Abstract
Astract
Background
Streptococcus suis serotype 2 (SS2), a major swine pathogen and an emerging zoonotic agent, has greatly challenged global public health. Systematical information about host immune response to the infection is important for understanding the molecular mechanism of diseases.
Results
104 and 129 unique genes were significantly up-regulated and down-regulated in the spleens of pigs infected with SS2 (WT). The up-regulated genes were principally related to immune response, such as genes involved in inflammatory response; acute-phase/immune response; cell adhesion and response to stress. The down-regulated genes were mainly involved in transcription, transport, material and energy metabolism which were representative of the reduced vital activity of SS2-influenced cells. Only a few genes showed significantly differential expression when comparing avirulent isogenic strain (ΔHP0197) with mock-infected samples.
Conclusions
Our findings indicated that highly pathogenic SS2 could persistently induce cytokines mainly by Toll-like receptor 2 (TLR2) pathway, and the phagocytosis-resistant bacteria could induce high level of cytokines and secrete toxins to destroy deep tissues, and cause meningitis, septicaemia, pneumonia, endocarditis, and arthritis.
Background
Streptococcus suis (S. suis) is an important pathogen associated with many diseases in pigs, including meningitis, septicaemia, pneumonia, endocarditis, and arthritis. S. suis serotype 2 (SS2) is considered the most pathogenic as well as the most prevalent capsular type among thirty-three serotypes (types 1 to 31, 33, and 1/2) in diseased pigs, and it is also the causative agent of serious infections in humans, especially in people in close contact with pig or pork byproducts [1-3]. Two recent large-scale outbreaks of human SS2 epidemics in China (one had 25 cases with 14 deaths in Jiangsu in 1998, the second had 204 cases with 38 deaths in Sichuan in 2005), featured clinical streptococcal toxic shock syndrome, have greatly challenged the global public health [4-7]. Recently, S. suis infection has also caused sporadic human illness in other countries, including Thailand [8,9], United Kingdom [10], Portugal [11], Australia [12], Netherlands [13] and United States [14,15], and been recognized as the third most common cause of community acquired bacterial meningitis in Hong Kong and as the leading cause of adult meningitis in Vietnam [5,16].
The past pathogenesis studies were performed mainly on the pathogenic bacteria and as a result, a few virulence-associated factors have been successfully identified. Polysaccharide capsule has been considered essential for the virulence of the bacterium [17,18], and other factors, such as suilysin, the so-called extracellular protein factor and muramidase-released protein have been shown to be linked to, but not essential for the full virulence of S. suis [19]. GapdH[20], Enolase[21,22], FbpS[19], Adhesin [23-27] have been proved to be involved in the adherence and virulence of S. suis. Recently, serum opacity-like factor [28], IgA1 protease[29], D-Alanylation of Lipoteichoic Acid [30] and pgdA [31] were identified as important factors in S. suis virulence. In addition, SalK/SalR [32] and CovR [33] were found to affect the virulence of S. suis Chinese isolates. These studies have contributed to the understanding of S. suis pathogenesis and also suggested that host responses also play essential roles in the development of the diseases.
Inducing excessive inflammation is recognized as one of the reasons why highly invasive SS2 strain could cause severe diseases [31,34]. A few previous studies indicated that high level of cytokines and chemokines could be released by human brain microvascular endothelial cells [35], a whole-blood culture system [36], macrophages [37] and monocytes [38] stimulated by SS2, and have important roles in the initiation and development of inflammation and meningitis [39]. More direct proofs were the studies on mice with different genetic background, which indicated that IL-10 was responsible, at least in part, for the high survival, which suggested that aberrant innate immune response contributed to SS2 diseases [40].
To be aware of the information about host immune response would enable people to better understand the disease. Transcriptional response of alveolar macrophages to SS2 has been performed and the results indicated that NF-kB and MAP-kinases signaling pathways were induced upon interaction with SS2 [41]. However, it is not easy to get more information since the primary macrophages are so sensitive to the interference. Spleen plays an important role in immune response and could be an ideal target to study host immune response against infection [42,43]. In the present study, the gene expression profiles of swine spleens which suffered from highly pathogenic SS2, avirulent isogenic strain and PBS respectively were investigated to reveal the host immune response to SS2 and the contributions of host response to SS2 diseases.
Results
Transcriptome analysis
The transcriptome analysis indicated that 14,992, 15,487 and 15,757 probe sets, corresponding to 62.1%, 64.2% and 65.3% of all probe sets, were detected in WT, ΔHP0197 and mock-infected pig spleens respectively (Additional file 1). The expression profiles of porcine spleens challenged with WT 3 days post inoculation were compared with those of the mock-infected group. After quantile normalization and statistical analysis, 1014 transcripts were identified at the global false discovery rate (FDR) of 10% (Additional file 2). Furthermore, the criteria of a two-fold or greater change in differential expression and a FDR of 10% were chosen to determine up-regulated and down-regulated genes in the WT infected replicates. Using these criteria, 120 and 132 transcripts, representing 104 and 129 unique genes, were significantly up-regulated and down-regulated respectively (Additional file 3). However, only a few genes showed significantly differential expressions when comparing ΔHP0197 with mock-infected samples (Figure 1A).
Figure 1.
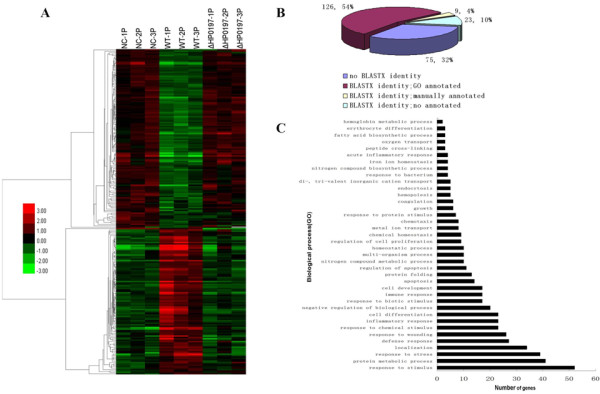
Clustering and characterization of the differential expression of genes. (A) 233 genes were selected for cluster analysis which is described in methods. Each row represents a separate transcript and each column represents a separate piglet. Color legend is on the left, the color scale ranges from saturated green for log ratios -3.0 and above to saturate red for log ratios 3.0 and above. Red indicates increased transcript expression levels, green indicates decreased levels compared with normal samples. (B) Percentage distribution of unique genes was from 233 differentially regulated transcripts after BLASTX searches and annotation. 158 unique genes had significant similarities based on BLASTX searches. 135(126+9) unique genes had been annotated by Biological Process (BP) Classification. (C) Categories of annotated genes genes based on biological process GO term. Many categories shared the same transcripts.
Of the 233 unique DE transcripts, 158 transcripts could be determined based on BLASTX searches and annotated with DAVID or by searching against the GenBank database (Figure 1B). Among these, 135 unique genes were grouped into 39 categories based on biological process Gene Ontology (GO) terms or according to their potential Biology Process Classification by referring to recent publications (Figure 1C). Unsurprisingly, the majority of genes were related to the immune response, Transcription, Transport, material and energy metabolism, etc. (Table 1).
Table 1.
Different expression of genes in spleens after S. suis infection 3 days
| Function classification | ENTREZ GENE_ID | Description | Fold change | Q-value (%) |
|---|---|---|---|---|
| Inflammatory response | ||||
| 929 | CD14 Antigen | 3.4 | 1.222 | |
| 6279 | S100 Calcium binding protein A8 | 19.3 | 1.508 | |
| 6280 | S100 Calcium binding protein A9 | 16.1 | 0 | |
| 3588 | Interleukin 10 receptor, beta | 2.7 | 3.911 | |
| 5743 | Prostaglandin-Endoperoxide synthase 2 | 4.7 | 7.146 | |
| 7057 | Thrombospondin 1 | 2.4 | 6.387 | |
| 3576 | Interleukin 8 | 5.6 | 6.387 | |
| 9547 | Chemokine (C-X-C Motif) Ligand 14 | 2.0 | 8.898 | |
| 6283 | S100 Calcium binding protein A12 | 18.6 | 0 | |
| 2908 | Nuclear receptor subfamily 3, group C, member 1 | 0.5 | 6.882 | |
| 6363 | Chemokine (C-C Motif) Ligand 19 | 2.2 | 1.508 | |
| 7097 | Toll-like receptor 2 | 2.0 | 6.387 | |
| 2920 | Chemokine (C-X-C Motif) Ligand 2 | 7.3 | 3.385 | |
| 246 | Arachidonate 15-Lipoxygenase | 0.2 | 2.181 | |
| 7052 | Transglutaminase 2 | 2.1 | 6.387 | |
| 9332 | CD163 antigen | 11.7 | 0 | |
| 6288 | Serum amyloid A1 | 6.4 | 1.222 | |
| 3553 | Interleukin 1, beta | 16.7 | 6.387 | |
| 3569 | Interleukin 6 (Interferon, Beta 2) | 4.8 | 6.387 | |
| 56729 | Resistin | 3.7 | 7.146 | |
| Response to stress | ||||
| 1153 | Cold inducible rna binding protein | 0.43 | 5.612 | |
| 3320 | Heat shock protein 90Kda alpha class A member 1 | 3.2 | 8.898 | |
| 6916 | Thromboxane A synthase 1 | 2.6 | 3.911 | |
| 10963 | Stress-induced-phosphoprotein 1 | 2.5 | 0 | |
| 130872 | AHA1, activator of heat shock 90Kda protein ATPase homolog 2 | 2.6 | 1.508 | |
| 3337 | Dnaj (Hsp40) homolog, subfamily B, member 1 | 2.8 | 1.222 | |
| 871 | Serpin peptidase inhibitor, clade H (Heat Shock Protein 47), member 1 | 2.7 | 1.222 | |
| 10808 | Heat shock 105Kda/110Kda protein 1 | 3.3 | 0 | |
| 3301 | Dnaj (Hsp40) homolog, subfamily A, member 1 | 2.4 | 0 | |
| 3304 | Heat Shock 70Kda Protein 1A | 11.1 | 0 | |
| Coagulation | ||||
| 5328 | Plasminogen activator, urokinase | 2.0 | 6.387 | |
| 2162 | Coagulationfactor XIII, A1 polypeptide | 6.8 | 3.385 | |
| Signal transduction | ||||
| 9465 | A kinase anchor protein 7 | 0.5 | 6.698 | |
| 8519 | Interferon induced transmembrane protein 1 | 2.0 | 6.387 | |
| 115265 | Dna-damage-inducible transcript 4-like | 0.3 | 2.181 | |
| 9770 | Ras association (Ralgds/Af-6) domain family 2 | 2.4 | 6.387 | |
| 9510 | Adamm etallopeptidase with thrombospondin type 1 motif, 1 | 2.3 | 0 | |
| 1363 | Carboxypeptidase E | 0.44 | 6.698 | |
| 54210 | Triggering receptor expressed on myeloid cells 1 | 3.2 | 6.387 | |
| 9289 | G protein-coupled receptor 56 | 0.46 | 6.698 | |
| 7043 | Transforming growth factor, beta 3 | 2.1 | 4.116 | |
| Transcription | ||||
| 2353 | V-Fos fbj murine osteosarcoma viral oncogene homolog | 2.8 | 3.911 | |
| 84969 | Chromosome 20 open reading frame 100 | 0.3 | 2.541 | |
| 55885 | Lim domain only 3 | 0.3 | 2.181 | |
| 3726 | Jun B proto-oncogene | 2.6 | 7.146 | |
| 91 | Activin a receptor, type ib | 3.4 | 1.222 | |
| 116448 | Oligodendrocyte transcription factor 1 | 2.4 | 6.387 | |
| 79365 | Basic helix-loop-helix domain containing, class B, 3 | 0.4 | 2.181 | |
| 64919 | B-cell cll/lymphoma 11B | 0.5 | 2.181 | |
| 23635 | Single-stranded dna binding protein 2 | 0.4 | 2.541 | |
| 23414 | Zinc finger protein, multitype 2 | 0.5 | 6.698 | |
| 7552 | Zinc finger protein 6 (Cmpx1) | 0.5 | 3.385 | |
| 6920 | Transcription elongation factor A (SII), 3 | 2.2 | 6.387 | |
| 4783 | Nuclear factor, interleukin 3 regulated | 2.4 | 3.911 | |
| 1052 | CCAAT/Enhancer binding protein (C/EBP), delta | 3.1 | 0 | |
| Cell adhesion | ||||
| 6401 | Selectin E | 3.5 | 1.222 | |
| 8174 | Mucosal vascular addressin cell adhesion molecule 1 | 2.3 | 6.387 | |
| 5067 | Contactin 3 | 0.5 | 6.794 | |
| 4867 | Nephronophthisis 1 (Juvenile) | 0.4 | 3.911 | |
| 1462 | Chondroitin sulfate proteoglycan 2 (Versican) | 9.1 | 0 | |
| 960 | CD44 antigen | 2.3 | 2.541 | |
| Ubiquitin cycle | ||||
| 115123 | Membrane-associated ring finger (C3HC4) 3 | 4.4 | 1.222 | |
| 7317 | Ubiquitin-activating enzyme E1 | 0.4 | 2.181 | |
| 11274 | Ubiquitin specific peptidase 18 | 0.4 | 6.698 | |
| 9666 | Zinc finger daz interacting protein 3 | 0.5 | 6.882 | |
| Transport | ||||
| 6556 | Solute carrier family 11, member 1 | 4.0 | 2.051 | |
| 4057 | Lactotransferrin | 5.9 | 3.385 | |
| 1356 | Ceruloplasmin (Ferroxidase) | 2.3 | 2.541 | |
| 1410 | Crystallin, alpha B | 2.8 | 6.387 | |
| 283652 | Solute carrier family 24, member 5 | 0.4 | 2.181 | |
| 54843 | Synaptotagmin-like 2 | 0.4 | 6.698 | |
| 6947 | Haptocorrin | 8.9 | 0 | |
| 3949 | Low density lipoprotein receptor | 2.1 | 5.612 | |
| 3043 | Hemoglobin, beta | 0.4 | 6.698 | |
| 3042 | Hemoglobin, alpha pseudogene 2 | 0.2 | 2.181 | |
| 3040 | Hemoglobin, alpha 1 | 0.2 | 2.181 | |
| 2554 | Gamma-aminobutyric acid (Gaba) a receptor, alpha 1 | 0.3 | 3.911 | |
| 2288 | Fk506 binding protein 4, 59Kda | 2.2 | 1.222 | |
| 6557 | Solute carrier family 12, member 1 | 0.4 | 6.882 | |
| 152789 | Janus kinase and microtubule interacting protein 1 | 0.5 | 6.794 | |
| Nucleic acid metabolic process | ||||
| 401251 | Muts homolog 5 | 0.5 | 6.698 | |
| 56952 | Phosphoribosyl transferase domain | 0.4 | 2.181 | |
| 51251 | 5'-Nucleotidase, cytosolic Iii | 0.4 | 6.698 | |
| 10492 | Synaptotagmin binding, cytoplasmic rna interacting protein | 0.4 | 4.116 | |
| 8347 | Histone 1,H2bd | 2.6 | 6.387 | |
| 8334 | Histone 1, H2ac | 5.6 | 1.222 | |
| 6430 | Splicing factor, arginine/serine-rich 5 | 0.5 | 0 | |
| 4302 | Myeloid/Lymphoid or mixed-lineage leukemia translocated to, 6 | 0.4 | 6.882 | |
| Response to stimulus | ||||
| 5806 | Pentraxin-related gene, rapidly induced by il-1 beta |
14.1 | 1.222 | |
| 6372 | Chemokine (C-X-C motif) ligand 6 | 5.5 | 1.222 | |
| 64135 | Interferon induced with helicase c domain 1 | 0.4 | 6.698 | |
| 3240 | Haptoglobin | 4.6 | 0 | |
| 6648 | Superoxide dismutase 2, mitochondrial | 4.6 | 1.508 | |
| 1843 | Dual specificity phosphatase 1 | 2.1 | 6.387 | |
| Cell differentiation/development | ||||
| 58189 | Wap four-disulfide core domain 1 | 2.1 | 1.222 | |
| 9531 | Bcl2-associated athanogene 3 | 3.7 | 0 | |
| 51454 | Gulp, engulfment adaptor ptb domain containing1 | 0.4 | 2.181 | |
| 212 | Aminolevulinate, delta-, synthase 2 | 0.4 | 6.698 | |
| 2012 | Epithelial membrane protein 1 | 2.0 | 7.146 | |
| 79689 | Steap family member 4 | 2.8 | 3.911 | |
| 9021 | Suppressor of cytokine signaling 3 | 2.4 | 3.385 | |
| 5270 | Serpin peptidase inhibitor, clade E, member 2 | 2.3 | 3.385 | |
| 1946 | Ephrin-A5 | 0.4 | 3.911 | |
| 85444 | Leucine rich repeat and coiled-coil domain containing 1 | 0.5 | 5.612 | |
| 54873 | Palmdelphin | 0.4 | 5.612 | |
| 10439 | Olfactomedin 1 | 3.3 | 6.387 | |
| Carbohydrate metabolic process | ||||
| 4199 | Malic enzyme 1, NADP(+)-dependent, cytosolic | 0.4 | 3.911 | |
| 80760 | Inter-alpha (Globulin) inhibitor H5 | 0.3 | 6.698 | |
| 152831 | Klotho beta | 2.5 | 0 | |
| 3101 | Hexokinase 3 (White Cell) | 2.9 | 6.387 | |
| 3099 | Hexokinase 2 | 2.3 | 8.898 | |
| 1116 | Chitinase 3-like 1 | 2.9 | 8.898 | |
| Protein metabolic process | ||||
| 85464 | Slingshot homolog 2 | 2.3 | 1.508 | |
| 51327 | Erythroid associated factor | 0.06 | 0 | |
| 7076 | Timp metallopeptidase inhibitor 1 | 4.4 | 1.222 | |
| 7053 | Transglutaminase 3 | 6.1 | 1.222 | |
| 114907 | F-box protein 32 | 0.4 | 6.794 | |
| 64844 | Membrane-associated ring finger (C3HC4) 7 | 0.5 | 2.181 | |
| 64172 | O-sialoglycoprotein endopeptidase-like 1 | 0.4 | 2.181 | |
| 55466 | Dnaj (Hsp40) homolog, subfamily A, member 4 | 2.7 | 2.541 | |
| 51056 | Leucine aminopeptidase 3 | 2.0 | 8.898 | |
| 2289 | Fk506 binding protein 5 | 2.5 | 6.387 | |
| 26235 | F-box and leucine-rich repeat protein 4 | 0.5 | 6.698 | |
| Nitrogen compound metabolic process | ||||
| 383 | Arginase | 0.2 | 2.181 | |
| 64850 | Alanine-glyoxylate aminotransferase 2-like 1 | 0.2 | 6.882 | |
| 6799 | Sulfotransferase family, cytosolic, 1A, phenol-preferring, member 2 | 2.0 | 6.387 | |
| 8974 | Procollagen-proline, 2-oxoglutarate 4-dioxygenase, alpha polypeptide ii | 3.2 | 6.387 | |
| Others | ||||
| 129446 | Cardiomyopathy associated 3 | 0.3 | 2.181 | |
| 128218 | Transmembrane protein 125 | 2.0 | 8.898 | |
| 57763 | Ankyrin repeat, family A, 2 | 0.4 | 2.181 | |
| 29970 | Schwannomin interacting protein 1 | 0.5 | 6.794 | |
| 23336 | Desmuslin | 0.5 | 6.882 | |
| 590 | Butyrylcholinesterase | 0.5 | 4.116 | |
| 84649 | Diacylglycerol o-acyltransferase homolog 2 | 3.2 | 1.222 | |
| 79887 | Hypothetical protein Flj22662 | 3.5 | 6.387 |
DE genes which putative functions assigned based on GO term and manual annotation. Manual annotations were listed in italics. Many genes with multiple functions were only listed in one category according to specific biology processes. "FC≥2" represents up regulation (infection/control), "FC ≤ 0.5" represents down regulation.
Validation of microarray data by quantitative real-time PCR (qPCR)
The qPCR was performed to validate the expression patterns during infection for specific genes identified in the microarray assay. In order to validate the differential expression of various identified genes, 16 up-regulated genes, with the increase ranging from 2.0-fold to 18.6-fold, and 3 down-regulated genes, with the decrease ranging from 2.5-fold to 5.9-fold, were selected for qPCR analysis. All the selected down-regulated genes could be amplified from the control samples but failed to achieve significant detectable signs from WT-infected spleens, except for ALOX15 which showed 3.2-fold down-regulated expression. All selected up-regulated genes showed higher expression in WT-infected samples than in the control samples (Table 2). Though variation in fold changes could be observed between qPCR and microarray (Table 2), the differential expression patterns were coincident between the results of the two techniques, which indicated the reliability of the microarray analysis.
Table 2.
Validation of microarray results by qPCR
| Gene | Accession | Microarray fold change |
qPCR fold change (p-value) |
|---|---|---|---|
| IL1B | CK468468 | 16.7 | 258.3 (0.0117) |
| S100A9 | BI402402 | 16.1 | 137.2(0.0007) |
| S100A12 | CB475695 | 18.6 | 76.7 (< 0.0001) |
| HSP90 | CF180819 | 3.18 | 48.5 (0.0321) |
| IL8 | NM_213867 | 5.58 | 35.5 (0.0066) |
| HSP70 | NM_213766 | 11.06 | 31.4 (0.0099) |
| TIMP1 | NM_213857 | 4.4 | 14.6 (0.0023) |
| IL6 | AF493992 | 4.8 | 10.5 (0.0074) |
| SOD2 | NM_214127 | 4.6 | 10.0 (< 0.0001) |
| NRAMP1 | U55068 | 3.97 | 7.2 (0.0035) |
| SELE | NM_214268 | 3.5 | 5.9 (0.0002) |
| PLAU | NM_213945 | 2.0 | 5.5 (0.0415) |
| CCL19 | BX672579 | 2.16 | 4.2 (0.0004) |
| haptocorrin | CB472702 | 3.78 | 2.1(0.0388) |
| TLR-2 | NM_213761 | 2.0 | 2.1 (< 0.0001) |
| ALOX15 | NM_213931 | 0.2 | 0.3 (0.038) |
Induction of inflammasomes and acute phase proteins by SS2 infection
Highly pathogenic SS2 infection could cause up-regulated expression of a large set of genes involved in the inflammatory response and acute phase proteins by microarray analysis. IL-1B, IL-6 and IL-8 could be induced by foreign pathogens and play essential roles in controlling infections [5,44]. However, they may also cause pathology when these productions are excessive or uncontrolled [45]. Ye et al. also found that significantly high level of cytokines could be induced by highly pathogenic SS2 strain and play important roles in sepsis [34], which is in coincidence with ours. In addition, quite a few genes related to inflammatory response were found up-regulated, such as S100 family proteins (S100A8, S100A9 and S100A12) [46], Pentraxin 3 [47] and Resistin [48,49]. They play important roles in mediating inflammatory responses, recruiting inflammatory cells to sites of tissue damage or contributing to resisting the invasion of various pathogens.
Acute phase proteins (APPs), such as Lactotransferrin [50], Haptoglobin [51], Serum amyloid A 2 [52] and coagulation factor XIII, were involved in physiologic reactions initiated early in the inflammatory process [53], and could be a response to S. suis infection [54]. CEBPD belonging to the CCAAT-enhancer binding protein (CEBP) family which is crucial in the regulation of genes involved in immunity and inflammation. These up-regulated genes are the representative of host acute response struggling to eliminate invading pathogens.
Induction of genes related in cell adhesion and stress response
Cell adhesion molecules (CAMs) have been implicated in the regulation of a wide variety of fundamental cellular processes, such as cell adhesion, cell polarization, survival, movement, and proliferation [55]. E-selectin is a cell adhesion molecule expressed on endothelial cells activated by cytokines, and plays an important role in recruiting leukocytes to the site of injury [56]. Versican can bind adhesion molecules on the surface of inflammatory leukocytes [57] and act as a TLR2 agonist in inducing the release of proinflammatory cytokines [58]. Thrombospondin 1 is an adhesive glycoprotein that mediates cell-to-cell and cell-to-matrix interactions and it could interact with numerous proteases involved in angiogenesis [59]. Mucosal vascular addressin cell adhesion molecule 1 is predominantly expressed on high endothelial venules in inflamed tissues, and could assist the extravasations of leucocyte [60]. The up-regulation of cell adhesion molecules after SS2 infection would contribute to recruiting leukocytes to the site of infection, which could control infection.
Genes related to oxidative stress and homeostasis were also identified to be up-regulated. SOD2 provides vital protection against reactive oxygen species (ROS), thus protecting tissues from damage in a broad range of disease states. The secretion of PGE2, together with nitric oxide production, is involved in disruption of the blood-brain barrier(BBB) in an experimental model of bacterial meningitis [61]. S. suis-mediated PGE2 production by human macrophages was also noticed by Jobin and contributed to the BBB disruption [62].
Toll-like receptors (TLRs) pathway analysis
Activation of the innate immune response is controlled in large part by the Toll-like receptor (TLR) family of pattern-recognition receptors. The previous study showed that S. suis was mainly recognized via TLR2 by THP-1 monocytes, which was associated with CD14 [38] and led to the release of pro-inflammatory mediators [63]. The strong activation of TLR2 and CD14 was also observed in murine brain parenchyma after the presence of S. suis bacteremia [39]. A recent research indicated that components released during S. suis infection as well as penicillin-treated whole bacteria could induce NF-kB activation through TLR2/6 [64]. The obvious elevation of TLR2 (2.0 fold) and CD14 (3.4 fold) was noticed at transcript level in spleens after highly pathogenic SS2 infection. Unsurprisingly, MyD88, an adaptor molecule in downstream signaling events with TLRs and CD14, was up-regulated at the level of 1.5 fold (q < 10%). In contrast, the effect could not be seen with avirulent SS2 infection.
Down-regulated transcripts following S. suis infection
The majority of down-regulated genes were related to transcription, transport, material and energy metabolism (Table 1). Highly pathogenic strain could show high level of toxicity to host cells [34], and as a result, the influenced cells could hardly to be active. So these down regulations could be regarded the representative of the reduced vital activity of SS2-influenced cells.
Discussion
Two recent SS2 outbreaks in China not only seriously challenged public health but also shocked the scientific community, calling for the basic and translational studies of S. suis. Until now, several proteins were identified as vaccine candidates [65,66] and drug targets [67,68] for controlling SS2. In addition, emphasis is also extended to the pathogenesis study. Several pathogenic factors were successfully identified and strengthened the understanding for the virulence of the bacterium. As infectious disease resulted from the interplay between pathogens and the defense of the hosts they infect, host immune response was especially essential for understanding the diseases [41,69].
In the present study, we tried to compare the gene expression profiles of spleens from swine suffering from highly pathogenic SS2, from swine infected with the avirulent isogenic strain, and from swine inoculated with PBS respectively to reveal the host immune response to SS2 and the contributions of host response to SS2 diseases. It is not accidental that significant changes of gene expression profiles could be noticed when infected with highly pathogenic SS2 compared with mock-infected samples, while avirulent isogenic strain would cause similar profiles to mock-infected samples (Figure 1A). These indicated that avirulent isogenic strain could hardly cause significant gene expression which was coincident with the fact that no significant clinical symptoms could be noticed in pigs. Moreover, the obvious changes in gene expression profiles were highly associated with significant clinical signs on day 3 post-inoculation with highly pathogenic strain. Further analysis of the present study indicated that the majority of down-regulated genes were mainly involved in transcription, transport, material and energy metabolism which were representative of the reduced vital activity of SS2-influenced cells. However, the up-regulated genes were principally related to immune response, such as genes involved in inflammatory response; acute-phase/immune response; cell adhesion and response to stress. Undoubtedly, it would be meaningful to explore the roles of these genes in SS2-caused diseases.
First of all, it is necessary to know how SS2 induces immune response. It is well acknowledged that TLRs are transmembrane proteins that could recognize specific PAMPs and eventually result in the activation of NF-kB and MAP kinases to elicit regulatory response [70]. Among these transmembrane proteins, TLR-2 could recognize bacterial LAM, BLP and PGN by following their initial interaction with CD14. Previous reports indicated that S. suis mainly induced proinflammatory cytokines by TLR2 of human macrophages and murine brain [39,63], and several proinflammatory cytokines, such as IL-1B, IL-6, IL-8, TNF-a and MCP-1 could be triggered [35,36,38,41]. In our study, large doses of bacteria could be isolated from spleens of WT-infected pigs while no bacterium could be found to exist in pigs infected with ΔHP0197. In coincidence with these, TLR-2 pathway and several proinflammatory cytokines were induced only in WT-infected pigs. ΔHP0197 showed similar transcript profile as control pigs due to either failing to invading or being easily eliminated by host. In contrast, the large doses of bacteria effected maximal cytokines release in WT-infected pigs [37]. The exaggerated high levels of cytokines perhaps exacerbate the inflammation and were considered to be responsible for S. suis caused diseases [39]. So the successful lethal pathogens could persistently induce cytokines secreted originally to clear the foreign invader, and as a result, the host's defense was utilized by S. suis to cause diseases, and to some extent to death.
As we all know that the secreted cytokine is an important part of a host defense system, which could recruit inflammatory cells to sites of tissue damage and help to eliminate the pathogens. However, this innate defense system is a double edged sword. If the recruiting inflammatory cells could kill the invader, the disease could be controlled. On the opposite side, if the recruiting phagocytes could not efficiently kill the bacteria, the tide would be turned to pathogen's favor, and the persistently induced cytokines would result in the exacerbated inflammation and lead to the death during the septic phase of infection. These might be the reason why the survival rate could be elevated when inflammation was inhibited by IL-10 [40], and why the level of cytokine was correlated inversely with survival time in patients with sepsis [45]. In coincidence with our analysis, pathogenic S. suis could effectively resist the uptake by phagocytes and CPS could inhibit activation of signaling pathways involved in phagocytosis [17,71,72]. In addition, several virulence-associated proteins such as FBPS[19], PDGA[31], LTA[30], HP0197 (unpublished data), serine protease [73] etc. were also contributed to the phagocytosis resistance, and the up-regulation of these proteins in vivo may suggest the better phagocytosis resistance [31,74,75]. Due to failing phagocytosis, bacteria could not only cause exacerbated inflammation but also contribute to its survival in the bloodstream in "modified Trojan Horse" theory in which bacteria travel extracellularly while attached to, but not phagocytosed [17,72], and then cause bacteremia and even septemia.
One of the key questions to be answered is how S. suis crosses the blood-brain barrier to cause meningitis, which was observed in all WT-infected pigs. The findings of the reported study presented that suilysin-positive strain could show toxin to produce functional alteration and increase the permeability of BBB; and Suilysin-negative strain might stimulate the production of proinflammatory cytokines resulting in alteration of BBB permeability [76,77]. And they also indicated that this highly pathogenic strain could produce high level of toxins in vivo-Suilysin, MRP, hyl [74], and undoubtedly it would contribute to the penetration of deep tissue and BBB. In addition, the stimulated production of proinflammatory cytokines would result in the alteration of BBB permeability, and it would be more feasible for S. suis to break through BBB. From our understanding, WT strain could utilize the synergic effect of toxins and high level of cytokines to accelerate the penetration of deep tissue and BBB. These might be the reason why the strain could cause severe human diseases in Sichuan, 2005.
Conclusions
Microarray technology has been used to analyse the globle porcine transcriptional response to infection with various pathogenic microorganisms recently. Study on the transcriptional response to the Gram-positive bacterium SS2 by using the Affymetrix GeneChip Porcine Genome Array has not been reported until now. Although great efforts have been made to understand the molecular basis of this infection, the response to SS2 infection is still largely unknown. Transcriptome analysis based on S. suis-infected spleens could improved the interference received by the cells analysis, and also supply the solid supplementary for analysis on alveolar macrophages. Highly pathogenic S. suis could persistently induce cytokines mainly by TLR2 pathway, and eventually the high level of cytokines and toxins secreted by phagocytosis-resistant bacteria could destroy deep tissues, and cause meningitis, septicaemia, pneumonia, endocarditis, and arthritis.
Methods
Bacterial strains
SS2 strain 05ZY (WT) which was isolated from the brain of a diseased piglet collected in Sichuan outbreak in China 2005 showed high virulence to pigs [4,78], and was applied to infect pigs. An isogenic HP0197 mutant (ΔHP0197) derived strain 05ZY showed no obvious virulence to pigs (unpublished data) was applied as a control.
Animals infection and tissue collection
All the experimental protocols were approved by the Laboratory Animal Monitoring Committee of Hubei Province and performed accordingly. A total of 12 pigs of high-health status (ages 4-5 weeks) were assigned to three groups, within four in each. The pigs were determined to be SS2-free by antibody-based ELISA and nasal swabs-based bacteriologic test. One hour before inoculation, all pigs were given 2 ml of 1% acetic acid (pH 2.9) intranasally to enhance the sensitivity of the S. suis challenge. Two groups were inoculated intranasally with 1 ml of 2×106CFU of WT strain or ΔHP0197 respectively, and the rest group inoculated with PBS was served as control. All pigs inoculated with WT showed typical symptoms at day 3 while pigs inoculated with ΔHP0197 or PBS showed no significant clinical signs. Blood samples from each group were detected for bacterial burden. Bacteria could be found in the blood of pigs in the WT group at day 3 post-inoculation while no bacterium was found from the blood of pigs inoculated with isogenic mutant strain or PBS at the same time point. All pigs were sacrificed at day 3, and their tissue samples were cultured to prove in vivo bacterial burden. Bacteria were found in the spleens of the WT group, and no bacterium was found in the other two groups. Spleen samples were aseptically collected and immediately frozen in liquid nitrogen for future RNA isolation. Total RNA was isolated from approximately 200 mg of each sample by using the TRIzol (Invitrogen) and RNeasy Midi kit (QIAGEN) based on the manufacturer's protocols. The integrity, quality, and quantity of RNA were assessed using the Agilent Bioanalyser 2100.
Microarray hybridizations and data analysis
The RNA labelling and hybridization were conducted by a commercial Affymetrix array service (CapitalBio Corp. Beijing, China). An aliquot of 2 μg of total RNA was converted to double-stranded cDNA with the one-cycle cDNA Synthesis Kit (Affymetrix), and then biotin-tagged cRNA was produced with MessageAmp™ II aRNA Amplification Kit. The resulting bio-tagged cRNA was fragmented to strands of 35 to 200 bases in length according to Affymetrix's protocols and then it was hybridized to GeneChip Porcine Genome Array. Hybridization was performed at 45°C with rotation for 16 h (Affymetrix GeneChip Hybridization Oven 640). The GeneChip arrays were washed and then stained (streptavidin-phycoerythrin) on an Affymetrix Fluidics Station 450 followed by scanning on GeneChip Scanner 3000.
The hybridization data were analyzed using GeneChip Operating software (GCOS 1.4). A global scaling factor of 500 was used to normalize the different arrays. We identified the differentially expressed genes according to change p-value calculated by GCOS 1.4, and 2-fold change as an empirical criterion. Then all DE genes were performed for hierarchical cluster (Ver.3.0) and TreeView (Ver.1.1.1) analyses. Genes with significant similarities to transcripts in nr database based on BLASTX searches were selected for GO analysis with DAVID http://david.abcc.ncifcrf.gov/home.jsp. Annotation results were obtained by inputting the gene list of ENTREZ_GENE_ID as identifier. All microarray results from this study were deposited in NCBI's Gene Expression Omnibus (GEO) database, accession numbers are: Platform, GPL3533; Series, GSE23596; Samples, GSM578704, GSM578705, GSM578706, GSM578707, GSM578708, GSM578709, GSM578710, GSM578711, GSM578712.
qPCR analysis
All tested RNAs from swine spleens were reversely transcribed to cDNA with the M-MLV Reverse Transcriptase (Promega). Each cDNA sample was used as a template for qPCR and the amplification mixture contained SYBR Green (TOYOBO, Japan), forward and reverse primers. Some primers were designed by the program Primer 5.0, the primer names, accession number, primer sequence and product size are shown in Table 3. The efficiency of the PCR reaction was 91-99% for all reactions (slope standard line between -3.3 and -3.6). The standard line consisted of five 10-fold dilutions of the samples. Analysis was performed using the ABI7500 Software (Applied Biosystems). PCRs were performed in ABI PRISM 7500 sequence detection system as follows: 1 cycle at 95°C for 10 min; 45 cycles at 95°C for 30 s, 60°C for 30 s and 72°C for 30 s. Melting curves were performed at the end of amplification for validating data quality by increasing the temperature from 65°C to 95°C, read every 0.2°C, hold 2 sec, then cooling at 25°C for 30 s. The PCR products were confirmed using agarose gel electrophoresis (1.5%). Amplification of the gapdh gene was used as internal control. All the tested genes are shown in Table 3. All reactions were performed in triplicate. For each run, to normalize the amount of sample cDNA added to each reaction, the Ct value of each test gene was subtracted by the Ct value of the endogenous control gapdh gene (delta Ct = Ct tested gene - Ct gapdh), and then for a comparison between the expression of the gene in treated samples and in control samples. The delta Ct values of the gene in treated samples were subtracted by the delta Ct value of the gene in control samples (delta-delta Ct = delta Ct treatment - delta Ct control). The fold changes were calculated by the formula of 2-delta-delta Ct described by Livak & Schmittgen [79]. Data were means ± SD of triplicate reactions for each gene transcript.
Table 3.
Primers for qPCR
| primer | Accession number |
Sequence | Product size |
|---|---|---|---|
| Plau | NM_213945 | Forward: CGAACTGTGGCTGTCT Reverse: AGCAGGTTTGCGATGTG |
126 bp |
| S100A9a | BI402402 | Forward: CCAGGATGTGGTTTATGGCTTTC Reverse: CGGACCAAATGTCGCAGA |
186 bp |
| S100A12a | CB475695 | Forward: GGCATTATGACACCCTTATC Reverse: GTCACCAGGACCACGAAT |
169 bp |
| Hsp70 | NM_213766 | Forward: AGGCGGAGAAGTACAAAGCG Reverse: GATGGGGTTACACACCTGCTC |
257 bp |
| Timp1 | NM_213857 | Forward: CGCCTCGTACCAGCGTTAT Reverse: GTGGAAGTATCCGCAGACGC |
127 bp |
| SOD2 | NM_214127 | Forward: TCTGGACAAATCTGAGCCCT Reverse: GACGGATACAGCGGTCAACTT |
119 bp |
| Il6b | AF493992 | Forward: GACAAAGCCACCACCCCTAA Reverse: CTCGTTCTGTGACTGCAGCTTATC |
69 bp |
| Sele | NM_214268 | Forward: GGATTTGAACTCATCGGACCT Reverse: CATTCTGAGGATGGCCGAC |
115 bp |
| Il1bb | NM_214055 | Forward: GGCCGCCAAGATATAACTGA Reverse: GGACCTCTGGGTATGGCTTTC |
70 bp |
| Nramp1 | U55068 | Forward: CGTGGTGACAGGCAAGGACT Reverse: TAGCCGTGCCGATGACTTC |
131 bp |
| Hsp90 | CF180819 | Forward: CCCAGTTGATGTCGTTG Reverse: CCGTCAGGCTTTCGTAT |
117 bp |
| Il8 b | NM_213867 | Forward: TTCGATGCCAGTGCATAAATA Reverse: CTGTACAACCTTCTGCACCCA |
176 bp |
| CCL19 | BX672579 | Forward: GCTAAGCCTCTGGACT Reverse: AATGAGCAGGTAGCGA |
121 bp |
| Haptocorrin | CB472702 | Forward: ATTCTCAGGGAGTATTCCGTCT Reverse: CTTTGGGGACAAGTAGCAGTT |
105 bp |
| Alox15 | NM_213931 | Forward: ACCGAGGGTTTCCTGTCT Reverse: AGGTGGTTGGAGGAGTGC |
100 bp |
| TLR2b | NM_213761 | Forward:TCACTTGTCTAACTTATCATCCTCTTG Reverse: TCAGCGAAGGTGTCATTATTGC |
162 bp |
| GAPDH b | AF017079 | Forward: TGCCAACGTGTCGGTTGT Reverse: TGTCATCATATTTGGCAGGTTTCT |
62 bp |
Abbreviations
SS2: Streptococcus suis serotype 2; DE: differentially expressed; FC: fold change; GO: Gene Ontology; FDR: false discovery rate; qPCR: quantitative real-time PCR; TLR: Toll-like receptors; PRRs: pattern-recognition receptors;
Authors' contributions
RL and BC carried out all works and drafted the manuscript. AZ made substantial contributions to bioinformatics and statistical analysis. LT and YW participated in the animal challenge experiment. HC participated in the experiment design and coordination. MJ helped to revise and finalize the manuscript. All authors read and approved the final manuscript.
Supplementary Material
Spleen transcriptome analysis following S. suis infection using the Affymetrix Porcine Genechip. Data of each probe is from the three piglets of the control group (NC-1P, NC-2P, NC-3P), the WT group (WT-1P, WT-2P, WT-3P) and the △HP0197 group (M97-1P, M97-2P, M97-3P). "P", present; "A", absent; "M", marginal; select while Count (P) ≥ 2 in two groups. Totally, 15,757, 14,992 and 15,487 probesets were detected expression in the control group, the WT group and △HP0197 group respectively.
transcripts expressed in porcine spleen following S. suis (WT) infection. "FC", Fold change, gene expression level following WT infection compared to the control. "≥2" represents up regulation, " < 1" represents down regulation. "q-value", significance level of differential expression for a particular gene. "Gene description", top informative BLASTX hit.
Differentially expressed transcripts in porcine spleen following S. suis (WT) infection (q < 10%, FC≥2). 120 transcripts (row 5-124) were significantly up-regulated, and 132 (row 125-256) were significantly down-regulated, "FC", Fold change, gene expression level following WT infection compared to the control.
Contributor Information
Ran Li, Email: lr001234@163.com.
Anding Zhang, Email: andye8019@webmail.hzau.edu.cn.
Bo Chen, Email: hzauchen@gmail.com.
Liu Teng, Email: tengliu2003@yahoo.com.cn.
Ya Wang, Email: wangya@webmail.hzau.edu.cn.
Huanchun Chen, Email: chenhch@mail.hzau.edu.cn.
Meilin Jin, Email: jml8328@126.com.
Acknowledgements
We thank Professor Yanxiu Liu for her revision of the language of this manuscript.
This work was supported by National Basic Research Program of China (program 973, grant 2006CB504404), the National Transgenic Major Program (2009ZX08009-141B), the National Natural Science Foundation of China (30871870), and Program for Changjiang Scholars and Innovative Research Team in University (IRT0726).
References
- Staats JJ, Feder I, Okwumabua O, Chengappa MM. Streptococcus suis: past and present. Vet Res Commun. 1997;21(6):381–407. doi: 10.1023/A:1005870317757. [DOI] [PubMed] [Google Scholar]
- Lun ZR, Wang QP, Chen XG, Li AX, Zhu XQ. Streptococcus suis: an emerging zoonotic pathogen. Lancet Infect Dis. 2007;7(3):201–209. doi: 10.1016/S1473-3099(07)70001-4. [DOI] [PubMed] [Google Scholar]
- Hill JE, Gottschalk M, Brousseau R, Harel J, Hemmingsen SM, Goh SH. Biochemical analysis, cpn60 and 16S rDNA sequence data indicate that Streptococcus suis serotypes 32 and 34, isolated from pigs, are Streptococcus orisratti. Vet Microbiol. 2005;107(1-2):63–69. doi: 10.1016/j.vetmic.2005.01.003. [DOI] [PubMed] [Google Scholar]
- Tang J, Wang C, Feng Y, Yang W, Song H, Chen Z, Yu H, Pan X, Zhou X, Wang H. et al. Streptococcal toxic shock syndrome caused by Streptococcus suis serotype 2. PLoS Med. 2006;3(5):e151. doi: 10.1371/journal.pmed.0030151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanier G, Segura M, Lecours MP, Grenier D, Gottschalk M. Porcine brain microvascular endothelial cell-derived interleukin-8 is first induced and then degraded by Streptococcus suis. Microb Pathog. 2009;46(3):135–143. doi: 10.1016/j.micpath.2008.11.004. [DOI] [PubMed] [Google Scholar]
- Haas G, Karaali G, Ebermayer K, Metzger WG, Lamer S, Zimny-Arndt U, Diescher S, Goebel UB, Vogt K, Roznowski AB. et al. Immunoproteomics of Helicobacter pylori infection and relation to gastric disease. Proteomics. 2002;2(3):313–324. doi: 10.1002/1615-9861(200203)2:3<313::AID-PROT313>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- Holden MT, Hauser H, Sanders M, Ngo TH, Cherevach I, Cronin A, Goodhead I, Mungall K, Quail MA, Price C. et al. Rapid evolution of virulence and drug resistance in the emerging zoonotic pathogen Streptococcus suis. PLoS One. 2009;4(7):e6072. doi: 10.1371/journal.pone.0006072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wangsomboonsiri W, Luksananun T, Saksornchai S, Ketwong K, Sungkanuparph S. Streptococcus suis infection and risk factors for mortality. J Infect. 2008;57(5):392–396. doi: 10.1016/j.jinf.2008.08.006. [DOI] [PubMed] [Google Scholar]
- Rusmeechan S, Sribusara P. Streptococcus suis meningitis: the newest serious infectious disease. J Med Assoc Thai. 2008;91(5):654–658. [PubMed] [Google Scholar]
- Watkins EJ, Brooksby P, Schweiger MS, Enright SM. Septicaemia in a pig-farm worker. Lancet. 2001;357(9249):38. doi: 10.1016/S0140-6736(00)03570-4. [DOI] [PubMed] [Google Scholar]
- Taipa R, Lopes V, Magalhaes M. Streptococcus suis meningitis: first case report from Portugal. J Infect. 2008;56(6):482–483. doi: 10.1016/j.jinf.2008.03.002. [DOI] [PubMed] [Google Scholar]
- Tramontana AR, Graham M, Sinickas V, Bak N. An Australian case of Streptococcus suis toxic shock syndrome associated with occupational exposure to animal carcasses. Med J Aust. 2008;188(9):538–539. doi: 10.5694/j.1326-5377.2008.tb01771.x. [DOI] [PubMed] [Google Scholar]
- van de Beek D, Spanjaard L, de Gans J. Streptococcus suis meningitis in the Netherlands. J Infect. 2008;57(2):158–161. doi: 10.1016/j.jinf.2008.04.009. [DOI] [PubMed] [Google Scholar]
- Smith TC, Capuano AW, Boese B, Myers KP, Gray GC. Exposure to Streptococcus suis among US swine workers. Emerg Infect Dis. 2008;14(12):1925–1927. doi: 10.3201/eid1412.080162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fittipaldi N, Collis T, Prothero B, Gottschalk M. Streptococcus suis Meningitis, Hawaii. Emerg Infect Dis. 2009;15(12):2067–2069. doi: 10.3201/eid1512.090825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wertheim HF, Nguyen HN, Taylor W, Lien TT, Ngo HT, Nguyen TQ, Nguyen BN, Nguyen HH, Nguyen HM, Nguyen CT. et al. Streptococcus suis, an important cause of adult bacterial meningitis in northern Vietnam. PLoS One. 2009;4(6) doi: 10.1371/journal.pone.0005973. e5973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chabot-Roy G, Willson P, Segura M, Lacouture S, Gottschalk M. Phagocytosis and killing of Streptococcus suis by porcine neutrophils. Microb Pathog. 2006;41(1):21–32. doi: 10.1016/j.micpath.2006.04.001. [DOI] [PubMed] [Google Scholar]
- Smith HE, Damman M, van der Velde J, Wagenaar F, Wisselink HJ, Stockhofe-Zurwieden N, Smits MA. Identification and characterization of the cps locus of Streptococcus suis serotype 2: the capsule protects against phagocytosis and is an important virulence factor. Infect Immun. 1999;67(4):1750–1756. doi: 10.1128/iai.67.4.1750-1756.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Greeff A, Buys H, Verhaar R, Dijkstra J, van Alphen L, Smith HE. Contribution of fibronectin-binding protein to pathogenesis of Streptococcus suis serotype 2. Infect Immun. 2002;70(3):1319–1325. doi: 10.1128/IAI.70.3.1319-1325.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brassard J, Gottschalk M, Quessy S. Cloning and purification of the Streptococcus suis serotype 2 glyceraldehyde-3-phosphate dehydrogenase and its involvement as an adhesin. Vet Microbiol. 2004;102(1-2):87–94. doi: 10.1016/j.vetmic.2004.05.008. [DOI] [PubMed] [Google Scholar]
- Esgleas M, Li Y, Hancock MA, Harel J, Dubreuil JD, Gottschalk M. Isolation and characterization of alpha-enolase, a novel fibronectin-binding protein from Streptococcus suis. Microbiology. 2008;154(Pt 9):2668–2679. doi: 10.1099/mic.0.2008/017145-0. [DOI] [PubMed] [Google Scholar]
- Zhang A, Chen B, Mu X, Li R, Zheng P, Zhao Y, Chen H, Jin M. Identification and characterization of a novel protective antigen, Enolase of Streptococcus suis serotype 2. Vaccine. 2009;27(9):1348–1353. doi: 10.1016/j.vaccine.2008.12.047. [DOI] [PubMed] [Google Scholar]
- Haataja S, Tikkanen K, Hytonen J, Finne J. The Gal alpha 1-4 Gal-binding adhesin of Streptococcus suis, a gram-positive meningitis-associated bacterium. Adv Exp Med Biol. 1996;408:25–34. doi: 10.1007/978-1-4613-0415-9_3. [DOI] [PubMed] [Google Scholar]
- Haataja S, Tikkanen K, Liukkonen J, Francois-Gerard C, Finne J. Characterization of a novel bacterial adhesion specificity of Streptococcus suis recognizing blood group P receptor oligosaccharides. J Biol Chem. 1993;268(6):4311–4317. [PubMed] [Google Scholar]
- Haataja S, Tikkanen K, Nilsson U, Magnusson G, Karlsson KA, Finne J. Oligosaccharide-receptor interaction of the Gal alpha 1-4Gal binding adhesin of Streptococcus suis. Combining site architecture and characterization of two variant adhesin specificities. J Biol Chem. 1994;269(44):27466–27472. [PubMed] [Google Scholar]
- Tikkanen K, Haataja S, Francois-Gerard C, Finne J. Purification of a galactosyl-alpha 1-4-galactose-binding adhesin from the gram-positive meningitis-associated bacterium Streptococcus suis. J Biol Chem. 1995;270(48):28874–28878. doi: 10.1074/jbc.270.48.28874. [DOI] [PubMed] [Google Scholar]
- Tikkanen K, Haataja S, Finne J. The galactosyl-(alpha 1-4)-galactose-binding adhesin of Streptococcus suis: occurrence in strains of different hemagglutination activities and induction of opsonic antibodies. Infect Immun. 1996;64(9):3659–3665. doi: 10.1128/iai.64.9.3659-3665.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baums CG, Kaim U, Fulde M, Ramachandran G, Goethe R, Valentin-Weigand P. Identification of a novel virulence determinant with serum opacification activity in Streptococcus suis. Infect Immun. 2006;74(11):6154–6162. doi: 10.1128/IAI.00359-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang A, Mu X, Chen B, Liu C, Han L, Chen H, Jin M. Identification and characterization of IgA1 protease from Streptococcus suis. Vet Microbiol. 2010;140(1-2):171–175. doi: 10.1016/j.vetmic.2009.06.034. [DOI] [PubMed] [Google Scholar]
- Fittipaldi N, Sekizaki T, Takamatsu D, Harel J, Dominguez-Punaro L Mde, Von Aulock S, Draing C, Marois C, Kobisch M, Gottschalk M. D-alanylation of lipoteichoic acid contributes to the virulence of Streptococcus suis. Infect Immun. 2008;76(8):3587–3594. doi: 10.1128/IAI.01568-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fittipaldi N, Sekizaki T, Takamatsu D, Dominguez-Punaro L Mde, Harel J, Bui NK, Vollmer W, Gottschalk M. Significant contribution of the pgdA gene to the virulence of Streptococcus suis. Mol Microbiol. 2008;70(5):1120–1135. doi: 10.1111/j.1365-2958.2008.06463.x. [DOI] [PubMed] [Google Scholar]
- Li M, Wang C, Feng Y, Pan X, Cheng G, Wang J, Ge J, Zheng F, Cao M, Dong Y. et al. SalK/SalR, a two-component signal transduction system, is essential for full virulence of highly invasive Streptococcus suis serotype 2. PLoS ONE. 2008;3(5):e2080. doi: 10.1371/journal.pone.0002080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan X, Ge J, Li M, Wu B, Wang C, Wang J, Feng Y, Yin Z, Zheng F, Cheng G. et al. The orphan response regulator CovR: a globally negative modulator of virulence in Streptococcus suis serotype 2. J Bacteriol. 2009;191(8):2601–2612. doi: 10.1128/JB.01309-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye C, Zheng H, Zhang J, Jing H, Wang L, Xiong Y, Wang W, Zhou Z, Sun Q, Luo X. et al. Clinical, Experimental, and Genomic Differences between Intermediately Pathogenic, Highly Pathogenic, and Epidemic Streptococcus suis. J Infect Dis. 2009;199(1):97–107. doi: 10.1086/594370. [DOI] [PubMed] [Google Scholar]
- Vadeboncoeur N, Segura M, Al-Numani D, Vanier G, Gottschalk M. Pro-inflammatory cytokine and chemokine release by human brain microvascular endothelial cells stimulated by Streptococcus suis serotype 2. FEMS Immunol Med Microbiol. 2003;35(1):49–58. doi: 10.1111/j.1574-695X.2003.tb00648.x. [DOI] [PubMed] [Google Scholar]
- Segura M, Vanier G, Al-Numani D, Lacouture S, Olivier M, Gottschalk M. Proinflammatory cytokine and chemokine modulation by Streptococcus suis in a whole-blood culture system. FEMS Immunol Med Microbiol. 2006;47(1):92–106. doi: 10.1111/j.1574-695X.2006.00067.x. [DOI] [PubMed] [Google Scholar]
- Segura M, Stankova J, Gottschalk M. Heat-killed Streptococcus suis capsular type 2 strains stimulate tumor necrosis factor alpha and interleukin-6 production by murine macrophages. Infect Immun. 1999;67(9):4646–4654. doi: 10.1128/iai.67.9.4646-4654.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segura M, Vadeboncoeur N, Gottschalk M. CD14-dependent and -independent cytokine and chemokine production by human THP-1 monocytes stimulated by Streptococcus suis capsular type 2. Clin Exp Immunol. 2002;127(2):243–254. doi: 10.1046/j.1365-2249.2002.01768.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dominguez-Punaro MC, Segura M, Plante MM, Lacouture S, Rivest S, Gottschalk M. Streptococcus suis serotype 2, an important swine and human pathogen, induces strong systemic and cerebral inflammatory responses in a mouse model of infection. J Immunol. 2007;179(3):1842–1854. doi: 10.4049/jimmunol.179.3.1842. [DOI] [PubMed] [Google Scholar]
- Dominguez-Punaro L Mde, Segura M, Radzioch D, Rivest S, Gottschalk M. Comparison of the susceptibilities of C57BL/6 and A/J mouse strains to Streptococcus suis serotype 2 infection. Infect Immun. 2008;76(9):3901–3910. doi: 10.1128/IAI.00350-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Greeff A, Benga L, Wichgers PJ Schreur, Valentin-Weigand P, Rebel JM, Smith HE. Involvement of NF-kappaB and MAP-kinases in the transcriptional response of alveolar macrophages to Streptococcus suis. Vet Microbiol. 2009;141(1-2):59–67. doi: 10.1016/j.vetmic.2009.07.031. [DOI] [PubMed] [Google Scholar]
- Zhao SH, Kuhar D, Lunney JK, Dawson H, Guidry C, Uthe JJ, Bearson SM, Recknor J, Nettleton D, Tuggle CK. Gene expression profiling in Salmonella Choleraesuis-infected porcine lung using a long oligonucleotide microarray. Mamm Genome. 2006;17(7):777–789. doi: 10.1007/s00335-005-0155-3. [DOI] [PubMed] [Google Scholar]
- Chen H, Li C, Fang M, Zhu M, Li X, Zhou R, Li K, Zhao S. Understanding Haemophilus parasuis infection in porcine spleen through a transcriptomics approach. BMC Genomics. 2009;10:64. doi: 10.1186/1471-2164-10-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Poll T, Keogh CV, Guirao X, Buurman WA, Kopf M, Lowry SF. Interleukin-6 gene-deficient mice show impaired defense against pneumococcal pneumonia. J Infect Dis. 1997;176(2):439–444. doi: 10.1086/514062. [DOI] [PubMed] [Google Scholar]
- Norrby-Teglund A, Pauksens K, Norgren M, Holm SE. Correlation between serum TNF alpha and IL6 levels and severity of group A streptococcal infections. Scand J Infect Dis. 1995;27(2):125–130. doi: 10.3109/00365549509018991. [DOI] [PubMed] [Google Scholar]
- Foell D, Wittkowski H, Vogl T, Roth J. S100 proteins expressed in phagocytes: a novel group of damage-associated molecular pattern molecules. J Leukoc Biol. 2007;81(1):28–37. doi: 10.1189/jlb.0306170. [DOI] [PubMed] [Google Scholar]
- Hojo K, Tamura A, Mizoguchi C, Kato D, Ohshima T, Maeda N. Predominant bacteria recovered from a periodontitis site in a hamster model raised by silk-ligature with Porphyromonas gingivalis infection. Biosci Biotechnol Biochem. 2008;72(5):1348–1351. doi: 10.1271/bbb.70653. [DOI] [PubMed] [Google Scholar]
- Patel L, Buckels AC, Kinghorn IJ, Murdock PR, Holbrook JD, Plumpton C, Macphee CH, Smith SA. Resistin is expressed in human macrophages and directly regulated by PPAR gamma activators. Biochem Biophys Res Commun. 2003;300(2):472–476. doi: 10.1016/S0006-291X(02)02841-3. [DOI] [PubMed] [Google Scholar]
- Bokarewa M, Nagaev I, Dahlberg L, Smith U, Tarkowski A. Resistin, an adipokine with potent proinflammatory properties. J Immunol. 2005;174(9):5789–5795. doi: 10.4049/jimmunol.174.9.5789. [DOI] [PubMed] [Google Scholar]
- Ward PP, Conneely OM. Lactoferrin: role in iron homeostasis and host defense against microbial infection. Biometals. 2004;17(3):203–208. doi: 10.1023/B:BIOM.0000027693.60932.26. [DOI] [PubMed] [Google Scholar]
- Knura-Deszczk S, Lipperheide C, Petersen B, Jobert JL, Berthelot-Herault F, Kobisch M, Madec F. Plasma haptoglobin concentration in swine after challenge with Streptococcus suis. J Vet Med B Infect Dis Vet Public Health. 2002;49(5):240–244. doi: 10.1046/j.1439-0450.2002.00556.x. [DOI] [PubMed] [Google Scholar]
- Thorn CF, Lu ZY, Whitehead AS. Tissue-specific regulation of the human acute-phase serum amyloid A genes, SAA1 and SAA2, by glucocorticoids in hepatic and epithelial cells. Eur J Immunol. 2003;33(9):2630–2639. doi: 10.1002/eji.200323985. [DOI] [PubMed] [Google Scholar]
- Baumann H, Gauldie J. The acute phase response. Immunol Today. 1994;15(2):74–80. doi: 10.1016/0167-5699(94)90137-6. [DOI] [PubMed] [Google Scholar]
- Sorensen NS, Tegtmeier C, Andresen LO, Pineiro M, Toussaint MJ, Campbell FM, Lampreave F, Heegaard PM. The porcine acute phase protein response to acute clinical and subclinical experimental infection with Streptococcus suis. Vet Immunol Immunopathol. 2006;113(1-2):157–168. doi: 10.1016/j.vetimm.2006.04.008. [DOI] [PubMed] [Google Scholar]
- Rikitake Y, Takai Y. Interactions of the cell adhesion molecule nectin with transmembrane and peripheral membrane proteins for pleiotropic functions. Cell Mol Life Sci. 2008;65(2):253–263. doi: 10.1007/s00018-007-7290-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Numani D, Segura M, Dore M, Gottschalk M. Up-regulation of ICAM-1, CD11a/CD18 and CD11c/CD18 on human THP-1 monocytes stimulated by Streptococcus suis serotype 2. Clin Exp Immunol. 2003;133(1):67–77. doi: 10.1046/j.1365-2249.2003.02189.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wight TN. Versican: a versatile extracellular matrix proteoglycan in cell biology. Curr Opin Cell Biol. 2002;14(5):617–623. doi: 10.1016/S0955-0674(02)00375-7. [DOI] [PubMed] [Google Scholar]
- Wang W, Xu GL, Jia WD, Ma JL, Li JS, Ge YS, Ren WH, Yu JH, Liu WB. Ligation of TLR2 by versican: a link between inflammation and metastasis. Arch Med Res. 2009;40(4):321–323. doi: 10.1016/j.arcmed.2009.04.005. [DOI] [PubMed] [Google Scholar]
- Simantov R, Silverstein RL. CD36: a critical anti-angiogenic receptor. Front Biosci. 2003;8:s874–882. doi: 10.2741/1168. [DOI] [PubMed] [Google Scholar]
- Nakache M, Berg EL, Streeter PR, Butcher EC. The mucosal vascular addressin is a tissue-specific endothelial cell adhesion molecule for circulating lymphocytes. Nature. 1989;337(6203):179–181. doi: 10.1038/337179a0. [DOI] [PubMed] [Google Scholar]
- Tilley SL, Coffman TM, Koller BH. Mixed messages: modulation of inflammation and immune responses by prostaglandins and thromboxanes. J Clin Invest. 2001;108(1):15–23. doi: 10.1172/JCI13416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jobin MC, Gottschalk M, Grenier D. Upregulation of prostaglandin E2 and matrix metalloproteinase 9 production by human macrophage-like cells: synergistic effect of capsular material and cell wall from Streptococcus suis. Microb Pathog. 2006;40(1):29–34. doi: 10.1016/j.micpath.2005.10.003. [DOI] [PubMed] [Google Scholar]
- Graveline R, Segura M, Radzioch D, Gottschalk M. TLR2-dependent recognition of Streptococcus suis is modulated by the presence of capsular polysaccharide which modifies macrophage responsiveness. Int Immunol. 2007;19(4):375–389. doi: 10.1093/intimm/dxm003. [DOI] [PubMed] [Google Scholar]
- Schreur PJ, Rebel JM, Smits MA, van Putten JP, Smith HE. Differential activation of the Toll-like receptor 2/6 complex by lipoproteins of Streptococcus suis serotypes 2 and 9. Vet Microbiol. pp. 363–370. [DOI] [PubMed]
- Baums CG, Valentin-Weigand P. Surface-associated and secreted factors of Streptococcus suis in epidemiology, pathogenesis and vaccine development. Anim Health Res Rev. 2009;10(1):65–83. doi: 10.1017/S146625230999003X. [DOI] [PubMed] [Google Scholar]
- Feng Y, Zhang H, Ma Y, Gao GF. Uncovering newly emerging variants of Streptococcus suis, an important zoonotic agent. Trends Microbiol. 2010;18(3):124–31. doi: 10.1016/j.tim.2009.12.003. [DOI] [PubMed] [Google Scholar]
- Zhang Q, Peng H, Gao F, Liu Y, Cheng H, Thompson J, Gao GF. Structural insight into the catalytic mechanism of gluconate 5-dehydrogenase from Streptococcus suis: Crystal structures of the substrate-free and quaternary complex enzymes. Protein Sci. 2009;18(2):294–303. doi: 10.1002/pro.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Q, Gao F, Peng H, Cheng H, Liu Y, Tang J, Thompson J, Wei G, Zhang J, Du Y. et al. Crystal structures of Streptococcus suis mannonate dehydratase (ManD) and its complex with substrate: genetic and biochemical evidence for a catalytic mechanism. J Bacteriol. 2009;191(18):5832–7. doi: 10.1128/JB.00599-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldmann O, von Kockritz-Blickwede M, Holtje C, Chhatwal GS, Geffers R, Medina E. Transcriptome analysis of murine macrophages in response to infection with Streptococcus pyogenes reveals an unusual activation program. Infect Immun. 2007;75(8):4148–4157. doi: 10.1128/IAI.00181-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akira S, Uematsu S, Takeuchi O. Pathogen recognition and innate immunity. Cell. 2006;124(4):783–801. doi: 10.1016/j.cell.2006.02.015. [DOI] [PubMed] [Google Scholar]
- Segura M, Gottschalk M. Streptococcus suis interactions with the murine macrophage cell line J774: adhesion and cytotoxicity. Infect Immun. 2002;70(8):4312–4322. doi: 10.1128/IAI.70.8.4312-4322.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segura M, Gottschalk M, Olivier M. Encapsulated Streptococcus suis inhibits activation of signaling pathways involved in phagocytosis. Infect Immun. 2004;72(9):5322–5330. doi: 10.1128/IAI.72.9.5322-5330.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu Q, Liu P, Yu Z, Zhao G, Li J, Teng L, Zhou M, Bei W, Chen H, Jin M. Identification of a cell wall-associated subtilisin-like serine protease involved in the pathogenesis of Streptococcus suis serotype 2. Microb Pathog. 2010;48(3-4):103–9. doi: 10.1016/j.micpath.2009.11.005. [DOI] [PubMed] [Google Scholar]
- Tan C, Liu M, Jin M, Liu J, Chen Y, Wu T, Fu T, Bei W, Chen H. The key virulence-associated genes of Streptococcus suis type 2 are upregulated and differentially expressed in vivo. FEMS Microbiol Lett. 2008;278(1):108–114. doi: 10.1111/j.1574-6968.2007.00980.x. [DOI] [PubMed] [Google Scholar]
- Zhang A, Chen B, Li R, Mu X, Han L, Zhou H, Chen H, Meilin J. Identification of a surface protective antigen, HP0197 of Streptococcus suis serotype 2. Vaccine. 2009;27(38):5209–5213. doi: 10.1016/j.vaccine.2009.06.074. [DOI] [PubMed] [Google Scholar]
- Gottschalk M, Segura M. The pathogenesis of the meningitis caused by Streptococcus suis: the unresolved questions. Vet Microbiol. 2000;76(3):259–272. doi: 10.1016/S0378-1135(00)00250-9. [DOI] [PubMed] [Google Scholar]
- Vanier G, Segura M, Friedl P, Lacouture S, Gottschalk M. Invasion of porcine brain microvascular endothelial cells by Streptococcus suis serotype 2. Infect Immun. 2004;72(3):1441–1449. doi: 10.1128/IAI.72.3.1441-1449.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang A, Xie C, Chen H, Jin M. Identification of immunogenic cell wall-associated proteins of Streptococcus suis serotype 2. Proteomics. 2008;8(17):3506–3515. doi: 10.1002/pmic.200800007. [DOI] [PubMed] [Google Scholar]
- Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25(4):402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Spleen transcriptome analysis following S. suis infection using the Affymetrix Porcine Genechip. Data of each probe is from the three piglets of the control group (NC-1P, NC-2P, NC-3P), the WT group (WT-1P, WT-2P, WT-3P) and the △HP0197 group (M97-1P, M97-2P, M97-3P). "P", present; "A", absent; "M", marginal; select while Count (P) ≥ 2 in two groups. Totally, 15,757, 14,992 and 15,487 probesets were detected expression in the control group, the WT group and △HP0197 group respectively.
transcripts expressed in porcine spleen following S. suis (WT) infection. "FC", Fold change, gene expression level following WT infection compared to the control. "≥2" represents up regulation, " < 1" represents down regulation. "q-value", significance level of differential expression for a particular gene. "Gene description", top informative BLASTX hit.
Differentially expressed transcripts in porcine spleen following S. suis (WT) infection (q < 10%, FC≥2). 120 transcripts (row 5-124) were significantly up-regulated, and 132 (row 125-256) were significantly down-regulated, "FC", Fold change, gene expression level following WT infection compared to the control.


