability were significantly increased. Again, this was an unexpected finding since the bioavailability of orally administered cyclosporine is greatly reduced after bile duct ligation (8). It is possible that presystemic metabolism of FK506 is impaired in animals after bile duct ligation resulting in increased oral bioavailability. It was not possible to explain these paradoxical results completely without further experimentation in additional dogs who had pure biliary diversion, which was done with choledochoureterostomy. This procedure eliminated the potential artifact of liver injury caused by duct ligation; hepatic function tests were minimally altered, and the livers were histopathologically normal at 2 weeks. Biliary diversion by itself did not significantly alter the extent of absorption of FK506. The increased time to reach peak FK506 plasma concentrations following biliary diversion presumably indicates a decreased rate of absorption of FK506. Addition of bile salts in the presence or in the absence of endogenous bile did not alter the extent of FK506 absorption.
Taking the biliary obstruction and diversion experiments together, the results indicate that absorption of FK506, in contrast to that of cyclosporine, which is bile salt-dependent (8–10), is actually not significantly altered by the absence of bile. The differential effect of bile on FK506 and cyclosporine absorption can be rationalized as follows. The dose of FK506 (about 0.15 mg/kg) is nearly one-fiftieth of that of cyclosporine (about 7.5 mg/kg). The fluid volume in the gut is sufficient to dissolve FK506 from the solid dispersion formulation and bile contributes minimally to FK 506 dissolution. On the other hand, bile is necessary for solubilizing the administered dose of cyclosporine and lack of bile results in decreased cyclosporine absorption.
Much further work will be required before the full explanation for this unexpected finding can be delineated. However, it is clear at a practical level that the assumption that past practices with cyclosporine will be applicable to oral FK506 administration are unwarranted. When the draining T tube of a patient on oral cyclosporine is clamped, it is necessary to reduce the dosage in order to prevent augmented absorption and consequent large increases in cyclosporine blood levels (11). It has already been noted in similar patients treated with FK506 that downward adjustments in FK506 dosages are not required (12, 13).
Footnotes
This work was supported by Research Grants from the Veterans Administration and by Project Grant OK 29961 from the National Institutes of Health, Bethesda, Maryland
REFERENCES
- 1.Kino T, Hatanaka H, Miyata S, et al. FK-506, a novel immunosuppressant isolated from a streptomyces: II. Immunosuppressive effect of FK-506 in vitro. J Antibiot (Tokyo) 1987;40:1249. doi: 10.7164/antibiotics.40.1256. [DOI] [PubMed] [Google Scholar]
- 2.Starzl TE, Todo S, Fung JJ, Groth C, editors. Transplant Proc. Vol. 22. 1990. FK 506, a potential breakthrough in immunosuppression—clinical implications; p. 5. [Google Scholar]
- 3.Venkataramanan R, Jain AB, Cadoff E, et al. Pharmacokinetics of FK 506: preclinical and clinical studies. Transplant Proc. 1990;22:52. [PMC free article] [PubMed] [Google Scholar]
- 4.Ptachcinski RJ, Venkataramanan R, Burckart GJ. Clinical pharmacokinetics of cyclosporin. Clin Pharmacol. 1986;11:107. doi: 10.2165/00003088-198611020-00002. [DOI] [PubMed] [Google Scholar]
- 5.Furukawa H, Todo S, Imventarza O, Wu YM, Starzl TE. Tube choledochoureterostomy: a simple method for bile diversion. J Surg Invest. 3:115. doi: 10.3109/08941939009140341. 199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tamura K, Kobayashi K, Hashimoto K, et al. A highly sensitive method to assay FK 506 levels in plasma. Transplant Proc. 1987;19:23. [PubMed] [Google Scholar]
- 7.Gibaldi M, Perrier D. Pharmacokinetics. 2nd ed. Marcel Dekker; New York: 1985. [Google Scholar]
- 8.Takaya S, Iwatsuki S, Starzl TE, et al. Experimental study about the influence of liver dysfunction upon cyclosporine pharmacokinetics. Transplant Proc. 1988;20(suppl 1):154. [Google Scholar]
- 9.Ericson BG, Todo S, Lynch S, et al. Role of bile and bile salts on cyclosporine absorption in dogs. Transplant Proc. 1987;19:1248. [PMC free article] [PubMed] [Google Scholar]
- 10.Venkataramanan R, Diliz-Perez H, Schwinghammer T, et al. Effect of bile on cyclosporine absorption in dogs. Res Commun Chem Pathol Pharmacol. 1986;53:137. [PMC free article] [PubMed] [Google Scholar]
- 11.Andrews W, Iwatauki S, Shaw B, Jr, Starzl TE. Bile diversion and cyclosporine dosage [Letter] Transplantation. 1985;39:338. [PubMed] [Google Scholar]
- 12.Jain AB, Venkataramanan R, Cadoff E, et al. Effect of hepatic dysfunction and T tube clamping on FK 506 pharmacokinetics and trough concentrations. Transplant Proc. 1990;22:57. [PMC free article] [PubMed] [Google Scholar]
- 13.Venkataramanan R, Jain AB, Warty VS, et al. Pharmacokinetics of FK 506 following oral administration: a comparison of FK 506 and cyclosporine. Transplant Proc. 1991;23:931. [PMC free article] [PubMed] [Google Scholar]